Abstract
Introduction
This article evaluates and reports on satisfaction of adult patients across the United States who received orthodontic treatment for anterior openbite malocclusion. The factors that influence satisfaction are also described.
Methods
Practitioners were recruited from the National Dental Practice-Based Research Network. Upon joining the Network, practitioner demographics and information on their practices were acquired. Practitioners enrolled their adult patients in active treatment for anterior openbite. Patient demographics, patient dentofacial characteristics, and details regarding previous and current treatment were collected through questionnaires at enrollment (T1). Pretreatment lateral cephalograms and intraoral frontal photographs were submitted. Treatment performed and details related to treatment outcome were recorded through questionnaires at the end of active treatment (T2). Post-treatment lateral cephalograms and intraoral frontal photographs were submitted. Patient satisfaction at the end of active treatment (T2) was assessed using a five-point, Likert-like scale and open-ended responses. Predictive univariate models were developed to evaluate the factors that influence patient satisfaction. Open-ended responses were reviewed for general trends.
Results
End of active treatment (T2) data were received for 260 patients, and 248 of these patients completed and returned the patient satisfaction questionnaires. High levels of satisfaction were found in this sample of adult patients receiving treatment for anterior openbite malocclusion. Specifically, 96% of the sample reported being very or somewhat satisfied. Only 10 patients (4%) were not satisfied with the treatment provided or an element of the final result. Successful openbite closure, treatment modality, and certain patient characteristics may influence patient satisfaction. However, there was insufficient power to demonstrate statistical significance, due to the very low number of dissatisfied patients. Open-ended responses directly associated with patient satisfaction were received from 23 patients (9%). They relayed positive, neutral, and negative feelings about the treatment received and final results. Additional responses regarding the orthodontic treatment in general, but not specifically linked to patient satisfaction, were received from 119 patients (48%). These comments depict an overwhelmingly positive experience.
Conclusions
Adult patients who received orthodontic treatment for anterior openbite malocclusion were generally satisfied with the treatment provided, as well as the final esthetic and functional results.
Introduction
Anterior openbite (AOB) was first described in the dental literature more than 150 years ago.1 It can be defined as a lack of vertical contact and overlap of the anterior teeth in maximum intercuspation.2–4 The prevalence of AOB in the United States ranges from 0.6% to 16.5%, depending on age and race.5 The etiology of AOB is complex and multifactorial. Oral habits, unfavorable growth patterns, respiratory factors, and neuromuscular imbalance have been suggested to play a role.6 AOB often results in significant esthetic and functional concerns, including difficulty incising food and speaking.3,7,8
AOB is widely considered to be one of the most challenging malocclusions to treat. Although numerous strategies have been proposed to treat AOB cases, there is no consensus as to which is the preferred treatment modality for a particular case. Current evidence on the success of AOB treatment is based primarily on retrospective case series.9 This literature only evaluates clinical outcomes. Patient satisfaction associated with treatment of AOB malocclusion has not been evaluated.
Over the past few decades, the healthcare literature has placed an increased emphasis on quality of life.10 Improvement in quality of life is a fundamental goal of medicine and dentistry.11 Orthodontic treatment, specifically, aims to enhance oral health-related quality of life through the correction of malocclusion,12,13 as well as improvement of dentofacial esthetics and oral function. Therefore, it is important for the orthodontic literature to evaluate patient-centered outcomes. Traditional orthodontic outcome measures do not necessarily reflect patient values and, until recently, patient perspectives have received limited attention in the orthodontic literature.10,14,15 In this report, we investigate satisfaction levels of adult patients after receiving orthodontic treatment for AOB malocclusion. We also describe the factors that are associated with satisfaction and dissatisfaction.
In 2015, the National Dental Practice-Based Research Network (PBRN) Adult Anterior Openbite Study was launched. The purpose of this large observational prospective cohort study was to explore treatment recommendations, outcomes, stability, and satisfaction of adult AOB patients. The study was divided into three phases: enrollment (T1), end of active treatment (T2), and 1-year post-treatment (T3). A prior publication characterizes the practitioners and patients enrolled in the study.16 Another previous publication details the factors that influence treatment recommendations.17 This paper describes patient satisfaction at the end of active treatment (T2). A concomitant publication addresses treatment success at the end of active treatment (T2).18 A subsequent publication will describe treatment success and patient satisfaction at 1-year post treatment (T3).
Materials and Methods
Providers were recruited from the National Dental PBRN, comprises six geographic regions: West, Midwest, Southwest, South Central, South Atlantic, and Northeast. Institutional Review Board approval for this study was obtained from several institutions, representing the regions of the Network. These included the University of Alabama at Birmingham Institutional Review Board acting as the central Institutional Review Board, the Kaiser Permanente Northwest Institutional Review Board for the Western region, and the University of Rochester Research Subjects Review Board for the Northeast region. Additionally, Institutional Review Board approval was obtained at individual academic settings when required.
Inclusion criteria for practitioners
Orthodontist or dentist that routinely performs orthodontic treatment.
Estimates to recruit three to eight adult patients in active treatment for AOB and expects to complete treatment within 24 months of enrollment into the study.
Routinely takes cephalometric radiographs before and after treatment.
Able to upload de-identified cephalometric radiographs and digital intraoral frontal photographs to a central data repository.
Affirms that the practice can devote sufficient time in patient scheduling to allow recording of the required data.
Does not anticipate retiring, selling the practice, or moving during the study.
Inclusion criteria for patients
At least 18 years of age at the time of enrollment.
Must have AOB, which is defined as one or more incisors that do not have vertical overlap with teeth in the opposing arch. The remaining incisors may have minimal incisor overlap, but cannot contact teeth in the opposing arch. This will be determined by examining the patient’s initial cephalometric radiograph, intraoral photographs, and/or initial plaster or digital casts.
Must be in active treatment for AOB and expects to have treatment completed within 24 months of enrollment in the study.
Must have an initial cephalometric radiograph (taken prior to the beginning of treatment). A cephalometric radiograph created from a cone-beam CT scan is acceptable.
Exclusion criteria for patients
Clefts, craniofacial conditions or syndromes.
Significant physical, mental, or medical conditions that would affect treatment compliance, cooperation, or outcome.
Expects to move before the completion of the study.
Initial treatment plans estimated to be more than 36 months.
Recruitment was restricted to patients eighteen years of age or older to minimize, though not completely eliminate, the influence of facial growth on treatment outcome. To avoid selection bias, practitioners were requested to enroll all eligible patients. A maximum of 15 patients per practitioner was established. If a practitioner had more than 15 eligible patients, patients were selected sequentially based upon their treatment start dates.
Upon joining the Network, practitioner demographics and information on their practices were acquired. Patient demographics, patient dentofacial characteristics, and details regarding previous and current treatment were collected through questionnaires at enrollment (T1). Changes to treatment (i.e., added or removed procedures) and details related to treatment outcome were recorded through questionnaires at the end of active treatment (T2). Patient satisfaction was assessed using a five-point, Likert-like scale and open-ended responses at the end of active treatment (T2). Patients placed completed satisfaction evaluations in sealed envelopes. Questionnaires were sent to regional centers, where they were reviewed for completeness and entered into a centralized database. More details on data collection from practitioners and patients can be found in a previously published paper.16 Study forms can be accessed at http://nationaldentalpbrn.org/anterior-openbite-malocclusions-in-adults-recommendations-treatment-and-stability.php. Intraoral frontal photographs were taken parallel to the occlusal plane. Practitioners were provided with sample photographs, demonstrating correct and incorrect vertical orientation.
