Abstract
Despite interest in unequal maternal and child health, previous research has not focused on educational differences in anxiety and depressive symptoms during pregnancy, although they threaten maternal and child wellbeing. Using the prospective FinnBrain Cohort Study data on 2763 pregnant women over the three pregnancy trimesters and Finnish register data, we estimated multilevel regressions to describe educational differences in prenatal anxiety and depressive symptoms and to analyze whether they can be explained by socioeconomic background, parental mental disorders and adverse experiences during childhood. Prenatal anxiety was measured by the Symptom Checklist (SCL-90-anxiety subscale) and depressive symptoms by the Edinburgh Postnatal Depression Scale (EPDS). The results showed less anxiety and depressive symptoms among more educated pregnant women. In accounting for the educational differences, we found support for both the social selection and the social causation perspectives. Adverse childhood experiences partly explained the educational differences, highlighting the role of an undisturbed childhood environment in prenatal mental health disparities. Results from the regression models as well as sensitivity analyses also suggested that education is likely to buffer against prenatal distress.
Keywords: Anxiety, Depression, Pregnancy, Education, Childhood adversity, Multilevel modeling
Highlights
-
•
Higher education predicted lower anxiety and depressive symptoms during pregnancy.
-
•
Educational differences were not attributable to childhood SES or parental mental health.
-
•
Adverse childhood experiences partly explained the educational differences.
-
•
Sensitivity analysis suggested education to buffer against prenatal distress.
Introduction
Anxiety and depressive symptoms are frequent during pregnancy. Anxiety symptoms affect 15%–25% of expecting mothers (Dennis et al., 2017, Fawcett et al., 2019), the prevalence for depression being 12–14% (Rubertsson et al., 2005; Woody et al., 2017). Prenatal anxiety and depression have been linked to adverse maternal and child outcomes, including postpartum depression (Beck, 2011; Lee et al., 2007; Robertson et al., 2004), compromised mother-child interaction and bonding (Dubber et al., 2015; Misri & Kendrick, 2008), low birth weight and preterm birth (Dunkel Schetter & Tanner, 2012), alterations in brain development (e.g. Buss et al., 2012), and an elevated risk of psychiatric problems in the offspring (e.g. Lahti et al., 2017). Despite their high prevalence and negative consequences, they often go under-diagnosed and -treated (Biaggi et al., 2016; Marcus, 2009).
Previous research has identified several risk factors for elevated and clinically significant levels of prenatal anxiety and depressive symptoms, including a history of anxiety and depression, low social support, and experience of life stressors (Biaggi et al., 2016; Gelaye et al., 2016; Lancaster et al., 2010). Given the well-documented negative relationships between education and anxiety or depression in the general population (Fryers et al., 2003; Pinto-Meza et al., 2013), results regarding educational differences in the prenatal period are surprisingly contradictory, ranging from weak negative associations to even positive ones (cf. Biaggi et al., 2016; Gelaye et al., 2016; Lancaster et al., 2010; Underwood et al., 2016). However, many of these studies have not focused explicitly on educational differences, and education has been analyzed together with several other factors, which can be on the causal pathway from education to anxiety or depression. These studies may thus have drawn premature conclusions of educational differences in prenatal distress.
In this study, we analyze educational differences in depressive and anxiety (distress) symptoms during pregnancy in a Finnish birth cohort. We use measures of anxiety and depressive symptoms validated in pregnant populations — the Edinburgh Postnatal Depression Scale (EPDS) (Cox et al., 1987) and the anxiety subscale of the Symptom Checklist −90 (SCL-90) (Derogatis & Cleary, 1977). Our study has two objectives. Given the contradictory results from previous studies, our first objective is to document the scope of educational differences in prenatal anxiety and depressive symptoms. Second, we analyze whether any educational differences are likely to be attributed to social causation (effect of education on prenatal distress) or to social selection (underlying factors that are related to both education and prenatal distress). We do so, first, by controlling for socioeconomic background, parents’ psychiatric problems, and adverse experiences during childhood and adolescence, and second, by performing a sensitivity analysis (VanderWeele & Ding, 2017) of the remaining association. Our analyses contribute to understanding inequality in prenatal stress as well as the broader literature on disparities in mental health.
Prenatal anxiety and depression
Anxiety and depression are the two most common psychiatric problems during pregnancy (Skouteris et al., 2009). They differ from pregnancy-related concerns, such as fears regarding delivery and the baby's health (Dunkel Schetter, 2011). Although anxiety and depression are more common during pregnancy than in the postpartum period, the postpartum symptoms have received more scholarly and clinical attention (Biaggi et al., 2016; Dennis et al., 2017; Fawcett et al., 2019; Gelaye et al., 2016). Sub-clinical anxiety and depressive symptoms often go unnoticed, although the mechanisms through which these phenomena are harmful to the mother and the fetus are likely to operate on a continuum. Symptomatology without a medical diagnosis may thus have adverse effects, especially at the population level.
Prenatal depression has received more scholarly and clinical attention than anxiety (Dennis et al., 2017). Despite their high comorbidity (Skouteris et al., 2009), anxiety and depression have partly independent effects on mothers' and children's well-being (Dennis et al., 2017) and partly independent trajectories over pregnancy both in prevalence rates and in the intra- and inter-individual symptom levels (BIaggi et al., 2016; Dennis et al., 2017; Gelaye et al., 2016; Korja et al., 2018; Lee et al., 2007). Research on non-pregnant populations suggests that comorbid anxiety and depression show more persistence than either syndrome alone (Merikangas et al., 2003). Long-lasting distress may have particularly negative effects on the child (e.g. Entringer et al., 2017).
A previous history of anxiety and depression are, unsurprisingly, strong predictors of these symptoms during pregnancy (e.g. Littleton et al., 2007). Yet it is not uncommon for the first episode of anxiety or depression to occur during pregnancy (Räisänen et al., 2014). Pregnancy is a major life course event, which can trigger anxiety and depression due to the associated hormonal, psychological and social changes (Dunkel Schetter, 2011; Gelaye et al., 2016), even though pregnancy is often associated with increased positive emotion (Myrskylä & Margolis, 2014). Often-reported risk factors of anxiety and depression during pregnancy include lack of social support, life stressors, poverty, low self-esteem, personality factors (e.g., low dispositional optimism), and experiences of abuse and other childhood adversities (Biaggi et al., 2016; Dunkel Schetter, 2011; Gelaye et al., 2016; Lancaster et al., 2010; Littleton et al., 2007; Underwood et al., 2016). In particular, the combined effects of biological risk and adverse social environment at different life stages are known to increase an individual's risk for diseases in general (Power & Hertzmant, 1997), which is likely to apply to prenatal distress symptoms as well.
Educational differences in prenatal anxiety and depression
Systematic reviews and meta-analyses have led to inconsistent conclusions of educational differences in prenatal anxiety and depression, many studies finding negative associations between education and distress, while others find no associations or even positive ones (Biaggi et al., 2016; Gelaye et al., 2016; Lancaster et al., 2010). However, these systematic reviews and meta-analyses are based on studies on general risk factors of prenatal anxiety and depression and included education together with several other variables, which may mediate the effect of education and thus underestimate educational differences. Other studies have been based on selective, non-representative samples.
The equivocal findings of the association between education and anxiety and depression among pregnant women stand in contrast to consistently reported educational and other disparities in anxiety and depression in the general population (Allen et al., 2014; Costello et al., 2003; Dohrenwend et al., 1992; Fryers et al., 2003; Muntaner et al., 2004; Reiss, 2013). Education is often considered the best overall indicator of socioeconomic resources, as it causally precedes occupational position, income, and other economic resources (Galobardes et al., 2006). Education is also regarded as an SES (socioeconomic status) indicator with health effects that are in favour of the social causation interpretation (Kröger et al., 2015). Education remains relatively stable over the adult life course, and entry into parenthood happens relatively late in Finland, at around the age of 30 (Statistics Finland, 2017), by which education is usually completed.
Social causation explanations
Explanations for educational disparities in mental health can be classified into the social causation and social selection perspectives (Costello et al., 2003; Dohrenwend, 2000; Dohrenwend et al., 1992; Miech et al., 1999; Muntaner et al., 2004). The former maintains that higher education improves mental health. It can do so by reducing life events and conditions that hamper mental health, and by providing resources that foster resilience in the face of them. Education improves economic security and reduces negative life events, both of which improve mental health in the general population (Allen et al., 2014; Haushofer & Fehr, 2014; Pulkki-Råback et al., 2012; Suokas et al., 2019), also during pregnancy (Biaggi et al., 2016; Gelaye et al., 2016; Lancaster et al., 2010; Littleton et al., 2007; Underwood et al., 2016). Additionally, lower-educated women are likely to have worse health status and habits and higher risk for health problems during pregnancy (Bouthoorn et al., 2015; Härkönen et al., 2018; Silva et al., 2008), which can also contribute to anxiety and depression (Biaggi et al., 2016; Gelaye et al., 2016; Lancaster et al., 2010).
