Abstract
Background
Since older population in India continue to rely on family and social networks for care and support, understanding the health outcomes associated with violence within and outside family may direct the development of policies and measures to aid the victims of violence. The present paper examines the health consequences of violence against older adults and its gender differentials in India.
Methods
Using data from Building Knowledge Base on Population Ageing in India (BKPAI), we employed bivariate and logistic regressions on a sample of 9181 older adults to fulfil the aims and objective of the paper.
Results
About 10.7% and 11.3% of men and women faced violence after turning 60 years respectively. Older adults who ever faced violence after turning age 60 years had 60%, 41% and 33% higher likelihood to have poor-SRH, low ADL and low IADL respectively in comparison to their counterparts. Further, it was found that older adults who ever faced violence after turning age 60 years had 97% and 62% higher likelihood to have lower psychological health and low subjective well-being. Additionally, it was found that women who faced violence had higher odds of having low psychological health [OR: 1.18, CI: 1.06, 1.63], low subjective well-being [OR: 1.70, CI: 1.24, 2.33] and low cognitive ability [OR: 1.32, CI: 1.04, 1.79] in comparison to men who faced violence.
Conclusion
Violence against older adults must be recognized as a key public health issue for older adults in India. Study findings indicate the immediate need for assessing victim health outcomes following any type of violence in later years to determine related policies and programs to protect the victims. Reducing violence will have a positive impact on physical and mental health outcomes late in life as well as the functional abilities of older adults, especially older women.
Keywords: Older adults, Violence, Health outcomes, Gender, India
Highlights
-
•
About 10.7% and 11.3% of men and women faced violence after turning 60 years respectively.
-
•
Older adults who faced violence after age 60 had poor-SRH, low ADL, IADL as well as low psychological health and SWB.
-
•
Older women who faced violence had low levels of psychological health, SWB and cognitive ability in comparison to men who faced violence.
Background
With about 12 per cent of the world's population aged 60 years and older, India has the second highest number of older persons after China. As older adults, a non-working and ill-health population grows, so too do concerns regarding violence against them. Older people are more likely to be exposed to some type of violence, isolation and abandonment than their younger counterparts (Patel & Prince, 2001; Srivastava, Bhatia, Rajoura, & Joseph, 2013). Longitudinal Ageing Study in India (LASI) pilot study reported that about 26 percent of the older adults faced some type of violence (Berkman, Sekher, Capistrant, & Zheng, 2012a).
Researchers have begun to argue that the recent changes in traditional Indian cultural values influence the nature and scope of violence against older adults (Iwaya et al., 2017). The older parents have continued to invest in their children and traditionally have expected to be cared for at an older age and if their investment is not reciprocated, their life is likely to be coloured by a sense of injustice and exploitation, which may lead to certain negative effects (Martin, Hagberg, & Poon, 1997; T, 2008). Since older adults may be perceived as a burden by the family and care-givers, such stressful and bitterness spills out in form of violence and negligence of older adults (Tiwari, 2000). The growing gap in cultures and beliefs, difference in thinking and expectations, and living conditions of children have affected the lives of older adults in their own family (Kumar & Bhargava, 2014).
The empirical works with longitudinal surveys show a lasting impact of violence on health outcomes in later years (Schofield, Powers, & Loxton, 2013; Wong & Waite, 2017a). Violence increases the risks of declines in later psychological and physical health among older adults. The negative correlates of emotional, physical, and sexual violence with respect to physical and mental health were demonstrated in a series of studies with Chinese participants (Dong, 2015; Dong & Simon, 2013; Li, Liang, & Dong, 2019). Risk factors associated with older victims of violence and neglect include cognitive impairment as well (Amstadter et al., 2010). Besides, it can also leave mistreated older adults devoid of their fundamental meaning of life (Chokkanathan, Natarajan, & Mohanty, 2014). Evidence also suggests that the violence is associated with distress and increased mortality in older people (Lachs, Williams, Brien, Pillemer, & Charlson, 1998; Li et al., 2019).
The World Health Organization (WHO, 2017) recognizes the connection between violence and mental health consequences among older adults, such as depression and anxiety, in its Comprehensive Mental Health Action Plan for 2013–2020. The negative outcomes associated with violence, such as depression, anxiety, and low level of life satisfaction, have been well-documented (Chokkanathan & Lee, 2005; Chokkanathan & Natarajan, 2018). Any type of violence is recognized as a stressful experience for older adults which has been found to have harmful effects on their mental health (T, 2008). In addition, older adults enduring more frequent mistreatment behaviours were more likely to have poor physical and mental health and chronic pain (Fisher & Regan, 2006). Qualitative research has found that selected later life mental disorders may be attributed to violence, neglect or lack of love from children (Patel & Prince, 2001).
Traditionally dominated by a joint family pattern, recent changes in the Indian society is not swallowed by the youth easily, due to which older people are more likely to be exposed to several types of violence (Seth, Yadav, Adichwal, & Kamble, 2019). The violence against older adults is multidimensional and arises due to differences in gender, socioeconomic status, and physical condition (Selwood, Cooper, & Livingston, 2007). On the other hand, the change in inter-generational relationships and increased role of women in the economic sector against the traditional caregiving role has led to frequent relationship conflicts and older parents are often ill-treated (Berkman, Sekher, Capistrant, & Zheng, 2012b). A recent study found that the proportion for verbal or economic violence, disrespect, and neglect was high among women when compared to men, and for physical violence, the gender disparity was more pronounced (Chaurasia & Srivastava, 2020), indicating the gender vulnerability of violence against older adults.
In the presence of traditional Asian cultural norms and the absence of effective social institutions, the older population in India will continue to rely on the care and support provided in the family and by social networks (Gupta, 2009a; Ugargol & Bailey, 2018, 2020). Understanding the health outcomes associated with violence can direct the development of policies and measures to aid victims of violence late in life. This study examines the health consequences of violence and its gender differentials by analysing the data of a large sample of older adults in seven major states in India.
Methods
Data
The present research used data from Building a Knowledge Base on Population Aging in India (BKPAI) which was National level survey and was conducted in 2011, across seven states of India. The survey was sponsored by Institute for social and economic change (ISEC), Bangalore, Tata Institute for social sciences (TISS), Mumbai, Institute for economic growth (IEG) and UNFPA, New Delhi. The survey gathered information on various socio-economic and health aspects of ageing among households of those aged 60 years and above. The data from seven states were collected which represents the various regions of India namely, North India, South India, Western India and Eastern India. The states were Punjab and Himachal from northern part, Kerala and Tamil Nadu from southern part, Orissa and West Bengal from eastern part and Maharashtra from western part.
Probability proportional to size (PPS) sampling method was used to select the PSU's and within each PSU older adults' households were selected through systematic sampling. A similar process was applied in urban areas also and then sample which represented individual from all seven states was represented. In all, 9850 older adults were interviewed from 8329 households aged 60 years and above. The sample included for the analysis after performing all pre-analysis procedures like dropping the missing data and outliers was 9540 older adults.
Outcome variable
The analysis contains health status of older adults as the outcome variables. The six outcome variables were poor self-rated health, low ability to do activities of daily living (ADL), low ability to do instrumental activities of daily living (IADL), low psychological health, low subjective well-being and low cognitive ability. Self-rated health was having a scale of 1–5 “poor to excellent” and was categorized as 0 “good” (representing good, very good and excellent) and 1 “poor” (representing poor or fair) (Joe, Perkins, & Subramanian, 2019). Ability to do activities of daily living was having a scale of 0–6 where in it represents higher the score higher the independence. A score of was categorized as 0 “high” which represents full independence and 5 and less was categorized as 1 “low” which represents not fully independent to do activities of daily living. Ability to do instrumental activities of daily living was having a scale of 0–8 representing higher the score higher the independence. A score of 6+ was categorized as 0 “high” representing high IADL and score of 5 and less was recoded as 1 “low” representing low IADL (Arokiasamy, 2016; Ladusingh & Ngangbam, 2016; Perkins et al., 2016).
Psychological health was having a scale of 0–12 on the basis of experiencing stressful symptoms and was recoded as 0 “high” (representing 6+ scores) and 1 “low” (representing score 5 and less) (Jacob, Bhugra, & Mann, 1997; Shidhaye & Patel, 2010). Subjective wellbeing was having a scale of 0–9 and was categorized as 0 “high” experiencing better experience (representing 6+ scores) and 1 “low” experiencing negative experience (representing score 5 and less) (Sell & Taylor, 1994). Cognitive ability was measured by number of words recall. To measure cognitive ability a scale of 0–8 was prepares representing higher the score better the cognitive ability. Five or more words were recoded as “0” “high” representing better cognitive ability and score of four or less was recoded as “1” “low “representing low cognitive ability (Skirbekk & James, 2014). All the outcome variables were based on Likert scaling (five point scale), and these were recoded as per the literature suggested (Joe et al., 2019). Here it has to be noted that high represents positive aspect whereas low represents negative one.
