Abstract
Background
Sarcopenia is a geriatric syndrome associated with negative health outcomes and the use of viable alternative screening tools may help in the diagnosis of this condition. This study aimed to analyze the association of sarcopenia with anthropometric indicators among community-dwelling older adults and to identify cut-off points for such indicators as a discriminant criterion for predicting sarcopenia.
Methods
This was a cross-sectional study conducted on community-dwelling older adults ≥60 years old (n = 411) of both sexes from Macapá, Amapá, Brazil. Socioeconomic, clinical and anthropometric data (arm circumference - AC, waist circumference - WC, calf circumference - CC and body mass index – BMI) were collected using a structured form. Sarcopenia was identified according to the EWGSOP 2 consensus. The association between anthropometric indicators and sarcopenia was performed using logistic regression and cut-off points established from the ROC Curve. Statistical significance was defined as p ≤ 0.05.
Results
Adjusted analysis indicated an independent and inverse association between sarcopenia and the anthropometric indicators: AC (odds ratio, OR: 0.63; 95% confidence interval, 95%CI: 0.53–0.76), CC (OR: 0.73; 95%CI: 0.62–0.85), WC (OR: 0.93; 95%CI: 0.90–0.97) and BMI (OR: 0.64; 95%CI: 0.53–0.76). The following cut-off points for older men and women represented the discriminant criterion for the presence of sarcopenia: WC (≤97 and ≤ 86 cm), CC (≤33 and ≤ 31 cm), AC (≤27 cm) and BMI (≤24.8 kg/m2 and ≤ 24.5 kg/m2) (area under the ROC curve superior to 0.70). BMI and AC were the indicators with the highest ability to discriminate older adults of both sexes with sarcopenia.
Conclusions
An increase of one unit of the indicators can reduce the probability of occurrence of sarcopenia. All indicators were considered to discriminate the occurrence of sarcopenia, with emphasis on BMI and AC, and could be used to screen for this condition among community-dwelling older adults.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-020-01923-y.
Keywords: Sarcopenia, Anthropometry, Older adult health, Urban population
Background
Sarcopenia is a muscle disease with cumulative characteristics in lifetime, defined by low levels of muscle strength, muscle quantity/quality and physical performance [1]. The condition is associated with negative health outcomes among older adults, impairing functional ability and the quality of life, causing falls and fractures, and involving high health care costs and mortality rates [2]. Its prevalence is 1 to 29% among community-dwelling older adults [2] and about 17% in the older Brazilian population [3].
In view of the impact of sarcopenia on the public health area, an early identification of the condition becomes relevant [4]. The diagnosis can be made by determining a reduction of muscle mass accompanied by reduced muscle strength and/or reduced physical performance, the latter conditions being assessed by dynamometry and gait speed, respectively [5]. Dual-energy X-ray emission absorptiometry (DXA), magnetic resonance (MR) or computed tomography (CT) are specifically recommended for the assessment of low muscle quality and quantity. However, these are expensive methods involving the risk of exposure to radiation and are little available to the public [6]. Thus, simpler low-cost, noninvasive and easily applicable methods such as anthropometry may represent viable alternative screening tools helping the diagnosis of sarcopenia [7, 8].
Several studies have pointed out the use of anthropometry for the screening of sarcopenia [5, 8–10], however these studies has been performed in different countries with different life-style as Australia, Korea, Japan and Turkey, which make difficult generalize data from them to use in South American countries. In addition, the World Health Organization (WHO) [11] considers calf circumference (CC) to be a more sensitive anthropometric index of muscle mass among older adults, although arm circumference (AC), Abdominal circumference (AbC) and body mass index (BMI) have also been used and documented in the scientific literature as predictors of sarcopenia [9, 12].
Studies conducted in Brazil are recent and have determined the viability of CC as a discriminator of muscle mass in older adults [13, 14], as well as BMI [15], waist-height ratio and waist circumference identified with DXA [7]. Besides, the majority of this studies have been mostly performed and developed in specifics regions or states in Brazil [3]. Thus, there are few studies conducted in the northern region of Brazil that investigate how these older adults are getting older and if they are sarcopenic. This information is important, mainly because the Northern Brazil region, or more specifically in Macapá city, the Amazon region, is located in one of the least developed regions of the country, which fortify the technological resource scarcity, considered the gold standard instrument to assess sarcopenia.
According to data estimated [16], in the year 2010, the city of Macapá had 16% of the population living in the subnormal agglomerations, or places with no planning and situated in areas considered as inappropriate called areas of “ressaca”, “baixadas” or stilt. The areas of “ressaca” cover 20% of the city’s urban perimeter [17], “they behave like natural water reservoirs in a complex and distinct ecosystem and suffering the effects of tidal action through an intricate network of canals and streams plus the seasonal rain cycle” [18]. For this, the subnormal agglomerations areas are locations which are low socioeconomic conditions and difficult to access readily, which make hard the dislocation of the residents from their houses to hospitals or the access of basic healthcare professionals. Thus, there is an urgent necessity to adopt easy-to-use instruments as anthropometric indicators to identify geriatrics syndromes as sarcopenia in these areas, once it is impossible take huge or expensive equipment in these areas.
In view of the scarcity of studies validating anthropometric measures as screening tools for sarcopenia among older persons, according to Cruz-Jentoft et al. [19], it is to be believed that such indicators may represent a viable and additional alternative to be used to facilitate screening in order to guide the diagnosis of sarcopenia and the appropriate interventions, with an impact on health care for the older population, especially in areas of the Brazilian Amazon region. Besides, validating the anthropometric measures and finding the cut-off points to determine the sarcopenia condition, it will be possible to analyze if this data is different from the other studies and understand the impact of environmental factors on the living conditions of population from the Northern Brazil region.
