Abstract
Background
Adults with congenital heart disease (CHD) are living longer with more complex disease. Maintaining lifelong care prevents morbidity and mortality, but many patients remain lost to follow-up or experience care gaps. We sought to assess barriers to care for patients with adult CHD (ACHD) in Saskatchewan, a Canadian province with no local congenital cardiac surgical support and no clear framework for ACHD care.
Methods
We performed a telephone survey of patients with CHD transferred from pediatric to adult cardiology from 2007 to 2014. Our primary outcome was loss to follow-up > 2 years from last recommended cardiology appointment and/or multiple missed cardiology appointments. Secondary outcomes were guideline-based care (specialist training, adherence to appropriate endocarditis prophylaxis, pre-pregnancy counselling for women), presence or absence of previously described barriers to care in ACHD, and health care autonomy using the Krantz Health Opinion Survey.
Results
We interviewed 32 patients (30% response rate). One-quarter met the primary outcome: lost to follow-up > 2 years from last recommended cardiology appointment and/or self-report of missed cardiology appointments. Only 69% of young adults in Saskatchewan were receiving guideline-based care for their CHD (appropriate level of specialist expertise and frequency of follow-up). Only 72% of patients were adhering to endocarditis prophylaxis recommendations and 61% of women surveyed received counselling regarding pregnancy. Patients indicated a low preference for participating in decision making regarding their care on the Krantz Health Opinion Survey.
Conclusions
With our survey, we have created a novel snapshot of CHD care in Saskatchewan and have identified significant deficits.
Résumé
Contexte
Les adultes souffrant d’une cardiopathie congénitale vivent de plus en plus longtemps avec une maladie complexe. Les soins qui leur sont prodigués toute leur vie aident à prévenir la morbidité et la mortalité, mais nombreux sont les patients qui sont perdus de vue en cours de route ou qui vivent des périodes sans recevoir de soins. Nous avons tenté d’évaluer les obstacles aux soins des patients adultes atteints d’une cardiopathie congénitale en Saskatchewan, une province canadienne où il n’existe aucun programme local de soutien en matière de chirurgie cardiaque pour les troubles congénitaux ni de cadre définissant clairement les soins à prodiguer aux adultes atteints d’une cardiopathie congénitale.
Méthodologie
Nous avons interviewé par téléphone des patients atteints d’une cardiopathie congénitale qui sont passés d’un suivi en cardiologie en soins pédiatriques aux soins aux adultes entre 2007 et 2014. Le critère d’évaluation principal était la perte de vue pendant plus de 2 ans après le dernier rendez-vous de suivi en cardiologie recommandé et/ou plusieurs rendez-vous en cardiologie manqués. Les critères d’évaluation secondaires étaient les soins recommandés dans les lignes directrices (formation spécialisée, observance d’une prophylaxie endocardite appropriée, counseling préalable à la grossesse chez les femmes), la présence ou l’absence d’obstacles aux soins relatifs à la cardiopathie congénitale chez l’adulte cités antérieurement et l’autonomie en matière de soins de santé selon le sondage d’opinion sur la santé de Krantz.
Résultats
Nous avons interviewé 32 patients (taux de réponse de 30 %). Le quart des patients interrogés répondaient au critère d’évaluation principal, soit la perte de vue pendant plus de 2 ans après le dernier rendez-vous de suivi en cardiologie recommandé et/ou plusieurs rendez-vous en cardiologie manqués autodéclarés. Seulement 69 % des jeunes patients adultes de la Saskatchewan recevaient les soins recommandés dans les lignes directrices en matière de cardiopathie congénitale (degré approprié d’expertise spécialisée du médecin et fréquence des consultations de suivi). Seulement 72 % des patients observaient les recommandations en matière de prophylaxie endocardite, et 61 % des femmes interrogées avaient reçu des services de counseling concernant la grossesse. Selon les résultats au sondage d’opinion sur la santé de Krantz, les patients étaient généralement peu disposés à participer aux décisions concernant leur programme de soins.
Conclusions
Grâce à notre enquête, nous disposons maintenant d’un portrait à jour des soins aux patients atteints de cardiopathie congénitale en Saskatchewan; l’exercice nous a par ailleurs permis de cerner d’importantes lacunes à cet égard.
