Abstract
Background:
Many systematic reviews have compared the short-term outcomes of anterior cruciate ligment (ACL)reconstruction with hamstring and patellar tendon autograft,but few differences have been observed. The purpose of this meta-analysis was to compare the medium-term outcome of bone–patellar tendon–bone and hamstring tendon autograft for anterior cruciate ligament reconstruction in terms of clinical function, knee stability, postoperativecomplications, and osteoarthritis changes.
Methods:
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The PubMed, Embase, and the Cochrane Library databases were searched from inception to November 2, 2019. This meta-analysis included only randomized controlled trials that compared BPTB and HT autografts for ACL reconstruction with a 5-year minimum follow-up. The Cochrane Collaboration's risk-of-bias tool was used to estimate the risk-of-bias for all included studies. RevMan 5.3 software was used to performed statistical analysis of the outcomes.
Results:
Fifteen RCTs, involving 1298 patients (610 patients in the BPTB group and 688 patients in the HT group) were included. In terms of clinical function, no significant difference was found in the objective International Knee Documentation Committee score (OR = 0.94, 95%CI: 0.64–1.37, P = .75), Lysholm knee score (MD = −2.26, 95%CI: −4.56 to 0.05, P = .06), return to preinjury activity level (OR = 1.01, 95%CI: 0.67–1.52, P = .96), and Tegner activity level (OR = 0.03, 95%CI: −0.36 to 0.41, P = .89). There was no statistically significant difference in the Lachman test (OR = 0.86, 95%CI: 0.5–1.32, P = .50), pivot-shift test (OR = 0.68, 95%CI: 0.44–1.06, P = .09), and side-to-side difference (MD = −0.32, 95%CI: −0.81 to 0.16, P = .19). As for postoperative complications and OA changes, there were no statistically significant difference in flexion loss (OR = 1.09, 95%CI: 0.47–2.54, P = .85) and OA changes (OR = 0.76, 95%CI: 0.52–1.10, P = .15), but we found significant differences in favor of the HT group in the domains of kneeling pain (OR = 1.67, 95%CI: 1.04–2.69, P = .03), anterior knee pain (OR = 2.90, 95%CI: 1.46–5.77, P = .002), and extension loss (OR = 1.75, 95%CI: 1.12–2.75, P = .01). There was a significant difference in favor of the BPTB group in the domain of graft failure (OR = 0.59, 95%CI: 0.38–0.91, P = .02).
Conclusions:
Based on the results above, HT autograft is comparable with the BPTB autograft in terms of clinical function, postoperative knee stability, and OA changes, with a medium-term follow-up. The HT autograft for ACL reconstruction carries a lower risk of complications, such as anterior knee pain, kneeling pain, and extension loss, but an increased incidence of graft failure. Patients should be informed of the differences when deciding on graft choice with their physician.
Keywords: anterior cruciate ligament, bone–patellar tendon–bone, hamstring tendon autograft, meta-analysis
1. Introduction
Anterior cruciate ligament (ACL) injury is one of the most common orthopedic injuries, with an annual incidence of isolated injury of 68.6 per 100,000 person-years.[1] A long-term follow-up study showed that the risk of secondary meniscus tear (hazard ratio 18.0), osteoarthritis (OA, hazard ratio 14.2), and the need for total knee arthroplasty (hazard ratio 5.0) in patients without ligament reconstruction after ACL tear was significantly higher than in those without ACL tear.[2] Although there was no consensus on whether to choose conservative treatment or ACLR after ACL injury in many studies,[3,4] numerous young and active individuals still choose ACLR. Typically, bone–patellar tendon–bone (BPTB) and hamstring tendon (HT) autografts are chosen for ACLR.
Historically, the BPTB autograft was the gold standard for ACLR, as it allowed proper bone-to-bone tunnel healing, involved a short fixation distance, and provided excellent biomechanical strength.[5] Some studies have shown that BPTB autograft had the advantage of appropriate size, high durability, a low level of laxity, a higher incidence of return to sport activity, and a low rate of revision.[6–9] However, many patients have complained about donor site diseases, such as anterior knee pain, kneeling pain, and extension loss.[9–12] In recent years, HT autografts have been increasingly more frequently used in ACLR[13] because of its lower short-term donor site morbidity.[14,15] However, compared to BPTB autografts, HT autografts could lead to delayed graft incorporation, a decrease in knee stability, and significant flexor torque deficiency.[16–19]
Numerous RCTs have been conducted to analyze the relative merits of the two mentioned autografts, and a large amount of data published on this topic have been used for several meta-analyses.[9,14,11,15,20,21] However, most previously published meta-analyses did not investigate the use of BPTB and HT autografts for ACLR after a medium-term follow-up. Xie et al's meta-analysis included 12 RCTs and two prospective cohort studies that used a minimum of 5 years’ follow-up, and finally concluded that ACL reconstruction with BPTB autografts resulted in increased anterior knee pain, kneeling pain, and incidence of OA, as compared with HT autograft.[22] Poehling-Monaghan et al[21] also reported a systematic review comparing BPTB and HT autografts for ACLR at a minimum of 5 years’ follow-up, but two of the included studies were cohort studies, and finally concluded that the clinical outcomes scores were lower, and greater motion loss and higher rates of OA were seen in the BPTB group. The above meta-analysis included prospective cohort studies, which markedly increased the risk of heterogeneity arising from variations in study design. In addition, some studies observed that the prevalence of OA was higher in the BPTB group during the long-term follow-up, while others found that there was no difference in the prevalence of OA between the BPTB group and the HT group.[23–26] Therefore, this issue remains controversial. In recent years, several RCTs[27–29] have compared BPTB autografts and HT autografts for ACLR after a medium-term follow-up. Therefore, there was a need for a new meta-analysis that included more recent and high-quality RCT studies to provide the latest evidence for clinical decision-making.
Therefore, this meta-analysis aimed to determine whether there are significant differences between BPTB autografts and HT autografts for ACLR in terms of the clinical function, knee stability, postoperative complications, and OA changes, by comparing RCTs with a minimum follow-up of 5 years.
2. Methods
All analyses were based on previous published studies, thus no ethical approval and patient consent are required. This study is based on the Cochrane review methods.
2.1. Search strategy
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.[30] PubMed, Embase, and Cochrane Library databases were the three major electronic databases used for the literature search from inception to November 2, 2019. Before conducting the search, a systematic review registration was completed on April 28, 2020 using the PROSPERO International prospective register of systematic reviews (registration number CRD42020170821). “anterior cruciate ligament,” “bone patellar tendon,” “hamstring,” were the key words used in different combinations, and the detailed search strategy is (ACL OR anterior cruciate ligament) AND (patella OR patellar OR bone patellar tendon OR bone patella tendon) AND (hamstring OR semitendinosus OR gracilis patellar tendon). Additional studies were identified by reviewing the reference lists in the pertinent articles. Bibliographies of all the relevant retrieved studies were scrutinized to identify additional studies. Two authors (Deng and Lu) independently implemented the literature search, study selection and data extraction, and the reasons for exclusion were recorded and discordance was resolved by discussion or a decision from the corresponding author (Zhao).
2.2. Selection criteria
The included studies were randomized controlled trials (RCTs) and that directly comparing BTPB graft and HT graft for primary ACLR. Studies should be required to be published to be English and to have a minimum of 5-year follow-up. Studies with a Level of Evidence I and II (based on the Oxford Centre for Evidence-Based Medicine, used by the American version of the Arthroscopy and Journal of Bone and Joint Surgery[31]). Studies that reported data on
-
1.
functional outcome—objective International Knee Documentation Committee score, Lysholm knee score, return to preinjury activity level, Tegner activity level;
-
2.
stability parameters—Lachman test, pivot test, side-to-side difference;
-
3.
postoperative complications—anterior knee pain, kneeling pain, failure of graft, loss of extension and flexion; and
-
4.
radiograph evidence of osteoarthritis were considered to be eligible.
The number of strands of the autografts and the fixation in the proximal and distal part were not limited. Excluded were non-English articles, allograft, in vitro, animal, or cadaveric studies, and systematic reviews and meta-analyses. When multiple studies existed utilizing the same patient population but reporting outcomes at different time points, the study with the longest follow-up was included in our review while the rest were excluded.