Thus, the objectives of the present study were to analyze the association between sarcopenia and anthropometric indicators among community-living older subjects and to identify cut-off points for the anthropometric indicators as a discriminant criterion for the prediction of sarcopenia.
Methods
Context and study population
This was a cross-sectional study conducted on 411 older adults residing in the urban area of Macapá, in 2017. Information about the characteristics of the population and sample calculation, as well as the procedures for data collection are available in a previously published study [20]. The present study was approved by the Research Ethics Committee (protocol n° 1.738.671).
The study was conducted on subjects aged 60 years or older who resided in the urban area of the municipality of Macapá, able to walk with or without help, and who gave written informed consent to participate. Subjects who could not be located after three attempts by the interviewer, who had moved to another city, who were hospitalized and who had neurological sequelae and/or conditions that would not permit their assessment, were excluded.
Also excluded were subjects with cognitive decline that would prevent them from responding to the questions of the interviewer and from performing the tests, as determined by the translated version of the Mini Mental State Examination (MMSE) validated for Brazil, which considers cut-off points based on schooling level [21].
Instruments for data collection
Sarcopenia (dependent variable)
Sarcopenia was established using the operational definition recommended by the European Working Group on Sarcopenia in Older People (EWGSOP) 2 and the diagnosis considered the associated of low muscle strength and low muscle mass [19]:
Low muscle mass: The muscle mass component was measured based on the total muscle mass (TMM) estimated by the equation proposed by Lee et al. [22], validated for use in Brazilian elderly [23] and used in previous population-based studies [20, 24]: [MMT (kg) = (0.244 x body weight) + (7.8 x height) - (0.098 x age) + (6.6 x sex) + (ethnicity - 3.3)]. The equation considers the parameters body mass, height, sex, age and race. For the sex variable, 0 = women and 1 = men; for ethnicity, 0 = white and indigenous, − 1.2 = yellow and 1.4 = black and brown were adopted. Based on the TMM, the muscle mass index (MMI = TMM / height2) was calculated. The cut-off point for muscle mass index (MMI) in the present study considered the 20th percentile of the sample studied, according to previous studies [25, 26] and represented values < 9.61 kg/m2 for men and < 6.92 kg/m2 for women [20, 24].
Reduction of muscle strength was measured with a manual hydraulic dynamometer, SAEHAN® Hydraulic Hand Dynamometer, model SH5001, using handgrip strength (HGS) in an isometric manner based on kg/force (kgf) as recommended by the American Society of Hand Therapists [27]. Three measurements were made at one-minute intervals in the dominant limb and their mean value was considered. Values of less than 27 kgf for men and less than 16 kgf for women were considered to indicate reduced muscle strength [28].
Anthropometric indicators (independent variable)
The following anthropometric indicators were assessed in the present study: Body Mass Index (BMI), calf circumference (CC), waist circumference (WC), and arm circumference (AC). The perimeters/circumferences were measured with an inelastic tape. BMI was determined with a portable digital scale (Whole Body Control Scale, Omron, Model HBF 514C, 150 kg), with the subject barefoot and wearing the minimum amount of clothing possible. As recommended, the height was measured with the person barefoot, standing straight with joined feet and with the heels, buttocks and head in contact with the wall, keeping his eyes fixed on a horizontal axis parallel to the floor. BMI was defined as kg/height2 [29, 30].
AC was measured at the midpoint between acromion and olecranon in the arm of the subject resting against his body in a relaxed manner [31, 32]. CC can be measured on the point of largest perimeter of the right or left leg, with the subject sitting or lying in dorsal decubitus without contracting the calf muscles [33]. In the present study we measured the left leg with the subject in the sitting position.
WC was measured using the protocol recommended by the WHO [34], i.e., at the approximate midpoint between the lower margin of the last palpable rib and the top of the iliac crest. Other elements were considered like as posture, breathing phase and abdominal tension. The posture recommended here was orthostatic position, arms along the sides of the body, joined feet and weight uniformly distributed between them. WC should be measured at the end of a normal expiration, and abdominal tension at the measuring point should be avoided, i.e., the subject should remain relaxed during the measurement [34, 35].
Adjustment variables
Variables such as age, sex, schooling, income, health perception, number of diseases and medications, hospitalization, and the occurrence of falls in the last ear were recorded on a structured form. The subjects were asked to report the use of tobacco and its duration (years) (yes/no). Functional capacity was assessed using the Katz independence Scale for basic activities of daily life (BADL) [36] and the Lawton and Brody scale [37] for instrumental activities of daily life (IADL). Older adults who did not show difficulty in performing any BADL or IADL were considered to be independent, while subjects with difficulty in performing one or more activity were considered to be dependent. The level of physical activity was determined using the long version of the International Physical Activity Questionnaire (IPAQ) [33]. Subjects were considered to be sufficiently active when they engaged in vigorous physical activity for 150 min or more per week and subjects who engaged in 0 to 149 min of vigorous or moderate weekly activity per week were considered to be inactive. The complete version of the interview guide is available in Additional file 1.
Statistical analysis
Data are reported as means, standard deviations, median (interquartile range), absolute number, and percentage. Comparative analysis between the sarcopenic and non-sarcopenic groups was carried out using the Student t-test and Mann Whitney U test, according to the data distribution verified by the Kolmogorov-Smirnov test, for the quantitative variables and the chi-square test for the categorical variables. The association between anthropometric indicators (independent variable) and sarcopenia (dependent variable) was determined by crude and adjusted analysis using the logistic regression model and the estimate of the odds ratio (OR), with the 95% confidence interval (95%CI), and the level of significance set at 5% (p < 0.05). The Hosmer and Lemeshow test (p > 0.05) was applied to analyze the degree of model fit. All analyses were carried out using the Statistical Package for the Social Sciences (SPSS) version 21.0.
