Abstract
Study objective:
Emergency physicians need to consider potential differences in quality of care across admitting services in their triage decisions. For emergency department (ED) patients with possible acute coronary syndrome who require hospitalization, there are relatively few data to guide emergency physicians in deciding whether admission to a cardiology service bed yields better outcomes than admission to a noncardiology service.
Methods:
We enrolled 544 ED patients who were admitted for symptoms of possible acute coronary syndrome after a nondiagnostic initial evaluation during a quality improvement trial at 2 university hospitals. Adverse events, inhospital treatment, and follow-up care were assessed by 30-day telephone interview and medical record review. We used a modified version of the Medical Outcomes Study Short Form 20 and the Duke Activity Status Index to assess functional status. To account for selection bias, we analyzed process and outcome variables after adjustment for the estimated propensity of being admitted to cardiology and predicted probability of acute cardiac ischemia.
Results:
Overall, 34% of admitted patients had confirmed acute coronary syndrome. Patients admitted to a cardiology service were significantly more likely to undergo evaluation for ischemic heart disease than those admitted to a noncardiology service (adjusted odds ratio for noninvasive testing 2.7; 95% confidence interval 1.7 to 4.2) but were not more likely to receive recommended therapies. The incidence of ED revisits and rehospitalizations, functional status, and adverse cardiovascular events were similar in both groups.
Conclusion:
ED patients admitted for evaluation of possible acute coronary syndrome do not experience worsened short-term outcomes if admitted to a noncardiology service bed.
INTRODUCTION
Given ongoing problems with crowding and prolonged waiting times for available hospital beds,1–4 emergency departments (EDs) are under increased pressure to expedite the triage of patients with noncritical conditions. If hospital beds are scarce, emergency physicians must often admit patients to the first available bed, with little choice of admitting service. Otherwise, the choice of admitting service is based on the emergency physician’s judgment. For the more than 5 million patients who present to the ED annually with symptoms of possible acute coronary syndrome (which includes unstable angina and acute myocardial infarction),5 there is relatively little outcome data to guide emergency physicians in deciding whether admission to a cardiology service bed (for those requiring hospitalization) is preferable to admission to a noncardiology service.
Potential advantages of cardiology care are improved recognition of acute coronary syndrome and greater use of recommended diagnostic tests and therapies.6–9 Potential advantages of generalist (noncardiology) care are the delivery of comprehensive and coordinated care for acute and chronic conditions.10 Most comparative studies of physician specialty have focused on the management of acute myocardial infarction, and the majority of these studies have demonstrated lower mortality for acute myocardial infarction patients treated by cardiologists (compared with noncardiologists).6,11–15 Other studies, however, have shown no significant differences in mortality between generalists’ and cardiologists’ patients after extensive adjustment for case mix and hospital characteristics.16–18
Goals of This Investigation
The aims of this study were (1) to compare ED patients with symptoms of possible acute coronary syndrome hospitalized on a cardiology service with patients admitted to noncardiology services and (2) to determine whether initial admission to a cardiology service is associated with improved care processes (delivery of guideline-recommended care) and better outcomes (need for subsequent emergency care or hospitalization, functional status, and 30-day mortality or inhospital complications).
MATERIALS AND METHODS
Study Design
We conducted a secondary analysis of data collected during an implementation trial of the Agency for Healthcare Policy and Research Unstable Angina guideline, which was conducted between January 2000 and May 2001. Using a pre-post design, this trial aimed to determine prospectively whether systematic use of the Agency for Healthcare Policy and Research recommendations for risk stratification would improve physician decisionmaking in ED patients with symptoms of possible acute coronary syndrome.19,20 Because this trial showed no significant impact of the guideline intervention on emergency physicians’ triage decisions, we pooled data from both the pre- and postintervention periods for analysis.
Setting
The study sites included 2 teaching hospitals in southern Wisconsin (1 university hospital and 1 university-affiliated community hospital) that participated in the above implementation trial. Neither hospital had a chest pain observation unit at this study. At both sites, there was considerable variability in decisions to admit to cardiology versus noncardiology service beds. This natural variability lent itself to comparison of processes and outcomes of care across patients hospitalized on both types of services.
Selection of Participants
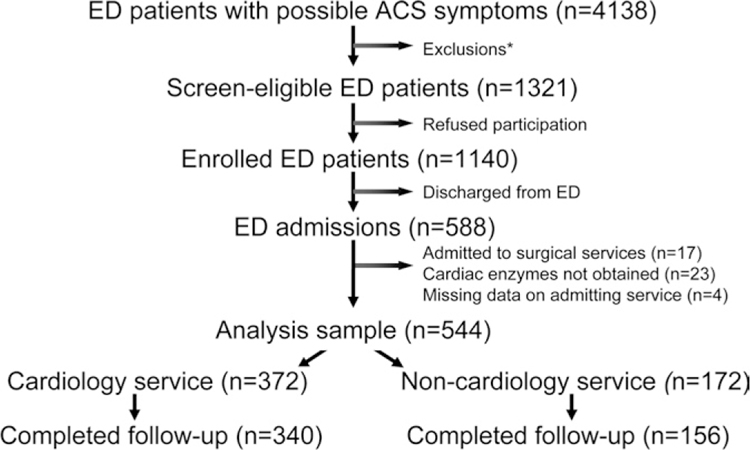
During the implementation trial, 4,138 ED patients who received a 12-lead ECG for evaluation of chest pain or other symptoms suggestive of acute coronary syndrome (shortness of breath, left arm pain, upper abdominal pain, nausea, or dizziness) were screened to determine eligibility during a 10-month period at each study hospital (Figure 1). These symptoms have been shown to capture more than 90% of patients with acute coronary syndrome in community-based studies.20 Research interviewers screened patients from 7 AM to 11 PM, including weekend days. Interviewers verified that the physician was considering acute coronary syndrome in the differential diagnosis of the patient’s symptoms at initial evaluation. Of the 1,321 eligible patients (see Figure 1 for exclusion criteria), 1,140 (86%) agreed to participate in the guideline implementation trial and 588 were admitted for further evaluation. Of these hospitalized patients, 544 (93%) comprised the analysis sample. This project was approved by the institutional review board at each study site.
Figure 1.
Derivation of the analysis sample. ACS, Acute coronary syndrome.
*Reasons for exclusion were as follows: (number in parentheses): known non-cardiac condition (eg, pneumothorax, panic attack) (883), inability to obtain informed consent (altered mental status, dementia, or language barrier) (759), age <30 (316), left emergency department prior to enrollment (138), trauma (127), medically unstable secondary to acute decompensation (85), unreachable at follow-up (65), prisoner (56), ECG diagnostic of acute MI (48), and miscellaneous causes (eg, direct admission to hospital, transfer to other EDs) (340).