Pre- and post-treatment lateral cephalograms and intraoral frontal photographs were uploaded to a centralized, Web-based system. De-identified images were forwarded to the research team at the University of Washington. The radiographs were imported into Dolphin imaging software (version 11.0; Dolphin Imaging and Management Solutions, Chatsworth, CA), landmarks were identified by two examiners, and an automated, custom cephalometric analysis was performed based on the selected landmarks. A depiction of the cephalometric landmarks can be found in a previously published article.16 Cephalometric landmarks were first identified by one examiner and then reviewed by the other examiner. Disagreements in landmark identification were resolved by means of consensus between the examiners.
A standard millimetric ruler in the lateral cephalogram was used to calibrate millimetric measurements. If a ruler was present in a patient’s pre-treatment lateral cephalogram, but absent in the post-treatment lateral cephalogram, the sella-nasion distance of the pretreatment lateral cephalogram, measured using the ruler, was used to calibrate the posttreatment lateral cephalogram. The same process was followed, in reverse, if a ruler was present in a patient’s post-treatment lateral cephalogram, but absent in the pre-treatment lateral cephalogram. If a ruler was absent on both a patient’s pre- and post-treatment lateral cephalograms, an average nasion-menton distance was used to calibrate the pretreatment lateral cephalogram.19,20 The post-treatment lateral cephalogram was then calibrated using the sella-nasion distance of the pre-treatment lateral cephalogram, as described above. This surrogate calibration method was validated by sensitivity analysis.
An index was developed to score the relative openbite severity using the intraoral frontal photographs. The Photographic Openbite Severity Index (POSI) has seven categories, defined by the type and number of teeth that do not have vertical overlap (Figure 1):
All four incisors with vertical overlap
One or two maxillary lateral incisors without vertical overlap (both maxillary central incisors have vertical overlap)
One maxillary central incisor without vertical overlap (the other maxillary central incisor has vertical overlap)
Both maxillary central incisors without vertical overlap (at least one maxillary lateral incisor has vertical overlap)
All four maxillary incisors without vertical overlap
All anterior teeth, including canines, without vertical overlap
All anterior teeth, plus at least one premolar, without vertical overlap
Figure 1.
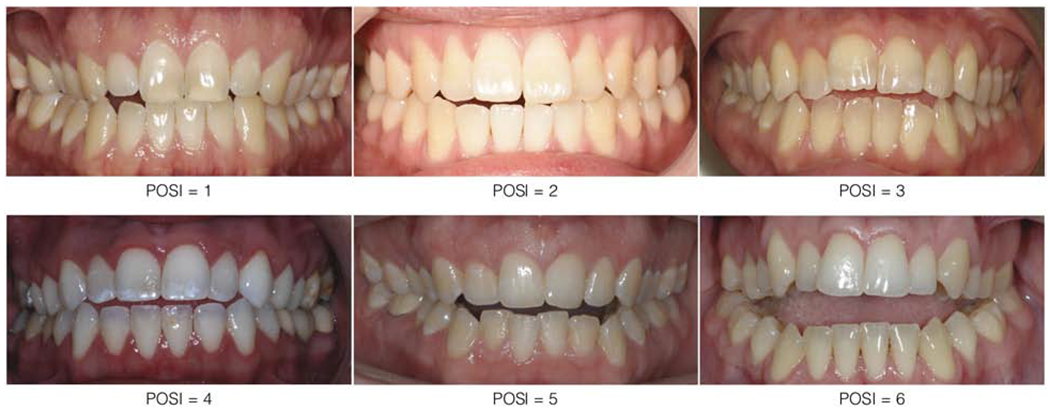
Photographic Openbite Severity Index (POSI), developed to score the relative openbite severity using the intraoral frontal photographs
The intraoral frontal photographs were rated, independently, by the same two examiners. Disagreements in POSI scores were resolved by means of consensus between the examiners.
Both examiners underwent training and calibration prior to landmarking lateral cephalograms and assessing intraoral frontal photographs. Ten lateral cephalograms and twenty intraoral frontal photographs were randomly selected to determine inter- and intra-rater reliability. The lateral cephalograms and intraoral frontal photographs were analyzed twice, one month apart, by both examiners. Inter- and intra-examiner reliability was assessed with an intraclass correlation coefficient. All values were greater than 0.90, indicating that landmark identification and POSI classification were reliable by each examiner over time, as well as between examiners.
Data Analysis
Patient satisfaction at the end of active treatment (T2) was assessed using a five-point, Likert-like scale: very satisfied, somewhat satisfied, neither satisfied nor dissatisfied, somewhat dissatisfied, very dissatisfied. Patients were asked to provide explanations following answers of somewhat or very dissatisfied. Satisfaction with the orthodontic treatment provided, satisfaction with esthetics, and satisfaction with function were evaluated separately. Whether or not treatment would be recommended to a friend with a similar malocclusion was also evaluated using a five-point, Likert-like scale: definitely recommend, probably recommend, undecided, probably not recommend, definitely not recommend. Patients were asked to provide explanations following answers of probably or definitely not recommend.
Satisfaction rates were calculated by grouping responses: Satisfied (very satisfied and somewhat satisfied) vs. Not Satisfied (neither satisfied nor dissatisfied, somewhat dissatisfied, and very dissatisfied). Whether or not treatment would be recommended to a friend can be consider a proxy for patient satisfaction with the orthodontic treatment provided. The likelihood of this recommendation was also quantified by grouping responses: Would Recommend (definitely recommend and probably recommend) vs. Would Not Recommend (undecided, probably not recommend, and definitely not recommend). Open-ended responses were reviewed for general trends.
Treatment Success
Several measures were used to evaluate treatment success. Patient-Perceived Treatment Success was determined at the end of active treatment (T2) by asking patients if their ir openbite was successfully closed. Practitioner-Reported Treatment Success was determined at the end of active treatment (T2) by asking practitioners if the openbite was successfully closed. Lateral cephalometric radiographs were used to evaluate treatment success, defined by positive overbite at the end of active treatment (T2). Specifically, posttreatment lateral cephalograms were analyzed to determine if positive incisor overlap was achieved. Finally, the POSI was used to evaluate treatment success (defined as a score of 0 at the end of active treatment [T2]).
Success can be defined by the 4 measures, described above. Patient-perceived and practitioner-reported treatment successes are subjective in nature. Treatment success defined by the cephalometric analysis only uses the most anterior maxillary and mandibular central incisors to calculate overbite, and therefore may not account for the vertical overlap of the other incisors. Alternately, the POSI scores the vertical overlap of all four incisors in maximum intercuspation. Preliminary analyses indicated that the POSI is the most discriminating measure to assess successful openbite closure (Appendix, Table 1).