Receiver Operating Characteristic (ROC) curves were constructed to determine the cut-off points of the anthropometric indicators as discriminators of sarcopenia, and the area under the ROC curve (AUC), the sensitivity and specificity were determined using the MedCalc 11.4.4 software, with 95%CI and a 5% level of significance (p < 0.05).
Results
The final sample consisted of 411 older adults recruited on the basis of inclusion and exclusion criteria. The characteristics of the selected subjects are listed in Table 1. The prevalence of sarcopenia was 6.1% (n = 25). Sarcopenic subjects had lower values of anthropometric indicators than non-sarcopenic subjects (p < 0.05) (Table 1).
Table 1.
Characteristics of the older adults according to sarcopenia
| Variables | Sarcopenic (n = 25) |
Non-sarcopenic (n = 386) |
p* Value | Total sample (n = 411) |
|---|---|---|---|---|
| Age (years) | 77.04 ± 8.99 | 69.69 ± 6.90 | < 0.001 | 70.15 ± 7.25 |
| Sex | ||||
| Male | 10 (40) | 128 (33.2) | 0.483 | 138 (33.6) |
| Female | 15 (60) | 258 (66.8) | 273 (66.4) | |
| Height (m) | 1.51 (1.46–1.58) | 1.54 (1.48–1.60) | 0.244 | 1.52 (1.48–1.60) |
| Weight (kg) | 50.28 ± 7.96 | 67.86 ± 12.86 | < 0.001 | 66.79 ± 12.29 |
| Schooling (years) | 3 (1.5–7) | 5 (2–10) | 0.202 | 4 (2–10) |
| Income | ||||
| None | 1 (4) | 43 (11.1) | 0.311 | 44 (10.7) |
| 1 minimum wage or less | 15 (60) | 178 (46.1) | 193 (47) | |
| 2 minimum wages or more | 9 (36) | 165 (42.7) | 174 (42.3) | |
| Health perception | ||||
| Positive | 8 (32) | 116 (30.1) | 0.844 | 124 (30.2) |
| Negative | 17 (68) | 269 (69.9) | 286 (69.8) | |
| MMI (kg/m2) | 7.17 ± 1.56 | 9.02 ± 1.70 | < 0.001 | 8.91 ± 1.74 |
| HGS (kgf) | 16.52 ± 4.73 | 25.18 ± 8.96 | < 0.001 | 24.65 ± 9.01 |
| Number of diseases | 4 (3–7) | 5 (3–7) | 0.803 | 5 (3–7) |
| Number of medications | 1 (0–2) | 1 (0–3) | 0.534 | 1 (0–3) |
| Falls in the last year | ||||
| Yes | 2 (8) | 81 (21) | 0.117 | 83 (20.2) |
| No | 23 (92) | 305 (79) | 328 (79.8) | |
| Hospitalization in the last year | ||||
| Yes | 5 (20) | 53 (13.7) | 0.485 | 58 (14.1) |
| No | 20 (80) | 333 (86.3) | 353 (85.9) | |
| Smoking habit | ||||
| Yes | 4 (16) | 35 (9.1) | 0.289 | 39 (9.5) |
| No | 21 (84) | 351 (90.9) | 372 (90.5) | |
| Physical activity | ||||
| Sufficiently active | 9 (36) | 209 (54.1) | 0.078 | 218 (53) |
| Insufficiently active | 16 (64) | 177 (45.9) | 193 (47) | |
| Dependence (Katz Scale) | ||||
| Yes | 2 (8) | 28 (7.3) | 0.891 | 30 (7.3) |
| No | 23 (92) | 358 (92.7) | 381 (92.7) | |
| Dependence (Lawton and Brody Scale) | ||||
| Yes | 20 (80) | 266 (68.9) | 0.243 | 286 (69.6) |
| No | 5 (20) | 120 (31.1) | 125 (30.4) | |
| Body mass index (BMI) | 21.69 ± 2.12 | 28.53 ± 4.81 | < 0.001 | 28.11 ± 4.97 |
| Calf circumference (CC) | 29.57 ± 2.64 | 33.45 ± 3.81 | < 0.001 | 33.22 ± 3.86 |
| Arm circumference (AC) | 24.10 ± 2.29 | 29.51 ± 3.70 | < 0.001 | 29.18 ± 3.85 |
| Waist circumference (WC) | 90 (79.75–96) | 98 (90–105) | < 0.001 | 97 (90–105) |
Data are reported as n: number of subjects; mean ± standard deviation; median (interquartile range); m: meters; kg: kilogram; MMI: muscle mass index; HGS: handgrip strength; kgf: kilogram force; Chi-square test, Student t-test and MannWhitney U test; *p < 0.05
Table 2 presents the adjusted analysis and indicates an independent and inverse association between sarcopenia and the anthropometric indicators, with the increase of one unit of BMI, AC, CC and WC reducing the probability of the subjects to have sarcopenia by approximately 36, 37, 27 and 7%, respectively.
Table 2.