In addition to reducing exposure to stressors that increase prenatal distress symptoms, education can improve coping in the face of major life changes, such as pregnancy (cf. Dohrenwend, 2000). Education can improve general psychological health through learned effectiveness, a sense of control, and knowledge and skills, which are important for taking care of one's health (Mirowsky & Ross, 2005; Ross & Mirowsky, 1999) and which can reduce depressive and anxiety symptoms over the transition to parenthood (Keeton et al., 2008).
Highly educated women are more likely to have highly educated partners (Mäenpää, 2014) and receive more support from their partners and the broader social environment (Taylor & Seeman, 1999). Social support facilitates coping and has been consistently found to predict fewer distress symptoms during pregnancy (Biaggi et al., 2016; Gelaye et al., 2016; Lancaster et al., 2010; Littleton et al., 2007; Underwood et al., 2016).
Social selection explanations
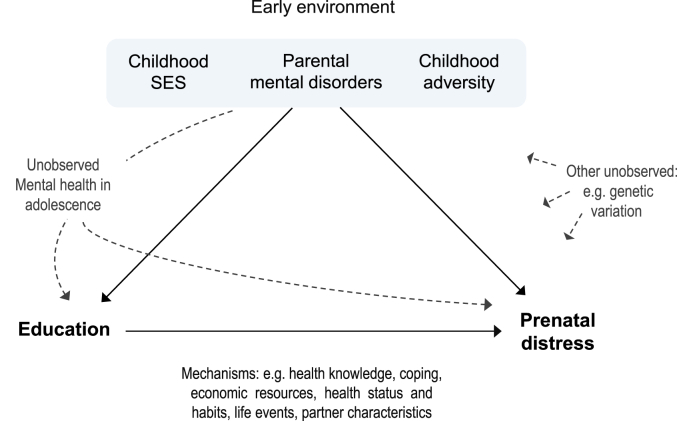
Social selection perspectives to educational disparities in anxiety and depression hold that the associations between education and mental health disorders result either from common underlying causes or causation from poor mental health to education. The first perspective posits that the origins of educational disparities in adulthood mental health may lie in an individual's childhood circumstances (Fig. 1). It is well known that socioeconomic background – including parental education and class, family structure, and economic conditions – shapes children's educational attainment (e.g., Breen & Jonsson, 2005; Erola et al., 2016). Children from low socioeconomic positions are two to three times more likely to develop mental health problems (Reiss, 2013), including anxiety and depressive disorders (Johnson et al., 1999). Economic stressors in the childhood home have been linked to non-optimal parenting styles (via psychological distress), through which they may weaken children's self-efficacy, cognitive and emotional wellbeing, and thereby also interfere with educational attainment (Devenish et al., 2017; Masarik & Conger, 2017; Whitbeck et al., 1997).
Fig. 1.
The applied causal framework of educational differences in prenatal distress.
The association between education and prenatal distress symptoms can also be shaped by negative childhood experiences outside the socioeconomic domain. Parental mental health problems predict offspring's health and cognitive development, partly mediated by negative and dysfunctional parenting (Kiernan & Huerta, 2008; Kurstjens & Wolke, 2001; Smith, 2004). Low parental emotional wellbeing, parental depression and poorer parenting practices are pathways through which socioeconomic adversity can trigger mental health problems in children (Bøe et al., 2014; Devenish et al., 2017). Furthermore, a history of childhood trauma, caused by exposure to physical, sexual, and/or emotional abuse, or emotional and/or physical neglect (Bernstein et al., 1994), is a strong predictor of anxiety and depression in adulthood (Heim et al., 2008; Kessler et al., 2010; Matthews et al., 2010; Repetti et al., 2002; Teicher & Samson, 2014), also during pregnancy (Biaggi et al., 2016). Childhood maltreatment has been consistently related to lower school performance and deficits in cognitive development and non-cognitive skills that foster educational attainment (Currie & Widom, 2010; Gilbert et al., 2009; Korgaonkar et al., 2013; Lupien et al., 2009; Matthews et al., 2010; Pechtel & Pizzagalli, 2011), with a few exceptions, where social, parental, or individual characteristics largely explained these links (Boden et al., 2007). Moreover, a physical environment, including prenatal and postnatal environmental toxins (e.g., alcohol, lead) and housing, may impact both cognitive and socioemotional development (Evans, 2006; Ferguson et al., 2013; Williams & Ross, 2007), and lead to lower education and poorer mental health.
Different dimensions of negative childhood circumstances are correlated, challenging the separation of their independent risks. In particular, the cumulative adversities experienced from childhood to adulthood appear to contribute to the socioeconomic inequalities in depression and anxiety, and thus both environmental influences from childhood as well as adult life short-term factors are reflected in the gradient (Muntaner et al., 2004; Power et al., 2002). Unmeasured (inherited) genetic dispositions can further add to the environmental risks or explain the links between childhood circumstances and later outcomes (Fig. 1). Moreover, educational disparities may result from earlier mental health disorders that have independently or cumulatively with other risk factors affected final educational attainment as well as mental health in pregnancy. Previous research has generally reported that, for example, attention and conduct problems are more detrimental for educational attainment than anxiety and depression (Evensen et al., 2016; Miech et al., 1999), the negative effects of the latter on education ranging from zero to moderate (Evensen et al., 2016; Fletcher, 2010).
Summing up, previous findings on educational differences in prenatal anxiety and depressive symptoms have been contradictory, potentially because earlier studies have had other objectives than a focus on educational differences. (1) Our first objective is to document the scope of educational differences in prenatal anxiety and depressive symptoms. (2) Our second objective is to assess whether the differences are primarily attributable to social causation or social selection, by estimating the role of socioeconomic background, parents’ psychiatric problems, and adverse experiences during childhood and adolescence, and by assessing the likelihood of unmeasured confounding to explain the remaining associations.
Methods
Study sample
We used data from the prospective FinnBrain Cohort Study, an ongoing study on pregnancy and early life outcomes, conducted at the University of Turku, Finland (Karlsson et al., 2018). The original sample consisted of 3808 pregnant women and their partners living in South-Western Finland. Recruitment took place at a free-of-charge ultrasound visit at gestational week 12 between December 2011 and April 2015. The questionnaire data were collected by online or paper self-report questionnaires, filled at home and linked to register data on socioeconomic variables (educational level and childhood SES) from Statistics Finland for those who gave consent (98%). The population registers provided by Statistics Finland are reliable and high-quality administrative data. We excluded 97 women born outside Finland due to missing register information on their childhood environment. 569 women who did not fill in any perinatal questionnaires were also excluded. After excluding another 374 individuals who lacked information on the explanatory variables, the analytical sample consisted of 2763 pregnant mothers. The study has been approved by the Ethics Committee of the Hospital District of Southwest Finland (decision number 57/180/2011).
The women in the final sample were 17–39 years old at childbirth, and 29.9 years on average (Table 1), similar to the mean age of all women at childbirth (30.8 years) in Finland in 2016 (Statistics Finland, 2017). Women were educated mostly to the tertiary (59.1%) or secondary vocational (21.9%) level and most often expecting their first child (51.1%).
Table 1.
Descriptive statistics for the analytical sample by educational level. Means, standard deviations (SD), and percentages.
| Education |
||||||
|---|---|---|---|---|---|---|
| Primary | Secondary vocational | Secondary general | Tertiary | Total | p | |
| N | 73 | 606 | 450 | 1,634 | 2,763 | |
| % | 2.7 | 21.9 | 16.3 | 59.1 | 100.0 | |
| Mean values (SD) | ||||||
| Depressiona | 6.4 | 5.9 | 5.2 | 4.5 | 5.0 | *** |
| (4.5) | (4.2) | (4.1) | (3.9) | (4.0) | ||
| Anxietya | 5.4 | 4.2 | 3.6 | 3.1 | 3.4 | *** |
| (5.2) | (4.6) | (4.1) | (3.7) | (4.0) | ||
| Childhood adversityb | 19.0 | 11.8 | 10.7 | 8.5 | 9.8 | *** |
| (17.0) | (12.3) | (11.3) | (9.3) | (10.8) | ||
| Age at childbirth | 26.4 | 28.0 | 28.8 | 31.1 | 29.9 | *** |
| (5.2) | (4.5) | (4.0) | (3.3) | (4.1) | ||
| Percentage values | ||||||
| Probable clinical depressionc | 20.6 | 14.4 | 10.5 | 8.2 | 10.3 | *** |
| Probable clinical anxietyc | 31.5 | 21.1 | 14.9 | 11.5 | 14.7 | *** |
| Childhood SES | *** | |||||
| Upper level employee | 8.2 | 13.5 | 22.2 | 36.1 | 28.1 | |
| Lower level employee | 49.3 | 45.9 | 48.7 | 39.8 | 42.8 | |
| Manual worker | 27.4 | 34.3 | 22.7 | 18.3 | 22.8 | |
| Other/not classifiedd | 15.1 | 6.3 | 6.4 | 5.9 | 6.3 | |
| Parents' mental disorders | *** | |||||
| No disorders | 53.4 | 61.1 | 65.8 | 65.5 | 64.2 | |
| Mother had | 24.7 | 27.1 | 22.9 | 21.1 | 22.8 | |
| Father had | 21.9 | 11.9 | 11.3 | 13.5 | 13.0 | |
| First child (yes) | 37.0 | 51.0 | 54.2 | 51.0 | 51.1 | *** |
*p < 0.05, **p < 0.01, ***p < 0.001.