Treatment Factors
Four treatment modalities were recognized:
ALN: aligners without fixed appliances or temporary anchorage devices (TADs) or orthognathic surgery
FA: fixed appliances without TADs or orthognathic surgery
TADs: TADs without orthognathic surgery
SX: orthognathic surgery
These categories represent an increasing ability to manage more complex malocclusions, as well as an increasing level of invasiveness. Patients treated with a combination of appliances were placed in the higher treatment category. For example, a patient treated with aligners and fixed appliances would be placed in treatment category #2. The effect of extractions on patient satisfaction was also explored.
Treatment duration was calculated as the time from appliance placement to appliance removal, based on information from the enrollment (T1) and end of active treatment (T2) questionnaires, respectively.
Patient Characteristics
Information about the age, gender, race, insurance coverage, education level, previous orthodontic treatment of the subjects was collected.
Practitioner Characteristics
Information about the age, gender, race, years in practice, geographic region of practice, and practice type of the practitioners was collected.
Univariate analyses of continuous variables (means, standard deviations [sd], and ranges) are presented. Bivariate analyses were used to evaluate the influence of the aforementioned predictors on patient satisfaction. Statistical significance was adjusted for clustering of patients within practitioners using generalized estimating equations. Statistics were processed using PROC GENMOD in SAS with CORR=EXCH option. However, due to the very small number of dissatisfied patients, most comparisons were not estimable statistically. Thus, with few exceptions, only descriptive frequencies of the bivariate analyses related to satisfaction are described.
Results
From October 2015 to June 2016, 91 practitioners were recruited for the study. The practitioners enrolled 358, patients of whom 347 met the inclusion criteria.
End of active treatment (T2) data were received for 260 patients, treated by 84 different practitioners. Twenty-four patients withdrew from the study. The remaining 63 patients did not finish treatment within the study period. End of active treatment (T2) questionnaires were collected for 254 patients, of which 248 included patient satisfaction data. Post-treatment intraoral frontal photographs were received for 234 patients. Post-treatment lateral cephalograms were available for 231 patients. No differences were found between practitioner demographics at enrollment (T1) and those at end of active treatment (T2). Patients who completed treatment within the study period were older (p = 0.04) and more educated (p = 0.04) than those who did not. The pre-treatment openbite severity was similar for patients who completed treatment within the study period and those who did not.
The patients had a mean age of 31.2 years (SD = 11.9 years; range = 18-71 years). Seventy-five percent of the patients were female. Just over 40% of the patients had a previous history of orthodontic treatment. The practitioners had a mean age of 48.8 years (SD = 9.8 years; range = 31-66 years). Seventy-three percent of the practitioners were male. Of the practitioners, 82 were orthodontists and 2 were general dentists. Patient and practitioner demographics are presented in Tables 1 and 2. Detailed demographics, describing the patients and practitioners at enrollment (T1), can be found in a previously published paper.16
Table 1.
Patient demographics
| N | % | |
|---|---|---|
| Sex (N = 253) | ||
| Male | 64 | 25% |
| Female | 189 | 75% |
| Age, years (N = 253) | ||
| 18 - 20 | 43 | 17% |
| 21 - 30 | 106 | 42% |
| 31 - 40 | 58 | 23% |
| ≥ 41 | 46 | 18% |
| Race and Ethnicity (N = 253) | ||
| White/Caucasian | 146 | 58% |
| Black/African-American | 23 | 9% |
| Asian | 24 | 9% |
| Multirace | 8 | 3% |
| Hispanic | 52 | 21% |
| Previous Orthodontic Treatment (N = 253) | ||
| Yes | 106 | 42% |
| No | 147 | 58% |
| Insurance Coverage | ||
| None | 54 | 21% |
| Yes - does not cover ortho or Og Sx | 64 | 25% |
| Yes - covers ortho, but not Og Sx | 74 | 29% |
| Yes - covers Og Sx | 62 | 24% |
| Education Level (N = 253) | ||
| High school graduate or less | 45 | 18% |
| Some college or associate degree | 79 | 31% |
| Bachelor degree | 84 | 33% |
| Graduate degree | 45 | 18% |
N = 254, unless indicated otherwise
Table 2.
Practitioner demographics
| N | % | |
|---|---|---|
| Status | ||
| Orthodontist | 82 | 98% |
| General practitioner | 2 | 2% |
| Sex | ||
| Male | 61 | 73% |
| Female | 23 | 27% |
| Age, years | ||
| < 45 | 32 | 38% |
| 45 - 54 | 24 | 29% |
| 55 - 64 | 23 | 27% |
| ≥ 65 | 5 | 6% |
| Race and Ethnicity (N = 83) | ||
| White/Caucasian | 52 | 63% |
| Asian | 19 | 23% |
| Multirace | 2 | 2% |
| Hispanic | 10 | 12% |
| Network Region | ||
| West | 34 | 41% |
| Midwest | 8 | 10% |
| Southwest | 16 | 19% |
| South Central | 6 | 7% |
| South Atlantic | 9 | 11% |
| Northeast | 11 | 13% |
N = 84, unless indicated otherwise
The mean pre-treatment overbite, measured using the lateral cephalograms, was −2.3 mm (SD = 2.1 mm). All four incisors exhibited no vertical overlap (POSI ≥ 4) in nearly two-thirds of the sample. Thus, most patients had significant AOBs prior to treatment.
Twenty-nine patients were treated only with clear aligners. One hundred fifty-two patients were treated with fixed appliances without TADs or orthognathic surgery. Twenty patients were treated with TADs without orthognathic surgery. Fifty-three patients were treated with orthognathic surgery. Extractions were performed in 49 patients. Treatment spanned an average of 24.8 months (SD = 11.3 months; range = 1-72 months). At the end of active treatment (T2), 84% of patients fell into POSI category 0, indicating that the openbite was successfully closed. The mean post-treatment overbite was 1.3 mm (SD = 1.1 mm). Additional details on treatment success can be found in a concomitant publication.18
High satisfaction levels were observed at the end of active treatment (T2). Specifically, two hundred thirty-eight patients (96%) reported being satisfied with the orthodontic treatment provided as well as the final esthetic and functional results. Only ten patients (4%) were not satisfied with treatment or an element of the final result (Table 3). Four of these patients were not satisfied with multiple aspects of treatment. Nearly 98% of patients would recommend treatment to a friend with a similar malocclusion (Table 3). Likert-like scale responses to satisfaction with the treatment provided, esthetics, and function are detailed, separately, in the following section (Appendix, Table 2).
Table 3.
Patient satisfaction and recommendation of treatment to a friend
| N | % | |
|---|---|---|
| Satisfied (N=245) | ||
| On all | 235 | 96% |
| Not on all | 10 | 4% |
| Recommend Treatment (N=246) | ||
| Would | 240 | 98% |
| Would not | 6 | 2 |
Only one patient reported being dissatisfied with the orthodontic treatment provided. Two patients did not provide a response. Only one patient indicated being dissatisfied with the final esthetic result. Five patients were neither satisfied nor dissatisfied with their ability to chew at the end of treatment. Two patients were dissatisfied with their ability to chew. Six patients were neither satisfied nor dissatisfied with their speech after treatment was completed. Two patients did not specify a response for each question related to function.