Adults with congenital heart disease (CHD) who maintain lifelong cardiology follow-up with specialized health care providers live longer.1,2 They have fewer hospitalizations, reduced emergency procedures, and lower morbidity and mortality from their underlying disease.3, 4, 5 Despite knowledge that specialized, lifelong care provides significantly improved outcomes, many adults with CHD are lost to follow-up.4,6 The etiology of this care gap is multifactorial; a mistaken impression of “being cured,” denial of illness impact, a lack of qualified CHD providers, and failure of transition from pediatric to adult care paradigms have all been implicated.7,8
More recently, recognition of neurocognitive dysfunction in young adults with CHD has begun to shift the thought process around transition of care.9 We now know that executive dysfunction in these patients results in deficits in planning, problem solving, and strategizing, all of which make managing chronic disease independently within the health care system a daunting challenge.10,11 Focus has shifted away from education regarding anatomy and disease-specific factors and toward fostering self-care and health care autonomy.12,13
Several studies have evaluated the problem and identified risk factors for loss to follow-up, but they have all been conducted in large tertiary care centres with established, multidisciplinary pediatric and adult CHD (ACHD) programs.6,7 We sought to evaluate a population that has not yet been assessed: young adults with CHD in the province of Saskatchewan. There is no formal mechanism for transition of care from pediatric to adult providers in the province, aside from a paper referral once children reach adulthood. As Saskatchewan has low population density compared with the rest of Canada (1.8 persons per square kilometre vs 3.7 persons per square kilometre), patients must often travel long distances to obtain care and many adults are cared for by general cardiologists with no specialized training in CHD.14 All surgical care occurs in Alberta, a province away at a distance of at least 250 km. We performed a telephone survey to evaluate established barriers to lifelong care, health care utilization, and health care autonomy among young adults with CHD in Saskatchewan.
Methods
This was a retrospective study using a telephone survey (Supplemental Appendix S1) and a chart review (Supplemental Appendix S2) that was approved by the research ethics board at the University of Saskatchewan. All patients with structural heart disease who were transferred from their pediatric cardiologist at the University of Saskatchewan to an adult cardiologist within a 7-year period (2007-2014) were contacted for possible inclusion. They must have had at least 1 visit to pediatric cardiology between the ages of 13 and 17, indicating that their heart disease was not cured in childhood. We excluded patients who had died, those with Wolff-Parkinson-White syndrome and morphologically normal hearts, isolated cardiomyopathy, or pulmonary hypertension without structural heart disease. We also excluded patients who received a heart transplant in childhood as their follow-up care needs are more complex than the average patient with CHD.
Patients were identified as meeting the inclusion criteria from the pediatric cardiology database at the University of Saskatchewan, Royal University Hospital. Telephone surveys were all conducted by MK who has a journalism degree and experience conducting telephone interviews. Potential participants were contacted using the last telephone contact information on the pediatric chart. As this was often outdated, if we ended up speaking to the participant’s parents, we informed them of the study and asked them either to have their child contact the study team or provide up-to-date contact information. If the call went to voicemail, 2 messages were left at an interval of several weeks inviting the potential participant to call the study team and schedule an interview.
The telephone survey was piloted by inviting adult congenital heart patients not meeting inclusion criteria (transitioned before 1999 and/or not cared for in Saskatchewan) and content experts not involved in the study team to participate. They were asked to provide feedback on the format and questions, and it was modified accordingly. The primary outcome was lost to follow-up > 2 years or self-reported multiple (at least 2) missed cardiology appointments. Secondary outcomes included whether or not the patients were receiving appropriate guideline-based follow-up as defined by the 2008 ACC ACHD Guidelines15 and description of possible barriers to care. To determine whether or not patients were receiving guideline-based care, we first determined their lesion severity. We then determined the level and frequency of specialist care required based on their lesion severity. If a patient was not receiving the appropriate level of specialist care and/or the appropriate frequency of care, we coded them as “not receiving Guideline-based care” (Supplemental Appendix S2). There is only 1 ACHD-trained cardiologist in Saskatchewan. In addition, whether or not patients were adhering to endocarditis prophylaxis guidelines and whether or not women received recommended pre-pregnancy counselling were assessed separately as surrogate markers of appropriate care. We also performed the Krantz Health Opinion Survey (HOS), a validated survey measure of preferences for different treatment approaches.16
Quantitative data were analyzed using SPSS (Version 25; IBM Corp., Armonk, NY). To determine sociodemographic, clinical, and patient factors associated with a lack of appropriate follow-up, multiple logistic regression was attempted using a backward stepwise method. Ultimately, our sample size prohibited completing a full logistic regression model, so only results of the initial bivariate analysis are presented (χ2, Student’s t-test as appropriate). Results were reported as odds ratios with 95% confidence intervals. A bivariate analysis P-value of 0.20 was used to identify variables that may predict the outcome of interest in larger models. Qualitative data were analyzed via thematic analysis.