Data Collection and Processing
After obtaining informed consent, the research technician at each site interviewed study patients to assess symptoms leading to ED presentation and pertinent cardiovascular history, and abstracted data on physical findings and test results (creatine kinase-MB, troponin I) from ED records.21 All patients received a 12-lead electrocardiogram in the ED. The nurse study coordinator reviewed hospital records to ascertain the occurrence of acute complications (see below).
Research personnel abstracted medical records to collect data on key noncardiovascular comorbidities to compute the Seattle Index of Comorbidity,22 because these items had not been collected prospectively during the implementation trial. We assessed whether patients received recommended therapy in the ED and during hospitalization by examining medical records and by searching computerized billing data for medications administered inhospital. Data on admitting service were obtained from hospital billing data, and specialty of the admitting physician was determined. For the purpose of this analysis, admitting physicians were classified as cardiologists or noncardiologists (including general internists, internal medicine subspecialists, and family practitioners); we combined generalists and medicine subspecialists (other than cardiology) to maximize power to detect differences between cardiologists and noncardiologists. We developed a training manual with definitions of all data elements,21 used standardized data collection forms, and monitored the accuracy of medical record reviewers by performing spot checks of 20% of all records; reviewers were blinded to study hypotheses.23
A structured telephone interview was administered to study patients at 30-day follow-up. If the patient was deceased, his or her spouse or other family member was interviewed to obtain further information on medical care before death. Self-reported adverse events, outpatient and inpatient visits, and procedures were confirmed by review of medical records. Vital status for patients who were lost to follow-up was determined by searching state death records. Thirty-day follow-up was similar in patients admitted to cardiology and noncardiology services (91% in both groups).
According to all available data, physician reviewers determined whether study patients had a diagnosis of acute coronary syndrome. The diagnosis of acute myocardial infarction was based on European Society of Cardiology/American College of Cardiology criteria,24 and the diagnosis of unstable angina was based on clinical history plus objective evidence of ischemia on diagnostic testing, which is consistent with current reporting guidelines.21,25 This approach to the definition of acute coronary syndrome showed high interrater reliability in the Unstable Angina Guideline Evaluation trial (κ = 0.73).19 Overall, 34% of admitted patients had confirmed acute coronary syndrome.
Outcome Measures
To assess the quality of care provided by cardiologists versus noncardiologists, we measured the following processes: (1) use of guideline-recommended therapy (specifically, acetylsalicylic acid, heparin, and β-blockers); and (2) diagnostic testing for cardiac ischemia, including resting and stress echocardiography, myocardial perfusion scanning with exercise or pharmacologic stress testing, or coronary angiography. To avoid underestimating the overall use of recommended therapies, we counted the administration of medications in the ED; for example, patients who received aspirin in the ED but did not receive additional doses while hospitalized were still classified as aspirin recipients. Analyses of β-blocker and heparin use were limited to patients with intermediate-to high-risk characteristics (as defined by the Agency for Healthcare Policy and Research guideline26 or increased troponin levels).
We measured the following outcomes: ED revisits or rehospitalization, health-related quality of life, and composite endpoint of 30-day mortality or inhospital complications. A trained nurse record reviewer identified possible inhospital complications in the medical record; a physician investigator then independently reviewed these records to verify the occurrence of complications. We identified the following inhospital complications: cardiogenic shock (defined as a systolic blood pressure less than 90 mm Hg for at least 30 minutes, end-organ hypoperfusion, and a pulse rate of greater than or equal to 60 beats/min), ventricular tachycardia or ventricular fibrillation requiring cardioversion or intravenous antiarrhythmic medication, cardiac arrest, respiratory failure requiring intubation, new complete heart block, late infarction (>24 hours after admission), and evidence of new heart failure without shock (>24 hours after admission).
To measure functional status, we used a modified version of the Medical Outcomes Study Short Form 20 (SF-20) to measure physical function, role function, pain, general health perception, social function, and mental health.27 SF-20 items were modified to reflect a 30-day recall period (rather than 3 months), and physical function response choices were adapted to indicate severity of limitation (a lot, a little, none) during the previous 30 days. Questions pertaining to role function determined whether the patient was limited in his or her ability to work at a job, to work around the house, or to perform schoolwork because of his or her health. Missing items were imputed with rules developed by SF-20 investigators.27
To measure disease-specific functional health, we administered a reduced version of the Duke Activity Status Index, which has been used to measure physical function in patients with angina and is significantly correlated with functional cardiac reserve.28 The emergency physician scale ranges from 0 to 58.2 (no impairment). Cases with more than 5 missing Duke Activity Status Index items were dropped from this analysis (M. Hlatky, written communication, April 2005). For those cases with 5 or fewer missing items, missing values were filled in using multiple imputation.29
Primary Data Analysis
Although observational studies are more representative of the broad spectrum of patients treated in clinical practice, they are susceptible to selection bias, which may confound the relationship between the exposure of interest and outcome. For example, patients who are admitted to cardiologists are typically younger and male, have fewer comorbid conditions, and may differ in other important characteristics from those who are admitted to noncardiologists.7,31 We explicitly addressed the issue of selection bias by using a propensity score approach to control for differences in the likelihood of patients being admitted to a cardiology service (see Appendix E1, available online at http://www.annemergmed.com).32,33 Propensity methods have been effectively used in observational studies to compare outcomes between generalist- and specialist-treated patients.15,34
We used logistic regression to compute the odds ratio (and 95% confidence interval [CI]) associated with admission to cardiology for all dichotomous outcomes, after adjustment for quintile of propensity score, quintile of Acute Cardiac Ischemia Time-Insensitive Predictive Instrument (ACI-TIPI) score, intervention period, and any unbalanced covariates. The ACI-TIPI computes a given patient’s probability (on a 0 to 100 scale) of having acute coronary syndrome according to age, sex, presenting symptoms, and details of the ECG.35,36 We used linear regression to assess the relationship between admission to cardiology and health-related quality-of-life scores, except for SF-20 role function (which was dichotomized at the median because these data were highly skewed). Because some of the observed patterns of care could have been triggered by between-group differences in the proportion of patients with diagnosed acute coronary syndrome, we also repeated the above analyses in the subgroup of patients without confirmed acute coronary syndrome (eg, chest pain of unknown cause). In our primary analysis, there are 8 comparisons of interest; we test each of these using a per-comparison α of .05.
