Abstract
Background
The global COVID-19 pandemic has generated major mental and psychological health problems worldwide. We conducted a meta-analysis to assess the prevalence of depression, anxiety, distress, and insomnia during the COVID-19 pandemic.
Methods
We searched online biomedical databases (PubMed, Embase, Web of Science, Ovid, CNKI, and Wanfang Data) and preprint databases (SSRN, bioRxiv, and MedRxiv) for observational studies from January 1, 2020 to March 16, 2020 investigating the prevalence of mental health problems during the COVID-19 pandemic.
Results
We retrieved 821 citations from the biomedical databases and 53 citations from the preprint databases: 66 studies with 221,970 participants were included in our meta-analysis. The overall pooled prevalence of depression, anxiety, distress, and insomnia was 31.4%, 31.9%, 41.1% and 37.9%, respectively. Noninfectious chronic disease patients, quarantined persons, and COVID-19 patients had a higher risk of depression (Q=26.73, p<0.01) and anxiety (Q=21.86, p<0.01) than other populations. The general population and non-medical staff had a lower risk of distress than other populations (Q=461.21, p< 0.01). Physicians, nurses, and non-medical staff showed a higher prevalence of insomnia (Q=196.64, p<0.01) than other populations.
Limitations
All included studies were from the early phase of the global pandemic. Additional meta-analyses are needed to obtain more data in all phases of the pandemic.
Conclusions
The COVID-19 pandemic increases the mental health problems of the global population, particularly health care workers, noninfectious chronic disease patients, COVID-19 patients, and quarantined persons. Interventions for mental health are urgently needed for preventing mental health problems.
Keywords: COVID-19, Depression, Anxiety, Distress, Insomnia, Systemic review
1. Introduction
COVID-19 has spread rapidly worldwide (Zhu et al., 2020a). On January 30, 2020, the International Health Regulations (2005) Emergency Committee declared the COVID-19 outbreak a Public Health Emergency of International Concern (World Health Organization, 2020a). Subsequently, COVID-19 was characterized as a pandemic by the World Health Organization (WHO) on March 11, 2020 (World Health Organization, 2020c). According to the latest data from the WHO, as of July 15, 2020 over 13 million people have been infected in 217 countries and regions worldwide, with more than 572,000 deaths reported (World Health Organization, 2020b). Individual and government responses to this major public health emergency have affected the lives of hundreds of millions of people and changed people's ways of socializing, working, studying and living. Mental health problems such as anxiety, sleep disorders, depression, frustration, and stress-related disorders may be caused by worry about becoming infected, increasing work pressure, lifestyle changes and worsening living conditions (Pulvirenti et al., 2020; Zhang et al., 2020d).
The types and severity of mental health problems may vary among people with different health conditions and social roles, due in turn to differences in the risk of becoming infected and influence on lifestyle (Tan et al., 2020). Previous studies on the health impacts of outbreaks of infectious diseases, such as severe acute respiratory syndrome (SARS) (Lu et al., 2006; Wing and Leung, 2012), influenza caused by H1N1 (Matsuishi et al., 2012), Middle East respiratory syndrome (MERS) (Jeong et al., 2016), and Ebola virus (Kisely et al., 2020), suggested that mental health problems may occur among health care workers and other populations during major public health emergencies. There have been similar reports during the COVID-19 outbreak (González-Sanguino et al., 2020; Kong et al., 2020; Tang et al., 2020; Zhang et al., 2020b). The United Nations reported that the COVID-19 pandemic is not only compromising physical health, but is also increasing psychological suffering (United Nations, 2020). Therefore, the mental health status of populations during this pandemic is of great importance.
The rapid spread of COVID-19 worldwide multiplied by forced quarantine and nationwide lockdowns could lead to public panic (Bao et al., 2020; Dubey et al., 2020), and cause rumors and conspiracy theories to spread (Addis et al., 2020; Ali, 2020). For health care workers, the stress of dealing with patients could affect their mental health, reduce their ability to work, and even lead to a lack of clinical competency (Greenberg et al., 2020; Liu et al., 2020c). These effects could ultimately be worse than the direct consequences of the COVID-19 pandemic itself (Bao et al., 2020). Therefore, comprehensive understanding of the prevalence of mental health problems during the COVID-19 pandemic on different populations is needed so that policymakers can implement effective countermeasures. Although many studies have evaluated the prevalence of the aforementioned mental health problems, most recent studies have focused on between one and three different populations (Huang and Zhao, 2020; Kong et al., 2020; Tan et al., 2020); comparative studies of multiple populations are still lacking. We conducted a systematic review and meta-analysis using data pooled from seven populations to provide a comprehensive perspective of the prevalence mental health problems during the COVID-19 pandemic and identify high risk groups of mental health problems related to COVID-19 pandemic. Governments should include mental health care in national public health emergency response plans, and prioritize interventions for high-risk populations.
2. Methods
2.1. Search strategy and study selection
The search strategy was designed based on MeSH terms and free-text keywords (shown in online Supplementary Table S1), and citation retrieval was conducted by two authors independently. Biomedical databases (PubMed, Embase, Web of Science, Ovid, CNKI, and Wanfang Data) and preprint databases (SSRN, bioRxiv, and MedRxiv) were searched for studies published between January 1, 2020 to March 16, 2020, without language restrictions. Two authors independently screened the titles and abstracts, and reviewed the full text of articles meeting the following criteria: (1) cross-sectional study, cohort study, case-control study, or intervention study; (2) use of a validated measurement tool to assess mental or psychological health outcomes including depression, anxiety, distress, and insomnia in the general, or a specific, population since the COVID-19 pandemic; (3) use of standardized measurement tools; and (4) inclusion of point prevalence data for each outcome. We also included the control group or baseline survey of the intervention studies in the searched citations into the analysis, and both randomized and non-randomized intervention studies were considered. The protocol for this systematic review and meta-analysis was registered on PROSPERO (CRD42020178045) and can be accessed at: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=178045
2.2. Data extraction
Two authors extracted the primary data independently using a standardized data extraction form; the data were then checked by a third author. The following data were extracted: title, first author names, country, date of survey, study participants, measurement tools, sample sizes, and number of positive cases for each symptom.