Due to the small number of dissatisfied patients, there was insufficient statistical power to investigate factors associated with patient satisfaction. Several trends were observed. First, patients who did not have a successful result were more likely to be dissatisfied (Table 4). The strength of this relationship varied with the measure of treatment success. Patients treated with clear aligners only or orthognathic surgery reported higher levels of dissatisfaction than those treated with other modalities (Table 5). Female patients were more than twice as likely to be dissatisfied with the orthodontic treatment provided or an element of the final results (Table 6). Patients with a higher level of education were more likely to be dissatisfied (Table 6). No trends were observed between patient satisfaction and practitioner characteristics. Compared to satisfied patients, dissatisfied patients were much less likely to recommend the treatment that they received to a friend with a similar malocclusion (Table 4). The 80% difference almost reached statistical significance.
Table 4.
Recommend treatment and treatment success according to whether NOT satisfied on some aspect of treatment and/or result
| ALL | Not satisfied | |||
|---|---|---|---|---|
| N=248 | N=10 | Row1 % | p2 | |
| Recommend Treatment | 0.056 | |||
| Would | 240 | 5 | 3% | |
| Would not | 6 | 5 | 83% | |
| Patient: OB Closed | 0.2 | |||
| Yes | 236 | 8 | 3% | |
| No | 11 | 2 | 18% | |
| Dentist: OB Closed | 0.4 | |||
| Yes | 228 | 8 | 4% | |
| No | 20 | 2 | 10% | |
| OB > 0mm | 0.4 | |||
| Yes | 211 | 7 | 3% | |
| No | 16 | 1 | 6% | |
| POSI = 0 | 0.4 | |||
| Yes | 190 | 5 | 3% | |
| No | 38 | 2 | 5% | |
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
Table 5.
Treatment performed according to whether NOT satisfied on some aspect of treatment and/or result
| ALL | Not satisfied | |||
|---|---|---|---|---|
| N=248 | N=10 | Row1 % | p2,3 | |
| Primary Treatment Rendered | NE | |||
| Aligners only | 29 | 2 | 7% | |
| Fixed appliances, no TADs or surger | 148 | 4 | 3% | |
| TADs, no surgery | 20 | 0 | 0% | |
| Surgery | 51 | 4 | 8% | |
| Surgery | NE | |||
| No | 197 | 6 | 3% | |
| Yes | 51 | 4 | 8% | |
| Extractions | NE | |||
| No | 202 | 10 | 5% | |
| Yes | 46 | 0 | 0% | |
| Treatment Duration, months | NE | |||
| < 17 | 56 | 3 | 5% | |
| 17 - 22 | 55 | 1 | 2% | |
| 23 - 29 | 72 | 2 | 3% | |
| ≥ 30 | 61 | 4 | 7% | |
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
NE: Not estimable
Table 6.
Patient demographic characteristics according to whether NOT satisfied on some aspect of treatment and/or result
| ALL | Not satisfied | |||
|---|---|---|---|---|
| N=248 | N=10 | Row1 % | p2,3 | |
| Sex | NE | |||
| Male | 63 | 1 | 2% | |
| Female | 184 | 9 | 5% | |
| Age, years | NE | |||
| 18 - 20 | 39 | 1 | 3% | |
| 21 - 30 | 105 | 5 | 5% | |
| 31 - 40 | 57 | 3 | 5% | |
| ≥ 41 | 46 | 1 | 2% | |
| Race and Ethnicity | NE | |||
| White/Caucasian | 143 | 7 | 5% | |
| Black/African-American | 21 | 0 | 0% | |
| Asian | 24 | 1 | 4% | |
| Multirace | 8 | 1 | 12% | |
| Hispanic | 51 | 1 | 2% | |
| Insurance Coverage | NE | |||
| None | 54 | 2 | 4% | |
| Yes - does not cover ortho or Og Sx | 63 | 5 | 8% | |
| Yes - covers ortho, but not Og Sx | 72 | 1 | 1% | |
| Yes - covers Og Sx | 59 | 2 | 3% | |
| Education Level | NE | |||
| High school graduate or less | 40 | 1 | 2% | |
| Some college or associate degree | 79 | 1 | 1% | |
| Bachelor degree | 84 | 4 | 5% | |
| Graduate degree | 44 | 4 | 9% | |
| Prior Orthodontic Treatment | NE | |||
| No | 144 | 5 | 3% | |
| Yes | 103 | 4 | 4% | |
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
NE: Not estimable
Open-ended responses were received from 2sources. Open-ended responses directly associated with patient satisfaction followed answers of somewhat or very dissatisfied on the Likert-like scale. Additional open-ended responses regarding the orthodontic treatment in general, but not specifically linked to patient satisfaction, were solicited separately. All open-ended responses were classified as positive, neutral, or negative. Neutral comments either indicate improvement with some minor reservations about the final result or do not provide any meaningful information.
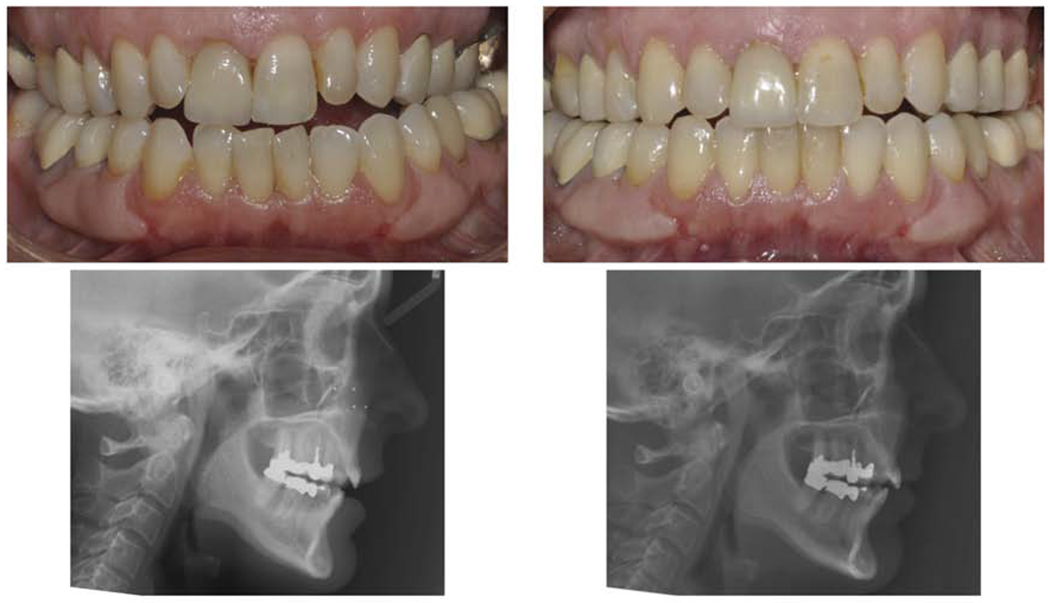
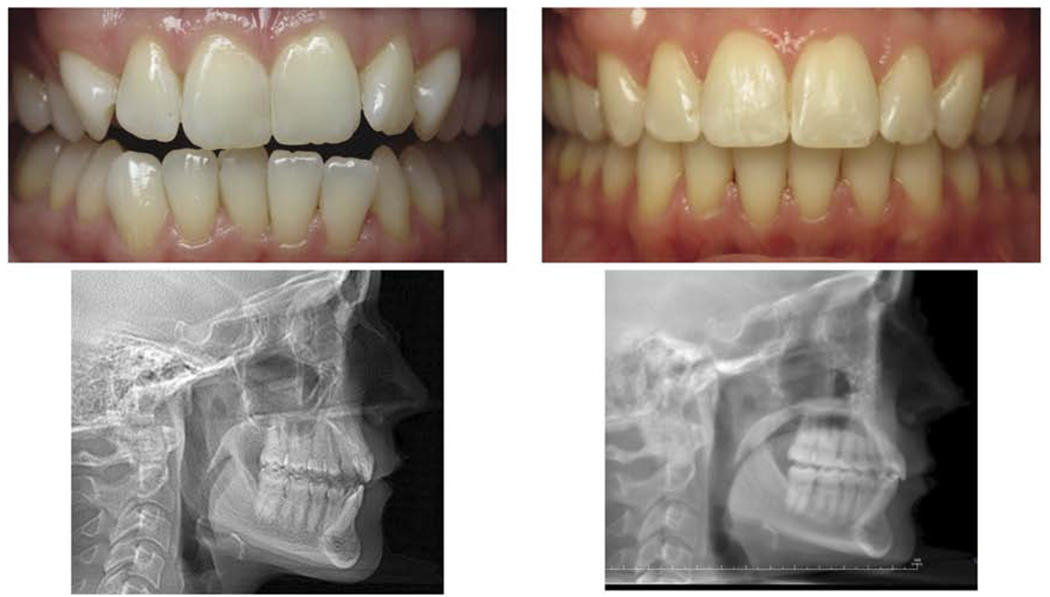
Open-ended responses directly associated with patient satisfaction were received from twenty-three patients (9%). Only two of these patients were among the ten who indicated that they were not satisfied with the orthodontic treatment provided or an element of the final result. Both these patients also would not recommend the treatment that they received to a friend with a similar malocclusion. Available records, treatment details, and satisfaction results for these two patients are presented in Figures 2 and 3. The remaining twenty-one patients reported high levels of satisfaction. There were nearly equal numbers of positive, neutral, or negative responses from the twenty-one satisfied patients. The two dissatisfied patients primarily entered negative comments, but also expressed some positivity. A representative sample of these open-ended responses is found in Table 7.