To confirm the results of the above analysis, we also performed a matched analysis in which each patient who was admitted to a cardiology service was matched by propensity score to one who was admitted to a noncardiology service. Matching on propensity score allows one to control for many background random covariates simultaneously by matching on a single variable.33 Thus, it provides a more intuitive comparison of outcomes between the 2 groups because the values have effectively been adjusted for the covariates used to create the propensity score. We included only those matches that were within 0.25 SD of the logit of the propensity score.37 Once a match was identified, we removed the matched pair from the sample and then repeated the process. For this analysis, we checked for balance of covariates by calculating the standardized difference, di, in covariate means between matched pairs:
(for continuous variables)
where xci and xnci are the sample means in the cardiology and noncardiology groups of the ith covariate, respectively, and s2ci and s2nci are the corresponding sample variances; pci and pnci the sample proportions in the cardiology and noncardiology groups of the ith covariate, respectively. Small absolute values of di (<10%) support the assumption of balance between treatment groups (Table 1).33,38
Table 1.
Characteristics of patients who were admitted to cardiology versus noncardiology services.
| Characteristic | Full sample | Matched patients | ||||
|---|---|---|---|---|---|---|
| Cardiology Service (n=372) | Non-Cardiology Service (n=172) | di-value* | Cardiology Service (n=156) | Non-Cardiology Service (n=156) | di-value* | |
| Mean age (sd) | 59.6 | 61.3 | 12.3 | 60.1 | 61.3 | 8.8 |
| Gender (% male) | 56 | 45 | −20.7 | 49 | 45 | −7.7 |
| Race (% non-white) | 20 | 26 | 14.2 | 20 | 23 | 7.8 |
| Married (%) | 55 | 44 | −22.0 | 49 | 46 | −7.7 |
| Insurance (%) | ||||||
| Commercial/indemnity | 23 | 20 | −6.7 | 21 | 21 | 0.0 |
| HMO/PPO | 44 | 44 | 0.7 | 47 | 46 | −3.8 |
| Medicaid | 13 | 20 | 18.5 | 13 | 18 | 14.2 |
| Self-pay/uninsured | 8 | 3 | −17.7 | 5 | 4 | −6.2 |
| Symptoms (%) | ||||||
| Chest pain | 90 | 74 | −41.7 | 81 | 78 | −7.9 |
| Dyspnea | 59 | 67 | 16.0 | 62 | 64 | 4.0 |
| Face or neck pain | 27 | 17 | −25.6 | 19 | 18 | −1.7 |
| Heartburn | 11 | 5 | −22.1 | 5 | 6 | 2.8 |
| Abdominal pain | 10 | 13 | 8.9 | 12 | 13 | 3.9 |
| Nausea | 36 | 27 | −19.3 | 27 | 27 | 0.0 |
| Dizziness | 44 | 44 | 0.7 | 44 | 44 | 1.3 |
| Ongoing symptoms in ED | 75 | 82 | 17.0 | 80 | 80 | 0.0 |
| Activity level at onset – light | 20 | 22 | 6.1 | 24 | 22 | −4.6 |
| Activity level at onset – moderate-strenuous | 13 | 5 | −28.4 | 4 | 5 | 6.2 |
| Any relief from nitroglycerin | 52 | 30 | −46.9 | 42 | 33 | −18.6 |
| Any relief from rest | 36 | 37 | 2.5 | 37 | 37 | −1.3 |
| Nocturnal symptoms | 29 | 26 | −8.3 | 26 | 26 | −1.5 |
| Medical history (%) | ||||||
| Hypertension | 65 | 67 | 4.4 | 64 | 66 | 4.0 |
| Diabetes mellitus | 24 | 28 | 10.4 | 24 | 26 | 4.4 |
| Hypercholesterolemia | 53 | 48 | −9.4 | 51 | 49 | −3.8 |
| Smoking - current | 24 | 20 | −11.3 | 19 | 19 | 0.0 |
| Smoking - former | 36 | 40 | 7.8 | 42 | 40 | −3.9 |
| Family history of CAD† | 26 | 17 | −22.5 | 22 | 19 | −9.5 |
| Myocardial infarction | 27 | 23 | −9.1 | 26 | 23 | −6.0 |
| Coronary artery disease | 41 | 31 | −20.3 | 32 | 32 | 0.0 |
| Congestive heart failure | 17 | 23 | 14.4 | 16 | 20 | 10.0 |
| Stroke | 6 | 4 | −9.6 | 6 | 4 | −5.8 |
| History of affective disorder | 20 | 17 | −6.3 | 17 | 18 | 3.4 |
| Mean comorbidity score (sd)‡ | 5.2 | 5.7 | 15.2 | 5.1 | 5.5 | 11.5 |
| Medication history (%) | ||||||
| Beta blockers | 27 | 27 | −1.5 | 31 | 28 | −7.0 |
| Calcium-channel blockers | 22 | 23 | 2.8 | 23 | 22 | −3.1 |
| ACE inhibitors | 26 | 31 | 13.0 | 27 | 31 | 8.5 |
| Angiotensin receptor blockers | 9 | 6 | −13.6 | 6 | 6 | 0.0 |
| Warfarin | 11 | 10 | −2.9 | 10 | 11 | 4.2 |
| Aspirin | 42 | 38 | −7.9 | 41 | 37 | −7.9 |
| Nitrates | 27 | 18 | −21.3 | 19 | 19 | 0.0 |
| Statin | 28 | 26 | −4.6 | 27 | 27 | 0.0 |
| Physical findings (%) | ||||||
| Rales present | 13 | 24 | 30.6 | 18 | 21 | 6.5 |
| Pulmonary edema on chest x-ray | 8 | 16 | 24.7 | 11 | 13 | 5.9 |
| Systolic blood pressure§ | 147 | 143 | −13.0 | 148 | 143 | −16.5 |
| Abnormal troponin (%) | 16 | 8 | −26.0 | 8 | 8 | 2.4 |
| Abnormal EKG findings (%) | ||||||
| Pathologic Q-waves | 13 | 9 | −12.3 | 12 | 10 | −6.1 |
| ST-segment depression (≥1 mm) | 8 | 3 | −20.9 | 3 | 3 | 0.0 |
| ST-segment elevation (≥1 mm) | 2 | 2 | −4.7 | 3 | 2 | −4.3 |
| T-wave inversion (≥1 mm) | 16 | 13 | −8.5 | 14 | 15 | 1.8 |
| ACI-TIPI score (0–100)** | 26.5 (16) | 20.2 (14) | −41.0 | 24.6 (16) | 20.0 (14) | −30.8 |
HMO, Health maintenance organization; PPO, preferred provider organization; ACE, angiotensin-converting enzyme; CAD, coronary artery disease.
di corresponds to the standardized difference in covariate means or proportions between comparison groups. Small absolute values of di (≤ 10%) support the assumption of balance between comparison groups (values of di >10% are shown in bold).