Results
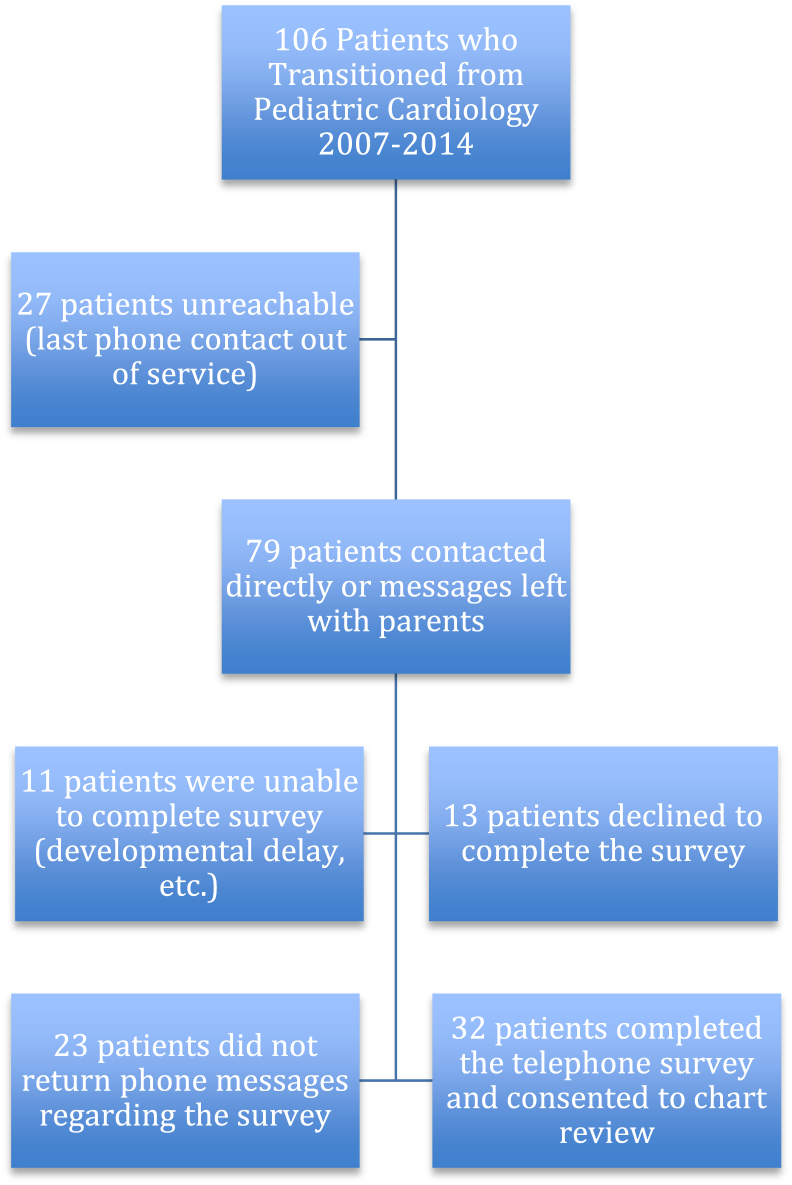
We identified 106 young adults who should have transferred to adult care between 2007 and 2014 (Fig. 1). Telephone contact with all 106 potential participants was attempted. Eleven patients were unable to complete the telephone survey; 2 were deceased, 1 was unwell and admitted to hospital, 7 were unable to complete the survey according to their parents as they had significant learning disabilities or were nonverbal, and 1 patient had a hearing impairment that precluded the performance of a telephone survey. In the case of 23 potential participants, telephone messages were left with either the patients or their parents regarding the survey but messages were never returned. Ultimately, 32 patients (30% response rate) consented to participate and completed the telephone survey.
Figure 1.
Potential participants and survey response rate.
