Abstract
Purpose
Safety culture is known to be related to a wide range of outcomes, and measurement of safety culture is now required for many hospitals in the U.S.A. In previous reviews, the association with outcomes has been limited by the research design and strength of the evidence. The goal of this review was to examine recent literature on the relationship between safety culture and infection prevention and control-related (IPC) processes and healthcare-associated infections (HAIs) in U.S. healthcare organizations. We also sought to quantitatively characterize the challenges to empirically establishing these relationships and limitations of current research.
Recent Findings
A PubMed search for U.S. articles published 2009–2019 on the topics of infection prevention, HAIs, and safety culture yielded 448 abstracts. After screening, 55 articles were abstracted for information on purpose, measurement, analysis, and conclusions drawn about the role of safety culture in the outcome. Approximately ½ were quality improvement (QI) initiatives and ½ were research studies. Overall, 51 (92.7%) concluded there was an association between safety culture and IPC processes or HAIs. However, only 39 studies measured safety culture and 26 statistically analyzed safety culture data for associations. Though fewer QI initiatives analyzed associations, a higher proportion concluded an association exists than among research studies.
Summary
Despite limited empirical evidence and methodologic challenges to establishing associations, most articles supported a positive relationship between safety culture, improvement in IPC processes, and decreases in HAIs. Authors frequently reported experiencing improvements in safety culture when not directly measured. The findings suggest that associations between improvement and safety culture may be bi-directional such that positive safety culture contributes to successful interventions and implementing effective interventions drives improvements in culture. Greater attention to article purpose, design, and analysis is needed to confirm these presumptive relationships.
Keywords: Safety culture, Infection prevention and control, Healthcare-associated infections, Organizational culture
Introduction
Why Understand the Relationship Between Safety Culture, Infection Prevention and Control, and Healthcare-Associated Infections
Given the major impact of healthcare-associated infections (HAI) on morbidity, mortality, and costs of care, there have been many efforts to prevent HAIs by improving infection prevention and control (IPC) practices in the last 20 years. These include establishing the U.S. Department of Health and Human Services (DHHS) National HAI Action Plan, required reporting of hospital HAIs to the Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN), state-based HAI prevention activities, Joint Commission National Patient Safety Goals specific to HAIs, public reporting of HAIs in Medicare data, and U.S. Agency for Healthcare Research and Quality (AHRQ) healthcare-associated infections program [1–8]. While substantial progress has been made, it remains difficult to ascertain the impact of individual initiatives on overall progress [9, 10].
Safety culture is one factor considered in recent years to have a major impact on patient outcomes including HAIs [11, 12]. The often-stated phrase “culture eats strategy for lunch (and breakfast and dinner)” exemplifies its presumed importance [13, 14]. Several initiatives are underway to improve culture related to patient and staff safety within healthcare settings [15–17]. Culture is also closely related to leadership [18–20].
What Is Safety Culture
Safety culture has been defined as the product of individual and group beliefs, values, attitudes, perceptions, competencies, and patterns of behavior that determine the organization’s commitment to quality and patient safety [21]. According to AHRQ, a culture of safety encompasses four key principles:
Acknowledgment of the high-risk nature of an organization’s activities and the determination to achieve consistently safe operations
A blame-free environment where individuals can report errors or near misses without fear of reprimand or punishment
Encouragement of collaboration across ranks and disciplines to seek solutions to patient safety problems
Organizational commitment of resources to address safety concerns [22].
The terms safety culture, safety climate, and organizational culture are conceptually distinct but often used interchangeably. Organizational culture refers to the deeply embedded norms, values, beliefs, and assumptions shared by members of an organization [23]. These elements evolve over time and are difficult to change. Organizational climate, by contrast, refers to the shared perceptions at a given point in time regarding organizational practices such as decision-making, advancement opportunities, and so on. These are more amenable to change. Safety climate is a subset (or microclimate) of overall organizational climate that focuses on people’s perceptions about the extent to which the organization values safety (for workers, patients, and/or the environment) [12, 24–26]. In this article, we use the broader term safety culture to include studies addressing safety climate and organizational climate when appropriate.
Why Safety Culture Should Be Measured
Healthcare quality oversight bodies and related groups recommend organizations address safety culture. Organizations accredited by The Joint Commission are expected to ensure that leaders maintain a culture of safety and regularly evaluate the culture using valid and reliable tools [27]. The National Quality Forum recommended measurement of culture in its Safe Practices for Healthcare [28]. Similarly, The Leapfrog Group, which conducts hospital surveys related to quality and safety, incorporates measurement and use of safety culture data in its ratings of hospital performance [29]. AHRQ also recommends yearly measurement of safety culture as one of its ten patient safety tips for hospitals [30]. The 2020 Institute for Healthcare Improvement (IHI) National Patient Safety Action Plan recommends assessing safety culture at least every 2 years [31].
The mechanism by which safety culture can influence the IPC process and HAIs has been described in several conceptual models, many of which derive from Donabedian’s model of structure, process, and outcome [25, 32]. Figure 1 presents a simplified conceptual model for the relationship between safety culture, IPC processes, and HAI rates derived from the previous work. Essentially, the input of individual characteristics (both patients and staff) interacts with organizational structural factors (such as staffing, equipment) and culture of safety (impacted by leadership) which then influences the process of care (e.g., adherence to recommended IPC processes such as contact precautions and hand hygiene). These inputs in turn collectively affect the outcome of HAIs for both patients and staff.
Fig. 1.
Conceptual framework for safety culture and infection prevention and control-related (IPC) process and outcomes
There is evidence from the Comprehensive Unit-based Safety Program (CUSP) initiative that driving large-scale improvement in IPC practices and HAI rates requires multi-faceted strategies that address clinician knowledge attitudes and behaviors as well as organizational factors. The CUSP implementation framework includes engagement of frontline clinicians and institutional senior leadership; education in the science of safety; assessment of safety culture and infection control policies and procedures; regional consortia of stakeholders; expert coaching, consultation, and technical assistance; peer support; educational materials, tools, and webinars; data collection and feedback for performance monitoring; and patient and family engagement. Originally demonstrated in the Michigan Keystone Project Collaborative ICU initiative to reduce central line–associated bloodstream infections (CLABSI), AHRQ has supported the implementation and evaluation of the CUSP model nationally and its application to other types of HAIs (e.g., catheter-associated urinary tract infections (CAUTI) and ventilator-associated pneumonia (VAP)) and settings (nursing homes, dialysis) as well as other outcomes [33, 34]. Safety culture remains a key component of the CUSP initiatives.
There are additional reasons to understand the relationship between safety culture, IPC process, and HAIs. If a strong relationship exists, one can focus interventions on improving safety culture. In theory, an intervention that improves safety culture could also improve non-IPC-related outcomes (“lift all boats”). For example, a recent systematic review of 62 high-quality studies by Braithwaite et al. found that positive organizational and workplace cultures were associated with a variety of patient outcomes such as reduced rates of mortality, falls, and HAIs and increased patient satisfaction [35]. Though a discussion of strategies to improve safety culture is beyond the scope of this article, there is little research on the modifiability of culture beyond knowing it to be a slow process and difficult to accomplish [36–39].
Another reason to understand the relationship between safety culture, IPC, and HAIs is to establish the value (or lack thereof) of safety culture measurement and analysis activities. Collecting and analyzing safety culture data can require significant effort, burden, and expense [40, 41]. The evidence base is needed to help justify these efforts.
Research on Safety Culture and Outcomes
Previous systematic reviews have examined the relationship between safety culture and the IPC process and/or HAIs. These reviews have been generally supportive of the relationship between these factors but are based on limited evidence. One systematic review examined the relationship between patient safety climate and adherence to standard precautions. After excluding intervention studies, Hessels and Larson found only 7 studies eligible for inclusion, all of which were cross-sectional designs [42•]. A recent systematic review by van Buitjene included 20 studies and found 90% produced supportive evidence for the hypothesis of a link between organizational culture and HAI rates, despite the fact that 8 included studies did not actually measure safety culture [43••]. DeBono synthesized studies on the relationship between organizational culture and behavioral attitudes toward IPC [44••]. They found that effective IPC relies directly upon the successful interplay of multiple management systems strongly influenced by corporate culture, and that improving organizational culture appears to be a promising albeit challenging target for IPC improvement campaigns, although better-quality studies are urgently needed.
Challenges to Linking Safety Culture, Infection Prevention and Control Activities, and Outcomes
There are several reasons why establishing a causal relationship between safety culture, IPC processes, and HAIs has been difficult in previous research. Challenges to measurement and analysis for each of these areas are described below.
Safety Culture
Studies that measure safety culture often use different instruments which vary in psychometric properties such as reliability, validity, and sensitivity to change [45].
Perceptions of safety culture are not necessarily related to actual practice. For example, a qualitative study by Szymczak eloquently describes how the situational complexity of interactions affects both the willingness and ability of staff to “speak up” to prevent an error [46].
Analyses of safety culture data may be too simplistic. For example, researchers debate whether to aggregate levels of agreement (consensus) within units and domains or to analyze data using dispersion models in which variability, the degree of disagreement among respondents, is more informative [47, 48].
Infection Prevention and Control Practices
Measuring adherence to IPC practices is not easy. There is no nationally standardized approach for hand hygiene measurement in the U.S.A., and interpretation of rates is often affected by threats to validity, such as the Hawthorne effect, and insufficient numbers of observations [49]. Measuring adherence to evidence-based care bundles using checklists, while more comprehensive, can be time consuming and variable in approach, timing, and numbers [50].
Healthcare-Associated Infections
Measurement of HAIs, though more standardized than IPC, is heavily dependent on time frames and surveillance processes. Some HAIs are more reliable to collect than others [51]. The unit of measurement—ICU level, hospital-wide, single HAI or multiple—also varies.
Factors that directly influence development of HAIs often differ according to the HAI of interest and are greatly affected by patient risk characteristics such as co-morbidities [52].
Establishing attribution for the HAI is challenging. As described by Gardam, during a hospital stay, a patient can be exposed to thousands of different environmental and human contacts that may lead to an infection [37]. While only one exposure may lead to infection, it is nearly impossible to determine which one was responsible.
Directionality and Causation
Directionality for cause and effect regarding IPC improvement and safety culture remains to be established. For example, can improving IPC processes result in enhanced safety culture or does improvement in safety culture result in better IPC processes?
The ability to establish relationships and causality is, of course, affected by the purpose of the initiative as well as the study design [53]. Articles are often based on uncontrolled, pre-post intervention QI projects never intended to be considered research studies [54–56]. However, some consider QI initiatives to be quasi-experimental designs when using pre-post or time series approaches, particularly when there is a control group [57]. While the common goal includes improving care processes and outcomes, QI research is distinct in its focus on broader, generalizable research questions with hypotheses, multiple sites, and advanced statistical analysis [58].
Purpose of This Review
In previous reviews, the association with outcomes has been limited by the research design and strength of the evidence. Authors rarely distinguished between reports of QI initiatives and research studies or explored safety culture measurement issues. For this review, we examined authors’ findings and interpretation of the relationship between safety culture, IPC processes, and HAIs in both QI and research articles. We also sought to quantitatively characterize the variation in measurement of safety culture, the IPC process, and HAIs. Though not intended to be a comprehensive scoping or systematic literature review, we performed a new search of PubMed to identify recent articles in this topic area.
Methods
Data Sources and Search Strategy
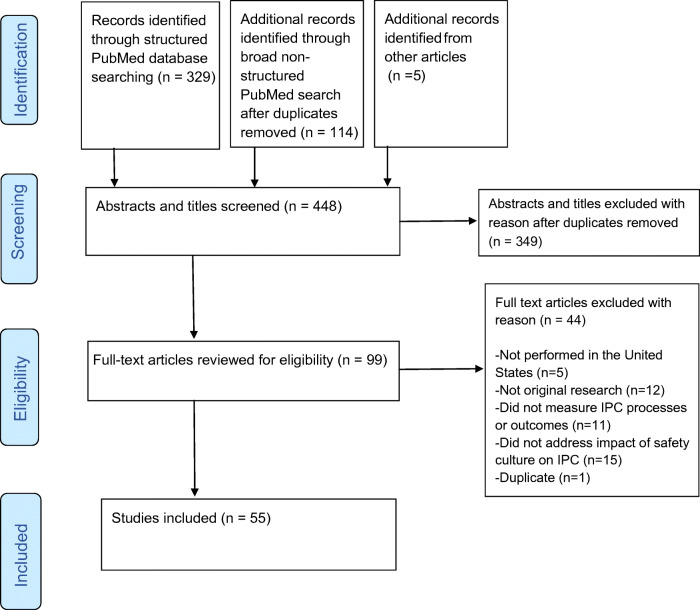
Two literature searches were performed by medical librarians. A structured literature search of PubMed was performed in November 2019 for relevant articles across all healthcare settings, published in English language in the past 10 years that included safety culture and infection control process and/or infection control outcomes. To broaden the search of safety culture, we also included terms such as safety climate and organizational culture. Shortly thereafter, a second broad non-structured search was also performed. The unstructured search utilized free text of terms “infection prevention and safety culture” and the “similar articles” function. The first search yielded 329 and the second yielded 114 abstracts and titles. An additional five records were identified from references in other articles. A total of 448 abstracts and titles were retrieved.
Eligibility Criteria, Screening, and Characterization Process
After de-duplication by the librarians, two researchers screened the 448 titles and abstracts for eligibility. We included studies that measured infection prevention processes or HAIs and also measured safety culture or included an intervention or objective to improve safety culture. We excluded commentaries, editorials, and related articles that were not studies or QI initiatives, and all articles involving healthcare organizations from outside the U.S.A. After 448 abstracts were screened, 99 full text articles were assessed for eligibility for inclusion and a total of 55 articles were included (Fig. 2).
Fig. 2.
PRISMA flow diagram for literature review process
Study data were collected and managed using a standardized data abstraction form in Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the University of Iowa [59, 60]. REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources.
Five researchers were sequentially assigned to abstract information from the 55 articles. Reviewers documented safety culture measurement and domains; conceptual model used, if any; IPC process(s) measured; HAIs measured; study-reported findings and relation to safety culture; and added comments. All articles were also classified by type as being either QI or research; research studies were then categorized by study design as qualitative, cross-sectional, or quasi-experimental.