Association between sarcopenia and anthropometric indicators among community-dwelling older adults
| Variables | Sarcopenia | ||
|---|---|---|---|
| Anthropometric indicators | OR | 95%CI | p* Value |
| Body mass index (BMI) | |||
| Unadjusted | 0.66 | 0.57–0.76 | < 0.001 |
| Adjusted | 0.64 | 0.53–0.76 | < 0.001 |
| Calf circumference (CC) | |||
| Unadjusted | 0.73 | 0.64–0.83 | < 0.001 |
| Adjusted | 0.73 | 0.62–0.85 | < 0.001 |
| Arm circumference (AC) | |||
| Unadjusted | 0.63 | 0.54–0.73 | < 0.001 |
| Adjusted | 0.63 | 0.53–0.76 | < 0.001 |
| Waist circumference (WC) | |||
| Unadjusted | 0.94 | 0.91–0.97 | < 0.001 |
| Adjusted | 0.93 | 0.90–0.97 | < 0.001 |
OR: Odds Ratio; 95%CI: 95% Confidence interval; * p < 0.05; Adjusted for age, sex, schooling, income, health perception, number of diseases and medications, hospitalization and occurrence of falls in the last year, smoking habit, level of physical activity, functional disability for basic and instrumental activities of daily life; Hosmer-Lemeshow test (p > 0.05)
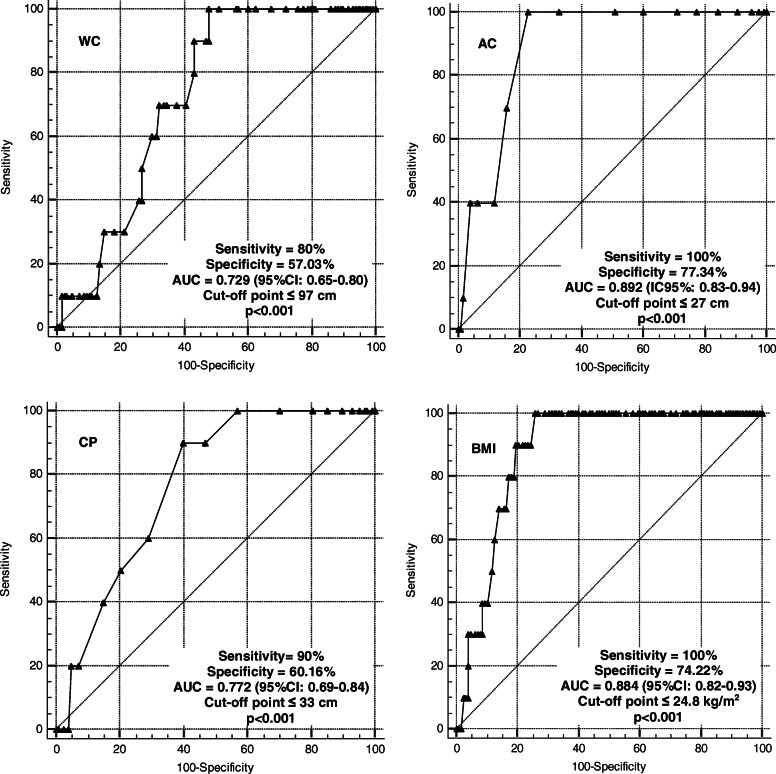
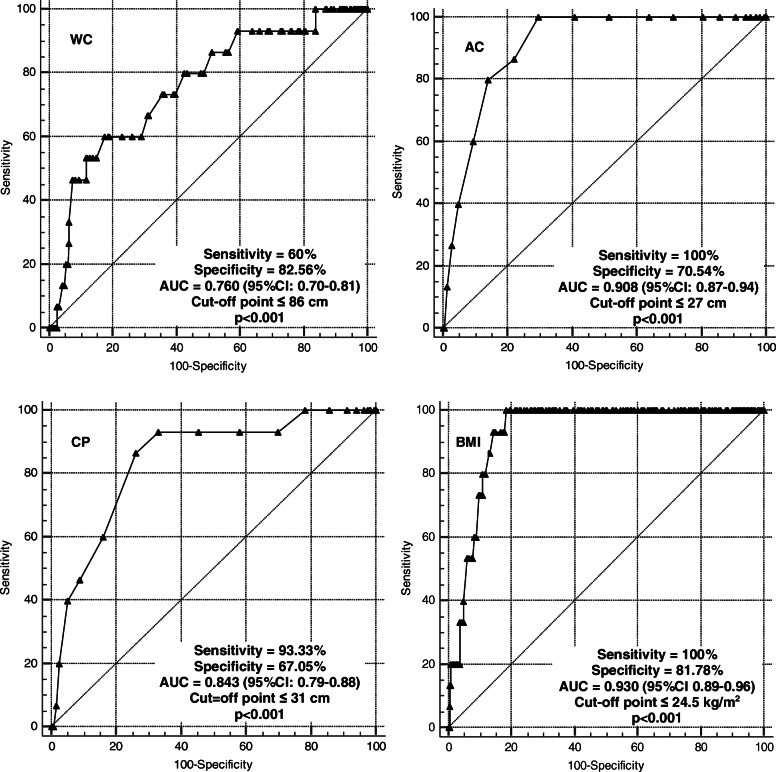
The results of the area under the ROC curve indicated coefficients higher than 0.7, representing acceptable discrimination (Figs. 1 and 2). The cut-off points for the older men and women, respectively, represented the discriminant criterion for the presence of sarcopenia, as follows: WC (≤97 and ≤ 86 cm), CC (≤33 and ≤ 31 cm), AC (≤27 cm) and BMI (≤24.8 kg/m2 and ≤ 24.5 kg/m2) (p < 0.05) [38]. BMI and AC were the indicators with the higher ability to discriminate older subjects with sarcopenia of both sexes.
