Abstract
Background:
As citizens have been forced to stay home during coronavirus disease of 2019 (COVID-19) pandemic, the crisis created unique trends in the neurotrauma patterns with changes in mode, severity, and outcome of head injured patients.
Methods:
Details of neurotrauma admissions under the neurosurgery department at our institute since the onset of COVID-19 pandemic in the country were collected retrospectively and compared to the same period last year in terms of demographic profile, mode of injury, GCS at admission, severity of head injury, radiological diagnosis, management (surgical/conservative), and outcome. The patients were studied according to which phase of pandemic they were admitted in – “lockdown” period (March 25 to May 31, 2020) or “unlock” period (June 1 to September 15, 2020).
Results:
The number of head injuries decreased by 16.8% during the COVID-19 pandemic. Furthermore, during the lockdown period, the number of admissions was 2.7/week while it was 6.8/week during the “unlock” period. RTA was the mode of injury in 29.6% patients during the lockdown, while during the unlock period, it was 56.9% (P = 0.000). Mild and moderate head injuries decreased by 41% and severe head injuries increased by 156.25% during the COVID-19 pandemic (P = 0.000). The mortality among neurotrauma patients increased from 12.4% to 22.5% during the COVID-19 era (P = 0.009).
Conclusion:
We observed a decline in the number of head injury admissions during the pandemic, especially during the lockdown. At the same time, there was increase in the severity of head injuries and associated injuries, resulting in significantly higher mortality in our patients during the ongoing COVID-19 pandemic.
Keywords: Coronavirus disease of 2019, Head injury, Lockdown, Motor vehicle accidents, Neurotrauma, Road traffic accidents, Unlock

INTRODUCTION
The ongoing coronavirus disease of 2019 (COVID-19) pandemic has affected 213 countries and territories across the world with a total of 33,116,863 confirmed cases and there have been 999,540 COVID-19 related deaths at the time of writing this article on date (September 27, 2020).[6] This war-like situation has forced governments and hospitals to take unprecedented steps to control the spread of the disease. Across the world, travel has been strictly restricted. “Social” distancing and universal use of masks have become the “norm.” India reported its first case of COVID-19 on January 30, 2020[24] and looking at the increasing number of cases in spite of the preventive measures, a nation-wide lockdown was implemented on March 25, 2020.[17] During the “lockdown,” the government advised the public to stay home as much as possible and leave home only when absolutely necessary. International travel was banned and domestic travel was majorly curtailed. Companies and offices were advised to allow their employees to work from home as much as possible. To prevent hospitals from becoming the “hot-spots” for the spread of COVID-19, the government advised patients to avoid going to hospitals for minor ailments. Practically, more than 135 million Indians were “locked up” inside their homes for 10 weeks, at the end of which “lockdown” was eased looking at the need to sustain the economy and resume “normalcy.”[9,14] This process of “unlocking” in the country was done in a phased manner and travel and routine work were allowed to a limited extent with necessary precautions. Factories and offices were now allowed to operate, but with reduced manpower while taking adequate precautions.
Our response to COVID-19 pandemic
The institute where the study was carried out is a 960-bedded hospital catering to the Himalayan state of Uttarakhand with a population of about 11 million. Boasting of the only helipad for air-ambulance services in the country,[2] the trauma center at our institute has facilities for neurotrauma, orthopedics, and general trauma specialties, taken care of by departments of neurosurgery, trauma-orthopedics, and trauma surgery respectively, supported by other specialties as and when required. Apart from a fully-functional radiology unit with a computed tomography machine, one magnetic resonance imaging machine, ultrasound, and X-ray facilities, trauma center has four operation rooms (ORs) dedicated for trauma patients, blood bank, and a 30-bedded general trauma ward. Trauma patients of various specialties were admitted in this ward as well as in the departments’ own respective areas. At the time of the onset of pandemic, another 30-bedded general trauma ward, a 15-bedded-private ward area, and a 20-bedded intensive care unit (ICU) dedicated to trauma patients were about to be operational soon in the trauma center. Since the onset of the pandemic, the trauma center in the hospital has been converted into dedicated COVID-19 area and the trauma ORs have been converted into dedicated COVID-19 ORs.