Primary outcome: health care utilization
Six patients (19%) reported missing clinic appointments with their cardiologist. Reasons cited for missing scheduled cardiology appointments included unstable housing leading to missed appointment letters, difficulty scheduling clinic visits with busy cardiology practitioners, and poor weather making driving long distances to clinic appointments difficult. One female patient cited significant anxiety about long-term cardiac health as a reason for many missed or rescheduled cardiology appointments. Overall, 3 patients (9%) were lost to follow-up from cardiology for more than 2 years at the time of the survey and 8 patients (25%) met the primary outcome (Table 1). All 3 lost patients were male. One patient had Williams syndrome and developmental delay and was unsure why he had not seen his cardiologist in some time. The other 2 reported that they had not been contacted by their cardiologist for an appointment and had not followed up. One of the patients with Ebstein’s anomaly characterized his understanding as such:
“I thought they would contact me and, since they didn’t, I figured I was fine and dandy … good to go!”
Table 1.
Population characteristics of patient with CHD surveyed stratified by primary outcome
| Participants lost to follow-up > 2 years and/or multiple missed cardiology appointments (cases, n = 8) | Participants with continuous cardiology follow-up (controls, n = 24) | |
|---|---|---|
| Age (mean ± SE) | 23.0 ± 0.8 | 21.5 ± 0.4 |
| Male sex, n (%) | 4 (50) | 15 (63) |
| Transition distance (km), mean ± SE | 38.6 ± 25.2 | 70.0 ± 18.9 |
| Self-identified race/ethnicity, n (%) | ||
| Caucasian | 6 (75) | 20 (83) |
| Aboriginal | 2 (25) | 1 (4) |
| Other | 0 (0) | 3 (13) |
| Presence of disability, n (%) | 1 (13) | 5 (21) |
| Highest education level achieved, n (%) | ||
| Advanced degree | 1 (13) | 0 (0) |
| College/university degree | 3 (38) | 7 (29) |
| Some college/university | 1 (13) | 9 (38) |
| Completed high school | 3 (38) | 7 (29) |
| Less than high school | 0 (0) | 1 (4) |
| Family income (CAD$), n (%) | ||
| > 100,000 | 1 (13) | 7 (29) |
| 50-100,000 | 3 (38) | 12 (50) |
| 25-50,000 | 1 (13) | 3 (13) |
| < 25,000 | 1 (13) | 1 (4) |
| ACHD lesion complexity, n (%) | ||
| Simple | 2 (25) | 8 (33) |
| Moderate | 4 (50) | 9 (38) |
| Great | 2 (25) | 4 (17) |
| Great+ | 0 (0) | 3 (13) |
| Number of cardiac surgeries, mean ± SE | 1.75 ± 0.7 | 1.5 ± 0.2 |
| Taking cardiac medications, n (%) | 3 (38) | 15 (63) |
| Low perceived social support, n (%) | 1 (12.5) | 0 (0) |
| Krantz Health Opinion Survey Score, n (%) | ||
| Low | 5 (63) | 21 (88) |
| Medium | 3 (38) | 3 (13) |
| High | 0 (0) | 0 (0) |
| Meets criteria for major depressive disorder, n (%) | 1 (13) | 1 (4) |
| Cared for by an ACHD-trained cardiologist, n (%) | 2 (25) | 10 (42) |
ACHD, adult congenital heart disease; CHD, congenital heart disease; SE, standard error.
A logistic regression model was attempted to determine variables that were associated with the outcome of interest. The outcome of interest was a dichotomous variable defined as loss to cardiology follow-up for more than 2 years and/or missed clinical appointments.
Bivariate analysis results for each of the 14 potential risk factors possibly predicting the primary outcome of interest (lost to cardiology follow-up for > 2 years and/or missed cardiology appointments) are provided in Table 2. The only variables that were potentially predictive of the primary outcome were age at survey, self-identification as Aboriginal, taking cardiac medications, and medium Krantz HOS. Because of low sample size, a multivariate analysis could not be validly performed. Therefore, we can only suggest that variables identified via bivariate analysis may have some correlation with the primary outcome of interest.
Table 2.
