With more than 53 million cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection worldwide (at the time of writing) and the recent new increase in contagion in many countries,1 the number of patients hospitalized for coronavirus disease 2019 (COVID-19)–related severe acute respiratory infection (SARI) has been exceptionally high.
Despite an extensive reorganization of hospitals2 to face this unparalleled situation in the modern history of medicine, intensive care unit (ICU) bed shortage remains a major issue, and most of these patients are cared for in the wards, with either oxygen supplementation or noninvasive supports such as continuous positive airway pressure (CPAP) with masks or helmets, high-flow nasal cannulae, or noninvasive ventilation.
Moreover, attending physicians in these wards sometimes have limited experience in acute respiratory failure and oxygen therapy/ventilatory support devices (for this reason, recently published educational papers on noninvasive respiratory support for redeployed hospital doctors and general practitioners can be found in the literature,3 and important scientific societies, such as the European Society of Intensive Care Medicine, now are offering training courses on critical care medicine for non-ICU doctors and nurses4).
In the early stages of the pandemic (or in the less-affected areas), cardiothoracic anesthesiologists/intensivists have been involved mainly in the rearrangement of cardiothoracic surgical activity and the protection of patients and healthcare workers from infection5 , 6 and in the management of cardiac complications (myocarditis, pericardial dysfunction, and other acute cardiac injuries have been reported in up to 20% to 30% of hospitalized COVID-19 patients7 , 8; moreover, severe acute respiratory syndrome coronavirus 2 infection may worsen preexisting heart diseases or lead to sepsis-related cardiomyopathy9). However, due to the significant reduction in the number of elective surgical procedures and to the pressing need for clinicians with airway management and mechanical ventilation skills, most cardiothoracic anesthesiologists/intensivists also have been directly involved in the primary care of patients with COVID-19–related SARI in the areas (or in the periods) with heavier epidemic burden.
In this context, intensivists (and redeployed anesthesiologists) are subjected to continuous requests for consultation, primarily to evaluate the need for tracheal intubation and, accordingly, for ICU admission and invasive mechanical ventilation. This is a rather challenging task. In fact, current guidelines say nothing8 , 10 or are vague, with little adherence to clinical reality, and not based on strong evidence11 about the indications for tracheal intubation in patients with COVID-19. Moreover, despite a longstanding debate (since the pandemic started) between supporters of early versus late tracheal intubation, there is no clear evidence of the superiority of one strategy over the other in outcome.12 For example, some authors recently claimed improved results with an early intubation protocol approach in patients with COVID-19,13 whereas others raised concerns about a possible patient self-inflicted lung injury in patients with severe respiratory failure left in spontaneous breathing.14 However, the criteria used for tracheal intubation in this early intubation protocol have been criticized heavily,15 and the observational design of the study did not allow proving that those patients would have had a worse outcome with a different treatment. Moreover, the considerations about patient self-inflicted lung injury, although very intriguing, are highly speculative and not supported yet by strong evidence (as opposed to the well-documented complications of invasive mechanical ventilation).16 Conversely, other (also observational) studies showed favorable outcomes with long-term noninvasive support (eg, CPAP with masks or helmets), with or without (awake) pronation.17 , 18
What should be kept in mind, finally, is that tracheal intubation and invasive mechanical ventilation expose patients to well-established (and, as mentioned, widely documented in the literature) complications, such as ventilator-associated pneumonia and ventilator-induced lung injury, in addition to those related to sedation and immobility, all possibly associated with increased mortality; accordingly, the decision to intubate a patient should be taken with extreme caution, and always when the benefits reasonably can be expected to outweigh the risks.12 , 15 , 16 All this, of course, must be contextualized in the clinical scenario described above, which comprises the ICU bed shortage on the one hand and the anxieties of the attending physicians in the wards on the other hand.