Fig. 1.
Areas under the ROC curve for the anthropometric indicators as discriminants for the presence of sarcopenia among older men. AUC: area under the ROC curve; CI: confidence interval; WC: waist circumference; AC: arm circumference; CC: calf circumference; BMI: body mass index
Fig. 2.
Areas under the ROC curve for the anthropometric indicators as discriminants for the presence of sarcopenia among older women. AUC: area under the ROC curve; CI: confidence interval; WC: waist circumference; AC: arm circumference; CC: calf circumference; BMI: body mass index
Discussion
The present study demonstrated an association between all anthropometric indicators and sarcopenia among community-living older adults, with good predictive and discriminatory power [39]. However, the cut-off points that provided the best balance between sensitivity and specificity were ≤ 24.8 kg/m2 and ≤ 24.5 kg/m2 for BMI among men and women, respectively, and ≤ 27 cm AC for both sexes.
Several studies have shown that anthropometric measurements are useful for the screening of sarcopenia associated with conditions of reduced muscle mass, falls, functionality, and mortality [8, 10, 12, 26, 40, 41]. However, few studies have investigated and validated in a single population all the measurements proposed in the present study.
Regarding CC, the literature has reported a cut-off point of < 31 cm for the screening of sarcopenia [15, 19, 33, 42–44]. A study on the Korean population [8] (mean age: 76.2 years) also reported CC values differing from those reported here, i.e., < 35 for men and < 33 cm for women. In the Japanese population [9] (mean age: 61 years for women and 63 years for men), it were obtained cut-off points for sarcopenia of < 34 cm for men and < 33 cm for women, those exact values were also obtained in a Brazilian study [14] (60 years of age for women and 70 years of age for men). Since the above studies were conducted on an older population of different age ranges, it is difficult to compare their results with the present ones, which involved subjects with a mean age of 77 years. This is confirmed by other studies [10] which reported different and significant results between anthropometric measurements according to age ranges of 60–64, 65–69, 70–74, 75–79, and > 80 years.
Another indicator that showed correlation with sarcopenia in the present study was WC, with cut-off points of ≤97 cm for men (sensitivity = 80% specificity = 57.03%) and ≤ 86 cm for women (sensitivity: 60%, specificity: 82,56%). These results agree with previous study [7] with cut-off points of 92 cm for men (sensitivity: 79.5%, specificity: 66.7%) and 88 cm for women (sensitivity: 65.1%, specificity 85.7%). Also WC, in addition to being a good indicator of sarcopenia, can also be used for the assessment of body composition and central obesity [7].
AC as a single indicator showed association with sarcopenia, with a significant difference from the non-sarcopenic group. The cut-off points obtained were ≤ 27 cm for both sexes, with 100% sensitivity and 77.34% specificity for men and de 100% sensitivity and 70.54% for women. Other studies [10, 25] used corrected arm muscle area and obtained results different from the present ones, with cut-off points of 24.7 cm, 23.8 cm and 21 cm for men and 23.3 cm, 24.7 cm, 23.9 cm e 19.8 cm for women. However, this difference may be justified by the fact that the researchers assessed older subjects aged on average 71.2 years [10] and subjects older than 80 years [25], i.e., older populations than the sarcopenic population investigated here. Although, AC is a valid measure [45] since these authors observed that corrected muscle area is strongly correlated with DEXA for lean mass data. In addition, the AC is the region least susceptible to changes in circumference caused by fluid retention, such as the edema that occurs in the lower limbs [10].
According to data from the present study, the BMI proved to be an acceptable anthropometric instrument for screening sarcopenia for both sexes, with good sensitivity and specificity. This agrees with another study [7] who reported similar cut-off points for BMI with our data [≤24.6 for men (sensitivity: 84.9%, specificity: 63.3%) and ≤ 26.2 for women (sensitivity: 74.6%, specificity: 85.7%)]. Besides, the BMI and advanced age are strongly associated with low musculoskeletal index (appendicular skeletal muscle mass/height) [12].
Anthropometric indicators are easily applied, representing useful measures recommended as part of a screening process since they can be easily obtained at primary health care centers [5, 15, 32, 46–48]. Thus, taking together the information from the present study with the updated recommendation from EWGSOP2 [19], it is proposed for screening sarcopenia an easy pathway to identify people with sarcopenia or its risk, and following this perspective, our data have shown that anthropometric measures could also be an additional and relevant strategy to detected sarcopenia indicators in remote areas such as the Amazon region of the country, mainly in view of the tendency to population aging in Brazil [49].
This data also indicates [49] the existence of a significant population contingent that does not reach the level of consumption of 1900 kcal per day and that is characterized by the consumption of foods with high fat, sugar and salt concentrations, poor variety, and a low consumption of fruits and vegetables. Likewise, reduction in protein intake has been related to the reduction of muscle mass, with a lean mass reduction of as much as 40% within 3 years without the ideal protein intake, which should be about 1–1.2 g/kg [50].
Moreover, it have been reported that several factors may interfere with the prevalence of older adults with sarcopenia such as age, sex, nutrition, geographical region, in addition to individual factors such as percentage of muscle mass, muscle strength and functional capacity [51]. Such factors may explain the divergence of the results obtained here both in relation to studies conducted in developed countries and studies conducted in other regions of Brazil. In Brazil, by the way, the prevalence of sarcopenia was 15.4% in São Paulo-SP [51], 10.8 to 18% among older subjects from Rio de Janeiro-RJ [52], 15.9% in from Pelotas-RS [13] and 17.8% in Lafaiete Coutinho-BA [15]. This clearly shows that divergence exists regarding the characteristics of the population among regions even within the same country.