2.3. Data extraction
The following information was extracted from the enrolled articles: the first author, date of publication, level of evidence, number of patients, number of depletions, mean age, sex, duration of follow-up, strands of the HT, type of graft fixation. The primary outcome was functional outcomes, such as an objective International Knee Documentation Committee (IKDC) score, return to preinjury activity level, Lysholm knee score. Other indicators include stability parameters, such as side-to-side difference, pivot-shift test, Lachman test; postoperative complications, such as anterior knee pain, kneeling pain, extension loss, flexion loss, and graft failure (defined as graft rupture or revision ACLR); and radiographic evidence of osteoarthritis. OA diagnosis was based on radiographic criteria, regarding of the classification or grading scale, OA was defined as the presence of joint-space narrowing of grade 2 and above in the Kellgren and Lawrence classification, grade 1 and above in the Ahlbäck rating system, and grade C and above in the IKDC classification.
2.4. Quality assessment
The quality of included studies was appraised by using the Cochrane Collaboration's risk-of-bias tool,[32] which contains the following seven items: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. Each of the above items was scored using three options: low risk, unclear risk, and high risk.
2.5. Statistical analysis
All data were analyzed using RevMan 5.3 (Cochrane Collaboration, Oxford, UK) software. The mean difference (MD) was used to compare continuous variables, such as the Lysholm knee score and side-to-side difference. The odds ratio (O ) was used for some continuous variables, such as return to preinjury activity level, objective IKDC score with grades C and D, pivot-shift test, Lachman test, anterior knee pain, kneeling pain, extension loss, flexion loss, and graft failure. All results were reported with 95% confidence intervals (95%CIs), and P values < .05 were considered to indicate statistical significance. I2 statistics and chi-square tests were used to evaluate heterogeneity. We chose the random-effects model if I2 > 50% and P < .1, because such studies had substantial heterogeneity. Alternatively, we chose the fixed-effects model if I2 < 50% and P > .1. Funnel plots were used to screen for potential publication bias.
) was used for some continuous variables, such as return to preinjury activity level, objective IKDC score with grades C and D, pivot-shift test, Lachman test, anterior knee pain, kneeling pain, extension loss, flexion loss, and graft failure. All results were reported with 95% confidence intervals (95%CIs), and P values < .05 were considered to indicate statistical significance. I2 statistics and chi-square tests were used to evaluate heterogeneity. We chose the random-effects model if I2 > 50% and P < .1, because such studies had substantial heterogeneity. Alternatively, we chose the fixed-effects model if I2 < 50% and P > .1. Funnel plots were used to screen for potential publication bias.
3. Results
3.1. Search
We initially searched 890 citations in the three databases and three citations were identified from other sources, of which 354 were excluded as duplicate articles. Screening the titles and abstracts of the remaining 539 citations, we excluded 514 citations, which were irrelevant to the topic of interest, or were not RCT or clinical studies, or were studies with follow-up of shorter than 5 years. The full text of the remaining 25 citations was analyzed by a senior author, and finally, 15 articles[23,24,27–29,33–42] were included in the meta-analysis (Fig. 1). All 15 studies that compared clinical outcomes between BPTB and HT autografts for ACLR were RCTs. The characteristics of the 15 included studies are summarized in Table 1. Overall, 1298 patients (n = 610 in BPTB, n = 688 in HT groups) were enrolled. The mean follow-up ranged from 60 months to 204 months.
Figure 1.
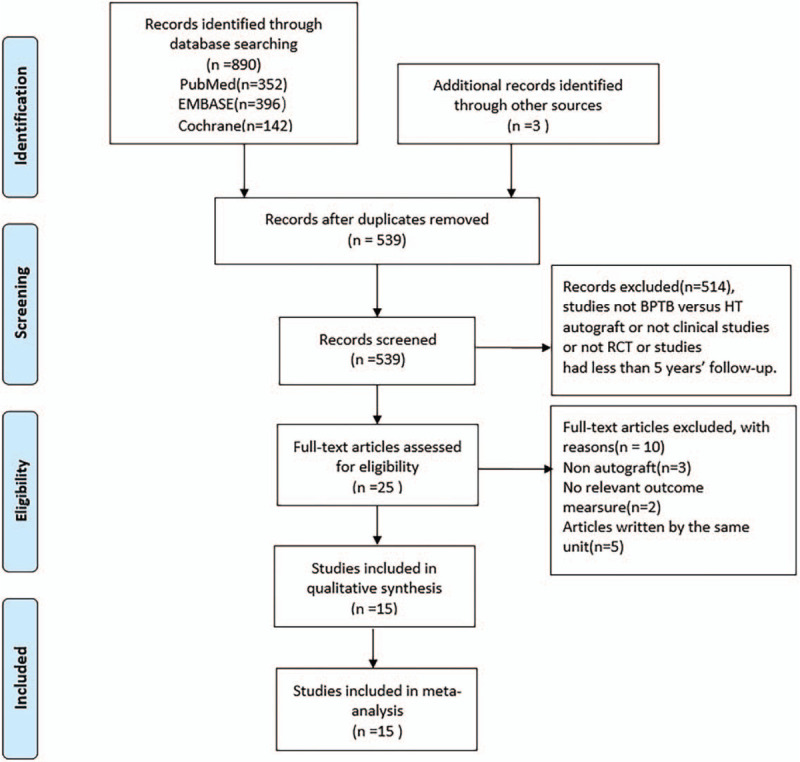
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flowchart of the literature search.
Table 1.
The baseline data and characteristics of the studies.
| NO. of follow up patients | Sex (male/female) | Mean age (year) | BPTB fixation | HT fixation | |||||||||||
| Study, year | Country | Level of evidence | BPTB | HT | BPTB | HT | BPTB | HT | Follow up (month) | NO. of depletions | Strands of HT | Femoral | Tibial | Femoral | Tibial |
| Gifstad[35] 2013 | Norway | II | 41 | 36 | NA | NA | 27 | 27 | 84 | 12 | 4 | ISC | ISC | Sc + WL | Sc + WL |
| Wipfler[40] 2011 | Germany | II | 28 | 25 | 19/12 | 18/13 | 29.8 | 34.2 | 105 | 8 | 4 | Press-fit | Su | Knot | Su |
| Ibrahim[37] 2005 | Kuwait | I | 40 | 45 | 40/0 | 45/0 | 22.3 | 22.3 | 81 | 25 | 4 | EB | ISc | EB | Sc + W/Pl + Sc + St |
| O’Neill[39] 2001 | America | I | 75 | 150 | 2/1 | 2/1 | Na | Na | 102 | 1 | 4 | Na | Na | Na | Na |
| Lidén[38] 2007 | Sweden | I | 32 | 36 | 23/11 | 26/11 | 28 | 29 | 86 | 3 | 3-4 | ISC | ISC | ISC | ISC |
| Harilainen[33] 2006 | Finland | I | 40 | 39 | Na | NA | Na | NA | 60 | 16 | 4 | ISC | ISC | EB | Sc+W |
| Holm[36] 2010 | Norway | I | 28 | 29 | 18/10 | 15/14 | 25 | 27 | 120 | 15 | 4 | ISC | ISC | EB | ISC |
| Konrads[27] 2016 | Germany | II | 24 | 23 | 22/9 | 23/8 | 29.8 | 29.8 | 120 | 14 | 3–4 | ISC | ISC | EB | Su |
| Zaffagnini[41] 2006 | Italy | I | 25 | 25 | 16/9 | 15/10 | 30.5 | 31.3 | 60 | 0 | 4 | ISC | ISC | EB | SC |
| Ahlden[23] 2009 | Sweden | I | 22 | 25 | 14/8 | 18/7 | 26 | 28 | 86 | 24 | 3–4 | ISC | ISC | ISC | ISC |
| Barenius[24] 2014 | Sweden | I | 69 | 66 | 35/34 | 44/21 | 39.2 | 41.6 | 169 | 29 | 4 | ISC | ISC | EB | Su |
| Mohtadi[29] 2019 | Canada | I | 103 | 105 | 60/43 | 58/47 | 33.8 | 33.7 | 60 | 12 | 4 | EB | ISC | EB | ISC |
| Sajovic[28] 2018 | Slovenia | II | 24 | 24 | 15/9 | 13/11 | 45.7 | 42.5 | 204 | 16 | 4 | ISC | ISC | ISC | ISC |
| Matsumoto[34] 2006 | Japan | I | 37 | 35 | 21/16 | 15/20 | 23.7 | 24.4 | 87 | 8 | 5 | ISC | ISC | ISC | ISC |
| Webster[39] 2016 | Australia | I | 22 | 25 | 16/6 | 20/5 | 26.6 | 26.1 | 184 | 18 | 4 | EB | ISC | EB | SC |
3.2. Quality
The details of the quality assessment are shown in Figure 2. RCTs were assessed by determining the risk-of-bias. For 15 (100%) studies, allocation sequence generation (Criterion 1) was scored as “Low risk.” Allocation concealment (Criterion 2) was scored as “Low risk” in 10 (66.7%) studies and “Unclear risk” in 5 (33.3%) studies. Criterion 3 was scored as “Low risk” in 2 (13.3%) and as “High risk” in 13 (86.7%) studies. Criterion 4 was scored as “Low risk” in 11 (73.3%) and as “Unclear risk” in 4 (26.7%) studies. Criterion 5 was scored as “Low risk” in 8 (53.3%) and as “High risk” in 7 (46.7%) studies. Criteria 6 and 7 were scored as “Low risk” in all (100%) studies.