2.3. Assessment of risk of bias
The methodological quality of the included studies was assessed using Strengthening the Reporting of Observational Studies in Epidemiology (STROBE), which assesses cross-sectional studies for risk of bias based on the design, participants, sample size, measurement tools, data collection methods, confounders, and statistical analyses (von et al., 2007). The risk of bias was classified as low risk (study reported sufficient data for quality assessment and fulfilled the criteria for the quality item), partial risk (study reported incomplete data for the quality item were reported or had an intermediate risk of bias), or high risk (study reported sufficient data for quality assessment but didn't fulfill the criteria for the quality item).
2.4. Mental health outcomes and subgroup comparisons
In this study, we focused on four mental health outcomes: depression, anxiety, distress, and insomnia. Several self-administered screening measurement tools were used to evaluate the four outcomes, each with its own threshold scores for a particular symptom. Articles that used a non-standard threshold to define a particular symptom were excluded.
We compared the mental health of different populations. The overall population was divided into seven groups: (1) general population; (2) noninfectious chronic disease patients, including patients with cancer, diabetes, or chronic kidney disease; (3) students, including university, college, and middle school students; (4) physicians and nurses working in clinical departments; (5) non-medical staff working in non-clinical departments, including technicians, administrators, clerical staff, and logistics staff; (6) quarantined persons; and (7) COVID-19 patients. Only one study (Hua et al., 2020) reported on the distress level of a group suspected as being infected by SARS CoV-2, so “suspected infection” was included as a further subgroup. We divided physicians and nurses into front-line (directly engaged in diagnosing, treating, or providing care to patients with elevated temperatures, or confirmed COVID-19) and second-line workers.
2.5. Data Synthesis and Statistical Analyses
Freeman-Tukey double arcsine transformation was used to stabilize the variance of the raw data (Freeman and Tukey, 1950). The I2 statistic was used to assess the statistical heterogeneity (Higgins et al., 2003). We used DerSimonian-Laird random-effects meta-analysis to pool the raw data for each outcome, and the Clopper-Pearson interval to calculate the confidence interval (CI) for each variable (DerSimonian and Laird, 1986). Egger regression and funnel plots were used to assess publication bias (Egger et al., 1997). A series of random-effects meta-regression models was performed to determine the effects of between-group difference of the following variables: participants, published language, gender, and measurement tools. Sensitivity analyses was conducted to evaluate the impact of methodological quality of included studies on pooled results and to explore potential sources of heterogeneity. We used the Cochran's Q test to compare the different populations. All statistical tests were two-tailed and p <s0.05 was considered statistically significant. The analyses were performed using R software (version 3.6.3; R Development Core Team, Vienna, Austria) and the ‘meta’ package (version 4.11-0).
3. Results
3.1. Studies selection
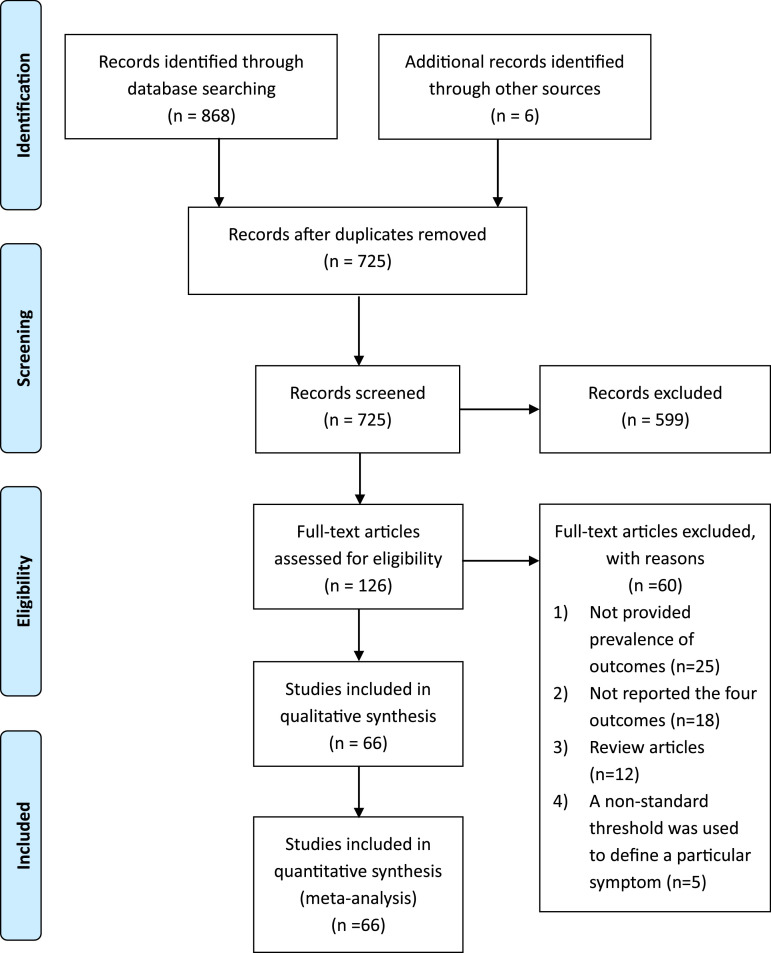
We retrieved 821 citations from the biomedical databases and 53 from the preprint databases, up to April 2020. 803 citations were excluded due to duplicate publication, review articles, did not focus on mental or psychological health, did not evaluate depression, anxiety, distress, or insomnia, or did not report point prevalence for the outcomes of interest. We excluded another five studies (Chen et al., 2020a; Hong et al., 2020; Nguyen et al., 2020; Qian et al., 2020; and Zhang and Ma, 2020) that used a non-standard threshold to define a particular symptom. Ultimately, we included 66 studies with a total of 221,970 participants. Figure 1 shows the study selection process.