Bivariate analysis results for each of the 14 potential risk factors
| Variable | Odds ratio | 95% CI of OR | P value |
|---|---|---|---|
| Age | 1.44 | (0.93, 2.23) | 0.10 |
| Sex | 0.60 | (0.12, 3.01) | 0.53 |
| Race | 0.35 | ||
| Aboriginal | 6.67 | (0.51, 86.93) | 0.15 |
| Other | 0.0 | (0, …) | 0.10 |
| Transition distance | 1.00 | (0.98, 1.01) | 0.39 |
| Education level (no college/university) | 0.83 | (0.158, 4.401) | 0.830 |
| Family income < CAD$25,000 | 3.50 | (0.15, 84.69) | 0.44 |
| Simple lesion complexity | 0.38 | (0.04, 4.00) | 0.42 |
| Disability | 0.54 | (0.05, 5.50) | 0.60 |
| Number of cardiac surgeries | 1.13 | (0.62, 2.06) | 0.70 |
| Taking cardiac medications | 0.36 | (0.07, 1.88) | 0.22 |
| Low perceived social support | Indeterminate | Indeterminate | Indeterminate |
| Krantz Health Opinion Score (medium with low as reference category) | 4.20 | (0.65, 27.36) | 0.13 |
| Major depressive disorder | 3.29 | (0.18, 59.60) | 0.40 |
| Cared for by a CHD cardiologist | 2.14 | (0.36, 12.89) | 0.40 |
CHD, congenital heart disease; CI, confidence interval; OR, odds ratio.
Almost all of the respondents, with the exception of 2, had regular follow-ups with their family physician (n = 30, 94%). All of the respondents, with the exception of one, were under the care of a cardiologist. Only 12 patients (38%) were under the care of a cardiologist with specialized training in ACHD. Of the 22 patients with moderate-to-severe complexity of their CHD, less than one-third (n = 7, 32%) were appropriately under the care of an ACHD specialized cardiologist. The remainder (n = 15, 68%) were being cared for by general cardiologists. Overall, only 69% (n = 22) of respondents were receiving appropriate guideline-based follow-up for their ACHD (Table 3).15
Table 3.
Secondary outcomes (guideline-derived measures of appropriate ACHD care)
| Yes, n (%) | No, n (%) | |
|---|---|---|
| Appropriate level of specialist care for disease severity | 22 (69) | 10 (31) |
| Adherence to endocarditis prophylaxis guidelines | 23 (72) | 9 (28) |
| Appropriate pre-pregnancy counselling (women respondents only) | 8 (61) | 5 (38) |
ACHD, adult congenital heart disease.
Surrogate markers of appropriate care (pregnancy counselling, endocarditis prophylaxis) were also assessed. Of the women who had been pregnant, all 3 reported having a discussion with their cardiologist before pregnancy delineating the cardiac risks. Of the women who had not been pregnant (n = 10), only 50% reported that their cardiologist had initiated a conversation about possible future pregnancy and the risks. Of the patients who were taking at least 1 cardiac medication, only slightly more than half (n = 11, 61%) knew why they were taking the medication or its physiological purpose. Only 72% (n = 23) of patients were appropriately adhering to endocarditis prophylaxis guidelines based on their anatomy (taking antibiotics before dental procedures if recommended) (Table 3).
Demographics of respondents
The majority of respondents were male (n = 19, 59%). All of the participants were born between 1990 and 1997, and the average age of the respondents at the time of the survey was 22 ± 2 years. All but one of the participants, who immigrated to Canada from the Philippines at age 14, were born in Canada and their first language was English. None of the participants reported asking for an interpreter during medical appointments as they were all comfortable communicating with health care practitioners in English. Most of the respondents self-identified as Caucasian (n = 26, 81%), whereas 3 identified as Aboriginal (9%), 2 identified as South Asian (6%), and 1 identified as black (3%).
The majority of respondents (n = 27, 84%) reported having no disabilities (learning, physical, visual, or hearing). Four identified as having learning disabilities and only 1 reported a physical disability (residual arm weakness due to a pediatric stroke). All respondents had completed high school with the exception of one who was finishing his last year at the time of the survey. Two respondents disclosed that they graduated from a modified educational program due to their learning disabilities. Ten respondents (31%) had completed university or college degrees and 1 reported achieving an advanced degree. Six (19%) were currently attending college or university in pursuit of a degree.