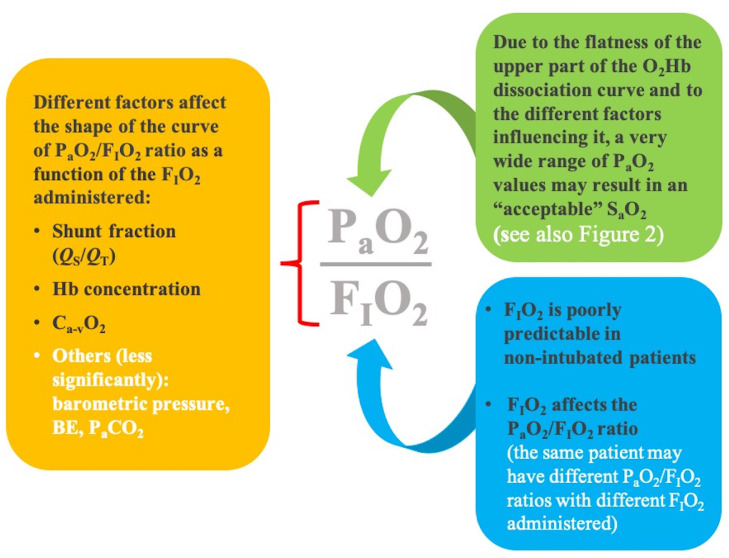
In the authors’ experience, a major concern of colleagues taking care of noninvasively supported COVID-19 patients is the low (<100 mmHg) arterial partial pressure of oxygen (PaO2)-to-oxygen inspiratory fraction (FIO2) ratio. Indeed, it seems that many clinicians today (probably since the COVID-19 pandemic started) consider hypoxemia in terms of the amount of oxygen provided to the patient.19 Of course, the PaO2/FIO2 ratio is a simple marker of the severity of respiratory failure, in particular of acute respiratory distress syndrome (ARDS), and it has been found to be an independent risk factor for 30-day mortality in a recent large observational cohort study of 10,362 COVID-19 patients (both mechanically ventilated or not) from 258 ICUs.20 However, the PaO2/FIO2 ratio is not as reliable as the alveolar-to-arterial oxygen gradient as a measure of gas exchange impairment.21 In fact, it is not independent from the FIO2 administered and it also is affected significantly by other factors unrelated to the degree of gas exchange compromise, such as hemoglobin concentration, the difference between arterial and venous oxygen content, and even (to a lesser extent) barometric pressure (see Fig 1 ).22 Moreover, the influence of these factors (including the FIO2 administered) on the PaO2/FIO2 ratio has been found to vary substantially according to the degree of intrapulmonary shunt.22 Regardless of all this, there is no evidence that using any value of the PaO2/FIO2 ratio as a trigger for tracheal intubation could affect the outcome of patients with COVID-19–related ARDS. Although, in the large cohort study mentioned above, the association between the PaO2/FIO2 ratio (during the first 24 hours after ICU admission) and 30-day mortality was a bit more pronounced in non-ventilated patients; thus, seemingly suggesting a better outcome in early mechanically ventilated patients. It was not reported if, after how long, and according to which criteria the initially non-ventilated patients subsequently were intubated.20 Most remarkably, ventilated patients with a PaO2/FIO2 ratio ≥300 mmHg had an almost doubled 30-day mortality compared to non-ventilated patients (hazard ratio = 1.89)20: this suggests that, in less-severely impacted patients, the detrimental effects of invasive mechanical ventilation prevailed over benefits, and may represent an argument against early “preventive” intubation strategies.
Fig 1.
The PaO2/FIO2 ratio has important limitations both as a marker of the severity of pulmonary gas exchange impairment and, even more, as a criterion to justify tracheal intubation in patients with COVID-19–related SARI/ARDS. COVID-19, coronavirus disease 2019; O2Hb, oxyhemoglobin; PaO2, partial pressure of oxygen; SaO2, arterial oxygen saturation; FIO2, inspiratory oxygen fraction; QS/QT, intrapulmonary shunt fraction; Ca-vO2, difference between arterial and venous oxygen content; BE, base excess; PaCO2, partial pressure of carbon dioxide
Also, the PaO2/FIO2 ratio in non-intubated patients undergoing either oxygen supplementation with devices such as nasal cannulae, Venturi masks, and reservoir bag masks or noninvasive ventilatory support with CPAP systems connected to high-flow oxygen, only can be estimated roughly: in fact, the FIO2 delivered to the patient as calculated according to the formulas reported in the literature or the charts provided by manufacturers is only theoretical (and quite reliable under physiologic conditions), but it can vary widely according to several factors such as the patient's ventilatory pattern (tidal volume, respiratory rate, respiratory pauses) or the presence of air leaks.21 , 23 , 24 Accordingly, the actual PaO2/FIO2 ratio often can be underestimated (because the FIO2 delivered is overestimated) in non-intubated patients.