Figure 2.

Pre-treatment records for a patient in the study. Neither a post-treatment lateral cephalogram nor intraoral frontal photograph was received. The patient was treated with clear aligners, only. No other treatment modalities were recommended. At the end of active treatment (T2), the patient indicated that he or she was somewhat dissatisfied with the final esthetic result and very dissatisfied with his or her ability to chew. The patient would not recommend the treatment that he or she received to a friend with a similar malocclusion. Open-ended responses describe a residual openbite and difficulty incising food. Despite this result, the patient was “extremely satisfied with (the) office staff’.
Figure 3.
Pre- and post-treatment records for a patient in the study. With treatment, the overbite increased from −2.9mm to 0.1mm. The POSI score decreased from 2 to 1, signifying that the openbite was not successfully closed. The patient was treated with clear aligners, only. This was the primary recommendation. The practitioner also recommended full-fixed appliances and full-fixed appliances with TADs. At the end of active treatment (T2), the patient indicated that he or she was somewhat dissatisfied with the treatment provided and very dissatisfied with his or her ability to chew. The patient would not recommend the treatment that he or she received to a friend with a similar malocclusion. Open-ended responses describe improved esthetics, but elevated temporomandibular dysfunction symptoms. No statement was included about the residual openbite.
Table 7.
Representative sample of open-ended responses directly associated with patient satisfaction
| Treatment Provided | Appearance | Biting and Chewing | Speech |
|---|---|---|---|
| Honestly, I wish my lower jaw was further forward, but that’s vanity. My teeth look great! I’m very happy! | |||
| Biting with front teeth is still not able to fully bite thru things [sic], but much better. | |||
| Doctor and his staff are wonderful and give high quality treatment. They are also very personable. | My teeth/bite look amazing and now I can comfortably smile [sic]. | I can chew/bite very comfortably with no issues. | I feel like it’s more clear [sic]. |
| They are almost too perfect. | |||
| Due to the appearance of my two front upper teeth, we could not align them 100% straight [sic]. Out of our control. | |||
| The openbite is a lot smaller than before. | |||
| Still have lingering numbness and lower jaw cant is very slightly tilted [sic]. | |||
| Would like to have had the tiny gaps closed up. | |||
| The staff were willing to experiment & do all that they could [sic]! I was extremely satisfied with office staff. The results did not meet my expectations. I still have openbite & pressure on back teeth. | It is very difficult to eat and bite down on food. | ||
| Front teeth still do not touch bottom teeth [sic]. | Front jaw moved forward more than anticipated [sic]. | ||
| Slightly imperfect center alignment. | |||
| They look great! It seems like maybe there’s still a little space between my teeth on the right where they removed my baby tooth, but that’s probably b/c I was inconsistent about wearing the bands [sic]. | |||
| Tipping/flaring of the tooth is a little more then expected [sic], but I’m still very happy with my teeth! | |||
| There is still occasional discomfort in my jaw. | |||
| Jaw clicking is worse. | Appearance has improved, but jaw clicking is worse. | Jaw clicking is worse. I need to avoid any chewy foods (i.e. bread). | Speech has not changed. |
| I can now eat raw vegetables, including lettuce. |
Additional open-ended responses regarding the orthodontic treatment in general, but not specifically linked to patient satisfaction, were received from 119 patients (48%). Five of these patients were among the ten who indicated that they were not satisfied with the orthodontic treatment provided or an element of the final result. The remaining 114 patients reported high levels of satisfaction. Eighty-seven patients (73%) recorded positive responses. Of the positive responses, 56 mention the treatment received and 78 describe a positive doctor-staff-patient relationship. Eighteen (15%) and eleven (9%) patients recorded neutral and negative responses, respectively. No obvious trends were observed for these comments. Three patients (3%) expressed some concern about the stability of treatment. A representative sample of these open-ended responses is found in Table 8.
Table 8.