Only 4 respondents (13%) were neither employed nor full-time students. Approximately one-third (n = 11, 34%) were working full time for pay. The remainder were either working part time for pay (n = 12, 38%) or identified as full-time students (n = 5, 16%). Many of the young adults surveyed performed manual labour (heavy equipment operation, waste disposal, etc.). Several (n = 4, 13%) worked in family businesses that they identified as providing flexibility and medical leave as required. Very few participants (n = 4, 13%) reported ever being unemployed because of their CHD with 3 saying they could not sustain employment due to medical appointments and surgeries. One respondent cited his learning disability and overall health status as the reasons for his unemployment.
As a marker of socioeconomic status, we queried the respondents regarding food insecurity. In response to the question “How often in the past year was the following statement true? The food that you and other household members bought just didn’t last and there wasn’t any money to buy more,” only 3 respondents (9%) signalled food insecurity by answering that the statement was “sometimes true.” Many of the young adults surveyed reported living in a home owned by their parents (n = 17, 53%). Three respondents lived in homes they had purchased and the remainder (n = 12, 38%) were renting. The median reported family income was between 50,000 and 100,000 Canadian dollars per year and that supported an average of 3.0 ± 1.7 household members. As a measure of travel distance from home to a tertiary cardiac centre, we collected postal codes from the pediatric charts of all respondents. About half of the respondents lived in major cities in Saskatchewan (n = 17, 53%), whereas the rest grew up in rural communities (n = 15, 47%). The mean distance from pediatric address to the adult cardiologist to whom the patient was transitioned was 62.1 ± 87.6 km.
The distribution of anatomic lesions present in survey respondents is presented in Table 4. Sixty-nine per cent of participants (n = 22) had CHD of moderate-severe complexity, whereas the remainder (n = 10, 31%) had simple CHD. The mean number of open cardiosurgical procedures was 1.6 ± 1.3 per patient. More than half of the respondents (n = 18, 56%) were taking at least 1 medication daily for their heart disease.
Table 4.
Congenital heart disease lesions of respondents
| Lesion | Number of respondents (%) (n = 32) |
|---|---|
| Bicuspid aortic valve | 8 (25) |
| Pulmonary stenosis | 3 (9) |
| Mitral valve dysfunction | 3 (9) |
| Ventricular septal defect | 1 (3) |
| Subaortic stenosis | 1 (3) |
| Coarctation of the aorta | 4 (13) |
| Atrioventricular septal defect | 1 (3) |
| Ebstein’s anomaly | 1 (3) |
| Tetralogy of Fallot | 3 (9) |
| Transposition of the great arteries | 4 (13) |
| Functional single ventricle with Fontan circulation | 3 (9) |
Health care autonomy
All 32 participants agreed to complete the Krantz HOS.16 Seventy-five per cent of participants (n = 24) received a low overall score on the Krantz HOS survey (6 or less). The remainder (n = 8, 25%) received a medium score. None of the patients surveyed received a high score suggestive of health care autonomy. When stratified based on preferences for receipt of medical information and self-care behaviours (Table 5), more participants (n = 17, 53%) indicated a preference for receiving information about their health than those who wanted to be actively involved in decision making about their health (n = 10, 31%).
Table 5.
Krantz HOS in young adults with CHD
| Krantz HOS | Number of respondents (%) (n = 32) |
|---|---|
| Information score | |
| Low (2 or less) | 15 (47) |
| Medium (3-5) | 14 (44) |
| High (6-7) | 3 (9) |
| Behaviour score | |
| Low | 22 (69) |
| Medium | 7 (22) |
| High | 3 (9) |
Note: A low score on the Krantz HOS Information score (2 or less) indicates a preference to not receive detailed information about health and a predilection to not ask questions of health care practitioners. A low score on the Krantz HOS Behaviour score (2 or less) indicates a preference to leave health care decisions to medical practitioners and not participate in care decisions.
CHD, congenital heart disease; HOS, Health Opinion Score.
When asked to agree or disagree with the following statement: “I’d rather have doctors or nurses make the decisions about what’s best than for them to give me a whole lot of choices,” 60% (n = 19) agreed. Eighty-one per cent (n = 26) agreed with the following statement: “recovery is usually quicker under the care of a doctor or nurse than when patients take care of themselves.” An even higher proportion (88%, n = 28) agreed with the following: “if it costs the same, I’d rather have a doctor or nurse give me treatments than to do the same treatments myself.”
Qualitative assessment of ACHD care
At the conclusion of the telephone survey, participants were invited to provide comments they thought would be useful for improving the care for adolescents with CHD.