Neurotrauma patients
In our institute, neurosurgery department manages head injury at the trauma center. The “on-call” attending neurosurgeon along with a neurosurgery trainee attends to neurotrauma according to duty roster. In the pre-COVID-19 era, head injury patients were admitted either in the main neurosurgery ward/ICU or in the general trauma ward, where ten beds are dedicated for neurotrauma patients. During the recent division of hospital into COVID-19 and non-COVID-19 areas,[9,17] another area has been designated for neurosurgery ward and ICU. Therefore, currently, all patients of head injury are being admitted along with other neurosurgery patients in this newly designated neurosurgery area.
Change in the work-flow of neurotrauma patients during the COVID-19 pandemic
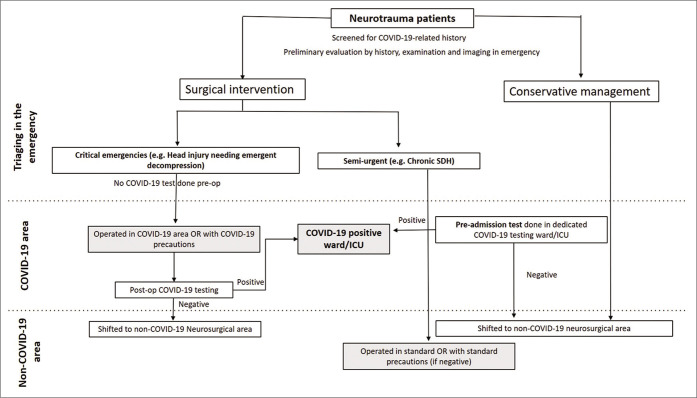
On presentation to the emergency, all patients of head injury are additionally screened for COVID-19 related history and triaged on the basis of management plan. Candidates for surgery are further triaged based on whether it is an acute emergency or a semi-urgent one. Those patients who require a semi-urgent surgery and those who are to be conservatively managed are initially shifted to the dedicated COVID-19 ward/ICU where they undergo COVID-19 testing. General medical management of these patients is initiated here and these patients are shifted to the non-COVID-19 neurosurgical area if they test negative. Patients requiring semi-urgent surgery, who test negative for COVID-19 undergo surgery in the non-COVID-19 OR with standard precautions. Patients, who do require emergent surgery, are assumed to be COVID-19 positive until proven otherwise, and managed accordingly in the OR in the COVID-19 area. In accordance with this, a level-III personal protective equipment (PPE) is worn. This is to mitigate the possible risk of operating on asymptomatic COVID-19-positive patients, which is increasing with the increased community prevalence,[8] and in the absence of preoperative COVID-19 testing. Such patients undergo COVID-19 testing in the postoperative period and are shifted to the non-COVID-19 area only after testing negative for COVID-19 [Figure 1].
Figure 1:
Protocol for triaging and coronavirus disease of 2019 (COVID-19) testing for neurotrauma patients at our institute during the COVID-19 pandemic.
The patients who test positive for COVID-19 are isolated for 14 days in the dedicated COVID-19 area (ward or ICU depending on their condition). These patients are tested again for COVID-19 on days 7 and 14. They are shifted to non-COVID-19 area only if they test negative after completing 14 days of isolation. All decisions of shifting such patients are taken in accordance with institute protocols as per suggestions of dedicated team of Community and Family Medicine at our institute.
Objective of the study
As a response to COVID-19 pandemic, hospitals and medical institutions across the world have undergone various changes such as restructuring of dedicated COVID-19 areas, doing widespread COVID-19 testing, rationing of material and human resources, and rescheduling of “non-emergent” surgeries.[1,3,7,13,15,16,20,22,27,28] Even though head injury is an “emergency,” which cannot be “rescheduled” or “postponed,” changes in typical head injury patterns are expected with most people staying inside their homes, especially during the “lockdown,” resulting in less interpersonal contact and decreased traffic on roads. To assess these possible changes, we conducted this study where data regarding all head injury patients admitted to our center during the COVID-19 pandemic was compared to data from the pre-COVID-19 era.
MATERIALS AND METHODS
We conducted a retrospective observational study by collecting details of all patients of head injury who were admitted under the department of neurosurgery at our institute since the onset of COVID-19 pandemic in the country from patient’s records and discharge summaries. The patients were studied according to which phase of pandemic they were admitted in – “lockdown” period (March 25 to May 31, 2020) or “unlock” period (June 1 to September 15, 2020). Data on the number of confirmed COVID-19 cases in the state of Uttarakhand were collected from the official website of Ministry of Health and Family welfare.[24] A comparison was made between the weekly numbers of head injury cases admitted in our department with the number of confirmed COVID-19 cases in the state of Uttarakhand.