Figure 1.
PRISMA Flowchart of citations selection
3.2. Characteristics of included studies
The characteristics of included studies are showed in online Supplementary Table S2. Depression data were reported by 48 studies with 125,121 participants drawn from seven populations, anxiety data were reported by 53 studies with 128,855 participants drawn from seven populations, distress data were reported by 10 studies with 67,950 participants drawn from five populations, and insomnia data were reported by 8 studies with 23,022 participants drawn from four populations. Of the included studies, 95.5% were cross-sectional, and most were online surveys; two were interventional studies (Huang and Ke, 2020; Yang et al., 2020b) and one was a qualitative interview (Cao et al., 2020b). Most of the studies (62 of 66) were for the Chinese population, although there was one each from Iran (Moghanibashi-Mansourieh, 2020), Jordan (Naser et al., 2020), Singapore (Tan et al., 2020), and India (Kazmi, 2020). All included surveys were conducted between January 1, 2020, and April 1, 2020.
3.3. Risk of bias in the included studies
The risk of bias in the included studies are shown in Figure S1 and S2. Of the 66 studies, none were judged as high risk on all risk of bias measures; 61 reported clear definitions and measurement methods for all four outcomes, 13 did not report participant recruitment dates, 32 reported using consecutive or random sampling, and 27 reported the number of individuals enrolled at each stage of the study. All 66 studies reported the characteristics of the study participants.
3.4. Prevalence of depression
The point prevalence of depression ranged from 3.1% to 87.3% among 48 studies and seven populations; the overall pooled prevalence was 31.4% (95% CI: 27.3–35.5%) and a high degree of heterogeneity was found (I2 = 99.6%), as shown in Table 1 and online Supplementary Figure S3. The point prevalence of depression showed a significant difference among the seven populations (Q = 26.73, p <0.01). In subgroup analyses, the prevalence of depression was in the following (descending order): noninfectious chronic disease patients (44.8%, 95% CI: 36.4–53.2%), COVID-19 patients (41.7%, 95% CI: 26.3–57.9%), quarantined persons (38.8%, 95% CI: 19.7–59.9%), students (34.8%, 95% CI: 16.4–55.9%), the general population (31.5%, 95% CI: 24.2–39.2%), physicians and nurses (31.0%, 95% CI: 24.7–37.5%), and non-medical staff (14.1%, 95% CI: 7.4–22.4%). We compared the medical personnel (physicians and nurses) between front- and second-line, as shown in Table 2 and online Supplementary Figure S7. The prevalence of depression was not significantly different (Q = 0.02, p = 0.88) between front- and second-line medical personnel.
Table 1.
Prevalence of mental health problems in difference populations.
| Mental health outcomes | No. of studies | Positive cases | Simple size | Pooled prevalence (%) | Heterogeneity I2 (%) | Q statistic | P value |
|---|---|---|---|---|---|---|---|
| Depression | |||||||
| Overall depression | 64 | 42,876 | 125,121 | 31.4 (27.3–35.5) | 99.6 | ||
| General population | 17 | 25,115 | 69,697 | 31.5 (24.2–39.2) | 99.8 | 26.73 | <0.01 |
| Noninfectious chronic disease patients | 2 | 72 | 161 | 44.8 (36.4–53.2) | 16.0 | ||
| Students | 7 | 3,697 | 10,128 | 34.8 (16.4–55.9) | 99.8 | ||
| Physicians and nurses | 23 | 13,360 | 41,889 | 31.0 (24.7–37.5) | 99.5 | ||
| Other medical staff | 6 | 296 | 2,471 | 14.1 (7.4–22.4) | 95.4 | ||
| Quarantined persons | 5 | 169 | 367 | 38.8 (19.7–59.9) | 93.6 | ||
| COVID-19 patients | 4 | 167 | 480 | 41.7 (26.3–57.9) | 90.3 | ||
| Anxiety | |||||||
| Overall anxiety | 69 | 41,498 | 128,855 | 31.9 (27.9–36.0) | 99.6 | ||
| General population | 18 | 21,310 | 57,898 | 29.8 (21.5–38.8) | 99.8 | 21.86 | <0.01 |
| Noninfectious chronic disease patients | 3 | 99 | 185 | 55.4 (37.8–72.3) | 82.7 | ||
| Students | 8 | 4,978 | 17,257 | 28.2 (16.8–41.2) | 99.7 | ||
| Physicians and nurses | 23 | 14,312 | 50,143 | 29.0 (23.6–34.7) | 99.4 | ||
| Other medical staff | 7 | 378 | 2,521 | 19.9 (12.4–28.6) | 94.8 | ||
| Quarantined persons | 5 | 235 | 367 | 57.9 (34.4–79.7) | 94.9 | ||
| COVID-19 patients | 5 | 186 | 484 | 42.3 (27.3–58.1) | 91.5 | ||
| Distress | |||||||
| Overall distress | 14 | 23,147 | 67,950 | 41.1 (32.6–49.8) | 99.6 | ||
| General population | 4 | 19,263 | 56,528 | 31.1 (25.8–36.8) | 97.2 | 461.68 | <0.01 |
| Noninfectious chronic disease patients | 2 | 110 | 232 | 49.1 (36.0–62.3) | 73.5 | ||
| Physicians and nurses | 5 | 3,325 | 10,165 | 41.2 (19.8–64.5) | 99.8 | ||
| Other medical staff | 2 | 194 | 769 | 17.3 (1.3–45.4) | 98.1 | ||
| Suspected infection | 1 | 255 | 256 | 99.6 (98.3–100.0) | - | ||
| Insomnia | |||||||
| Overall insomnia | 11 | 6,430 | 23,022 | 37.9 (29.9–46.2) | 99.3 | ||
| General population | 1 | 1,317 | 7,236 | 18.2 (17.3–19.1) | - | 196.64 | <0.01 |
| Students | 1 | 79 | 1,031 | 7.7 (6.1–9.4) | - | ||
| Physicians and nurses | 7 | 4,606 | 13,375 | 47.3 (38.8–55.8) | 98.7 | ||
| Other medical staff | 2 | 428 | 1,380 | 31.8 (27.2–36.5) | 37.5 |
Table 2.
