Abstract
Although it was long believed that the complement system helps the body to identify and remove transformed cells, it is now clear that complement activation contributes to carcinogenesis and can also help tumors to escape immune-elimination. Complement is activated by several different mechanisms in various types of cancer, and complement activation fragments have multiple different downstream effects on cancer cells and throughout the tumor microenvironment. Thus, the role of complement activation in tumor biology may vary among different types of cancer and over time within a single tumor. In multiple different pre-clinical models, however, complement activation has been shown to recruit immunosuppressive myeloid cells into the tumor microenvironment. These cells, in turn, suppress anti-tumor T cell immunity, enabling the tumor to grow. Based on extensive pre-clinical work, therapeutic complement inhibitors hold great promise as a new class of immunotherapy. A greater understanding of the role of complement in tumor biology will improve our ability to identify those patients most likely to benefit from this treatment and to rationally combine complement inhibitors with other cancer therapies.
Keywords: complement, cancer, immunity, myeloid cells, therapeutics
1. Introduction
It was long assumed that the complement cascade contributes to the immunosurveillance of cancers, helping the body to recognize and eliminate transformed cells. In 2008, however, Markiewski and colleagues reported that mice with targeted deletion of the genes for C3 or C4 are protected from cancer in an implantation model [1]. This landmark study revealed that complement activation can promote tumor growth in some settings. Since then, studies from many different research groups have confirmed and expanded on these findings. It is now clear that the complement cascade is activated in many tumors, and that this component of the innate immune system plays a complex role in carcinogenesis and anti-tumor immunity. The mechanisms of complement activation seem to vary among different types of cancer, and the cancer cells themselves often play an active role in modulating complement activation within the tumor microenvironment (TME). For example, various types of cancer express proteins that both activate and inhibit the complement cascade within the TME.
2. How Does Carcinogenesis Occur?
Cancer is a disease of dysregulated growth. While our knowledge of cancer dates back centuries, it has been more challenging to actually define the critical properties of cancer. Starting in the 1980s, studies identified several somatic mutations as critical to the disease. These included activating mutations in drivers of proliferation, designated as oncogenes, and loss of function mutations in tumor suppressor genes. These mutations result in the development of the “transformed” phenotype. Transformed cells acquire new features such as the loss of contact inhibition and the ability to grow in suspension. The biological consequences of these mutations were formally characterized as the “Hallmarks of Cancer” in a seminal review by Hanahan and Weinberg in 2000 [2]. However, solid tumors originate in specific organs and are surrounded by a variety of non-transformed cells. The surrounding cell populations and stroma have been designated as the TME. The TME includes vascular cells, inflammatory and immune cells, fibroblasts, and extracellular matrix. While the initial focus on the transformed epithelial cell did not consider the TME as a driver of cancer progression, it has become apparent that the interactions between cancer cells and the TME are critical. Studies performed in the first decade of this century identified important features of the TME that regulate anti-tumor immunity and cancer metabolism and define additional “Hallmarks” of cancer [3].
A current view of cancer development needs to take into account the complexity of the interactions between cancer cells and the TME, as well as how these interactions change in a spatiotemporal fashion. Thus, epithelial cells undergo initial somatic mutations resulting in activation of oncogenic signaling or loss of tumor suppressor function. This results in increased “fitness” of these cells, giving them a survival advantage. Additional mutations occur which lead to improved cell-autonomous fitness and/or altered interactions with the surrounding TME. Thus, targeting these interactions therapeutically has become a major focus of research.
Additional complexity in this setting is the degree of heterogeneity observed in human tumors. This is reflected by differences in mutational status and metabolic qualities of cancer cells within the same tumor. This variability makes the development of novel therapeutic approaches particularly challenging. Developing rational combinations of therapeutic agents to target this heterogeneity is often limited by the fact that most preclinical models of cancer fail to recapitulate these critical features of human disease.
3. Cancer, Inflammation, and Immunity
The immune system has a complex relationship with carcinogenesis. Chronic inflammation is strongly linked with the risk for many cancers, and it is generally associated with the promotion of tumor progression and metastasis. Cancer-causing inflammation can be produced by infections [4,5], environmental irritants [6,7], and autoimmune diseases [8]. For example, chronic viral infections, such as the human papillomavirus, are associated with the development of head and neck cancers. Chronic pancreatitis, hepatitis, and inflammatory bowel disease are strongly predictive of pancreatic, hepatocellular, and colon cancer, respectively. Perhaps most notably, cigarette smoking leads to the development of chronic lung inflammation and chronic obstructive pulmonary disease (COPD), and it is a major contributor to lung cancer. The immune response in these diverse settings probably contributes to genomic instability, cellular proliferation, and remodeling in the target tissues. Tissue-specific mechanisms are also undoubtedly important, however, as some organs are particularly susceptible to inflammation-associated cancers. Inflammatory changes also occur within the TME of cancers after they have formed, even in tumors for which inflammation is not an initial predisposing factor. As a result, essentially all tumors engage with the immune system as they develop and grow.
Inflammatory responses within tumors induce the recruitment of myeloid cells, including neutrophils and macrophages. Myeloid cells are initially recruited to the site of tumors as a result of specific molecules produced by the cancer cells, including cytokines, growth factors, and other molecules that attract myeloid cells and modulate their phenotype [9,10]. Macrophages are the most abundant leukocyte subtype in the TME, and they continually infiltrate the tumor [11]. This process appears to depend on the trafficking of monocytes from the bone marrow in response to specific chemokines produced by the cancer cells, such as (C-C motif) ligand 2 (CCL2). These innate immune cells are critical to the general response to injury and acute infection and act to eliminate infections and promote healing. Similar to what is seen during infection, the initial phenotype of myeloid cells in the TME is generally proinflammatory, designated as M1 macrophages and N1 neutrophils. The phenotypes of these cells become altered in the setting of chronic inflammation, however. Similarly, cross-talk between cancer cells and myeloid cells eventually results in modulation to alternatively activated phenotypes, designated as M2 or N2 [12]. These cells then actually promote tumor progression through the production of growth factors and proangiogenic cytokines which, in turn, signal back to the cancer cells. While this model is definitely an oversimplification, it serves as a framework for understanding the interactions between the cancer cells and these innate immune cell populations.
Cancer cells express mutated or aberrantly expressed proteins on their cell surface. These so-called neoantigens can be recognized by the adaptive immune system (CD8 and CD4 T cells) potentially leading to immune elimination. However, cancer cells can evade immune attack through multiple mechanisms. A model for this, designated as immunoediting, was proposed several years ago by Schreiber and colleagues [13]. This model comprises three stages of interaction with the immune system. Initially, tumor cells can be eliminated by the immune system; however, responses of the tumor lead to an equilibrium where the tumors are not eliminated but held in check by the immune system. Eventually, through the activation of additional cancer cell-autonomous and non-autonomous mechanisms, the cancers evade immune attack and escape.
Numerous mechanisms control these events. Cancer cells can develop additional mutations that target antigen-presentation pathways, thus becoming invisible to the immune system. Alternatively, myeloid cells within the TME can undergo phenotypic modulation, acquiring anti-inflammatory properties [14]. The cells can then inhibit CD4 T cells and block CD8 T cell-mediated killing. Finally, a variety of pathways that regulate the immune system under non-cancerous conditions can be co-opted by cancer cells to block T cell function. Prominent among these are immune checkpoints expressed on the surface of cancer cells and other cell types which block T cell activation and lead to an “exhausted” T cell phenotype [15]. Targeting these pathways through the use of checkpoint inhibitors can result in T cell reactivation and tumor regression. These agents have been approved in a variety of cancers and have revolutionized the treatment of many types of cancer [16,17]. For several reasons that are only partially understood, however, the majority of patients either do not respond to these agents or develop resistance.
A major challenge, therefore, is the development of rational combinations of therapies that will increase the number of responders as well as the duration of the response to treatment. In particular, targeting inflammation and the cross-talk between innate and adaptive immunity could enhance the ability of the immune system to eliminate tumors.
4. The Role of the Complement System in Carcinogenesis
The complement system is a cascade of proteins that form part of the innate immune system. Complement factors circulate as inactive precursor proteins (zymogens) that are cleaved and activated by three different pathways: the classical, lectin, and alternative [18]. Activation of these pathways generates soluble fragments (C3a and C5a, or the “anaphylatoxins”) and also covalently fixes protein fragments (C3 and C4 fragments) on the surface of target cells. Immune cells express specific receptors for the anaphylatoxins and C3 fragments and this interaction links complement activation fragments with modulation of immune cell function. Consequently, complement activation has strong effects on innate and adaptive immunity. Full complement activation also generates multimeric complexes that form pores in target cells. In the literature, this is variably referred to as the membrane attack complex (MAC), the terminal complement complex, or C5b-9.