Seven respondents (22%) noted that they feel rushed during appointments with their adult cardiologist and that pediatric providers had more time for detailed explanation and relationship building. One young woman noted that she feels out of place in her adult cardiologists’ office because “everyone else is 80 plus (years old) in the clinic.” She wished that she could see a dedicated ACHD cardiologist as she would like to be in a clinic with “a younger clientele.” Another young woman said she feels like “just a number in the system” in adult care as opposed to pediatric cardiology where she had a more congenial relationship with her providers. One man felt that his adult cardiologist was too busy and that his administrative staff was overwhelmed. He related an episode where his adult cardiologists’ office failed to schedule a planned follow-up appointment; “we had to phone and follow-up. I would have got lost if it wasn’t for my Mom.” Another young man attributed his ongoing follow-up to his own persistence; “I feel like I’ve gotten lost.”
Discussion
This is the first comprehensive study of young adults with CHD in a Canadian province without a robust framework for ACHD care. We found that many patients were not receiving guideline-based care, defined as a lack of specialized care by ACHD-trained practitioners. This clearly highlights the need to train more cardiologists in the care of moderate-to-complex CHD to serve this growing patient population.
Ours is also the first study to assess Krantz HOS scores in young adults with CHD. Instead of assessing self-care behaviours and autonomy, this score is validated to assess patient preferences in receiving health care. Interestingly, young adults with CHD exhibit a preference to not obtain knowledge about their disease and to leave decisions to health care providers instead of being active participants in their own care.
It has been suggested that higher degrees of health care autonomy correlate with successful long-term cardiology follow-up.17 Despite that, our data surprisingly suggest that young adults with CHD have little interest in taking control of their own health care and that they want physicians to make decisions on their behalf. Previous literature has demonstrated that young adults with CHD have low levels of knowledge about their CHD.18,19 Our research suggests that this may be purposeful and not a result of a negligent lack of education by pediatric providers.
Contemporary transition programs focusing on disease education and fostering self-care behaviours have shown some early success.12 In the long term, this may be hampered by desires of patients with ACHD to remain passive in their health care journey. Parents of adolescents with CHD have told providers that their children are not mature enough to manage their own health care.20 As ACHD providers, should we respect this preference away from self-management and provide more paternalistic care than is usually acceptable in adult care?
As the mortality of patients with CHD shifts out of childhood and into adulthood, complex decision making also shifts from the shoulders of parents to the patients themselves.21 Patients with ACHD often must make high-stakes decisions regarding repeat surgeries, cardiac transplant, and palliative care.22 In an era of shared decision making and informed consent, managing involvement of patients with ACHD in high-risk decisions becomes a quandary. The results of our study suggest that patient preferences vary and that many patients with ACHD would prefer physicians make decisions on their behalf. Before any discussions regarding intervention, an attempt should be made to evaluate the individual patient’s readiness and willingness to participate in such a conversation.
In addition, many patients with ACHD have medical post-traumatic stress disorder or anxiety and can relate traumatic childhood medical experiences with little prompting.23,24 This combination of an external locus of control, a preference away from receiving medical information regarding their own health, and trauma highlights the importance of multidisciplinary care for patients with ACHD. Cardiologists receive little training on how to navigate the mental health needs of their patients, and our research highlights the importance of involving psychologists and social workers in long-term ACHD care. Our primary outcome (loss to follow-up and/or multiple missed cardiologist appointments) is dependent on both health system factors and patient nonadherence. Both of these factors need to be addressed in ACHD care paradigms to ensure adequate long-term follow-up care.
Our study also highlights the difficulty in tracking patients as they transition from pediatric to adult care paradigms. A major limitation of this study was our participation rate and low sample size as we were unable to contact many young adults who met inclusion criteria. Marelli et al.25 used population-level data to show that approximately 20% of adults living with CHD have severe disease. Of our respondents, 28% had CHD of great complexity, indicating that our sample skewed toward patients with more significant disease. This, therefore, resulted in a selection bias, and our results cannot be generalized to the entire ACHD population in Saskatchewan.