Details of head injury patients admitted during the same period last year, that is, March 25, 2019, to September 15, 2019, were also retrieved. The decision to include the patients operated during the same time of the year last year was made to remove any seasonal variation in the patient profile. We compared the demographic profile, mode of injury, GCS at admission, severity of head injury, radiological diagnosis, management (surgical/conservative), and outcome in these two groups. For patients with more than one finding on radiology, the finding considered most important was noted for categorization.
Statistical analysis
Statistical analysis was performed using IBM Statistical Package for the Social Sciences version 25.0, SPSS, Inc., Chicago, IL, USA. Continuous variables were expressed as mean and range while categorical variables were expressed as frequencies. Chi-square test was used to test for the association between groups of categorical variables.
RESULTS
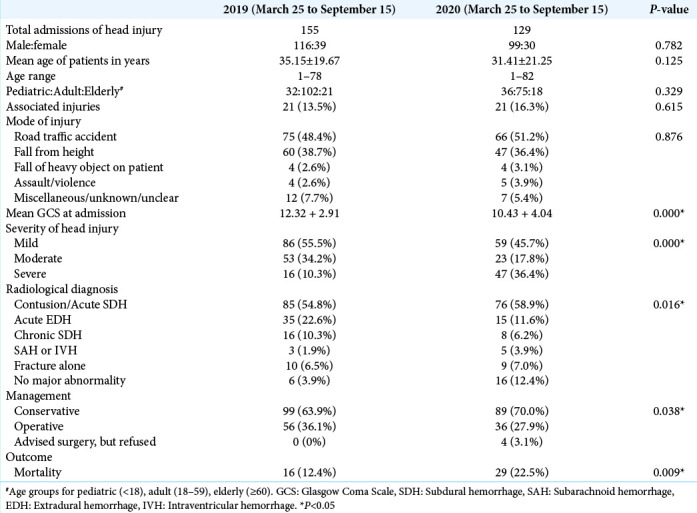
Two hundred and eighty-four patients were included in the study, of which 129 were admitted during the COVID-19 related pandemic (from March 25 to September 15, 2020). These 129 patients (99 males and 30 females) had a mean age of 31.41 years (range 1–82 years). During the same period in 2019, there were 155 head injury admissions (116 males and 39 females) with mean age of 35.15 years (range 1–78 years) [Table 1]. Overall, the number of head injuries decreased by 16.8% during the COVID-19 pandemic compared to preCOVID-19 era.
Table 1:
Comparison of the data of head injury admissions for the period of ongoing COVID-19 pandemic (March 25 to September 15, 2020) with the same duration the past year.
Comparison with COVID-19 cases in the state
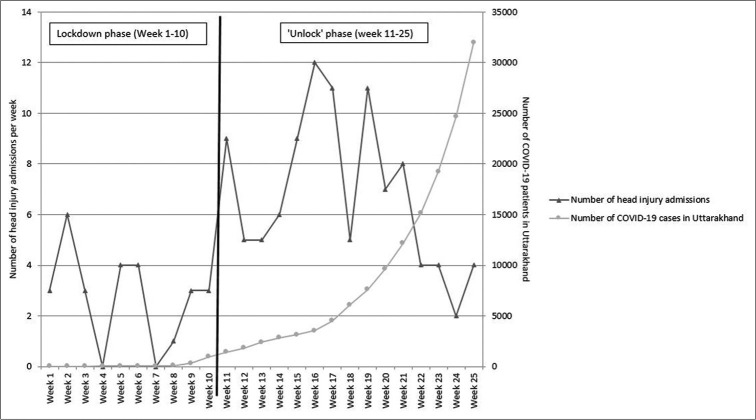
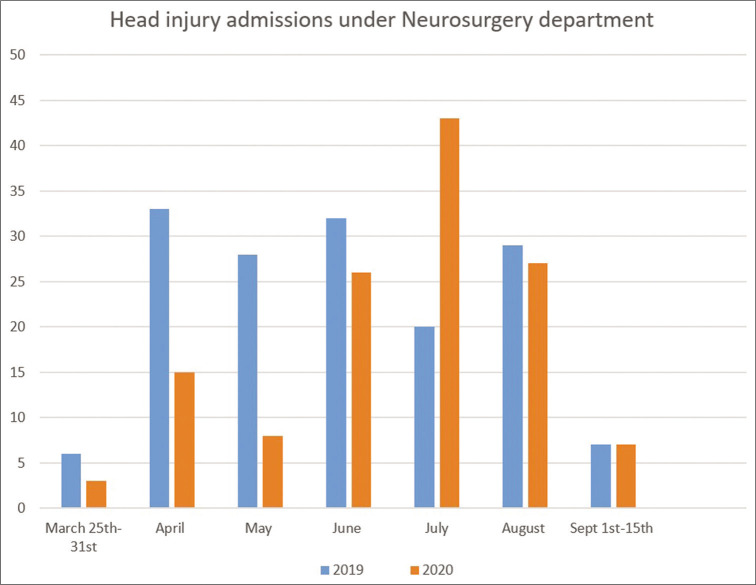
In the state of Uttarakhand, there were 907 COVID-19 patients at the end of “lockdown” on May 31, 2020, while on September 15, 2020, this number had increased to 33,016. On classifying head injury admissions during the pandemic into “lockdown” period and “unlock” period, we observed that 27 patients were admitted during the 10 weeks’ “lockdown” period, while 102 patients were admitted during the 15 weeks of “unlock” period. Thus, the number of admissions per week increased from 2.7 during lockdown period to 6.8 during the ‘unlock’ period [Figure 2]. When this data were compared with data from the same duration last year, it was observed that during the “lockdown” period (March 25 to May 31), there were only 38.8% hospital admissions of head injury patients as compared to the previous year. Whereas in the “unlock” period (June 1 to September 15), this proportion increased to 117.0% compared to the same duration in the previous year. This change was found to be statistically significant (P < 0.0001) [Figure 3]. The number of admissions reached the lowest point during the “lockdown” in May when only eight cases of head injury were admitted, compared to 28 admissions in May, 2019.