Family history of premature CAD defined as 1 or more family members with onset of CAD < 55 years old.
Seattle Index of Comorbidity score.
At time of initial triage (mm Hg).
ACI-TIPI = Acute Cardiac Ischemia Time-Insensitive Predictive Instrument. The ACI-TIPI computes a given patient’s probability (on a 0–100 scale) of having ACS based on age, sex, presenting symptoms and details of the ECG.
The sample size of 372 cardiology and 172 noncardiology patients allowed us to detect the changes shown below with at least 80% power (2-sided α=.05):
19%, 14%, and 18% increases in the proportion of patients who received aspirin, heparin, and β-blocker during hospitalization, respectively
15% increase in the proportion of patients who received noninvasive testing
6% increase in cardiac catheterizations
8% decrease in ED revisits or rehospitalizations
6- and 7-point increases in Duke Activity Status Index and SF-20 physical function scores, respectively
For these calculations, we accounted for clustering within each admitting physician by use of the intraclass correlation coefficient for each outcome.30 We had insufficient power to detect a decrease in the occurrence of adverse events in cardiology patients and thus consider this variable to be a secondary outcome.
Statistical analyses were performed using STATA, version 8.0 (StataCorp, College Station, TX). A SAS (SAS Institute, Inc., Cary, NC) macro (IVEware) was used for multiple imputation of missing emergency physician data39; we used the MICOMBINE routine in STATA to combine imputed data sets (5 in total). In all analyses, we corrected for clustering (by admitting physician) with robust estimates of variance.40,41
RESULTS
Figure 1 shows the derivation of the analysis sample. Noncardiology patients were admitted to the following services: general internal medicine (n=80), internal medicine subspecialties other than cardiology (n=45), and family practice (n=47). According to data available at initial ED presentation, patients initially admitted to cardiology showed a higher mean predicted probability of acute cardiac ischemia than those admitted to a noncardiology service (27% and 20%, respectively). Overall, 41% and 17% of patients who were admitted to cardiology versus noncardiology service beds had confirmed acute coronary syndrome (17% and 6% had acute myocardial infarction, respectively). Of those who received noninvasive testing, however, the proportion with positive test results was similar in cardiology and noncardiology patients (21.8% versus 19.5%, respectively).
Characteristics of Study Participants
Cardiology patients were more likely to be men and married and were less likely to be covered by Medicaid (Table 1). A greater proportion of cardiology patients presented with typical acute coronary syndrome symptoms (chest pain, neck/jaw pain) and were more likely to have developed acute coronary syndrome symptoms with exertion. Cardiology patients were more likely to have obtained partial or full relief from sublingual nitroglycerin and were more likely to have a history of known coronary artery disease (41% versus 31%). Number of medical comorbidities and history of depression or anxiety disorders were similar in both groups.
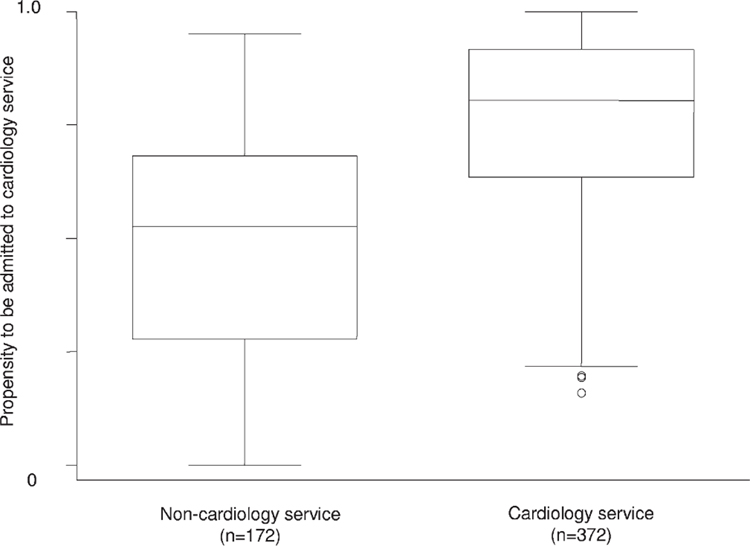
As expected, patients initially admitted to cardiology were also more likely to have abnormal ECG findings (ST-segment depression) and an abnormal troponin level; noncardiology patients were more likely to have signs of congestive heart failure. Inclusion of all variables (except ACI-TIPI score) in a multivariable logistic regression model predicting admission to cardiology showed a c-statistic of .80 and excellent model calibration (P=.75, Hosmer-Lemeshow goodness-of-fit test). There was considerable overlap between propensity scores for patients who were initially admitted to cardiology or to a noncardiology service (Figure 2). Matched analysis showed generally excellent covariate balance (with the exception of the variables highlighted in Table 1, last column).
Figure 2.
Box-and-whisker plot of propensity scores for patients initially admitted to a noncardiology or cardiology service.
Main Results
A substantial proportion of patients in this study did not receive aspirin for possible acute coronary syndrome or diagnostic evaluation for cardiac ischemia. Cardiology patients were more likely to receive aspirin (71% versus 49%), heparin (28% versus 20%), and β-blockers (38% versus 29%), but none of these differences were statistically significant after risk adjustment (Table 2, column 4). Cardiology patients were more likely to receive noninvasive testing (73% versus 54%; odds ratio [OR] 2.5; 95% CI 1.7 to 3.8) and cardiac catheterization (33% versus 6%; OR 3.9; 95% CI 1.7 to 8.9) during 30-day follow-up. Similar results were observed in the matched analysis (Table 2, last column) and in the subgroup of 360 patients without confirmed acute coronary syndrome (Table 3).
Table 2.
Association between initial cardiology admission and use of recommended medications, use of diagnostic procedures for coronary artery disease, follow-up care, and adverse events (inpatient complications or death) during 30-day follow-up.*
| Complete Data |
Propensity-Matched Data |
|||||
|---|---|---|---|---|---|---|
| Process Measure | Cardiology Service (n=372) | Noncardiology Service (n=172) | Adjusted OR (95% CI)† | Cardiology Service (n=156) | Noncardiology Service (n=156) | Adjusted OR (95% CI)‡ |
| Inhospital medication, % | ||||||
| Aspirin use | 71 | 49 | 1.2 (0.6–2.4) | 56 | 53 | 0.95 (0.5–1.9) |
| Heparin use§ | 28 | 20 | 1.1 (0.6–2.2) | 20 | 20 | 0.93 (0.5–1.9) |
| β-Blocker use§ | 38 | 29 | 1.2 (0.6–2.6) | 31 | 29 | 1.0 (0.4–2.3) |
| Diagnostic evaluation, % | ||||||
| Noninvasive testing | 73 | 54 | 2.5 (1.7–3.8) | 72 | 55 | 2.0 (1.4–3.0) |
| Cardiac catheterization | 33 | 6 | 3.9 (1.7–8.9) | 21 | 6 | 3.2 (1.3–7.4) |
| Subsequent care, % | ||||||
| ED revisit or readmission | 15 | 18 | 0.86 (0.5–1.6) | 13 | 19 | 0.79 (0.4–1.5) |
| Outpatient follow-up | 71 | 74 | 0.96 (0.6–1.5) | 74 | 75 | 0.84 (0.5–1.4) |
| Inpatient complications or 30-day mortality | 2.4 | 1.7 | 1.9 (0.5–7.7) | 3.2 | 1.9 | 2.4 (0.6–10) |
Reference group is noncardiology patients.