Figure 2.
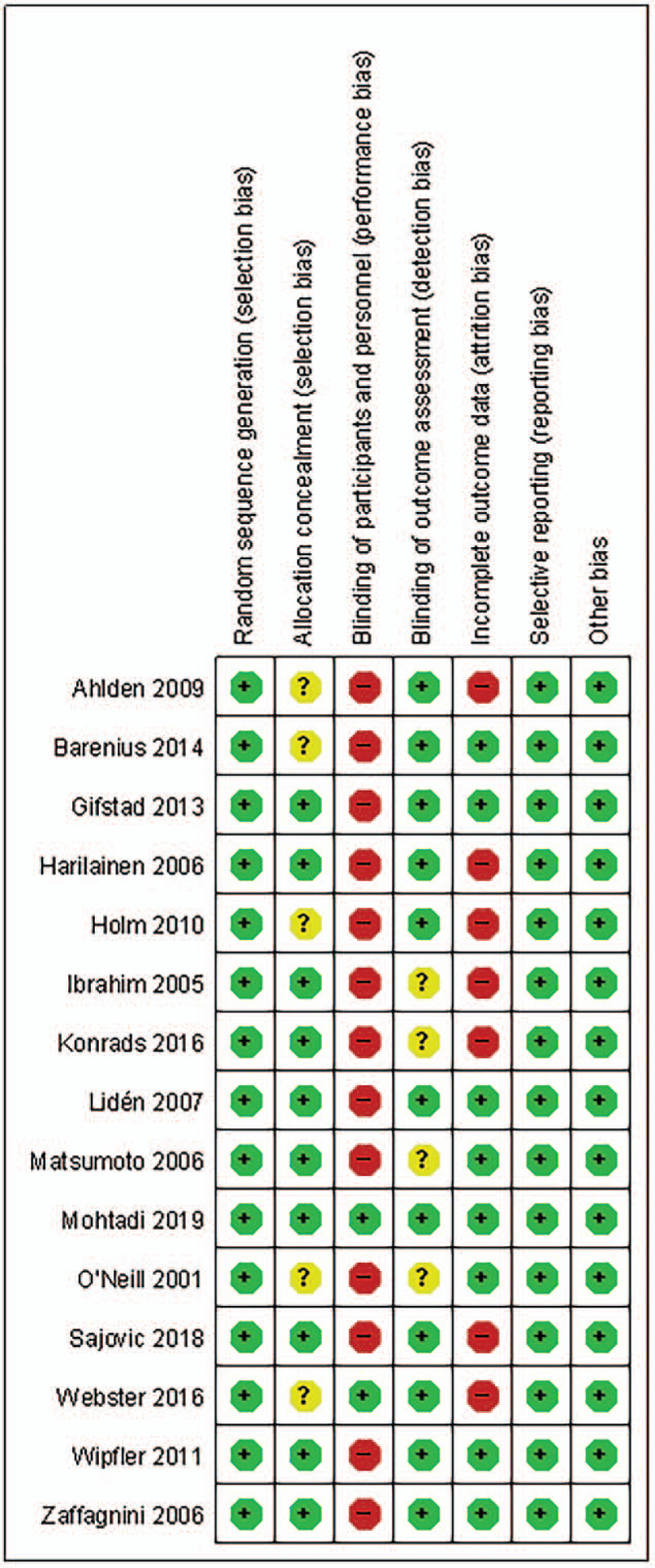
Assessment of risk-of-bias.
3.3. Functional outcomes
3.3.1. Objective IKDC score
Overall, 863 patients were included in nine studies[28,29,33,34,37,38–41] in which patients with IKDC grades C and D were found in 71 of 469 patients in the BPTB group and 69 of 394 patients in the HT group. There was no heterogeneity among the studies (P = .76, I2 = 0%), and the difference was not significant between the two groups (OR = 0.94, 95%CI [0.64, 1.37], Z = 0.32, P = .75). These results are shown in Figure 3.
Figure 3.

Forest plot of comparison of the postoperative objective International Knee Documentation Committee (IKDC) score with grades C and D between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.2. Lysholm knee score
Eight studies[23,27,28,33,36–38,40] were analyzed for the Lysholm knee score, involving a total of 484 patients (238 BPTB, 246 HT). The analysis showed that there was significant heterogeneity among the studies (P = .004, I2 = 66%), and the difference was not significant between the two groups (MD = −2.26, 95%CI [−4.56, 0.05], Z = 1.92, P = .06). These results are shown in Figure 4.
Figure 4.
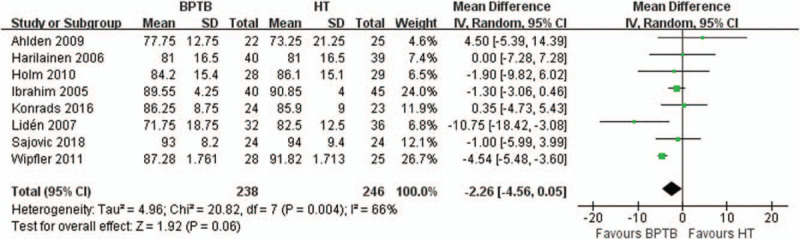
Forest plot of comparison of Lysholm knee score between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.3. Return to preinjury activity level
We reviewed five studies[28,29,34,36,41] for the return to preinjury activity level, which included 396 patients (203 BPTB, 193 HT). There was no heterogeneity among the studies (P = .33, I2 = 12%), and the difference was not significant between the two groups (OR = 1.01, 95%CI [0.67, 1.52], Z = 0.05, P = .96). The results are shown in Figure 5.
Figure 5.
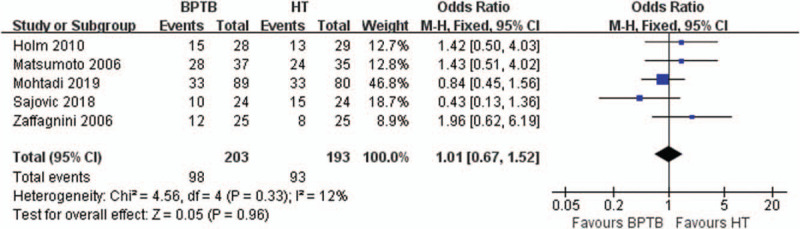
Forest plot of comparison of return to preinjury activity level between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.4. Tegner activity level
We reviewed nine studies,[23,24,27,33,36–38,40,41] which included 620 patients (308 BPTB, 312 HT) for the postoperative Tegner activity level. There was significant heterogeneity among the studies (P = .0005, I2 = 72%), but the difference was not statistically significant between the two groups (OR = 0.03, 95%CI [−0.36, 0.41], Z = 0.13, P = .89). The results are shown in Figure 6.