Some limitations of the study should be considered. The use of the total muscle mass equation [22] offers an estimated calculation; however, it is a method of easy application that does not require expensive equipment and that has been validated and extensively used. Also, by being a cross-sectional study, the present investigation did not permit to infer causality relations between the variables studied. On the other hand, the study provides information about a representative sample of community-living older adults from a municipality of the Amazon region.
In Brazil, the older population increases considerably each year. The vast territory of the country poses many challenges, one of them being, among other aspects, the understanding of how the population aging is occurring in each region. It should be pointed out that a parcel of the population residing in the northern region lives in areas of difficult access for both older people and health agents, aspects that can impair the implementation of actions. Thus, it is clearly important to identify new tools of easy access and handling for the early screening of sarcopenia, especially among older adults living in the northern region of Brazil. According to the results of the present study, anthropometric measures proved to be effective for this purpose, thus permitting the development of new preventive and therapeutic strategies for this population.
Conclusion
Sarcopenic older adults had lower mean values of anthropometric measurements than non-sarcopenic subjects. An increase of one unit of these indicators may reduce the probability of the occurrence of sarcopenia among community-living older adults. All anthropometric indicators were considered to discriminate for sarcopenia with the cut-off points for BMI and AC showing a better equilibrium in the sensitivity and specificity relationship.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- AC
Arm circumference
- WC
Waist circumference
- CC
Calf circumference
- BMI
Body mass index
- OR
Odds ratio
- CI
confidence intervals
- DXA
Dual-energy X-ray emission absorptiometry
- MR
Magnetic resonance
- CT
Computed tomography
- WHO
World Health Organization
- AbC
Abdominal circumference
- MMSE
Mini Mental State Examination
- EWGSOP 2
European Working Group on Sarcopenia in Older People
- TMM
Total muscle mass
- MMI
Muscle mass index
- HGS
Handgrip strength
- BADL
Basic activities of daily life
- IADL
Instrumental activities of daily life
- IPAQ
International Physical Activity Questionnaire
- ROC
Receiver Operating Characteristic
- SPSS
Statistical Package for the Social Sciences
- AUC
Area under the ROC curve
Authors’ contributions
DGO, MSP, APM, VTKF and NCRI contributed to the conception of the project and to a critical revision and approved the version to be published; CLE contributed to the conception, design and writing of the paper; MSP contributed to data analysis and to text writing. All authors reviewed and approved the manuscript.
Funding
This research was financed by the Foundation for Research Support of the State of Amapá (FAPEAP, Concession n° 250.203.029/2016). This research agency had no influence on the design of the study, in the collection, analysis and interpretation of data, and in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study received approval from the Research Ethics Committee of the Federal University of Amapá, number 1.738.671. All participants provided their written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–2646. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 2.Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative [EWGSOP and IWGS] Age Ageing. 2014;43(6):48–759. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diz JBM, Leopoldino AAO, de Souza Moreira B, Henschke N, Dias RC, Pereira LSM, et al. Prevalence of sarcopenia in older Brazilians: A systematic review and meta-analysis. Geriatr Gerontol Int. 2017;17(1):5–16. doi: 10.1111/ggi.12720. [DOI] [PubMed] [Google Scholar]
- 4.Visvanathan R, Chapman I. Preventing sarcopaenia in older people. Maturitas. 2010;66(4):383–388. doi: 10.1016/j.maturitas.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 5.Yu S, Appleton S, Chapman I, et al. An anthropometric prediction equation for appendicular skeletal muscle mass in combination with a measure of muscle function to screen for sarcopenia in primary and aged care. J Am Med Dir Assoc. 2015;16(1):25–30. doi: 10.1016/j.jamda.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 6.Lustgarten MS, Fielding RA. Assessment of analytical methods used to measure changes in body composition in the elderly and recommendations for their use in phase II clinical trials. J Nutr Heal Aging. 2011;15(5):368–375. doi: 10.1007/s12603-011-0049-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Confortin SC, Meneghini V, Ono LM, Schneider IJC, Barbosa AR, D’Orsi E. Anthropometric indicators as a screening tool for sarcopenia in older adults from Florianópolis, Santa Catarina: EpiFloripa ageing study. Rev Nutr. 2017;30(3):287–296. doi: 10.1590/1678-98652017000300002. [DOI] [Google Scholar]
- 8.Kim S, Kim M, Lee Y, Kim BS, Yoon TY, Won CW. Calf circumference as a simple screening marker for diagnosing sarcopenia in older Korean adults: the Korean frailty and aging cohort study [KFACS] J Korean Med Sci. 2018;33(20):1–10. doi: 10.3346/jkms.2018.33.e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawakami R, Murakami H, Sanada K, et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int. 2015;15(8):969–976. doi: 10.1111/ggi.12377. [DOI] [PubMed] [Google Scholar]
- 10.Akin S, Mucuk S, Öztürk A, et al. Muscle function-dependent sarcopenia and cut-off values of possible predictors in community-dwelling Turkish elderly: calf circumference, midarm muscle circumference and walking speed. Eur J Clin Nutr. 2015;69(10):1087–1090. doi: 10.1038/ejcn.2015.42. [DOI] [PubMed] [Google Scholar]
- 11.World health organization . WHO 1995 Physical status. Use and anthropometry. 1995. [Google Scholar]
- 12.Beaudart C, McCloskey E, Bruyère O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):1–10. doi: 10.1186/s12877-016-0349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barbosa-Silva TG, Bielemann RM, Gonzalez MC, Menezes AMB. Prevalence of sarcopenia among community-dwelling elderly of a medium-sized south American city: results of the COMO VAI? Study. J Cachexia Sarcopenia Muscle. 2016;7(2):136–143. doi: 10.1002/jcsm.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pagotto VI. Ferreira dos Santos KI, Gomes Malaquias SI, et al. calf circumference: clinical validation for evaluation of muscle mass in the elderly. Rev Bras Enferm. 2018;71(2):343–350. doi: 10.1590/0034-7167-2017-0121. [DOI] [PubMed] [Google Scholar]
- 15.Pinheiro PA, da Silva Coqueiro R, Carneiro JAO, Correia TML, Pereira R, Fernandes MH. Anthropometric indicators as screening tools for sarcopenia in older adult women. Enferm Clin. 2019;S1130-8621(19):30041–30045. doi: 10.1016/j.enfcli.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Instituto Brasileiro de Geografia e Estatística, 2010. Cidades. Macapá. Available: https://cidades.ibge.gov.br/brasil/ap/macapa/pesquisa/23/25359. Accessed 02 december 2019.