Complement activation is traditionally regarded as proceeding through three different pathways: the classical, lectin, and alternative pathways. The classical and lectin pathways are activated by specific proteins that activate these cascades after binding to target ligands. IgG and IgM bound to target antigens activate the classical pathway, and mannose-binding lectin bound to target sugars activates the lectin pathway [19]. The alternative pathway is spontaneously activated in plasma through a process called “tickover”. It is also secondarily activated by the classical and lectin pathways, thereby amplifying their effects.
4.1. Complement Activation as a Cause of Cancer
Carcinogenesis involves several steps, including the acquisition of a series of mutations that give a cell growth or survival advantages (“initiation”) and proliferation and/or decreased death of the transformed cells (“promotion”) [20]. The immune system is integrally involved with both of these stages of carcinogenesis. In most inflammatory settings, complement activation occurs as part of a broader immune response, so it is difficult to distinguish the effects of complement activation from those of other components of the immune system. Nevertheless, we recently published a study showing that chronic complement activation in the liver causes cancer [21]. Mice with targeted deletion of the gene for factor H, a key complement regulatory protein, have spontaneous complement activation within the liver [21]. As the mice aged, they developed hepatocellular carcinoma at a greater rate than control mice, whereas complement deficient mice did not. Although the experiments did not determine which stage(s) of tumorigenesis complement directly affects, it did demonstrate that, at least in the liver, chronic complement activation is sufficient to cause tumor formation.
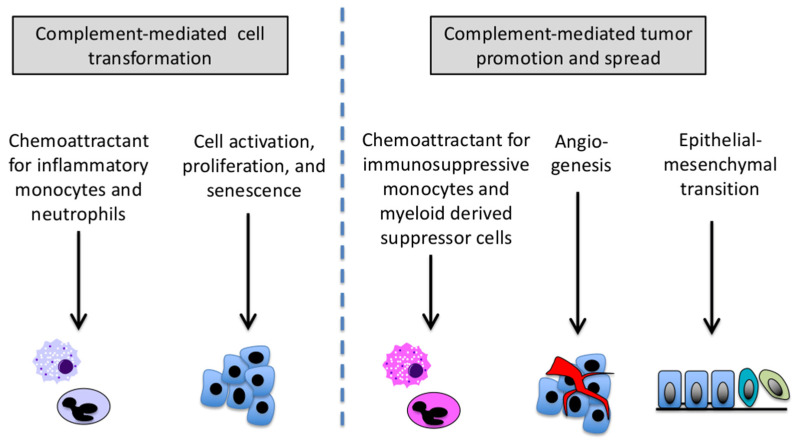
There is a rationale for suspecting that the complement system plays a part in tumor initiation (Figure 1). Activated macrophages [22] and neutrophils [23] produce reactive oxygen species and reactive nitrogen intermediates, molecules that can cause DNA mutations [24]. C3a and C5a are strongly chemotactic for these cells and induce the cells to undergo oxidative burst. Thus, complement activation within inflamed tissues is probably integrally involved in these initiation events [25]. In support of this, Bonavita and colleagues studied the role of pentraxin-3 (PTX3) in models of chemically induced sarcomas and skin carcinomas [26]. PTX3 is expressed by many types of cancers, and it can bind to circulating factor H, tethering this inhibitor to cells and suppressing complement activation within the TME. The authors found that PTX3-deficient mice were susceptible to chemically induced sarcomas and skin carcinomas, presumably because inadequate control of complement activation increases carcinogenesis in affected tissues. Furthermore, complement deficiency reversed this tumorigenic effect. The authors also noted that PTX3-deficient mice developed a greater degree of DNA damage and a higher number of P53 mutations at early timepoints compared to wild-type mice, further supporting the conclusion that complement-mediated inflammation contributes to genomic instability and cancer initiation.
Figure 1.
Possible roles for complement in tumor initiation and promotion. Complement activation is a frequent component of the acute inflammatory response. Complement fragments are chemotactic for myeloid cells, and also elicit the production of chemokines by epithelial cells. This contributes to inflammatory injury. Complement also directly stimulates cell activation and proliferation in target tissues. Once cancers have developed, complement fragments protect the tumor from immune-elimination by attracting immune-suppressive myeloid cells into the tumor microenvironment. Complement fragments may be involved with angiogenesis, which supports the expanding tumor mass. It may also trigger epithelial-mesenchymal transition, which contributes to tissue remodeling and tumor spread.
Once cells have acquired cancer-causing mutations, the promotion of the nascent tumor requires the proliferation and survival of the transformed cells [27,28]. This involves pro-mitotic signals as well as angiogenic signals to support the expanding tumor, processes that have been linked to inflammatory cytokines. The complement system may indirectly contribute to this process by inducing the production of cytokines and chemokines [29]. Furthermore, in vitro experiments have also shown that C3a and/or C5a directly stimulate cancer cell proliferation [30,31,32]. Consistent with these mitogenic effects on cancer cells, studies in non-cancer models have also shown that C3a and C5a induce survival and proliferation of cells during tissue regeneration [33,34,35]. In addition to C3a and C5a, the insertion of MAC in tumor cell membranes can stimulate cell proliferation [36] and induce chemokine and metalloprotease production by the cells [37]. These findings support a role for complement activation in tumor promotion.
Regions of hypoxia develop in solid tumors as they expand, and angiogenesis becomes essential for all tumor growth. Complement is frequently activated within ischemic tissues, and hypoxia induces some cell types, including non-small cell lung cancer cells, to decrease expression of complement regulatory proteins in vitro [38]. Thus, complement may be preferentially activated in hypoxic regions of a tumor. Complement activation has been linked with angiogenesis [39], raising the possibility that the complement activation provides a link between tissue hypoxia and the production of angiogenic signals. A comprehensive analysis of the mutational landscape in tumors revealed that there is cross-talk between the complement system and hypoxic signals in some cancers [40]. Nevertheless, in one study of non-small cell lung cancer, the C5a blockade did not have a detectable effect on vascular density within tumors [41].
4.2. Complement as a Mechanism of Immune Evasion
The study by Markiewski and colleagues used an implantation model of cancer [1]. Because the mice were injected with cells that were already transformed, the study implicated complement in the growth of existing tumors rather than in cancer initiation per se. In that study, the investigators showed that the generation of C5a attracted myeloid-derived suppressor cells (MDSCs) to the tumor, which reduced the anti-tumor response of CD8 T cells. Complement activation in that model, therefore, is analogous to an immune checkpoint insofar as it suppresses the immune-elimination of cancers (Figure 1). Over the subsequent 12 years, additional pre-clinical studies have reported a similar role for complement activation in promoting the growth of other types of cancer, including lung [42], squamous cell [43], melanoma [44], colon [45], and ovarian cancer [30]. Many other effects of complement on cancer cells and the TME have been identified, but the pattern of inducing myeloid cells to suppress the adaptive immune system has been generalizable across tumor types.
Studies in multiple different types of cancer have also confirmed that the pro-tumorigenic effects of complement are mediated by immunosuppressive myeloid cells, such as MDSCs [1,41,46]. The anaphylatoxins generally have pro-inflammatory effects, but studies in solid organ transplant models have shown that C5a can also attract immunosuppressive myeloid cells into tissues [47]. It is not clear whether it is the context or the duration of complement signaling that determines whether the net effect is pro or anti-inflammatory. Interestingly, studies have revealed that both C3a and C5a contribute to the immunosuppressive effect of complement within tumors [42,44]. Furthermore, C3 produced by stellate cells in the liver affects dendritic cell maturation and attracts MDSCs, facilitating the growth of hepatocellular carcinoma [48]. Another study of stellate cells indicated that this immunomodulatory effect is caused by the iC3b fragment [49]. Thus, multiple different complement activation fragments seem to interact with myeloid cells in the TME, helping the tumor to evade immune-elimination.
Complement activation may also play a role in protective anti-tumor immune responses. For example, it has been shown to be involved in the formation of tertiary lymphoid structures (TLS), which are structures consisting of B and T cells as well as dendritic cells. Interactions between these cells result in strong immune activation, and the presence of these structures is associated with a good response to immunotherapy in multiple cancers [50]. Complement activation in the setting of chemotherapy has been shown to promote a subset of B cells that regulate the formation of these structures [51].