Representative sample of open-ended responses regarding the orthodontic treatment in general, but not specifically linked to patient satisfaction
| General Open-Ended Responses |
|---|
| Everything worked out great! |
| I’m very happy with my results. My bite feels amazing and now I can smile with confidence. |
| Dr. X and staff were (and continue to be) wonderful! All aspects of these past 9 months was above expectations [sic]! |
| I am extremely pleased with my results. They are life changing! I never dreamed my teeth would look this great! I now have a smile I won’t be embarrassed of! |
| The process was smooth. Staff is great [sic]. I have already referred a friend that got his braces on [sic]. |
| Dr. X and his staff are amazing! |
| Interested to see how long it is maintained. |
| Awesome experience. Great doctor. |
| Very satisfied. Very professional staff and doctor. |
| Dr. X and her team are top notch! Extremely satisfied with my results! |
| Would have like a more thorough explanation of the treatment plan at each appointment [sic]. |
| I couldn’t have asked for better treatment or a better team than Dr. X and his staff. Thank you! |
| The jaw surgery part of the treatment was quite intense and I don’t quite have normal feelings back yet, but it continues to progress and the ortho experience was pretty normal [sic]. |
| I’ll bet I had the best orthodontist out there [sic]! Loved the treatment, fantastic work and results! |
| Very happy that I completed the course [sic], had the surgery, and Dr. X was awesome. |
| The only concern that I have is the possibility of my teeth moving out of alignment. |
| My orthodontic treatment was lengthy but well worth it. My orthodontists were very thorough and cared about my opinion and overall outcome of my teeth. |
| Excellent care at all times! Thank you! |
| Satisfied with the result! I would definitely recommend! |
| The entire staff was very nice and was always able and willing to answer questions about treatment. |
| Teeth shifting and developing openbite even with regular retainer wear and speech therapy to correct tongue thrust. |
| Overall great service and staff. |
| This is one of the best decisions I’ve ever made. To get a new smile is all that I’ve wanted and the staff is wonderful here. They make me feel like family. |
| Very happy with the results! Can bite/tear food with my teeth! |
Discussion
Patient satisfaction with orthodontic treatment has received limited analysis in the orthodontic literature.14,15 Instead, most current orthodontic research reports on morphologic changes that result from treatment.14 Morphologic changes, obtained from analysis of casts, radiographs, and clinical examination21, are important and necessary for clinicians to evaluate treatment efficacy. However, these traditional outcome measures do not typically reflect patient values. As orthodontic treatment aims to improve a patient’s dentofacial appearance, oral function, and psychosocial state, it is important for orthodontic literature to evaluate patient-centered outcomes, such as patient satisfaction.10,14
Extraordinarily high levels of patient satisfaction were found in our sample of adults, who received orthodontic treatment for AOB malocclusion across the United States. Specifically, 96% of the patients reported being satisfied with the treatment provided as well as the final esthetic and functional results. Only ten patients, out of the two hundred and forty-eight for whom satisfaction data were available, were not satisfied. The high satisfaction level is substantiated by the fact that 98% of the patients would recommend the treatment that they received to a friend with a similar malocclusion. The available literature on patient satisfaction describes high levels of contentment with orthodontic care.15
Numerous factors have been suggested to influence satisfaction with orthodontic treatment. A recent systematic review15 concluded satisfaction after orthodontic treatment was strongly associated with perceived esthetic outcomes, perceived psychological benefits of treatment, positive patient psychological traits, and the quality of the doctor-staff-patient relationship. Dissatisfaction after orthodontic treatment was correlated with increased discomfort or pain, problems with the usage of retention appliances, and negative patient psychological traits. Our results indicate that treatment outcome, treatment modality, and some patient characteristics may influence the satisfaction of adult, AOB patients. Statistical significance could not be assessed due to the small number of dissatisfied patients. Trends are reported in the following three paragraphs.
In our study, a direct relationship may exist between openbite closure and patient satisfaction. The relationship is strongest for patient-perceived treatment success and weakest when treatment success is defined by POSI = 0. The potential correlation between success and satisfaction is not surprising for several reasons. Adult patients tend to be more aware of their initial malocclusion and final treatment outcome.22 This natural awareness was likely heightened by their enrollment in the National Dental PBRN adult, AOB study. Two recent studies corroborate the close relationships between treatment outcome and patient satisfaction in adults. Reidmann, et al.23 found that 97% of adult patients were satisfied with their treatment outcome. Lee, et al.24 calculated an overall satisfaction rate of 84.9% and a 92.6% rate specifically related to treatment outcome.
The treatment modality may also affect the satisfaction of adult patients receiving treatment for AOB malocclusion. Patients treated with clear aligners only or orthognathic surgery report higher levels of dissatisfaction. Clear aligner therapy is the most esthetic and least invasive treatment modality. For these reasons, one may expect aligner patients to be exceedingly satisfied. On the contrary, patients who specifically request this esthetic treatment option may be more particular about the appearance of their teeth during treatment, as well as their outcomes. This higher level of discrimination might be associated with the higher levels of dissatisfaction observed in aligner patients. A recent study described high levels of patient satisfaction with clear aligner therapy, however satisfaction was most strongly correlated to the doctor-patient relationship.25 Another study found similar satisfaction levels between aligner therapy and conventional fixed appliances.26 High levels of patient satisfaction have traditionally been reported after orthodontic treatment combined with orthognathic surgery.27
Satisfaction is presumably due to the significant esthetic and functional improvements produced by surgical correction. Conversely, dissatisfaction is often associated with functional impairment or dysfunction after surgery. This association was evident in the open-ended responses, as three of the fifty-three surgical patients (6%) described residual numbness and/or pain following the procedure. One patient stated, “the jaw surgery was quite intense”. He or she does not “quite have normal feelings back yet”. Overall, the possible inverse relationship between orthognathic surgery and satisfaction found in this study is likely due to the invasiveness of the procedure and the residual side effects following the procedure.
Trends were observed between satisfaction and two patient characteristics, namely sex and education level. Previous research has established that patient satisfaction is associated with sex. Specifically, female patients have higher expectations about dentofacial improvement and, in turn, are more critical of treatment.15,24,28,29 In the present study, female patients reported higher levels of dissatisfaction with the orthodontic treatment provided and the final result. Educated patients also tended to be less satisfied. Patients with higher education levels are more discriminating, which likely predisposes them to be dissatisfied with an aspect of treatment.30
Open-ended responses provide valuable insight into patient perspectives. Following answers of somewhat or very dissatisfied on the Likert-like scale, patients were asked to specify the reason for their dissatisfaction. Interestingly, comments were only entered by two of the ten patients who were not satisfied with treatment or an element of the final result. Dissatisfied patients may elect not to provide open-ended responses due to the time it takes to write a response, therefore preventing us from fully understand their dissatisfaction. For example, a patient with a seemingly large functional change indicated that he or she was not satisfied with his or her ability to chew at the end of treatment (Figure 4). Instead, the vast majority of the responses were provided by patients who reported high levels of satisfaction.
Figure 4.
Pre- and post-treatment records for a patient in the study. With treatment, the overbite increased from −2.5mm to 2.4 mm. The POSI score decreased from 6 to 0, signifying that the openbite was successfully closed. The patient was treated with full-fixed appliances and orthognathic surgery. Despite a successful result, the patient indicated that he or she was not satisfied with his or her ability to chew at the end of treatment.
Positive and negative open-ended responses were received from both satisfied and dissatisfied patients, regardless of whether their openbite was successfully closed. For example, a satisfied patient indicated that he or she “would like to have had the tiny gaps closed up”. The patient had a successful result. His or her comment referred to black triangles that developed following the alignment of overlapping incisors (Figure 5). This implies that the significant esthetic and functional improvements produced by AOB closure likely override minor discontent with treatment. Another patient was satisfied with an unsuccessful result. He or she reported being “totally happy”, as the openbite “was closed as much as possible” (Figure 6). In contrast, a different patient was dissatisfied with an unsuccessful result, stating that the residual openbite makes “it very difficult to eat and bite down on food” (Figure 2). Despite these functional concerns, the patient “was extremely satisfied with the office staff”. This distribution of responses suggests two principles. First, if practitioners set realistic expectations, patients are usually satisfied at the end of treatment.22,31 Second, satisfaction may be most closely associated with positive patient personality traits15,31,32 and a quality doctor-staff-patient relationship.15,28,29,33–37 The value of the doctor-staff-patient relationship was substantiated by additional comments, separate from those directly associated with patient satisfaction (Table 8). These additional responses were overwhelmingly positive and clearly demonstrate the value of a positive patient-provider relationship.