Prevalence of mental health problems between front-line and second-line medical workers
| Mental health outcomes | No. of studies | Positive cases | Simple size | Pooled prevalence (%) | Heterogeneity I2 (%) | Q statistic | P value |
|---|---|---|---|---|---|---|---|
| Depression | |||||||
| Overall depression | 13 | 9,412 | 29,866 | 32.9 (26.9–39.2) | 99.2 | ||
| Front-line physicians and nurses | 7 | 3,628 | 10,466 | 33.3 (23.8–43.5) | 99.0 | 0.02 | 0.88 |
| Second-line physicians and nurses | 6 | 5,784 | 19,400 | 32.4 (24.0–41.3) | 99.3 | ||
| Anxiety | |||||||
| Overall anxiety | 12 | 7,205 | 29,829 | 27.5 (21.9–33.4) | 99.2 | ||
| Front-line physicians and nurses | 6 | 2,874 | 10,429 | 28.8 (20.7–37.6) | 98.9 | 0.18 | 0.67 |
| Second-line physicians and nurses | 6 | 43,310 | 19,400 | 26.2 (18.4–34.8) | 99.4 |
3.5. Prevalence of anxiety
The point prevalence of anxiety ranged from 6.3% to 87.5% in the 53 studies with 7 populations. The pooled prevalence of anxiety was 31.9% (95% CI: 27.9–36.0%) with and a high degree of heterogeneity was found (I2 = 99.6%), as shown in Table 1 and online Supplementary Figure S4. The prevalence of anxiety was significantly different among the seven populations (Q = 21.86, p <0.01). In subgroup comparisons, quarantined persons (57.9%, 95% CI: 34.4–79.7%) showed the highest prevalence of anxiety, followed in descending order by noninfectious chronic disease patients (55.4%, 95% CI: 37.8–72.3%), COVID-19 patients (42.3%, 95% CI: 27.3–58.1%), the general population (29.8%, 95% CI: 21.5–38.8%), physicians and nurses (29.0%, 95% CI: 23.6–34.7%), students (28.2%, 95% CI: 16.8–41.2%), and non-medical staff (19.9%, 95% CI: 12.4–28.6%). We also compared the physicians and nurses between front- and second-line, as shown in Table 2 and online Supplementary Figure S8. The prevalence of anxiety didn't show significant difference (Q = 0.18, p = 0.67) between front- and second-line medical personnel.
3.6. Prevalence of distress
In the 10 studies with five populations, the point prevalence of distress ranged from 6.4% to 99.6% and there was a high degree of heterogeneity (I2 = 99.6%). The overall prevalence of distress was 41.1% (95% CI: 32.6–49.8%), as shown in Table 1 and online Supplementary Figure S5. The prevalence of distress was significantly different among the five populations (Q = 461.21, p <0.01). Patients suspected of infection had the highest point prevalence of distress (99.6%, 95% CI: 98.3–100.0%), followed by noninfectious chronic disease patients (49.1%, 95% CI: 36.0–62.3%), physicians and nurses (41.5%, 95% CI: 19.4–65.4%), the general population (31.1%, 95% CI: 25.8–36.8%), and non-medical staff (17.3%, 95% CI: 1.3–45.4%).
3.7. Prevalence of insomnia
The point prevalence of insomnia was reported by the eight studies with four populations; the overall pooled prevalence was 37.9% (95%CI: 29.9–46.2%) and there was a high degree of heterogeneity (I2 = 99.3%), as shown in Table 1 and online Supplementary Figure S6. Subgroup analyses showed a significant difference among the four populations (Q = 196.64, p <0.01). Physicians and nurses had the highest rate of insomnia, at 47.3% (95% CI: 38.8–55.8%), followed by non-medical staff, at 31.8% (95% CI: 27.2–36.5%). The general population (18.2%, 95% CI: 17.3–19.1%) and students (7.7%, 95% CI: 6.1–9.4%) showed the lowest rates of insomnia.
3.8. Meta-regression and sensitivity analyses
The results of the meta-regression for each outcome (depression, anxiety, distress, and insomnia) are showed in online Supplementary Table S3, S4, S5, and S6, and the results of the sensitivity analyses for each outcome are presented in online Supplementary Table S7 and S8. Meta-regression showed no significant effects of published language and gender on pooled prevalence of depression and anxiety, while the effect on distress and insomnia were significant. We found significant effects of three measurement tools (GHQ-9, SDS, and WHO-5) in depression, and four measurement tools in distress (GHQ-12, IES, K6, PSS-10) on pooled results. Sensitivity analyses showed that in the methodological quality assessment, when item 1 (key elements of study design presented), item 3 (eligibility criteria, and methods of selection of participants provided), or item 6 (numbers of individuals at each stage of study reported) was assessed as partial or high risk, it would affect the pooled results. We used funnel plots to visualize and Egger regression to test the file-drawer effects for each of the outcomes. The funnel plots and the results of Egger regression are presented in online Supplementary Figure S9, S10, S11, and S12. We didn't find significant publication biases for the four outcomes.