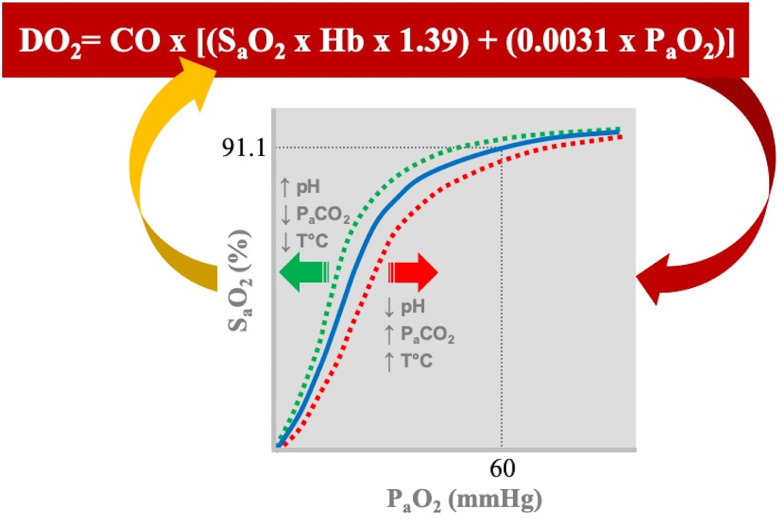
Perhaps absolute PaO2 and, even more, the resulting oxygen arterial saturation (SaO2) are much more important. Ultimately, as shown in Figure 2 , SaO2 (not PaO2) is the major respiratory determinant of oxygen delivery and, according to the well-known factors affecting the O2-hemoglobin dissociation curve, a PaO2 between 50 and 60 mmHg may correspond to an acceptable SaO2 (≥90%-92%).19, 20, 21 As an (extreme) example, a patient with a PaO2 around 60 mmHg may have an SaO2 > 91% in conditions of normothermia, but a much lower SaO2 if he or she has a high fever (see Fig 2)19; accordingly, even administering an antipyretic may prevent the patient from tracheal intubation. Clinicians also should be advised to always rely on SaO2 values measured by blood gas analysis rather than on pulse oximetry; the latter, in fact, only provides an estimation of SaO2, with well-known limitations.21 , 25 Finally, what tells us which SaO2 (or PaO2) is acceptable is also the evaluation of signs and symptoms of significant respiratory distress or tissue hypoxia (eg, respiratory rate above 25-30 per minute, use of accessory respiratory muscles, sweating, dyspnea, tachycardia, increased blood lactate levels, etc.). In the absence of severe absolute hypoxemia (usually defined as a PaO2 < 50 mmHg) and of the abovementioned signs and symptoms, and with a patient who well-tolerates the ongoing noninvasive support, does it matter how much oxygen you need to provide (even assuming to be able to calculate it accurately) to obtain such a stability, or how severe is the disease? In this regard, not even the radiologic severity of the COVID-19–related pneumonia should be considered per se as a criterion for tracheal intubation, despite the potentially misleading titles of some retrospective studies that, rather predictably, found an association between worse initial chest computed tomography findings and the risk of subsequent need for tracheal intubation, invasive mechanical ventilation, or ICU admission.26 , 27
Fig 2.
The partial pressure of oxygen (PaO2) provides a negligible direct contribution to oxygen delivery (DO2), but it affects the SaO2, a major determinant of DO2, according to the O2-hemoglobin (O2Hb) dissociation curve. The O2Hb dissociation curve, in turn, is affected by several factors such as pH, partial pressure of carbon dioxide (PaCO2), and temperature (T°C). For example, a PaO2 of 60 mmHg corresponds to a SaO2 of about 91% with a temperature of 37°C, a pH of 7.40, and a PaCO2 of 40 mmHg,19 but SaO2 would be lower (for the same PaO2) in case of acidosis or hyperthermia. Moreover, because of the flatness of the upper part of the curve, a normal or acceptable SaO2 (92%-100%) can be associated with a PaO2 ranging from 60 mmHg (or less according to the abovementioned factors) to 500 mmHg. Hb, hemoglobin; CO, cardiac output.
In summary (see also Table 1 ), indications for tracheal intubation in patients with COVID-19 should be substantially limited to (1) airway protection (alteration of consciousness); (2) severe decompensated acidosis (eg, pH < 7.2-7.25 according to widespread clinical practice); (3) severe absolute hypoxemia (PaO2 < 50 mmHg or SaO2 < 90%-92%) despite (reasonably) maximal noninvasive respiratory support; (4) signs and symptoms of significant respiratory distress or tissue hypoxia despite (reasonably) maximal noninvasive support; (5) decision to implant extracorporeal membrane oxygenation (ECMO) support; for example, venoarterial ECMO in patients with severe myocarditis and low-cardiac-output syndrome9 or venovenous (VV) ECMO in patients with severe pneumonia/ARDS.9 , 28 In fact, the Extracorporeal Life Support Organization COVID-19 interim guidelines recommend against awake cannulation.28 However, VV ECMO only should be indicated in patients with COVID-19–related SARI/ARDS who are refractory (PaO2/FIO2 ratio < 100 mmHg, arterial partial pressure of carbon dioxide above 60 mmHg, pH < 7.20) to optimal standard treatment (including lung-protective invasive mechanical ventilation, prone positioning, and neuromuscular blocking drugs); accordingly, they usually are already intubated when VV ECMO is considered.