Figure 2:
Frequency polygon depicting the number of head injury admissions per week in relation to the rising trend of coronavirus disease of 2019 cases in Uttarakhand during the pandemic. During the lockdown period, there were a total of 27 head injury admissions over 10 weeks, thus accounting for 2.7 admissions per week, while during the 15 weeks of “unlock” period, there were a total of 102 head injury admissions, accounting for 6.8 admissions per week. Thus, head injury admissions per week increased to 2.52 times during the “unlock” period.
Figure 3:
Monthly frequency of neurotraumas admissions during the study period (March 25 to September 15, 2020) compared to the same duration in 2019. During the “lockdown” period (March 25 to May 31), there were only 38.8% hospital admissions of head injury patients as compared to the previous year, whereas in the “unlock”’ period (June 1 to September 15), this proportion increased to 117.0% compared to the same duration in the previous year. This change was found to be statistically significant (P < 0.0001).
Mode of injury
Overall, the most common mode of injury was road traffic accident (141; 49.65%), followed by fall from height (107; 37.67%) [Table 1]. During the “lockdown” period, out of 27 admitted cases, eight (29.6%) had suffered RTA, while 11 (40.7%) had history of fall from height. While out of 102 cases admitted during the “unlock” period, 58 (56.9%) suffered injury due to RTA and 36 (35.3%) due to fall from height. This difference in the mode of injury between the lockdown and unlock periods was statistically significant (P = 0.000).
Radiological diagnosis and management
Overall, the most common radiological abnormality was the presence of contusions/acute subdural hemorrhage (SDH) in 161 patients (56.7%), followed by acute extradural hematoma (EDH) (50; 17.6%) and chronic SDH (24; 8.5%). Notably, acute EDH decreased from 35 patients (22.6%) in the preCOVID-19 era to 15 patients (11.6%) during the COVID-19 pandemic. Chronic SDH, which is different from other head injuries as it is a “semi-urgent” indication, decreased from 16 during the pre-COVID-19 era to 8 during the COVID-19 era. The difference in radiological diagnoses was statistically significant (p=0.016). During the COVID-19 pandemic, 36 patients (27.9%) underwent surgical intervention, compared to 36.1% (56 out of 155 patients) during the preCOVID-19 era and this difference was statistically significant (P = 0.038) [Table 1].