4. Discussion
This meta-analysis of 66 studies (221,970 participants) was conducted to analyze the prevalence of mental health problems (depression, anxiety, distress, and insomnia) during the COVID-19 pandemic in different populations. Mental health problems were common in the different populations. The overall pooled prevalence of depression, anxiety, distress, and insomnia were 31.4% (95%CI: 27.3–35.5%), 31.9% (95% CI: 27.9–36.0%), 41.1% (95% CI: 32.6–49.8%) and 37.9% (95% CI: 29.9–46.2%), respectively. Subgroup comparisons showed that noninfectious chronic disease patients, quarantined persons, patients suspected of infection, and physicians and nurses had the highest prevalence of depression, anxiety, distress and insomnia, while non-medical staff had the lowest prevalence of depression, anxiety and distress. We did not find significant differences in the prevalence of depression and anxiety between front- and second-line medical personnel (physicians and nurses).
4.1. The COVID-19 pandemic increased the prevalence of mental health problems
Higher than normal levels of depression, anxiety, distress and insomnia have been reported since the outbreak of COVID-19. Previous studies found that 6.6% (95% CI: 5.9%–7.3%) of the general population of the USA were affected by major depressive disorder (Kessler et al., 2003), while 10.8% (95% CI: 9.1%–12.5%) and 14.7% (95% CI: 12.7%–16.6%) of the 3,001 adults selected at random from the general population of Sweden underwent depression and anxiety in 2009, respectively (Johansson et al., 2013). Elsewhere, 6.2% (95% CI: 3.4%–10.4%) of the adult indigenous population of Panama reported serious psychological distress under normal circumstances (Walker et al., 2019). All of these rates were much lower than those of all of the populations included in our analysis. Similarly, before the outbreak of COVID-19, the prevalence of insomnia in the general population of Turkey was 12.2% (95%CI: 11.2%–13.1%) (Benbir et al., 2015), while a meta-analysis reported a prevalence of insomnia among the general population of China of 15.0% (95% CI: 12.1%–18.5%) (Cao et al., 2017). Although a relatively high prevalence of insomnia was reported among the adult population of the USA, at 27.3% (Olfson et al., 2018), this did not exceed the prevalence of 47.3% and 31.8% for non-medical staff and physicians/nurses, respectively, in this study.
Therefore, a higher prevalence of mental health problems has resulted from COVID-19, as seen previously after other novel disease epidemics and natural disasters. All major emergencies, not just COVID-19, undoubtedly create mental health problems. Studies of past outbreaks showed that about 35% of SARS survivors in Hong Kong, and 31.2% of persons quarantined due to SARS in Toronto reported anxiety and/or depressive symptoms (Cheng et al., 2004; Hawryluck et al., 2004). Moreover, a meta-analysis of 27 studies revealed that the rates of psychological distress (overall standardized mean difference = 0.63, 95% CI: 0.27–0.98, p = 0.005) and psychiatric disorders (overall odds ratio = 1.84, 95% CI: 1.43–2.38, p < 0.001) increased after natural disasters (Beaglehole et al., 2018). With the continued spread of COVID-19, more attention should be paid to its potentially harmful effects on the mental health of the entire population (Cui et al., 2020). Physical activity was beneficial to mental health (Lavie et al., 2016) and immunity (Laddu et al., 2020). Encouraging and helping individuals be physically active during the COVID-19 pandemic could reduce the risk of mental health problems and achieve optimal immune support (Hall et al., 2020).
4.2. Focus on the high-risk groups
The patients with noninfectious chronic diseases in this study had the highest prevalence of depression, and high rates of anxiety and distress, which may be associated with local restrictions on movements (Brooks et al., 2020), inconvenient routine screening and medical treatments, and high economic costs (Egede and Zheng, 2003). Although no relevant study was found pertaining to previous epidemics, almost all cancer survivors’ comorbid chronic diseases were reportedly associated with anxiety (Yan et al., 2019), and type 2 diabetes patients were more likely to have major depressive disorder compared with the general population (odds ratio = 1.73, 95% CI:1.38–2.16) (Wang et al., 2019), even in the absence of infectious disease. This suggests that medical monitoring and treatments for patients with chronic diseases should be preoptimized during the COVID-19 pandemic to reduce the incidence of mental health problems. Other groups with serious mental health problems were those infected, or suspected to be infected with SARS-CoV-2 (Rogers et al., 2020), including COVID-19 patients, quarantined persons, and suspected cases. This may be due to fear of the consequences of infection (Xiang et al., 2020) or worry about being stigmatized or discriminated because of COVID-19 (Siu, 2008). Longer quarantine duration and infection fears could serve as stressors leading to serious emotional and psychological distress (Brooks et al., 2020). The prevalence of anxiety in quarantined persons was reported to be higher than in the general population, and even in confirmed patients (Chen et al., 2004; Jin et al., 2003), which may be related to the unknown outcomes (Li et al., 2020b). It is worth noting that SARS survivors continued to show higher levels of depression, anxiety, and posttraumatic symptoms 1 year after the outbreak, so the long-term adverse mental health effects of infectious diseases should not be ignored (Lee et al., 2007). In another study, almost all of 256 suspected COVID-19 patients underwent distress (Cao et al., 2020b), the high rate of distress for suspected cases warrants further investigation. The prevalence of depression and anxiety in students were close to those of the general population, but were higher compared with normal conditions; this may be due to the implementation of distance learning, which reduced the opportunity for socializing (Lewnard and Lo, 2020; Main et al., 2011).