Each full-text article was reviewed by one researcher. However, when the researcher had doubts regarding the inclusion/exclusion criteria of an article or results were not clear, the article was independently reviewed by a second reviewer. Eighteen articles were reviewed by at least two reviewers. Disagreements between reviewers were discussed and resolved by group consensus. Since the review focused exclusively on published articles, it was not considered to be human subject research.
What Does the Research Show
Settings and Populations
Of 55 articles, most (49, 89.1%) were based on initiatives in hospitals, 6 of which focused on pediatric populations and 3 on veterans. Other settings included nursing homes (n = 3), dialysis clinics (n = 2), and dental offices (n = 1). The majority, 36 (65.5%), involved multiple sites and 19 were single-site studies.
Purpose and Design
When stratified by type, slightly more than ½ (28, 50.9%) were primarily QI initiatives, four of which were large scale involving more than 100 sites [33, 61–63]. The remaining 27 were research articles with the following designs: 17 cross-sectional, 6 quasi-experimental, and 4 qualitative.
Thirty-eight articles (69.1%) included an intervention, 15 of which utilized the CUSP approach.
Safety Culture Measurement
Articles varied considerably in measuring safety culture with respect to instruments, mode of survey administration, timing relative to an intervention (e.g., baseline only or multiple measurements over time), unit of analysis (e.g., hospital-wide or ICU specific), and respondents (e.g., all staff vs only infection prevention leaders). Overall, 39 (70.9%) articles measured safety culture with a standardized tool such as the AHRQ Hospital Survey of Patient Safety Culture (HSOPSC) (n = 16) [47, 64–78]; Nursing Home Survey on Patient Safety Culture (NHSPSC) (n = 2) [79, 80]; the Safety Attitudes Questionnaire (SAQ) (n = 9) [62, 81–87]; the National Database of Nursing Quality Indicators (NDNQI) (n = 2) [74, 88]; or qualitative methods (n = 4). Not all articles mentioned which safety culture domains were assessed, while some only assessed one domain of safety culture (e.g., teamwork) [78, 84].
Of the 39 articles, 25 (64.1%) measured safety culture at a single point in time (e.g., baseline) while 14 (35.9%) measured safety culture multiple times over the study period.
Most measurements occurred at a hospital level, but some were performed at a unit level: ICUs or NICUs (n = 11), surgical units (n = 2), cardiac surgery unit (n = 1), medical wards (n = 1), medical unit for the elderly (n = 1), and hemato-oncology unit (n = 1). Of note, eight articles reported information from hundreds of ICUs [47, 61–63, 69, 82, 89, 90] and at least two articles reported data from a wide variety of both ICU and non-ICU units [63, 68].
Most respondents to the safety culture assessments were physicians, nurses, and other staff working in the participating units. However, some articles focused exclusively on hospital epidemiologists or infection preventionists (such as [89, 91–93]), nurses (such as [64, 76, 94]), or members of a dental hygienist professional association [95].
Research articles measured safety culture more frequently than QI articles. All the 27 research articles measured safety culture compared with less than ½ of QI articles (12 of 28).
Outcomes of Interest: IPC Processes of Care and HAIs
Tables 1, 2, and 3 describe which aspects of IPC process were evaluated, what HAIs were measured, and the author’s findings and conclusions on the relationship between safety culture and IPCs and/or HAIs.
Table 1.
Studies on the relationship between safety culture and infection prevention and control processes
| First author, year | Design, number and types of sites or units and study period | Intervention(s) | Safety culture measurement tool and domains | Infection prevention and control process(s) measured | Study-reported findings and relation to safety culture | Comments |
|---|---|---|---|---|---|---|
| Daugherty 2012 | Cross-sectional research; 46 units in 1 academic hospital; 6-month period between 2009 and 2010 | No intervention | Safety Attitudes Questionnaire (SAQ): teamwork, safety climate, management support, job satisfaction, stress recognition, working conditions, perceptions of hospital management, and perceptions of unit management | Hand hygiene adherence |
Higher safety culture scores were significantly associated with higher hand hygiene adherence across 4 SAQ domains (safety climate, job satisfaction, working conditions, and perceptions of hospital management Significant absolute differences of 5–8% in mean hand hygiene adherence were found between units with the highest domain scores and those with the lowest domain scores. “It remains unclear whether certain domains are more significant than others in predicting staff behaviors” |
Single time measurement of safety culture Single-site study |
| Garland 2013 | Cross-sectional research; proportional stratified random sample of dental hygienists across about 750 offices; study period not reported | None |
Questionnaire regarding attitudes about infection control guidelines: knowledge, attitudes and practice behaviors, dentists’ barriers influencing implementing infection control guidelines, and compliance with practice guidelines. Items include supervisor expectations and access to infection control supplies. Qualitative thematic analysis of open-ended questions |
Dental hygienists self-reported compliance with infection control guidelines |
Significant association between the attitude that “infection control is not practical” and other negative attitudes: infection control guidelines are inconvenient and cumbersome to use (Spearman Rho rs = 0.540), having no time to use infection control guidelines (rs = 0.582), and not wanting to change infection control behaviors (rs = 0.549) Significant association between infection control guidelines implementation and positive attitudes regarding: familiarity with the infection control guidelines (rs = 0.537), belief in the relevance of infection control guidelines to patients (rs = 0.462), access to necessary supplies (rs = 0.549), belief that supervisors expects them to use infection control guidelines (rs = 0.529). “Higher compliance with infection control guidelines was associated with positive safety beliefs and practices. Safety culture appears to be a factor in compliance with infection control guidelines” |
Single time measurement of safety culture 99% of respondents belonged to the American Dental Hygienists’ Association; results might not be representative of members of other professional associations |
| Hessels and Genovese-Schek 2016 | Cross-sectional research; 11 units in 5 hospitals including community, acute care, trauma, teaching and non-teaching; 7-month period in 2015 | No intervention | Two tools combined: (1) Hospital Survey on Patient Safety Culture (HSOPSC): teamwork within units, supervisor/manager expectations and actions promoting patient safety, organizational learning-continuous improvement, management support for patient safety, overall perceptions of patient safety, feedback and communication about error, communication openness, teamwork across units, staffing, handoffs and transitions, nonpunitive response to errors; and (2) Gershon Standard Precaution and Safety Climate Survey: frequency of events reported, standard precaution practices, standard precaution environment | Adherence to standard precautions. Specifically, hand hygiene, personal protective equipment, disposal of needles or other sharp, and soiled linen handling |
Although 94% of nurses reported positive scores on unit safety climate, observed standard precautions adherence was 62% (unit range 31–80%) Better self-reported staffing was significantly associated with lower standard precautions adherence (r2 = − 0.85, p = 0.03) but not teamwork within units (r2 = − 0.6, p = 0.09). Significant relationships between safety climate dimensions and specific standard precautions items included: teamwork within units and sharps adherence (r2 = − 0.75, p = 0.03); management support for patient safety and hand hygiene (r2 = − 0.70, p < 0.01); staffing and hand hygiene (r2 = − 0.84, p < 0.01). “The relationship between safety climate and adherence to standard precautions warrants further investigation.” |
Single time measurement of safety culture Nurses were the only respondents for culture measurement |
| Hsu 2020 (ePub 2015) |
Cross-sectional research; 103 ICUs in Michigan Keystone project; 2004 |
Adoption of CUSP | Safety attitudes questionnaire, (scales of teamwork climate, safety climate, job satisfaction, stress recognition, perceptions of management, and working conditions) | Process was assessed at ICU level regarding willingness to adopt CUSP interventions | ICUs with lower perceived safety climate, greater stress recognition, higher perceptions of management, and better working conditions were more likely to adopt CUSP | Safety culture at baseline was used in the analysis |
| Lyles 2014 | Qualitative research; 4 long-term acute-care hospitals; 2012 | None | 18 items from a previously validated tool by Sinkowicz-Cochran | Attitudes and beliefs about a Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae (KPC) control program and QI at the facility | Administrative staff reported higher organizational culture than frontline staff. The high degree of convergence in motivation, understanding, and beliefs related to implementation of a KPC control bundle suggests that all levels of staff may be able to align perspectives when faced with a key infection control problem and quality improvement initiative | |
| Meeks 2011 | Cross-sectional research; 2 county hospitals; 2006–2008 | None | Safety Attitudes Questionnaire; domain of teamwork safety climate. Also, another potential measure of teamwork, time from entry into the operating room to time to incision (cut time) | Compliance with all Surgical Care Improvement Project antibiotic prophylaxis guidelines |
Gynecologic surgery was the only independent predictor of compliance for elective procedures. Contrary to expected, safety domain scores and agreement with statements on collaboration and teamwork were not predictive of compliance. However, a shorter surgical cut time, particularly in emergency cases, was identified at the hospital with better teamwork scores. |
Safety culture measured at a single point in time Did not find significant association |
| Miller M 2012 | Cross-sectional research; 386 academic and community hospitals with intensive care units; 2003–2009 | None | A 5-point Likert scale measuring 3 items: leadership driving safety culture, staff receptivity to change in clinical processes, whether the respondent would feel safe being treated at the facility as a patient. Respondents were lead infection control professionals. | Daily interruption of sedation in mechanically ventilated patients |
Leadership emphasis on safety culture (odds ratio 1.87, 95% confidence interval 1.02–3.43); staff receptivity to change (odds ratio 2.17, 95% confidence interval 1.16–4.06); and involvement in an infection prevention collaborative (odds ratio 1.78, 95% confidence interval 1.02–3.12) significantly associated with daily interruption of sedation use The perception by respondents that they “would feel safe being treated” at the hospital was not statistically associated with routine use of daily interruption of sedation |
Safety culture measured at a single point in time |
| Nelson 2011 | Two cross-sectional research surveys; 149 academic and community hospitals; fall 2008 | No intervention | Two tools adapted from Patient Safety Climate in Healthcare Organizations (PSCHO), including: (1) Senior Management Engagement scale: understanding of current safety issues in the facility, taking supportive care when necessary, appreciating that frontline care providers are often best qualified to solve patient safety issues; and (2) Leadership on Patient Safety scale: senior executives’ ability to articulate values consistent with patient safety and reducing hospital-associated infections | Measures of structure: presence of hospital epidemiologist and infection preventionist |
An independent budget for the infection prevention and control department was a significant predictor of more positive perceptions of safety culture Infection preventionists perceived senior management engagement more positively than quality directors (21.4% vs 20.4%, p < 0.01) |
Single time measurement of safety culture This study evaluated measures of structure (not a process). It examined perceptions of two patient safety climate measures from infection preventionists and quality directors |
| Pogorzelska-Maziarz 2016 | Cross-sectional research; 972 teaching and non-teaching acute-care hospitals; winter 2011 | No intervention |
Leading a Culture of Quality for Infection Prevention (LCQ-IP): quality focus, change orientation, openness, change actions, work group cooperation and respect, alignment (with leadership and direction), accountability, workload, psychological safety. Respondents were infection preventionists. |
CLABSI policies | Mean LCQ-IP scores increased with number of CLABSI policies in place (p = 0.047) |
Single time measurement of safety culture. Study goal was to evaluate psychometric properties of the LCQ-IP instrument; study findings supported tool validity |
| Robbins 2016 |
Qualitative; 158 key informants; 6 hospitals; study period not specified |
Comprehensive unit-based safety programs (CUSP) —Stop BSI initiative | Qualitative methods addressed management and organizational factors that contribute to creating a nonpunitive environment for speaking up | How hospital CLABSI prevention efforts encouraged or hindered employees’ efforts to speak up to prevent errors or identify opportunities for improvement | Leader behavior, employee training, and error reporting systems facilitated employees improvement-oriented speaking in hospitals implementing evidence-based practices for CLABSI prevention | |
| Sinkowitz-Cochran 2012 | Two cross-sectional research surveys; 16 VA Medical Centers; October 2006 and July 2007 | None | Organizational Culture (OC) – staff engagement, overwhelmed stress/chaos, leadership | Hand hygiene; gowning and gloving practices |
Higher staff engagement and hospital leadership were associated with better hand hygiene (p < 0.01 and = 0.04, respectively) and gowning/gloving practices (p < 0.01). Conversely, higher overwhelmed/stress-chaos scores were associated with poorer hand hygiene (p < 0.01) and gowning/gloving practices (p < 0.01). All 3 OC factors of Staff Engagement, Hospital Leadership, and Overwhelmed/Stress-Chaos were significantly associated with gowning and gloving among nurses (p < 0.01, < 0.01, and = 0.02, respectively). “Differences by job type also suggest that OC may influence not only knowledge and attitudes of health care personnel, but also practices and outcomes.” |
Multi-site study evaluated differences in organizational culture by staff role |
| Talbot 2013 | QI initiative; 1 academic medical center; 2009–2012 | To improve hand hygiene adherence and align efforts with pursuit of a culture of safety, the hospital adopted multiple strategies including training, peer feedback, marketing and financial incentives, as well as structured unit-based and individual accountability interventions | Not measured directly, although the response of underperforming units’ improvement plans provided leaders with insight into the safety culture in each poorly performing clinical area (e.g., exhibiting a collegial mindset and desire to work as a team or, alternatively, dysfunction and a lack of leadership) | Hand hygiene | Improvements in hand hygiene were sustained across the entire health system. Leadership engagement through a formal accountability structure coupled with institutional financial incentives encouraged both nursing and physician leadership to pursue a culture of consistent, sustained HH adherence | Safety culture not measured |
| Yanke 2018 | Qualitative study; one VA 57-bed facility; July–November 2013; four focus groups including attending physicians (1), resident physicians (1), and RNs and HTs (2) |
Department of Veteran Affairs C. difficile prevention bundle |
Qualitatively identified domains include organizational support, communication | C. difficile prevention bundle adherence, hand hygiene; contact isolation precautions | Following hand hygiene protocol of increased time required for handwashing and contact isolation precautions were prominent barriers to bundle adherence among all groups. Another barrier was patient care workload |
Table 2.