Distinct from systemic production of complement, recent studies have identified key functional roles for intracellular production of complement, specifically in human CD4+ T cells [52,53]. Activation of T cells is associated with translocation of intracellular C3a and C3b to the cell surface, where these fragments regulate T cell activation and metabolism through the engagement of the C3a receptor (C3aR) and the regulatory protein CD46, respectively. These data would indicate that in the setting of cancer progression complement activation in cancer cells and T cells play opposing roles, with cancer cell complement mediating immunosuppression and T cell complement mediating T cell activation. Further research is required to dissect out the relevant importance of these pathways in specific malignancies. One complication in studying the T cell intracellular complement pathway is the fact that CD46 is not expressed in mice, making it difficult to assess this pathway in preclinical models.
4.3. Complement Activation and Metastatic Spread of Cancer
Beyond its effects on carcinogenesis and tumor growth, there is also experimental evidence that the complement cascade increases the invasiveness and metastatic potential of cancer [recently reviewed in [41]]. Complement activation has been linked to the metastatic potential of colon cancer [54] as well as leptomeningeal metastases of cancer cells [55]. The effect of complement fragments on metastases may be due to their direct effects on cancer cells as well as their effect on tissue remodeling in the TME and metastatic niche. C5a, for example, directly induces epithelial-mesenchymal transformation (EMT) of hepatocellular carcinoma [56] and gastric cancer cells [57], and can induce expression of metalloproteinases [58]. Conversely, the C5a receptor blockade reduces some hallmarks of EMT [59]. Work in animal models has also shown that the C5a blockade reduces metastasis of colon and lung cancers by regulating immune responses and the premetastatic niche [46,54].
5. Cancer as a Cause of Complement Activation
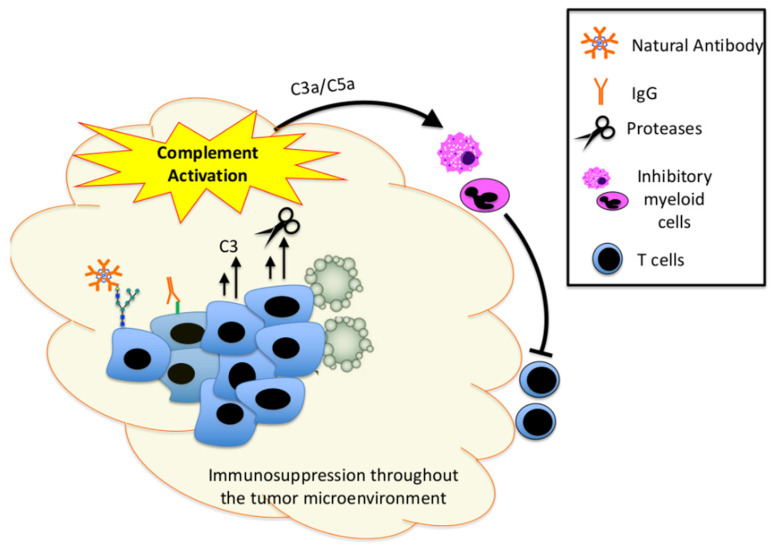
Complement activation contributes to the development of cancer by the mechanisms discussed above, but the reverse is true too: tumors actively promote complement activation within the TME (Figure 1). Inflammatory cells and molecules are present within the TME of essentially all cancers, regardless of their tissue of origin [60]. The adaptive immune response to cancer cells is a function of tumor immunogenicity, which is determined by both the antigenic burden in the cancer and the host immune system [61]. Inflammation can cause DNA damage, but DNA damage can cause the production of mutant proteins that are antigenic and elicit an immune response [62]. Cancer cells that cannot evade the immune system will be eliminated, so the cancer must either stop producing the target antigen, downregulate MHC, or suppress the immune response to the tumor antigen through immunoediting [63,64]. Although the anti-tumor immunity is primarily executed by CD4 T cells, CD8 T cells, and natural killer (NK) T cells, B cells are also seen within the TME of some tumors, and patients often develop IgG that is specifically reactive with tumor antigens [65,66]. This can serve as a link between the adaptive immune response to a tumor with complement activation within the TME.
There is evidence of classical pathway activation in several animal models of cancer. The growth of TC-1 tumors was significantly reduced in mice with targeted deletion of C4 (classical and lectin pathway deficient), but tumor growth was not affected by the deletion of factor B (alternative pathway deficient) [1]. Similarly, studies in non-small cell lung cancer showed that IgM and C4 are deposited in both a mouse model and in human samples, pointing to the involvement of the classical pathway in this type of cancer [42]. Furthermore, tumor growth was not affected by factor B deficiency in this model. A study using the TC-1 cell line also found that C1q was required for tumor growth, further supporting the involvement of the classical pathway [67]. C1q deposits are seen in human lung, colon, breast, and pancreatic adenocarcinoma, as well as melanoma [68]. Because patients so frequently develop antibodies against tumor antigens, it is logical that classical pathway activation would be a frequent occurrence. In a mouse model of melanoma, however, investigators have also shown that C1q contributes to tumor growth in a complement-independent fashion [68]. Studies in models of systemic lupus erythematosus, an autoimmune disease, revealed that C1q directly affects the CD8 T cell response to antigens independent of the classical pathway [69]. In that study, C1q-deficient CD8 T cells displayed greater reactivity against autoantigens and viruses. Such an effect could also potentially modulate anti-tumor immunity.
In addition to the adaptive B cell response to foreign antigens, natural antibodies are produced by B-1 cells in the absence of an antigenic stimulus and often react with carbohydrate epitopes [70]. Tumor cells frequently display abnormal post-translational modifications, including altered glycosylation patterns. Natural antibodies can bind to carbohydrate epitopes, and they have been found to react to glycans displayed on the surface of cancer cells [71]. Interestingly, a hybridoma generated from a patient with signet-ring cell carcinoma of the stomach reacts specifically with an N-linked carbohydrate on CD55 [72]. CD55 is a cell surface complement regulatory protein that protects cancer cells from complement-mediated lysis and contributes to chemoresistance of the cells [51]. Antibodies that bind to neo-epitopes displayed on the surface of CD55 could activate the classical pathway on the target cell while simultaneously impairing complement regulation by CD55 on the cell surface.
Although the requirement of C4 expression for tumor growth could also reflect a role for the lectin pathway in the TC-1 model, there is less published evidence for specific involvement of this pathway in cancer models. However, one recent study found that certain species of gut fungi can migrate to the pancreas and foster the development of pancreatic ductal adenocarcinoma [73]. MBL was required for tumor growth in this model, indicating that the lectin pathway activation was probably involved. This study also showed that signaling through the C3a receptor was necessary for tumor growth.
Although several studies have found that an intact alternative pathway is not necessary for tumor growth [1,42], it is notable that alternative pathway proteins are expressed by most tumors [74]. The alternative pathway also amplifies complement activation that is initiated through the other pathways, so this pathway may contribute to tumor growth by increasing the overall magnitude and duration of complement activation, even if it is not essential for the reaction. Our recent study using factor H deficient mice showed that chronic alternative pathway activation in the liver is sufficient to cause HCC [21]. However, it is possible that the liver—as the source of the alternative proteins factor B and C3—may be uniquely susceptible to alternative pathway-mediated injury.
It is striking that cancer cells and other cells within the TME synthesize complement proteins [74]. Several inflammatory cytokines induce parenchymal cells to produce complement proteins, and the transcription factor twists basic helix-loop-helix transcription factor 1 (TWIST1) has been identified as a key regulator of the expression of C3 by cancer cells [75]. Although high levels of complement proteins are already present in plasma, studies in organ transplantation revealed the importance of locally produced proteins in activation within tissues [76]. Similarly, studies in cancer models have revealed that complement proteins produced by the cancer cells, themselves, contribute to tumor growth in vivo despite the expression of the same proteins by the host [30].
Various proteases are also able to directly activate complement proteins, potentially bypassing the conventional initiation mechanisms and convertases. The cathepsins, for example, are a family of serine proteases that are upregulated and secreted by many different types of cancer [77], and cathepsin L can cleave C3 into C3a and C3b [52]. Human melanoma cells express cathepsin L and cleavage of C3 by the protease is associated with growth and metastasis [78]. Similarly, thrombin is capable of directly cleaving complement C5 [79]. Cancer cells can, directly and indirectly, activate thrombin [80], providing a mechanism for the direct generation of the terminal complement components. Additional cancer-associated proteases capable of activating complement proteins have also been identified, including prostate-specific antigen [81].