Our results suggest that physicians and nurses experienced significant mental health problems in association with COVID-19, particularly insomnia. As front-line medical personnel, physicians and nurses experienced the fear associated with a novel infectious disease and close contact with infected patients, and had to work under extreme pressure to diagnose, treat, and care for COVID-19 patients; such conditions would put them at high risk of developing mental health problems (Greenberg et al., 2020; Lu et al., 2020a). The non-medical staff in our analysis had the lowest prevalence of mental health problems, except for insomnia, which may be due to not being in direct contact with COVID-19 or other febrile patients. No significant differences in mental health problems between front- and second-line medical personnel were seen; both had a high prevalence of depression and anxiety, which may be due to the stress associated with providing intense treatment, and working toward prevention and control, over long periods (Xiao et al., 2020). Effective interventions should be implemented to safeguard the mental and physical wellbeing of health care workers (Wu et al., 2020a).
4.3. Strengths and limitations
There were several strengths to this study. First, to the best of our knowledge, this is the first systematic review and meta-analysis of four different mental health problems related to COVID-19; moreover, it involved multiple populations, including patients with noninfectious chronic diseases and students. Second, we used a comprehensive search strategy to identify relevant studies, and ultimately analyzed 66 studies, 24 studies from preprint databases. Finally, English and Chinese articles were both included in this meta-analysis. As the first country affected by COVID-19, the population of China was surveyed at an early stage regarding mental health problems. Therefore, Chinese studies should be included in any analysis seeking to comprehensively address this issue.
There were also some limitations to our study. Although we searched for all relevant literature from January 1, 2020 to March 16, 2020, most published studies in the early phase of the global pandemic were conducted for the Chinese population; therefore, additional meta-analyses are needed to obtain more data on the mental health of different populations, during all phases of the pandemic. Also, most research has focused on depression and anxiety; distress and insomnia have not been studied comprehensively, which limited our analyses of these symptoms. Only one study focused on suspected COVID-19 patients, who are vulnerable to mental health problems due to the pressure of being physically unwell and the uncertainty of the outcome; their mental health status merits attention. In addition, as COVID-19 is still a worldwide pandemic, it is not yet possible to assess its long-term impact on mental health. A further limitation was that significant heterogeneity existed among the studies of noninfectious chronic disease patients, which may be due to the use of different measurement tools. Therefore, the results regarding noninfectious chronic disease patients should be interpreted carefully.
5. Conclusions
In conclusion, the worldwide COVID-19 pandemic has imposed a huge mental health burden on society, particularly health care workers, COVID-19 patients and quarantined persons, and noninfectious chronic disease patients; these populations all showed a high risk of mental health problems in this meta-analysis. We recommend that preventative interventions for mental health problems as part of the global response to the pandemic.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
Contributors
Dr. Tianchen Wu designed this study and registered on PROSPERO, searched the online databases and assessed the risk of bias of included studies, carried out the initial statistical analysis, drafted the initial manuscript, reviewed and revised the manuscript. Dr. Xiaoqian Jia designed this study and registered on PROSPERO, drafted the initial manuscript, reviewed and revised the manuscript. Dr. Huifeng Shi searched the online databases, assessed the risk of bias of included studies, reviewed and revised the manuscript. Ms. Jieqiong Niu searched the online databases and evaluated all searched citations and extracted the primary data. Mr. Xiaohan Yin searched the online databases, evaluated all searched citations. Mr. Jialei Xie searched the online databases and extracted the primary data. Prof. Xiaoli Wang designed this study and registered on PROSPERO, reviewed and revised the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
None
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.11.117.
Appendix. Supplementary materials
References
- Addis A., Genazzani A., Trotta M.P., Magrini N. Ann Intern Med; 2020. Promoting Better Clinical Trials and Drug Information as Public Health Interventions for the COVID-19 Emergency in Italy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali I. The COVID-19 Pandemic: Making Sense of Rumor and Fear. Medical anthropology. 2020;39:376–379. doi: 10.1080/01459740.2020.1745481. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. Vol. 395. Lancet; London, England: 2020. pp. e37–e38. (2019-nCoV epidemic: address mental health care to empower society). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaglehole B., Mulder R.T., Frampton C.M., Boden J.M., Newton-Howes G., Bell C.J. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. The British journal of psychiatry: the journal of mental science. 2018;213:716–722. doi: 10.1192/bjp.2018.210. [DOI] [PubMed] [Google Scholar]
- Benbir G., Demir A.U., Aksu M., Ardic S., Firat H., Itil O., Ozgen F., Yılmaz H., Karadeniz D. Prevalence of insomnia and its clinical correlates in a general population in Turkey. Psychiatry and clinical neurosciences. 2015;69:543–552. doi: 10.1111/pcn.12252. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. Vol. 395. Lancet; London, England: 2020. pp. 912–920. (The psychological impact of quarantine and how to reduce it: rapid review of the evidence). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao J., Wei J., Zhu H., Duan Y., Geng W., Hong X., Jiang J., Zhao X., Zhu B. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychotherapy and psychosomatics. 2020;89:252–254. doi: 10.1159/000507453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao X., Wang S., Zhong B., Zhang L., Ungvari G., Ng C., Li L., Chiu H., Lok G., Lu J., Jia F., Xiang Y. The prevalence of insomnia in the general population in China: A meta-analysis. PloS one. 2017;12 doi: 10.1371/journal.pone.0170772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Liu J., Huang S. Analyses of SCL-90 in isolators and non-isolators during SARS period. J Clin Psychosom Dis. 2004;10:29–31. [Google Scholar]