Figure 5.

Pre- and post-treatment intraoral frontal photographs for a patient in the study. The openbite was closed and the patient was satisfied with treatment. However, the patient expressed minor misgivings about the final esthetics result, specifically the black triangles.
Figure 6.

Pre- and post-treatment intraoral frontal photographs for a patient in the study. The openbite was not successfully closed, but the patient was still satisfied with treatment. In his or her words, the openbite “was closed as much as possible”.
Given the high levels of success18 and patient satisfaction immediately following treatment, it will be extremely important to assess these outcomes in retention. Long-term patient satisfaction with orthodontic treatment has been shown to be high.38 It will be interesting to determine whether this is true for openbite patients, who have a high tendency for vertical relapse.9 A subsequent publication will describe treatment success and patient satisfaction in retention.
Limitations
This study has several limitations. The sample of practitioners was not randomly or consecutively chosen. Practitioners were recruited from the National Dental PBRN and some self-selection certainly occurred. These practitioners may have had a particularly high interest or skill level in treating anterior openbite patients. Patients also were not randomly chosen, but steps were taken to minimize selection bias. Practitioners were asked to enroll all eligible patients in their practice, up to a maximum of fifteen. If a practitioner had more than fifteen eligible patients, patients were selected sequentially based upon their treatment start dates. Although the analysis was adjusted for clustering, a residual effect could remain and the quality of the doctor-staff-patient relationship has been shown to positively influence patient satisfaction.15 Also, 63 of the 347 originally enrolled patients had not completed treatment at the time that data collection closed. There could be many reasons why these patients did not complete treatment during the study period, including more challenging malocclusions, poor cooperation, modifications to treatment plans, and refractory oral habits. It is possible that these patients may have a lower success rate than those who finished treatment during the study period, which might lessen the high satisfaction levels that we observed.
Although the study is prospective in design, details related to treatment were collected through questionnaires at enrollment (T1), after treatment had begun. As these data were acquired retrospectively, there is a risk for recall bias. Patient satisfaction was assessed immediately following appliance removal. Patients placed completed questionnaires in sealed envelopes, allowing their responses to remain anonymous. The process was as confidential as possible given the use of paper forms. However, satisfaction levels may be inflated if patients were concerned about confidentiality, specifically the influence of a negative response on their relationship with the doctor and/or staff. As the satisfaction questionnaire was typically administered on the day of appliance removal, patients may not have had sufficient time to evaluate their satisfaction, specifically related to function. Additionally, high levels of satisfaction may be expected on the day of appliance removal. Finally, due to the high levels of satisfaction, there was insufficient power for inferential statistics.
Conclusions
Very high levels of satisfaction were observed for adult patients who received orthodontic treatment for AOB malocclusion. Although there were too few dissatisfied patients to conduct any meaningful statistical analyses, our results suggested that satisfaction may be associated with successful openbite closure, as well as treatment modality, gender, and education level.
Supplementary Material
Acknowledgements
This study was funded by NIDCR grants U19-DE-22516 and U19-DE-28717. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully. An Internet site devoted to details about the nation’s network is located at http://NationalDentalPBRN.org and is conducted under the auspices of the National Dental PBRN. We gratefully acknowledge all the practitioners and patients who made this study possible. We are also grateful to the network’s regional coordinators, Sarah Basile, RDH, MPH, Chris Enstad, BS, and Hannah Van Lith, BA (Midwest); Stephanie Hodge, MA, and Kim Stewart (Western); Pat Ragusa (Northeast); Deborah McEdward, RDH, BS, CCRP, and Danny Johnson (South Atlantic); Claudia Carcelén, MPH, Shermetria Massingale, MPH, CHES, and Ellen Sowell, BA (South Central); Stephanie Reyes, BA, Meredith Buchberg, MPH, and Monica Castillo, BA (Southwest). We also thank Kavya Vellala and the Westat Coordinating Center staff, the American Association of Orthodontists (AAO), Jackie Hittner (AAO Librarian), Gregg Gilbert, DDS, MBA (National Network Director), and Dena Fischer, DDS, MSD, MS (NIDCR Program Director).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Samuel A. Finkleman, Private Practice Seattle, Washington.
Lauren S. Todoki, Private Practice Seattle, Washington.
Ellen Funkhouser, Division of Preventive Medicine, School of Medicine, University of Alabama, Birmingham.
Geoffrey M. Greenlee, Department of Orthodontics, University of Washington, Seattle.
Kelly W. Choi, Private Practice, San Francisco, California.
Hsiu-Ching Ko, Department of Orthodontics, University of Washington, Seattle.
Hsuan-Fang Wang, Department of Orthodontics, University of Washington, Seattle Attending Physician, Division of Orthodontics, Department of Dentistry, Far Eastern Memorial Hospital, Taipei, Taiwan.
Peter A. Shapiro, Department of Orthodontics, University of Washington, Seattle.
Rooz Khosravi, Department of Orthodontics, University of Washington, Seattle.
Camille Baltuck, Western Region, National Dental Practice-Based Research Network.
Veerasathpurush Allareddy, Department Head, Department of Orthodontics, University of Illinois at Chicago.
Calogero Dolce, Department of Orthodontics, University of Florida.
Chung Hao Kau, Department of Orthodontics, University of Alabama at Birmingham.
Kyungsup Shin, Department of Orthodontics, University of Iowa.
Jaime de Jesus-Vinas, Private Practice, San Juan, Puerto Rico.
Michael Vermette, Private Practice Concord, New Hampshire.
Cameron Jolley, Private Practice Trophy Club, TX.
Greg J. Huang, Department of Orthodontics University of Washington, Seattle.