Studies on the relationship between safety culture and healthcare-associated infections
| Authors, year | Design and number of sites or units; study period | Intervention(s) | Safety culture measurement and domains | Healthcare-associated infection(s) measured | Study-reported findings and relation to safety culture | Comments |
|---|---|---|---|---|---|---|
| Abusalem 2019 | Cross-sectional research; 5 Medicaid-certified long-term care facilities; 2014 | None | Nursing Home Survey on Patient/Resident Safety Culture (NHSPSC): teamwork, staffing, compliance with procedures, training and skills, nonpunitive response to mistakes, handoffs, feedback and communication about incidents, supervisor expectations and actions promoting resident safety, overall perceptions of resident safety, management support for resident safety, organizational learning | UTIs |
The risk of UTI rates increased with greater number of residents (risk ratio 1.01, 95% confidence interval 1.01–1.01), with greater licensed practical nurse/licensed vocational nurse hours per resident day (risk ratio 61.5, 95% confidence interval 36.3–102.4), and decreased 79% with higher total number of licensed nursing staff hours per resident day (risk ratio 0.21, 95% confidence interval 0.15–0.31) Culture of safety was significantly associated with reduced rates for UTIs (risk ratio 0.80, 95% confidence interval 0.75–0.86) Handoffs between nursing shifts was inversely related to UTIs (r = − 0.143, p < 0.05) “There is a need to build strong culture of safety and foster patient-centered culture of safety attributes among nursing staff providing care in long-term care facilities” |
Single time measurement of safety culture |
| Braddock 2015 (ePub 2014) | QI initiative; 4 medical and surgical units in an academic medical center; 2009–2011 | Four improvement strategies: (1) early detection and treatment of hospital complications with in situ simulation training; (2) identification of safety risks by debriefing of medical urgencies and emergencies; (3) quality improvement of interdisciplinary care issues; (4) individual recognition of exemplary teamwork performance | Hospital Survey on Patient Safety Culture (HSOPSC): teamwork within units, manager expectations, organizational learning, management support, error feedback and communication, communication openness, non-punitive response, staffing, teamwork across units, handoffs and transitions, overall perceptions of safety outcomes, frequency of events | Hospital-acquired severe sepsis/septic shock |
Rates of hospital-acquired severe sepsis/septic shock decreased from 1.78 to 0.64 per 1000 unit discharges Scores of safety culture significantly improved after the 1-year intervention for nurses (64.9% to 84.7%; p < 0.001), but not for residents (61.2 to 65.8%; p = 0.06) Scores significantly improved in 9 out of 12 survey dimensions for nurses, compared to 4 dimensions for residents “Interventions led to the discovery of safety issues on clinical microsystems that involved complex, interdisciplinary care practices that directly influenced patient safety” |
Safety culture measured at baseline and after 1 year Single-site study Did not statistically analyze the association between safety culture and outcomes Resident rotation to different medical centers and their intermittent presence on study units may have prohibited their exposure to program interventions and affected their perceptions of safety culture |
| Chang 2020 (ePub 2019) | QI initiative; cardiac surgery units in 11 hospitals (11 cardiovascular operating rooms, 8 ICUs, 9 floor units, 3 universal-bed units); 2011–2014 | Comprehensive Unit-based Safety Program* to improve safety culture and evidence-based bundles to prevent HAIs | Hospital Survey on Patient Safety (HSOPSC): teamwork within units, manager expectations and actions promoting safety, organizational learning, hospital management support, feedback and communication about error, communication openness, non-punitive response to error, staffing, teamwork across units, hospital handoffs and transitions, overall perceptions of safety, frequency of event reporting | CLABSI, SSI, and VAP |
CLABSI and SSI rates showed a downward trend over 2 years, then the rates returned to levels similar to baseline in the third year (after June 2013) VAP rates mostly remained at a median of zero throughout the project Significant improvement of the patient safety culture domain “hospital management support” on measurements at time points 2 and 3 compared to baseline. Significant decline in patient safety domains “feedback and communication errors, and staffing at time points 2/3 and time 3 compared to baseline, respectively “These findings highlight the importance of sustainment efforts and suggest future work should anticipate both positive and negative changes in safety culture dimensions” |
Safety culture was measured at 3 time points: baseline (July 2011–October 2011), time 2 (October 2012–March 2013), time 3 (April 2014–October 2014) VAP rate variations difficult to interpret because of changes in the VAP definition during the study period Did not statistically analyze the association between SC and outcomes |
| Fan 2016 | Cross-sectional research; surgical units in 7 community hospitals; 2012–2013 | No intervention | Hospital Survey on Patient Safety Culture (HSOPSC): overall perceptions of safety, supervisor expectation/actions, teamwork within units, communication openness, feedback, non-punitive response to error, staffing, management support, teamwork across units, handoffs and transitions, organizational learning, frequency of events reported | Colon SSI |
Safety culture scores ranged from 16 to 92 (on a scale from 0 to 100). Nine out of 12 dimensions were significantly associated with lower colon SSI rates Only three out of 12 dimensions (communication openness, staffing, and non-punitive response to error) were not associated with colon SSIs “These data suggest an important role for positive safety and teamwork culture and engaged hospital management in producing high-quality surgical outcomes” |
Single time measurement of safety culture |
| Harnage 2012 | QI initiative; 1 community hospital; 2005–2011 | Implementation of CLABSI bundle with 7 components along with education about the bundle | None | CLABSI |
CLABSI reduced to zero after implementation of a CLABSI bundle No findings related to culture beyond conclusions which state “The bundle might be insufficient if it was not executed by a skilled vascular access team and if that team was not supported by administrations who emphasized patient safety over all considerations” |
Safety culture not measured No baseline data of CLABSI rates provided |
| Hsu 2016 |
QI initiative; 103 ICUs in Michigan Keystone project; 2004–2006 |
Adoption of CUSP | Safety attitudes questionnaire, (scales of teamwork climate, safety climate, job satisfaction, stress recognition, perceptions of management, and working conditions) | CLABSI |
The use of CUSP was associated with improved safety climate, job satisfaction, and working conditions after a 2-year period. The use of CUSP was not associated with reduced CLABSI rates but insufficient data was considered to be inconclusive. |
Safety culture was measured at two time points |
| Kelly 2013 | Retrospective cross-sectional research; 320 hospitals; 2005–2008 | None | The Practice Environment Scale of the Nursing Work Index was used to measure critical care work environments: staffing and resource adequacy, nurse participation in hospital affairs, nursing foundations for quality of care, collegial nurse-physician relations, nurse manager ability, leadership and support of nurses | Nurse-reported frequency of CLABSIs, UTIs, VAPs |
Nurses working in better work environments were 36 to 41% less likely to report that healthcare-associated infections occurred frequently “Health care–associated infections are less likely in favorable critical care work environments. These findings, based on the largest sample of critical care nurses to date, substantiate efforts to focus on the quality of the work environment as a way to minimize the frequency of health care–associated infections” |
Single time measurement of safety culture Study based on critical care nurse work environment Respondents were nurses. |
| Meddings 2017 | Quasi-experimental research, two prospective cohort studies; 1079 hospitals for CLABSI and 949 hospitals for CAUTI; 2008–2011 for CLABSI and 2011–2013 for CAUTI | Interventions used principles from Comprehensive Unit-based Safety Program* | Hospital Survey on Patient Safety Culture (HSOPSC): expectations, teamwork within, communication, feedback, non-punitive, staffing, management support, teamwork across, handoffs, overall perceptions, continuous improvement, organizational learning, frequency of event reporting, patient safety grade | CLABSI, CAUTI |
Infection rates declined over the project periods (by 47% for CLABSI and 23% for CAUTI) No significant association between individual dimensions of safety culture with CLABSI or CAUTI outcomes measured at baseline or post-intervention. “It might be possible to improve CLABSI and CAUTI rates without making significant changes in safety culture, particularly as measured by instruments like Hospital Survey on Patient Safety Culture” |
Safety culture measured at baseline and again 1 year later (post-intervention) Study assessing two large national collaboratives focused on prevention of CLABSI and CAUTI Involved a large number and wide variety of hospitals and unit types (ICU and non-ICU) Did not find significant association |
| Miller K 2016 | QI initiative; 1 ICU each at 2 hospitals; 2010–2012 | Adoption of CUSP | Not measured | CLABSI, CAUTI, and VAP | Implementation of CUSP was associated with significant decreases in CLABSI, CAUTI, and VAP. CUSP principles created a process improvement culture... and allowed for a grassroots, frontline team-based approach…which not only improved accountability but also increased teamwork within the units. | Safety culture not measured |
| Phipps 2018 | QI initiative; 2014–2016; one 145-bed pediatric hospital | The No Harm Patient Safety Program included the following interventions: safety moments; leadership rounding; revising the cause analysis methodology; safety event reporting system enhancements; error prevention training; leadership methods training; identification of priority HACs; the Eye on Safety Campaign; and a safety coach program. | Not measured | CLABSI, CAUTI, SSI, ventilator-associated pneumonia (VAP), venous thrombo-embolism (VTE) |
CLABSI rate significantly declined from 2.8 per 1000 line-days in 2015 to 1.6 in 2016, for a difference of − 0.00118 (95% CI − 0.002270, − 0.00008; p = 0.036). SSI rates declined from a 2015 rate of 3.8 infections per 100 procedures to a 2016 rate of 2.6 (p = 0.2962) CAUTI rates declined from a 2015 rate of 2.7 per 1000 catheter-days to a 2016 rate of 1.4 (p = 0.2770). “Outcomes of the patient safety program demonstrated sustained mindfulness of safety as an organizational imperative.” |
Rates initially increased but were then followed by declines when interventions were fully in place |
| Profit 2017 | Cross-sectional research; 44 NICUs (10 regional, 28 community, and 6 intermediate); 2010–2012 | No intervention | Safety Attitudes Questionnaire (SAQ): teamwork items: “Nurse input is well received in this NICU”; “in this NICU, it is difficult to speak up if I perceive a problem with patient care”; “disagreements in this NICU are appropriately resolved”; “I have the support I need from others in this NICU to care for patients”; “It is easy for personnel here to ask questions when there is something they do not understand”; and “The physicians and nurses here work together as a well-coordinated team” | Hospital-associated infections in very low birth weight infants (without further detail) |
Teamwork climate was independently associated with hospital-associated infection rates (odds ratio 0.82, 95% confidence interval 0.73–0.92) “Improving teamwork may be an important element in infection control efforts” |
Single time measurement of safety culture Study focused on teamwork dimensions |
|
Profit 2020 (ePub 2018) |
Cross-sectional research; 44 NICUs in California; 2010 to 2012 | California Perinatal Quality Care Collaborative (details of which are not described in this paper) | Safety Attitude Questionnaire six domains: teamwork climate, safety climate, job satisfaction, perceptions of management, stress recognition, and working conditions | 9 perinatal-related metrics of quality in the composite outcome measure, one of which was healthcare-associated infection |
Of the 9 metrics, only HAI exhibited a statistically significant relationship with teamwork and safety climate. “Overall, our findings reflect a weaker than expected correlation of metrics of quality with teamwork and safety climate. Caution is needed in equating efforts to improve safety culture with expectations for broad-based quality improvement” |
Safety culture measured at single point in time |
| Richter 2018 | Quasi-experimental research; 435 hospitals; 75% of units were ICUs; 2009–2012 |
Comprehensive Unit-based Safety Program. A conceptual model was used: Standard Comprehensive Unit-based Safety Program model to fit High Reliability Organizations theory |
Hospital Survey on Patient Safety Culture (HSOPSC): supervisor support for safety, teamwork within units, communication openness, error feedback, non-punitive response to errors, staffing levels, management support, teamwork across units, successful handoffs, organizational learning, error reporting | CLABSI |
Units with stronger safety culture prior to Comprehensive Unit-based Safety Program implementation were significantly associated with zero or reduced CLABSI rates after implementation. Dimensions significantly associated with zero or reduced CLABSI rates were baseline organizational learning, communication openness, staffing, and teamwork across units |
Safety culture measured pre-intervention |
| Sakowski 2012 |
QI initiative; 6 community hospitals; 5 years (likely beginning in the end 2006 or 2007) |
Nurses led quality improvement councils and clinical transformation directors. Clinical champions. Each hospital chose 6 areas for improvement, but varied across sites. Education and training for all council members |
Hospital Survey on Patient Safety Culture (HSOPSC) Domains: not listed |
CLABSI, CAUTI, VAP |
Hospital-associated infection rates decreased during and after the intervention Favorable safety culture showed “modest increase” (57% pre-intervention and 61% post-intervention) Council participation improved job satisfaction. External support facilitated time dedicated to improvement “Staff-led councils have the potential to improve patient safety and quality of care” |
Safety culture measured pre- and post-intervention: at baseline, at year 2 and year 4 Statistical association between safety culture and hospital-associated infections was not analyzed Low survey response rate pre-intervention (27%), and this might limit the conclusions regarding the change in safety culture during the study period |
| Smith S A 2017 | Cross-sectional research; 164 hospitals; study period could not be determined | None |
AHRQ Hospital Survey on Patient Safety Culture (HSOPSC): 12 composites of patient safety culture 1. Communication openness 2. Frequency of events reports 3. Feedback and communication about error 4. Handoffs and transitions 5. Management support for patient safety 6. Nonpunitive response to error 7. Organizational learning 8. Overall perceptions of patient safety 9. Staffing 10. Supervisor/manager expectations and actions promoting patient safety 11. Teamwork across units 12. Teamwork within units |
Hospital-acquired infections (not specified) | Higher patient safety culture scores for four composites were associated with lower hospital-acquired infections, ranging from β = 0.19 to β = 0.24. | Single time measure of safety culture |
| Smith S N 2018 | Quasi-experimental research; prospective cohort study; 196 nursing homes; June 2014 and June 2016. Cohort entry was on rolling basis. Cohorts 1–3 had a 12-month intervention phase. Cohort 4 had a compressed timetable of 10 months. | Agency for Healthcare Research and Quality (AHRQ) Safety Program for Long-term Care: Preventing CAUTI and Other HAIs |
Nursing Home Survey on Patient Safety Culture (NHSPSC) Socio adaptive components—leadership engagement; empowering staff to implement change; and promoting effective team communication for supporting and implementing infection prevention activities |
Catheter-associated urinary tract infection rates (CAUTI) |