Predictor variables
The main predictor variable was “whether respondent faced any type of violence after turning age 60 years and above”? and the variable was coded as “0” no and “1” yes. Age was coded as (60–69 years, 70–79 years and 80+ years), educational status was coded as (no education, below than 5 years, 6–10 years and 11+ years), marital status was coded as (not in union and currently in union), working status was coded as (no and yes), community involvement was coded as (no and yes), trust over someone was coded as (no and yes) and living arrangement was coded as (living alone, with spouse, with children and others). Chronic morbidity was coded as (no and yes) and disability was coded as (no and yes). Wealth was coded as (poorest, poorer, middle, richer and richest), religion was coded as (Hindu, Muslim, Sikh and Others), caste was coded as (Scheduled Caste, Scheduled Tribe, Other Backward Class and Others), and place of residence was coded as (rural and urban). Data was collected for seven states in India Himachal Pradesh, Punjab, Kerala, Tamil Nadu, Orissa, West Bengal and Maharashtra.
Statistical analysis
Descriptive statistics and bivariate analysis was used to find the preliminary results. Further, multivariate analysis (binary logistic) has been done to fulfil the objective of the study. The outcome variables used for analysis were self-rated health (0 “good” and 1 “poor”), ADL (0 “high” and 1 “low”), IADL (0 “high” and 1 “low”), psychological health (0 “high” and 1 “low”), subjective well-being (0 “high” and 1 “low”) and cognitive ability (0 “high” and 1 “low”). The results were presented in the form of odds ratio (OR) with a 95% confidence interval (CI).
The model is usually put into a more compact form as follows:
Where are regression coefficients indicating the relative effect of a particular explanatory variable on the outcome. These coefficients change as per the context in the analysis in the study.
Results
Table 1 represents the socio-economic characteristics of the study population. About 10.7% of men and 11.3% of women faced violence after crossing age 60 years. Nearly 11% of men and only 3% women had 11 and more years of education. Near about 16% of men and 61% of women in India were not in union. Huge disparity in working status among men and women in older ages can be observed i.e., about 39% of men were currently working where only 11% of women were working in their older ages. Interestingly, 2% of men and 9.5% of women were living alone. About 62% of men and 68% of women suffered from chronic diseases whereas 71% of men and 74% of women had disability in older ages.
Table 1.
Socio-economic characteristics of study population.
| Background characteristics | Men | Women | ||
| Sample | % | Sample | % | |
| Experienced violence | ||||
| No | 3889 | 89.3 | 4283 | 88.7 |
| Yes | 464 | 10.7 | 545 | 11.3 |
| Age (years) | ||||
| 60-69 | 2690 | 61.8 | 2980 | 61.7 |
| 70-79 | 1189 | 27.3 | 1337 | 27.7 |
| 80+ | 474 | 10.9 | 511 | 10.6 |
| Educational status | ||||
| No education | 1502 | 34.5 | 3151 | 65.3 |
| Below 5 years | 998 | 22.9 | 894 | 18.5 |
| 6–10 Years | 1433 | 32.9 | 642 | 13.3 |
| 11+ years | 420 | 9.7 | 140 | 2.9 |
| Marital status | ||||
| Not in union | 687 | 15.8 | 2942 | 60.9 |
| Currently in union | 3666 | 84.2 | 1886 | 39.1 |
| Working status | ||||
| No | 2666 | 61.3 | 4301 | 89.1 |
| Yes | 1687 | 38.7 | 527 | 10.9 |
| Community involvement | ||||
| No | 688 | 15.8 | 1199 | 24.8 |
| Yes | 3665 | 84.2 | 3629 | 75.2 |
| Trust over someone | ||||
| No | 629 | 14.5 | 941 | 19.5 |
| Yes | 3724 | 85.5 | 3887 | 80.5 |
| Living arrangement | ||||
| Alone | 88 | 2.0 | 457 | 9.5 |
| With spouse | 916 | 21.0 | 548 | 11.3 |
| With children | 3071 | 70.6 | 3409 | 70.6 |
| Others | 278 | 6.4 | 415 | 8.6 |
| Chronic morbidity | ||||
| No | 1672 | 38.4 | 1570 | 32.5 |
| Yes | 2681 | 61.6 | 3258 | 67.5 |
| Disability | ||||
| No | 1260 | 29.0 | 1246 | 25.8 |
| Yes | 3093 | 71.1 | 3582 | 74.2 |
| Wealth index | ||||
| Poorest | 982 | 22.6 | 1187 | 24.6 |
| Poorer | 939 | 21.6 | 1086 | 22.5 |
| Middle | 886 | 20.4 | 1019 | 21.1 |
| Richer | 861 | 19.8 | 847 | 17.5 |
| Richest | 684 | 15.7 | 688 | 14.3 |
| Religion | ||||
| Hindu | 3499 | 80.4 | 3804 | 78.8 |
| Muslim | 271 | 6.2 | 374 | 7.8 |
| Sikh | 409 | 9.4 | 439 | 9.1 |
| Others | 175 | 4.0 | 211 | 4.4 |
| Caste | ||||
| Scheduled Caste | 921 | 21.2 | 976 | 20.2 |
| Scheduled Tribe | 234 | 5.4 | 281 | 5.8 |
| Other Backward Class | 1575 | 36.2 | 1778 | 36.8 |
| Others | 1622 | 37.3 | 1794 | 37.2 |
| Place of residence | ||||
| Rural | 3249 | 74.6 | 3541 | 73.3 |
| Urban | 1104 | 25.4 | 1287 | 26.7 |
| State | ||||
| Kerala | 568 | 13.1 | 771 | 16.0 |
| Himachal Pradesh | 714 | 16.4 | 742 | 15.4 |
| Punjab | 595 | 13.7 | 645 | 13.4 |
| West Bengal | 537 | 12.3 | 590 | 12.2 |
| Orissa | 739 | 17.0 | 714 | 14.8 |
| Maharashtra | 582 | 13.4 | 653 | 13.5 |
| Tamil Nadu | 617 | 14.2 | 712 | 14.7 |
| Total | 4353 | 100.0 | 4828 | 100.0 |
%: Percentage.
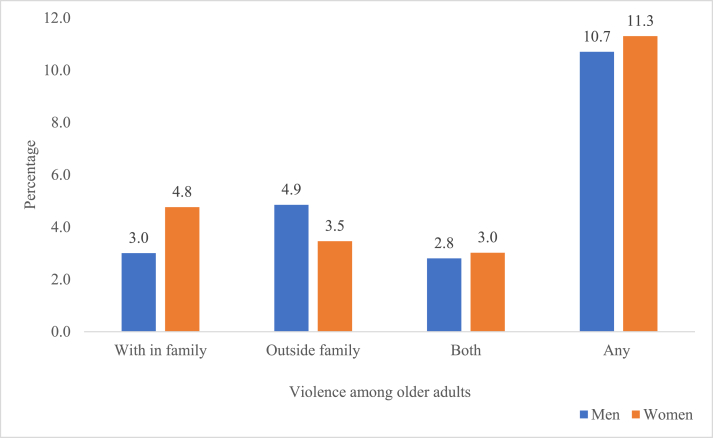
Fig. 1 depicts percentage of older adults faced violence in India. About 3.0 per cent and 4.8 per cent of older men and women faced violence within family. Nearly, 4.9 per cent and 3.5 per cent of older men and women faced violence outside family and similarly, almost 2.8 per cent and 3.0 per cent of older men and women faced violence within and outside family in India respectively.
Fig. 1.
Percentage of older adults faced violence in India.
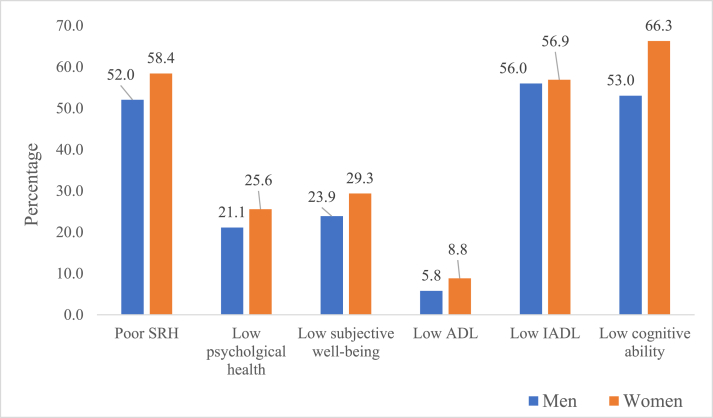
Fig. 2 represents the percentage of older adults living having adverse health outcome. It was found that older women were at disadvantageous state in every health outcome i.e. having poor health outcome for SRH, ADL, IADL, psychological health, subjective well-being and cognitive ability.
Fig. 2.
Percentage of health outcomes among older adults in India.
Table 2 and 3 represents the association of health of older adults with background characteristics in India. Health indicators include poor-SRH, low ADL, low IADL, low psychological health, low subjective well-being and low cognitive ability. The results in tables show clear gender differentials for overall health among older adults. For instance in table-2 and 3 it was revealed that older adults who ever faced violence after turning age 60 years and above had lower health status i.e., poor-SRH (men: 58.9% and women: 64.7%), low ADL (men: 8.2% and women: 9.1%), low IADL (men: 59.6% and women: 65,4%), low psychological health (men: 27.9% and women: women: 38.6%) and low subjective well-being (men: 30.7% and women: 48.7%) and low cognitive ability (men: 58.8% and women: 68.1%). It was revealed that older women who experienced violence had high percentage of poor health outcomes in comparison to men who faced violence.