6. Complement Regulatory Proteins
In addition to the many molecules that activate the complement pathways, the body also expresses a family of proteins that inhibit activation of the cascade [82]. Some soluble regulators circulate in plasma and other body fluids, as well as regulators expressed on the outer membrane of all cells. The various regulatory proteins inhibit complement activation by distinct mechanisms and at different sites within the cascade.
All cancer cells express cell surface complement regulators, and most cancer cells express more than one of the proteins. The cell surface regulators CD46, CD55, and CD59, for example, are all expressed by squamous cell cancers [83] and uveal melanomas [84]. Multiple studies have also shown that cancer cells overexpress complement regulators compared to the corresponding tissue of origin [85,86,87]. For years, the presumption was that overexpression of the complement regulatory proteins is a mechanism by which cancer cells evade complement-mediated elimination. In support of this, functional studies in which expression of the proteins is knocked down with small interfering RNA (siRNA) have confirmed that the regulatory proteins protect the cells from lysis [88]. Expression levels of the regulatory proteins have also been shown to correlate with complement activation with the tumor and with patient outcomes [89,90]. Interestingly, cancer cells frequently overexpress factor H, and factor H-like protein 1 (FHL-1), soluble proteins that are already present at high concentrations in plasma [91]. Studies have shown that factor H is expressed by ovarian, squamous, and colon cancer cells [92,93]. Knockdown of factor H production can reduce tumor cell survival, proliferation, and migration in vivo [94,95]. Although liver-derived factor H and FHL-1 is almost certainly present in the TME, production of these proteins by cancer cell may ensure that local concentrations are sufficient to protect the cells. Cancer cells can also express non-complement proteins, such as osteopontin, that bind to factor H, holding it within the TME [96].
Several studies have linked the expression of complement regulatory proteins by tumors with adverse clinical outcomes [97,98]. In patients with breast cancer, for example, the expression of CD59 was associated with lung metastasis and shorter [98]. Similarly, in cholangiocarcinoma higher expression of CD55 is associated with shorter survival [97]. Unsurprisingly, being able to control complement activation gives a cancer cell a survival advantage, but this does lead to a paradox. On the one hand, complement activation supports tumor growth in many contexts, yet cancer cells also actively express proteins that inhibit the complement system. It is noteworthy, however, that the expression of complement regulatory proteins by cancer cells is quite heterogeneous, and cells within the same tumor can express different repertoires of regulatory proteins [99]. Expression of these proteins is also dynamic, changing in response to local conditions such as hypoxia and inflammatory cytokines [100,101]. One model to account for these data would suggest that regulatory proteins protect cancer cells from the deleterious effects of complement, such as lysis through the MAC complex while allowing the pro-tumorigenic effects mediated by C3a/C5a to act on the TME leading to immunosuppression. Thus, complement activation may have opposing effects on tumor growth, and the effects may fluctuate depending on time and location within the tumor. Furthermore, while complement activation may destroy a limited number of cells within the tumor mass, the immunosuppressive effects of C3a and C5a may suppress the immune system throughout the TME (Figure 2).
Figure 2.
Mechanisms by which cancer cells activate complement to control the tumor microenvironment. Tumor cells actively promote complement activation by several mechanisms. The natural antibody binds to glycans on the cell surface, and IgG binds to tumor neoepitopes. Cancer cells also produced complement proteins, such as C3, which fuels local activation. Cancer cells can also release proteases, such as cathepsin L, which directly activate complement proteins. Complement activation within tumors likely causes apoptosis and necrosis of some target cells, but it also produces C3a and C5a which recruit inhibitory myeloid cells into the tumor microenvironment. These myeloid cells suppress the anti-tumor function of CD4 and CD8 T cells.
7. Complement Inhibitors as Cancer Treatment
As outlined above, complement inhibitory drugs are effective for reducing tumor size in multiple different pre-clinical cancer models [1,41,42,44,102,103,104]. Inhibitory anti-C5 antibodies have been approved for several non-malignant diseases [105,106], and many additional complement inhibitory agents are in development [107]. Some of the new drugs block all activation, some selectively block the various activation pathways, and others target specific complement fragments and receptors. Thus, shortly there will likely be a range of therapeutic options for blocking the complement system. C3 fragments clearly play a role in tumor biology, but multiple studies have shown that C5aR antagonism is an effective cancer treatment. Several C5a antagonists are currently in clinical development for other indications, so this approach is already feasible.
If complement inhibitors are to be used to treat cancer, then it will be important to understand: (1) which types of cancer are responsive to this approach, (2) when in the course of the disease is complement inhibition most effective, and (3) which components of the complement system contribute to tumor growth. Furthermore, based on the experience with immune checkpoint inhibitors, complement inhibitory drugs will be most effective when combined with other therapies. The efficacy of including complement inhibitors in combination therapy likely depends on the treatments with which they are paired. For example, the efficacy of monoclonal antibodies often involves complement-mediated cytotoxicity. Consequently, the use of complement inhibitors could undermine the efficacy of these drugs. Indeed, some drugs impair the ability of cancer cells to regulate the complement cascade, thereby increasing complement activation on the cell surface. These agents have been used as a means of sensitizing tumors to monoclonal antibody treatments [108].
The combination of anti-complement drugs with immune checkpoint inhibitors may also represent a special case. In many studies, complement blockade has been shown to affect existing tumors via its effects on myeloid cell recruitment and polarization. This, in turn, enhances the anti-tumor effects of T cells. Complement inhibition and immune checkpoint inhibition, therefore, have similar, and possibly redundant, effects on anti-tumor immunity. However, preclinical studies also suggest that these drugs work by different mechanisms and can have additive effects on tumor size [104,109]. Indeed, a clinical trial is currently underway in which an anti-C5aR antibody is being combined with a PD-L1 antagonist for the treatment of solid tumors (NCT03665129; the type of cancer has not been disclosed). Finally, the development of novel targeted complement inhibitors might represent a therapeutic strategy to selectively regulate complement at the site of the tumor, without the adverse effects that might occur with systemic complement inhibition. Several fusion proteins have been developed which need to be tested in appropriate preclinical models [110].
8. Conclusions
One of the most unexpected and powerful discoveries in complement research is the critical role of this system in cancer biology. Although the full range of effects that complement fragments have on cancer initiation and tumor growth are not yet known, a frequent finding is that complement inhibition increases anti-tumor immunity and reduces tumor size. This is, in many respects, analogous to checkpoint inhibition. Many different complement inhibitors are in clinical development, and this class of drugs holds great promise for the treatment of cancer. Based on what is currently known about the role of complement in carcinogenesis, there is reason to suspect that complement inhibition can reduce the risk of tumor initiation in patients with some chronic inflammatory diseases, and it can slow the growth and spread of many types of cancer.
The optimal use of complement inhibitory drugs will entail a greater understanding of the role of complement activation in specific types of cancer, as well as the potential and limitations of combining complement inhibitory drugs with various other cancer therapies. Studies have shown that cancer cells express many different proteins that promote and inhibit complement activation, highlighting a complex interaction between cancer cells and complement proteins that may vary over time and throughout the tumor. Although disentangling all the details of this relationship will be challenging, many of the tools developed for complement research in other fields are being applied to cancer models. Furthermore, activation of the complement system generates several tissue bound and soluble biomarkers, which may provide accurate methods by which complement activation within a tumor can be monitored in the clinic.
Funding
This research was funded by National Institutes of Health Grant numbers DK113586, DK076690, CA225840, CA236222, the Department of Defense Grant LR180050 (JMT), and a grant from LUNGevity.