Figure 6.
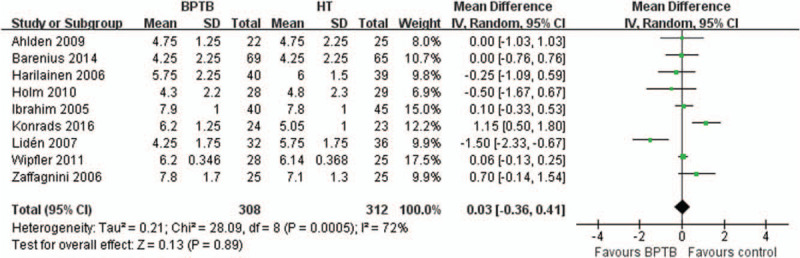
Forest plot of comparison of postoperative Tegner activity level between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.5. Stability
3.3.5.1. Side-to-side difference
Nine studies,[23,28,33–36,38,40,42] including 548 patients (274 BPTB, 274 HT) reported data regarding side-to-side difference. There was significant heterogeneity among the studies (P = .005, I2 = 64%), and the difference was not significant between the two groups (MD = −0.32, 95%CI [−0.81,0.16], Z = 1.31, P = .19). The results are shown in Figure 7.
Figure 7.

Forest plot of comparison of postoperative side-to-side difference between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.5.2. Lachman test
Eight studies[23,27,28,33,35,37,38,41] were analyzed for the Lachman test, involving 501 patients (248 BPTB, 253 HT). There was no heterogeneity among the studies (P = .73, I2 = 0%), and the difference was not significant between the two groups (OR = 0.86, 95%CI [0.56, 1.32], Z = 0.67, P = .50). The results are shown in Figure 8.
Figure 8.
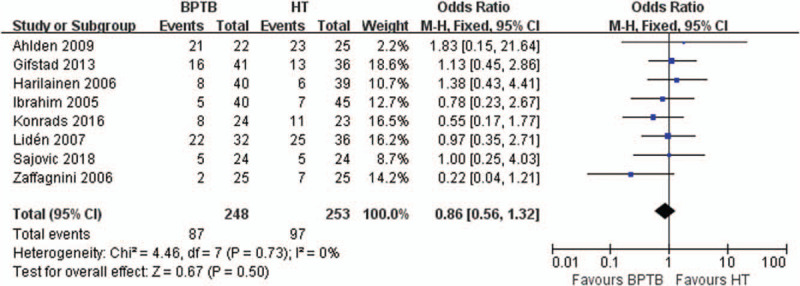
Forest plot of comparison of the postoperative Lachman test results between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.5.3. Pivot-shift test
Five studies,[29,33,37,28,41] involving 455 patients (225 BPTB, 230 HT) reported the outcomes of the pivot-shift test. The analysis showed that there was no heterogeneity among the studies (P = .56, I2 = 0%), and the difference was not significant between the two groups (OR = 0.68, 95%CI [0.44, 1.06], Z = 1.70, P = .09). The results are shown in Figure 9.
Figure 9.
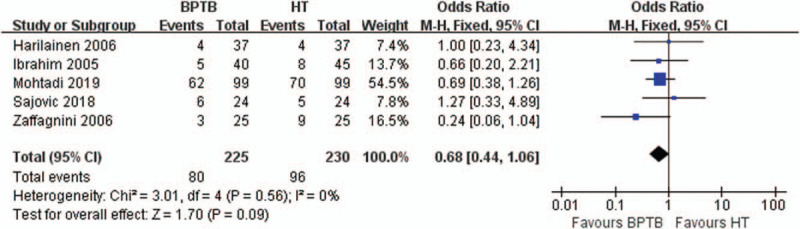
Forest plot of comparison of the postoperative pivot-shift test results between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.6. Postoperative complications
3.3.6.1. Kneeling pain
Six studies,[28,29,34,38,41,42] including 481 patients (238 BPTB, 243 HT), reported data regarding postoperative kneeling pain. There was no heterogeneity among these studies (P = .25, I2 = 25%), and there was a significant difference between the two groups (OR = 1.67, 95%CI [1.04, 2.69], Z = 2.12, P = .03). The results are shown in Figure 10. Three studies[29,34,38] reported on the degree of kneeling pain; moderate or severe pain occurred in 21/167 (12.6%) in the BPTB group and in 6/168 (3.6%) in the HT group.
Figure 10.
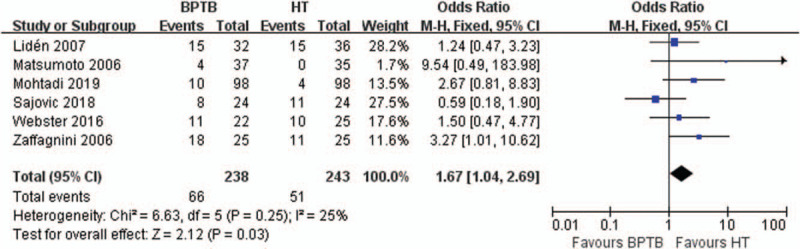
Forest plot of comparison of the postoperative kneeling pain between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.6.2. Anterior knee pain
Five studies,[34,35,37,41,42] involving 331 patients (165 BPTB, 166 HT), reported postoperative anterior knee pain. There was no heterogeneity among these studies (P = .73, I2 = 0%), and there was a significant difference between the two groups (OR = 2.90, 95%CI [1.46, 5.77], Z = 3.04, P = .002). The results are shown in Figure 11. Only one study[34] reported the degree of anterior knee pain; moderate or severe pain occurred in 2/37 (5.4%) in the BPTB group, that in 1/34 (2.9%) of the HT group.
Figure 11.

Forest plot of comparison of the postoperative anterior knee pain between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
3.3.6.3. Extension loss
Nine studies,[23,24,27–29,34,35,37,41] involving 749 patients, reported postoperative extension loss. Extension loss occurred postoperatively in 61 of 377 patients in the BPTB group and in 38 of 372 patients in HT group. There was no heterogeneity among the studies (P = .12, I2 = 38%), and the difference was significant between the two groups (OR = 1.75, 95%CI [1.12, 2.75], Z = 2.46, P = .01). The results are shown in Figure 12. The specific conditions of extension loss between the two groups are shown in Table 2.
Figure 12.

Forest plot of comparison of postoperative extension loss between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
Table 2.
The specific conditions of extension loss and flexion loss in each study.
| Study | Measuring method | BPTB: extension loss | HT: extension loss | BTBP: flexion loss | HT: flexion loss |
| Ibrahim[37] | Physical examination | ≥10°:2 (5%),≤5°:12 (30%) | ≤5°:8 (17.7%) | ≥15°:5 (12.5%) | ≥15°: 1 (3%) |
| Gifstad[35] | Physical examination | ≥5°:2 (5%) | ≥5°:3 (8%) | ≥5°:4 (10%) | ≥5°:6 (17%) |
| Ahlden[23] | Unknown | 3 (14%) | 3 (12%) | 6 (27%) | 12 (48%) |
| Barenius[24] | Unknown | 3–5°:26 (39%) | 3–5°:8 (13%) | 6–15°:13 (19%) | 6–15°:16 (27%) |
| Matsumoto[34] | Unknown | 5°:3 (8.1%),10°:1 (2.7%) | 5°:2 (5.7%) | 10°:2 (5.4%) | 10°:1 (2.8%) |
| Konrads[27] | Unknown | 5°:1 (4.2%) | Normal | Normal | Normal |
| Mohtadi[29] | Long-arm goniometer | >3°:0 (0%) | >3°:0 (0%) | Passive flexion: 142.5°±7.3° | Passive flexion: 142.2°±7.8° |
| Zaffagnini3[41] | Physical examination | ≤2°:21 (84%),3–5°:3 (12%),6–10°:0 (0%),>10°:2 (8%) | ≤ 2°:18 (72%),3–5°:5 (20%),6–10°:1 (4%),>10°:1 (4%) | ≤5°:16 (64%),6–15°:6 (24%), 16–25°: 2 (8%),>25°:1 (4%) | ≤5°:22 (88%),6–15°:2 (8%),16–25°:1 (4%),>25°:0 (0%) |
| Sajovic[28] | Unknown | 2 (8.3%) | 1 (4.2%) | 0 (0%) | 0 (0%) |
3.3.6.4. Flexion loss
Seven studies,[23,24,27,34,35,37,41] including 505 patients (257 BPTB, 248 HT), reported data regarding postoperative flexion loss. There was heterogeneity among these studies (P = .06, I2 = 52%), and the difference was not significant between the two groups (OR = 1.09, 95%CI [0.47, 2.54], Z = 0.19, P = .85). The results are shown in Figure 13. The specific conditions of flexion loss between the two groups are shown in Table 2.
