Background
Social containment measures (‘stay at home’ and ‘closure’ periods) introduced during the COVID-19 pandemic are reported to have led to a substantial reduction in emergency admissions for ST-segment elevation myocardial infarction (STEMI) but there is limited data on the duration of this reduction and whether this is subsequently followed by an increase [1]. In this study, we evaluated the association of social containment on rates of STEMI presentations in three European Heart Attack Centres (HAC) from major epicentres during the pandemic.
Methods
We recruited all patients with STEMI 4–6 weeks after the date of the first registered case of COVID-19 from three HACs: King’s College Hospital (KCH), London (4 March 2020 to 16 April 2020), Hospital Clinico San Carlos (HCSC), Madrid (1 March 2020 to 17 April 2020) and Spedali Civili (SC), Brescia (04 March 2020 to 31 March 2020). Cumulative STEMI incidence was tracked from the date of social containment – 23 March 2020 (UK), 15 March 2020 (Spain) and 09 March 2020 (Italy). Piecewise linear regression was performed for the 30-day period after closure and then by using visual estimations of significant cut-points in slope. Differences between the splines were determined by Student’s t-test. Second, patients during the COVID-19 pandemic were compared with a time-matched 2019 cohort, with in-hospital mortality as the primary end-point.
Results
During the COVID-19 pandemic of 2020, 105 patients were admitted from the date of social containment in each city to a time period ~30 days after announcement – 57 from KCH (54.3%), 25 (23.8%) from HCSC and 23 (21.9%) from SC. Cumulative incidence showed significant differences in cases between KCH, SC and HCSC (slopes 1.29, 0.79 and 0.58, respectively). However, quiescent phases (defined as flattening of the rate of admission curves) across all systems which was shortest and least acute at KCH (7 days, slope 1.05), compared to SC (10 days, slope 0.41) and longest and most manifest for HCSC (14 days, slope 0.09) (Fig. 1).
Fig. 1.
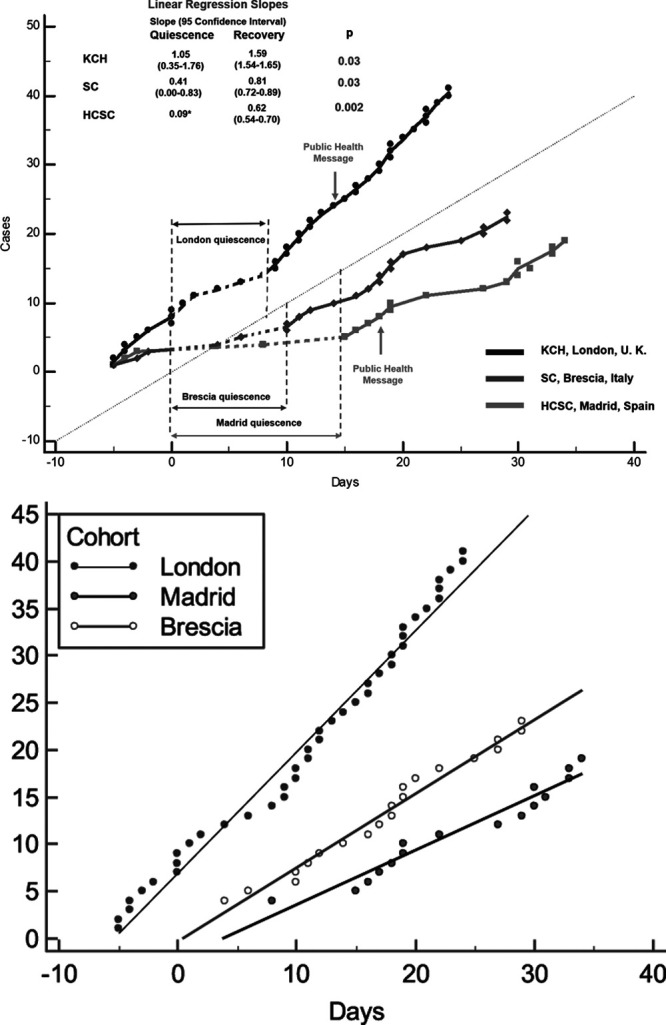
STEMI cases after social containment measures for the COVID-19 pandemic. (a) Scatter plot with linear regression analysis depicting quiescent (dashed lines) and recovery phases (lines). Colours depict different centres. Fitted linear regression analysis for both quiescent and recovery phases are shown with 95% confidence intervals and P values. STEMI, ST-segment elevation myocardial infarction.
We observed no decrease in the number of patients compared with the time-matched 2019 historical control group (n = 109) (Table 1). There was an overall predominance of men (83%) of middle age (mean 63 years) with no differences between cohorts. In 2020, the rates of hypertension were significantly higher (59% vs. 40.4%, P = 0.01) and smoking tended to be more prevalent (54.3% vs. 41.3%, P = 0.06). Patients in all centres were, however, significantly more likely to present very late (>12 hours from symptom onset) in 2020 than in 2019 (26.2% vs. 10.3%, P = 0.003). Cardiogenic shock and out-of-hospital cardiac arrest (OOHCA) tended to be less frequent in 2020 but not of statistical significance (7.6% vs. 15.6%, P = 0.07 and 12.2% vs. 20.2%, P = 0.12). Rates of TIMI 0 flow at baseline and post-procedure were similar but there was a higher TIMI thrombus burden grade 4–5 (large size thrombus and complete thrombotic occlusion) in the 2020 group (59.5% vs. 43.3%, P = 0.02). Interestingly, there was no difference in discharge LVEF (46.1% vs. 45.7%, P = 0.79) or in-hospital mortality (7.0% vs. 8.3%, P = 0.94) but median time to discharge was significantly shorter in the 2020 cohort (4 vs. 6 days, P < 0.001).