Adjusted for propensity of being admitted to cardiology, comorbidity score, predicted probability of acute cardiac ischemia, and intervention period.
Adjusted for covariates with differences that persisted after matching (Medicaid insurance, symptom relief from nitroglycerin, history of congestive heart failure, comorbidity score, initial systolic blood pressure), predicted probability of acute cardiac ischemia, and intervention period.
Limited to 511 patients with intermediate to high characteristics (as defined by the Agency for Healthcare Policy and Research guideline or elevated troponin levels).
Table 3.
Association between initial cardiology admission and process of care in the subgroup of patients without confirmed ACS.
| Cardiology Service (n=218) | Noncardiology Service (n=142) | Adjusted OR (95% CI)* | |
|---|---|---|---|
| Inhospital medication, % | |||
| Aspirin use | 39 | 35 | 1.0 (0.4–2.6) |
| Heparin use | 14 | 15 | 0.8 (0.4–1.7) |
| β-Blocker use | 27 | 21 | 1.3 (0.5–3.1) |
| Ca2+-channel blocker use | 5 | 4 | 1.6 (0.4–5.7) |
| Diagnostic evaluation, % | |||
| Noninvasive testing | 78 | 51 | 3.3 (2.0–5.2) |
| Cardiac catheterization | 10 | 1 | 6.9 (1.0–47) |
| Subsequent care, % | |||
| ED revisit or readmission | 11 | 16 | 1.1 (0.6–2.1) |
| Outpatient follow-up | 69 | 70 | 1.1 (0.7–1.8) |
Adjusted for propensity of being admitted to cardiology, comorbidity score, predicted probability of acute cardiac ischemia, and intervention period. Reference group is noncardiology patients.
Although cardiology patients were more likely to receive guideline-concordant evaluation for coronary artery disease, the proportion of cardiology patients who revisited the ED or were readmitted during follow-up did not significantly differ from that of noncardiology patients (OR 0.81; 95% CI 0.4 to 1.5). In addition, there was no meaningful difference in the combined endpoint of inpatient complications or 30-day mortality, which was uncommon: 9 of 372 (2.4%) versus 3 of 172 (1.7%) in the cardiology and noncardiology groups, respectively. Similar results were obtained in the matched analysis.
With regard to functional status, there was a trend toward higher (better) SF-20 physical function and bodily pain scores in cardiology versus noncardiology patients (Table 4). Mean Duke Activity Status Index scores were similar in both groups, however, and the 2 groups showed no significant differences across the remaining SF-20 domains, including role function. We also did not observe any clinically important health-related quality-of-life differences between cardiology and noncardiology patients within acute coronary syndrome and non–acute coronary syndrome subgroups (data not shown).
Table 4.
Modified SF-20 and Duke Activity Status Index scores for patients initially admitted to cardiology and noncardiology services at 30-day follow-up. Higher scores indicate better functional status.
| Complete Data† |
Propensity-Matched Data‡ |
|||||
|---|---|---|---|---|---|---|
| HRQOL Domain Mean (SD)* | Cardiology Service | Noncardiology Service | Adjusted Mean Difference (95% CI)§ | Cardiology Service | Noncardiology Service | Adjusted Mean Difference (95% CI)ǁ |
| Physical function | 78 (20) | 73 (22) | 4.0 (−0.9 to 8.9) | 80 (18) | 73 (21) | 4.1 (−0.2 to 8.4) |
| Pain | 66 (26) | 63 (28) | 5.0 (−1.5 to 11) | 69 (26) | 63 (28) | 5.7 (−1.1 to 13) |
| General health perception | 55 (26) | 54 (27) | −0.7 (−7.0 to 5.5) | 57 (25) | 55 (27) | −0.3 (−6.9 to 6.3) |
| Social | 81 (27) | 78 (28) | −0.4 (−8.2 to 7.4) | 81 (27) | 79 (28) | −0.1 (−8.1 to 8.3) |
| Mental health | 75 (18) | 74 (17) | −0.2 (−4.9 to 4.5) | 75 (19) | 74 (17) | 0.4 (−4.4 to 5.2) |
| DASI score | 36 (18) | 32 (19) | 1.7 (−1.8 to 5.1) | 36 (18) | 33 (19) | 0.6 (−3.1 to 4.2) |
HRQOL, Health-related quality of life; DASI, Duke Activity Status Index.
Role function was dichotomized and analyzed with logistic regression (see text for results).
Based on all patients with available SF-20 and covariate data (n=490–496, varying across SF-20 subscales).
Based on matched patients with available SF-20 and covariate data (n=280–286, varying across SF-20 subscales).
Mean differences between groups were calculated using linear regression to adjust for propensity of being admitted to cardiology, comorbidity score, predicted probability of acute cardiac ischemia, and intervention period.
Adjusted for covariates with differences that persisted after matching (Medicaid insurance, symptom relief from nitroglycerin, history of congestive heart failure, comorbidity score, initial systolic blood pressure), predicted probability of acute cardiac ischemia, and intervention period.
LIMITATIONS
First, our sample size did not allow us to detect small but potentially meaningful differences in the occurrence of adverse cardiovascular events, because of the relative rarity of these outcomes; larger differences in the occurrence of adverse cardiovascular events may have become manifest only with longer follow-up.42 Second, this was a cross-sectional analysis and we did not collect data on baseline functional status at initial evaluation. Third, the study findings could still be explained by residual confounding, despite our attempt to control for selection bias. For example, we did not collect information on severity of comorbid conditions or patient preferences for aggressive cardiovascular care.31 Moreover, propensity scores can account for only measured covariates; patients admitted to cardiology may be different from those who are admitted to noncardiology beds across 1 or more unmeasured covariates. Fourth, we cannot rule out the possibility that the difference in cardiac catheterization between groups may be related to differences in interpretation of test results (and different thresholds for pursuing coronary angiography). Finally, the results of this trial may not be generalizable to nonteaching EDs or to hospitals with chest pain observation units. Patterns of ED triage and admission may differ in nonteaching hospitals because of differences in patient acuity (or case mix) and reduced access to cardiology care in some nonteaching hospitals.