Nursing homes saw a 52% reduction in CAUTI rates over the intervention period. Multivariate models did not show a significant association between CAUTI rates and initial or over-time NHSOPS domains. |
Safety culture measured twice over time Did not find significant association |
| Sreeramoju 2018 | Quasi-experimental research; observational study; 6 medical wards at one 800-bed public academic hospital; retrospective 6-month baseline period, positive deviance (PD) intervention implemented over 9 months, with 9 months of follow-up |
3 units randomly assigned to intervention of positive deviance (PD) intervention on healthcare personnel (HCP). The PD approach explores the social aspects of infection prevention practices among HCP. In addition to identifying barriers and potential solutions, the approach focuses on identifying and deploying peer role models to generate positive peer pressure and mobilize change. |
Hospital survey of patient safety climate/culture (HSOPSC) adapted to infection prevention: Teamwork within teams, teamwork across teams, respect, safety climate, leadership, communication, frequency of events reported |
Monthly HAI rate—a composite of central line–associated bloodstream infection (CLABSI), Clostridium difficile infection (CDI), catheter-associated urinary tract infection (CAUTI), and hospital-acquired pneumonia (HAP) per 1000 patient-days |
Fitted time series of monthly HAI rates showed a decrease from 4.8 to 2.8 per 1000 patient-days (95% confidence interval [CI] 2.1 to 3.5) in wards without PD, and 5.0 to 2.1 per 1000 patient-days (95% CI − 0.4 to 4.5) in wards with PD. The measured patient safety culture was steady over time at 69% aggregate percent positive responses in wards with PD vs decline from 79 to 75% in wards without PD (F statistic 10.55; p = 0.005). “A positive deviance approach appeared to have a significant impact on patient safety culture among HCP who received the intervention.” |
Patient safety culture surveyed at 6, 15, and 24 months |
| Vigorito 2011 | Quasi-experimental research; 23 units from 11 hospitals; fall 2007 and 2008 | Rhode Island ICU Collaborative—a unit-based patient safety program and evidenced-based practices (see also DePalo 2010). This study tested the impact of a unit-level Safety Attitudes Questionnaire Action Plan (SAQAP). The action plan focused on interventions intended to improve safety culture (rather than clinical outcomes) | Safety Attitudes Questionnaire—safety climate, teamwork climate, job satisfaction, stress recognition, working condition, perception of management |
ICU central line-associated bloodstream infections (CLABSIs) per 1000 line days and ventilator-associated pneumonia (VAP) infections per 1000 ventilator days |
The 9 units that completed an SAQAP demonstrated a higher rate of improvement from 2007 to 2008 in five of six domains of safety culture, with teamwork climate and job satisfaction (p < .07). Nine units with an SAQAP decreased CLABSI rates by 10.2% in 2008 compared with 2007, while those without an SAQAP had only a 2.2% decrease in rates (p = 0.59). Similarly, VAP rates decreased by 15.2% in SAQAP units, while VAP rates increased by 4.8% in those without an SAQAP. “Teams that developed an SAQAP not only had close to significant improvements in unit culture but also improved in CLABSI and VAP clinical outcomes, which suggests that an active targeted intervention in culture may carry over onto improved outcomes for patients.” |
Safety culture measured annually. Unique in that tailored unit-level intervention designed to improve safety culture (rather than clinical outcomes) Did not find significant association |
| Weaver and Weeks 2014 | Quasi-experimental research; retrospective analysis of a study; 237 ICUs; 2005–2011 | Comprehensive Unit-based Safety Program, including education, checklist and audit tools, audit and feedback* |
Hospital Survey on Patient Safety Culture (HSOPSC): supervisor expectations, teamwork within ICUs, communication openness, feedback about error, non-punitive, staffing and workload, management support, teamwork across ICUs, handoffs and care transitions, organizational learning This study applied a “pattern-based” approach to analyze safety culture: profile elevation, variability and shape |
CLABSI |
Relationship between safety culture and hospital-associated infections depends on the climate profile characteristics assessed: climate profile shape was a significant predictor of infection risk, but profile elevation and profile variability were not (p = 0.74 and p = 0.48, respectively) The incidence rate of infection was 77% higher in units with a non-punitive climate shape (incidence risk ratio 1.77, p < 0.001) and 57% higher in units with a conflicting climate shape (incidence risk ratio 1.57, p < 0.001) “Pattern-based methods should be used for examining safety culture rather than examining narrow dimensions of safety culture and outcomes such as CLABSI” |
Safety culture measured pre-intervention |
| Wick 2015 | QI initiative; 2013–2014; one tertiary care, academic medical center | Expanded on existing comprehensive unit-based safety program infrastructure (CUSP) with goal of improving teamwork and safety culture, plus trust-based accountability model for leadership and Integrated Recovery Pathway | Not measured | Surgical site infection (SSI); urinary tract infection (UTI) |
Significant decrease in hospital length of stay (LOS) of 2 days; greater than 50% reduction in SSI; significant improvement in patient experience, and improved value, as well as a trend toward reduction in VTE and UTI. Their trust-based accountability model together with CUSP components resulted in a rapid improvement in patient outcomes, patient experience, and cost. Article title is “Organizational Culture Changes Result in Improvement in Patient-Centered Outcomes: Implementation of an Integrated Recovery Pathway for Surgical Patients” |
Safety culture not measured |
Table 3.
Studies that address the relationship between safety culture, infection prevention and control processes (IPC), and healthcare-associated infections (HAIs)
| First author, year | Design, number of sites or units, and study period | Intervention(s) | Safety culture measurement and domains | Infection prevention and control process(s) measured | Healthcare-associated infection(s) measured | Study-reported findings and relation to safety culture | Comments |
|---|---|---|---|---|---|---|---|
| Berenholtz 2011 | QI initiative; 112 ICUs in 72 hospitals; 2003–2006 |
Comprehensive Unit-based Safety Program. A 5-step intervention to improve safety culture and communication: (1) education of staff on the science of improving patient safety; (2) asked teams to identify defects (anything clinically or operationally that should not recur); (3) engaging senior executives; and (4) asked staff to choose and learn from 1 defect per month; and (5) asked teams to implement tools to help improve teamwork and communication An intervention focused on reducing the incidence on VAP. Implementation of 5 evidence-based recommendations: (1) semirecumbent positioning; (2) gastrointestinal stress ulcer prophylaxis; (3) deep venous thrombosis prophylaxis; (4) adjustment of sedation; and (5) daily assessment of readiness to extubate |
Safety Attitudes Questionnaire (domains or measurements not reported in this article) | VAP bundle compliance | VAP |
The median VAP significantly decreased from 5.5 cases per 1000 ventilator days to 0 cases per 1000 ventilator days at both 16–18 months and 28–30 months after implementation Compliance with evidence-based therapies increased from 32 at baseline to 75% at 16–18 months after implementation, and 84% at 28–30 months after implementation “This project demonstrated significant reductions in VAP rates that were likely the result of translating evidence into practical behavior and building them in a multifaceted quality improvement intervention that also included safety culture and communication improvements” |
Safety culture measured at baseline and annually thereafter, but results not reported in this article This study is part of the Michigan Keystone Project by Pronovost et al. |
| Brilli 2013 | QI initiative; 1 urban children’s hospital; 2009–2012 |
Implementation of a “Zero Hero” patient safety program: (1) training in basic error prevention; (2) training leaders in leadership methods; (3) training frontline staff in coaching their peers on effective use of the error prevention techniques Deployment of microsystem-based teams focused on each HAI subset. Implementation of HAI prevention bundles |
Safety Attitudes Questionnaire (domains not reported in this article) | Compliance with established HAI prevention bundles (results not reported in this article) | Number of HAI events, including CLABSI, VAP, SSI, and CAUTI |
Decrease in annual HAIs (76 events in 2009 vs 50 events in 2012; not statistically significant) Decrease in CLABSI, CAUTI, SSI rates (not statistically significant) Significant decrease in VAP rates (from 0.04 per 1000 ventilator days in 2009 to 0.0 per 1000 ventilator days in 2012; p < 0.01) Significant improvement in overall safety climate scores after the intervention (72% in 2009 vs 76% in 2011; p < 0.05) |
Safety culture was measured at baseline and 6 months after the conclusion of the “Zero Hero” training Single-site study Did not statistically analyze the association between SC and outcomes |
| Choi 2013 | QI initiative; pediatric hematology-oncology unit in a single children’s hospital; 2005–2011 |
A multidisciplinary CLABSI working group was created. Team members developed techniques to improve the safety culture related to catheter care, identified best practices for the insertion and maintenance of catheters, and disseminated the information to clinical care providers Central line maintenance bundle was implemented A root cause analysis was conducted for every CLABSI event |
Hospital Survey on Patient Safety (HSOPSC) | CLABSI bundle adherence | CLABSI |
Significant decrease (45%) in CLABSI rates after the intervention (from 2.92 per 1000 patient days to 1.61 per 1000 days; p < 0.004) Self-reported complete adherence to recommended maintenance bundle practice increased from 51% in the early intervention period to 86% in the later period Responses to HSOPS reflected improvement in nearly all domains when comparing pre- and post-intervention data: overall unit safety (40 to 89%; p < 0.07); organizational learning and continuous improvement (64 to 85%, p < 0.31); teamwork within the unit (79 to 95%; p < 0.37); hospital management support for patient safety (51 to 93%, p > 0.25) “By adopting and effectively implementing uniform maintenance of catheter care practices, learning multidisciplinary teamwork, and promoting a culture of patient safety, the CLABSI incidence was significantly reduced and maintained” |
Safety culture was measured bi-annually Single-site study Did not statistically analyze the association between SC and outcomes |
| Cumbler 2013 | QI initiative; 13-bed acute care for the elderly medicine unit in academic medical center; 2010–2012 | Improve adherence and culture through: (1) real-time peer feedback and request for correction when nonadherence was observed; (2) shared responsibility for hand hygiene auditing using random assignment of responsibility to all members of nursing staff; (3) follow-up communication by unit leadership for failure to correct or repeated nonadherence by individual of any role or rank; (4) delivery of nonadherence “tickets” and positive reinforcement of adherence with individually wrapped “lifesavers”; unit dashboard; unit champions | Not measured | Hand hygiene adherence with rotating auditors | CLABSI, CAUTI |
Hand hygiene rates increased from 78 to 97.2%; no CLABSI or CAUTI for 2 years. “Peer pressure and conforming norms can be harnessed to drive improvement through social punishment and intermittent immediate rewards” “Hand hygiene should be interpreted in the context of the social milieu but is amenable to change using simple psychological principles” |
Safety culture not measured. One unit in a single-site study |
| Day 2009 | QI initiative; 1 academic medical center; fall 2017 | Evidence-based guideline with 5 recommendations: (1) hand hygiene campaign to draw awareness of HCWs and patients to importance of hand hygiene; (2) education of HCWs regarding protocols and techniques; (3) HCW hand hygiene performance feedback; (4) product selection and availability to enhance performance; (5) leadership interventions to promote and support hand hygiene | Not measured | Compliance with hand hygiene guidelines | Infection rates including MRSA and VRE (measured, but results not reported in this article) |
Hand hygiene compliance improved from 45 to 85% during the first 6 months of a multimodal intervention Safety culture mentioned in the results-discussion section: “Multimodal interventions over a period of time can support changing the culture” “Chief nursing officers and other leaders can change the organizational culture related to hand hygiene by utilizing an evidence-based practice guideline …” |
Safety culture not measured Single-site study |
| DePalo 2010 | QI initiative; 23 ICUs in 11 hospitals; 2006–2008 | Adaptation of Michigan Keystone Project. Intervention was Comprehensive Unit-based Safety Program: educating staff on the science of safety, identifying hazards, identifying senior executive partners, learning from defects and implementing teamwork tools | Not measured |
VAP bundle compliance (CLABSI bundle compliance either not measured or not reported in this article) |
CLABSI, VAP |
Mean CLABSI rates decreased 74% (from 3.73 infections per 1000 catheter-days to 0.97) VAP rates decreased 15% (from 3.44 to 2.92 VAPs per 1000 ventilator days); VAP rates decreased as ventilator bundle compliance rates increased Safety culture mentioned in the abstract and result sections: “Hospital executives and intensive care unit staff…worked together to implement evidence-based interventions and change safety culture in ICUs” |
Safety culture not measured |
| Foulk 2012 |
QI initiative; 35-bed surgical step-down unit in 1 hospital; 2009–2011 |
Shared governance model for nursing including unit level quality and safety council, raising hand hygiene awareness, a game called “hot hands” in which the charge nurse for each shift would give out red, laminated hands to any staff members witnessed not performing proper hand hygiene. Also created music video with catchy “jingle about hand hygiene” | Not measured | Hand hygiene adherence |
Clostridioides difficile infections |
Increase from 73 to 98% in hand hygiene compliance in unit; decreased C. difficile rate 1.23 to 0.61. “Nurturing a workplace where creativity and innovation drive the staff to strive for excellence in nursing measures has positive effects on the care provided to patients” |
Safety culture not measured One unit in a single-site study Measurement methods for processes and outcomes not described Statistical significance of changes not reported |
| Gilmartin 2016 | Cross-sectional research; 614 hospitals; 2011 | None | Two tools: (1) Leading a Culture of Quality for Infection Prevention (LCQ-IP) and nine subscales with factors loading on organizational climate, leadership and psychological safety; and (2) Relational Coordination Survey (RCS) which measures relational coordination between infection preventionists, physicians, bedside nurses, environmental services, and hospital administration | Adherence to central line insertion bundles. Specifically, hand hygiene, using maximal barrier precaution, using chlorhexidine to prepare the skin, and selecting the optimal catheter site | CLABSI |
There was a positive association (beta = 0.23, p < 0.01) between adherence to central line bundle and organizational context (which was a second-order model combining items from the two major culture tools) There was no statistically significant relationship between CLABSI and organizational context (beta = − 0.20, p = 0.78) |
Single time measurement of safety culture) Infection preventionists were the respondents for culture measurement Includes large number of hospitals |
| Jain 2011 | QI initiative; 150 Veterans Affairs hospitals; 2005–2010 | MRSA bundle consisted of universal active nasal surveillance for MRSA, contact precautions for patients colonized or infected with MRSA, hand hygiene, and “a change in the institutional culture whereby infection control would become the responsibility of everyone who had contact with patients” | Not measured | MRSA screening adherence | MRSA VAP, MRSA BSI, MRSA UTI, MRSA skin or soft tissue, VRE C. difficile |