- Chen J., Liu X., Wang D., Jin Y., He M., Ma Y., Zhao X., Song S., Zhang L., Xiang X., Yang L., Bai T., Song J., Hou X. Medical Staffs: A Cross-Sectional Study at the Outbreak of SARS-CoV-2 in China. SSRN.; 2020. Multiple Risk Factors of Depression and Anxiety. [DOI] [Google Scholar]
- Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychological medicine. 2004;34:1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Cui L., Wang X., Wang H. Challenges facing coronavirus disease 2019: Psychiatric services for patients with mental disorders. Psychiatry and clinical neurosciences. 2020;74:371–372. doi: 10.1111/pcn.13003. [DOI] [PubMed] [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Controlled clinical trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes & metabolic syndrome. 2020;14:779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede L.E., Zheng D. Independent factors associated with major depressive disorder in a national sample of individuals with diabetes. Diabetes care. 2003;26:104–111. doi: 10.2337/diacare.26.1.104. [DOI] [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M., Minder C. Clinical research ed. Vol. 315. BMJ; 1997. Bias in meta-analysis detected by a simple; pp. 629–634. (graphical test). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman M.F., Tukey J.W. Transformations related to the angular and the square root. Ann Math Stat. 1950;21:607–611. [Google Scholar]
- González-Sanguino C., Ausín B., ÁngelCastellanos M., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain, behavior, and immunity. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. research Clinical., editor. Managing mental health challenges faced by healthcare workers during covid-19 pandemicBMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- Hall G., Laddu D.R., Phillips S.A., Lavie C.J., Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Progress in cardiovascular diseases. 2020 doi: 10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine. Emerging infectious diseases. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. research Clinical., editor. Measuring inconsistency in meta-analysesBMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong X., Cao J., Wei J., Duan Y., Zhao X., Jing J., Jiang Y., Geng W., Zhu H. The Stress and Psychological Impact of the COVID-19 Outbreak on Medical Workers at the Fever Clinic of a Tertiary General Hospital in Beijing: A Cross-Sectional Study. SSRN. 2020 doi: 10.2139/ssrn.3566244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua Y., Mingli L., Zhixiong L., Weiyi X., Yiwen Y., Yaya L., Zhe L., Zhenzhen X. Coping style, social support and psychological distress in the general Chinese population in the early stages of the COVID-2019 epidemic. SSRN. 2020 doi: 10.2139/ssrn.3551415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X., Ke P. The effect of standardized training on the anxiety of staff in the disinfection supply center during the pandemic of COVID-19 [In Chinese] Chinese General Practice Nursing. 2020;18:548–550. [Google Scholar]
- Huang Y., Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychology, health & medicine. 2020;14:1–12. doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiology and health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin N., Zuo Y., Zhang X., Tang H., Ma X. Psychological Intervention on Anxiety of 138 College Students Quarantined. Chinese Mental Health Journal. 2003;17 598-598. [Google Scholar]
- Johansson R., Carlbring P., Heedman Å., Paxling B., Andersson G. Vol. 1. PeerJ; 2013. Depression, anxiety and their comorbidity. (the Swedish general population: point prevalence and the effect on health-related quality of life). e98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazmi S.S.H. COVID-19 and lockdown: a study on the Impact on mental health. SSRN. 2020 doi: 10.2139/ssrn.3577515. [DOI] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Koretz D., Merikangas K.R., Rush A.J., Walters E.E., Wang P.S. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) Jama. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369,:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong X., Zheng K., Tang M., Kong F., Zhou J., Diao L., Wu S., Jiao P., Su T., Dong Y. Prevalence and Factors Associated with Depression and Anxiety of Hospitalized Patients with COVID-19. medRxiv. 2020 doi: 10.1101/2020.03.24.20043075. [DOI] [Google Scholar]
- Laddu D.R., Lavie C.J., Phillips S.A., Arena R. Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic. Progress in cardiovascular diseases. 2020 doi: 10.1016/j.pcad.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavie C.J., Menezes A.R., De Schutter A., Milani R.V., Blumenthal J.A. Impact of Cardiac Rehabilitation and Exercise Training on Psychological Risk Factors and Subsequent Prognosis in Patients With Cardiovascular Disease. The Canadian journal of cardiology. 2016;32:S365–s373. doi: 10.1016/j.cjca.2016.07.508. [DOI] [PubMed] [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C., Chu C.M., Wong P.C., Tsang K.W., Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Canadian journal of psychiatry. Revue canadienne de psychiatrie. 2007;52:233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Lewnard J.A., Lo N.C. Scientific and ethical basis for social-distancing interventions against COVID-19. The Lancet. Infectious diseases. 2020;20:631–633. doi: 10.1016/S1473-3099(20)30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Zhang C., Luo J., Zhang H., Wu H., Yang B., Zhu Y., Li H., Fan B., Li C. Psychological status among different populations during COVID-19 epidemic: a systematic review and meta-analysis. Journal of Tongji University(Medical Science) 2020;41:147–154. [Google Scholar]