DISCUSSION
The improved performance of cardiologists has been attributed in part to better knowledge of cardiovascular conditions and treatment guidelines,16,47 an increased caseload of acute coronary syndrome patients among cardiologists,12,14 and a more aggressive approach to diagnostic evaluation.6,7 As in previous comparative studies of acute coronary syndrome management,7,31 we found that patients admitted to a cardiology service were more likely to be men, to have known CAD, and to present with typical acute coronary syndrome symptoms. Even after adjustment for case mix, however, we found that cardiology patients were significantly more likely than noncardiology patients to undergo diagnostic testing for CAD (as recommended by American College of Cardiology/American Heart Association guidelines). This finding is consistent with previous studies of hospitalized patients with unstable angina8 and patients admitted with suspected non–ST elevation acute coronary syndrome.9,48 Unlike previous studies,8,9,48 however, we did not identify any significant differences in the use of guideline-recommended therapies (including aspirin, heparin, and β-blockers).
Does improved diagnostic evaluation warrant admission to a cardiology service for patients with possible acute coronary syndrome? Although cardiology patients tended to require subsequent acute care less often than noncardiology patients in our matched analysis, our findings did not attain statistical significance and are consistent with those of Shaver et al,49 who showed no impact of diagnostic testing during the initial hospitalization on need for follow-up ED care. In contrast, other investigators have also shown a lower rate of return visits in patients with possible acute coronary syndrome who receive myocardial perfusion imaging or coronary angioplasty during their index hospitalization (versus those who do not),50,51 which has been attributed to reduced diagnostic uncertainty and anxiety related to acute coronary syndrome symptoms after diagnostic testing for CAD.52 Moreover, our results suggest that cardiologists may be overly aggressive in their care of low-risk patients,9 as shown by their greater use of cardiac catheterization in patients without confirmed acute coronary syndrome, and serve as a reminder of the potential for iatrogenic injury with cardiology care.53,54 Despite these differences in use of diagnostic procedures, admission to a cardiology service did not translate into a significantly reduced incidence of adverse events or better functional status at 30-day follow-up.
Our results were similar to those of Bosch et al,48 who also found no differences between cardiology and internal medicine inpatients with regard to nonfatal acute myocardial infarction or death, after risk adjustment. Other investigators, however, have shown a tendency toward increased mortality in internal medicine versus cardiology inpatients who were discharged with a diagnosis of unstable angina (4.0% versus 1.8%; P=.06); these findings were attributed to less frequent use of recommended medical therapies and angioplasty in the internal medicine group.8 In an analysis of the CRUSADE registry, inpatient mortality was significantly lower for acute coronary syndrome patients who were treated by cardiologists compared with those treated by noncardiologists (adjusted OR 0.75; 95% CI 0.6 to 0.9).55 These differences in clinical outcome most likely reflect differences in the underlying risk of adverse events across study samples; for example, the 30-day mortality rate was less than 1% in the current study versus 3% to 5% in studies of patients with diagnosed acute coronary syndrome.8,55
Another possible explanation for the lack of difference in clinical outcomes between groups is the use of cardiology consultation in patients initially admitted to a noncardiology service. Although we did not specifically assess whether patients had received formal or informal “curbside” consultation, it was routine practice at both study hospitals to obtain a cardiology consultation (and in some cases to transfer) those patients who “ruled in” for myocardial injury or had an abnormal noninvasive test result (suggestive of reversible myocardial ischemia). Cardiology consultation would tend to minimize differences between groups in processes of care (eg, use of inpatient medications), need for subsequent acute care, and clinical outcomes. Only 2 noncardiology patients were transferred to (and discharged from) the cardiology service during their hospitalization; our results showed minimal change after exclusion of these patients from the analysis.
Our results suggest that ED patients who require inpatient evaluation of possible acute coronary syndrome do not experience worsened short-term outcomes if admitted to a noncardiology service bed. These findings should be confirmed in larger comparative studies with longer follow-up because even small differences in outcomes between generalists and cardiologists might have important implications for public health. By performing additional risk stratification in the ED before making a final triage decision,43,44 emergency physicians can further identify patients who are more likely to benefit from inpatient cardiology care (and a generally more aggressive approach to diagnostic testing). Conversely, emergency physicians are well positioned to identify patients with multiple comorbid conditions and those with less clear-cut presentations, who may be more likely to benefit from generalist care.45 Future studies should also evaluate collaborative systems of care in which the involvement of cardiologists and generalists varies according to the hospitalized patient’s underlying risk of adverse cardiovascular (and noncardiovascular) events.46
Editor’s Capsule Summary.
What is already known on this topic
Emergency physicians have to choose whether to admit patients to specialty or generalist services.
What question this study addressed
Whether patients with “possible” acute coronary syndromes have different outcomes according to admitting service.
What this study adds to our knowledge
The 372 patients admitted to cardiologist services received more tests but did not have better outcomes than the 172 patients admitted to generalist services.
How this might change clinical practice
Practice should not be changed (in either direction) according to this small study at 2 institutions.
Acknowledgments
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article, that might create any potential conflict of interest. See the Manuscript Submission Agreement in this issue for examples of specific conflicts covered by this statement. Funded by the Agency for Healthcare Research and Quality (R01 HS10466), Robert Wood Johnson Foundation Generalist Physician Faculty Scholars Program (Dr. Katz), with supplemental support from the University of Wisconsin Department of Medicine.
APPENDIX E1. Development of propensity models.
To derive the propensity score, we first identified a set of variables that could potentially influence the decision to admit patients to a cardiology service, based on previous literature and expert opinion (shown in Table 1). We then fitted a logistic regression model to predict admission to cardiology in the data set. The independent variables in the propensity models included sociodemographic variables, symptoms associated with ED presentation, physical findings, cardiovascular risk factors, current use of cardiovascular medications, comorbid medical conditions,22 history of depression or anxiety (or current use of medication for these conditions), EKG variables, biomarker results, and cardiovascular medications received in the ED.
We assessed accuracy of the propensity models by computing the c-statistic (which is equivalent to the area under the receiver operating characteristic curve).56 Model calibration was evaluated using the Hosmer-Lemeshow goodness of fit test.57 To assess whether the propensity score helped to achieve balance in the covariates, we assessed whether each covariate remained a statistically significant predictor of cardiology admission, after adjustment for propensity score quintile in logistic regression models. Those covariates that remained significant predictors of triage disposition (at P<.10) after adjustment for propensity score quintile were included in all models of outcome. We also assessed balance of the comparison groups by checking for differences in the predicted probability of acute cardiac ischemia (ACI-TIPI score)35 after adjusting for propensity score in linear regression models.
