Abstract
Corona-virus infection that arose from China is now a global pandemic. It presents with a variety of pulmonary manifestations, most commonly in the form of ground glass pulmonary lesions and opacities. Less common manifestation such as pnuemothorax has been reported by some authors. In this study we report a 56-year-old man with Corona-virus disease presenting with tension pneumothorax, a rare and life-threatening complication of Corona-virus infection that has not been reported previously. In our case, after insertion of thoracostomy tube, the patient's symptoms improved. After about 1 year of Corona-virus pandemic, it still presents with some rare pulmonary and extrapulmonary manifestations, so, familiarity with these manifestations is important for a correct diagnosis and treatment.
Key words: COVID-19, Corona virus, Tension pneumothorax, pneumomediastinum
Introduction
Corona-virus disease (COVID-19) is a recent pandemic infection, that the first case was detected in December 2019 in Wuhan, Hubei Province, China. The disease has spread rapidly since then, and many countries soon became involved in this disease, as the World Health Organization (WHO) announced on January 20, 2020 a global pandemic. To date (November 25, 2020), the number of confirmed cases have reached more than 59.2 million and the number of deaths have reached more than 1.4 million, which is still increasing [1]. Accordingly, COVID-19 has become a major health issue in most countries. Various pulmonary manifestations of COVID-19 infection have been reported. In this study, we report a case with COVID-19 infection with a pulmonary complication of tension pneumothorax.
Case report
A 56-year-old man referred to our hospital with symptoms of high-grade fever (40.2 °C), frequent nonproductive cough with weakness, mild respiratory distress, and partial anosmia from 4 days ago. The patient was admitted to the emergency department and diagnostic tests were conducted. At the admission time, the patient's vital signs were stable and peripheral capillary oxygen saturation (SpO2) was 94%. Computed tomography (CT) scan of the lungs showed bipulmonary peripheral distributed Ground Glass Opacities and consolidations, but no evidence of underlying emphysema or bullae (Fig. 1). Real time polymerase chain reaction (RT-PCR) assay test from the patient's pharyngeal swabs sample was also positive. The patient was diagnosed with COVID-19 infection and was treated with Azithromycin, Lopinavir/Ritonavir (KALETRA), low-dose dexamethasone, and nasal cannula supplemental oxygen at a rate of 5 liters per minute. He was not intubated during the hospitalization period. In laboratory data, the patient's white blood cells count was 8400/mm3 with 74% neutrophils and 14% lymphocytes. The estimated sedimentation rate was 46. The patient was hospitalized for 5 days and was discharged with good general condition and improvement of symptoms.
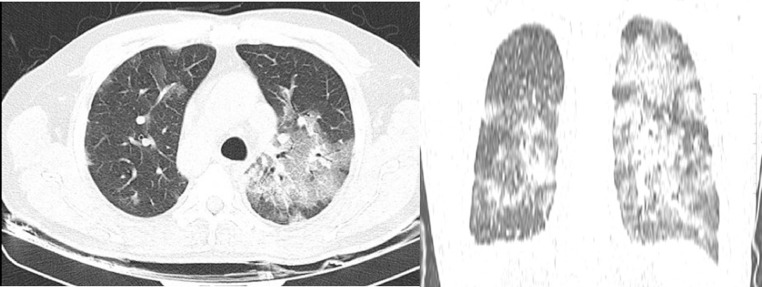
Fig. 1.
Lung CT scan at first admission demonstrates ground glass opacities (GGO) and consolidations in left pulmonary parenchyma
Eleven days later, the patient returned to emergency department with complaint of sudden respiratory distress, tachypnea, shortness of breathing, and chest pain from preceding 5 hours. During the period of discharging from the hospital to his readmission, his general condition was good, he did not have respiratory distress and only mentioned cough. At the time of readmission, the patient obviously had respiratory distress and was using his accessory muscles of respiration. His respiratory rate was 42 beats per minute (bpm) with 110 bpm of pulse rate and blood pressure of 105/70 mm Hg. In auscultation, he had a decreased pulmonary sound on the left lung and had hyper-resonancy in percussion. The peripheral oxygen saturation (SpO2) was 82%. A chest CT scan was performed and tension pneumothorax on the left side was specified, which caused shifting the heart and trachea to the right mediastinum (Fig. 2). A thoracostomy tube was inserted in the left hemithorax emergently. After insertion of the chest tube, the patient's symptoms improved clearly, respiratory distress decreased, and in about an hour later, respiratory rate was 26 bpm, heart rate was 90 bmp, patient's blood pressure was 115/80 mm Hg, and his SpO2 was 96%. The patient was treated with nasal cannula supplemental oxygen at a rate of 4-5 liters per minute. The chest bottle was connected to low suction for 48 hours at a pressure of −20 mmH2O.
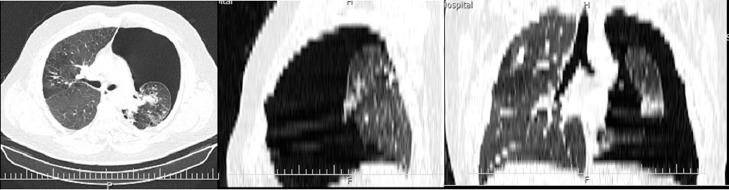
Fig. 2.