Table 1.
Suggested Criteria for Tracheal Intubation in Patients With COVID-19–related SARI Undergoing Oxygen Therapy or Noninvasive Ventilatory Support
| Prompt tracheal intubation should be performed in the presence of one of the following conditions: | The following criteria probably do not justify by themselves tracheal intubation: |
|---|---|
| Alteration of consciousness | Low PaO2/FiO2 ratio |
| Risk of airway inhalation | Prevention of clinical worsening |
| Severe decompensated acidosis (pH < 7.2-7.25) | Severity of chest CT findings |
| Severe hypoxemia (PaO2 < 50 mmHg or SaO2 < 90%)* despite maximal noninvasive support | Logistical, organizational, or medicolegal considerations |
| Signs or symptoms of significant respiratory distress or tissue hypoxia (eg, respiratory rate above 25-30 per minute, use of accessory respiratory muscles, sweating, dyspnea, tachycardia, increased blood lactate levels, etc.) | |
| Decision to implant VA ECMO |
Abbreviations: COVID-19, coronavirus disease 2019; CT, computed tomography; FIO2, inspiratory oxygen fraction; PaO2, partial pressure of oxygen; SaO2, arterial oxygen saturation; SARI, severe acute respiratory infection; VA ECMO, venoarterial extracorporeal membrane oxygenation.
Consider tracheal intubation for SaO2 between 90% and 92%.
Ultimately, in leaving an awake and cooperative patient with COVID-19 in the ward with a CPAP mask with the maximum FIO2 allowed (which probably will be much lower than 1.0 whatever the mask instructions and charts say), a compensated blood gas analysis with a PaO2 above 50 or 60 mmHg (whatever the estimated PaO2/FIO2 ratio), normal lactate levels, and an acceptable respiratory rate, we should be convinced that this is probably the best choice at the moment, and that we are not doing so (only) because there is no ICU bed availability.
Conflict of Interest
None.
References
- 1.World Health Organization. WHO coronavirus disease (COVID-19) dashboard. Available at: https://covid19.who.int/table. Accessed November 15, 2020.
- 2.Zangrillo A, Beretta L, Silvani P, et al. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: Facing the COVID-19 pandemic emergency. Crit Care Resusc. 2020;22:91–94. doi: 10.51893/2020.2.pov1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicholson TW, Talbot NP, Nickol A, et al. Respiratory failure and non-invasive respiratory support during the covid-19 pandemic: An update for re-deployed hospital doctors and primary care physicians. BMJ. 2020;369:m2446. doi: 10.1136/bmj.m2446. [DOI] [PubMed] [Google Scholar]
- 4.European Society of Intensive Care Medicine (ESICM) Academy website. Covid-19 Skills PrepAration CoursE (C-19 SPACE) training. Available at: https://academy.esicm.org. Accessed November 15, 2020.
- 5.Pisano A, Landoni G, Zangrillo A. Protecting high-risk cardiac patients during the COVID-19 outbreak. J Cardiothorac Vasc Anesth. 2020;34:1698. doi: 10.1053/j.jvca.2020.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pisano A, Landoni G, Verniero L, Zangrillo A. Cardiothoracic surgery at the time of the coronavirus disease-2019 pandemic: Lessons from the East (and from a previous epidemic) for Western battlefields. J Cardiothorac Vasc Anesth. 2020;34:2338–2340. doi: 10.1053/j.jvca.2020.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res. 2020;126:1443–1455. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Institutes of Health. Coronavirus disease 2019 (COVID-19) treatment guidelines. Available at: https://www.covid19treatmentguidelines.nih.gov. Accessed November 16, 2020. [PubMed]
- 9.Kowalewski M, Fina D, Słomka A, et al. COVID-19 and ECMO: The interplay between coagulation and inflammation–a narrative review. Crit Care. 2020;24:205. doi: 10.1186/s13054-020-02925-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care (SIAARTI) recommendations on the management of the critically ill coronavirus disease 2019 (COVID-19) patient. Available at: http://www.siaarti.it/News/COVID19%20-%20documenti%20SIAARTI.aspx.