Depressive symptoms [sample range 0–30], anxiety symptoms [sample range 0–40] during trimesters 1–3.
The trauma and distress (TADS) score [sample range 0–89].
Depression: ≥13 EPDS points, anxiety: ≥10 SCL-90 points; at least once in pregnancy.
Not classified, never worked, or unemployed.
Dependent variables: prenatal anxiety and depressive symptoms
We measured prenatal anxiety and depressive symptoms using two commonly used measures, the anxiety subscale of the Symptom Checklist −90 (SCL-90) (Derogatis & Cleary, 1977) and the Edinburgh Postnatal Depression Scale (EPDS) (Cox et al., 1987). Both have been validated for pregnant women in general, and in the FinnBrain cohort (Korja et al., 2018; Rubertsson et al., 2011).
SCL-90 is one of the most widely used measures of psychological distress in clinical practice and research. The anxiety subscale was designed to assess current symptom status, state anxiety, and it is regarded as a consistent and reliable measure (Holi, 2003). The scale includes 10 items with an item score range of 0–4 and a theoretical range of 0–40, measuring trembling, sudden fright without reason, insecurity, heart palpitations, tension/agitation, bouts of fear or panic, restlessness that prevents sitting still, common things feeling weird and absurd, feeling of being pressured, and nervousness/inner restlessness.
EPDS has been identified as the best screening tool for measuring both minor and major prenatal depression, and it excludes somatic symptoms of depression that are normal during pregnancy, such as fatigue (Nast et al., 2013; Rubertsson et al., 2011). The scale consists of 10 questions with an item score of 0–3 and a theoretical range of 0–30, measuring ability to laugh, to be amused, and to feel positive about forthcoming events, self-accusation, irrelevant fear/distress, the feeling of growing burden, sadness, sleep disturbance, tearfulness, and thoughts of self-harm.
Anxiety and depressive symptoms were measured using self-reported questionnaires at each pregnancy trimester at gestational weeks 14 (T1), 24 (T2), and 34 (T3). Due to intra-individual variation in the symptoms as well as measurement error, repeated prospective measures of anxiety and depressive symptoms are better measures of distress during pregnancy than single or retrospective measures (Biaggi et al., 2016; Entringer et al., 2017). Anxiety and depressive symptoms were moderately correlated in this sample ( = 0.64, p < 0.001).
We used SCL-90 anxiety and EPDS scores both as continuous and dichotomized variables. Continuous measures are common screening tools in non-patient populations (Dunkel Schetter & Tanner, 2012), and produce more robust associations between mental health and socioeconomic status than dichotomous classifications (e.g. Miech et al., 1999). On the other hand, clinically significant levels of anxiety and depressive symptoms are of practical importance. For dichotomization, we applied validated cut-off points: ≥ 13 points for EPDS (Matthey et al., 2006; Rubertsson et al., 2011) and ≥10 points for SCL-90 (Karlsson et al., 2018).
Missing item values in anxiety and depressive symptom measurements at each time point were imputed by the individual mean of available responses, if a maximum of three items out of ten were missing. The number of persons with imputed values (% of the analytical sample) for SCL-90 anxiety were T1: 93 (3.4), T2: 68 (2.7), T3: 54 (2.4), and for EPDS T1: 64 (2.3), T2: 68 (2.9), T3: 46 (2.1). Attrition analyses showed that lower-educated and more depressed women had a higher propensity to discontinue the study during pregnancy, with the total number of withdrawals being 310 families (Karlsson et al., 2018). Resulting from the overrepresentation of higher-educated and less symptomatic women, tests on the educational differences in prenatal distress symptoms were conservative.
Independent variables
The main independent variable, mother's educational level, measures the last completed educational degree before childbirth, following the International Standard Classification of Education (ISCED) 2011 (UNESCO, 2012). The variable was re-coded to primary, vocational secondary, general secondary (including combined vocational and academic secondary degrees) and tertiary (university and post-secondary vocational degrees) levels (Table 1). Information on education came from the registers, or in the case of missing data, from the FinnBrain questionnaires.
We included three potential confounding variables in the analysis. Childhood SES was measured using register data on the pregnant mother's childhood household's reference person's occupational class and used Statistics Finland's classification to upper level employees, lower level employees, manual workers and others/not classified. Parents' psychiatric problems (i.e. mental disorders) were based on the woman's report on whether her mother or father had depression, anxiety disorder, substance use disorder, schizophrenia or other psychosis, or other psychiatric problems, when she was 0–6, 7–12, and/or 13–18 years old.
Childhood adversity was measured by using the Trauma and Distress Scale (TADS), which is a valid and reliable instrument for assessing retrospectively reported childhood maltreatment (Salokangas et al., 2016). TADS is a five-domain measure evaluating how often the mother experienced emotional neglect, emotional abuse, physical neglect, physical abuse or sexual abuse in her childhood. We used the sum of all five domain scores at different stages of childhood (at ages 0–6, 7–12, and/or 13–18) as a continuous variable [theoretical range 0–268, sample range 0–89], to measure both early traumatization as well as its duration. The TADS score was centered at its mean in the regression analysis.
To avoid overadjustment bias caused by controlling for mediating variables (Schisterman et al., 2009), we did not adjust for age of the mother or the number of children, as these are predicted by the mother's education.
Analytical strategy
First, we produced descriptive results on the mean levels of anxiety and depressive symptoms as well as of clinically significant level prevalences by education at each pregnancy trimester. Second, we performed simultaneous equations estimation of the two outcomes in a multilevel analysis framework, which acknowledges the co-morbidity between the symptoms, while analyzing them as separate outcomes. Our model is written as
| (1) |
and are the depressive and anxiety symptom scores, respectively, for mother i at measurement t. are the measurement points, are the independent variables, and are the coefficients for the fixed effects to be estimated for the two outcomes l, anxiety (a) and depression (d), respectively. is a shared individual-level random effect for both of the outcomes, and it can be interpreted as the individual's fixed (during the pregnancy) propensity for the two distress symptoms. and are crossed random coefficients nested within individuals. are two random coefficients of individual-level deviations in anxiety (a) and depressive symptom (d) scores from . They capture individual differences in symptomatology of distress as well as differences in measurement. are two random coefficients that indicate within-individual variation in the outcomes over the three trimesters. are residual errors for the two outcomes that capture random variance as well as measurement error. The variances of , and for the two outcomes l are constrained to be equal. The model was estimated as a four-level multilevel model.
The primary purpose of the regression models was to analyze whether educational differences in prenatal distress could be attributable to social selection by socioeconomic background, parents’ mental health problems, and adverse experiences in childhood and adolescence. This was done by a sequence of four models, where the empty model with no covariates was estimated first, and the covariates were entered in the above order. Linear models were estimated both for the continuous (symptom scores) and binary (clinically relevant levels) outcomes. For the latter, the models were (multilevel) linear probability models, in which the coefficients tell the change in the outcome variable on the percentage point scale.
Next to the coefficients of the independent variables, we were interested in the stability in distress symptoms over the pregnancy. We calculated two intraclass correlations (ICC) (cf. Rabe-Hesketh & Skrondal, 2012, pp. 392–393). The first was the symptom-specific ICC, which estimated the within-individual correlation between trimesters in a specific outcome (anxiety or depressive symptoms) and was calculated without scripts as
| (2) |
The second was the general distress ICC, which estimates the within-individual correlation between trimesters in the overall propensity for anxiety or depressive symptoms. It is given by
| (3) |
In addition, we analyzed whether the distress trajectories vary systematically by education. For this, we first calculated interactions between education and trimester, after which we ran the Likelihood ratio -tests.
Finally, we performed a postestimation sensitivity analysis using E-values (VanderWeele & Ding, 2017). The E-value provides a single estimate of how strongly the confounder should be associated with both the exposure (education) and the outcome (anxiety or depressive symptoms) to reduce the association between the two to zero or to statistical non-significance (at the 5% level). By providing a single measure of association with both the exposure and the outcome, the E-value avoids potentially arbitrary decisions for choosing the values for these associations. The E-value is expressed on the risk ratio (RR) scale, which is a natural scale for assessing confounding by a binary unmeasured confounder on a binary outcome. It is more difficult to interpret for the continuous measures of prenatal distress, and we converted it back to standardized effect sizes for continuous outcomes (cf. VanderWeele & Ding, 2017).
Results
Descriptive results
The women reported rather low anxiety and depressive symptom levels (Table 2), in line with results concerning other rich countries (Dunkel Schetter & Tanner, 2012; Fawcett et al., 2019; Woody et al., 2017). 14.7% of the women showed clinically significant levels of anxiety and 10.3% had clinically significant depressive symptoms at least once during the pregnancy.
Table 2.