Table 2.
Bivariate association between poor-SRH, low ADL and low IADL by background characteristics among older adults in India.
| Background characteristics | Poor-SRH |
Low ADL |
Low IADL |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Men (%) |
Women (%) |
Women-Men (%) |
Men (%) |
Women (%) |
Women-Men (%) |
Men (%) |
Women (%) |
Women-Men (%) |
|
| P < 0.05 | P < 0.05 | P < 0.05 | |||||||
| Experienced violence | |||||||||
| No | 51.2 | 57.6 | 6.4* | 5.5 | 8.8 | 3.3* | 55.5 | 55.8 | 0.3 |
| Yes | 58.9 | 64.7 | 5.8* | 8.2 | 9.1 | 0.9 | 59.6 | 65.4 | 5.8* |
| Age (years) | |||||||||
| 60-69 | 46.3 | 52.8 | 6.5* | 2.5 | 4.1 | 1.6* | 48.2 | 45.8 | −2.4 |
| 70-79 | 59.3 | 65.1 | 5.7* | 7.4 | 11.4 | 4.1* | 62.3 | 70.3 | 8.0* |
| 80+ | 66.1 | 73.5 | 7.4* | 20.6 | 29.5 | 8.9* | 84.4 | 86.6 | 2.2 |
| Educational status | |||||||||
| No education | 59.3 | 62.0 | 2.8 | 7.0 | 10.0 | 2.9 | 71.8 | 68.4 | −3.5* |
| Below 5 years | 55.8 | 58.4 | 2.6 | 7.6 | 7.6 | 0.0 | 57.1 | 45.1 | −12.0* |
| 6–10 Years | 45.6 | 43.5 | −2.2 | 4.0 | 5.5 | 1.5* | 47.1 | 24.7 | −22.3* |
| 11+ years | 39.2 | 46.2 | 7.0* | 3.1 | 5.8 | 2.7 | 27.2 | 21.8 | −5.3 |
| Marital status | |||||||||
| Not in union | 59.2 | 61.9 | 2.7 | 9.8 | 10.8 | 0.9 | 66.1 | 61.9 | −4.2 |
| Currently in union | 50.7 | 53.0 | 2.3* | 5.0 | 5.8 | 0.8 | 54.1 | 49.1 | −5.0* |
| Working status | |||||||||
| No | 55.6 | 59.5 | 3.9* | 8.6 | 9.8 | 1.2 | 63.1 | 59.5 | −3.6 |
| Yes | 46.4 | 49.6 | 3.2 | 1.3 | 0.6 | −0.8 | 44.7 | 35.9 | −8.8* |
| Community involvement | |||||||||
| No | 61.8 | 65.8 | 3.9 | 15.6 | 18.9 | 3.3* | 68.6 | 76.1 | 7.5* |
| Yes | 50.2 | 56.0 | 5.8* | 3.9 | 5.5 | 1.6 | 53.6 | 50.6 | −3.0 |
| Trust over someone | |||||||||
| No | 59.1 | 61.6 | 2.5 | 11.3 | 10.3 | −1.1 | 66.9 | 66.0 | −0.9 |
| Yes | 50.8 | 57.6 | 6.8* | 4.8 | 8.5 | 3.6* | 54.1 | 54.7 | 0.6 |
| Living arrangement | |||||||||
| Alone | 56.8 | 56.6 | −0.2 | 2.0 | 3.4 | 1.4 | 41.4 | 34.9 | −6.6 |
| With spouse | 48.6 | 52.4 | 3.7* | 4.4 | 2.5 | −1.9 | 54.4 | 37.2 | −17.2* |
| With children | 52.3 | 59.0 | 6.7* | 6.3 | 10.2 | 3.9* | 56.8 | 62.5 | 5.7* |
| Others | 59.3 | 63.6 | 4.3 | 6.4 | 12.1 | 5.8* | 56.3 | 60.9 | 4.6* |
| Chronic morbidity | |||||||||
| No | 37.9 | 43.4 | 5.5* | 2.1 | 3.8 | 1.7* | 54.8 | 52.3 | −2.6 |
| Yes | 60.8 | 65.6 | 4.8* | 8.1 | 11.2 | 3.1* | 56.7 | 59.1 | 2.5* |
| Disability | |||||||||
| No | 31.0 | 37.0 | 6.0* | 0.5 | 1.6 | 1.1 | 50.2 | 43.1 | −7.1* |
| Yes | 60.6 | 65.9 | 5.3* | 7.9 | 11.3 | 3.4* | 58.3 | 61.7 | 3.4* |
| Wealth index | |||||||||
| Poorest | 59.1 | 64.1 | 5.0 | 7.6 | 8.4 | 0.8 | 69.0 | 66.2 | −2.8 |
| Poorer | 53.7 | 57.9 | 4.2 | 5.2 | 9.5 | 4.3* | 57.8 | 60.3 | 2.4 |
| Middle | 50.9 | 55.7 | 4.9* | 7.4 | 8.4 | 1.0 | 58.3 | 52.0 | −6.3* |
| Richer | 45.5 | 52.0 | 6.4* | 4.0 | 9.0 | 5.1* | 51.0 | 51.3 | 0.3 |
| Richest | 49.3 | 61.3 | 12.0* | 4.2 | 9.0 | 4.7* | 38.0 | 49.7 | 11.7* |
| Religion | |||||||||
| Hindu | 49.8 | 55.7 | 5.8* | 5.9 | 8.4 | 2.5* | 57.2 | 57.0 | −0.2 |
| Muslim | 60.8 | 70.7 | 9.9* | 7.3 | 15.1 | 7.8* | 52.3 | 60.8 | 8.5* |
| Sikh | 63.5 | 68.3 | 4.8* | 4.4 | 6.8 | 2.4 | 61.2 | 62.0 | 0.9 |
| Others | 56.0 | 65.7 | 9.7 | 3.8 | 9.0 | 5.2* | 24.2 | 36.6 | 12.4* |
| Caste | |||||||||
| Scheduled Caste | 57.5 | 62.6 | 5.1 | 6.9 | 8.7 | 1.8* | 60.3 | 65.7 | 5.4* |
| Scheduled Tribe | 44.4 | 48.2 | 3.8 | 5.1 | 6.2 | 1.1 | 63.0 | 64.9 | 1.9 |
| Other Backward Class | 50.2 | 55.8 | 5.6* | 6.6 | 8.4 | 1.8* | 56.8 | 49.6 | −7.2* |
| Others | 51.8 | 60.3 | 8.5* | 4.5 | 9.7 | 5.2* | 51.8 | 58.1 | 6.4* |
| Place of residence | |||||||||
| Rural | 53.7 | 60.0 | 6.2* | 6.2 | 9.1 | 2.8* | 57.7 | 60.9 | 3.2 |
| Urban | 47.1 | 54.1 | 7.0* | 4.5 | 8.2 | 3.6* | 50.8 | 45.8 | −5.0 |
| State | |||||||||
| Kerala | 62.5 | 70.5 | 8.0* | 5.2 | 12.8 | 7.6* | 65.2 | 33.9 | −31.3 |
| Himachal Pradesh | 42.1 | 50.2 | 8.1* | 5.0 | 9.8 | 4.8* | 44.3 | 64.0 | 19.7* |
| Punjab | 63.2 | 69.6 | 6.3* | 3.8 | 6.4 | 2.6* | 40.5 | 60.7 | 20.3 |
| West Bengal | 75.0 | 80.5 | 5.6* | 9.3 | 12.9 | 3.6* | 36.3 | 74.4 | 38.1* |
| Orissa | 46.1 | 48.9 | 2.8 | 8.2 | 8.9 | 0.7 | 33.8 | 76.1 | 42.3* |
| Maharashtra | 38.0 | 44.0 | 6.0 | 4.5 | 3.8 | −0.7 | 56.4 | 51.4 | −5.0* |
| Tamil Nadu |
43.6 |
48.3 |
4.7 |
4.4 |
6.8 |
2.4 |
35.0 |
42.1 |
7.1* |
| Total | 52.0 | 58.4 | 6.4* | 5.8 | 8.8 | 3.0* | 56.0 | 56.9 | 0.9* |
%: Percentage; *if p < 0.05.
SRH: Self-Rated Health (coded in binary form i.e. poor “poor or Fair” and good “Excellent, very good and good”).
ADL: Activities of Daily living (coded in binary i.e. low “scores of 5 or less” and high “scores 6+”).
IADL: Instrumental Activities of Daily living (coded in binary i.e. low “scores of 5 or less” and high “scores 6+”).
Table 3.