“A program of universal surveillance, contact precautions, hand hygiene, and institutional culture change was associated with a decrease in health care-associated transmissions of and infections with MRSA in a large health care system” “The increase in adherence to active surveillance in the months after issuance of the VHA directive and the subsequent declines in healthcare–associated MRSA infections were consistent with an institutional culture change that resulted in health care workers being more aware of health care-associated MRSA infections and increasing their adherence to hand hygiene and contact precautions” |
Safety culture not measured Mentioned positive deviance as recommended approach to culture change but no further description. Includes large number of hospitals caring for veterans and a wide variety unit type (ICU and non-ICU) |
| Johnson 2014 | QI initiative; 1 academic medical center; 2006–2012 | Education, checklist and audit tools, reminders, audit and feedback, staff accountability, product selection and accessibility, organizational culture (including patient and family engagement) | Not measured | Hand hygiene adherence | CLABSI |
Adherence to hand hygiene improved from 58 to 98%, and CLABSI decreased from 4.08 to 0.42 per 1000 device days “Another key element of our QI project was to effect an organization-wide culture change, resulting in all healthcare workers recognize failure to practice good hand hygiene is unacceptable and all healthcare workers categories and hierarchies levels will be held accountable” |
Safety culture not measured Single-site study |
| Joyce 2011 | QI initiative; 6 hospitals within 1 health system; 2008–2010 | Education, audit and feedback, evidence-based best practice bundles (CLABSI, CAUTI, SSI, VAP), daily multidisciplinary rounds with bedside huddles, large graphic dashboard, overall effort intended to improve teamwork, communication and engagement | Not measured | Compliance with bundles, completion of rounds, hand hygiene, checklist compliance | CLABSI, CAUTI, VAP, SSI, mortality rates |
CAUTI average monthly incidence declined from 43.9 to 15.8 (64% reduction, p < 0.001) SSI and VAP monthly incidence also declined (24.9 to 18.8, p = 0.13 and 2.4 to 1.5, p = 0.29, respectively) CLABSI average monthly incidence increased from 3.2 to 5.0 (p = 0.15) Non-risk adjusted mortality dropped from 1.63 deaths per 1000 discharges to 1.41 (p = 0.16) implementation of the initiative resulted in a significant reduction in hospital-acquired infections (infection dropped from 74.4 to 41.2) |
Safety culture not measured |
| Lin 2018 | QI initiative; 15 hospitals; 2013–2015 | CUSP with individualized bundles of interventions to reduce SSI | AHRQ Hospital Survey on Patient Safety Culture (HSOPSC) | Chlorhexidine wash, wipe before operation, and surgical preparation; appropriate antibiotic choice, dose, and timing; standardized post-surgical debriefing; and differentiating clean-dirty-clean with anastomosis tray and closing tray | SSI |
The collaborative colorectal SSI rate decreased (from 12.08 to 4.63%; p < 0.01). Safety culture increased significantly in 10 of 12 domains: Overall Perception/Patient Safety; Teamwork Across Units; Management-Support Patient Safety, Nonpunitive Response to Error, Communication Openness; Frequency of Events Reported; Feedback/Communication about Error); Organizational Learning/Continuous Improvement; Supervisor/Manager Expectations and Actions Promoting Safety and Teamwork Within Units. There was a change in SSI rates and a change in safety culture, but correlations between the 2 were negligible or weak for most domains of safety culture |
Safety culture measured two points in time 18 months apart. Did not find significant associations |
| Mayer 2011 | QI initiative; 2 ICUs (pediatric ICU and surgical ICU) in 1 academic medical center; 2007–2009 | TeamSTEPPS, an Agency for Healthcare Research and Quality (AHRQ)- supported training program that focuses on 4 core areas of competency: team leadership, situation monitoring, mutual support, and communication |
Three tools: (1) Hospital Survey of Patient Safety Culture (HSOPSC): teamwork-specific domains, overall perception of safety, and communication openness; (2) Employee opinion survey (EOS): teamwork domains; and (3) National Database of Nursing Quality Indicators (NDNQI): teamwork items. Also observation of teamwork performance using Teamwork Evaluation of Non-technical skills (TENTS) Staff interviews were also performed to address components of teamwork aligned with the training and outcome objectives |
Average time for placing patients on extracorporeal membrane oxygenation (ECMO) and average duration of adult surgery rapid response team events | Nosocomial infection rate (without further details) |
Improvement seen in all clinical process and outcome measures Nosocomial infection rate post-implementation was below the upper control limit for 7 out of 8 months in both the PICU and the SICU Observed team performance improved significantly for leadership, mutual support, and overall leadership. No significant change in communication, situation monitoring, and overall teamwork HSOPSC score significantly improved for at least one unit in overall perception of safety, communication openness, teamwork within unit. Similarly, significant improvement was shown in two EOS teamwork measures “Significant improvement on overall perceptions of safety, teamwork within units and staff interactions across several measures” |
Single-site study Safety culture measured at baseline and 12 and 18 months with several established tools Did not statistically analyze the association between safety culture and outcomes |
| Medina 2014 | QI initiative; 8 units in 1 academic medical center; 2011–2013 | Bundle in which chlorhexidine bathing was primary intervention. Other 4 simultaneous support strategies included staff education, making sure there was strong leadership support, ensuring availability of resources, and increasing staff awareness and accountability (including “visibility walls”) | None | Hand hygiene, use of pre-insertion checklist, compliance with chlorhexidine bathing and central line maintenance practices | CLABSI |
CLABSIs rates decreased from 1.46 to 0.52 infections per 1000 patient days after the 8-month intervention period No findings related to culture beyond the abstract which states “4 strategies were used to promote a change in practice and culture” |
Safety culture not measured |
| Millson 2019 | QI initiative; intervention at single dialysis clinic with 5 control sites; 2017–2018 |
Comprehensive Unit-based Safety Program (CUSP)* “Objectives were to improve understanding of safety culture on the unit and align clinical practice with CDC core interventions…” |
Hospital Survey of Patient Safety Culture (HSOPSC) modified for dialysis clinics. Domains: teamwork, communication, management support, continuous improvement, organizational learning |
Monthly infection prevention practice audits, hemodialysis bundle, and procedures considered critical to prevent CLABSI | Bloodstream infections |
Infection rates decreased from 2.33 to 1.07 events per 100 patient months, and the standardized infection ratios decreased from 1.96 to 0.99 in the 12 months after implementation Baseline data from 6 sites indicated a strong negative relationship between staff perception of safety and BSI rates (p = 0.017). The lower the staff perceived the safety culture, the higher the BSI rated tended to be at the beginning of the project “Enhanced patient safety culture is correlated with improved patient outcomes” |
Safety culture measured pre-intervention and compared with baseline infection rates Demonstration project Setting is dialysis clinics |
| Pronovost 2011 | Summary description of several QI initiatives studies involving hundreds of hospitals and ICUs; 2001–2009 | Comprehensive Unit-based Safety Program*. Also, culture was addressed at 3 levels: (1) the microsystem or unit by forming safety teams with focused training; (2) engaging senior executives; and (3) creating a social community at the state level | Not described in this paper | Adherence to central line insertion bundles | CLABSI |
Multiple collaborative efforts across public and private stakeholders led to a nationwide 63% reduction in CLABSI in ICUs “Programs to improve quality must address culture.” Programs focused at 3 levels (microsystem, leadership, and social community) helped create new norms regarding bloodstream infections. |
Safety culture either not measured or not described in this paper |
| Raveis 2014 | Qualitative research; in-depth interviews at 11 hospitals; 2010–2011 | None (premise of study was to understand how best to implement process changes that impact outcomes) | Interviews with 116 staff addressed how to change safety culture | HAI prevention strategies including change in policies, process implementation, facilitators, barriers | HAIs not specified, although the importance of linking IPC adherence to patient outcomes was a key theme |
Three themes related to implementation of IPC practices: (1) implement institution-wide; (2) promote culture change to sustain adherence; and (3) contend with opposition to new infection control mandates Promoting an institutional culture to sustain adherence should be done by (1) linking IC adherence to patient outcomes, (2) generating group accountability and ownership, (3) taking action for the collective good, and (4) facilitating teamwork |
Safety culture assessed using qualitative process Process and outcome measurements not specific |
| Rawat 2017 | QI initiative; longitudinal; 56 intensive care units (ICUs) at 38 hospitals; October 2012 to March 2013, April 2013–March 2015 | Comprehensive unit-based safety programs (CUSP); two state collaborative with goals to decrease ventilator-associated events (VAEs) by improving compliance with evidence-based interventions, unit teamwork, and patient safety culture | Hospital Survey on Patient Safety Culture (HSOPSC); domains of teamwork and safety culture | Head-of-bed elevation (HOB), use of subglottic suctioning for endotracheal tubes (Sub-G ETT), oral care (OC) 6 times per day, chlorhexidine mouth care (CHG) two times per day, performance of spontaneous awakening trials (SAT), and performance of spontaneous breathing trials (SBT) | Infection-related ventilator-associated complication (IVAC) and ventilator-associated pneumonia (PVAP) |
After 24 months of implementation, infection-related ventilator-associated complication (IVAC) and possible and probable ventilator-associated pneumonia (PVAP) rates decreased from 3.15 to 1.56 and 1.41 to 0.31 cases per 1000 ventilator-days (p = 0.018, p = 0.012), respectively. The six technical interventions, or bundle of evidence-based practices, were executed using models designed to change care practices and improve safety culture |
Safety culture measured annually. Did not statistically analyze the association between SC and outcomes; however, they planned to do so. Thus results related to associations are not reported in this paper |
| Robinson 2018 | QI initiative; in 7 adult ICUs one hospital 2010–2015 | Implementation of a quality and safety RN champion model aimed to educate, support, and engage frontline RNs to implement and ensure continued compliance of the VAP Evidence Based Practice bundle in each of the 7 ICUs | Not measured |
VAP Evidence Based Practice bundle Oral CHG/Peridex with subglottic suctioning; head of bed at more than 30°; perioperative deep oral suction and oral care every 4 h and at end of case; leaving gastric tubes in place in patients who will remain intubated, intermittent gastric suctioning; updated signage on beds of patients traveling to the OR; and hand-off tools |
Ventilator-associated pneumonia (VAP) |
Reduction of 39.5% in ICU length of stay (LOS) over 6 years utilizing the RN champion model. Bundle compliance versus confirmed VAP data showed total bundle compliance rate of 95% and decrease in confirmed cases from 19 to 4 in the 4th quarter of 2015 “The integration of this RN champion model positively changed culture by educating healthcare providers and reinforcing quality and safety initiatives with the goal of improving patient outcomes” |
Single site |
| Rosenberg 2015 | QI initiative; 109-bed children’s service within academic medical center (ICU and non-ICU units); 2012–2014 | CLABSI insertion and maintenance bundles, rounding, multi-disciplinary team, bedside champions, publicly posted unit-based feedback, accountable action plan, family engagement | Not measured | Adherence to central venous catheter bundles | CLABSI |
Significantly decreased variation, increased bundle reliability, and decreased annual CLABSI rates from 2.7 to 0.5 per 1000 line days over time “We believe that key elements contributing to initial success with evolving QI capacity and resources were likely multifactorial, including staff and leadership engagement, culture change, consistent guidelines, and accountability” “Basic QI techniques drove an equally important part of this culture change, including transparent, respectful data sharing on both reliability and outcomes, and peer and leadership education at all levels of children’s services, including increasing awareness among nursing, house staff, and physicians about the preventable nature of CLABSI.” |
Safety culture not measured Single children’s service |
| Southworth 2012 | QI initiative; 1 teaching hospital; 2003–2008 | Daily rounding, checklists, promoting culture of advocacy by nurses and enhanced autonomy, empowerment to speak up, observation of insertions, resident education |
National Database of Nursing Quality Indicators (NDNQI) Domains: Nurses satisfaction with relationship between physicians and nurses, nurse autonomy |
Adherence to CLABSI bundle | CLABSI |
An important feature of the culture change was for the nurse to feel empowered to speak up if expectations for proper procedure were not met. During implementation of the new process, there was no decrease in nurse satisfaction with relationships between nurses and physicians or nurse autonomy “Although the evidence described the processes necessary to decrease the occurrence of CLABSIs, it was the change in culture by our nursing staff and physicians that drove the change. The performance expectations for CLABSI went from accepting an average number of 8 or 9 infections per quarter to tolerating zero infections. This culture change was very clearly demonstrated in fiscal year 2008, when the ICU went 12 months without a single CLABSI” |
Annual measurement of NDNQI Statistical significance of changes in safety culture not reported Did not statistically analyze the association between safety culture and outcomes |
| Thomas-Hawkins 2015 | Cross-sectional research; 422 registered nurses in outpatient dialysis facilities; September–November 2007 | None |
Hospital Survey on Patient Safety Culture (HSOPSC): Handoff and Transitions scale; patient safety scale. Respondents were nurses. |
Handoff and transitions safety | Vascular access infection |
Negative ratings of overall patient safety culture in dialysis units were independently associated with increased odds of frequent occurrences of vascular access infection. Negative patient safety culture ratings were also associated with medication errors by nurses, patient hospitalization, vascular access infection, and patient complaints |
Measured safety culture single time |
Table 1 presents 13 articles that address the relationship between safety culture and IPC processes. The IPC processes measured varied and included 4 articles that measured compliance with policies and guidelines ([64, 89, 92, 95]), two that measured compliance with HAI prevention bundles (e.g., CLABSI, daily interruption of sedation, antibiotic prophylaxis, standard precautions) ([83, 96]), and 3 articles that focused on hand hygiene ([81, 97, 98]). One article measured aspects of infection control structure [91]. Other process-related measures included willingness to adopt CUSP interventions [82], attitudes and beliefs about a Klebsiella pneumoniae carbapenemase (KPC)-producing Enterobacteriaceae control program [99], and how hospital CLABSI prevention efforts encouraged employees’ efforts to speak up and prevent errors [100].
Table 2 presents 20 articles that address the relationship between safety culture and HAIs. There was also substantial heterogeneity in the type of HAIs measured. However, most of them (n = 15, 75%) measured CLABSIs, CAUTIs, VAPs, or SSIs either exclusively or as a combined outcome [47, 61, 66, 68–70, 77, 79, 80, 86, 94, 101–104]. Other HAIs in single articles were colon SSIs [67], hospital-acquired sepsis [65], and C. difficile [77], and 3 did not specify the type of HAI measured [71, 84, 85].