Conflicts of Interest
JMT receives royalties from Alexion Pharmaceuticals, Inc. and is a consultant for Q32 Bio, Inc., a company developing complement inhibitors. He also holds stock and will receive royalty income from Q32 Bio, Inc. The funders had no role in the writing of the manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Markiewski M.M., DeAngelis R.A., Benencia F., Ricklin-Lichtsteiner S.K., Koutoulaki A., Gerard C., Coukos G., Lambris J.D. Modulation of the antitumor immune response by complement. Nat. Immunol. 2008;9:1225–1235. doi: 10.1038/ni.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hanahan D., Weinberg R.A. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 3.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 4.De Martel C., Franceschi S. Infections and cancer: Established associations and new hypotheses. Crit. Rev. Oncol./Hematol. 2009;70:183–194. doi: 10.1016/j.critrevonc.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441:431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 6.Takahashi H., Ogata H., Nishigaki R., Broide D.H., Karin M. Tobacco smoke promotes lung tumorigenesis by triggering IKKbeta- and JNK1-dependent inflammation. Cancer Cell. 2010;17:89–97. doi: 10.1016/j.ccr.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doerner S.K., Reis E.S., Leung E.S., Ko J.S., Heaney J.D., Berger N.A., Lambris J.D., Nadeau J.H. High-Fat Diet-Induced Complement Activation Mediates Intestinal Inflammation and Neoplasia, Independent of Obesity. Mol. Cancer Res. 2016;14:953–965. doi: 10.1158/1541-7786.MCR-16-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waldner M.J., Neurath M.F. Colitis-associated cancer: The role of T cells in tumor development. Semin. Immunopathol. 2009;31:249–256. doi: 10.1007/s00281-009-0161-8. [DOI] [PubMed] [Google Scholar]
- 9.Franklin R.A., Liao W., Sarkar A., Kim M.V., Bivona M.R., Liu K., Pamer E.G., Li M.O. The cellular and molecular origin of tumor-associated macrophages. Science. 2014;344:921–925. doi: 10.1126/science.1252510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colegio O.R., Chu N.-Q., Szabo A.L., Chu T., Rhebergen A.M., Jairam V., Cyrus N., Brokowski C.E., Eisenbarth S.C., Phillips G.M., et al. Functional polarization of tumour-associated macrophages by tumour-derived lactic acid. Nature. 2014;513:559–563. doi: 10.1038/nature13490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murray P.J. Nonresolving macrophage-mediated inflammation in malignancy. FEBS J. 2018;285:641–653. doi: 10.1111/febs.14210. [DOI] [PubMed] [Google Scholar]
- 12.Allavena P., Sica A., Solinas G., Porta C., Mantovani A. The inflammatory micro-environment in tumor progression: The role of tumor-associated macrophages. Crit. Rev. Oncol./Hematol. 2008;66:1–9. doi: 10.1016/j.critrevonc.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Schreiber R.D., Old L.J., Smyth M.J. Cancer immunoediting: Integrating immunity’s roles in cancer suppression and promotion. Science. 2011;331:1565–1570. doi: 10.1126/science.1203486. [DOI] [PubMed] [Google Scholar]
- 14.Woo S.R., Corrales L., Gajewski T.F. Innate immune recognition of cancer. Annu. Rev. Immunol. 2015;33:445–474. doi: 10.1146/annurev-immunol-032414-112043. [DOI] [PubMed] [Google Scholar]
- 15.Wherry E.J. T cell exhaustion. Nat. Immunol. 2011;12:492–499. doi: 10.1038/ni.2035. [DOI] [PubMed] [Google Scholar]
- 16.Pardoll D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer. 2012;12:252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Topalian S.L., Drake C.G., Pardoll D.M. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–461. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walport M.J. Complement. First of two parts. N. Engl. J. Med. 2001;344:1058–1066. doi: 10.1056/NEJM200104053441406. [DOI] [PubMed] [Google Scholar]
- 19.Merle N.S., Church S.E., Fremeaux-Bacchi V., Roumenina L.T. Complement System Part I—Molecular Mechanisms of Activation and Regulation. Front. Immunol. 2015;6:262. doi: 10.3389/fimmu.2015.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coussens L.M., Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laskowski J., Renner B., Pickering M.C., Serkova N.J., Smith-Jones P.M., Clambey E.T., Nemenoff R.A., Thurman J.M. Complement factor H-deficient mice develop spontaneous hepatic tumors. J. Clin. Investig. 2020 doi: 10.1172/JCI135105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coussens L.M., Raymond W.W., Bergers G., Laig-Webster M., Behrendtsen O., Werb Z., Caughey G.H., Hanahan D. Inflammatory mast cells up-regulate angiogenesis during squamous epithelial carcinogenesis. Genes Dev. 1999;13:1382–1397. doi: 10.1101/gad.13.11.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fridlender Z.G., Albelda S.M. Tumor-associated neutrophils: Friend or foe? Carcinogenesis. 2012;33:949–955. doi: 10.1093/carcin/bgs123. [DOI] [PubMed] [Google Scholar]
- 24.Kraus S., Arber N. Inflammation and colorectal cancer. Curr. Opin. Pharmacol. 2009;9:405–410. doi: 10.1016/j.coph.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Guglietta S., Chiavelli A., Zagato E., Krieg C., Gandini S., Ravenda P.S., Bazolli B., Lu B., Penna G., Rescigno M. Coagulation induced by C3aR-dependent NETosis drives protumorigenic neutrophils during small intestinal tumorigenesis. Nat. Commun. 2016;7:11037. doi: 10.1038/ncomms11037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonavita E., Gentile S., Rubino M., Maina V., Papait R., Kunderfranco P., Greco C., Feruglio F., Molgora M., LaFace I., et al. PTX3 is an extrinsic oncosuppressor regulating complement-dependent inflammation in cancer. Cell. 2015;160:700–714. doi: 10.1016/j.cell.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Guerra C., Schuhmacher A.J., Cañamero M., Grippo P.J., Verdaguer L., Pérez-Gallego L., Dubus P., Sandgren E.P., Barbacid M. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell. 2007;11:291–302. doi: 10.1016/j.ccr.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 28.Sieweke M.H., Thompson N.L., Sporn M.B., Bissell M.J. Mediation of wound-related Rous sarcoma virus tumorigenesis by TGF-beta. Science. 1990;248:1656–1660. doi: 10.1126/science.2163544. [DOI] [PubMed] [Google Scholar]
- 29.Thurman J.M., Lenderink A.M., Royer P.A., Coleman K.E., Zhou J., Lambris J.D., Nemenoff R.A., Quigg R.J., Holers V.M. C3a is required for the production of CXC chemokines by tubular epithelial cells after renal ishemia/reperfusion. J. Immunol. 2007;178:1819–1828. doi: 10.4049/jimmunol.178.3.1819. [DOI] [PubMed] [Google Scholar]
- 30.Cho M.S., Vasquez H.G., Rupaimoole R., Pradeep S., Wu S., Zand B., Han H.-D., Rodriguez-Aguayo C., Bottsford-Miller J., Huang J., et al. Autocrine effects of tumor-derived complement. Cell Rep. 2014;6:1085–1095. doi: 10.1016/j.celrep.2014.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fan Z., Qin J., Wang D., Geng S. Complement C3a promotes proliferation, migration and stemness in cutaneous squamous cell carcinoma. J. Cell. Mol. Med. 2019;23:3097–3107. doi: 10.1111/jcmm.13959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu Y., Hu X.B. C5a stimulates the proliferation of breast cancer cells via Akt-dependent RGC-32 gene activation. Oncol. Rep. 2014;32:2817–2823. doi: 10.3892/or.2014.3489. [DOI] [PubMed] [Google Scholar]