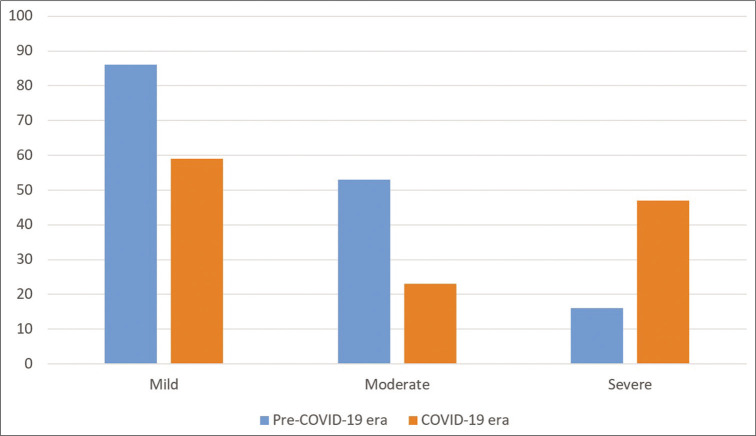
Severity of injury and outcome
The mean GCS of the patients admitted during the ongoing COVID-19 pandemic was significantly worse (10.43 ± 4.04) than during the pre-COVID-19 era (12.32 ± 2.91) (P = 0.000). During the ongoing pandemic, of the 129 admitted patients, 59 were mild, 23 were moderate, and 47 were severe head injuries. During the pre-COVID-19 era, among 155 admissions, 86 were mild, 53 were moderate, and 16 were severe head injuries [Figure 4]. Thus, compared with preCOVID-19 era, mild, and moderate cases decreased by 41% and severe cases increased by 193.75% during the COVID-19 pandemic. This change was found to be statistically significant (P = 0.000) [Table 1]. Associated injuries were present in 16.3% of patients in the COVID-19 era, which was higher than that in the pre-COVID-19 era (13.5%) (P = 0.615). The mortality among neurotrauma patients increased from 12.4% to 22.5% during the COVID-19 era and this result was statistically significant (P = 0.009).
Figure 4:
Vertical bar graph depicting the severity of head injury in admitted patients during the ongoing coronavirus disease of 2019 (COVID-19) pandemic compared to pre-COVID-19 era. Compared with pre-COVID-19 era, mild, and moderate cases decreased by 41% and severe cases increased by 193.75% during the COVID-19 pandemic. This change was found to be statistically significant (P = 0.000).
COVID-19 positive patients
Two patients (1.55%) tested positive for COVID-19 out of the 129 head injury patients admitted during the ongoing COVID-19 pandemic. One was an 80-year-old man with the left-sided chronic subdural hematoma. He tested negative on initial COVID-19 testing on admission and therefore, underwent surgery in the standard (non-COVID-19) OR. In the postoperative period, due to contact with a relative who later tested positive, he was again tested and was found to be positive this time. Therefore, he was isolated for 14 days and discharged only after two negative COVID-19 tests. Second patient was a 15-year-old boy, case of severe traumatic brain injury with right frontal contusion. He tested positive on initial screening COVID-19 testing and was therefore isolated in the COVID-19 ICU for 14 days. He was managed conservatively and discharged only after testing negative for COVID-19.[15]
DISCUSSION
In our previous articles, we have described the change in pattern of neurosurgical patients as a result of postponement/ cancellation of “non-emergent” cases.[9,13-17] Similar patterns have been reported from across the globe.[4,10,11,15,17,19-23] The decline in the volume of cases during the ongoing pandemic is not restricted to “non-emergent” cases alone and even “emergent” cases including neurotrauma have been affected. Zoia et al. reported a decrease in the number of traumatic cases during lockdown in Italy.[29] Christey et al. have also reported reduction in injury-related admissions in New Zealand during the lockdown there.[5] In our previous study on the operative volumes at our department during the COVID-19 pandemic, we observed a decline of almost 43% in the number of surgeries for head injury during the lockdown period.[17] This prompted us to evaluate the patterns of neurotrauma admissions at our center during the COVID-19 pandemic.
Although “emergent,” we observed significant changes in the patterns of head injury in our study. These changes may probably be attributed to the measures advocated by the authorities to prevent the spread of the pandemic. These changes include advising population at large to stay home as much as possible, follow social distancing, working from home to decrease contact between people, avoiding public transport, and defining containment zones. Furthermore, strict quarantine rules after travel also discouraged the general population against travelling. We hypothesized that these unique circumstances would have decreased the frequency of neurotrauma accordingly.