Anxiety and depressive symptoms in the analytical sample. Means, standard deviations (SD), and percentages.
| Trimester | 1st |
2nd |
3rd |
Average T1–3 |
At least once T1–3 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| N = 2,763 | N = 2,394 | N = 2,249 | N = 3,091 | N = 3,091 | ||||||
| Anxiety | N = 2,760 | N = 2,370 | N = 2,227 | N = 2,763 | N = 2,763 | |||||
| Symptom score: Mean, SDa | 3.3 | 3.9 | 3.9 | 4.2 | 3.2 | 3.9 | 3.4 | 4.0 | ||
| Clinically significant level: N, %b | 213 | 7.7 | 234 | 9.9 | 170 | 7.6 | 206 | 8.4 | 406 | 14.7 |
| Depression | N = 2,758 | N = 2,371 | N = 2,230 | N = 2,762 | N = 2,762 | |||||
| Symptom score: Mean, SDa | 5.2 | 4.0 | 4.9 | 4.1 | 4.8 | 4.0 | 5.0 | 4.0 | ||
| Clinically significant level: N, %b | 139 | 5.0 | 109 | 4.6 | 115 | 5.2 | 121 | 4.4 | 283 | 10.3 |
Depressive symptoms [sample range 0–30], anxiety symptoms [sample range 0–40] during trimesters 1–3.
Depression: ≥13 EPDS points, anxiety: ≥10 SCL-90 points.
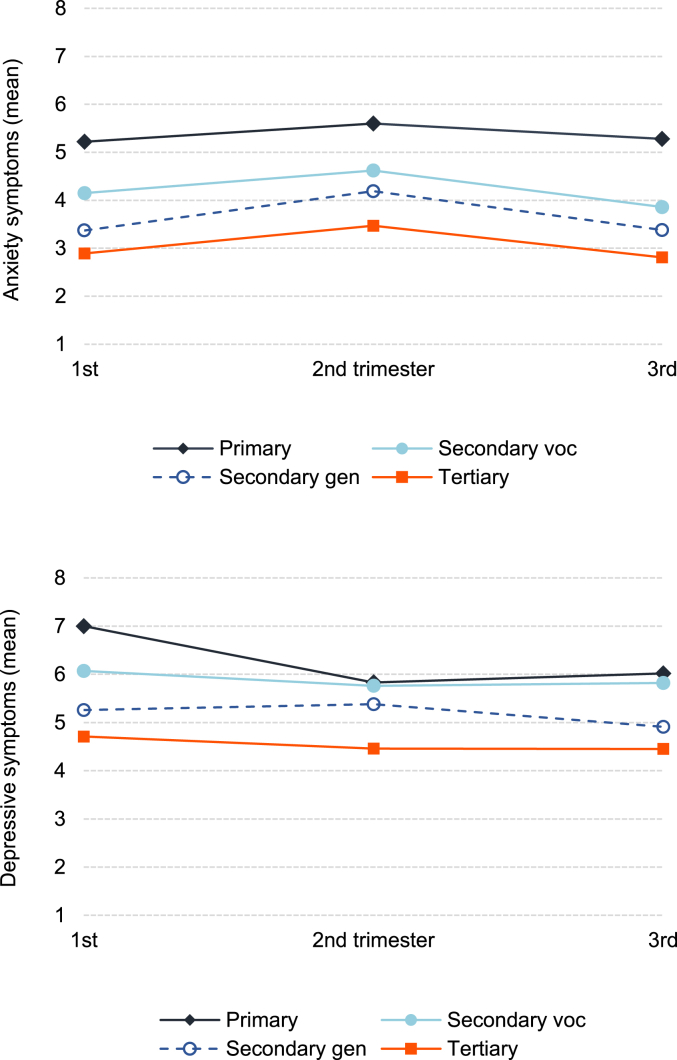
The intensity of prenatal anxiety and depressive symptoms remained relatively stable and over half of the total variance was between mothers rather than intra-individual variance over the pregnancy (intraclass correlations [not shown in the table] being 0.65 for anxiety and 0.59 for depressive symptoms). On average, the higher educated women reported fewer distress symptoms, but there was no clear pattern of educational differences in trajectories of distress over the pregnancy (Fig. 2).
Fig. 2.
Anxiety and depressive symptoms (means) over pregnancy T1–T3 by education.
Educational differences in anxiety and depressive symptoms
Table 3 presents the coefficient estimates from the baseline Model 1 and the fully adjusted Model 4. The coefficient estimates show differences between educational levels, measured in symptom score points. Model 1, which controlled only for the three measurement points (trimesters), showed clear and gradient-like educational disparities in both prenatal distress symptoms. Compared to tertiary educated pregnant women, women with general secondary (academic high school) education had 0.6 points higher scores in anxiety and 0.7 points higher scores in depressive symptoms, corresponding to 0.15 (0.6/4.0) and 0.18 (0.7/4.0) standard deviations (SD), respectively. Further, women with secondary vocational education had 1.2 points (0.30 SDs) higher anxiety and 1.3 points (0.33 SDs) higher depressive symptom scores, whereas the primary educated women had 2.4 points (0.60 SD) higher anxiety and 1.9 points (0.48 SD) higher depressive symptom scores.
Table 3.
Educational differences in prenatal anxiety and depressive symptom scores, estimated with linear multilevel regression. Coefficient estimates with 95% CIs [ ] present differences in symptom score points.
| Nested models | M1 |
M4 |
||
|---|---|---|---|---|
| Baseline |
Fully adjusted |
|||
| Anxietya | Depressionb | Anxietya | Depressionb | |
| Education (ref. tertiary) | ||||
| Primary | 2.431*** | 1.875*** | 1.451** | 0.868 |
| [1.302, 3.560] | [0.911, 2.839] | [0.383, 2.520] | [-0.046, 1.782] | |
| Secondary vocational | 1.162*** | 1.343*** | 0.891*** | 1.015*** |
| [0.801, 1.522] | [1.012, 1.674] | [0.543, 1.239] | [0.687, 1.344] | |
| Secondary general | 0.611** | 0.701*** | 0.424* | 0.480** |
| [0.234, 0.988] | [0.324, 1.079] | [0.068, 0.780] | [0.122, 0.839] | |
| Childhood SES (ref. upper level employee) | ||||
| Lower level employee | −0.197 | 0.071 | ||
| [-0.498, 0.103] | [-0.233, 0.374] | |||
| Manual worker | −0.385* | −0.059 | ||
| [-0.744, −0.027] | [-0.409, 0.292] | |||
| Other/not classifiedc | −0.467 | −0.416 | ||
| [-1.109, 0.176] | [-1.036, 0.203] | |||
| Parent's mental disorder (ref. none) | ||||
| Mother had | 0.037 | −0.001 | ||
| [-0.311, 0.386] | [-0.340, 0.339] | |||
| Father had | −0.054 | −0.095 | ||
| [-0.438, 0.329] | [-0.482, 0.292] | |||
| Childhood adversityd | 0.101*** | 0.098*** | ||
| [0.085, 0.118] | [0.082, 0.114] | |||
| Trimester (ref. 1st) | ||||
| 2nd | 0.613*** | −0.202** | 0.611*** | −0.205** |
| [0.480, 0.747] | [-0.343, −0.060] | [0.478, 0.744] | [-0.346, −0.064] | |
| 3rd | −0.071 | −0.229** | −0.075 | −0.232** |
| [-0.211, 0.069] | [-0.382, −0.076] | [-0.215, 0.065] | ['0.385, −0.079] | |
| Intercept | 2.890*** | 4.702*** | 2.201*** | 3.891*** |
| [2.723, 3.060] | [4.525, 4.880] | [1.945, 2.473] | [3.624, 4.158] | |
| Variance components | ||||
| Individual (θ) | 7.491 [6.729, 8.340] | 6.380 [5.698, 7.144] | ||
| Measure (ϑ) | 2.461 [2.213, 2.737] | 2.453 [2.205, 2.728] | ||
| Time (γ) | 2.685 [2.378, 3.030] | 2.684 [2.378, 3.029] | ||
| Residual (ε) | 3.299 [3.107, 3.502] | 3.298 [3.107, 3.501] | ||
| Intraclass correlations | ||||
| Symptom-specific | 0.62 | 0.60 | ||
| General distress | 0.47 | 0.43 | ||
| N (person-time) | 7,366 | 7,366 | ||
| N (women) | 2,763 | 2,763 | ||
*p < 0.05, **p < 0.01, ***p < 0.001.
Anxiety symptoms [sample range 0–40] at pregnancy trimesters 1–3.
Depressive symptoms [sample range 0–30] at pregnancy trimesters 1–3.
Not classified, never worked, or unemployed.
The trauma and distress scale (TADS) score [sample range 0–89].