Bivariate association between low psychological health, low subjective well-being and low cognitive ability by background characteristics among older adults in India.
| Background characteristics |
Low Psychological health |
Low subjective well-being |
Low cognitive ability |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Men (%) |
Women (%) |
Women-Men (%) |
Men (%) |
Women (%) |
Women-Men (%) |
Men (%) |
Women (%) |
Women-Men (%) |
|
| P<0.05 | P<0.05 | P<0.05 | |||||||
| Experienced violence | |||||||||
| No | 20.3 | 23.9 | 3.6* | 23.1 | 26.9 | 3.8* | 53.3 | 66.1 | 12.7* |
| Yes | 27.9 | 38.6 | 10.8* | 30.7 | 48.7 | 18.1* | 50.8 | 68.1 | 17.3* |
| Age (years) | |||||||||
| 60-69 | 18.5 | 21.1 | 2.7* | 21.0 | 25.3 | 4.3* | 45.8 | 59.8 | 14.1* |
| 70-79 | 23.1 | 30.5 | 7.4* | 25.9 | 33.6 | 7.8* | 60.3 | 75.2 | 14.9* |
| 80+ | 30.9 | 38.5 | 7.6 | 35.2 | 41.9 | 6.6* | 76.2 | 80.7 | 4.5* |
| Educational status | |||||||||
| No education | 30.3 | 30.7 | 0.4 | 35.6 | 35.6 | 0.1 | 66.5 | 72.6 | 6.1* |
| Below 5 years | 23.5 | 21.0 | −2.5* | 27.0 | 20.8 | −6.2* | 62.9 | 64.4 | 1.4 |
| 6–10 Years | 13.5 | 10.5 | −3.0 | 13.7 | 14.1 | 0.4 | 38.7 | 45.3 | 6.5 |
| 11+ years | 8.4 | 8.3 | −0.2 | 9.6 | 12.4 | 2.8 | 30.4 | 32.7 | 2.3 |
| Marital status | |||||||||
| Not in union | 25.6 | 29.3 | 3.7 | 30.4 | 33.5 | 3.1* | 65.3 | 69.8 | 4.5* |
| Currently in union | 20.3 | 19.8 | −0.5 | 22.7 | 22.9 | 0.3 | 50.8 | 60.8 | 10.1* |
| Working status | |||||||||
| No | 23.1 | 25.7 | 2.6* | 26.9 | 28.4 | 1.5* | 55.4 | 66.4 | 11.0* |
| Yes | 17.9 | 24.6 | 6.7* | 19.2 | 37.4 | 18.2* | 49.3 | 65.0 | 15.8* |
| Community involvement | |||||||||
| No | 32.3 | 35.8 | 3.5 | 39.4 | 40.9 | 1.5 | 61.8 | 75.1 | 13.3* |
| Yes | 19.0 | 22.2 | 3.2* | 21.0 | 25.5 | 4.6* | 51.4 | 63.4 | 12.0* |
| Trust over someone | |||||||||
| No | 35.9 | 39.0 | 3.1 | 43.4 | 42.8 | −0.6 | 64.4 | 70.2 | 5.8* |
| Yes | 18.6 | 22.3 | 3.7* | 20.6 | 26.1 | 5.5* | 51.1 | 65.3 | 14.2* |
| Living arrangement | |||||||||
| Alone | 35.8 | 32.4 | −3.4 | 36.6 | 40.4 | 3.8 | 66.8 | 61.9 | −5.0 |
| With spouse | 21.8 | 19.0 | −2.7 | 25.1 | 27.0 | 1.9 | 47.1 | 57.1 | 10.0* |
| With children | 20.3 | 25.4 | 5.1* | 22.8 | 27.7 | 5.0* | 53.4 | 67.7 | 14.3* |
| Others | 23.3 | 28.3 | 5.0 | 28.2 | 33.5 | 5.3 | 64.5 | 71.9 | 7.4* |
| Chronic morbidity | |||||||||
| No | 19.2 | 21.1 | 1.9 | 21.0 | 25.8 | 4.8* | 44.5 | 59.0 | 14.5* |
| Yes | 22.3 | 27.8 | 5.5* | 25.7 | 31.0 | 5.4* | 58.4 | 69.8 | 11.4* |
| Disability | |||||||||
| No | 12.5 | 11.5 | −1.0 | 13.4 | 18.3 | 4.9* | 36.9 | 49.5 | 12.6* |
| Yes | 24.6 | 30.5 | 5.9* | 28.2 | 33.2 | 5.0* | 59.6 | 72.1 | 12.5* |
| Wealth index | |||||||||
| Poorest | 35.8 | 38.1 | 2.3 | 44.0 | 49.9 | 5.9* | 68.0 | 73.9 | 5.9* |
| Poorer | 27.2 | 31.4 | 4.3 | 31.6 | 32.9 | 1.3 | 58.8 | 70.6 | 11.8* |
| Middle | 18.2 | 21.2 | 3.0 | 20.0 | 21.8 | 1.8 | 52.4 | 66.9 | 14.5* |
| Richer | 12.5 | 17.0 | 4.5* | 11.0 | 18.3 | 7.3* | 39.6 | 57.9 | 18.2* |
| Richest | 6.4 | 11.8 | 5.4* | 5.7 | 13.0 | 7.3* | 41.5 | 55.9 | 14.5* |
| Religion | |||||||||
| Hindu | 23.5 | 27.7 | 4.2* | 26.0 | 30.6 | 4.6* | 52.6 | 66.1 | 13.4* |
| Muslim | 17.6 | 27.3 | 9.7* | 25.2 | 33.2 | 8.0* | 58.7 | 72.9 | 14.2* |
| Sikh | 7.7 | 7.4 | −0.4 | 9.1 | 15.5 | 6.5* | 50.9 | 60.9 | 10.0* |
| Others | 9.6 | 21.9 | 12.3* | 14.1 | 27.7 | 13.6* | 57.3 | 69.6 | 12.3* |
| Caste | |||||||||
| Scheduled Caste | 25.3 | 31.0 | 5.7* | 31.5 | 36.0 | 4.5* | 61.2 | 71.0 | 9.8* |
| Scheduled Tribe | 31.7 | 33.0 | 1.3 | 32.7 | 37.1 | 4.4 | 69.5 | 73.0 | 3.5* |
| Other Backward Class | 24.5 | 26.7 | 2.2* | 25.4 | 30.2 | 4.8* | 48.9 | 63.1 | 14.2* |
| Others | 13.9 | 20.4 | 6.5* | 16.9 | 23.7 | 6.8* | 50.0 | 65.8 | 15.7* |
| Place of residence | |||||||||
| Rural | 22.8 | 27.3 | 4.5* | 25.6 | 30.8 | 5.2* | 56.0 | 69.3 | 13.3* |
| Urban | 16.2 | 21.0 | 4.8* | 19.0 | 25.4 | 6.5* | 44.2 | 58.0 | 13.8* |
| State | |||||||||
| Kerala | 8.6 | 17.5 | 8.9* | 11.7 | 17.1 | 5.4* | 60.6 | 70.5 | 9.9* |
| Himachal Pradesh | 12.7 | 20.8 | 8.1* | 13.2 | 16.3 | 3.0* | 42.0 | 65.8 | 23.7* |
| Punjab | 7.2 | 6.9 | −0.3 | 8.8 | 13.9 | 5.1* | 50.3 | 59.2 | 9.0* |
| West Bengal | 26.6 | 31.8 | 5.2* | 43.0 | 53.0 | 10.0* | 75.4 | 87.7 | 12.3* |
| Orissa | 35.3 | 39.7 | 4.4* | 33.8 | 36.7 | 2.9 | 65.0 | 73.7 | 8.7* |
| Maharashtra | 20.5 | 24.6 | 4.0 | 28.2 | 39.6 | 11.3* | 47.2 | 62.2 | 15.1* |
| Tamil Nadu |
34.5 |
37.7 |
3.3 |
29.3 |
33.8 |
4.5* |
33.4 |
47.1 |
13.8* |
| Total | 21.1 | 25.6 | 4.5* | 23.9 | 29.3 | 5.5* | 53.0 | 66.3 | 13.2* |
%: Percentage; *if p < 0.05.
Psychological health: General Health Scale (coded in binary form i.e. low “scores 5 or less” and high “scores more than 6”).
Subjective well-being: Subjective Well-Being (coded in binary form i.e. low “scores of 5 or less” and high “scores 6+”).
Cognitive ability (coded in binary i.e. low “scores of 4 or less” and high “scores 5+”).
Table 4 and 5 represents logistic regression estimates for poor-SRH, low ADL, low IADL, low psychological health, low subjective well-being and low cognitive ability. Gender differential was observed using interaction model (model-2) for every health outcome. In table 4 (model-1) it was found that older adults who ever faced violence after turning age 60 years had 60%, 41% and 33% higher likelihood to have poor-SRH [OR: 1.60, CI: 1.35,1.89], low ADL [OR: 1.41, CI: 1.05,1.88] and low IADL [OR: 1.33, CI: 1.12,1.58] in comparison to older adults who never faced violence after turning 60 years. In table 5 (model-1) it was found that older adults who ever faced violence after turning age 60 years had 97% and 62% higher likelihood to have lower psychological health [OR: 1.97, CI: 1.65,2.35] and low subjective well-being [OR: 1.62, CI: 1.36,1.92]. Moreover, it was found that no gender differential was found for poor-SRH, low ADL and low IADL via violence. However, in table 5 (model-2) it was found that older women who experienced violence had higher odds of having low psychological health [OR: 1.18, CI: 1.06, 1.63], low subjective well-being [OR: 1.70, CI: 1.24, 2.33] and low cognitive ability [OR: 1.32, CI: 1.04, 1.79] in comparison to men who faced violence.