Table 3 presents 22 articles that measured both IPC processes and HAIs to address the relationship with safety culture. In this group, most articles (14, 90.9%) measured process compliance with HAI prevention bundles (e.g., CLABSI, VAP, MRSA screening adherence) [62, 63, 72, 73, 75, 87, 88, 90, 93, 105–109] or hand hygiene adherence [110–113] or adherence to policy and guidelines [76, 78, 114]. Regarding HAIs, most (n = 17, 81.8%) measured CLABSIs, CAUTIs, VAPs, or SSIs either exclusively or as a combined outcome [62, 63, 72, 73, 75, 76, 78, 87, 88, 90, 93, 105–110, 113]. Of note, C. difficile was only explored as an outcome by two [63, 112], and two articles focused on organism-specific HAIs (e.g., MRSA and VRE) [63, 111]. Two articles did not specify the type of HAI measured [74, 114].
Relationship Between Safety Culture and Improvements in IPC Process and Patient Outcomes
Across all 55 articles (regardless of whether they measured or analyzed safety culture), 51 (92.7%) concluded there was an association between safety culture and IPC process and/or HAIs. A summary of the conclusions about the relationship between safety culture, IPC, and HAI is presented in Table 4.
Table 4.
Summary of articles that related safety culture to infection prevention and control (IPC) processes or healthcare-associated infections (HAIs)
| Study design and sites | Total number of studies | Number measured safety culture | Number attempted to statistically associate safety culture and IPC process or HAI | Number identifying a statistically significant association between safety culture and IPC process or HAIs | Number concluding safety culture influenced IPC process or HAI or that safety culture improved |
|---|---|---|---|---|---|
| Qualitative; single site | 1 | 1 | n/a | n/a | 1 |
| Qualitative; multiple sites | 3 | 3 | No | n/a | 3 |
| Cross-sectional; single site | 1 | 1 | 1 | 1 | 1 |
| Cross-sectional; multiple sites | 16 | 16 single time | 16 | 15 | 14 |
| Quality improvement initiative; single site | 16 | 5 multiple times | – | – | 16 |
| Quality improvement initiative; multiple sites | 12 |
1 single time 6 multiple times |
3 | 2 | 11 |
| Quasi-experimental research; single site | 1 | 1 | 1 | 1 | 1 |
| Quasi-experimental research; multiple sites | 5 |
2 single time 3 multiple times |
5 | 2 | 3 |
| Total | 55 | 39 | 26 | 21 | 51 |
Of the 39 that measured safety culture, only 26 (67%) tried via statistical analysis to establish an association between safety culture and IPC process or HAIs. Statistical analyses varied by design.
Among the 28 QI projects, only 12 measured safety culture and 3 tried to establish a statistical association between safety culture and IPC process or HAIs. Nevertheless, almost all QI projects (27 out of 28, 96%) concluded there was a relationship between safety culture and outcomes. One of the 3 QI projects that measured safety culture and tried to establish a statistical association between safety culture and outcomes did not find a statistically significant relationship between culture and IPC process or HAIs [73].
By comparison, all 27 research articles measured safety culture. Of these, 23 (85.2%) tried to establish a statistical association between safety culture and IPC process or HAIs. Nineteen of the 23 (82.6%) identified a statistically significant association with IPC process, HAIs, or both. Among those that did not find an association were 2 of the largest quasi-experimental studies [68, 80] and 1 cross-sectional study [83]. Another smaller quasi-experimental study with an intervention exclusively focused on improving safety culture also did not find significant association [86].
Discussion
The goal of this review was to examine recent literature on the relationship between safety culture and IPC processes and outcomes in U.S. healthcare organizations. In so doing, we also sought to characterize the challenges to empirically establishing these relationships as well as limitations of current research.
The 55 articles reviewed varied considerably regarding purpose, design, safety culture measurement tools and respondent, and outcome (IPC process and/or HAI) measurement, although several were based on the CUSP model. This heterogeneity contributes to the previously described challenges to linking safety culture, IPC processes and outcomes.
Nevertheless, most of the QI and research articles that measured safety culture and statistically analyzed the associations concluded that safety culture was positively associated with IPC processes and negatively associated with HAIs. Thus, our findings are generally consistent with other reviews supporting the notion that an association exists [42•, 43••, 44••].
Interestingly, a greater proportion of QI articles than research articles concluded there was a relationship with safety culture. All but one of the QI projects concluded that safety culture improved over time, even though less than ½ of the QI projects actually measured safety culture.
Why is it that so many QI studies concluded there was a relationship even in the absence of measuring safety culture? Do the QI studies share a common assumption that safety culture must have improved? In the absence of empirical data, should we dismiss all the QI studies that did not measure culture and limit conclusions to the traditional research studies? Were this a systematic review that only included studies with rigorous designs, we would have to conclude there is limited evidence to support the relationship between safety culture and IPC and HAIs because of weak designs.
We propose an alternative explanation. Perhaps one should instead accept the experience reported by authors that culture did change, even if not measured in a quantifiable way. As described in the tables, authors often expressed that they saw or felt a culture change which was integral to the effectiveness of the improvement effort. In fact, it is quite possible that culture did improve in certain domains because of the increased attention of leadership, extra resources, incentives, and momentum to drive change. Awareness and attitudes about the preventability of HAIs likely changed through education, and a sense of teamwork likely improved through the shared experience of working toward a common, measurable goal. This notion is highly consistent with the multi-faceted CUSP approach to improvement initiatives.
On the other hand, it is important to note that some research studies with the strongest methodologies (large numbers of sites, multiple outcomes, and longitudinal design) did not find an association between safety culture, IPC process, and HAIs (e.g., [68, 80]). Meddings et al. suggest that improvements in HAIs occurred by means other than improving safety culture, such as a strong emphasis on standardizing technical components of care, and that changing safety culture may not be critical to improvement [68]. Alternatively, they also suggest that safety culture may have improved and been instrumental in improving outcomes but could have been inadequately measured. In response, others have argued that the conclusions drawn by Meddings were unrelated to the instrument and inadequately supported by the methods and analyses [115].
So, what are the practical implications of the findings? Should one continue measuring safety culture and trying to establish relationships with outcomes? What does this say about targeting interventions to improve safety culture? Some insight into this question comes from the review by De Bono [44••]. They state that strategies aimed at achieving long-term improvement in IPC performance need to be multi-modal in order to both reflect and address the multidimensionality of the structure and the dynamic of organizational culture. They state “the link between compliant behavior and culture may seem to be plausible and sometimes obvious. But when empirically measured, the relationship might be weaker than expected, probably due to a long chain of mitigating factors and confounders.”
De Bono and colleagues also argue that strategy and organizational culture are inextricably intertwined in that all attempts at organizational culture change should be viewed as strategic changes [44••]. The notion that strategy and culture are inextricably intertwined helps explain why so many healthcare organizations in this review experienced a culture change while implementing strategies for improvement. Regarding causal direction, it may well be that implementing effective QI intervention strategies influences culture as much or more than interventions to change culture affect IPC processes and HAIs.
Regardless of the inter-relationships between safety culture, process, and outcome, there remains value in assessing safety culture. This value includes the ability to better understand staff perceptions and attitudes, identify opportunities for improvement, find differences across units and healthcare worker roles, comply with recommendations and requirements of oversight groups, and effectively implement interventions that ultimately benefit staff and patients.
Research Gaps
We identified several gaps in need of future research. Foremost is the need for longitudinal, cluster randomized trials with the explicit purpose of assessing the impact of safety culture, while controlling for the effect of specific interventions. Greater rigor in design would overcome many of the weaknesses inherent in uncontrolled observational studies. More research is also needed in non-hospital settings. It would be interesting to know if the relationships would be similar, stronger, or weaker in settings that are less organizationally complex than hospital, such as nursing homes and specialty clinics.
Similarly, more studies that directly measure safety culture over time are needed to better understand the sensitivity to change of safety culture instruments. Greater attention to fine tuning analysis for specific subgroups is also needed. For example, do associations between safety culture and IPC process vary depending on the role of the person completing the safety culture assessment (frontline staff vs leadership), the domains within safety culture (e.g., teamwork, communication, leadership), or the HAI of interest? Also, to what extent do studies at the unit-level generalize to organizational level findings?
Limitations
Our review has several important limitations. It was not intended to be a systematic review, and we did not formally evaluate the quality of studies. Nor should it be considered a comprehensive scoping review because we did not strive to assess the breadth of literature on this topic. We did not include gray literature that was not peer reviewed.
We only searched one citation database (PubMed). Other databases such as CINAHL, PsycINFO, EMBASE, and Cochrane might have yielded more studies. We excluded studies done outside the U.S.A. in part because of differences in facility characteristics and payment systems across borders which could confound the relationships of interest. There is a substantial body of work on this topic in European, Asian, and other regions which might have led to different conclusions (e.g., [116, 117]). The choice of search terms and PubMed field types may have been too limited. We also may have missed studies due to publication bias in that studies lacking associations between safety culture and IPC process or HAIs may never have been submitted or published.
Finally, in our analysis, we did not consider other related factors such as leadership styles and issues specific to the measurement tools. Admittedly, lumping together tools that measure culture and climate further conflates the distinction in instruments and does nothing to address psychometric concerns related to validity, reliability, and domain-specific issues.
Conclusions
Safety culture appears to be related to IPC processes and HAI outcomes. The associations with the IPC process may be bi-directional in that positive safety culture contributes to the success of interventions and implementing interventions drives improvements in safety culture. In the absence of longitudinal controlled trials, it may not be possible to separate the effect of safety culture from that of implementing effective intervention strategies on HAIs. Nevertheless, there remains value in evaluating safety culture in order to understand staff perceptions, identify opportunities for improvement, and implement interventions that ultimately benefit staff and patients.
Acknowledgments
The authors are sincerely grateful to medical librarians Janet Aleccia MALS and Laura Shedore MLIS, to Tasha Mearday BS for administrative assistance, and to Brette Tschurtz MPH, Scott Williams PsyD, and Kenneth Soyemi MD MPH MBA for thoughtful review.
Authors’ Contributions
The project was conceptualized by BB and SC based on a presentation at the 2019 Society for Healthcare Epidemiology Annual Meeting. All authors participated in abstracting data from included articles and manuscript review. MP led the analysis and manuscript preparation was completed by BB, SC and MP.
Funding
No funding was received for conducting this study. Access to REDCap software was provided through Institute for Clinical and Translational Science grant support (NIH and CTSA grant number: UL1TR002537) at the University of Iowa.
Data Availability
Available upon request.
Compliance with Ethical Standards
Conflict of Interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Ethics Approval
This review was not considered to be human subject research.
Informed Consent
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Footnotes
This article is part of the Topical Collection on Healthcare Associated Infections
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Barbara I. Braun, Email: bbraun@jointcommission.org
Salome O. Chitavi, Email: schitavi@jointcommission.org
Hiroyuki Suzuki, Email: hiroyuki-suzuki@uiowa.edu.
Caroline A. Soyemi, Email: carolinesoyemi@yahoo.com
Mireia Puig-Asensio, Email: mireia-puigasensio@uiowa.edu.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.US Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Health Care Associated Infections. HHS: National HAI Action Plan. National action plan to prevent health care-associated infections: road map to elimination [internet]. [cited: 24 Jul 2020]. Available from: https://health.gov/our-work/health-care-quality/health-care-associated-infections/national-hai-action-plan.
- 2.Centers for Disease Control and Prevention (CDC). National healthcare safety network (NHSN) [internet]. [cited: 1 Nov 2019]; Available from: https://www.cdc.gov/nhsn/index.html.
- 3.Centers for Disease Control and Prevention (CDC): State-based HAI prevention activities [internet]. [cited: 9 Sept 2020]. Available from: https://www.cdc.gov/hai/state-based/index.html.
- 4.Stoessel K, Truscott W. National patient safety goal 7: recommendations for compliance [internet]. Infection Control Today: [cited: 8 Jul 2009]. Available from: https://www.infectioncontroltoday.com/view/national-patient-saf4)ety-goal-7-recommendations-compliance.
- 5.Medicare.gov. Hospital compare. Infections [internet]. [cited:10 Sept 2020]. Available from: https://www.medicare.gov/hospitalcompare/Data/Healthcare-Associated-Infections.html.
- 6.Srinivasan A, Craig M, Cardo D. The power of policy change, federal collaboration, and state coordination in healthcare-associated infection prevention. Clin Infect Dis. 2012;55(3):426–431. doi: 10.1093/cid/cis407. [DOI] [PubMed] [Google Scholar]
- 7.Pogorzelska-Maziarz M, de Cordova PB, Herzig C, Dick A, Reagan J, Stone PW. Perceived impact of state-mandated reporting on infection prevention and control departments [internet] Am J Infect Control. 2019;47(2):118–122. doi: 10.1016/j.ajic.2018.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality (AHRQ). AHRQ’s healthcare-associated infections program [internet]. Agency for Healthcare Research and Quality, Rockville, MD. 2019. Available from: https://www.ahrq.gov/hai/index.html. Accessed 20 Nov 2020.
- 9.Centers for Disease Control and Prevention (CDC): Data summary of HAIs in the US: assessing progress 2006-2016: a story of progress. [internet] Available from: https://www.cdc.gov/hai/data/archive/data-summary-assessing-progress.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fhai%2Fsurveillance%2Fdata-reports%2Fdata-summary-assessing-progress.html. Accessed 20 Nov 2020.
- 10.Poots AJ, Reed JE, Woodcock T, Bell D, Goldmann D. How to attribute causality in quality improvement: lessons from epidemiology. [internet] BMJ Qual Saf. 2017;26(11):933–937. doi: 10.1136/bmjqs-2017-006756. [DOI] [PubMed] [Google Scholar]
- 11.Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5):369–74. 10.7326/0003-4819-158-5-201303051-00002. [DOI] [PMC free article] [PubMed]
- 12.Singer SJ, Vogus TJ. Reducing hospital errors: interventions that build safety culture. Annu Rev Public Health. 2013;34(1):373–396. doi: 10.1146/annurev-publhealth-031912-114439. [DOI] [PubMed] [Google Scholar]
- 13.Torben R. Organizational culture eats strategy for breakfast, lunch and dinner. [internet] 2014; Available from: https://www.torbenrick.eu/blog/culture/organisational-culture-eats-strategy-for-breakfast-lunch-anddinner/. Accessed 20 Nov 2020.
- 14.Melnyk BM. Making an evidence-based case for urgent action to address clinician burnout [internet]. AJAC® [cited: 13 Jun 2019]. 2019;7(2):12–14. Available from: https://nam.edu/wp-content/uploads/2019/09/American-Journal-of-Managed-Care-Clinician-Burnout-Article-Bern-Melnyk-June-2019.pdf.
