The coronavirus disease-2019 (COVID-19) pandemic has reportedly resulted in more than one and a half million deaths worldwide. It has been proposed that people of older age and those with certain medical conditions are at higher risk of adverse outcomes, including death. Yet, a plethora of people that have surpassed the average life expectancy have recovered from COVID-19 infections, including more than fifty centenarians.1 Interestingly, these older survivors do not phenotypically manifest signs of metabolic syndrome, as their BMI appears to be within the normal range. It is important to shine light in what prevents adverse outcomes in survivors with COVID-19.
A meta-analysis described an increased risk of mortality for overweight (BMI > 25.0 kg m−2) people with COVID-19.2 These accumulating data raise the question whether obesity and its associated comorbidities, such as diabetes, hypertension and cardiovascular disease may be better predictors of adverse outcomes for COVID-19 infections, than the ageing-associated immunosenescence. Reports indicate that, of the deceased due to COVID-19, only 6% in the US,3 9% in Australia4 and 3.9% in Italy5 had no known comorbidities.
The case fatality ratio is also higher in American, European, and Middle Eastern countries that exhibit higher prevalence rates of obesity and metabolic syndrome, compared with African countries.6 A possible explanation is the likely greater production of Vitamin D due to increased sun exposure in the African continent. Vitamin D is known to possess immunomodulatory properties and its deficiency has been linked to COVID-19 hospitalisations.7 Another explanation is a possible link between obesity prevalence and adverse outcomes.
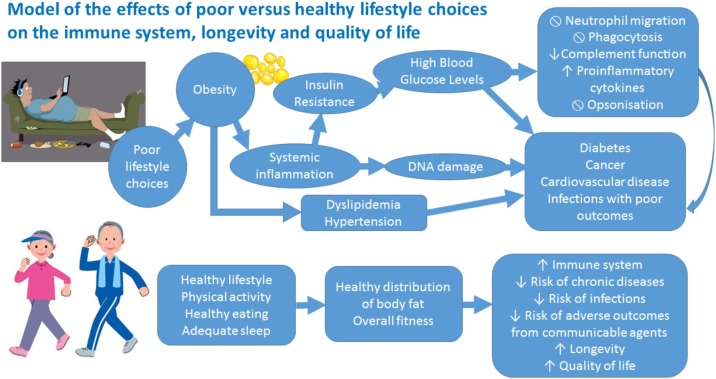
Lifestyle can affect weight management and it has been discussed in terms of its effect on COVID-19 hospitalisations, with physical inactivity, increased body fat and smoking all independently increasing hospital admissions in COVID-19 patients.8 Low grade inflammation has been proposed as a possible mechanism. A chronic state of low-grade systemic inflammation characterises obesity due to an increase in the production of reactive oxygen species. Visceral adipose tissue inflammation has been linked to the development of insulin resistance. The concomitant hyperglycaemia results in an impaired immune system function and an increased susceptibility to infections (Fig. 1 ). Diet, physical activity and sleep can all independently improve body composition, lower chronic inflammation and boost the immune system’s function.
Fig. 1.
Model of the effects of poor versus healthy lifestyle choices on the immune system, longevity and quality of life. Poor lifestyle choices such as poor nutrition, inadequate physical activity and insufficient sleep increase the risk of obesity. Obesity is characterised by systemic inflammation that can alter the DNA and promote carcinogenesis and can drive insulin resistance, leading to hyperglycaemia and, if uncontrolled, diabetes. Hyperglycaemia is deleterious to the immune system, inhibiting neutrophil migration, phagocytosis and immunoglobulin-mediated opsonisation, while promoting proinflammatory cytokine production and inhibiting complement fixation to pathogens. Obesity also increases the risk of high blood pressure and dyslipidaemia, that if untreated, can lead to cardiovascular disease. Healthy lifestyle choices, such as being physically active, eating a healthy diet and sleeping well, promote overall fitness and a healthy distribution of body fat. The result is a potent immune system, reduced risk of chronic diseases, infections and of adverse-effects by communicable agents, such as COVID-19 and influenza virus. This healthy lifestyle increases chances for longevity, improves quality of life and promotes an overall sense of wellbeing.
Data demonstrate that elite athletes, such as professional basketball players, appear protected from the adverse effects of COVID-19 infections. During the resumption of the National Basketball Association (NBA) league between July and October 2020, at least 41 elite basketball players tested positive for COVID-19.9 They all reportedly recovered successfully, with no signs of loss in performance or other adverse effects. Some of these players achieved career high performances following recovery from the infection,10, 11 indicating no decline in acceleration, endurance or reaction rate and therefore suggesting no adverse effects on the anaerobic and aerobic capacity and on the nervous system of elite basketball players.
Athletes exhibit an improved maximal aerobic capacity and a favourable body composition compared to sedentary people, with the latter being evident even when the two populations have the same total amount of body fat. A recent review highlighted the effect of the differential fat distribution on cardiometabolic outcomes.12 Physical activity promotes reduction in visceral adipose tissue, decreasing thus the risk of adverse cardiometabolic outcomes.