Table 4.
Logistic regression estimates for poor-SRH, low ADL and low IADL by background characteristics among older adults in India.
| Background characteristics | Poor-SRH |
Low ADL |
Low IADL |
|||
|---|---|---|---|---|---|---|
| Model-1 |
Mode-2 |
Model-1 |
Mode-2 |
Model-1 |
Mode-2 |
|
| AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | |
| Experienced violence | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 1.60*(1.35,1.89) | 1.41*(1.05,1.88) | 1.33*(1.12,1.58) | |||
| Age (years) | ||||||
| 60-69 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 70-79 | 1.27*(1.14,1.42) | 1.27*(1.14,1.42) | 2.1*(1.7,2.6) | 2.1*(1.7,2.6) | 1.86*(1.66,2.08) | 1.86*(1.66,2.08) |
| 80+ | 1.51*(1.27,1.79) | 1.51*(1.27,1.79) | 4.98*(3.91,6.35) | 4.97*(3.9,6.34) | 4.82*(3.92,5.92) | 4.84*(3.93,5.95) |
| Gender | ||||||
| Men | Ref. | Ref. | Ref. | |||
| Women | 0.93(0.83,1.04) | 1.07(0.86,1.33) | 0.59*(0.52,0.67) | |||
| Educational status | ||||||
| No education | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Below 5 years | 0.84*(0.74,0.96) | 0.84*(0.74,0.96) | 1.05(0.82,1.34) | 1.05(0.82,1.34) | 0.59*(0.51,0.67) | 0.59*(0.52,0.67) |
| 6–10 Years | 0.63*(0.55,0.73) | 0.63*(0.55,0.73) | 0.99(0.74,1.33) | 0.99(0.74,1.33) | 0.43*(0.37,0.49) | 0.43*(0.37,0.49) |
| 11+ years | 0.43*(0.35,0.53) | 0.43*(0.35,0.53) | 1.07(0.69,1.66) | 1.07(0.69,1.67) | 0.18*(0.14,0.22) | 0.18*(0.14,0.22) |
| Marital status | ||||||
| Not in union | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Currently in union | 1.01(0.9,1.14) | 1.01(0.9,1.14) | 1.16(0.92,1.45) | 1.16(0.92,1.45) | 0.85*(0.76,0.97) | 0.85*(0.76,0.97) |
| Working status | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.75*(0.66,0.85) | 0.75*(0.66,0.85) | 0.19*(0.12,0.29) | 0.19*(0.12,0.29) | 0.47*(0.41,0.53) | 0.47*(0.41,0.53) |
| Community involvement | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.79*(0.7,0.89) | 0.79*(0.7,0.89) | 0.28*(0.23,0.33) | 0.28*(0.23,0.33) | 0.49*(0.43,0.56) | 0.49*(0.43,0.56) |
| Trust over someone | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.81*(0.71,0.93) | 0.81*(0.71,0.93) | 0.72*(0.57,0.91) | 0.72*(0.57,0.91) | 0.83*(0.72,0.96) | 0.83*(0.72,0.96) |
| Living arrangement | ||||||
| Alone | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| With Spouse | 1.22(0.95,1.56) | 1.22(0.96,1.57) | 2.07*(1.16,3.69) | 2.05*(1.15,3.65) | 3.22*(2.48,4.19) | 3.26*(2.5,4.23) |
| With children | 1.33*(1.07,1.65) | 1.33*(1.08,1.65) | 3.64*(2.21,5.99) | 3.61*(2.19,5.94) | 4.82*(3.82,6.09) | 4.88*(3.86,6.16) |
| Others | 1.25(0.96,1.63) | 1.26(0.96,1.63) | 3.53*(2.01,6.2) | 3.49*(1.99,6.13) | 4.18*(3.16,5.53) | 4.23*(3.19,5.59) |
| Chronic morbidity | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.99*(1.79,2.21) | 1.99*(1.79,2.21) | 2.92*(2.27,3.76) | 2.92*(2.27,3.76) | 1.2*(1.07,1.33) | 1.2*(1.07,1.33) |
| Disability | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 2.35*(2.1,2.63) | 2.35*(2.1,2.63) | 5.61*(3.71,8.5) | 5.61*(3.71,8.49) | 1.26*(1.12,1.42) | 1.26*(1.12,1.42) |
| Wealth index | ||||||
| Poorest | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Poorer | 0.69*(0.59,0.81) | 0.69*(0.59,0.81) | 1.01(0.76,1.34) | 1.01(0.76,1.34) | 0.89(0.75,1.04) | 0.88(0.75,1.04) |
| Middle | 0.58*(0.49,0.69) | 0.58*(0.49,0.69) | 0.85(0.62,1.16) | 0.85(0.62,1.15) | 0.86(0.72,1.02) | 0.86(0.72,1.02) |
| Richer | 0.5*(0.41,0.6) | 0.5*(0.41,0.6) | 0.62*(0.44,0.88) | 0.62*(0.44,0.88) | 0.74*(0.61,0.9) | 0.74*(0.61,0.9) |
| Richest | 0.5*(0.4,0.61) | 0.5*(0.4,0.61) | 0.65*(0.45,0.95) | 0.65*(0.45,0.95) | 0.71*(0.58,0.88) | 0.71*(0.58,0.88) |
| Religion | ||||||
| Hindu | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Muslim | 1.08(0.88,1.32) | 1.08(0.88,1.32) | 1.54*(1.11,2.14) | 1.54*(1.1,2.14) | 1.5*(1.22,1.84) | 1.5*(1.22,1.84) |
| Sikh | 1.07(0.84,1.35) | 1.07(0.84,1.35) | 1.23(0.75,2.02) | 1.23(0.75,2.03) | 1.16(0.91,1.47) | 1.16(0.91,1.48) |
| Others | 1.06(0.84,1.34) | 1.06(0.84,1.34) | 0.93(0.58,1.49) | 0.93(0.58,1.5) | 0.84(0.65,1.1) | 0.84(0.64,1.09) |
| Caste | ||||||
| Scheduled Caste | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Scheduled Tribe | 0.82(0.65,1.04) | 0.82(0.65,1.04) | 0.87(0.53,1.41) | 0.86(0.53,1.41) | 0.93(0.73,1.19) | 0.93(0.73,1.19) |
| Other Backward Class | 1.12(0.96,1.29) | 1.12(0.96,1.29) | 1.07(0.81,1.41) | 1.07(0.81,1.4) | 1(0.86,1.16) | 1(0.86,1.17) |
| Others | 0.97(0.85,1.12) | 0.97(0.85,1.12) | 0.94(0.73,1.22) | 0.94(0.73,1.22) | 0.91(0.79,1.05) | 0.91(0.79,1.05) |
| Place of residence | ||||||
| Rural | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Urban | 0.98(0.89,1.09) | 0.98(0.89,1.09) | 1.05(0.86,1.27) | 1.04(0.86,1.27) | 0.9(0.81,1) | 0.9(0.81,1) |
| State | ||||||
| Kerala | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Himachal Pradesh | 0.42*(0.35,0.51) | 0.42*(0.35,0.51) | 1.05(0.73,1.51) | 1.05(0.73,1.5) | 2.57*(2.1,3.16) | 2.58*(2.1,3.16) |
| Punjab | 0.93(0.74,1.18) | 0.93(0.74,1.18) | 0.6*(0.37,0.99) | 0.6*(0.37,0.98) | 2.76*(2.15,3.53) | 2.75*(2.15,3.53) |
| West Bengal | 1.55*(1.25,1.92) | 1.55*(1.25,1.92) | 1.43*(1.01,2.02) | 1.43*(1.01,2.02) | 5.05*(4.06,6.27) | 5.05*(4.06,6.28) |
| Orissa | 0.32*(0.26,0.39) | 0.32*(0.26,0.39) | 1.05(0.74,1.5) | 1.05(0.74,1.5) | 5.09*(4.11,6.3) | 5.08*(4.11,6.29) |
| Maharashtra | 0.24*(0.2,0.29) | 0.24*(0.2,0.29) | 0.43*(0.29,0.66) | 0.44*(0.29,0.66) | 1.7*(1.4,2.08) | 1.7*(1.39,2.08) |
| Tamil Nadu | 0.55*(0.45,0.67) | 0.55*(0.45,0.67) | 1.39(0.96,2.03) | 1.39(0.96,2.03) | 3.22*(2.61,3.97) | 3.22*(2.61,3.97) |
| Gender # experienced violence | ||||||
| Men # yes | Ref. | Ref. | Ref. | |||
| Men # no | 0.65*(0.52,0.83) | 0.61*(0.4,0.94) | 0.90(0.7,1.15) | |||
| Women # no | 0.60*(0.47,0.77) | 0.68(0.44,1.04) | 0.51*(0.4,0.66) | |||
| Women # yes | 1.00(0.74,1.36) | 0.86(0.51,1.45) | 0.79(0.58,1.09) | |||
*if p < 0.05; AOR: Adjusted odds ratio; CI: Confidence interval; #: Interaction term; Ref: Reference.