- Liu X., Cheng Y., Wang M., Pan Y., Guo H., Jiang R., Wang Q. Psychological state of nursing staff in a large scale of general hospital during COVID-19 epidemic. Chin J Nosocomiol. 2020;30:1634–1639. [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry research. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y.C., Shu B.C., Chang Y.Y., Lung F.W. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychotherapy and psychosomatics. 2006;75:370–375. doi: 10.1159/000095443. [DOI] [PubMed] [Google Scholar]
- Main A., Zhou Q., Ma Y., Luecken L.J., Liu X. Relations of SARS-related stressors and coping to Chinese college students' psychological adjustment during the 2003 Beijing SARS epidemic. Journal of counseling psychology. 2011;58:410–423. doi: 10.1037/a0023632. [DOI] [PubMed] [Google Scholar]
- Matsuishi K., Kawazoe A., Imai H., Ito A., Mouri K., Kitamura N., Miyake K., Mino K., Isobe M., Takamiya S., Hitokoto H., Mita T. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry and clinical neurosciences. 2012;66:353–360. doi: 10.1111/j.1440-1819.2012.02336.x. [DOI] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian journal of psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., Abidine A., Bokhary M.A., AL-Hadithi H.T., Ali D., Abuthawabeh R., Abdelwahab G.M., Alhartani Y.J., Al Muhaisen H., Dagash A. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. medRxiv. 2020 doi: 10.1101/2020.04.09.20056374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen H.C., Nguyen M.H., Do B.N., Tran C.Q., Nguyen T.T.P., Pham K.M., Pham L.V., Tran K.V., Duong T.T., Tran T.V., Duong T.H., Nguyen T.T., Nguyen Q.H., Hoang T.M., Nguyen K.T., Pham T.T.M., Yang S.H., Chao J.C., Duong T.V. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. Journal of clinical medicine. 2020;9:965. doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M., Wall M., Liu S.M., Morin C.M., Blanco C. Insomnia and Impaired Quality of Life in the United States. J Clin Psychiatry. 2018;79:17m12020. doi: 10.4088/JCP.17m12020. [DOI] [PubMed] [Google Scholar]
- Pulvirenti F., Cinetto F., Milito C., Bonanni L., Pesce A.M., Leodori G., Garzi G., Miglionico M., Tabolli S., Quinti I. Health-Related-Quality of Life in Common Variable Immunodeficiency Italian patients switched to remote assistance during the COVID-19 pandemic. The journal of allergy and clinical immunology. In practice. 2020;8:1894–1899. doi: 10.1016/j.jaip.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian M., Wu Q., Wu P., Hou Z., Liang Y., Cowling B.J., Yu H. China: a population based cross-sectional survey. medRxiv.; 2020. Psychological responses, behavioral changes and public perceptions during the early phase of the COVID-19 outbreak. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., Zandi M.S., Lewis G., David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. The lancet. Psychiatry. 2020;7:611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu J.Y. The SARS-associated stigma of SARS victims in the post-SARS era of Hong Kong. Qualitative health research. 2008;18:729–738. doi: 10.1177/1049732308318372. [DOI] [PubMed] [Google Scholar]
- Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L., Zhang K., Chin H.K., Ahmad A., Khan F.A., Shanmugam G.N., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Ho C.S., Ho R.C., Sharma V.K. Ann Intern Med; 2020. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of affective disorders. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations, 2020. UN leads call to protect most vulnerable from mental health crisis during and after COVID-19.
- von Elm, E. Altman, D.G. Egger, M. Pocock, S.J. Gøtzsche, P.C. Vandenbroucke. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- Walker R.J., Campbell J.A., Dawson A.Z., Egede L.E. Prevalence of psychological distress, depression and suicidal ideation in an indigenous population in Panamá. Social psychiatry and psychiatric epidemiology. 2019;54:1199–1207. doi: 10.1007/s00127-019-01719-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Wang S., Zong Q.Q., Zhang Q., Ng C.H., Ungvari G.S., Xiang Y.T. Prevalence of comorbid major depressive disorder in Type 2 diabetes: a meta-analysis of comparative and epidemiological studies. Diabetic medicine: a journal of the British Diabetic Association. 2019;36:961–969. doi: 10.1111/dme.14042. [DOI] [PubMed] [Google Scholar]
- Wing Y.K., Leung C.M. Mental health impact of severe acute respiratory syndrome: a prospective study. Hong Kong medical journal. 2012;3:24–27. 18 Suppl. [PubMed] [Google Scholar]
- World Health Organization, 2020a. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV).
- World Health Organization, 2020b. WHO Coronavirus Disease (COVID-19) Dashboard.
- World Health Organization, 2020c. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020.
- Wu J., Rong X., Chen F., Diao Y., Chen D., Jing X., Gong X. Investigation on sleep quality of first⁃line nurses in fighting against corona virus disease 2019 and its influencing factors. Chinese Nursing Research. 2020;34:558–562. [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The lancet. Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao C., Wang L., Liu J., Shen X., Li B., Zhang S., Huang G. Anxiety and depression status among non-first-line medical staff during the outbreak of COVID-19. Sichuan Mental Health. 2020;33:15–18. [Google Scholar]
- Yan R., Xia J., Yang R., Lv B., Wu P., Chen W., Zhang Y., Lu X., Che B., Wang J., Yu J. Association between anxiety, depression, and comorbid chronic diseases among cancer survivors. Psycho-oncology. 2019;28:1269–1277. doi: 10.1002/pon.5078. [DOI] [PubMed] [Google Scholar]
- Yang Y., Zhong L., Peng L. Mental health of tumor patients during the pandemic of COVID-19 [In Chinese] Chinese General Practice Nursing. 2020;18:691–693. [Google Scholar]
- Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Su M., Zhang J., Liu Z., Zhang B. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Frontiers in psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain, behavior, and immunity. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ma Z.F. Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. International journal of environmental research and public health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A Novel Coronavirus from Patients with Pneumonia in China. The New England journal of medicine. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.