Footnotes
The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
Presented as preliminary results at the Society of General Internal Medicine annual meeting, May 2003, Washington, DC.
Contributor Information
David A. Katz, Departments of Medicine and Epidemiology, University of Iowa Carver College of Medicine and College of Public Health, Iowa City, IA; Center for Research in the Implementation of Innovative Strategies in Practice, Iowa City VA Medical Center, Iowa City, IA.
Tom P. Aufderheide, Department of Emergency Medicine, Medical College of Wisconsin, Milwaukee, WI.
Mark Bogner, Section of Emergency Medicine, University of Wisconsin, Madison, WI.
Peter S. Rahko, Division of Cardiology, University of Wisconsin, Madison, WI.
Stephen L. Hillis, Center for Research in the Implementation of Innovative Strategies in Practice, Iowa City VA Medical Center, Iowa City, IA.
Harry P. Selker, Institute for Clinical Research and Health Policy Studies, Tufts-New England Medical Center, Boston, MA.
REFERENCES
- 1.Derlet R Overcrowding in emergency departments: increased demand and decreased capacity. Ann Emerg Med 2002;39:430–32. [DOI] [PubMed] [Google Scholar]
- 2.Asplin BR, Magid DJ, Rhodes KV, et al. A conceptual model of emergency department crowding. Ann Emerg Med 2003;42:173–180. [DOI] [PubMed] [Google Scholar]
- 3.Weiss SJ, Derlet R, Arndahl J, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS). Acad Emerg Med 2004;11:38–50. [DOI] [PubMed] [Google Scholar]
- 4.Cowan RM, Trzeciak S. Clinical review: emergency department crowding and the potential impact on the critically ill. Crit Care. 2005;9:291–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nourjah P National Ambulatory Medical Care Survey: 1997 Emergency Department Summary. Advance Data from Vital and Health Statistics; No. 304 Hyattsville, MD: National Center for Health Statistics, 1999. [PubMed] [Google Scholar]
- 6.Jollis J, DeLong E, Peterson E, et al. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med 1996;335:1880–1887. [DOI] [PubMed] [Google Scholar]
- 7.Go A, Rao R, Dauterman K, et al. A systematic review of the effects of physician specialty on the treatment of coronary disease and heart failure in the United States. Am J Med 2000; 108:216–226. [DOI] [PubMed] [Google Scholar]
- 8.Schreiber T, Elkhatib A, Grines C, et al. Cardiologist versus internist management of patients with unstable angina: treatment patterns and outcomes. J Am Coll Cardiol 1995;26:577–582. [DOI] [PubMed] [Google Scholar]
- 9.Reis S, Holubkov R, Zell K, et al. Unstable angina: specialty-related disparities in implementation of practice guidelines. Clin Cardiol 1998;21:207–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grumbach K, Bodenheimer T. A primary care home for Americans: putting the house in order. JAMA 2002;288:889–893. [DOI] [PubMed] [Google Scholar]
- 11.Casale P, Jones J, Wolf F, et al. Patients treated by cardiologists have a lower in-hospital mortality for acute myocardial infarction. J Am Coll Cardiol 1998;32:885–889. [DOI] [PubMed] [Google Scholar]
- 12.Nash I, Corrato R, Dlutowski M, et al. Generalist versus specialist care for acute myocardial infarction. Am J Cardiol 1999;83:650–654. [DOI] [PubMed] [Google Scholar]
- 13.Frances C, Go A, Dauterman K, et al. Outcome following acute myocardial infarction: are differences among physician specialties the result of quality of care or case mix? Arch Intern Med 1999; 159:1429–1436. [DOI] [PubMed] [Google Scholar]
- 14.Norcini JJ, Kimball HR, Lipner RS. Certification and specialization: do they matter in the outcome of acute myocardial infarction? Acad Med 2000;75:1193–1198. [DOI] [PubMed] [Google Scholar]
- 15.Ayanian J, Landrum M, Guadagnoli E, et al. Specialty of ambulatory care physicians and mortality among elderly patients after myocardial infarction. N Engl J Med 2002;347:1678–1686. [DOI] [PubMed] [Google Scholar]
- 16.Ayanian J, Guadagnoli E, McNeil B, et al. Treatment and outcomes of acute myocardial infarction among patients of cardiologists and generalist physicians. Arch Intern Med 1997; 157:2570–2576. [PubMed] [Google Scholar]
- 17.Frances C, Shlipak MG, Noguchi H, et al. Does physician specialty affect the survival of elderly patients with myocardial infarction? Health Serv Res 2000;35:1093–1116. [PMC free article] [PubMed] [Google Scholar]
- 18.Chen J, Radford MJ, Wang Y, et al. Care and outcomes of elderly patients with acute myocardial infarction by physician specialty: the effects of comorbidity and functional limitations. Am J Med 2000;108:460–469. [DOI] [PubMed] [Google Scholar]
- 19.Katz D, Aufderheide T, Bogner M, et al. Impact of unstable angina guidelines in the triage of emergency department patients with possible acute coronary syndrome. Med Decis Making 2006;26: 606–616. [DOI] [PubMed] [Google Scholar]
- 20.Katz D, Williams G, Brown R, et al. Emergency physicians’ fear of malpractice in evaluating patients with possible acute cardiac ischemia. Ann Emerg Med 2005;46:525–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cannon C, Battler A, Brindis R, et al. ACC key elements and data definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes: a report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee). J Am Coll Cardiol 2001;38:2114–2130. [DOI] [PubMed] [Google Scholar]
- 22.Fan V, Au D, Heagerty P, et al. Validation of case-mix measures derived from self-reports of diagnoses and health. J Clin Epidemiol 2002;55:371–380. [DOI] [PubMed] [Google Scholar]
- 23.Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med 1996;27:305–308. [DOI] [PubMed] [Google Scholar]
- 24.The Joint European Society of Cardiology/American College of Cardiology Committee. Myocardial infarction redefined—A consensus document of the Joint European Society of Cardiology/American College of Cardiology committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000;36: 959–969. [DOI] [PubMed] [Google Scholar]
- 25.Hollander J, Blomkalns A, Brogan G, et al. Standardized reporting guidelines for studies evaluating risk stratification of emergency department patients with potential acute coronary syndromes. Ann Emerg Med 2004;44:589–598. [DOI] [PubMed] [Google Scholar]