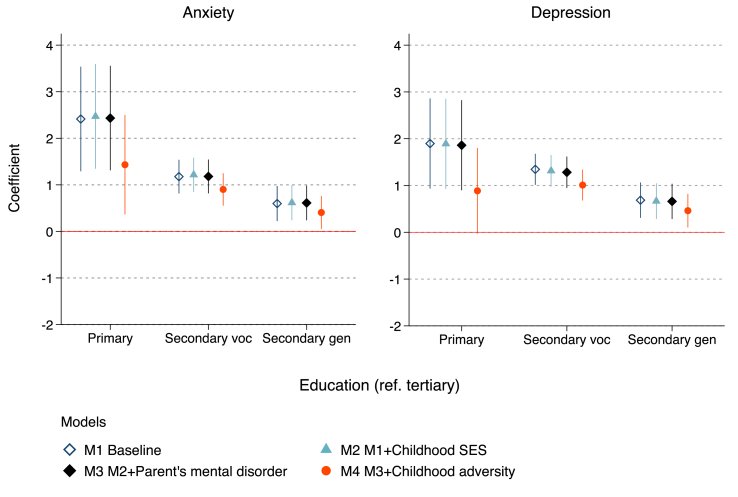
Fig. 3 presents graphically how the estimates of education changed across the three subsequent models that entered the childhood variables stepwise. Fig. 3 shows that neither childhood SES nor parents’ mental health problems confounded the educational differences. However, childhood adversity due to maltreatment experiences was a strong confounder. The point estimates were reduced by up to over 50% (depression among the primary educated) and always by at least 20% between Models 1 and 4. In Model 4, the disparity in depressive symptoms between the primary and tertiary educated was no longer statistically significant. In standard deviations, the weakened educational gradient ranged from small to moderate differences of approximately 0.1–0.35 SDs. These results support both the social causation and selection perspectives.
Fig. 3.
Estimates of education predicting prenatal anxiety and depressive symptom score points. Coefficients with 95% CIs from linear multilevel regression. Childhood SES = socioeconomic background.
Further, Model 4 in Table 3 shows the estimates of each childhood confounder. Childhood adversity was the only covariate that predicted prenatal distress symptoms, whereas the estimates for childhood SES and parents' mental health were rather small or statistically non-significant. Interestingly, mother's (not the father's) mental health problems predicted increased symptoms when childhood adversities were not controlled for (Model 3, not shown), suggesting a mechanism between parental mental health and prenatal distress symptoms.
The variance component estimates show the sources of the remaining variance (net of the independent variables) in the distress outcomes (Table 3). Of these, the individual variance component is clearly the largest. The symptom-specific ICC of 0.62 in Model 1 shows that after controlling for education and systematic variation in the outcomes over the pregnancy, women who showed high anxiety or depressive symptoms in one trimester were likely to show them in the other trimesters as well. The general distress ICC 0.47 in Model 1 suggests moderate stability in the overall propensity for these distress symptoms, and also points to comorbidity in them so that women with higher anxiety scores were likely to show higher depressive symptoms as well. The general distress ICC was, however, lower than the symptom-specific one, meaning that prenatal anxiety and depression partly capture different forms of distress (Korja et al., 2018).
Finally, we tested whether the distress trajectories differ by education. Based on Likelihood ratio -tests, educational differences in anxiety (chi2 (6) = 5.79, p = 0.447) and depressive (chi2 (6) = 10.79, p = 0.095) symptoms remained stable over time, indicating that some pregnant mothers experience persistent distress with potentially more adverse consequences (e.g. Entringer et al., 2017).
Educational differences in clinically significant levels of anxiety and depression
Educational differences in clinically defined symptom levels provide important insight into severe symptomatology. Table 4 presents results from the multilevel linear probability models (the baseline and fully adjusted models) with binary outcomes of symptom levels exceeding the validated clinical cut-off scores (anxiety ≥ 10, depression ≥ 13). The coefficient estimates show differences in the fractions of clinically significant symptoms between the educational levels.
Table 4.
Educational differences in clinical levels of prenatal anxiety or depressive symptoms, estimated with multilevel linear probability regression. Coefficient estimates with 95% CIs [ ] present differences in the fractions experiencing clinical symptom levels.
| Nested models | M1 |
M4 |
||
|---|---|---|---|---|
| Baseline |
Fully adjusted |
|||
| Anxietya | Depressionb | Anxietya | Depressionb | |
| Education (ref. tertiary) | ||||
| Primary | 0.149*** | 0.072** | 0.100* | 0.032 |
| [0.070, 0.229] | [0.018, 0.125] | [0.021, 0.179] | [-0.018, 0.084] | |
| Secondary vocational | 0.067*** | 0.032*** | 0.052*** | 0.021* |
| [0.043, 0.091] | [0.016, 0.049] | [0.029, 0.075] | [0.005, 0.037] | |
| Secondary general | 0.025* | 0.019* | 0.015 | 0.011 |
| [0.001, 0.048] | [0.001, 0.038] | [-0.008, 0.037] | [-0.007, 0.029] | |
| Childhood SES (ref. upper level employee) | ||||
| Lower level employee | −0.010 | 0.005 | ||
| [-0.029, 0.009] | [-0.009, 0.019] | |||
| Manual worker | −0.012 | −0.011 | ||
| [-0.036, 0.011] | [-0.026, 0.005] | |||
| Other/not classifiedc | −0.028 | 0.002 | ||
| [-0.064, 0.008] | [-0.026, 0.031] | |||
| Parent's mental disorder (ref. none) | ||||
| Mother had | −0.002 | 0.007 | ||
| [-0.025, 0.022] | [-0.011, 0.025] | |||
| Father had | −0.010 | −0.001 | ||
| [-0.035, 0.014] | [-0.019, 0.017] | |||
| Childhood adversityd | 0.005*** | 0.004*** | ||
| [0.004, 0.006] | [0.003, 0.005] | |||
| Trimester (ref. 1st) | ||||
| 2nd | 0.025*** | −0.002 | 0.025*** | −0.002 |
| [0.013, 0.037] | [-0.122, 0.008] | [0.013, 0.037] | [-0.012, 0.007] | |
| 3rd | 0.003 | 0.004 | 0.003 | 0.004 |
| [-0.008, 0.015] | [-0.006, 0.015] | [-0.009, 0.015] | [-0.006, 0.015] | |
| Intercept | 0.055*** | 0.039*** | 0.021* | 0.007 |
| [0.044, 0.065] | [0.299, 0.047] | [0.004, 0.038] | [-0.006, 0.019] | |
| Variance components | ||||
| Individual (θ) | 0.015 [0.012, 0.019] | 0.013 [0.010, 0.016] | ||
| Measure (ϑ) | 0.008 [0.006, 0.011] | 0.008 [0.006, 0.011] | ||
| Time (γ) | 0.010 [0.008, 0.013] | 0.010 [0.008, 0.013] | ||
| Residual (ε) | 0.029 [0.026, 0.032] | 0.029 [0.026, 0.032] | ||
| Intraclass correlations | ||||
| Symptom-specific | 0.37 | 0.35 | ||
| General distress | 0.24 | 0.22 | ||
| N (person-time) | 7,366 | 7,366 | ||
| N (women) | 2,763 | 2,763 | ||
*p < 0.05, **p < 0.01, ***p < 0.001.
Clinically significant anxiety: ≥ 10 SCL-90 points at pregnancy trimesters 1–3.
Clinically significant depression: ≥ 13 EPDS points at pregnancy trimesters 1–3.
Not classified, never worked, or unemployed.
The trauma and distress scale (TADS) score [sample range 0–89].
There were large educational disparities in clinically relevant levels of prenatal anxiety and depressive symptoms. In the baseline Model 1, women with primary education were 7.2 percentage points (0.072 × 100%) more likely to be probably clinically depressed and 14.9 percentage points more likely to have clinical levels of anxiety, compared to tertiary educated women. The respective estimates for vocational secondary educated women were 3.2 and 6.7 percentage points, and 1.9 and 2.5 percentage points, respectively, for general secondary educated women.
The differences in the clinically significant distress levels were similarly explained as in continuously measured outcomes (Model 4). The intercept estimates showed that 6.9% of tertiary educated women with the baseline characteristics showed clinically significant levels of prenatal anxiety, and 4.6% had clinically significant depressive symptoms. The only statistically significant difference in depression was between women with tertiary and vocational secondary education, the latter having 2.1 percentage points (or at baseline values (4.6% + 2.1%)/4.6% = 1.4 times) higher probability of clinically significant depressive symptoms. The educational differences in clinically relevant prenatal anxiety were larger. Compared to tertiary educated pregnant mothers, mothers with secondary vocational education had 5.2 percentage points (1.8 times) and mothers with primary education had 10.0 percentages points (2.4 times) higher probability of clinically significant anxiety. Compared with the relatively moderate educational differences in prenatal anxiety symptoms, the differences in the clinically significant symptom levels were more substantively meaningful. Furthermore, the ICCs were clearly lower than for the continuous outcomes. This suggests lower stability in clinically relevant levels of anxiety and depression over pregnancy, which may reflect changes above and below the cut-off points that the diagnostics using a binary tool is not able to capture.
Sensitivity analysis of unmeasured confounding
The remaining educational differences in anxiety and depressive symptoms after controlling for childhood circumstances might be further confounded by unmeasured variables, such as psychological symptomatology during childhood or adolescence (Evensen et al., 2016; Fletcher, 2010) or by genetic dispositions. We performed a sensitivity analysis using E-values, to assess the strength of this unmeasured confounding (VanderWeele & Ding, 2017).
Table 5 shows the E-values for the statistically significant point estimates and the lower 95% confidence intervals for both the standardized estimates of mean difference (Table 3) and the clinically significant levels (Table 4). The E-value was calculated on the risk ratio (RR) scale and this is shown in the upper panel of Table 5. We use the difference in clinically significant levels of prenatal anxiety between women with primary and tertiary education as an example. The E-value shows that a potential confounder should have an RR of at least 4.33 with both the exposure (primary compared to tertiary education) and with the outcome to explain away the difference (i.e., the point estimate is zero). The RRs should be at least 2.15 so that the difference would not be statistically significant at the 5% level (i.e., 95% CI overlaps zero).