- 17.Santos Filho H, Almeida MG, Ribeiro MM. Mapeamento e classificação das áreas de ressaca na região metropolitana de Macapá-AP utilizando imagens do satélite CBERS-2B. Anais XVI Simp Bras Sensoriamento Remoto - SBSR, 2013; 2211–17. Available: https://www2.unifap.br/herondino/files/2018/06/p0108.pdf. Accessed 02 december 2019.
- 18.Neri SHA. A utilização das ferramentas de geoprocessamento para identificação de comunidades expostas a hepatite a nas áreas de ressacas dos municípios de Macapá e Santana. Rio de Janeiro: Federal University of Rio de Janeiro; 2004. [Google Scholar]
- 19.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ohara DG, Pegorari MS, Oliveira dos Santos NL, et al. Respiratory muscle strength as a discriminator of sarcopenia in community-dwelling elderly: a cross-sectional study. J Nutr Heal Aging. 2018;22(8):952–958. doi: 10.1007/s12603-018-1079-4. [DOI] [PubMed] [Google Scholar]
- 21.Bertolucci PHF, Brucki SMD, Campacci SR, JuliaPno Y. O mini exame do estado mental em uma população geral: impacto da escolaridade. Arquivos de Neuropsiquiatria. 1994. 10.1590/S0004-282X1994000100001. [PubMed]
- 22.Lee RC, Wang Z, Heo M, Ross R, Janssen I, Heymsfield SB. Total-body skeletal muscle mass: development and cross-validation of anthropometric prediction models. Am J Clin Nutr. 2018;72(3):796–803. doi: 10.1093/ajcn/72.3.796. [DOI] [PubMed] [Google Scholar]
- 23.Rech CR, Dellagrana RA, Marucci MFN, et al. Validity of anthropometric equations for the estimation of muscle mass in the elderly. Rev Bras Cineantropom Desempenho Hum. 2012;14:23–31. doi: 10.5007/1980-0037.2012v14n1p23. [DOI] [Google Scholar]
- 24.Ohara DG, Pegorari MS, Oliveira dos Santos NL, et al. Cross-Sectional Study on the Association Between Pulmonary Function and Sarcopenia in Brazilian Community-Dwelling Elderly from the Amazon Region. J Nutr Heal Aging. 2019. 10.1007/s12603-019-1290-y. [DOI] [PubMed]
- 25.Delmonico MJ, Harris TB, Lee JS, et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc. 2007;55(5):769–774. doi: 10.1111/j.1532-5415.2007.01140.x. [DOI] [PubMed] [Google Scholar]
- 26.Landi F, Calvani R, Tosato M, et al. Impact of physical function impairment and multimorbidity on mortality among community-living older persons with sarcopaenia: results from the ilSIRENTE prospective cohort study. BMJ Open. 2016;6(7):1–7. doi: 10.1136/bmjopen-2015-008281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Society of Hand Therapists [ASHT]. Clinical Assessment Recommendations. Chigaco; 1992. Accessed 19 June 2018. https://www.asht.org/practice/clinical-assessment-recommendations.
- 28.Dodds RM, Syddall HE, Cooper R, Benzeval M, Deary IJ, Dennison EM, Der G, et al. Grip strength across the life course: normative data from twelve British studies. PLoS One. 2014;9(12):e113637. doi: 10.1371/journal.pone.0113637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frisancho AR. New standards of weight and body composition by frame size and height for assessment of nutritional status of adults and the elderly. Am J Clin Nutr. 1984;40(4):808–819. doi: 10.1093/ajcn/40.4.808. [DOI] [PubMed] [Google Scholar]
- 30.Zhang L, Shen Y, Zhou J, et al. Relationship between waist circumference and elevation of carotid intima-media thickness in newly-diagnosed diabetic patients. Biomed Environ Sci. 2014;27(5):335–342. doi: 10.3967/bes2014.058. [DOI] [PubMed] [Google Scholar]
- 31.Callaway CW, Chumlea WC, Bouchard C, et al. Anthropometric standardization reference manual. 1. USA: Human Kinetics Books; 1988. p. 39e55. [Google Scholar]
- 32.Tosato M, Marzetti E, Cesari M, et al. Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res. 2017;29(1):19–27. doi: 10.1007/s40520-016-0717-0. [DOI] [PubMed] [Google Scholar]
- 33.Benedetti TRB, Mazo GZ, Barros MVG. Aplicação do Questionário Internacional de Atividades Físicas para avaliação do nível de atividades físicas de 15 mulheres idosas: validade concorrente e reprodutibilidade teste-reteste. R. bras. Ci. e Mov. Brasília. 2004. doi: 10.18511/rbcm.v12i1.538.