- 15.National Academies of Sciences Engineering Medicine. Taking action against clinician burnout: a systems approach to professional well-being. The role of health care leadership [internet]. NAM. 2019; Available from: https://nam.edu/wp-content/uploads/2019/12/CR-report-leadership-brief-final.pdf. Accessed 20 Nov 2020. [PubMed]
- 16.American Medical Association. AMA Joy in medicine recognition program. Chicago, IL [internet]. AMA. 2020. Available from: https://www.ama-assn.org/system/files/2020-04/joy-award-brochure.pdf. Accessed 20 Nov 2020.
- 17.American Nurses Association. Healthy work environment [internet]. ANA. [cited: 24 May 2019]. Available from: https://www.nursingworld.org/practice-policy/work-environment/health-safety/culture-of-safety/.
- 18.Leonard M, Frankel A. How can leaders influence a safety culture [internet]. The Health Foundation; May 2012 [cited: 10 Sept 2020]. Available from: https://www.health.org.uk/sites/default/files/HowCanLeadersInfluenceASafetyCulture.pdf.
- 19.Sexton JB, Adair KC, Leonard MW, Frankel TC, Proulx J, Watson SR, Magnus B, Bogan B, Jamal M, Schwendimann R, Frankel AS. Providing feedback following leadership walk rounds is associated with better patient safety culture, higher employee engagement and lower burnout. [internet] BMJ Qual Saf. 2018;27(4):261–270. doi: 10.1136/bmjqs-2016-006399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Emergency Care Research Institute (ECRI). Culture of safety: an overview [internet]. Healthcare Risk Control. 14 Jun 2019. Available from: https://www.ecri.org/components/HRC/Pages/RiskQual21.aspx.
- 21.Joint Commission. The essential role of leadership in developing a safety culture [internet]. Sentinel Alert Event. [cited: 1 Mar 2017];57. Available from: https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_57_safety_culture_leadership_0317pdf.pdf. [PubMed]
- 22.Agency for Healthcare Research and Quality (AHRQ). Culture of safety [internet]. In: Patient Safety Network. [cited: 7 Sept 2019]. Available from: https://psnet.ahrq.gov/primer/culture-safety.
- 23.Schein EH. Organizational culture and leadership. 4. San Francisco: EH Schein; 2010. [Google Scholar]
- 24.Joint Commission. Improving patient and worker safety: opportunities for synergy, collaboration and innovation [internet]. 2012 [cited: 10 Sept 2020]. Available from: https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/topics-library/tjc-improvingpatientandworkersafety-monographpdf.pdf?db=web&hash=2772E4D4E100BCE47F731AA1F39471A4.
- 25.Stone PW, Hughes R, Dailey M. Creating a safe and high-quality health care environment [internet]. In: Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses, vol. 21. Rockville: AHRQ (US); 2008. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2634. Accessed 20 Nov 2020.
- 26.Gershon RRM, Stone PW, Bakken S, Larson E. Measurement of organizational culture and climate in healthcare. J Nurs Adm. 2004;34(2):33–40. doi: 10.1097/00005110-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Joint Commission. 2020 Comprehensive accreditation manual for hospitals. 15 Nov 2019.
- 28.National Quality Forum Safe Practices Consensus Committee. Safe practices for better healthcare–2010 update: a consensus report [internet]. NQF [cited: Apr 2010];1–446. Available from: http://www.qualityforum.org/Publications/2010/04/Safe_Practices_for_Better_Healthcare_%E2%80%93_2010_Update.aspx.
- 29.Leapfrog Group. Raising the bar for safer health care. Building a movement for transparency [internet]. [cited: 3 Sept 2020]. Available from: https://www.leapfroggroup.org/about.
- 30.Agency for Healthcare Research and Quality (AHRQ). 10 patient safety tips for hospitals [internet]. Patient Safety Network. 29 Nov 2006. Available from: https://www.psnet.ahrq.gov/issue/10-patient-safety-tips-hospitals. Accessed 20 Nov 2020.
- 31.National Steering Committee for Patient Safety. Self-assessment tool: a national action plan to advance patient safety [internet]. Boston, Massachusetts: Institute for Healthcare Improvement. 2020. Available from: http://www.ihi.org/Engage/Initiatives/National-Steering-Committee-Patient-Safety/Pages/National-Action-Plan-to-Advance-Patient-Safety.aspx. Accessed 20 Nov 2020.
- 32.Donabedian A. Evaluating the quality of medical care. The Milbank Quarterly. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, Bander J, Kepros J, Goeschel C. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355(26):2725–2732. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 34.Agency for Healthcare Research and Quality (AHRQ). Healthcare-Associated Infections Program. The CUSP method [internet]. 2019. Available from: https://www.ahrq.gov/hai/cusp/index.html. Accessed 20 Nov 2020.
- 35.Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G. Association between organizational and workplace cultures, and patient outcomes: systematic review. BMJ Open. 2017;7(11):e017708. doi: 10.1136/bmjopen-2017-017708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DeJoy DM. Behavior change versus culture change: divergent approaches to managing workplace safety. Saf Sci. 2005;43:105–129. doi: 10.1016/j.ssci.2005.02.001. [DOI] [Google Scholar]
- 37.Gardam M, Reason P, Gitterman L. Healthcare associated infections: new initiatives and continuing challenges. Healthcare quarterly special issue sixth in a series papers patient safety. Johnson Johnson Med Co. 2012;15(6):36–41. doi: 10.12927/hcq.2012.22843. [DOI] [PubMed] [Google Scholar]
- 38.Clancy CM. New research highlights the role of patient safety culture and safer care. J Nurs Care Qual. 2011;26(3):193–196. doi: 10.1097/NCQ.0b013e31821d0520. [DOI] [PubMed] [Google Scholar]
- 39.American College of Healthcare Executives and IHI/NPSF Lucian Leape Institute. Leading a culture of safety: a blueprint for success [internet]. American College of Healthcare Executives and Institute for Healthcare Improvement. 2017; Available from: http://safety.ache.org. Accessed 20 Nov 2020.
- 40.Ginsburgh L, Gilin D, Tregunno D, Norton PG, Flemons W, Fleming M. Advancing measurement of patient safety culture HSR. Health Serv Res. 2009;44:1. doi: 10.1111/j.1475-6773.2008.00937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hodgen A, Ellis L, Churruca K, Bierbaum M. Safety culture assessment in health care: a review of the literature on safety culture assessment modes. ACSQHC: Sydney; 2017. [Google Scholar]
- 42.Hessels A, Larson E. The relationship between patient safety climate and standard precaution adherence: a systematic review of the literature. [internet] J Hosp Infect. 2016;92(4):349–362. doi: 10.1016/j.jhin.2015.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Buijtene A, Foster D. Does a hospital culture influence adherence to infection prevention and control and rates of healthcare associated infection? A literature review. J Infect Prev. 2019;20(1):5–17. doi: 10.1177/1757177418805833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Bono S, Heling G, Borg MA. Organizational culture and its implications for infection prevention and control in healthcare institutions. J Hosp Infect. 2014;86(1):1–6. doi: 10.1016/j.jhin.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 45.Alsalem G, Bowie P, Morrison J. Assessing safety climate in acute hospital settings: a systematic review of the adequacy of the psychometric properties of survey measurement tools. [internet] BMC Health Serv Res. 2018;18:353. doi: 10.1186/s12913-018-3167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Szymczak JE. Infections and interaction rituals in the organization: clinician accounts of speaking up or remaining silent in the face of threats to patient safety. [internet]. Sociol Health Illn. 2016;38(2):325–39. 10.1111/1467-9566.12371. [DOI] [PubMed]
- 47.Weaver SJ, Weeks K, Pham JC, Pronovost PJ. On the CUSP: stop BSI: evaluating the relationship between central line-associated bloodstream infection rate and patient safety climate profile. Am J Infect Control. 2014;42(10 Suppl):S203–S208. doi: 10.1016/j.ajic.2014.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ginsburgh L, Oore DG. Patient safety climate strength: a concept that requires more attention. [internet] BMJ Qual Saf. 2016;25(9):680–687. doi: 10.1136/bmjqs-2015-00415053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Joint Commission. Measuring hand hygiene adherence: overcoming the challenges. [internet]. 2009. Available from: https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/topics-library/hh_monographpdf.pdf?db=web&hash=7F1A70731D44DC2D183B1038CE34EC46. Accessed 20 Nov 2020.
- 50.Haraden C. What is a bundle? IHI. 2020. Available from: http://www.ihi.org/resources/Pages/ImprovementStories/WhatIsaBundle.aspx. Accessed 20 Nov 2020.
- 51.Wright MO, Allen-Bridson K, Hebden JN. Assessment of the accuracy and consistency in the application of standardized surveillance definitions: a summary of the American Journal of Infection Control and National Healthcare Safety Network case studies, 2010-2016. Am J Infect Control. 2017;45(6):607–611. doi: 10.1016/j.ajic.2017.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rodríguez-Acelas AL, de Abreu AM, Engelman B, Cañon-Montañez W. Risk factors for health care-associated infection in hospitalized adults: systematic review and meta-analysis. [internet] Am J Infect Control. 2017;45(12):e149–e156. doi: 10.1016/j.ajic.2017.08.016. [DOI] [PubMed] [Google Scholar]
- 53.Eccles M, Grimshaw J, Campbell M, Ramsay C. Research designs for studies evaluating the effectiveness of change and improvement strategies. Qual Saf Health Care. 2003;12(1):47–52. doi: 10.1136/qhc.12.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Knudsen SV, Laursen HVB, Johnsen SP, Bartels PD, Ehlers LH. Mainz, J. can quality improvement improve the quality of care: a systematic review of reported effects and methodological rigor in plan-do-study-act projects. [internet] BMC Health Serv Res. 2019;19:683. doi: 10.1186/s12913-019-4482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hirschhorn LR, Ramaswamy R, Devnani M, Wandersman A, Simpson LA, Garcia-Elorrio E. Research versus practice in quality improvement? Understanding how we can bridge the gap. Int J Qual Health Care. 2018;30(1):24–28. doi: 10.1093/intqhc/mzy018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hsu YJ, Kosinski AS, Wallace AS, Saha-Chaudhuri P, Chang BH, Speck K, et al. Using a society database to evaluate a patient safety collaborative: the cardiovascular surgical translational study. [internet] J Comp Eff Res. 2019;8(1):21–32. doi: 10.2217/cer-2018-0051. [DOI] [PubMed] [Google Scholar]
- 57.Itri JN, Bakow E, Probyn L, Kadom N, Duong PT, Gettle LM, et al. The science of quality improvement. Acad Radiol. 2017;24(3):253–262. doi: 10.1016/j.acra.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 58.Finkelstein JA, Brickman AL, Capron A, Ford DE, Gombosev A, Greene SM, et al. Oversight on the borderline: quality improvement and pragmatic research [internet] Clin Trials. 2015;12(5):457–466. doi: 10.1177/1740774515597682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. REDCap Consortium, The REDCap consortium: building an international community of software partners [internet]. J Biomed Inform. 2019. 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed]
- 61.Hsu YJ, Marsteller JA. Influence of the comprehensive unit-based safety program in ICUs: evidence from the keystone ICU project. [internet]. 2016, 2015;31(4):349–57. 10.1177/1062860615571963. [DOI] [PubMed]
- 62.Berenholtz SM, Pham JC, Thompson DA, Needham DM, Lubomski LH, Hyzy RC, et al. Collaborative cohort study of an intervention to reduce ventilator-associated pneumonia in the intensive care unit. [internet]. Infect Control Hosp Epidemiol. 2011;32(4):305–14 Available from: https://pubmed.ncbi.nlm.nih.gov/21460481/. Accessed 20 Nov 2020. [DOI] [PubMed]
- 63.Jain R, Kralovic SM, Evans ME, Ambrose M, Simbartl LA, Obrosky DS, Render ML, Freyberg RW, Jernigan JA, Muder RR, Miller LTJ, Roselle GA. Veterans affairs initiative to prevent methicillin-resistant staphylococcus aureus infections. N Engl J Med. 2011;364(15):1419–1430. doi: 10.1056/NEJMoa1007474. [DOI] [PubMed] [Google Scholar]
- 64.Hessels AJ, Genovese-Schek V, Agarwal M, Wurmser T, Larson EL. Relationship between patient safety climate and adherence to standard precautions. Am J Infect Control. 2016;44(10):1128–1132. doi: 10.1016/j.ajic.2016.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Braddock CH, Szaflarski N, Forsey L, Abel L, Hernandez-Boussard T, Morton J. The TRANSFORM patient safety project: a microsystem approach to improving outcomes on inpatient units [internet] J Gen Intern Med. 2015;30(4):425–433. doi: 10.1007/s11606-014-3067-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chang BH, Hsu YJ, Rosen M, Gurses AP, Huang S, Xie A, et al. Reducing three infections across cardiac surgery programs: a multisite cross-unit collaboration [internet] Am J Med Qual. 2020;35(1):37–45. doi: 10.1177/1062860619845494. [DOI] [PubMed] [Google Scholar]
- 67.Fan CJ, Pawlik TM, Daniels T, Vernon N, Banks K, Westby P, et al. Association of safety culture with surgical site infection outcomes [internet] J Am Coll Surg. 2016;222(2):122–128. doi: 10.1016/j.jamcollsurg.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 68.Meddings J, Reichert H, Greene MT, Safdar N, Krein SL, Olmsted RN, et al. Evaluation of the association between hospital survey on patient safety culture (HSOPS) measures and catheter-associated infections: results of two national collaboratives. [internet] BMJ Qual Saf. 2017;26:226–235. doi: 10.1136/bmjqs-2015-005012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Richter JP, McAlearney AS. Targeted implementation of the comprehensive unit-based safety program through an assessment of safety culture to minimize central line-associated bloodstream infections [internet]. Health Care Manage [cited: Jan/Mar 2018];43(1):42–49. Available from: https://pubmed.ncbi.nlm.nih.gov/27529403/. [DOI] [PubMed]