Table 5.
Sensitivity analysis using E-value estimates. Minimum association strength (risk ratio) of a confounder needed to explain away (point estimate) or reduce to statistical non-significance (lower 95% CI, in parentheses) the stat. sig. educational differences in prenatal anxiety and depressive symptoms.
| Risk ratio scale | Continuous outcomes |
Clinically significant levels |
|||
|---|---|---|---|---|---|
| Anxiety | Depression | Anxiety | Depression | ||
| Education (ref. higher) | |||||
| Primary | 2.13 | 4.33 | |||
| (1.41) | (2.15) | ||||
| Secondary vocational | 1.75 | 1.83 | 2.90 | 2.27 | |
| (1.52) | (1.61) | (2.49) | (1.53) | ||
| Secondary general | 1.44 | 1.47 | |||
| (1.14) | 1.20 | ||||
| Continuous scale approximation | Anxiety | Depression | |||
| Education (ref. higher) | |||||
| Primary | 0.83 | 0.60 | |||
| (0.38) | (0) | ||||
| Secondary vocational | 0.61 | 0.67 | |||
| (0.46) | (0.53) | ||||
| Secondary general | 0.40 | 0.43 | |||
| (0.15) | (0.20) | ||||
RRs are difficult to interpret for continuous outcomes, and the lower panel shows E-values that were converted back to (an approximation of) the continuous scale and shown as standardized effects (cf. VanderWeele & Ding, 2017). The largest E-value estimate needed for explaining away the association was 0.83, for the disparity in anxiety scores between women with primary and tertiary education. The smallest E-value for reducing an association to statistical non-significance was 0.53 (vocational secondary vs. tertiary in depressive symptoms).
Many of the E-values for educational differences were relatively large. Given that candidate confounders, anxiety and depression during adolescence, have had no to moderate effects on educational attainment (Evensen et al., 2016; Fletcher, 2010; Miech et al., 1999), it appears unlikely that they alone would fully confound the associations.
Discussion
Prior research provides inconsistent evidence of educational differences in prenatal anxiety and depression (cf. Biaggi et al., 2016; Gelaye et al., 2016; Lancaster et al., 2010; Underwood et al., 2016). A potential reason is that previous studies have not focused primarily on educational differences and their models have included covariates which are possible mediators of the effect of education, increasing the risk of overadjustment (Schisterman et al., 2009). This was the first study focusing on educational differences in prenatal distress and to assess the causation and selection processes involved.
We had three main findings. First, we observed lower symptom scores and lower probability of having clinically significant symptom levels in pregnant women with higher education. The educational differences were gradient-like and substantively meaningful. In particular, we found clear educational disparities in clinically relevant levels of both symptoms. These results are in line with the findings on disparities in anxiety and depression in the general population.
Our second main finding relates to the role of social selection as an explanation to these associations, based on measured confounders. Parents’ SES (social class) and mental disorders did not account for the educational differences in prenatal distress. This is surprising, because childhood SES has been linked to educational attainment and mental health (Johnson et al., 1999; Reiss, 2013); however, having information on parental education could have altered these findings. The results concerning parental health problems can partly reflect error in the retrospective measurement, although it has been suggested to be of sufficient validity (Kurstjens & Wolke, 2001).
Adverse childhood experiences (ACE) measured through the Trauma and Distress Scale were the most important explaining factor for the relationship between education and prenatal distress symptoms. Controlling for it attenuated the educational disparities in prenatal anxiety and depressive symptoms by up to a half, suggesting that early adversities affect both educational attainment and prenatal mental health. The finding provides support for both the social causation and selection perspectives and suggests the importance of ACE measures for understanding educational inequalities in mental health in the general population as well.
Our third main finding relates to the role of social causation. Because of our small number of control variables, we conducted a sensitivity analysis of unmeasured confounding using E-values (VanderWeele & Ding, 2017). In particular, we ruled out the possibility of complete confounding by anxiety and depression in adolescence, which are theoretically potential but empirically relatively weak predictors of education (Evensen et al., 2017; Fletcher, 2010). Based on the sensitivity analysis, we concluded that education and the resources it provides — such as improved skills, and self-efficacy (Mirowsky & Ross, 2005) — are likely to protect from prenatal distress, in line with results concerning distress in the general population (Allen et al., 2014; Pinto-Meza et al., 2013; Reiss, 2013). Although this supports the social causation hypothesis, the available data and methods are limited in providing conclusive evidence, and multiple unmeasured factors during the life course may alone or cumulatively explain the remaining educational differences.
The strength of this study is a combination of both socioeconomic and psychological measures ofthe life course. In addition, carrying out a sensitivity analysis for unmeasured confounding has not been a common practice previously. The main limitations relate to the reliability of recall measures, such as childhood adversities. The measure is known to involve bias, but no better method to measure those adversities retrospectively exists (Hardt & Rutter, 2004). Recall measures generally have been more accurate in emotionally strongly loaded experiences than in cognitive domains (Bell & Bell, 2018), and previous results suggest sufficient validity when compared to more objective measures (Kurstjens & Wolke, 2001). However, the results based on retrospective measurement should be interpreted with caution. The non-random drop-out rate of more disadvantaged and symptomatic women (Karlsson et al., 2018) also may have caused bias to our estimates.
Prenatal depression and anxiety have been less studied than postpartum depression, regardless of their negative consequences (Beck, 2011; Lee et al., 2007; Robertson et al., 2004), and despite the fact that many first episodes occur during pregnancy (Räisänen et al., 2014). Our findings supported both the social causation and selection perspectives. The former suggests that educational resources may buffer against prenatal distress and thus contribute to child health, potentially in long-term. Future research can analyze these relationships in other populations, further examine whether the educational differences in prenatal distress reflect the protective effects of education or disparities formed earlier in life, as well as attempt to understand the mechanisms which may translate education into less prenatal distress. Another future challenge is to equal out the role of gene-environment interplay in these disparities. We found that the educational differences were partly explained by adverse childhood experiences, underlining that particularly undisturbed psychological growth environment can protect from mental health problems among pregnant women. This finding implies high relevance for both research and policy. Childhood maltreatment can leave long-term scars, the effects of which can extend to the next generation.
Declaration of competing interest
None.
Acknowledgements
The previous versions of the article have been presented in the Nordic Demographic Symposium (NDS) 2019, in the European Consortium for Sociological Research (ECSR) annual conference 2019 as well as in other seminars and meetings. We thank all participants for their valuable comments. We also thank the reviewers of this article for their useful feedback. The study has been funded by Academy of Finland (grant numbers: 134950, 253270, and 287908), Signe and Ane Gyllenberg Foundation, and University of Turku, and the open access fee was covered by INVEST Flagship funded by Academy of Finland (grant number: 320162).