The COVID-19 pandemic presents an opportunity to raise awareness on the importance of leading a healthy lifestyle to reduce morbidity and mortality and to increase lifespan and improve quality of life. In addition to the spread of infectious diseases, it has been demonstrated that obesity can too be spread through social connections, with chances of becoming obese increasing by 57% for people who have an obese friend.13
The development of an effective and safe COVID-19 vaccine is necessary to address the urgent short-term problem, however, given the worldwide obesity prevalence, the population will remain prone to all the chronic and other communicable risk factors if emphasis is not placed on treating the underlying cause for most of the global morbidity and mortality. The increasing obesity prevalence also poses an opportunity for more potent communicable agents, as it has been demonstrated that the chance of more virulent strains is increased in obese populations due to prolonged viral shedding that may increase the overall mortality rate.14
The World Health Organisation laid down the principles of health promotion in the “Ottawa Charter” in 1986. Thirty-four years later, obesity rates have been increasing and physical activity has been decreasing. A 2009 review indicated declining rates of fitness and physical activity in young people, raising the alarm for the future.15 It is recommended that strong physical activity initiatives are employed on a population level. The education on maintaining hygienic practices, such as washing hands regularly, wearing a mask and socially distancing, should be followed by education on the importance of physical activity and achieving a favourable body composition. The unique opportunity for a drastic and sustainable change in public health that COVID-19 presents should not be wasted.
Funding
Nil for this study. George Siopis is a recipient of the University of Sydney International Scholarship Strategic Fund and of the Neville Whiffen Scholarship. Neither of these bodies had any role in the preparation, writing or approval of the manuscript; or decision to submit the manuscript for publication.
References
- 1.Gerontology Wiki. List of oldest people with Covid-19. Available from https://gerontology.wikia.org/wiki/List_of_oldest_people_with_COVID-19. (Accessed 19 November 2020).
- 2.Hussain A., Mahawar K., Xia Z., et al. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract. 2020;14:295–300. doi: 10.1016/j.orcp.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 3.Centers for Disease and Control Prevention. National Center for Health Statistics. Weekly Updates by Select Demographic and Geographic Characteristics. Provisional Death Counts for Coronavirus Disease 2019 (COVID-19). Updated September 16 2020. Available from https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm?fbclid=IwAR3-wrg3tTKK5-9tOHPGAHWFVO3DfslkJ0KsDEPQpWmPbKtp6EsoVV2Qs1Q&_ga=2.83596054.1497558416.1598967201-386365132.1598967194#Comorbidities. (Accessed 19 November 2020).
- 4.COVID-19 National Incident Room Surveillance Team. COVID-19, Australia: Epidemiology Report 20. Fortnightly reporting period ending 5 July 2020. [DOI] [PubMed]
- 5.Statista. Number of comorbidities observed in COVID-19 deceased patients in Italy as of July 22, 2020. Available from https://www.statista.com/statistics/1110906/comorbidities-in-covid-19-deceased-patients-in-italy/. (Accessed 19 November 2020).
- 6.Johns Hopkins. Coronavirus Resource Center. Mortality Analysis. Mortality in the most affected countries. Available from https://coronavirus.jhu.edu/data/mortality?fbclid=IwAR14OFu1-qNvOCHuctDoRp6s0_rImbxBN83sU0dEHn8Ogp1tce7hKytPXg8. (Accessed 19 November 2020).
- 7.Hernández J.L., Nan D., Fernandez-Ayala M., et al. Vitamin D status in hospitalized patients with SARS-CoV-2 infection. J Clin Endocrinol Metabolism. 2020 doi: 10.1210/clinem/dgaa733. dgaa733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamer M., Kivimäki M., Gale C.R., Batty G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav Immun. 2020;87:184–187. doi: 10.1016/j.bbi.2020.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CBS Sports. Coronavirus: Russell Westbrook, Nikola Jokic, Eric Bledsoe among NBA players who tested positive. Available from https://www.cbssports.com/nba/news/coronavirus-russell-westbrook-nikola-jokic-eric-bledsoe-among-nba-players-who-tested-positive/. (Accessed 19 November 2020).
- 10.NBA.com. Donovan Mitchell’s 57 points rank third in NBA single-game playoff history. Available from https://www.nba.com/article/2020/08/17/donovan-mitchell-third-most-points-playoff-history#:∼:text=Though%20it%20wasn't%20enough,most%20in%20NBA%20postseason%20history (Accessed 19 November 2020).
- 11.Essentially sports. Nikola Jokic sets multiple records during historic performance in game 7 against clippers. Available from https://www.essentiallysports.com/nba-news-basketball-denver-nuggets-nikola-jokic-sets-multiple-records-during-historic-performance-in-game-7-against-la-clippers-orlando-bubble/. (Accessed 19 November 2020).
- 12.Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8:616–627. doi: 10.1016/S2213-8587(20)30110-8. [DOI] [PubMed] [Google Scholar]
- 13.Christakis N.A., Fowler J.H. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 14.Luzi L., Radaelli M.G. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020;57:759–764. doi: 10.1007/s00592-020-01522-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knuth A.G., Hallal P.C. Temporal trends in physical activity: a systematic review. J Phys Act Health. 2009;6:548–559. doi: 10.1123/jpah.6.5.548. [DOI] [PubMed] [Google Scholar]