Our data show a decrease in the overall volume of head injury admissions during the ongoing pandemic compared to the same period in the pre-COVID-19 era. When further analyzed, we found that the number of admissions decreased significantly during the “lockdown” phase and has increased during the “unlock” phase compared to the past year. The decrease in number of head injury admissions can be attributed to decreased mobility during the “lockdown” and decreased traffic on the road, which is the most common mode of head injury in this part of the world.[25]
These findings are in accord with the quarterly data provided by states and UTs to the Supreme Court committee on road safety, which showed that there were 123,150 road crashes between April and June 2019, which reduced to 60,118 during the same period in this year. Between April and June this year, 20,732 lives were lost in road traffic accidents compared to 41,032 during the same period last year – a reduction of 49.5%.[26] Further analysis suggested that while the number of road accidents had declined significantly, deaths per 100 crash had increased suggesting that accidents during the lockdown were more severe and fatal.[19]
Similar patterns were observed in our study, which showed that during the “lockdown,” head injury cases due to road traffic accident decreased significantly. Moreover, we observed that during the ongoing COVID-19 pandemic, the number of mild and moderate head injuries have decreased and the number of severe head injury cases have increased significantly. The decrease in mild and moderate head injuries can be attributed to patients avoiding visiting hospitals for what they consider minor injuries. The significant decline in number of chronic SDH during the COVID-19 pandemic indicates that many patients avoided coming to the hospitals for these conditions, as most patients of chronic SDH are elderly and may not present with any acute symptoms. As COVID-19 is known to affect elderly population badly,[12,18] the attendants of these patients of chronic SDH might have preferred to keep them home for the fear of contracting COVID-19. In certain cases, difficulty in transporting head injury victims during lockdown in our hilly state might also have been responsible for under-reporting of mild and moderate head injured patients. These patients might have presented later with more progressed condition, leading to a higher proportion of severe head injuries.
The increased speeds of vehicles due to decreased traffic on the roads may also be responsible for increased severity of head injury as well as higher incidence of poly-trauma during the pandemic. These findings should act as a directive to the government authorities to ensure better compliance of speed limits on the road. This is especially important in hilly areas, like ours, where roads are narrow and curvaceous and over-speeding can be extra-dangerous. Now that the hospitals are somewhat better prepared for COVID-19 as compared to before the lockdown,[14] government should send a clear message to the public not to ignore head injuries, otherwise there is a significant risk of collateral damage to the general population due to trauma in an endeavor to protect them from COVID-19. Overall, the mortality in our head injury patients increased during the COVID-19 pandemic, which may be explained by the higher proportion of severe head injuries and poly-trauma during this time.
In their study of head trauma admissions in New York city, Lara-Reyna et al. have described patterns of head injury patients, which are similar to ours. They reported decreased number of neurotrauma admissions during the early COVID-19 pandemic, which again started increasing as COVID-19 cases decreased in New York City. There were a few key differences. In their experience, overall, the most common mode of head injury was mechanical fall (40.8%) and MVA/transit-related injuries accounted for only 18.4%. This difference may be because of the difference in quality of roads and better implementation of traffic rules in USA compared to India. Road traffic accidents and violence-related trauma showed a statistically significant increase in frequency during COVID-19 in their experience.[21]
In our experience, the majority of the patients were managed conservatively in both time periods, with a statistically significant decrease in number of surgical cases during the COVID-19 period. This was similar to the experience of LaraReyna et al. Since May 2, 2020, we are testing every patient for COVID-19 by reverse transcriptase-polymerase chain reaction (RT-PCR) of oropharyngeal and nasopharyngeal swabs. In our experience, only two patients (1.55%) of head injury admitted during the pandemic tested positive for COVID-19. This is lower compared to the figures reported by Lara-Reyna et al. from New York, who reported positive COVID-19 test in three of their 49 neurotrauma patients (6.1%). This difference can be attributed to the much higher prevalence of COVID-19 in New York which had become the center of the pandemic when their study was conducted.
We have presented our institute protocols and modification in our work-flow for neurotrauma management in the hope that our fellow neurosurgeons/trauma-surgeons from across the world find it useful. Our experience shows that though there has been a decline in the neurotrauma volume during the ongoing pandemic, the severity of head injury and proportion of those with associated injuries have increased, thereby resulting in overall increased mortality at our center. As the number of COVID-19 cases is expected to increase further in the coming days, it will be a challenge to manage neurotrauma patients as resources and man-power will be stretched.
Limitations
One of the biggest limitations of our study is the single center nature of the data, which may limit the generalizability of the results. The type of trauma may vary between institutions, with hospitals in the developed world reporting fall as the most common mode of injury. Similarly, assault may be more common in another area where violence is more prevalent. We only explored the results of neurotrauma and not the total number of traumas, which might better reflect the impact of decreased movement and traffic during the present situation. The true incidence of mild cases of neurotraumas may be underestimated because patients may have preferred to stay at home and avoid hospitals due to the fear of getting the infection. Furthermore, difficulty in reaching hospital and the triage system might have acted as a deterrent for patients of mild head injury. Even though patients of head injury may have multiple radiological findings, for keeping the data simple and legible, we have documented the predominant finding.