References
- Allen J., Balfour R., Bell R., Marmot M. Social determinants of mental health. International Review of Psychiatry. 2014;26:392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- Beck C.T. Predictors of postpartum depression: An update. Nursing Research. 2011;50:275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Bell D.C., Bell L.G. Accuracy of Retrospective Reports of Family Environment. Journal of Child and Family Studies. 2018;27(4):1029–1040. doi: 10.1007/s10826-017-0948-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein D.P., Fink L., Handelsman L., Foote J., Lovejoy M., Wenzel K., Sapareto E., Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Biaggi A., Conroy S., Pawlby S., Pariante C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of Affective Disorders. 2016;191:62–77. doi: 10.1016/j.jad.2015.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden J.M., Horwood L.J., Fergusson D.M. Exposure to childhood sexual and physical abuse and subsequent educational achievement outcomes. Child Abuse & Neglect. 2007;31:1101–1114. doi: 10.1016/j.chiabu.2007.03.022. [DOI] [PubMed] [Google Scholar]
- Bøe T., Sivertsen B., Heiervang E. Socioeconomic status and child mental health: The role of parental emotional well-being and parenting practices. Journal of Abnormal Child Psychology. 2014;42:705–715. doi: 10.1007/s10802-013-9818-9. [DOI] [PubMed] [Google Scholar]
- Bouthoorn S.H., Silva L.M., Murray S.E., Steegers E.A.P., Jaddoe V.W.V., Moll H., Hofman A., Mackenbach J.P., Raat H. Low-educated women have an increased risk of gestational diabetes mellitus: The generation R study. 2015. 445-452. [DOI] [PubMed]
- Breen R., Jonsson J.O. Inequality of opportunity in comparative perspective: Recent research on educational attainment and social mobility. Annual Review of Sociology. 2005;31:223–243. doi: 10.1146/annurev.soc.31.041304.122232. [DOI] [Google Scholar]
- Buss C., Poggi E., Shahbaba B., Pruessner J.C., Head K., Sandman C.A. Maternal cortisol over the course of pregnancy and subsequent child amygdala and hippocampus volumes and affective problems. Proceedings of the National Academy of Sciences. 2012;109 doi: 10.1073/pnas.1201295109/-/DCSupplemental.www.pnas.org/cgi/doi/10.1073/pnas.1201295109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E.J., Compton S.N., Keeler G., Angold A. Relationships between poverty and psychopathology: A natural experiment. Journal of the American Medical Association. 2003;290:2023–2029. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression development of the 10-item Edinburgh postnatal depression scale. British Journal of Psychiatry. 1987;150:782–787. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Currie J., Widom C.S. Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreatment. 2010;15:111–120. doi: 10.1177/1077559509355316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis C.L., Falah-Hassani K., Shiri R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. British Journal of Psychiatry. 2017;210:315–323. doi: 10.1192/bjp.bp.116.187179. [DOI] [PubMed] [Google Scholar]
- Derogatis L.R., Cleary P.A. Confirmation of the dimensional structure of the scl‐90: A study in construct validation. Journal of Clinical Psychology. 1977;33:981–989. doi: 10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0. [DOI] [Google Scholar]
- Devenish B., Hooley M., Mellor D. The pathways between socioeconomic status and adolescent outcomes: A systematic review. American Journal of Community Psychology. 2017;59:219–238. doi: 10.1002/ajcp.12115. [DOI] [PubMed] [Google Scholar]
- Dohrenwend B.P. The role of adversity and stress in psychopathology: Some evidence and its implications for theory and research. Journal of Health and Social Behavior. 2000;41:1–19. [PubMed] [Google Scholar]
- Dohrenwend B.P., Levav I., Shrout P.E., Schwartz S., Naveh G., Link B.G., Skodol A.E., Stueve A. Socioeconomic status and psychiatric disorders: The causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- Dubber S., Reck C., Müller M., Gawlik S. Postpartum bonding: The role of perinatal depression, anxiety and maternal–fetal bonding during pregnancy. Archives of Women's Mental Health. 2015;18:187–195. doi: 10.1007/s00737-014-0445-4. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C., Tanner L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Current Opinion in Psychiatry. 2012;25:141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entringer S., Buss C., Wadhwa P.D. Prenatal stress, development, health and disease risk: A psychobiological perspective. Psychoneuroendocrinology. 2017;62:366–375. doi: 10.1016/j.antiviral.2015.06.014.Chronic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erola J., Jalonen S., Lehti H. Parental education, class and income over early life course and children’ s achievement. Research in Social Stratification and Mobility. 2016;44:33–43. doi: 10.1016/j.rssm.2016.01.003. [DOI] [Google Scholar]
- Evans G.W. Child development and the physical environment. Annual Review of Psychology. 2006;57:423–451. doi: 10.1146/annurev.psych.57.102904.190057. [DOI] [PubMed] [Google Scholar]
- Evensen M., Lyngstad T.H., Melkevik O., Mykletun A. The role of internalizing and externalizing problems in adolescence for adult educational attainment: Evidence from sibling comparisons using data from the young HUNT study. European Sociological Review. 2016;32:552–566. doi: 10.1093/esr/jcw001. [DOI] [Google Scholar]
- Fawcett E.J., Fairbrother N., Cox M.L., White I.R., Fawcett J.M. 2019. The prevalence of anxiety disorders during pregnancy and the postpartum period: A multivariate bayesian meta-analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson K.T., Cassells R.C., MacAllister J.W., Evans G.W. The physical environment and child development: An international review. International Journal of Psychology. 2013;48:437–468. doi: 10.1080/00207594.2013.804190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher J.M. Adolescent depression and educational attainment: Results using sibling fixed effects. Health Economics. 2010;19:855–871. doi: 10.1002/hec.1526. [DOI] [PubMed] [Google Scholar]
- Fryers T., Melzer D., Jenkins R. Social inequalities and the common mental disorders - a systematic review of the evidence. Social Psychiatry and Psychiatric Epidemiology. 2003;38:229–237. doi: 10.1007/s00127-003-0627-2. [DOI] [PubMed] [Google Scholar]
- Galobardes B., Shaw M., Lawlor D.A., Lynch J.W., Smith G.D. Indicators of socioeconomic position (part 1) Journal of Epidemiology & Community Health. 2006;60:7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B., Rondon M.B., Araya R., Williams M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. The Lancet Psychiatry. 2016;3:973–982. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert R., Widom C.S., Browne K., Fergusson D., Webb E., Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Hardt J., Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Härkönen J., Lindberg M., Karlsson L., Karlsson H., Scheinin N.M. Education is the strongest socio-economic predictor of smoking in pregnancy. Addiction. 2018;113:1117–1126. doi: 10.1111/add.14158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haushofer J., Fehr E. On the psychology of poverty. Science. 2014;344:862–867. doi: 10.1126/science.1232491. [DOI] [PubMed] [Google Scholar]
- Heim C., Newport D.J., Mletzko T., Miller A.H., Nemeroff C.B. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Holi M. 2003. Assessment of psychiatric symptoms using the SCL-90. [Google Scholar]
- Johnson J.G., Cohen P., Dohrenwend B.P., Link B.G., Brook J.S. A longitudinal investigation of social causation and social selection processes involved in the association between socioeconomic status and psychiatric disorders. Journal of Abnormal Psychology. 1999;108:490–499. doi: 10.1037/0021-843X.108.3.490. [DOI] [PubMed] [Google Scholar]
- Karlsson L., Tolvanen M., Scheinin N.M., Uusitupa H.M., Korja R., Ekholm E., Tuulari J.J., Pajulo M., Huotilainen M., Paunio T., Karlsson H. Cohort profile: The FinnBrain birth cohort study (FinnBrain) International Journal of Epidemiology. 2018;47:15–16j. doi: 10.1093/ije/dyx173. [DOI] [PubMed] [Google Scholar]
- Keeton C.P., Perry-Jenkins M., Sayer A.G. Sense of control predicts depressive and anxious symptoms across the transition to parenthood. Journal of Family Psychology. 2008 doi: 10.1037/0893-3200.22.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., McLaughlin K.A., Green J.G., Gruber M.J., Sampson N.A., Zaslavsky A.M., Aguilar-Gaxiola S., Alhamzawi A.O., Alonso J., Angermeyer M., others Childhood adversities and adult psychopathology in the WHO World mental health surveys. British Journal of Psychiatry. 2010;197:378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiernan K.E., Huerta M.C. Economic deprivation, maternal depression, parenting and children's cognitive and emotional development in early childhood 1. British Journal of Sociology. 2008;59:783–806. doi: 10.1111/j.1468-4446.2008.00219.x. [DOI] [PubMed] [Google Scholar]
- Korgaonkar M.S., Antees C., Williams L.M., Gatt J.M., Bryant R.A., Cohen R., Paul R., O'Hara R., Grieve S.M. Early exposure to traumatic stressors impairs emotional brain circuitry. PLoS One. 2013;8 doi: 10.1371/journal.pone.0075524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korja R., Nolvi S., Kataja E.L., Scheinin N., Junttila N., Lahtinen H., Saarni S., Karlsson L., Karlsson H. The courses of maternal and paternal depressive and anxiety symptoms during the prenatal period in the Finnbrain birth cohort study. PLoS One. 2018;13:1–19. doi: 10.1371/journal.pone.0207856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kröger H., Pakpahan E., Hoffmann R. What causes health inequality? A systematic review on the relative importance of social causation and health selection. The European Journal of Public Health. 2015;25:951–960. doi: 10.1093/eurpub/ckv111. [DOI] [PubMed] [Google Scholar]
- Kurstjens S., Wolke D. Effects of maternal depression on cognitive development of children over the first 7 years of life. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 2001;42:623–636. [PubMed] [Google Scholar]