SRH: Self-Rated Health (coded in binary form i.e. poor “poor or Fair” and good “Excellent, very good and good”).
ADL: Activities of Daily living (coded in binary i.e. low “scores of 5 or less” and high “scores 6+”).
IADL: Instrumental Activities of Daily living (coded in binary i.e. low “scores of 5 or less” and high “scores 6+).
Table 5.
Logistic regression estimates for low psychological health, low subjective well-being and low cognitive ability by background characteristics among older adults in India.
| Background characteristics | Low Psychological health |
Low subjective well-being |
Low cognitive ability |
|||
|---|---|---|---|---|---|---|
| Model-1 |
Mode-2 |
Model-1 |
Mode-2 |
Model-1 |
Mode-2 |
|
| AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | AOR [95% CI) | |
| Experienced violence | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 1.97*(1.65,2.35) | 1.62*(1.36,1.92) | 0.79(0.45,1.15) | |||
| Age (years) | ||||||
| 60-69 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 70-79 | 1.22*(1.08,1.39) | 1.22*(1.08,1.39) | 1.26*(1.11,1.43) | 1.26*(1.11,1.43) | 1.5*(1.34,1.68) | 1.5*(1.34,1.68) |
| 80+ | 1.52*(1.27,1.83) | 1.53*(1.27,1.84) | 1.56*(1.31,1.87) | 1.58*(1.32,1.89) | 2.17*(1.8,2.61) | 2.18*(1.81,2.62) |
| Gender | ||||||
| Men | Ref. | Ref. | Ref. | |||
| Women | 0.86*(0.75,0.99) | 0.95(0.83,1.09) | 1.13*(1,1.27) | |||
| Educational status | ||||||
| No education | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Below 5 years | 0.73*(0.63,0.85) | 0.73*(0.63,0.85) | 0.73*(0.63,0.84) | 0.73*(0.63,0.85) | 0.65*(0.57,0.74) | 0.65*(0.57,0.74) |
| 6–10 Years | 0.47*(0.39,0.56) | 0.47*(0.39,0.56) | 0.5*(0.43,0.6) | 0.5*(0.43,0.6) | 0.39*(0.34,0.45) | 0.39*(0.34,0.45) |
| 11+ years | 0.33*(0.24,0.46) | 0.33*(0.24,0.45) | 0.35*(0.25,0.47) | 0.34*(0.25,0.46) | 0.2*(0.16,0.25) | 0.2*(0.16,0.25) |
| Marital status | ||||||
| Not in union | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Currently in union | 1(0.87,1.16) | 1(0.87,1.16) | 0.96(0.84,1.1) | 0.96(0.84,1.1) | 0.93(0.83,1.05) | 0.93(0.83,1.05) |
| Working status | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.79*(0.68,0.91) | 0.79*(0.68,0.91) | 0.8*(0.69,0.92) | 0.8*(0.7,0.92) | 0.87*(0.77,0.98) | 0.87*(0.77,0.98) |
| Community involvement | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.63*(0.56,0.72) | 0.63*(0.56,0.72) | 0.59*(0.52,0.67) | 0.59*(0.52,0.67) | 0.68*(0.6,0.78) | 0.68*(0.6,0.78) |
| Trust over someone | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.69*(0.59,0.79) | 0.68*(0.59,0.79) | 0.61*(0.53,0.71) | 0.61*(0.53,0.7) | 0.74*(0.64,0.85) | 0.74*(0.64,0.85) |
| Living arrangement | ||||||
| Alone | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| With spouse | 0.78(0.59,1.03) | 0.79(0.6,1.04) | 1.09(0.83,1.43) | 1.11(0.85,1.45) | 0.97(0.75,1.24) | 0.97(0.76,1.25) |
| With children | 1.06(0.84,1.34) | 1.07(0.84,1.35) | 1.07(0.85,1.35) | 1.09(0.87,1.37) | 1.11(0.89,1.38) | 1.12(0.9,1.39) |
| Others | 1.26(0.94,1.69) | 1.28(0.95,1.71) | 1.25(0.94,1.66) | 1.28(0.96,1.7) | 1.18(0.9,1.54) | 1.19(0.9,1.55) |
| Chronic morbidity | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.52*(1.33,1.72) | 1.52*(1.33,1.73) | 1.47*(1.3,1.66) | 1.47*(1.3,1.66) | 1.33*(1.2,1.48) | 1.33*(1.2,1.48) |
| Disability | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 2.71*(2.31,3.19) | 2.71*(2.31,3.19) | 2.03*(1.76,2.35) | 2.04*(1.76,2.35) | 1.58*(1.42,1.77) | 1.58*(1.42,1.77) |
| Wealth index | ||||||
| Poorest | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Poorer | 0.99(0.84,1.16) | 0.99(0.84,1.16) | 0.73*(0.62,0.85) | 0.72*(0.62,0.84) | 1.03(0.88,1.21) | 1.03(0.87,1.21) |
| Middle | 0.83(0.69,1.01) | 0.83(0.69,1.01) | 0.51*(0.43,0.62) | 0.51*(0.43,0.62) | 0.85(0.71,1.01) | 0.85(0.71,1.01) |
| Richer | 0.68*(0.55,0.84) | 0.68*(0.55,0.84) | 0.43*(0.35,0.53) | 0.43*(0.35,0.52) | 0.61*(0.51,0.74) | 0.61*(0.51,0.74) |
| Richest | 0.5*(0.39,0.64) | 0.5*(0.39,0.64) | 0.28*(0.22,0.36) | 0.28*(0.22,0.36) | 0.56*(0.45,0.68) | 0.56*(0.45,0.68) |
| Religion | ||||||
| Hindu | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Muslim | 1.23(0.98,1.55) | 1.23(0.98,1.54) | 1.18(0.95,1.47) | 1.18(0.95,1.46) | 0.95(0.77,1.17) | 0.95(0.77,1.16) |
| Sikh | 1.01(0.68,1.5) | 1.01(0.68,1.51) | 1.16(0.82,1.64) | 1.16(0.82,1.65) | 0.96(0.76,1.21) | 0.96(0.76,1.21) |
| Others | 0.93(0.68,1.28) | 0.92(0.67,1.27) | 1.09(0.81,1.46) | 1.07(0.79,1.44) | 1.29*(1.01,1.64) | 1.28*(1.01,1.64) |
| Caste | ||||||
| Scheduled Caste | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Scheduled Tribe | 0.87(0.68,1.12) | 0.88(0.68,1.13) | 0.86(0.67,1.1) | 0.86(0.67,1.11) | 1.02(0.8,1.31) | 1.02(0.8,1.31) |
| Other Backward Class | 0.82*(0.69,0.97) | 0.82*(0.7,0.97) | 1.02(0.87,1.2) | 1.03(0.88,1.21) | 0.99(0.85,1.15) | 0.99(0.85,1.15) |
| Others | 0.83*(0.71,0.98) | 0.83*(0.71,0.98) | 0.83*(0.71,0.97) | 0.83*(0.71,0.97) | 0.95(0.83,1.1) | 0.96(0.83,1.1) |
| Place of residence | ||||||
| Rural | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Urban | 0.96(0.84,1.08) | 0.96(0.84,1.08) | 1.16*(1.03,1.31) | 1.16*(1.03,1.31) | 0.92(0.82,1.02) | 0.92(0.82,1.02) |
| State | ||||||
| Kerala | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Himachal Pradesh | 1.1(0.85,1.42) | 1.1(0.85,1.43) | 0.88(0.68,1.13) | 0.88(0.68,1.13) | 0.43*(0.35,0.52) | 0.43*(0.35,0.52) |
| Punjab | 0.44*(0.3,0.65) | 0.44*(0.3,0.65) | 0.62*(0.44,0.87) | 0.62*(0.44,0.87) | 0.49*(0.38,0.62) | 0.49*(0.38,0.62) |
| West Bengal | 2.14*(1.68,2.74) | 2.15*(1.68,2.75) | 4.24*(3.36,5.35) | 4.25*(3.37,5.37) | 2.19*(1.75,2.75) | 2.2*(1.75,2.75) |
| Orissa | 2.39*(1.87,3.04) | 2.38*(1.87,3.04) | 1.62*(1.28,2.05) | 1.61*(1.27,2.04) | 0.7*(0.57,0.86) | 0.7*(0.57,0.86) |
| Maharashtra | 1.22(0.96,1.56) | 1.22(0.95,1.56) | 2.18*(1.75,2.73) | 2.19*(1.75,2.74) | 0.49*(0.41,0.6) | 0.49*(0.41,0.6) |
| Tamil Nadu | 5.47*(4.28,6.99) | 5.47*(4.28,7) | 2.32*(1.83,2.94) | 2.32*(1.83,2.94) | 0.31*(0.25,0.38) | 0.31*(0.26,0.38) |
| Gender # experienced violence | ||||||
| Men # yes | Ref. | Ref. | Ref. | |||
| Men # no | 0.63*(0.48,0.81) | 0.9(0.7,1.17) | 1.39*(1.1,1.76) | |||
| Women # no | 0.51*(0.39,0.67) | 0.79(0.61,1.03) | 1.54*(1.21,1.97) | |||
| Women # yes | 1.18*(1.06,1.63) | 1.70*(1.24,2.33) | 1.32*(1.04,1.79) | |||
*if p < 0.05; AOR: Adjusted odds ratio; CI: Confidence interval; #: Interaction term; Ref: Reference.