- 33.Lara-Astiaso D., Izarra A., Estrada J.C., Albo C., Moscoso I., Samper E., Moncayo-Arlandi J., Solano A., Bernad A., Diez-Juan A. Complement anaphylatoxins C3a and C5a induce a failing regenerative program in cardiac resident cells. Evidence of a role for cardiac resident stem cells other than cardiomyocyte renewal. Springerplus. 2012;1:63. doi: 10.1186/2193-1801-1-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Daveau M., Benard M., Scotte M., Schouft M.-T., Hiron M., Francois A., Salier J.-P., Fontaine M. Expression of a functional C5a receptor in regenerating hepatocytes and its involvement in a proliferative signaling pathway in rat. J. Immunol. 2004;173:3418–3424. doi: 10.4049/jimmunol.173.5.3418. [DOI] [PubMed] [Google Scholar]
- 35.Strey C.W., Markiewski M., Mastellos D., Tudoran R., Spruce L.A., Greenbaum L.E., Lambris J.D. The proinflammatory mediators C3a and C5a are essential for liver regeneration. J. Exp. Med. 2003;198:913–923. doi: 10.1084/jem.20030374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vlaicu S.I., Tegla C.A., Cudrici C.D., Danoff J., Madani H., Sugarman A., Niculescu F., Mircea P.A., Rus V., Rus H. Role of C5b-9 complement complex and response gene to complement-32 (RGC-32) in cancer. Immunol. Res. 2013;56:109–121. doi: 10.1007/s12026-012-8381-8. [DOI] [PubMed] [Google Scholar]
- 37.Towner L.D., Wheat R.A., Hughes T.R., Morgan B.P. Complement Membrane Attack and Tumorigenesis: A systems biology approach. J. Biol. Chem. 2016;291:14927–14938. doi: 10.1074/jbc.M115.708446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Okroj M., Corrales L., Stokowska A., Pio R., Blom A.M. Hypoxia increases susceptibility of non-small cell lung cancer cells to complement attack. Cancer Immunol. Immunother. CII. 2009;58:1771–1780. doi: 10.1007/s00262-009-0685-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kurihara R., Yamaoka K., Sawamukai N., Shimajiri S., Oshita K., Yukawa S., Tokunaga M., Iwata S., Saito K., Chiba K., et al. C5a promotes migration, proliferation, and vessel formation in endothelial cells. Inflamm. Res. 2010;59:659–666. doi: 10.1007/s00011-010-0178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Olcina M.M., Balanis N.G., Kim R.K., Aksoy B.A., Kodysh J., Thompson M.J., Hammerbacher J., Graeber T.G., Giaccia A.J. Mutations in an Innate Immunity Pathway Are Associated with Poor Overall Survival Outcomes and Hypoxic Signaling in Cancer. Cell Rep. 2018;25:3721–3732.e6. doi: 10.1016/j.celrep.2018.11.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Corrales L., Ajona D., Rafail S., Lasarte J.J., Riezu-Boj J.I., Lambris J.D., Rouzaut A., Pajares M.J., Montuenga L.M., Pio R. Anaphylatoxin C5a creates a favorable microenvironment for lung cancer progression. J. Immunol. 2012;189:4674–4683. doi: 10.4049/jimmunol.1201654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kwak J.W., Laskowski J., Li H.Y., McSharry M.V., Sippel T.R., Bullock B.L., Johnson A.M., Poczobutt J.M., Neuwelt A.J., Malkoski S.P., et al. Complement Activation via a C3a Receptor Pathway Alters CD4(+) T Lymphocytes and Mediates Lung Cancer Progression. Cancer Res. 2018;78:143–156. doi: 10.1158/0008-5472.CAN-17-0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Medler T.R., Murugan D., Horton W., Kumar S., Cotechini T., Forsyth A.M., Leyshock P., Leitenberger J.J., Kulesz-Martin M., Margolin A.A., et al. Complement C5a Fosters Squamous Carcinogenesis and Limits T Cell Response to Chemotherapy. Cancer Cell. 2018;34:561–578.e6. doi: 10.1016/j.ccell.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nabizadeh J.A., Manthey H.D., Steyn F.J., Chen W., Widiapradja A., Akhir F.N.M., Boyle G.M., Taylor S.M., Woodruff T.M., Rolfe B.E. The Complement C3a Receptor Contributes to Melanoma Tumorigenesis by Inhibiting Neutrophil and CD4+ T Cell Responses. J. Immunol. 2016;196:4783–4792. doi: 10.4049/jimmunol.1600210. [DOI] [PubMed] [Google Scholar]
- 45.Downs-Canner S., Magge D., Ravindranathan R., O’Malley M.E., Francis L., Liu Z., Guo Z.S., Obermajer N., Bartlett D.L. Complement Inhibition: A Novel Form of Immunotherapy for Colon Cancer. Ann. Surg. Oncol. 2016;23:655–662. doi: 10.1245/s10434-015-4778-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vadrevu S.K., Chintala N.K., Sharma S.K., Sharma P., Cleveland C., Riediger L., Manne S., Fairlie D.P., Gorczyca W., Almanza O., et al. Complement c5a receptor facilitates cancer metastasis by altering T-cell responses in the metastatic niche. Cancer Res. 2014;74:3454–3465. doi: 10.1158/0008-5472.CAN-14-0157. [DOI] [PubMed] [Google Scholar]
- 47.Llaudo I., Fribourg M., Medof M.E., Conde P., Ochando J., Heeger P.S. C5aR1 regulates migration of suppressive myeloid cells required for costimulatory blockade-induced murine allograft survival. Am. J. Transplant. 2019;19:633–645. doi: 10.1111/ajt.15072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu Y., Huang Y., Xu W., Zheng X., Yi X., Huang L., Wang Y., Wu K. Activated Hepatic Stellate Cells (HSCs) Exert Immunosuppressive Effects in Hepatocellular Carcinoma by Producing Complement C3. OncoTargets Ther. 2020;13:1497–1505. doi: 10.2147/OTT.S234920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hsieh C.-C., Chou H.-S., Yang H.-R., Lin F., Bhatt S., Qin J., Wang L., Fung J.J., Qian S., Lu L. The role of complement component 3 (C3) in differentiation of myeloid-derived suppressor cells. Blood. 2013;121:1760–1768. doi: 10.1182/blood-2012-06-440214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sautes-Fridman C., Petitprez F., Calderaro J., Fridman W.H. Tertiary lymphoid structures in the era of cancer immunotherapy. Nat. Rev. Cancer. 2019;19:307–325. doi: 10.1038/s41568-019-0144-6. [DOI] [PubMed] [Google Scholar]
- 51.Lu Y., Zhao Q., Liao J.-Y., Song E., Xia Q., Pan J., Li Y., Li J., Zhou B., Ye Y., et al. Complement Signals Determine Opposite Effects of B Cells in Chemotherapy-Induced Immunity. Cell. 2020;180:1081–1097.e24. doi: 10.1016/j.cell.2020.02.015. [DOI] [PubMed] [Google Scholar]
- 52.Liszewski M.K., Kolev M., Le Friec G., Leung M., Bertram P.G., Fara A.F., Subias M., Pickering M.C., Drouet C., Meri S., et al. Intracellular complement activation sustains T cell homeostasis and mediates effector differentiation. Immunity. 2013;39:1143–1157. doi: 10.1016/j.immuni.2013.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.West E.E., Kunz N., Kemper C. Complement and human T cell metabolism: Location, location, location. Immunol. Rev. 2020;295:68–81. doi: 10.1111/imr.12852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Piao C., Zhang W.-M., Li T.-T., Zhang C.-C., Qiu S., Liu Y., Liu S., Jin M., Jia L.-X., Song W.-C., et al. Complement 5a stimulates macrophage polarization and contributes to tumor metastases of colon cancer. Exp. Cell Res. 2018;366:127–138. doi: 10.1016/j.yexcr.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 55.Boire A., Zou Y., Shieh J., Macalinao D.G., Pentsova E., Massague J. Complement Component 3 Adapts the Cerebrospinal Fluid for Leptomeningeal Metastasis. Cell. 2017;168:1101–1113.e13. doi: 10.1016/j.cell.2017.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hu W.H., Hu Z., Shen X., Dong L.Y., Zhou W.Z., Yu X.X. C5a receptor enhances hepatocellular carcinoma cell invasiveness via activating ERK1/2-mediated epithelial-mesenchymal transition. Exp. Mol. Pathol. 2016;100:101–108. doi: 10.1016/j.yexmp.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 57.Kaida T., Nitta H., Kitano Y., Yamamura K., Arima K., Izumi D., Higashi T., Kurashige J., Imai K., Hayashi H., et al. C5a receptor (CD88) promotes motility and invasiveness of gastric cancer by activating RhoA. Oncotarget. 2016;7:84798–84809. doi: 10.18632/oncotarget.12656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nitta H., Wada Y., Kawano Y., Murakami Y., Irie A., Taniguchi K., Kikuchi K., Yamada G., Suzuki K., Honda J., et al. Enhancement of human cancer cell motility and invasiveness by anaphylatoxin C5a via aberrantly expressed C5a receptor (CD88) Clin. Cancer Res. 2013;19:2004–2013. doi: 10.1158/1078-0432.CCR-12-1204. [DOI] [PubMed] [Google Scholar]