- Lahti M., Savolainen K., Tuovinen S., Pesonen A.-K., Lahti J., Heinonen K., Hämäläinen E., Laivuori H., Villa P.M., Reynolds R.M., Kajantie E., Räikkönen K. Maternal depressive symptoms during and after pregnancy and psychiatric problems in children. Journal of the American Academy of Child & Adolescent Psychiatry. 2017;56:30–39. doi: 10.1016/j.jaac.2016.10.007. e7. [DOI] [PubMed] [Google Scholar]
- Lancaster C.A., Gold K.J., Flynn H.A., Yoo H., Marcus S.M., Davis M.M. Risk factors for depressive symptoms during pregnancy: A systematic review. American Journal of Obstetrics and Gynecology. 2010;202:5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A.M., Lam S.K., Sze Mun Lau S.M., Chong C.S.Y., Chui H.W., Fong D.Y.T. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstetrics & Gynecology. 2007;110:1102–1112. doi: 10.1097/01.AOG.0000287065.59491.70. [DOI] [PubMed] [Google Scholar]
- Littleton H.L., Breitkopf C.R., Berenson A.B. Correlates of anxiety symptoms during pregnancy and association with perinatal outcomes: A meta-analysis. American Journal of Obstetrics and Gynecology. 2007;196:424–432. doi: 10.1016/j.ajog.2007.03.042. [DOI] [PubMed] [Google Scholar]
- Lupien S.J., McEwen B.S., Gunnar M.R., Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Mäenpää E. Homogamy in educational level and parental social class in Finland: A log-linear analysis. European Sociological Review. 2014;31:253–267. doi: 10.1093/esr/jcu088. [DOI] [Google Scholar]
- Marcus S.M. Depression during pregnancy: Rates, risks and consequences. The Canadian Journal of Clinical Pharmacology. 2009;16:15–22. [PubMed] [Google Scholar]
- Masarik A.S., Conger R.D. Stress and child development: A review of the family stress model. Current Opinion in Psychology. 2017;13:85–90. doi: 10.1016/j.copsyc.2016.05.008. [DOI] [PubMed] [Google Scholar]
- Matthews K.A., Gallo L.C., Taylor S.E. Are psychosocial factors mediators of socioeconomic status and health connections? A progress report and blueprint for the future. Annals of the New York Academy of Sciences. 2010;1186:146–173. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- Matthey S., Henshaw C., Elliott S., Barnett B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale--implications for clinical and research practice. Archives of Women's Mental Health. 2006;9:309–315. doi: 10.1007/s00737-006-0152-x. [DOI] [PubMed] [Google Scholar]
- Merikangas K.R., Zhang H., Avenevoli S., Acharyya S., Neuenschwander M., Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: The Zurich cohort study. Archives of General Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- Miech R.A., Caspi A., Moffitt T.E., Wright B.R.E., Silva P.A. Low socioeconomic status and mental disorders: A longitudinal study of selection and causation during young adulthood. American Journal of Sociology. 1999;104:1096–1131. doi: 10.1086/210137. [DOI] [Google Scholar]
- Mirowsky J., Ross C.E. Education, learned effectiveness and health. London Review of Education. 2005;3:205–220. doi: 10.1080/14748460500372366. [DOI] [Google Scholar]
- Misri S., Kendrick K. Perinatal depression, fetal bonding, and mother-child attachment: A review of the literature. Current Pediatric Reviews. 2008;4:66–70. doi: 10.2174/157339608784462043. [DOI] [Google Scholar]
- Muntaner C., Eaton W.W., Miech R., O'Campo P. Socioeconomic position and major mental disorders. Epidemiologic Reviews. 2004;26:53–62. doi: 10.1093/epirev/mxh001. [DOI] [PubMed] [Google Scholar]
- Myrskylä M., Margolis R. Happiness: Before and after the kids. Demography. 2014;51:1843–1866. doi: 10.1007/s13524-014-0321-x. [DOI] [PubMed] [Google Scholar]
- Nast I., Bolten M., Meinlschmidt G., Hellhammer D.H. How to measure prenatal stress? A systematic review of psychometric instruments to assess psychosocial stress during pregnancy. Paediatric & Perinatal Epidemiology. 2013;27:313–322. doi: 10.1111/ppe.12051. [DOI] [PubMed] [Google Scholar]
- Pechtel P., Pizzagalli D.A. Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacology. 2011;214:55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto-Meza A., Moneta M.V., Alonso J., Angermeyer M.C., Bruffaerts R., Caldas de Almeida J.M., de Girolamo G., de Graaf R., Florescu S., Kovess Masfety V., O'Neill S., Vassilev S., Haro J.M. Social inequalities in mental health: Results from the EU contribution to the World mental health surveys initiative. Social Psychiatry and Psychiatric Epidemiology. 2013;48:173–181. doi: 10.1007/s00127-012-0536-3. [DOI] [PubMed] [Google Scholar]
- Power C., Hertzmant C. Social and biological pathways linking early life and adult disease. British Medical Bulletin. 1997;53:210–221. doi: 10.1093/oxfordjournals.bmb.a011601. [DOI] [PubMed] [Google Scholar]
- Power C., Stansfeld S.A., Matthews S., Manor O., Hope S. Childhood and adulthood risk factors for socio-economic differentials in psychological distress: Evidence from the 1958 British birth cohort. Social Science & Medicine. 2002;55:1989–2004. doi: 10.1016/S0277-9536(01)00325-2. [DOI] [PubMed] [Google Scholar]
- Pulkki-Råback L., Ahola K., Elovainio M., Kivimäki M., Hintsanen M., Isometsä E., Lönnqvist J., Virtanen M. Socio-economic position and mental disorders in a working-age Finnish population: The health 2000 study. The European Journal of Public Health. 2012;22:327–332. doi: 10.1093/eurpub/ckr127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S., Skrondal A. 3rd ed. Stata Press; College Station (TX): 2012. Multilevel and longitudinal modeling using Stata. [Google Scholar]
- Räisänen S., Lehto S.M., Nielsen H.S., Gissler M., Kramer M.R., Heinonen S. Risk factors for and perinatal outcomes of major depression during pregnancy: A population-based analysis during 2002-2010 in Finland. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-004883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Social Science & Medicine. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- Repetti R.L., Taylor S.E., Seeman T.E. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. doi: 10.1037/0033-2909.128.2.330. [DOI] [PubMed] [Google Scholar]
- Robertson E., Grace S., Wallington T., Stewart D.E. Antenatal risk factors for postpartum depression: A synthesis of recent literature. General Hospital Psychiatry. 2004;26:289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Ross C.E., Mirowsky J. Refining the association between education and health: The effects of quantity, credential, and selectivity. Demography. 1999;36:445–460. doi: 10.2307/2648083. [DOI] [PubMed] [Google Scholar]
- Rubertsson C., Börjesson K., Berglund A., Josefsson A., Sydsjö G. The Swedish validation of Edinburgh postnatal depression scale (EPDS) during pregnancy. Nordic Journal of Psychiatry. 2011;65:414–418. doi: 10.3109/08039488.2011.590606. [DOI] [PubMed] [Google Scholar]
- Rubertsson C., Wickberg B., Gustavsson P., Rådestad I. Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Archives of Women's Mental Health. 2005;8:97–104. doi: 10.1007/s00737-005-0078-8. [DOI] [PubMed] [Google Scholar]
- Salokangas R.K.R., Schultze-Lutter F., Patterson P., Graf von Reventlow H., Heinimaa M., From T., Luutonen S., Hankala J., Kotimäki M., Tuominen L. Psychometric properties of the Trauma and Distress Scale, TADS, in an adult community sample in Finland. European Journal of Psychotraumatology. 2016;7 doi: 10.3402/ejpt.v7.30062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schisterman E.F., Cole S.R., Platt R.W. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva L.M., Coolman M., Steegers E.A.P., Jaddoe V.W.V., Moll H.A., Hofman A., Mackenbach J.P., Raat H. Maternal educational level and risk of gestational hypertension: The generation R study. Journal of Human Hypertension. 2008;22:483. doi: 10.1038/jhh.2008.22. [DOI] [PubMed] [Google Scholar]
- Skouteris H., Wertheim E.H., Rallis S., Milgrom J., Paxton S.J. Depression and anxiety through pregnancy and the early postpartum: An examination of prospective relationships. Journal of Affective Disorders. 2009;113:303–308. doi: 10.1016/j.jad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- Smith M. Parental mental health: Disruptions to parenting and outcomes for children. Child & Family Social Work. 2004;9:3–11. [Google Scholar]
- Statistics Finland Syntyneet 2016. 2017. www.stat.fi/til/synt/2016/02/synt_2016_02_2017-12-04_tie_001_en.html [Births 2016]. Web:
- Suokas K., Koivisto A.M., Hakulinen C., Kaltiala R., Sund R., Lumme S., Kampman O., Pirkola S. Association of income with the incidence rates of first psychiatric hospital admissions in Finland, 1996-2014. JAMA Psychiatry. 2019;77:274–284. doi: 10.1001/jamapsychiatry.2019.3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.E., Seeman T.E. Psychosocial Resources and the SES-Health Relationship. Annals of the New York Academy of Sciences. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- Teicher M.H., Samson J.A. Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. American Journal of Psychiatry. 2014;170:1114–1133. doi: 10.1176/appi.ajp.2013.12070957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underwood L., Waldie K., D'Souza S., Peterson E.R., Morton S. A review of longitudinal studies on antenatal and postnatal depression. Archives of Women's Mental Health. 2016;19:711–720. doi: 10.1007/s00737-016-0629-1. [DOI] [PubMed] [Google Scholar]
- UNESCO . UNESCO Institute for Statistics; Montreal: 2012. International standard classification of education ISCED 2011. [Google Scholar]
- VanderWeele T.J., Ding P. Sensitivity analysis in observational research: Introducing the E-value. Annals of Internal Medicine. 2017;167:268–274. doi: 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- Whitbeck L.B., Simons R.L., Conger R.D., Wickrama K.A.S., Ackley Kevin A., Elder Glen H. The effects of parents' working conditions and family economic hardship on parenting behaviors and children’ s self-efficacy. Social Psychology Quarterly. 1997;60:291–303. [Google Scholar]
- Williams J.H.G., Ross L. Consequences of prenatal toxin exposure for mental health in children and adolescents. European Child & Adolescent Psychiatry. 2007;16:243–253. doi: 10.1007/s00787-006-0596-6. [DOI] [PubMed] [Google Scholar]
- Woody C.A., Ferrari A.J., Siskind D.J., Whiteford H.A., Harris M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. Journal of Affective Disorders. 2017;219:86–92. doi: 10.1016/j.jad.2017.05.003. [DOI] [PubMed] [Google Scholar]