- 70.Sakowski JA, Hooper L, Holton T, Brody AA. Partners advancing clinical excellence: building professional councils for quality improvement at six community hospitals. Creat Nurs. 2012;18(4):177–186. doi: 10.1891/1078-4535.18.4.177. [DOI] [PubMed] [Google Scholar]
- 71.Smith SA, Yount N, Sorra J. Exploring relationships between hospital patient safety culture and consumer reports safety scores. [internet] BMC Health Serv Res. 2017;17:143. doi: 10.1186/s12913-017-2078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Choi SW, Chang L, Hanauer DA, Shaffer-Hartman J, Teitelbaum D, Lewis I, et al. Rapid reduction of central line infections in hospitalized pediatric oncology patients through simple quality improvement methods. [internet] Pediatr Blood Cancer. 2013;60(2):262–269. doi: 10.1002/pbc.24187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lin DM, Carson KA, Lubomski LH, Wick EC, Cuong J. Statewide collaborative to reduce surgical site infections: results of the Hawaii surgical unit-based safety program [internet]. J Am Coll Surg; 1 Aug 2018 [cited: 18 May 2018]. 227(2):189–197.E1. Available from: https://www.journalacs.org/article/S1072-7515(18)30330-2/fulltext [DOI] [PubMed]
- 74.Mayer CM, Cluff L, Lin W-T, Willis TS, Stafford RE, Williams C, Saunders R, Short KA, Lenfestey N, Kane HL, Amoozegar JB. Evaluating efforts to optimize TeamSTEPPS implementation in surgical and pediatric intensive care units. Jt Comm J Qual Patient Saf. 2011;37(8):365–AP3. doi: 10.1016/s1553-7250(11)37047-x. [DOI] [PubMed] [Google Scholar]
- 75.Millson T, Hackbarth D, Bernard HL. A demonstration project on the impact of safety culture on infection control practices hemodialysis. [internet]. Am J Infect Control. 2019;47(9):1122–9. 10.1016/j.ajic.2019.02.026. [DOI] [PubMed]
- 76.Thomas-Hawkins C, Flynn L. Patient safety culture and nurse-reported adverse events in outpatient hemodialysis units [internet] Res Theory Nurs Pract Int J. 2015;29(1):53–65. doi: 10.1891/1541-6577.29.1.53. [DOI] [PubMed] [Google Scholar]
- 77.Sreeramoju P, Dura L, Fernandez ME, Minhajuddin A, Simacek K, Fomby TB, et al. Using a positive deviance approach to influence the culture of patient safety related to infection prevention. [internet] Open Forum Infect Dis. 2018;5(10):ofy231. doi: 10.1093/ofid/ofy231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rawat N, Yang T, Ali KJ, Catanzaro M, Cohen MD, Farley DO, et al. Two-state collaborative study of a multifaceted intervention to decrease ventilator-associated events. [internet] Crit Care Med. 2017;45(7):1208–1215. doi: 10.1097/CCM.0000000000002463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Abusalem S, Polivka B, Coty MB, Crawford TN, Furman CD, Alaradi M. The relationship between culture of safety and rate of adverse events in long-term care facilities. J Patient Saf. 2019. 10.1097/PTS.0000000000000587. [DOI] [PubMed]
- 80.Smith SN, Greene MT, Mody L, Banaszak-Holl J, Peterson LD, Meddings J. Evaluation of the association between nursing home survey on patient safety culture (NHSOPS) measures and catheter-associated urinary tract infections: results of a national collaborative. BMJ Qual Saf. 2018;27:464–473. doi: 10.1136/bmjqs-2017-006610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Daugherty EL, Paine LA, Maragakis LL, Sexton JB, Rand CS. Safety culture and hand hygiene: linking attitudes to behavior. [internet]. Infect Control Hosp Epidemiol. 2012;33(12):1280–2 Available from: http://www.jstor.org/stable/10.1086/668432. Accessed 20 Nov 2020. [DOI] [PubMed]
- 82.Hsu YJ, Marsteller JA. Who applies an intervention to influence cultural attributes in a quality improvement collaborative? J Patient Saf. 2015;16(1):1–6 Available from: https://pubmed.ncbi.nlm.nih.gov/26164707/. Accessed 20 Nov 2020. [DOI] [PubMed]
- 83.Meeks DW, Lally KP, Carrick MM, Lew DF, Thomas EJ, Doyle PD, et al. Compliance with guidelines to prevent surgical site infections: as simple as 1-2-3. [internet] Am J Surg. 2011;201(1):76–83. doi: 10.1016/j.amjsurg.2009.07.050. [DOI] [PubMed] [Google Scholar]
- 84.Profit J, Sharek PJ, Kan P, Rigdon J, Desai M, Nisbet CC, et al. Teamwork in the NICU setting and its association with healthcare-associated infections in very low birth weight infants. [internet] Am J Perinatol. 2017;34(10):1032–1040. doi: 10.1055/s-0037-1601563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Profit J, Sharek PJ, Cui X, Nisbet CC, Thomas EJ, Tawfik DS, et al. The correlation between NICU safety culture and quality of care. J Patient Saf. 2020;2018(7):1–21 Available from: https://pubmed.ncbi.nlm.nih.gov/30407963/. Accessed 20 Nov 2020. [DOI] [PMC free article] [PubMed]
- 86.Vigorito MC, McNicoll L, Adams L, Sexton B. Improving safety culture results in Rhode Island ICUs: lessons learned from the development of action-oriented plans. Jt Comm J Qual Saf. 2011;37(11):509–14 AP1. [DOI] [PubMed]
- 87.Brilli RJ, McClead RE, Crandall WV, Stoverock L, Berry JC, Wheeler TA. A comprehensive patient safety program can significantly reduce preventable harm, associated costs, and hospital mortality. J Pediatr Dec. 2013;163(6):1638–1645. doi: 10.1016/j.jpeds.2013.06.031. [DOI] [PubMed] [Google Scholar]
- 88.Southworth SL, Henman LJ, Kinder LA, Sell JL. The journey to zero central catheter-associated bloodstream infections: culture change in an intensive care unit. Crit Care Nurse. 2012;32(2):49–54. doi: 10.4037/ccn2012915. [DOI] [PubMed] [Google Scholar]
- 89.Miller MA, Krein SL, Saint S, Kahn JM, Iwashyna TJ. Organizational characteristics associated with the use of daily interruption of sedation in US hospitals: a national study. BMJ Qual Saf. 2012;21(2):145–151. doi: 10.1136/bmjqs-2011-000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pronovost PJ, Marsteller JA, Goeschel CA. Preventing bloodstream infections: a measurable national success story in quality improvement. Health Aff (Millwood) 2011;30(4):628–634. doi: 10.1377/hlthaff.2011.0047. [DOI] [PubMed] [Google Scholar]
- 91.Nelson S, Stone PW, Jordan S, Pogorzelska M, Halpin H, Vanneman M, et al. Patient safety climate: variation in perceptions by infection preventionists and quality directors. Interdiscip Perspect Infect Dis. 2011;2011:357121. doi: 10.1155/2011/357121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pogorzelska-Maziarz M, Nembhard IM, Schnall R, Nelson S, Stone PW. Psychometric evaluation of an instrument for measuring organizational climate for quality: evidence from a national sample of infection preventionists. [internet]. Am J Med Qual. 2016;31(5):441–7. 10.1177/1062860615587322. [DOI] [PMC free article] [PubMed]
- 93.Gilmartin HM, Sousa KH. Testing the quality health outcomes model applied to infection prevention in hospitals. [internet] Qual Manag health care. 2016;25(3):149–161. doi: 10.1097/QMH.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kelly D, Kutney-Lee A, Lake ET, Aiken LH. The critical care work environment and nurse-reported health care-associated infections. Am J Crit Care. 2013;22(6):482–488. doi: 10.4037/ajcc2013298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Garland KV. A survey of United States dental hygienists’ knowledge, attitudes, and practices with infection control guidelines. J Dent Hyg. 2013;87(3):140–151. [PubMed] [Google Scholar]
- 96.Yanke E, Moriarty H, Carayon P, Safdar N. A qualitative, interprofessional analysis of barriers to and facilitators of implementation of the Department of Veterans Affairs’ Clostridium difficile prevention bundle using a human factors engineering approach. Am J Infect Control. 2018;46(3):276–284. doi: 10.1016/j.ajic.2017.08.027. [DOI] [PubMed] [Google Scholar]
- 97.Sinkowitz-Cochran RL, Burkitt KH, Cuerdon T, Harrison C, Gao S, Obrosky DS, Jain R, Fine MJ, Jernigan JA. The associations between organizational culture and knowledge, attitudes, and practices in a multicenter veterans affairs quality improvement initiative to prevent methicillin-resistant Staphylococcus aureus. Am J Infect Control. 2012;40:138–143. doi: 10.1016/j.ajic.2011.04.332. [DOI] [PubMed] [Google Scholar]
- 98.Talbot TR, Johnson JG, Fergus C, Domenico JH, Schaffner W, Daniels TL, Wilson G, Slayton J, Feistritzer N, Hickson GB. Sustained improvement in hand hygiene adherence: utilizing shared accountability and financial incentives. Infect Control Hosp Epidemiol. 2013;34(11):1129–1136. doi: 10.1086/673445. [DOI] [PubMed] [Google Scholar]
- 99.Lyles RD, Moore NM, Weiner SB, Sikka M, Lin MY, Weinstein RA, et al. Understanding staff perceptions about klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae control efforts in Chicago long-term acute care hospitals [internet] Infect Control Hosp Epidemiol. 2014;35(4):367–374. doi: 10.1086/675596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Robbins J, McAlearney AS. Encouraging employees to speak up to prevent infections: opportunities to leverage quality improvement and care management processes. Am J Infect Control. 2016;44(11):1224–30. 10.1016/j.ajic.2016.03.007. [DOI] [PubMed]
- 101.Harnage S. Seven years of zero central-line associated bloodstream infections. Br J Nurs. 2012;21(21):S6–S12. doi: 10.12968/bjon.2012.21.Sup21.S6. [DOI] [PubMed] [Google Scholar]
- 102.Miller K, Briody C, Casey D, Kane JK, Mitchell D, Patel B, Ritter C, Seckel M, Wakai S, Drees M. Using the comprehensive unit-based safety program model for sustained reduction in hospital infections. Am J Infect Control. 2016;44:969–976. doi: 10.1016/j.ajic.2016.02.038. [DOI] [PubMed] [Google Scholar]
- 103.Phipps AR, Paradis M, Peterson KA, Jensen J, Nielsen K, Hall M, et al. Reducing serious safety events and priority hospital-acquired conditions in a pediatric hospital with the implementation of a patient safety program. The Joint Commission. 2018;44:334–340. doi: 10.1016/j.jcjq.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 104.Wick EC, Galante DJ, Hobson DB, Benson AR, Lee K, Berenholtz SM, et al. Organizational culture changes result in improvement in patient-centered outcomes: implementation of an integrated recovery pathway for surgical patients [internet] J Am Coll Surg. 2015;221(3):669–677. doi: 10.1016/j.jamcollsurg.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 105.DePalo VA, McNicoll L, Cornell M, Rocha MC, Adams L, Pronovost PJ. The Rhode Island ICU collaborative: a model for reducing central line-associated bloodstream infection and ventilator-associated pneumonia statewide [internet]. Qual Saf Health Care. 2010;19:555–61. 10.1136/qshc.2009.038265. [DOI] [PubMed]
- 106.Joyce JS, Cioffi GA, Petriwsky JG, Robinson JS. Legacy Health’s ‘Big Aims’ initiative to improve patient safety reduced rates of infection and mortality among patients. Health Aff (Millwood). 2011;30(4):619–627. doi: 10.1377/hlthaff.2011.0024. [DOI] [PubMed] [Google Scholar]
- 107.Medina A, Serratt T, Pelter M, Brancamp T. Decreasing central line-associated bloodstream infections in the non-ICU population. J Nurs Care Qual. 2014;29(2):133–140. doi: 10.1097/NCQ.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 108.Robinson C, Hevener S, Hoze M, Nichols AA. Ventilator-associated pneumonia patients in the intensive care unit. JONA. 2018;48(2):79–84. doi: 10.1097/NNA.0000000000000578. [DOI] [PubMed] [Google Scholar]
- 109.Rosenberg RE, Devins L, Geraghty G, Bock S, Dugan CA, Transou M, et al. Engaging frontline staff in central line-associated bloodstream infection prevention practice in the wake of superstorm Sandy. The Joint Commission. 2015;41(10):462–468. doi: 10.1016/s1553-7250(15)41060-8. [DOI] [PubMed] [Google Scholar]
- 110.Cumbler E, Castillo L, Satorie L, Ford D, Hagman J, Hodge T, Price L, Wald H. Culture change in infection control. Applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013;28(4):304–311. doi: 10.1097/NCQ.0b013e31829786be. [DOI] [PubMed] [Google Scholar]
- 111.Day C. Engaging the nursing workforce. An evidence-based tool kit. Nurs Adm Q. 2009;33(3):238–244. doi: 10.1097/NAQ.0b013e3181accb31. [DOI] [PubMed] [Google Scholar]
- 112.Foulk KC, Tocydlowski P, Snow TM, McCloud K, Cuevas M, Bishop D, et al. Infusing fun into quality and safety initiatives. Nurs. 2012:14–6. [DOI] [PubMed]
- 113.Johnson L, Grueber S, Schlotzhauer C, Phillips E, Bullock P, Basnett J, Hahn-Cover K. A multifactorial action plan improves hand hygiene adherence and significantly reduces central line-associated bloodstream infections. Am J Infect Control. 2014;42:1146–1151. doi: 10.1016/j.ajic.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 114.Raveis VH, Conway LJ, Uchida M, Pogorzelska-Maziarz M, Larson EL, Stone PW. Translating infection control guidelines into practice: implementation process within a health care institution. Qual Health Res. 2014;24(4):551–560. doi: 10.1177/1049732314524488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Campione JR, Yount ND, Sorra J. Questions regarding the authors’ conclusions about the lack of change in hospital survey on patient safety culture (HSOPS) scores related to reduction of hospital-acquired infections [internet] BMJ Qual Saf. 2018;27:e3. doi: 10.1136/bmjqs-2017-007360. [DOI] [PubMed] [Google Scholar]
- 116.Borg MA, Camilleri L, Waisfisz B. Understanding the epidemiology of MRSA in Europe: do we need to think outside the box? J Hosp Infect. 2012;81:251e256. doi: 10.1016/j.jhin.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 117.Su G. A collaborative approach to reduce healthcare-associated infections. Br J Nurs. 2016;25:582–586. doi: 10.12968/bjon.2016.25.11.582. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available upon request.