CONCLUSION
A temporary decrease was observed in the number of head injury admissions during the lockdown phase of the pandemic, especially due to decline in the road traffic accidents and implementation of social distancing policies in the country. At the same time, there has been an increase in the severity of head injuries and higher incidence of associated injuries, resulting in significantly higher mortality in our patients during the ongoing COVID-19 pandemic.
Footnotes
How to cite this article: Goyal N, Swain SK, Gupta K, Chaturvedi J, Arora RK, Sharma SK. “Locked up inside home”- Head injury patterns during coronavirus disease of 2019 pandemic. Surg Neurol Int 2020;11:395.
Contributor Information
Nishant Goyal, Email: drnishantgoyal@gmail.com.
Srikant Kumar Swain, Email: srikantswainvss@gmail.com.
Kanav Gupta, Email: vanak1190@gmail.com.
Jitender Chaturvedi, Email: drjittu28@gmail.com.
Rajnish Kumar Arora, Email: rajnish_19@yahoo.com.
Suresh K. Sharma, Email: suresh.nur@aiimsrishikesh.edu.in.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ahuja S, Shah P, Mohammed R. Impact of COVID-19 pandemic on acute spine surgery referrals to UK tertiary spinal unit: Any lessons to be learnt? Br J Neurosurg. 2020;1:1–5. doi: 10.1080/02688697.2020.1777263. [DOI] [PubMed] [Google Scholar]
- 2.AIIMS Rishikesh Becomes First Government Hospital in India to Have Helipad Facility Dehradun News-Times of India. 2020. Available from: https://www.timesofindia.indiatimes.com/city/dehradun/aiims-rishikesh-becomes-first-govt-hospital-in-india-to-have-helipad-facility/articleshow/77491255.cms [Last accessed on 2020 Sep 25]
- 3.Antony J, James WT, Neriamparambil AJ, Barot DD, Withers T. An Australian response to the COVID-19 pandemic and its implications on the practice of neurosurgery. World Neurosurg. 2020;139:e864–71. doi: 10.1016/j.wneu.2020.05.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bajunaid K, Alqurashi A, Alatar A, Alkutbi M, Alzahrani AH, Sabbagh AJ, et al. Neurosurgical procedures and safety during the COVID-19 pandemic: A case-control multicenter study. World Neurosurg. 2020;143:e179–187. doi: 10.1016/j.wneu.2020.07.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133:81–8. [PubMed] [Google Scholar]
- 6.Countries Where Coronavirus has Spread-Worldometer. 2020. Available from: https://www.worldometers.info/coronavirus/countries-where-coronavirus-has-spread [Last accessed on 2020 Aug 08]
- 7.Dash C, Venkataram T, Goyal N, Chaturvedi J, Raheja A, Singla R, et al. Neurosurgery training in India during COVID-19 pandemic: Straight from the horse’s mouth. Neurosurg Focus. 2020 doi: 10.3171/2020.9.FOCUS20537. [DOI] [PubMed] [Google Scholar]
- 8.Delhi Corona News: Delhi’s Sero-Prevalence Study Finds 23.48 Per Cent people Affected by COVID-19, Delhi News-Times of India. 2020. Available from: https://www.timesofindia.indiatimes.com/city/delhi/delhis-sero-prevalence-study-finds-23-48-per-cent-people-affected-by-covid-19/articleshow/77085162.cms [Last accessed on 2020 Aug 10]
- 9.Deployment of Neurosurgeons at the Warfront against COVID-19-Science Direct. 2020. Available from: https://www.sciencedirect.com/science/article/pii/S1878875020320179#aep-article-footnote-id14 [Last accessed on 2020 Sep 10] [DOI] [PMC free article] [PubMed]
- 10.Gandía-González ML, Sáez-Alegre M, Roda JM. Neurosurgeons on the frontline of COVID-19: No place for surgery? Acta Neurochir (Wien) 2020;162:1503–4. doi: 10.1007/s00701-020-04390-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gilligan J, Gologorsky Y. Collateral damage during the coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020;140:413–4. doi: 10.1016/j.wneu.2020.05.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goyal A, Saigal S, Niwariya Y, Sharma J, Singh P. Successful use of tPA for thrombolysis in COVID related ARDS: A case series. J Thromb Thrombolysis. 2020:1–4. doi: 10.1007/s11239-020-02208-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goyal N, Chaturvedi J, Arora RK. Letter to the editor regarding-neurosurgical referral patterns during the COVID-19 pandemic: A United Kingdom experience. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.09.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goyal N, Gupta K, Chaturvedi J, Swain SK, Singh V, Akhil T. Getting neurosurgery services back on its feet: Learning to live with COVID-19. World Neurosurg. 2020 doi: 10.4103/ajns.AJNS_497_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goyal N, Gupta K. Letter to the editor regarding-COVID-19 impact on neurosurgical practice: Lockdown attitude and experience of a European academic center. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.09.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goyal N, Venkataram T, Dash C, Chandra P. Letter to the editor regarding-Impact of COVID-19 on an academic neurosurgery department: The Johns Hopkins experience. World Neurosurg. 2020;143:599–600. doi: 10.1016/j.wneu.2020.07.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goyal N, Venkataram T, Singh V, Chaturvedi J. Collateral damage caused by COVID-19: Change in volume and spectrum of neurosurgery patients. J Clinical Neurosci. 2020;80:156–61. doi: 10.1016/j.jocn.2020.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan W, Liang W, Zhao Y, Liang H, Chen Z, Li Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.How Lockdown Saved 9, 000 lives-Road accidents, Public Releases Percentage. 2020. Available from: https://www.publicreleases.com/2020/06/26/how-lockdown-saved-9000-lives-road-accidents [Last accessed on 2020 Sep 26]
- 20.Khalafallah AM, Jimenez AE, Lee RP, Weingart JD, Theodore N, Cohen AR, et al. Impact of COVID-19 on an academic neurosurgery department: The Johns Hopkins experience. World Neurosurg. 2020;139:e877–84. doi: 10.1016/j.wneu.2020.05.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lara-Reyna J, Yaeger KA, Rossitto CP, Camara D, Wedderburn R, Ghatan S, et al. Staying home-early changes in patterns of neurotrauma in New York city during the COVID-19 pandemic. World Neurosurg. 2020;143:e344–350. doi: 10.1016/j.wneu.2020.07.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lubansu A, Assamadi M, Barrit S, Dembour V, Yao G, Hadwe SE, et al. COVID-19 impact on neurosurgical practice: Lockdown attitude and experience of a European academic center. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.08.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mathiesen T, Arraez M, Asser T, Balak N, Barazi S, Bernucci C, et al. A snapshot of European neurosurgery December 2019 vs. March 2020 Just before and during the COVID-19 pandemic. Acta Neurochir (Wien) 2020;162:2221–33. doi: 10.1007/s00701-020-04482-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.MoHFW. 2020. Available from: https://www.mohfw.gov.in [Last accessed on 2020 Jul 27]
- 25.Road Accidents Claimed Over 1.5 Lakh Lives in 2018 Over-Speeding Major Killer-The Economic Times. 2020. Available from: https://www.m.economictimes.com/news/politics-andnation/road-accidents-claimed-over-1-5-lakh-lives-in-2018-over-speeding-major-killer/amp_articleshow/72127418.cms?__twitter_impression=true [Last accessed on 2020 Sep 27]
- 26.Road Accidents in India: Coronavirus May Have Saved 20, 000 Lives on Indian Roads-Times of India. 2020. Available from: https://www.timesofindia.indiatimes.com/india/covid-may-have-saved-20000-lives-on-indian-roads/articleshow/77649949.cms [Last accessed on 2020 Sep 25]
- 27.Venkataram T, Goyal N, Dash C, Chandra PP, Chaturvedi J, Raheja A, et al. Impact of the COVID-19 pandemic on neurosurgical practice in India: Results of an anonymized national survey. Neurol India. 2020;68:595–602. doi: 10.4103/0028-3886.289004. [DOI] [PubMed] [Google Scholar]
- 28.Wittayanakorn N, Nga VD, Sobana M, Bahuri NF, Baticulon RE. Impact of COVID-19 on neurosurgical training in Southeast Asia. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.08.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zoia C, Bongetta D, Veiceschi P, Cenzato M, di Meco F, Locatelli D, et al. Neurosurgery during the COVID-19 pandemic: Update from Lombardy, Northern Italy. Acta Neurochir (Wien) 2020;162:1221–2. doi: 10.1007/s00701-020-04305-w. [DOI] [PMC free article] [PubMed] [Google Scholar]