Table 1.
Characteristics and outcomes of ST-segment elevation myocardial infarction patients from 2019 to 2020
| Patient and angiographic characteristics | |||
|---|---|---|---|
| Demographic variables | 2019 cohort (n = 109) | 2020 cohort (n = 105) | P value |
| Mean age (SD) | 62.7 (13.8) | 63.7 (12.4) | 0.29 |
| Male, n (%) | 90 (82.6) | 87 (82.9) | 0.96 |
| CV risk factors | |||
| Hypertension, n (%) | 44 (40.4) | 62 (59.0) | 0.01 |
| Diabetes any type, n (%) | 24 (22.0) | 19 (18.1) | 0.48 |
| Smoking, n (%) | 45 (41.3) | 57 (54.3) | 0.06 |
| Presentation | |||
| Symptom to procedure time (min) | 189 | 232 | 0.08 |
| (117–360) | (118–729) | ||
| Late Presentation (>6 h) | 28 (26.2) | 39 (37.9) | 0.07 |
| Very Late Presentation (>12 h) | 11 (10.3) | 27 (26.2) | 0.003 |
| Cardiac arrest, n (%) | 22 (20.2) | 13 (12.4) | 0.12 |
| Intubated at time of procedure, n (%) | 16 (14.7) | 7 (6.7) | 0.06 |
| Cardiogenic shock, n (%) | 17 (15.6) | 8 (7.6) | 0.07 |
| Angiographic findings and adjunctive treatment | |||
| TIMI flow pre-PCI | |||
| 0 | 74 (76.0) | 73 (69.5) | 0.046 |
| 1 | 4 (3.8) | 8 (7.6) | |
| 2 | 12 (11.5) | 5 (4.8) | |
| 3 | 9 (8.7) | 19 (18.1) | |
| TIMI flow post-PCI | |||
| 0 | 4 (3.8) | 9 (8.6) | 0.45 |
| 1 | 3 (2.9) | 5 (4.8) | |
| 2 | 10 (9.6) | 10 (9.5) | |
| 3 | 87 (83.7) | 81 (77.1) | |
| TIMI thrombus burden score ≥4 | 45 (43.3) | 62 (59.0) | 0.02 |
| GP2B3A use, n (%) | 26 (23.9) | 34 (32.4) | 0.17 |
| Thrombectomy, n (%) | 21 (19.3) | 26 (24.8) | 0.33 |
| Outcome | |||
| Discharge LVEF (%) | 45.7 (11.1) | 46.1 (10.4) | 0.79 |
| Length of stay, median (IQR) | 6 (4–11) | 4 (2–6) | <0.0001 |
| In-hospital mortality, n (%) | 9 (8.3) | 7 (7.0) | 0.94 |
Bold indicates statistical significance of P values.
Demographic, angiographic and outcome difference between 2019 and 2020.
CV, cardiovascular; DM, diabetes mellitus; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention.
Conclusions
This cohort study indicates a quiescent period of STEMI presentations after social containment followed by a subsequent increase. There are several speculative reasons for this including fear of contagion, perceived burdening of the healthcare system or from a true reduction in events due to lower physical/emotional stress or competing events (since patients with cardiovascular disease are more susceptible to COVID-19). The extent and duration differed relatively by healthcare system, perhaps related to variations in the extent and strict adherence to social containment. In London, there was limited impact that might be due to pre-emptive preparation for the pandemic reducing requirement for service centralisation or perhaps due to a more relaxed approach to confinement. The reduction phase in Brescia was more prolonged, though, of note, this centre was a nominated local hub, doubling its coverage area. The sharper reduction in Madrid might be partly explained by saturation of medical systems and centralisation of services to other local hubs or to a stricter adherence to social containment. Transition from a quiescent to recovery phase might be explained by altered patient behaviour or a real change in incidence of MI. Public health messaging was initiated in London and Madrid on the basis of the quiescence but our study importantly indicates that this was performed too late to have had a positive impact, unless a further peak is to be observed [2].
Compared with the previous year, there was a marked increase in very late presentations with higher angiographic thrombus burden [3]. There was a tendency towards lower rates of OOHCA/cardiogenic shock, perhaps due to ‘competing conditions’ as recently reported [3], or due to death in the community. Despite lower rates of OOHCA, in-hospital mortality was similar between both years, which might indicate an underlying deleterious impact of later presentation. Shorter length of stay was also noted, perhaps due to earlier discharge to avoid nosocomial acquisition and for capacity in an overstretched system. Longer-term follow-up is required to fully understand the impact of these findings.
This study’s limitation is that it is an early report of a cohort comparison with small numbers and short follow-up, albeit from multiple centres from the major European clusters of the COVID-19 pandemic. It nevertheless highlights the critical importance of prospectively monitoring STEMI presentations and outcomes as the pandemic evolves to understand the impact of societal containment measures and proactively implementing public health interventions and strategic responses to prevent avoidable mortality from STEMI in future pandemics. This report also serves to highlight the need for more in-depth analysis of STEMI presentations to understand the impact of the pandemic and social containment on outcomes in this important illness.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scally G, Jacobson B, Abbasi K. The UK’s public health response to COVID-19. BMJ. 2020;369:m1932. doi: 10.1136/bmj.m1932. [DOI] [PubMed] [Google Scholar]
- 3.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. Lombardia CARe Researchers. Out-of-hospital cardiac arrest during the COVID-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]