Figure 13.
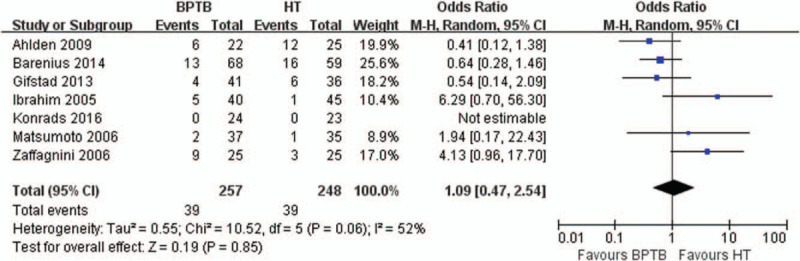
Forest plot of comparison of postoperative flexion loss between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
Graft failure
Twelve studies,[24,27–29,33–36,38,39,40,42] involving 1280 patients (678 BPTB, 602 HT), reported postoperative graft failure. There was no heterogeneity among these studies (P = .78, I2 = 0%), and there was a significant difference between the two groups (OR = 0.59, 95%CI [0.38, 0.91], Z = 2.38, P = .02). The results are shown in Figure 14. The proportion of graft failure was 5.5% (37/678) in the BPTB group and 9.0% (54/602) in the HT group.
Figure 14.
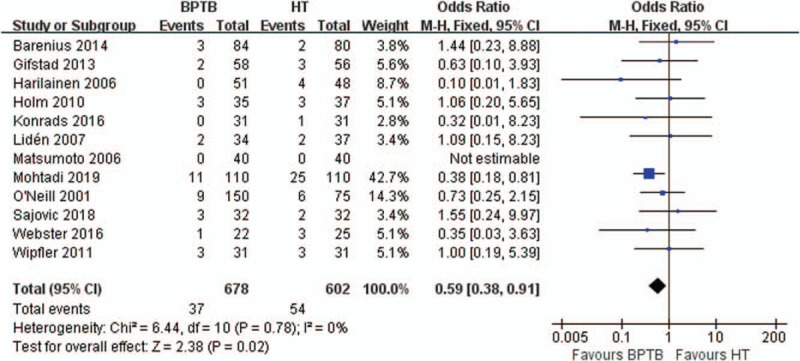
Forest plot of comparison of postoperative graft failure between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
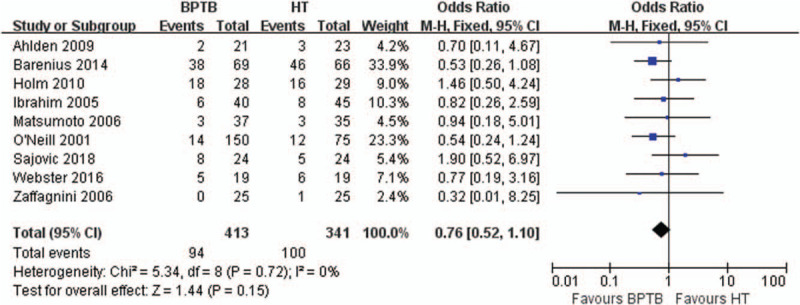
3.3.6.5. Radiographic evidence of osteoarthritis
Nine of the 15 studies[23,24,28,34,36,37,39,41,42] presented information about degenerative OA of the knee (Table 3). Three studies[28,34,42] reported OA using the IKDC score, according to radiograph evidence, two[23,36] used the Kellgren and Lawrence classification, and one[23] used the Ahlbäck rating system. Zaffagnini et al[41] measured the tibiofemoral space on Rosenberg X-rays preoperatively and at follow-up, and diagnosed OA when there was a difference of ≥2 mm between the two X-ray images. In another two studies,[37,39] the methods used to evaluate change related to OA were not clear. The following cases with tibiofemoral joint or medial tibiofemoral compartment OA were combined in our meta-analysis: grade 2 and above in the Kellgren and Lawrence classification, grade 1 and above in the Ahlbäck rating system, and grade C and above in the IKDC classification. Pooled outcomes showed that there was no heterogeneity among the studies (P = .72, I2 = 0%), and the difference was not significant between the two groups (OR = 0.76, 95%CI [0.52, 1.10], Z = 1.44, P = .15) (Fig. 15).
Table 3.
Radiographic outcome measures.
| Study | Time (months) from injury to operation (BPTB/HT) | Radiographic grading scale | BPTB: radiographic evidence of OA | HT: radiographic evidence of OA |
| Holm[36] | 41.3 ± 41.0/40.5 ± 41.6 | Kellgren and Lawrence classification | (grade 0-1-2-3-4):2-8-11-7-0 | (grade 0-1-2-3-4):4-9-14-2-0 |
| Barenius[24] | 13.9 ± 23/16.3 ± 23 | Kellgren and Lawrence classification | (grade 0-1/2-4):31/38 | (grade 0-1/2-4):20/46 |
| Webster[42] | NA | Kellgren and Lawrence classification | (grade 0-1/2-3):14/5 | (grade 0-1/2-3):13/6 |
| Ahlden[23] | 11 (2-252)/17 (3-240) | Ahlbäck rating system | (grade 0-1-2-3-4-5):19-2-0-0-0-0 | (grade 0-1-2-3-4-5):20-2-0-0-0-1 |
| Sajovic[28] | 22.1 ± 28.8/27.5 ± 43.5 | IKDC | (grade A-B-C-D):0-16-5-3 | (grade A-B-C-D):7-12-3-2 |
| Matsumoto[34] | 11.4 ± 9.9/8.9 ± 9.9 | IKDC | 3 | 3 |
| Ibrahim[37] | 9.7 (4-13)/9.7 (4-13) | NA | PFJ:8,MTFC:6 | PFJ:3,MTFC:8 |
| O’Neill[39] | NA | NA | TFJ:14/150 | TFJ:12/75 |
| Zaffagnini[41] | 8 (3-13)/9 (2-12) | NA | MTFC:0/25 | MTFC:1/25 |
Figure 15.
Forest plot of comparison of osteoarthritis (OA) between the bone–patellar tendon–bone (BPTB) vs hamstring tendon (HT) autograft groups for anterior cruciate ligament reconstruction.
The results of all the above forest plot are summarized in Table 4.
Table 4.
Summary of the meta-analyses.
| Analyses item | Number of studies | Heterogeneity and P | Analysis model | MD/OR (95%CI) | P |
| Objective IKDC score | 9 | 0% (.66) | Fixed-effects | 0.94 (0.64,1.37) | .75 |
| Lysholm knee score | 8 | 66% (.004) | Random-effects | −2.26 (−4.56,0.05) | .06 |
| Return to preinjury activity level | 5 | 12% (.33) | Fixed-effects | 1.01 (0.67,1.52) | .96 |
| Tegner activity level | 9 | 72% (.0005) | Random-effects | 0.03 (−0.36,0.41) | .89 |
| Side-to-side difference | 9 | 0% (.72) | Fixed-effects | 0.76 (0.52,1.10) | .15 |
| Lachman test | 8 | 0% (.73) | Fixed-effects | 0.86 (0.56,1.32) | .50 |
| Pivot shift test | 5 | 0% (.56) | Fixed-effects | 0.68 (0.44,1.06) | .09 |
| Kneeling pain | 6 | 25% (.25) | Fixed-effects | 1.67 (1.04,2.69) | .03 |
| Anterior knee pain | 5 | 0% (.73) | Fixed-effects | 2.90 (1.46,5.77) | .002 |
| Extension loss | 9 | 38% (.12) | Fixed-effects | 1.75 (1.12,2.75) | .01 |
| Flexion loss | 7 | 52% (.06) | Random-effects | 1.09 (0.47,2.54) | .85 |
| Graft failure | 12 | 0% (.78) | Fixed-effects | 0.59 (0.38,0.91) | .02 |
| Radiograph evidence of osteoarthritis | 9 | 0% (.72) | Fixed-effects | 0.76 (0.52,1.10) | .15 |
3.4. Publication bias
A funnel plot was created to assess if there was bias in this study. The funnel plot appeared mild asymmetrical, suggesting publication bias in the data (Fig. 16).