Psychological health: General Health Scale (coded in binary form i.e. low “scores 5 or less” and high “scores more than 6”).
Subjective well-being: Subjective Well-Being (coded in binary form i.e. low “scores of 5 or less” and high “scores 6+”).
Cognitive ability (coded in binary i.e. low “scores of 4 or less” and high “scores 5+”).
Discussion
The responsibility of caring for the older adults in India is traditionally borne by the immediate family (Gupta, 2009b). Recent studies have also reported a negative feeling about care-giving among the younger generation, which has resulted in a higher level of intergenerational conflict and high levels of conflict between caregivers and older parents (Dhar, 2012). Further, the older adults are more vulnerable and often experience violence due to their progressive dependence, worsened physical and functional health and feelings of helplessness and loneliness (Yadav et al., 2018).
Present study found that 1 in 10 older men and women reported any type of violence from within or outside their family alike. The analyses also suggest that the violence has a significant negative association with the health-related outcomes of older adults in India. The results support the hypothesis outlined in this study that the violence may be thought as a stressful event in later life which has negative impact on the health outcomes of older adults. A large number of studies in India highlight that older women are more likely than men to experience violence (Bhattacharya & Bhattacharya, 2014; Kumar & Bhargava, 2014; Sathya & Premkumar, 2020; Sebastian & Sekher, 2010; Skirbekk & James, 2014; Soneja, 2011).
The results in our study also suggest that women are more vulnerable than men when encountering any type of violence from within or outside their family. This might be because those women have fewer psychosocial resources to cope with the negative environment (Soneja, 2011). Besides, previous studies have suggested that women experience greater health problems such as disability, functional limitations and psychological distress than men (Bora & Saikia, 2015; Kastor & Mohanty, 2016). The interaction effect of gender and violence in the present study significantly shows that the older women who experienced any violence reported poor health-related outcomes than men in all aspects.
The findings on the psychological effects of violence predominate in the literature on violence against older adults (Acierno et al., 2019; Amstadter et al., 2011; Dong, 2015; Evandrou, Falkingham, Qin, & Vlachantoni, 2017; Farhat, Berbiche, & Vasiliadis, 2020; Wong & Waite, 2017b). Qualitative studies in India have also shown that older adults reported feelings of being neglected, higher degrees of loneliness, and poor health status (Dhar, 2012; Gupta, Pillai, & Levy, 2012; Patel & Prince, 2001; Sharma, 2012; Soneja, 2011). Consistent with other studies, suggesting that there is a harmful link between violence and psychological health, our results demonstrate that in the seven major Indian states represented in this study, the older adults especially women who had faced violence reported poor psychological health.
Moreover, the earlier studies reported reduced quality of life and satisfaction with life associated with abuse against older adults (Chokkanathan & Lee, 2005). Abuse against older adults has also been associated with physical problems (Farhat et al., 2020; Lacey & Mouzon, 2016). Consistently, the present study also found that those who experienced violence reported low subjective well-being and that the older adults who had experienced violence from within or outside their family reported poorer self-rated health. Further, the family members assume the daily activities of older adults as an additional job in their personal daily routine, which might lead to increased conflict at the family level, which in turn puts them at risk of violence (Lachs, Williams, O'Brien, Hurst, & Horwitz, 1997). This also indicates that the older adults with poor health status are incapable of performing activities for themselves and are at higher risk of facing violence and it may eventually worsen their health. The results in agreement with this show that ADL and IADL were reported worse by the older parents who faced any type of violence.
Conclusion
The results show a positive association between violence and poor health related-outcomes among a large sample of older adults in India, while adjusting for many demographic and socioeconomic characteristics. The study also suggests important gender differences in how violence predicts health outcomes for older women than for older men. Study findings indicate the immediate need for assessing victim health outcomes following any type of violence in later years to determine related policies and programs to protect the victims. The violence against older adults must be recognized as a key public health issue and appropriate policies and practices must be put in place to stop ill-treatment that affect physical and mental health of older Indians. Reducing violence will have a positive impact on physical and mental health outcomes late in life as well as the functional independence of older adults.
An important limitation of this study was that the abuse against older adults might be under-reported, as the study suggests (Chokkanathan et al., 2014), the older adults in India derive meaning and purpose from familial relationships and, thus, may not report any type of violence for fear of disrupting familial harmony and losing their family permanently. Another limitation is that concerning the presence of any type of violence within or outside family, several types of violence might have cumulative effect on different health outcomes of older people that may bias our study results.
Declarations
Ethics approval and consent to participate: The data is freely available in public domain and survey agencies that conducted the field survey for the data collection have collected a prior consent from the respondent. Local ethics committee of Institute for Social And Economic Change, Bangalore, ruled that no formal ethics approval was required to carry out research from this data source.
Consent for publication
Not applicable.
Availability of data and materials
The study utilises secondary source of data which is freely available in public domain through http://www.isec.ac.in/
Funding
Authors did not received any funding to carry out this research.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
Contributor Information
Shobhit Srivastava, Email: shobhitsrivastava889@gmail.com.
T. Muhammad, Email: muhammad@iips.net, muhammad.iips@gmail.com.
Abbreviations
- SRH
Self-rated health
- ADL
Activities of daily living
- IADL
Instrumental activities of daily living
- OR
Odds ratio
- CI
Confidence Interval
- BKPAI
Building a Knowledge Base on Population Aging in India
References
- Acierno R., Watkins J., Hernandez-Tejada M.A., Muzzy W., Frook G., Steedley M. Mental health correlates of financial mistreatment in the national elder mistreatment study wave II. Journal of Aging and Health. 2019;31(7):1196–1211. doi: 10.1177/0898264318767037. [DOI] [PubMed] [Google Scholar]
- Amstadter A.B., Begle A.M., Cisler J.M., Hernandez M.A., Muzzy W., Acierno R. Prevalence and correlates of poor self-rated health in the United States: The national elder mistreatment study. American Journal of Geriatric Psychiatry. 2010;18(7):615–623. doi: 10.1097/JGP.0b013e3181ca7ef2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter A.B., Zajac K., Strachan M., Hernandez M.A., Kilpatrick D.G., Acierno R. Prevalence and correlates of elder mistreatment in South Carolina: The South Carolina elder mistreatment study. Journal of Interpersonal Violence. 2011;26(15):2947–2972. doi: 10.1177/0886260510390959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arokiasamy P. Age and socioeconomic gradients of health of Indian Adults : An assessment of self-reported and biological measures of health. Journal of Cross-Cultural Gerontology. 2016 doi: 10.1007/s10823-016-9283-3. [DOI] [PubMed] [Google Scholar]
- Berkman L.F., Sekher T.V., Capistrant B., Zheng Y. Ageing in Asia. 2012. Social networks, family, and care giving among older adults in India. [Google Scholar]
- Berkman L.F., Sekher T.V., Capistrant B., Zheng Y. Population aging. 2012. Social networks, family, and care giving among older adults in India; pp. 209–225. [DOI] [Google Scholar]
- Bhattacharya S., Bhattacharya S. What happens to the “hand that rocked the cradle”? A study of elderly abuse in India. The Journal of Adult Protection. 2014;16(3):166–179. doi: 10.1108/JAP-03-2013-0012. [DOI] [Google Scholar]
- Bora J.K., Saikia N. Gender differentials in self-rated health and self-reported disability among adults in. 2015. 1-14. [DOI] [PMC free article] [PubMed]
- Chaurasia H., Srivastava S. Abuse, neglect, and disrespect against older adults in India. Journal of Population Ageing. 2020 doi: 10.1007/s12062-020-09270-x. [DOI] [Google Scholar]
- Chokkanathan S., Lee A.E.Y. Elder mistreatment in urban India: A community based study. Revista HCPA, Porto Alegre. 2005;6566(December 2012):37–41. doi: 10.1300/J084v17n02. [DOI] [PubMed] [Google Scholar]
- Chokkanathan S., Natarajan A. Perceived quality of life following elder mistreatment in rural India. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2018;73(5):e69–e80. doi: 10.1093/geronb/gbx043. [DOI] [PubMed] [Google Scholar]