References
- 1.Anderson GM. Practical Orthodontics. St. Louis, MO: Mosby; 1948. [Google Scholar]
- 2.Subtelny JD, Sakuda M. Open-bite: Diagnosis and treatment. American Journal of Orthodontics and Dentofacial Orthopedics. 1964;50(5):337–358. [Google Scholar]
- 3.Abu Alhaija ES, Al-Khateeb SN. Attractiveness ratings of anterior open bites and reverse overjets using the aesthetic component of the Index of Orthodontic Treatment Need. Eur J Orthod. 2005;27(2):134–139. [DOI] [PubMed] [Google Scholar]
- 4.Artese A, Drummond S, Nascimento JMd, Artese F. Criteria for diagnosing and treating anterior openbite with stability. Dental Press Journal of Orthodontics. 2011;16:136–161. [Google Scholar]
- 5.Kelly JE, Sanchez M, Van Kirk LE. An Assessment of the Occlusion of the Teeth of Children 6-11Years, United States. Vital Health Stat 11 1973(130):1–60. [PubMed] [Google Scholar]
- 6.Lentini-Oliveira DA, Carvalho FR, Rodrigues CG, et al. Orthodontic and orthopaedic treatment for anterior open bite in children. Cochrane Database Syst Rev. 2014(9):CD005515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw WC, Addy M, Ray C. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dent Oral Epidemiol. 1980;8(1):36–45. [DOI] [PubMed] [Google Scholar]
- 8.Maciel CT, Leite IC. [Etiological aspects of anterior open bite and its implications to the oral functions]. Pro Fono. 2005;17(3):293–302. [DOI] [PubMed] [Google Scholar]
- 9.Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: a meta-analysis. Am J Orthod Dentofacial Orthop. 2011;139(2):154–169. [DOI] [PubMed] [Google Scholar]
- 10.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. J Orthod. 2001;28(2):152–158. [DOI] [PubMed] [Google Scholar]
- 11.Kravitz R Patient satisfaction with health care: critical outcome or trivial pursuit? J Gen Intern Med. 1998;13(4):280–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Z, McGrath C, Hagg U. The impact of malocclusion/orthodontic treatment need on the quality of life. A systematic review. Angle Orthod. 2009;79(3):585–591. [DOI] [PubMed] [Google Scholar]
- 13.Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod. 2015;37(3):238–247. [DOI] [PubMed] [Google Scholar]
- 14.Tsichlaki A, O’Brien K. Do orthodontic research outcomes reflect patient values? A systematic review of randomized controlled trials involving children. Am J Orthod Dentofacial Orthop. 2014;146(3):279–285. [DOI] [PubMed] [Google Scholar]
- 15.Pachêco-Pereira C, Pereira JR, Dick BD, Perez A, Flores-Mir C. Factors associated with patient and parent satisfaction after orthodontic treatment: a systematic review. Am J Orthod Dentofacial Orthop. 2015;148(4):652–659. [DOI] [PubMed] [Google Scholar]
- 16.Choi KW, Ko HC, Todoki LS, et al. The National Dental Practice-Based Research Network adult anterior open bite study: A description of the practitioners and patients. Angle Orthod. 2018;88(6):675–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang G, Baltuck C, Funkhouser E, et al. The National Dental Practice-Based Research Network Adult Anterior Open Bite Study: Treatment recommendations and their association with patient and practitioner characteristics. Am J Orthod Dentofacial Orthop. 2019;156(3):312–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Todoki LS. The National Dental Practice-Based Research Network Adult Anterior Openbite Study: Treatment Success. In:2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.An Atlas of craniofacial growth : cephalometric standards from the University school growth study, the University of Michigan. In: Riolo ML, ed. Ann Arbor: :: Center for Human Growth and Development, University of Michigan; 1974. [Google Scholar]
- 20.Scheideman GB, Bell WH, Legan HL, Finn RA, Reisch JS. Cephalometric analysis of dentofacial normals. Am J Orthod. 1980;78(4):404–420. [DOI] [PubMed] [Google Scholar]
- 21.Bondemark L, Holm AK, Hansen K, et al. Long-term stability of orthodontic treatment and patient satisfaction. A systematic review. Angle Orthod. 2007;77(1):181–191. [DOI] [PubMed] [Google Scholar]
- 22.Oliveira PG, Tavares RR, Freitas JC. Assessment of motivation, expectations and satisfaction of adult patients submitted to orthodontic treatment. Dental Press J Orthod. 2013;18(2):81–87. [DOI] [PubMed] [Google Scholar]
- 23.Riedmann T, Georg T, Berg R. Adult patients’ view of orthodontic treatment outcome compared to professional assessments. J Orofac Orthop. 1999;60(5):308–320. [DOI] [PubMed] [Google Scholar]
- 24.Lee R, Hwang S, Lim H, Cha JY, Kim KH, Chung CJ. Treatment satisfaction and its influencing factors among adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2018;153(6):808–817. [DOI] [PubMed] [Google Scholar]
- 25.Pacheco-Pereira C, Brandelli J, Flores-Mir C. Patient satisfaction and quality of life changes after Invisalign treatment. Am J Orthod Dentofacial Orthop. 2018; 153(6) :834–841. [DOI] [PubMed] [Google Scholar]
- 26.Flores-Mir C, Brandelli J, Pacheco-Pereira C. Patient satisfaction and quality of life status after 2 treatment modalities: Invisalign and conventional fixed appliances. Am J Orthod Dentofacial Orthop. 2018;154(5):639–644. [DOI] [PubMed] [Google Scholar]
- 27.Pachêco-Pereira C, Abreu LG, Dick BD, De Luca Canto G, Paiva SM, Flores-Mir C. Patient satisfaction after orthodontic treatment combined with orthognathic surgery: A systematic review. Angle Orthod. 2016;86(3):495–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bergström K, Halling A, Wilde B. Orthodontic care from the patients’ perspective: perceptions of 27-year-olds. Eur J Orthod. 1998;20(3):319–329. [DOI] [PubMed] [Google Scholar]
- 29.Bos A, Vosselman N, Hoogstraten J, Prahl-Andersen B. Patient compliance: a determinant of patient satisfaction? Angle Orthod. 2005;75(4):526–531. [DOI] [PubMed] [Google Scholar]
- 30.Jafari Kelarijani SE, Jamshidi R, Heidarian AR, Khorshidi M. Evaluation of factors influencing patient satisfaction in social security hospitals in Mazandaran province, North of Iran. Caspian J Intern Med. 2014;5(4):232–234. [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Omiri MK, Abu Alhaija ES. Factors affecting patient satisfaction after orthodontic treatment. Angle Orthod. 2006;76(3):422–431. [DOI] [PubMed] [Google Scholar]
- 32.Barker MJ, Thomson WM, Poulton R. Personality traits in adolescence and satisfaction with orthodontic treatment in young adulthood. Aust Orthod J. 2005;21(2):87–93. [PubMed] [Google Scholar]
- 33.Fernandes LM, Espeland L, Stenvik A. Patient-centered evaluation of orthodontic care: a longitudinal cohort study of children’s and parents’ attitudes. Am J Orthod Dentofacial Orthop. 1999;115(3):227–232. [DOI] [PubMed] [Google Scholar]
- 34.Mascarenhas AK, Vig K, Joo BH. Parents’ satisfaction with their child’s orthodontic care: a comparison of orthodontists and pediatric dentists. Pediatr Dent. 2005;27(6):451–456. [PubMed] [Google Scholar]
- 35.Anderson LE, Arruda A, Inglehart MR. Adolescent patients’ treatment motivation and satisfaction with orthodontic treatment. Do possible selves matter? Angle Orthod. 2009;79(5):821–827. [DOI] [PubMed] [Google Scholar]
- 36.Keles F, Bos A. Satisfaction with orthodontic treatment. Angle Orthod. 2013;83(3): 507–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feldmann I Satisfaction with orthodontic treatment outcome. Angle Orthod. 2014;84(4):581–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maia NG, Normando D, Maia FA, Ferreira MA, do Socorro Costa Feitosa Alves M. Factors associated with long-term patient satisfaction. Angle Orthod. 2010;80(6):1155–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