- 34.WHO expert Consultation. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation. World Health. 2008;[December]:8–11. doi:10.1038/ejcn.2009.139.
- 35.Madden AM, Smith S. Body composition and morphological assessment of nutritional status in adults: A review of anthropometric variables. J Hum Nutr Diet. 2016;29:7–25. doi: 10.1111/jhn.12278. [DOI] [PubMed] [Google Scholar]
- 36.Lino VTS, Pereira SRM, Camacho LAB, Ribeiro Filho ST, Buksman S. Adaptação transcultural da Escala de Independência em Atividades da Vida Diária [Escala de Katz] Cad Saude Publica. 2008;24(1):103–112. doi: 10.1590/s0102-311x2008000100010. [DOI] [PubMed] [Google Scholar]
- 37.Santos RL, Júnior JSV. Confiabilidade da versão brasileira da Escala de Atividades Instrumentais da Vida Diária. Rev Bras em Prom da Saud. 2008;21(1):290–296. doi: 10.5020/18061230.2008.p290. [DOI] [Google Scholar]
- 38.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Marcel E, Salive MPH, Wallace RB. Lower-extremity function in persons over the age of 70 years as predictor of subsequent disability. N Engl J Med. 1995;332(9):556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakano MM. Versão Brasileira da Short Physical Performance Battery – SPPB: Adaptação Cultural e Estudo da Confiabilidade [Dissertation] Faculdade de Educação: Universidade Estadual de Campinas; 2007. [Google Scholar]
- 40.Saka B, Ozkaya H, Karisik E, et al. Malnutrition and sarcopenia are associated with increased mortality rate in nursing home residents: a prospective study. Eur Geriatr Med. 2016;7(3):232–238. doi: 10.1016/j.eurger.2015.12.010. [DOI] [Google Scholar]
- 41.Tsai AC, Chang T-L. The effectiveness of BMI, calf circumference and mid-arm circumference in predicting subsequent mortality risk in elderly Taiwanese. Br J Nutr. 2011;105(2):275–281. doi: 10.1017/s0007114510003429. [DOI] [PubMed] [Google Scholar]
- 42.Bastiaanse LP, Hilgenkamp TIM, Echteld MA, Evenhuis HM. Prevalence and associated factors of sarcopenia in older adults with intellectual disabilities. Res Dev Disabil. 2012;33(6):2004–2012. doi: 10.1016/j.ridd.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 43.Rolland Y, Lauwers-Cances V, Cournot M, et al. Sarcopenia, calf circumference, and physical function of elderly women: a cross-sectional study. J Am Geriatr Soc. 2003;51(8):1120–1124. doi: 10.1046/j.1532-5415.2003.51362.x. [DOI] [PubMed] [Google Scholar]
- 44.Velazquez-Alva MC, Irigoyen Camacho ME, Lazarevich I, Delgadillo Velazquez J, Acosta Dominguez P, Zepeda Zepeda MA. Comparison of the prevalence of sarcopenia using skeletal muscle mass index and calf circumference applying the European consensus definition in elderly Mexican women. Geriatr Gerontol Int. 2017;17(1):161–170. doi: 10.1111/ggi.12652. [DOI] [PubMed] [Google Scholar]
- 45.Noori N, Kopple JD, Kovesdy CP, et al. Mid-arm muscle circumference and quality of life and survival in maintenance hemodialysis patients. Clin J Am Soc Nephrol. 2010;5(12):2258–2268. doi: 10.2215/CJN.02080310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bruyère O, Beaudart C, Reginster JY, et al. Assessment of muscle mass, muscle strength and physical performance in clinical practice: an international survey. Eur Geriatr Med. 2016;7(3):243–246. doi: 10.1016/j.eurger.2015.12.009. [DOI] [Google Scholar]
- 47.Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. 2015;74(4):355–366. doi: 10.1017/s0029665115000129. [DOI] [PubMed] [Google Scholar]
- 48.Perissinotto E, Pisent C, Sergi G, Grigoletto F, Enzi G. Anthropometric measurements in the elderly: age and gender differences. Br J Nutr. 2002;87(2):177–186. doi: 10.1079/bjn2001487. [DOI] [PubMed] [Google Scholar]
- 49.Brasil, Ministério da Saúde. [2005]. Estudo de Caso Brasil: A Integração Das Ações de Alimentação e Nutrição Nos Planos de Desenvolvimento Nacional Para Alcance Das Metas Do Milênio No Contexto Do Direito Humano à Alimentação Adequada 2005, ISBN 85-334-0878-1. http://bvsms.saude.gov.br/bvs/publicacoes/estudo_caso_brasil_alimentacao_adequada.pdf.
- 50.Shaw SC, Dennison EM, Cooper C. Epidemiology of sarcopenia: determinants throughout the Lifecourse. Calcif Tissue Int. 2017;101(3):229–247. doi: 10.1007/s00223-017-0277-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alexandre TDS, Duarte YADO, Santos JLF, Wong R, Lebrão ML. Prevalence and associated factors of sarcopenia among elderly in Brazil: findings from the sabe study. J Nutr Heal Aging. 2014;18(3):284–290. doi: 10.1007/s12603-013-0413-0. [DOI] [PubMed] [Google Scholar]
- 52.Moreira VG, Perez M, Lourenço RA. Prevalence of sarcopenia and its associated factors: the impact of muscle mass, gait speed, and handgrip strength reference values on reported frequencies. Clinics. 2019. 10.6061/clinics/2019/e477. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.