- 26.Braunwald E, Brown J, Brown L, et al. Unstable Angina: Diagnosis and Management Clinical Practice Guideline Number 10 Rockville, MD: Agency for Health Care Policy and Research, US Public Health Service, US Department of Health and Human Services; 1994. [Google Scholar]
- 27.Stewart A, Ware J. Measuring Functioning and Well-being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992. [Google Scholar]
- 28.Hlatky M, Boineau R, Higginbotham M, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol 1989;64:651–654. [DOI] [PubMed] [Google Scholar]
- 29.Schafer JL. Book Analysis of Incomplete Multivariate Data. New York, NY: Chapman & Hall; 1997. [Google Scholar]
- 30.Donner A, Klar N. Book Design and Analysis of Cluster Randomization Trials in Health Research. London, England: Arnold; 2000. [Google Scholar]
- 31.Hartz A, James PA. A systematic review of studies comparing myocardial infarction mortality for generalists and specialists: lessons for research and health policy. J Am Board Fam Med 2006;19:291–302. [DOI] [PubMed] [Google Scholar]
- 32.Rubin D Estimating causal effects from large data sets using propensity scores. Ann Intern Med 1997;127:757–763. [DOI] [PubMed] [Google Scholar]
- 33.D’Agostino R Propensity score methods for bias reduction in the comparison of a treatment or a non-randomized control group. Stat Med 1998;17:2265–2281. [DOI] [PubMed] [Google Scholar]
- 34.Regueiro CR, Hamel MB, Davis RB, et al. A comparison of generalist and pulmonologist care for patients hospitalized with severe chronic obstructive pulmonary disease: resource intensity, hospital costs, and survival. Am J Med 1998;105:366–372. [DOI] [PubMed] [Google Scholar]
- 35.Selker H, Griffith J, D’Agostino R. A tool for judging coronary care unit admission appropriateness valid for both real-time and retrospective use: a time-insensitive predictive instrument (TIPI) for acute cardiac ischemia: a multicenter study. Med Care. 1991; 29:610–627. [DOI] [PubMed] [Google Scholar]
- 36.Selker HP, Beshansky JR, Griffith JL, et al. Use of the Acute Cardiac Ischemia Time-Insensitive Predictive Instrument (ACI-TIPI) to assist with triage of patients with chest pain or other symptoms suggestive of acute cardiac ischemia. A multicenter, controlled clinical trial. Ann Intern Med 1998;129:845–855. [DOI] [PubMed] [Google Scholar]
- 37.Rosenbaum P, Rubin D. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat 1985;39:33–38. [Google Scholar]
- 38.Normand S-LT, Landrum M, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol 2001;54:387–398. [DOI] [PubMed] [Google Scholar]
- 39.Raghunathan TE, Solenberger PW, Van Hoewyk J. IVEware: Imputation and Variance Estimation Software: Survey Methodology Program. Ann Arbor, MI: Survey Research Center, Institute for Social Research, University of Michigan; 2005. [Google Scholar]
- 40.Huber P The Behavior of Maximum Likelihood Estimates under Non-Standard Conditions Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability, Berkeley, CA: University of California Press; Vol. 1 1967. [Google Scholar]
- 41.Rogers W Regression standard errors in clustered samples. Stata Tech Bull 1993;13:19–23. [Google Scholar]
- 42.Manini AF, Gisondi MA, van der Vlugt TM, et al. Adverse cardiac events in emergency department patients with chest pain six months after a negative inpatient evaluation for acute coronary syndrome. Acad Emerg Med 2002;9:896–902. [DOI] [PubMed] [Google Scholar]
- 43.Farkouh M, Smars P, Reeder G, et al. A clinical trial of a chest-pain observation unit for patients with unstable angina. N Engl J Med 1998;339:1882–1888. [DOI] [PubMed] [Google Scholar]
- 44.Goodacre S, Nicholl J, Dixon S, et al. Randomised controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ 2004;328:254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smetana G, Landon B, Bindman A, et al. A comparison of outcomes resulting from generalist vs specialist care for a single discrete medical condition: a systematic review and methodologic critique. Arch Intern Med 2007;167:10–20. [DOI] [PubMed] [Google Scholar]
- 46.Ayanian JZ. Generalists and specialists caring for patients with heart disease: united we stand, divided we fall. Am J Med 2000; 108:259–261. [DOI] [PubMed] [Google Scholar]
- 47.Hlatky M, Cotugno H, Mark D, et al. Trends in physician management of uncomplicated acute myocardial infarction, 1970 to 1987. Am J Cardiol 1988;61:515–518. [DOI] [PubMed] [Google Scholar]
- 48.Bosch X, Verbal F, López de Sá E, et al. Differences in the management and prognosis of patients with non-ST segment elevation acute coronary syndrome according to the department of initial admission. Rev Esp Cardiol 2004;57:283–290. [PubMed] [Google Scholar]
- 49.Shaver K, Marsan RJ Jr, Sease K, et al. Impact of a negative evaluation for underlying coronary artery disease on one-year resource utilization for patients admitted with potential acute coronary syndromes. Acad Emerg Med 2004;11:1272–1277. [DOI] [PubMed] [Google Scholar]
- 50.Shoyeb A, Bokhari S, Sullivan J, et al. Value of definitive diagnostic testing in the evaluation of patients presenting to the emergency department with chest pain. Am J Cardiol 2003;91: 1410–1414. [DOI] [PubMed] [Google Scholar]
- 51.de Filippi CR, Rosanio S, Tochhi M, et al. Randomized comparison of a strategy of predischarge coronary angiography versus exercise testing in low-risk patients in a chest pain unit: in-hospital and long-term outcomes. J Am Coll Cardiol 2001;37: 2024–2049. [DOI] [PubMed] [Google Scholar]
- 52.Mushlin A, Kern L, Paris M, et al. The value of diagnostic information to patients with chest pain suggestive of coronary artery disease. Med Decis Making. 2005;25:149–157. [DOI] [PubMed] [Google Scholar]
- 53.Donohoe M Comparing generalist and specialty care: discrepancies, deficiencies, and excess. Arch Intern Med 1998; 158:1596–1608. [DOI] [PubMed] [Google Scholar]
- 54.Lewis W, Amsterdam E. Defining the role of chest pain units. J Am Coll Cardiol 2001;37:2050–2205. [DOI] [PubMed] [Google Scholar]
- 55.Peterson ED, Roe MT, Li Y, et al. Influence of physician specialty on care and outcome of acute coronary syndrome patients: results from CRUSADE. J Am Coll Cardiol 2003;41:A534. [Google Scholar]
- 56.Hanley J, McNeil B. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–843. [DOI] [PubMed] [Google Scholar]
- 57.Hosmer D, Lemeshow S. Applied Logistic Regression. New York, NY: Wiley; 1989. [Google Scholar]