- 59.Gu J., Ding J.-Y., Lu C., Lin Z.-W., Chu Y., Zhao G.-Y., Guo J., Ge D. Overexpression of CD88 predicts poor prognosis in non-small-cell lung cancer. Lung Cancer. 2013;81:259–265. doi: 10.1016/j.lungcan.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 60.Coussens L.M., Zitvogel L., Palucka A.K. Neutralizing tumor-promoting chronic inflammation: A magic bullet? Science. 2013;339:286–291. doi: 10.1126/science.1232227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Blankenstein T., Coulie P.G., Gilboa E., Jaffee E.M. The determinants of tumour immunogenicity. Nat. Rev. Cancer. 2012;12:307–313. doi: 10.1038/nrc3246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rodier F., Coppé J.-P., Patil C.K., Hoeijmakers W.A.M., Muñoz D.P., Raza S.R., Freund A., Campeau E., Davalos A.R., Campisi J. Persistent DNA damage signalling triggers senescence-associated inflammatory cytokine secretion. Nat. Cell Biol. 2009;11:973–979. doi: 10.1038/ncb1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dunn G.P., Koebel C.M., Schreiber R.D. Interferons, immunity and cancer immunoediting. Nat. Rev. Immunol. 2006;6:836–848. doi: 10.1038/nri1961. [DOI] [PubMed] [Google Scholar]
- 64.Shankaran V., Ikeda H., Bruce A.T., White J.M., Swanson P.E., Old L.J., Schreiber R.D. IFNgamma and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature. 2001;410:1107–1111. doi: 10.1038/35074122. [DOI] [PubMed] [Google Scholar]
- 65.Garaud S., Zayakin P., Buisseret L., Rulle U., Siliņa K., De Wind A., Eyden G.V.D., Larsimont D., Willard-Gallo K., Linē A. Antigen Specificity and Clinical Significance of IgG and IgA Autoantibodies Produced in situ by Tumor-Infiltrating B Cells in Breast Cancer. Front. Immunol. 2018;9:2660. doi: 10.3389/fimmu.2018.02660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu W., Peng B., Lu Y., Xu W., Qian W., Zhang J.Y. Autoantibodies to tumor-associated antigens as biomarkers in cancer immunodiagnosis. Autoimmun. Rev. 2011;10:331–335. doi: 10.1016/j.autrev.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roumenina L.T., Daugan M.V., Noe R., Petitprez F., Vano Y.A., Sanchez-Salas R., Becht E., Meilleroux J., Le Clec’H B., A Giraldo N., et al. Tumor Cells Hijack Macrophage-Produced Complement C1q to Promote Tumor Growth. Cancer Immunol. Res. 2019;7:1091–1105. doi: 10.1158/2326-6066.CIR-18-0891. [DOI] [PubMed] [Google Scholar]
- 68.Bulla R., Tripodo C., Rami D., Ling G.S., Agostinis C., Guarnotta C., Zorzet S., Durigutto P., Botto M., Tedesco F. C1q acts in the tumour microenvironment as a cancer-promoting factor independently of complement activation. Nat. Commun. 2016;7:10346. doi: 10.1038/ncomms10346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ling G.S., Crawford G., Buang N., Bartok I., Tian K., Thielens N.M., Bally I., Harker J.A., Ashton-Rickardt P.G., Rutschmann S., et al. C1q restrains autoimmunity and viral infection by regulating CD8(+) T cell metabolism. Science. 2018;360:558–563. doi: 10.1126/science.aao4555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ehrenstein M.R., Notley C.A. The importance of natural IgM: Scavenger, protector and regulator. Nat. Rev. Immunol. 2010;10:778–786. doi: 10.1038/nri2849. [DOI] [PubMed] [Google Scholar]
- 71.Vollmers H.P., Brandlein S. Natural antibodies and cancer. New Biotechnol. 2009;25:294–298. doi: 10.1016/j.nbt.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 72.Hensel F., Hermann R., Schubert C., Abe N., Schmidt K., Franke A., Shevchenko A., Mann M., Müller-Hermelink H.K., Vollmers H.P. Characterization of glycosylphosphatidylinositol-linked molecule CD55/decay-accelerating factor as the receptor for antibody SC-1-induced apoptosis. Cancer Res. 1999;59:5299–5306. [PubMed] [Google Scholar]
- 73.Aykut B., Pushalkar S., Chen R., Li Q., Abengozar R., Kim J.I., Shadaloey S.A., Wu D., Preiss P., Verma N., et al. The fungal mycobiome promotes pancreatic oncogenesis via activation of MBL. Nature. 2019;574:264–267. doi: 10.1038/s41586-019-1608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Roumenina L.T., Daugan M.V., Petitprez F., Sautes-Fridman C., Fridman W.H. Context-dependent roles of complement in cancer. Nat. Rev. Cancer. 2019;19:698–715. doi: 10.1038/s41568-019-0210-0. [DOI] [PubMed] [Google Scholar]
- 75.Cho M.S., Rupaimoole R., Choi H.J., Noh K., Chen J., Hu Q., Sood A.K., Afshar-Kharghan V. Complement Component 3 Is Regulated by TWIST1 and Mediates Epithelial-Mesenchymal Transition. J. Immunol. 2016;196:1412–1418. doi: 10.4049/jimmunol.1501886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pratt J.R., Basheer S.A., Sacks S.H. Local synthesis of complement component C3 regulates acute renal transplant rejection. Nat. Med. 2002;8:582–587. doi: 10.1038/nm0602-582. [DOI] [PubMed] [Google Scholar]
- 77.Gocheva V., Joyce J.A. Cysteine cathepsins and the cutting edge of cancer invasion. Cell Cycle. 2007;6:60–64. doi: 10.4161/cc.6.1.3669. [DOI] [PubMed] [Google Scholar]
- 78.Frade R., Rodrigues-Lima F., Huang S., Xie K., Guillaume N., Bar-Eli M. Procathepsin-L, a proteinase that cleaves human C3 (the third component of complement), confers high tumorigenic and metastatic properties to human melanoma cells. Cancer Res. 1998;58:2733–2736. doi: 10.1016/S0161-5890(98)90609-5. [DOI] [PubMed] [Google Scholar]
- 79.Krisinger M.J., Goebeler V., Lu Z., Meixner S.C., Myles T., Pryzdial E.L., Conway E.M. Thrombin generates previously unidentified C5 products that support the terminal complement activation pathway. Blood. 2012;120:1717–1725. doi: 10.1182/blood-2012-02-412080. [DOI] [PubMed] [Google Scholar]
- 80.Reddel C.J., Tan C.W., Chen V.M. Thrombin Generation and Cancer: Contributors and Consequences. Cancers. 2019;11:100. doi: 10.3390/cancers11010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Manning M.L., Williams S.A., Jelinek C.A., Kostova M.B., Denmeade S.R. Proteolysis of complement factors iC3b and C5 by the serine protease prostate-specific antigen in prostatic fluid and seminal plasma. J. Immunol. 2013;190:2567–2574. doi: 10.4049/jimmunol.1200856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schmidt C.Q., Lambris J.D., Ricklin D. Protection of host cells by complement regulators. Immunol. Rev. 2016;274:152–171. doi: 10.1111/imr.12475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ravindranath N.M., Shuler C. Expression of complement restriction factors (CD46, CD55 & CD59) in head and neck squamous cell carcinomas. J. Oral Pathol. Med. 2006;35:560–567. doi: 10.1111/j.1600-0714.2006.00466.x. [DOI] [PubMed] [Google Scholar]
- 84.Goslings W.R., Blom D.J., De Waard-Siebinga I., Van Beelen E., Claas F.H., Jager M.J., Gorter A. Membrane-bound regulators of complement activation in uveal melanomas. CD46, CD55, and CD59 in uveal melanomas. Investig. Ophthalmol. Visual Sci. 1996;37:1884–1891. [PubMed] [Google Scholar]
- 85.Bjorge L., Vedeler C.A., Ulvestad E., Matre R. Expression and function of CD59 on colonic adenocarcinoma cells. Eur. J. Immunol. 1994;24:1597–1603. doi: 10.1002/eji.1830240722. [DOI] [PubMed] [Google Scholar]