Figure 16.

Funnel plot with 95% CL is showing mild publication bias for comparison of graft failure between BPTB and HT autograft.
4. Discussion
The results of this meta-analysis indicated that, compared with BPTB autografts, HT autografts were associated with a decreased incidence of anterior knee pain, kneeling pain, and extension loss, but increased incidence of graft failure after ACLR in medium-term follow-up. Differences in other measures were not statistically significant between the two types of autografts used for ACLR.
Although ACL reconstruction is a mature technology, there is still considerable controversy about which autograft provides the best results for ACLR. BPTB autografts raise concerns about donor site morbidity, including anterior knee pain, kneeling pain, patella fracture, and patellar tendon rupture.[42,43] In their review, Kartus et al[44] pointed out that 40% to 60% of patients reported various donor site problems after harvesting of the BPTB autograft. It has been reported that patella fracture and patellar tendon rupture after ACLR are quite rare (with an incidence of 0.4% to 1.3% and 0.18% to 0.25%, respectively), and are related to irregular surgical procedures, such as deep and irregular saw cutting, poor centralization during the harvest leading to the lateral or medial side being too thin.[43] However, anterior knee pain and kneeling pain were quite common after ACLR with BPTB autograft, and it has been reported that these pains are related to injury to the infrapatellar branches of the saphenous nerve during the operation;[43] In BPTB autografts, their incidences were 52% and 65% at the 2-year follow-up, respectively, which was higher than the 17% and 35% incidences, respectively, of HT autograft.[42] It has been reported that the transplantation of β-tricalcium phosphate or autologous bone to the donor-site bone defects at the tibial and patellar tubercle can effectively reduce the occurrence of anterior knee pain and kneeling pain.[45,46] Additionally, the double-incision technique has been used to avoid injury of the saphenous nerve infrapatellar branches and to preserve the paratenon and the patellar tendon, which can also reduce the donor site morbidity associated with BPTB.[47] Gaudot et al[48] used the double-incision technique to reduce the frequency of anterior knee pain to 18% (as compared to 58% for the single-incision technique), but there was no significant difference in the degree of anterior knee pain between the two techniques. The results of this meta-analysis showed that the HT group had apparent advantages in anterior knee pain and kneeling pain during medium-term follow-up. The incidence of moderate or severe kneeling pain was significantly higher in the BPTB group than in the HT group. Clinically, the technique of double-incision and bone grafting could be used to reduce donor site morbidity. BPTB may thus not be recommended for patients who need to kneel frequently during their work. The HT autograft also has some disadvantages. The gracilis and semitendinosus muscle mainly function as internal tibial rotators and knee flexors, so that HT autograft harvests may lead to flexion strength deficits. Gifstad et al[35] reported that the peak flexion torque of the operated knee decreased significantly after 1 year in the HT group. However, there was no difference after 2 years and after 7 years.[49] The results of this meta-analysis showed that the HT group had apparent advantages in terms of anterior knee pain and kneeling pain during the medium-term follow-up. This finding was consistent with the results of previous published meta-analyses.[9,14,15]
Another focus of the debate about the two autografts was graft failure. The leading causes of postoperative graft failure include graft rupture and graft laxity after ACLR, which might be affected by the biomechanical and histologic properties of the graft. One of the advantages of BPTB autografts is its excellent biomechanical properties, which was similar to that of the ACL. Woo et al[50] proved that, when the ACL was tested in the anatomical direction, for young patients (aged 22–35 years), the maximum load to failure of the ACL was 2160N, while those of the BPTB autograft and quadrupled HT graft were 800N and 4590N, respectively.[51,52] These studies mentioned above suggested that the HT autograft may have better mechanical properties than the BPTB autograft. However, the present meta-analysis suggested that, at medium-term follow-up, the HT group had a higher incidence of graft failure than the BPTB group; these results were mainly consistent with Samuelsen et al[53] and Chee et al's meta-analysis.[14] In terms of postoperative knee stability, the results of the present study showed that there was no significant difference in side-to-side difference, Lachman test, and pivot-shift test results between the two groups after medium-term follow-up.[14] This was mainly consistent with the result of Samuelsen et al[53] and Xie et al's meta-analysis.[22] The above results show that some indexes of knee stability, including the side-to-side difference, Lachman test, and pivot-shift test, have limitations in that they are carried out on an open kinetic chain with a relaxed lower limb and cannot reliably predict the functional stability of the knee in sports activities.[54–60] In this study, the graft failure rate was 5.5% in the BPTB group and 9.0% in the HT group. This finding may indicate that it was not only the strength of the graft itself that affected the structural strength of the graft structure, but also the fixation points on both the femoral and tibial side, which seem to be the weakest points.[61] The proper bone-to-bone tunnel healing of the BPTB autograft could provide firm fixation, while the HT autograft involved a slow tendon to bone healing process and a lack of rigid fixation.[62] A previous study[63] has shown that soft tissue could frequently take up to 6 weeks longer to incorporate into the host bone than the BPTB autograft. Therefore, the increased failure and laxity of the graft may be a clinical manifestation of the slower ligamentization process and different biomechanical characteristics of the HT autograft.[64]
The occurrence of OA after ACLR was also a concern. In the published meta-analysis, there was not much discussion about the occurrence of OA after ACLR, but the problem was universal. However, it was not clear which type of autograft would increase the risk of OA progression. Xie et al's meta-analysis showed that the incidence of OA in the BPTB group might be increased, as compared with that in the HT group.[22] However, the above meta-analysis did not limit the included studies to RCTs. The results of present meta-analysis showed that there was no significant difference in the incidence of OA between the two autografts after medium-term follow-up, which was consistent with the conclusion of Belk et al's systematic review.[65] ACL injury is often accompanied by cartilage injury of the knee joint, which persists after ACLR. After injury, some inflammatory responses in the knee could ultimately lead to OA progression.[66] Therefore, according to our knowledge of the mechanism of post-traumatic OA[65] and the results of this meta-analysis, the degree of a knee injury after trauma, rather than the types of autograft, might be the key factor affecting the progression of OA after ACLR. However, these results should be cautiously interpreted. First, the occurrence of OA after ACLR may be related to meniscectomy. We were unable to confirm whether the results were affected by meniscectomy due to the lack of information in the included study. Second, different radiological classification systems for OA (such as Kellgren and Lawrence, Ahlback, IKDC) were used in this meta-analysis, and a conversion methods for various OA score need to be developed to allow subsequent statistical analysis. In addition, due to the lack of information provided in the included studies, we did not further explore whether the progression of OA was mainly based on the patellofemoral joint or the tibiofemoral joint. If it was mainly the progression of patellofemoral osteoarthritis, it may represent technique of graft harvest and suggest that extreme care be taken during harvest to avoid chondral injury. If it was mainly the progression of tibiofemoral osteoarthritis, it may be related to meniscectomy and the increased rate of stiffness after utilizing BPTB autograft reported by some authors. Regardless of the cause of the effect, it was recommended that both BPTB and HT autograft could be selected in patients who already exhibit early signs of osteoarthritis.
Several potential limitations of this study should be noted. First, the final clinical results may be affected by the differences in population heterogeneity, follow-up duration, follow-up loss, method of graft fixation, and postoperative rehabilitation regimen, but it is not possible to control these variables individually. Second, although the flexion torque after HT harvest is important in the discussion between choosing BPTB and HT autografts for ACLR, there have been few reports about this in the included studies, and the reported indicators are different, making it impossible to carry out a meta-analysis of flexion torque. Third, not all the studies use the same scale to grade radiographic signs of OA and there was an apparent lack of reported data combining both clinical and radiological aspects of OA. More high-quality RCTs with long-term follow-up are needed to come to a definite conclusion in future.