- Chokkanathan S., Natarajan A., Mohanty J. Elder abuse and barriers to help seeking in Chennai, India: A qualitative study. Journal of Elder Abuse & Neglect. 2014;26(1):60–79. doi: 10.1080/08946566.2013.782786. [DOI] [PubMed] [Google Scholar]
- Dhar R.L. Caregiving for elderly parents: A study from the Indian perspective. Home Health Care Management & Practice. 2012;24(5):242–254. doi: 10.1177/1084822312439466. [DOI] [Google Scholar]
- Dong X.Q. Elder abuse: Systematic review and implications for practice. Journal of the American Geriatrics Society. 2015;63(6):1214–1238. doi: 10.1111/jgs.13454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X.Q., Simon M.A. Elder abuse as a risk factor for hospitalization in older persons. JAMA Internal Medicine. 2013;173(10):911–917. doi: 10.1001/jamainternmed.2013.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evandrou M., Falkingham J.C., Qin M., Vlachantoni A. Elder abuse as a risk factor for psychological distress among older adults in India: A cross-sectional study. BMJ Open. 2017;7(10) doi: 10.1136/bmjopen-2017-017152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhat S.M.M., Berbiche D., Vasiliadis H.M. Family violence associated with self-rated health, satisfaction with life, and health service use in primary care older adults. Journal of Interpersonal Violence. 2020 doi: 10.1177/0886260520938513. [DOI] [PubMed] [Google Scholar]
- Fisher B.S., Regan S.L. The extent and frequency of abuse in the lives of older women and their relationship with health outcomes. The Gerontologist. 2006;46(2):200–209. doi: 10.1093/geront/46.2.200. [DOI] [PubMed] [Google Scholar]
- Gupta R. Systems perspective: Understanding care giving of the elderly in India. Health Care for Women International. 2009;30(12):1040–1054. doi: 10.1080/07399330903199334. [DOI] [PubMed] [Google Scholar]
- Gupta R. Systems perspective: Understanding care giving of the elderly in India. Health Care for Women International. 2009;30(12):1040–1054. doi: 10.1080/07399330903199334. [DOI] [PubMed] [Google Scholar]
- Gupta R., Pillai V.K., Levy E.F. Relationship quality and elder caregiver burden in India. Journal of Social Intervention: Theory and Practice. 2012;21(2):39. doi: 10.18352/jsi.285. [DOI] [Google Scholar]
- Iwaya T., Doi T., Seichi A., Hoshino Y., Ogata T., Akai M. Characteristics of disability in activity of daily living in elderly people associated with locomotive disorders. BMC Geriatrics. 2017;17(1):1–13. doi: 10.1186/s12877-017-0543-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob K.S., Bhugra D., Mann A.H. General health questionnaire -12 : Psychometric properties and factor structure among Indian women living in the United Kingdom. Indian Journal of Psychiatry. 1997;39(3):196–199. [PMC free article] [PubMed] [Google Scholar]
- Joe W., Perkins J.M., Subramanian S.V. Community involvement, trust, and health-related outcomes among older adults in India: A population-based, multilevel, cross-sectional study. Age and Ageing. 2019;48(1):87–93. doi: 10.1093/ageing/afy154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastor A., Mohanty S.K. Associated covariates of functional limitation among older adults in India: An exploration. Ageing International. 2016;41(2):178–192. doi: 10.1007/s12126-016-9241-y. [DOI] [Google Scholar]
- Kumar Y., Bhargava A. Elder abuse in Indian families: Problems and preventive actions. International Journal of Scientific and Research Publications. 2014;4(10):1–8. www.ijsrp.org Retrieved from. [Google Scholar]
- Lacey K.K., Mouzon D.M. Severe physical intimate partner violence and the mental and physical health of U.S. Caribbean black women. Journal of Women's Health. 2016;25(9):920–929. doi: 10.1089/jwh.2015.5293. [DOI] [PubMed] [Google Scholar]
- Lachs M.S., Williams C.S., Brien S.O., Pillemer K.A., Charlson M.E. The Mortality of Elder Mistreatment. 1998;280(5) doi: 10.1001/jama.280.5.428. [DOI] [PubMed] [Google Scholar]
- Lachs M.S., Williams C., O'Brien S., Hurst L., Horwitz R. Risk factors for reported elder abuse and neglect: A nine-year observational cohort study. The Gerontologist. 1997;37(4):469–474. doi: 10.1093/geront/37.4.469. [DOI] [PubMed] [Google Scholar]
- Ladusingh L., Ngangbam S. Domains and determinants of well-being of older adults in India. Journal of Cross-Cultural Gerontology. 2016 doi: 10.1007/s10823-016-9279-z. [DOI] [PubMed] [Google Scholar]
- Li M., Liang Y., Dong X.Q. Different definitions of elder mistreatment and mortality: A prospective cohort study from 2011 to 2017. Journal of the American Geriatrics Society. 2019;67:S506–S512. doi: 10.1111/jgs.15641. [DOI] [PubMed] [Google Scholar]
- Martin P., Hagberg B., Poon L.W. Predictors of loneliness in centenarians: A parallel study. Journal of Cross-Cultural Gerontology. 1997;12(3):203–224. doi: 10.1023/A:1006587502257. [DOI] [PubMed] [Google Scholar]
- Patel V., Prince M. Ageing and mental health in a developing country: Who cares? Qualitative studies from Goa, India. Psychological Medicine. 2001;31(1):29–38. doi: 10.1017/S0033291799003098. [DOI] [PubMed] [Google Scholar]
- Perkins J.M., Lee H. young, James K.S., Oh J., Krishna A., Heo J. Marital status, widowhood duration, gender and health outcomes: A cross-sectional study among older adults in India. BMC Public Health. 2016;16(1):1–12. doi: 10.1186/s12889-016-3682-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sathya T., Premkumar R. Association of functional limitations and disability with elder abuse in India: A cross-sectional study. BMC Geriatrics. 2020;20(1):220. doi: 10.1186/s12877-020-01619-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield M.J., Powers J.R., Loxton D. Mortality and disability outcomes of self-reported elder abuse: A 12-year prospective investigation. Journal of the American Geriatrics Society. 2013;61(5):679–685. doi: 10.1111/jgs.12212. [DOI] [PubMed] [Google Scholar]
- Sebastian D., Sekher T.V. Abuse and neglect of elderly in Indian families: Findings of elder abuse screening test in Kerala. Journal of the Indian Academy of Geoscience. 2010;2(6):54–60. [Google Scholar]
- Sell H., Taylor P. The subjective well-being inventory ( SUBI ) 1994;23(3):89–102. [Google Scholar]
- Selwood A., Cooper C., Livingston G. What is elder abuse - who decides? International Journal of Geriatric Psychiatry. 2007;22(10):1009–1012. doi: 10.1002/gps.1781. [DOI] [PubMed] [Google Scholar]
- Seth N., Yadav A., Adichwal N.K., Kamble S.B. Elder abuse and its association with socio-demographic variables in India. Clinical Epidemiology and Global Health. 2019;7(2):188–191. doi: 10.1016/j.cegh.2018.05.002. [DOI] [Google Scholar]
- Sharma B. Elderly abuse: An emerging public health problem. Health Prospect. 2012;11(1):57–60. doi: 10.3126/hprospect.v11i0.7438. [DOI] [Google Scholar]
- Shidhaye R., Patel V. Association of socio-economic, gender and health factors with common mental disorders in women: A population-based study of 5703 married rural women in India. International Journal of Epidemiology. 2010;39(6):1510–1521. doi: 10.1093/ije/dyq179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirbekk V., James K.S. 2014. Abuse against elderly in India – the role of education. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneja S. 2011. Elder abuse in India: Country report for world health organization.https://www.who.int/ageing/projects/elder_abuse/alc_ea_ind.pdf Retrieved from. [Google Scholar]
- Srivastava S., Bhatia M.S., Rajoura O.P., Joseph J. Elder neglect in changing Indian scenario. Delhi Psychiatry Journal. 2013;16:273–276. [Google Scholar]
- T W. The experience of loneliness of battered old women. Journal of Women & Aging. 2008;17(February 2014):37–41. doi: 10.1300/J074v17n04. [DOI] [PubMed] [Google Scholar]
- Tiwari S.C. Geriatric psychiatric morbidity in rural northern India: Implications for the future. International Psychogeriatrics. 2000;12(1):35–48. doi: 10.1017/S1041610200006189. [DOI] [PubMed] [Google Scholar]
- Ugargol A.P., Bailey A. Family caregiving for older adults: Gendered roles and caregiver burden in emigrant households of Kerala, India. Asian Population Studies. 2018;14(2):194–210. doi: 10.1080/17441730.2017.1412593. [DOI] [Google Scholar]
- Ugargol A.P., Bailey A. Vols. 1–27. Ageing and Society; India: 2020. (Reciprocity between older adults and their care-givers in emigrant households of Kerala). [DOI] [Google Scholar]
- WHO . 2017. Mental health of older adults.https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults Retrieved from. [Google Scholar]
- Wong J.S., Waite L.J. Elder mistreatment predicts later physical and psychological health: Results from a national longitudinal study. Journal of Elder Abuse & Neglect. 2017;29(1):15–42. doi: 10.1080/08946566.2016.1235521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J.S., Waite L.J. Elder mistreatment predicts later physical and psychological health: Results from a national longitudinal study. Journal of Elder Abuse & Neglect. 2017;29(1):15–42. doi: 10.1080/08946566.2016.1235521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav U.N., Tamang M.K., Paudel G., Kafle B., Mehta S., Sekaran V.C. The time has come to eliminate the gaps in the under-recognized burden of elder mistreatment: A community-based, cross-sectional study from rural eastern Nepal. PloS One. 2018;13(6):1–14. doi: 10.1371/journal.pone.0198410. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The study utilises secondary source of data which is freely available in public domain through http://www.isec.ac.in/