- 86.Simpson K.L., Jones A., Norman S., Holmes C.H. Expression of the complement regulatory proteins decay accelerating factor (DAF, CD55), membrane cofactor protein (MCP, CD46) and CD59 in the normal human uterine cervix and in premalignant and malignant cervical disease. Am. J. Pathol. 1997;151:1455–1467. [PMC free article] [PubMed] [Google Scholar]
- 87.Murray K.P., Mathure S., Kaul R., Khan S., Carson L.F., Twiggs L.B., Martens M.G., Kaul A. Expression of complement regulatory proteins-CD 35, CD 46, CD 55, and CD 59-in benign and malignant endometrial tissue. Gynecol. Oncol. 2000;76:176–182. doi: 10.1006/gyno.1999.5614. [DOI] [PubMed] [Google Scholar]
- 88.Geis N., Zell S., Rutz R., Li W., Giese T., Mamidi S., Schultz S., Kirschfink M. Inhibition of membrane complement inhibitor expression (CD46, CD55, CD59) by siRNA sensitizes tumor cells to complement attack in vitro. Curr. Cancer Drug Targets. 2010;10:922–931. doi: 10.2174/156800910793357952. [DOI] [PubMed] [Google Scholar]
- 89.Blok V.T., Daha M.R., Tijsma O.M., Weissglas M.G., van den Broek L.J., Gorter A. A possible role of CD46 for the protection in vivo of human renal tumor cells from complement-mediated damage. Lab. Investig. 2000;80:335–344. doi: 10.1038/labinvest.3780038. [DOI] [PubMed] [Google Scholar]
- 90.Surowiak P., Materna V., Maciejczyk A., Kaplenko I., Spaczyński M., Dietel M., Lage H., Zabel M. CD46 expression is indicative of shorter revival-free survival for ovarian cancer patients. Anticancer Res. 2006;26:4943–4948. [PubMed] [Google Scholar]
- 91.Ajona D., Castaño Z., Garayoa M., Zudaire E., Pajares M.J., Martínez A., Cuttitta F., Montuenga L.M., Pio R. Expression of complement factor H by lung cancer cells: Effects on the activation of the alternative pathway of complement. Cancer Res. 2004;64:6310–6318. doi: 10.1158/0008-5472.CAN-03-2328. [DOI] [PubMed] [Google Scholar]
- 92.Wilczek E., Rzepko R., Nowis D., Legat M., Golab J., Glab M., Gorlewicz A., Konopacki F., Mazurkiewicz M., Śladowski D., et al. The possible role of factor H in colon cancer resistance to complement attack. Int. J. Cancer. 2008;122:2030–2037. doi: 10.1002/ijc.23238. [DOI] [PubMed] [Google Scholar]
- 93.Junnikkala S., Hakulinen J., Jarva H., Manuelian T., Bjørge L., Bützow R., Zipfel P.F., Meri S. Secretion of soluble complement inhibitors factor H and factor H-like protein (FHL-1) by ovarian tumour cells. Br. J. Cancer. 2002;87:1119–1127. doi: 10.1038/sj.bjc.6600614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ajona D., Hsu Y.F., Corrales L., Montuenga L.M., Pio R. Down-regulation of human complement factor H sensitizes non-small cell lung cancer cells to complement attack and reduces in vivo tumor growth. J. Immunol. 2007;178:5991–5998. doi: 10.4049/jimmunol.178.9.5991. [DOI] [PubMed] [Google Scholar]
- 95.Riihilä P., Nissinen L., Farshchian M., Kivisaari A., Ala-Aho R., Kallajoki M., Grénman R., Meri S., Peltonen S., Peltonen J., et al. Complement factor I promotes progression of cutaneous squamous cell carcinoma. J. Investig. Dermatol. 2015;135:579–588. doi: 10.1038/jid.2014.376. [DOI] [PubMed] [Google Scholar]
- 96.Fedarko N.S., Fohr B., Robey P.G., Young M.F., Fisher L.W. Factor H binding to bone sialoprotein and osteopontin enables tumor cell evasion of complement-mediated attack. J. Biol. Chem. 2000;275:16666–16672. doi: 10.1074/jbc.M001123200. [DOI] [PubMed] [Google Scholar]
- 97.Meng Z.W., Liu M.C., Hong H.J., Du Q., Chen Y.L. Expression and prognostic value of soluble CD97 and its ligand CD55 in intrahepatic cholangiocarcinoma. Tumour Biol. 2017;39 doi: 10.1177/1010428317694319. [DOI] [PubMed] [Google Scholar]
- 98.Ouyang Q., Zhang L., Jiang Y., Ni X., Chen S., Ye F., Du Y., Huang L., Ding P., Wang N., et al. The membrane complement regulatory protein CD59 promotes tumor growth and predicts poor prognosis in breast cancer. Int. J. Oncol. 2016;48:2015–2024. doi: 10.3892/ijo.2016.3408. [DOI] [PubMed] [Google Scholar]
- 99.Niehans G.A., Cherwitz D.L., Staley N.A., Knapp D.J., Dalmasso A.P. Human carcinomas variably express the complement inhibitory proteins CD46 (membrane cofactor protein), CD55 (decay-accelerating factor), and CD59 (protectin) Am. J Pathol. 1996;149:129–142. [PMC free article] [PubMed] [Google Scholar]
- 100.Bjorge L., Jensen T.S., Ulvestad E., Vedeler C.A., Matre R. The influence of tumour necrosis factor-alpha, interleukin-1 beta and interferon-gamma on the expression and function of the complement regulatory protein CD59 on the human colonic adenocarcinoma cell line HT29. Scand. J. Immunol. 1995;41:350–356. doi: 10.1111/j.1365-3083.1995.tb03578.x. [DOI] [PubMed] [Google Scholar]
- 101.Spiller O.B., Criado-Garcia O., Rodriguez De Cordoba S., Morgan B.P. Cytokine-mediated up-regulation of CD55 and CD59 protects human hepatoma cells from complement attack. Clin. Exp. Immunol. 2000;121:234–241. doi: 10.1046/j.1365-2249.2000.01305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Janelle V., Langlois M.P., Tarrab E., Lapierre P., Poliquin L., Lamarre A. Transient Complement Inhibition Promotes a Tumor-Specific Immune Response through the Implication of Natural Killer Cells. Cancer Immunol. Res. 2014;2:200–206. doi: 10.1158/2326-6066.CIR-13-0173. [DOI] [PubMed] [Google Scholar]
- 103.Wang X., Schoenhals J.E., Li A., Valdecanas D.R., Ye H., Zhang F., Tang C., Tang M., Liu C.-G., Liu X., et al. Suppression of Type I IFN Signaling in Tumors Mediates Resistance to Anti-PD-1 Treatment That Can Be Overcome by Radiotherapy. Cancer Res. 2017;77:839–850. doi: 10.1158/0008-5472.CAN-15-3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ajona D., Ortiz-Espinosa S., Moreno H., Lozano T., Pajares M.J., Agorreta J., Bértolo C., Lasarte J.J., Vicent S., Hoehlig K., et al. A Combined PD-1/C5a Blockade Synergistically Protects against Lung Cancer Growth and Metastasis. Cancer Discov. 2017;7:694–703. doi: 10.1158/2159-8290.CD-16-1184. [DOI] [PubMed] [Google Scholar]
- 105.Rondeau E., Scully M., Ariceta G., Barbour T., Cataland S., Heyne N., Miyakawa Y., Ortiz S., Swenson E., Vallee M., et al. The long-acting C5 inhibitor, Ravulizumab, is effective and safe in adult patients with atypical hemolytic uremic syndrome naive to complement inhibitor treatment. Kidney Int. 2020;97:1287–1296. doi: 10.1016/j.kint.2020.01.035. [DOI] [PubMed] [Google Scholar]
- 106.Rother R.P., Rollins S.A., Mojcik C.F., Brodsky R.A., Bell L. Discovery and development of the complement inhibitor eculizumab for the treatment of paroxysmal nocturnal hemoglobinuria. Nat. Biotechnol. 2007;25:1256–1264. doi: 10.1038/nbt1344. [DOI] [PubMed] [Google Scholar]
- 107.Mastellos D.C., Ricklin D., Lambris J.D. Clinical promise of next-generation complement therapeutics. Nat. Rev. Drug Discov. 2019;18:707–729. doi: 10.1038/s41573-019-0031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fishelson Z., Donin N., Zell S., Schultz S., Kirschfink M. Obstacles to cancer immunotherapy: Expression of membrane complement regulatory proteins (mCRPs) in tumors. Mol. Immunol. 2003;40:109–123. doi: 10.1016/S0161-5890(03)00112-3. [DOI] [PubMed] [Google Scholar]
- 109.Wang Y., Sun S.-N., Liu Q., Yu Y.-Y., Guo J., Wang K., Xing B.-C., Zheng Q.-F., Campa M.J., Patz E.F., et al. Autocrine Complement Inhibits IL10-Dependent T-cell-Mediated Antitumor Immunity to Promote Tumor Progression. Cancer Discov. 2016;6:1022–1035. doi: 10.1158/2159-8290.CD-15-1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tomlinson S., Thurman J.M. Tissue-targeted complement therapeutics. Mol. Immunol. 2018;102:120–128. doi: 10.1016/j.molimm.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]