5. Conclusions
Based on the results above, HT autograft is comparable with the BPTB autograft in terms of clinical function, postoperative knee stability, and OA changes, with a medium-term follow-up. The HT autograft for ACL reconstruction carries a lower risk of complications, such as anterior knee pain, kneeling pain, and extension loss, but an increased incidence of graft failure. Patients should be informed of the differences when deciding on graft choice with their physician.
Author contributions
LL Z and MF L have made substantial contributions to conception and design of the study, written the manuscript; MC D, LL H, CB W, and JS X unsearched literature, extracted data from the collected literature and analyzed the data; LL Z revised the manuscript; all authors have read and approved the final version of the paper for submission.
Data curation: Jisi Xing.
Formal analysis: Lilei He.
Resources: Mingcong Deng, Changbing Wang.
Writing – original draft: Mingfeng Lu.
Writing – review & editing: Lilian Zhao.
Footnotes
Abbreviations: ACL = anterior cruciate ligament, ACLR = anterior cruciate ligament reconstruction, BPTB = bone–patellar tendon–bone, HT = hamstring tendon, IKDC = International Knee Documentation Committee, OA = osteoarthritis, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCT = randomized controlled trial.
How to cite this article: Zhao L, Lu M, Deng M, Xing J, He L, Wang C. Outcome of bone–patellar tendon–bone vs hamstring tendon autograft for anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials with a 5-year minimum follow-up. Medicine. 2020;99:48(e23476).
LZ and ML contributed equally to this work.
This study was funded by grants from the Science and Technology Planning Project of Guangdong Province (No. A2016580) and Administration of Traditional Chinese Medicine of Guangdong Province (No. 20192095).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the present study are publicly available.
BPTB = bone-patellar tendon-bone, CP = cross pins, EB = Endobutton, HT = hamstring tendon, ISC = interference screw, NA = not available, P = post, Pl = plate, Sc = screw, St = staple, Su = sutures, TcSc = transcondylar screw, W = washer, WL = washerlock.
BPTB = bone-patellar tendon-bone, HT = hamstring tendon.
BPTB = bone-patellar tendon-bone, HT = hamstring tendon, IKDC = International Knee Documentation Committee score, MTFC = medial tibiofemoral compartment, NA = not available, OA = osteoarthritis, PFJ = Patellofemoral joint, TFJ = tibiofemoral joint.
IKDC = International Knee Documentation Committee.
References
- [1].Sanders TL, Maradit KH, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 2016;44:1502–7. [DOI] [PubMed] [Google Scholar]
- [2].Sanders TL, Pareek A, Kremers HM, et al. Long-term follow-up of isolated ACL tears treated without ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2016;25:1–8. [DOI] [PubMed] [Google Scholar]
- [3].Krause M, Freudenthaler F, Frosch KH, et al. Operative versus conservative treatment of anterior cruciate ligament rupture. Dtsch Arztebl Int 2018;115:855–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Monk AP, Davies LJ, Hopewell S, et al. Surgical versus conservative interventions for treating anterior cruciate ligament injuries. Cochrane Database Syst Rev 2016;4:CD011166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Delay BS, Smolinski RJ, Wind WM, et al. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Sports Med 2001;14:85–91. [PubMed] [Google Scholar]
- [6].Bourke HE, Salmon LJ, Waller A, et al. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med 2012;40:1985–92. [DOI] [PubMed] [Google Scholar]
- [7].Fu FH, Bennett CH, Ma CB, et al. Current trends in anterior cruciate ligament reconstruction part II. Operative procedures and clinical correlations. Am J Sports Med 2009;22:7–12. [DOI] [PubMed] [Google Scholar]
- [8].Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with Hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med 2014;42:2319–28. [DOI] [PubMed] [Google Scholar]
- [9].Xie X, Liu X, Chen Z, et al. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee 2015;22:100–10. [DOI] [PubMed] [Google Scholar]
- [10].Kim SJ, Yoon JY, Kim SM, et al. A comparative study on the postoperative outcomes of anterior cruciate ligament reconstruction using patellar bone-tendon autografts and bone-patellar tendon-bone autografts. Arthroscopy 2016;32:1072–107. [DOI] [PubMed] [Google Scholar]
- [11].Goldblatt JP, Fitzsimmons SE, Balk E, et al. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus Hamstring tendon autograft. Arthroscopy 2005;21:791–803. [DOI] [PubMed] [Google Scholar]
- [12].Li SZ, Su W, Zhao J, et al. A meta-analysis of hamstring autografts versus bone-patellar tendon-bone autografts for reconstruction of the anterior cruciate ligament. Knee 2011;18:287–93. [DOI] [PubMed] [Google Scholar]
- [13].Rahr-Wagner L, Thielemann TM, Pedersen AB, et al. Comparison of Hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish Registry of knee ligament reconstruction. Am J Sports Med 2014;42:278–84. [DOI] [PubMed] [Google Scholar]
- [14].Chee MY, Chen Y, Pearce CJ, et al. Outcome of patellar tendon versus 4-strand Hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy 2017;33:450–63. [DOI] [PubMed] [Google Scholar]
- [15].Mohtadi NG, Chan DS, Dainty KN, et al. Patellar tendon versus hamstring autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 2011. CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bizzini M, Gorelick M, Munzinger U, et al. Joint laxity and isokinetic thigh muscle strength characteristics after anterior cruciate ligament reconstruction. Clin J Sport Med 2006;16:4–9. [DOI] [PubMed] [Google Scholar]
- [17].Heijne A, Hagströmer M, Werner S. A two- and five-year follow-up of clinical outcome after ACL reconstruction using BPTB or hamstring tendon grafts: a prospective intervention outcome study. Knee Surg Sports Traumatol Arthrosc 2015;23:799–807. [DOI] [PubMed] [Google Scholar]
- [18].Fineberg MS, Zarins B, Sherman OH. Practical considerations in anterior cruciate ligament replacement surgery. Arthroscopy 2000;16:715–24. [DOI] [PubMed] [Google Scholar]
- [19].Schuette HB, Kraeutler MJ, Houck DA, et al. Bone-patellar tendon-bone versus Hamstring tendon autografts for primary anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses [published online November 5]. Orthop J Sports Med 2017;doi: 10.1177/2325967117736484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Prodromos CC, Joyce BT, Shi K, et al. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy 2005;21:1202. [DOI] [PubMed] [Google Scholar]
- [21].Poehling-Monaghan KL, Salem H, Ross KE, et al. Long-term outcomes in anterior cruciate ligament reconstruction: a systematic review of patellar tendon versus Hamstring autografts. Orthop J Sports Med 2017;5:2325967117709735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Xie X, Xiao Z, Li Q, et al. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol 2015;25:149–59. [DOI] [PubMed] [Google Scholar]
- [23].Ahldén M, Kartus J, Ejerhed L, et al. Knee laxity measurements after anterior cruciate ligament reconstruction, using either bone–patellar–tendon-bone or hamstring tendon autografts, with special emphasis on comparison over time. Knee Surg Sports Traumatol Arthrosc 2009;17:1117–24. [DOI] [PubMed] [Google Scholar]
- [24].Barenius B, Ponzer S, Shalabi A, et al. Increased risk of osteoarthritis after ACL reconstruction—a 14-year follow-up study of a randomized controlled trial. Am J Sports Med 2014;42:1049–57. [DOI] [PubMed] [Google Scholar]
- [25].Leys T, Salmon L, Waller A, et al. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med 2012;40:595–605. [DOI] [PubMed] [Google Scholar]
- [26].Keays SL, Bullock-Saxton JE, Keays AC, et al. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med 2007;35:729–39. [DOI] [PubMed] [Google Scholar]
- [27].Konrads C, Reppenhagen S, Plumhoff P, et al. No significant difference in clinical outcome and knee stability between patellar tendon and semitendinosus tendon in anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg 2016;136:521–5. [DOI] [PubMed] [Google Scholar]