- 12.Cabrini L, Ghislanzoni L, Severgnini P, et al. Early versus late tracheal intubation in COVID-19 patients: A pro-con debate also considering heart-lung interactions [e-pub ahead of print] Minerva Cardioangiol. 2020 Oct 15 doi: 10.23736/S0026-4725.20.05356-6. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad I, Jeyarajah J, Nair G, et al. A prospective, observational, cohort study of airway management of patients with COVID-19 by specialist tracheal intubation teams [e-pub ahead of print] Can J Anaesth. 2020 Sep 4:1–8. doi: 10.1007/s12630-020-01804-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA. 2020;323:2329–2330. doi: 10.1001/jama.2020.6825. [DOI] [PubMed] [Google Scholar]
- 15.Tobin MJ. The criteria used to justify endotracheal intubation of patients with COVID-19 are worrisome [e-pub ahead of print] Can J Anaesth. 2020 Nov 10 doi: 10.1007/s12630-020-01853-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tobin MJ, Laghi F, Jubran A. Caution about early intubation and mechanical ventilation in COVID-19. Ann Intensive Care. 2020;10:78. doi: 10.1186/s13613-020-00692-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramirez GA, Bozzolo EP, Castelli E, et al. Continuous positive airway pressure and pronation outside the intensive care unit in COVID 19 ARDS [e-pub ahead of print] Minerva Med. 2020 Sep 30 doi: 10.23736/S0026-4806.20.06952-9. [DOI] [PubMed] [Google Scholar]
- 18.Paternoster G, Sartini C, Pennacchio E, et al. Awake pronation with helmet continuous positive airway pressure for COVID-19 acute respiratory distress syndrome patients outside the ICU: A case series [e-pub ahead of print] Med Intensiva. 2020 Sep 6 doi: 10.1016/j.medin.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tobin MJ, Laghi F, Jubran A. Why COVID-19 silent hypoxemia is baffling to physicians. Am J Respir Crit Care Med. 2020;202:356–360. doi: 10.1164/rccm.202006-2157CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferrando-Vivas P, Doidge J, Thomas K, et al. Prognostic factors for 30-day mortality in critically ill patients with coronavirus disease 2019: An observational cohort study [e-pub ahead of print] Crit Care Med. 2020 Oct 28 doi: 10.1097/CCM.0000000000004740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tobin MJ. Basing respiratory management of COVID-19 on physiological principles. Am J Respir Crit Care Med. 2020;201:1319–1320. doi: 10.1164/rccm.202004-1076ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feiner JR, Weiskopf RB. Evaluating pulmonary function: An assessment of PaO2/FIO2. Crit Care Med. 2017;45:e40–e48. doi: 10.1097/CCM.0000000000002017. [DOI] [PubMed] [Google Scholar]
- 23.Coudroy R, Frat J-P, Girault C, et al. Reliability of methods to estimate the fraction of inspired oxygen in patients with acute respiratory failure breathing through non-rebreather reservoir bag oxygen mask. Thorax. 2020;75:805–807. doi: 10.1136/thoraxjnl-2020-214863. [DOI] [PubMed] [Google Scholar]
- 24.Wagstaff TAJ, Soni N. Performance of six types of oxygen delivery devices at varying respiratory rates. Anaesthesia. 2007;62:492–503. doi: 10.1111/j.1365-2044.2007.05026.x. [DOI] [PubMed] [Google Scholar]
- 25.Pisano A. In: Physics for Anesthesiologists. Pisano A, editor. Springer; Cham, Switzerland: 2017. Light, air pollution, and pulse oximetry: The Beer-Lambert law; pp. 117–127. [Google Scholar]
- 26.Büttner L, Aigner A, Fleckenstein FN, et al. Diagnostic value of initial chest CT findings for the need of ICU treatment/intubation in patients with COVID-19. Diagnostics (Basel) 2020;10:E929. doi: 10.3390/diagnostics10110929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lanza E, Muglia R, Bolengo I, et al. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Eur Radiol. 2020;30:6770–6778. doi: 10.1007/s00330-020-07013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shekar K, Badulak J, Peek G, et al. Extracorporeal Life Support Organization Coronavirus Disease 2019 Interim Guidelines: A consensus document from an International Group of Interdisciplinary Extracorporeal Membrane Oxygenation Providers. ASAIO J. 2020;66:707–721. doi: 10.1097/MAT.0000000000001193. [DOI] [PMC free article] [PubMed] [Google Scholar]