CT scan at second admission (11 days after discharge) shows tension pneumothorax in left hemithorax that causes cardiac and mediastinal shifting.
After complete lung expansion on control chest X-ray and CT scan (Fig. 3), after 4 days of hospitalization, the patient's chest tube was removed and the patient was discharged home with good conditions.
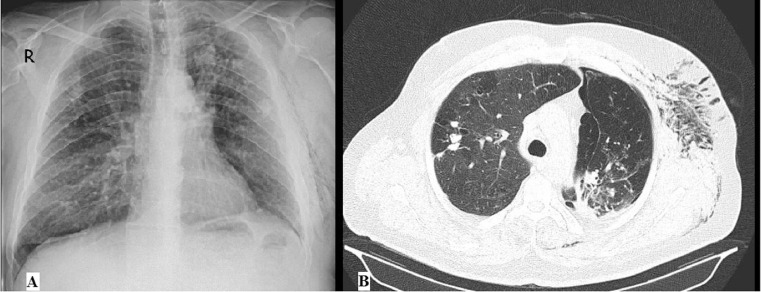
Fig. 3.
(A) Chest radiograph and (B) chest CT scan after chest tube insertion demonstrate resolution of pneumothorax and complete expansion of the left lung.
Discussion
Chest CT scan is considered to be a suitable and important screening tool for diagnosis of COVID-19 due to its relatively high sensitivity and availability, especially when PCR testing is not available or its access is limited [2]. Some articles reported pneumothorax in patients with COVID-19. Sun et al introduced a patient with COVID-19 who had large bullae that possibly rupture of the bullae caused pneumothorax and pneumomediastinum in that patient [3]. Lei et al in China also reported a case of mild pneumomediastinum in a COVID-19 patient [4]. In other studies, the prevalence of pneumothorax in patients with COVID-19 infection was reported to be about 1% and 2% [5]. But tension pneumothorax in patients with COVID-19 disease has been reported in only 2 previous studies. First, Flower et al reported a 36-year-old man in London with COVID-19 disease with left tension pneumothorax [6]. Second study, Spiro et al in Germany described a 47-year-old man with COVID-19 infection with right-sided tension pneumothorax [2]. Pneumothorax is a well-known complication in patients with ARDS, which the main cause is alveolar rupture due to increased alveolar pressure and volume [7]. Histological examinations of lung biopsy specimens in patients with COVID-19 infection show alveolar swelling and exudate accumulation within it and inflammation of the alveolar membrane, leading to pneumocyte destruction and eventual ARDS [8]. In our case, the patient had no previous history of lung disease but was smoker. He had not undergone invasive mechanical ventilation during hospitalization as a cause for increased alveolar pressure, but had frequent nonproductive coughs over the past 3 weeks since the onset of the disease; possibly increasing the pressure of inflamed and brittle alveoli membrane that caused small emphysema and bullae started to develop, and eventually led to tension pneumothorax.
In conclusion, COVID-19 infection may present with a variety of pulmonary manifestations, most commonly in the form of GGO pulmonary lesions and opacities, which may be superinfected by bacterial infections. But other manifestations such as pneumothorax, pneumomediastinum, and rare and more life-threatening than all, tension pneumothorax, may also be seen in the disease. After about 1 year of COVID-19 pandemic, it still presents with rare pulmonary and extrapulmonary manifestations. Such rare manifestations may present as first symptoms or like in this case, may present with delay as secondary symptoms and familiarity with these manifestations is important for a correct diagnosis and treatment.
Acknowledgment
We thank the patient for his cooperation.
Footnotes
Funding: None.
Conflict of interest: The authors declare no conflict of interest.
References
- 1.World Health Organization. Coronavirus Disease (COVID-19) Dashboard. Available at: Https://covid19.who.int.
- 2.Spiro JE, Sisovic S, Ockert B, Böcker W, Siebenbürger G. Secondary tension pneumothorax in a COVID-19 pneumonia patient: a case report. Infection. 2020:1–4. doi: 10.1007/s15010-020-01457-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun R, Liu H, Wang X. Mediastinal emphysema, giant bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020 doi: 10.3348/kjr.2020.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lei P, Mao J, Wang P. Spontaneous Pneumomediastinum in a Patient with Coronavirus Disease 2019 Pneumonia and the Possible Underlying Mechanism. Korean J Radiol. 2020:21. doi: 10.3348/kjr.2020.0426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020 doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 6.Flower L, Carter JL, Rosales Lopez J, Henry AM. Tension pneumothorax in a patient with COVID-19. BMJ Case Rep. 2020 doi: 10.1136/bcr-2020-235861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woodside KJ, vanSonnenberg E, Chon KS, Loran DB, Tocino IM, Zwischenberger JB. Pneumothorax in patients with acute respiratory distress syndrome: pathophysiology, detection, and treatment. J Intensive Care Med. 2003;18:9–20. doi: 10.1177/0885066602239120. [DOI] [PubMed] [Google Scholar]
- 8.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30076-X. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]