- [28].Sajovic M, Stropnik D, Skaza K. Long-term comparison of semitendinosus and Gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: a 17-year follow-up of a randomized controlled trial. Am J Sports Med 2018;46:1800–8. [DOI] [PubMed] [Google Scholar]
- [29].Mohtadi NG, Chan DS. A randomized clinical trial comparing patellar tendon, Hamstring tendon, and double-bundle ACL reconstructions: patient-reported and clinical outcomes at 5-year follow-up. J Bone Joint Surg Am 2019;101:949–60. [DOI] [PubMed] [Google Scholar]
- [30].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2010;8:336–41. [DOI] [PubMed] [Google Scholar]
- [31].Cowan J, Lozano-Calderon S, Ring D. Quality of prospective controlled randomized trials. Analysis of trials of treatment for lateral epicondylitis as an example. J Bone Joint Surg Am 2007;89:1693–9. [DOI] [PubMed] [Google Scholar]
- [32].Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. New York, NY: Cochrane Collaboration, John Wiley & Sons; 2008. [Google Scholar]
- [33].Harilainen A, Linko E, Sandelin J. Randomized prospective study of ACL reconstruction with interference screw fixation in patellar tendon autografts versus femoral metal plate suspension and tibial post fixation in hamstring tendon autografts: 5-year clinical and radiological follow-up results. Knee Surg Sports Traumatol Arthrosc 2006;14:517–28. [DOI] [PubMed] [Google Scholar]
- [34].Matsumoto A, Yoshiya S, Muratsu H, et al. A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med 2006;34:213–9. [DOI] [PubMed] [Google Scholar]
- [35].Gifstad T, Sole A, Strand T, et al. Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 2013;21:576–83. [DOI] [PubMed] [Google Scholar]
- [36].Holm I, Oiestad BE, Risberg MA, et al. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand Hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med 2010;38:448–54. [DOI] [PubMed] [Google Scholar]
- [37].Ibrahim SA, Al-Kussary IM, Al-Misfer AR, et al. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: Patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy 2005;21:412–7. [DOI] [PubMed] [Google Scholar]
- [38].Lidén M, Kartus J, Sernert N, et al. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-Year follow-up. Am J Sports Med 2007;35:740–8. [DOI] [PubMed] [Google Scholar]
- [39].O’Neill DB. Arthroscopically assisted reconstruction of the anterior cruciate ligament: a follow-up report. J Bone Joint Surg Am 2001;83:1329–32. [DOI] [PubMed] [Google Scholar]
- [40].Wipfler B, Donner S, Zechmann CM, et al. Anterior cruciate ligament reconstruction using patellar tendon versus Hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy 2011;27:653–65. [DOI] [PubMed] [Google Scholar]
- [41].Zaffagnini S, Marcacci M, Presti ML, et al. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc 2006;14:1060–9. [DOI] [PubMed] [Google Scholar]
- [42].Webster KE, Feller JA, Hartnett N, et al. Comparison of patellar tendon and Hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med 2016;44:83–90. [DOI] [PubMed] [Google Scholar]
- [43].Nawabi DH, van der List JP, Williams A. Technical considerations for patellar tendon harvest. Springer Berlin Heidelberg 2017. 103–20. [Google Scholar]
- [44].Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 2001;17:971–80. [DOI] [PubMed] [Google Scholar]
- [45].Higuchi H, Kobayashi A, Ikeda K, et al. Efficacy of β-tricalcium phosphate graft into the bone defects after bone-patellar tendon-bone anterior cruciate ligament reconstruction. J Knee Surg 2017;30:467–73. [DOI] [PubMed] [Google Scholar]
- [46].Tsuda E, Okamura Y, Ishibashi Y, et al. Techniques for reducing anterior knee symptoms after anterior cruciate ligament reconstruction using a bone-patellar tendon-bone autograft. Am J Sports Med 2001;29:450–6. [DOI] [PubMed] [Google Scholar]
- [47].Kartus J, Ejerhed L, Sernert N, et al. Comparison of traditional and subcutaneous patellar tendon harvest. A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med 2000;28:328–35. [DOI] [PubMed] [Google Scholar]
- [48].Gaudot F, Leymarie JB, Drain O, et al. Double-incision mini-invasive technique for BTB harvesting: its superiority in reducing anterior knee pain following ACL reconstruction. Orthop Traumatol Surg Res 2009;95:28–35. [DOI] [PubMed] [Google Scholar]
- [49].Drogset JO, Strand T, Uppheim G, et al. Autologous patellar tendon and quadrupled hamstring grafts in anterior cruciate ligament reconstruction: a prospective randomized multicenter review of different fixation methods. Knee Surg Sports Traumatol Arthrosc 2010;18:1085–93. [DOI] [PubMed] [Google Scholar]
- [50].Woo LY, Hollis JM, Adams DJ, et al. Tensile properties of the human femur-anterior cruciate ligament-tibia complex: the effects of specimen age and orientation. Am J Sports Med 1991;19:217–25. [DOI] [PubMed] [Google Scholar]
- [51].Cooper DE. Biomechanical properties of the central third patellar tendon graft: effect of rotation. Knee Surg Sports Traumatol Arthrosc 1998;6:S16–9. [DOI] [PubMed] [Google Scholar]
- [52].Hamner DL, Brown CH, Steiner ME, et al. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: Biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 1999;81:549–57. [DOI] [PubMed] [Google Scholar]
- [53].Samuelsen BT, Webster KE, Johnson NR, et al. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate?A meta-analysis of 47,613 patients. Clin Orthop Relat Res 2017;475:2469–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Hildebrandt C, Muller L, Zisch B, et al. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part I: development of a new test battery. Knee Surg Sports Traumatol Arthrosc 2015;23:1273–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Lephart SM, Perrin DH, Fu FH, et al. Relationship between selected physical characteristics and functional capacity in the anterior cruciate ligament-insufficient athlete. J Orthop Sports Phys Ther 1992;16:174–81. [DOI] [PubMed] [Google Scholar]
- [56].Herbst E, Hoser C, Hildebrandt C, et al. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part II: clinical application of a new test battery. Knee Surg Sports Traumatol Arthrosc 2015;23:1283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Jang SH, Kim JG, Ha JK, et al. Functional performance tests as indicators of returning to sports after anterior cruciate ligament reconstruction. Knee 2014;21:95–101. [DOI] [PubMed] [Google Scholar]
- [58].Gustavsson A, Neeter C, Thomee P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2006;14:778–88. [DOI] [PubMed] [Google Scholar]
- [59].Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med 1991;19:513–8. [DOI] [PubMed] [Google Scholar]
- [60].Itoh H, Kurosaka M, Yoshiya S, et al. Evaluation of functional deficits determined by four different hop tests in patients with anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc 1998;6:241–5. [DOI] [PubMed] [Google Scholar]
- [61].Shino K, Pflaster DS. Comparison of eccentric and concentric screw placement for hamstring graft fixation in the tibial tunnel. Knee Surg Sports Traumatol Arthrosc 2000;8:73–5. [DOI] [PubMed] [Google Scholar]
- [62].Cristiani R, Sarakatsianos V, Engström B, et al. Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: a cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2019;27:381–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Wall A, Board T. Tendon Healing in a Bone Tunnel: A Biomechanical and Histological Study in the Dog. 2014;London: Springer, 453–456. [Google Scholar]
- [64].Mayr HO, Stoehr A, Dietrich M, et al. Graft-dependent differences in the ligamentization process of anterior cruciate ligament grafts in a sheep trial. Knee Surg Sports Traumatol Arthrosc 2012;20:947–56. [DOI] [PubMed] [Google Scholar]
- [65].Belk JW, Kraeutler MJ, Carver TJ, et al. Knee osteoarthritis after anterior cruciate ligament reconstruction with bone-patellar tendon-bone versus Hamstring tendon autograft: a systematic review of randomized controlled trials. Arthroscopy 2018;34:1358–65. [DOI] [PubMed] [Google Scholar]
- [66].Brophy RH, Cai L, Duan X, et al. Proteomic analysis of synovial fluid identifies periostin as a biomarker for anterior cruciate ligament injury. Osteoarthritis Cartilage 2019;27:1778–89. [DOI] [PMC free article] [PubMed] [Google Scholar]