Although the pediatric cardiology program in Saskatoon has an internal electronic database, once patients are transitioned to adult care, their electronic health information does not travel with them. A paper referral is sent to the adult cardiologist, and the onus is on his or her office to book the first appointment. Often, each hospital or clinic has its own internal database that does not easily communicate with others, making movement of patient information between facilities and health regions almost impossible. Also, as many patients were transitioned to general cardiologists in private offices, a major limitation of our study was our inability to assess measures to bring young adults back into care. We cannot, therefore, accurately attribute the loss to follow-up of patients with ACHD to either their adult cardiologist or to the patients themselves.
Also, the transfer from pediatric to adult care occurs at a period of general transition in the adolescent life cycle. Patients often move for work or to pursue higher education. In the cases of several patients we were ultimately able to contact, we were provided with accurate contact information by their parents. This suggests that those children with less stable social circumstances (parents who move frequently) were more difficult to contact and our sample is, therefore, skewed toward young adults with stable home lives during childhood. Another complicating factor is the changing landscape of communication. For more than one quarter of potential participants, we were unable to make phone contact as their land lines were out of service. This highlights the difficulty of communicating with young patients by traditional methods (letter mail and/or telephone). Research has shown that more primary care physicians are communicating with patients via text messaging and e-mail.26 Our study highlights the urgent need for health systems to address the current technology gap between modern communication and methods for privacy protection, especially when dealing with young adults.
Although we were able to establish that young adults with CHD exhibit passive preferences for receiving information about their health and would rather not participate in decisions about their care, the etiology of these preferences was not explored. Future research exploring these preferences is warranted. Does heavy contact with the health care system as children make young adults dependent on care providers? Can interventions targeted at enhancing health care autonomy change these preferences? Do these preferences affect complex decision making?
In conclusion, we have established that young adults with CHD are not always receiving guideline-based care. Young patients with ACHD also exhibit passive preferences toward health information and decision making. These factors could combine to create a high risk of morbidity and mortality for young adults with CHD. This study highlights the need for complete data regarding the care of patients with ACHD in Saskatchewan and Canada as a whole. This could be achieved by creating a clear framework for ACHD care in the province and a prospective registry.
Funding Sources
No funding was received for this study.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: The research presented was approved by and adhered to the standards of the Ethical Review Board of the University of Saskatchewan.
See page 445 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2020.05.008.
Supplementary Material
References
- 1.Mylotte D., Pilote L., Ionescu-Ittu R. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation. 2014;129:1804–1812. doi: 10.1161/CIRCULATIONAHA.113.005817. [DOI] [PubMed] [Google Scholar]
- 2.Kempny A., Diller G.H., Dimopoulos K. Determinants of outpatient clinic attendance amongst adults with congenital heart disease and outcome. Int J Cardiol. 2016;203:245–250. doi: 10.1016/j.ijcard.2015.10.081. [DOI] [PubMed] [Google Scholar]
- 3.Yeung E., Kay J., Roosevelt G.E., Brandon M., Yetman A.T. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol. 2008;125:62–65. doi: 10.1016/j.ijcard.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 4.Wray J., Frigiola A., Bull C. Loss to specialist follow-up in congenital heart disease; out of sight, out of mind. Heart. 2013;99:485–490. doi: 10.1136/heartjnl-2012-302831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Bono J., Freeman L.J. Aortic coarctation repair—lost and found: the role of local long term specialized care. Int J Cardiol. 2005;104:176–183. doi: 10.1016/j.ijcard.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Reid G., Irvine M., McCrindle B. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113(Pt 1):e197–205. doi: 10.1542/peds.113.3.e197. [DOI] [PubMed] [Google Scholar]
- 7.Goossens E., Stephani I., Hilderson D. Transfer of adolescents with congenital heart disease from pediatric cardiology to adult heath care. J Am Coll Cardiol. 2011;57:2368–2374. doi: 10.1016/j.jacc.2010.11.068. [DOI] [PubMed] [Google Scholar]
- 8.Hilderson D., Saidi A.W., Ven Deyk K. Attitude toward and current practice of transfer and transition of adolescents with congenital heart disease in the United States of America and Europe. Pediatr Cardiol. 2009;30:786–793. doi: 10.1007/s00246-009-9442-1. [DOI] [PubMed] [Google Scholar]
- 9.Keir M., Ebert P., Kovacs A.H. Neurocognition in adult congenital heart disease: how to monitor and prevent progressive decline. Can J Cardiol. 2019;35:1675–1685. doi: 10.1016/j.cjca.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 10.Tyagi M., Austin K., Stygall J. What do we know about cognitive functioning in adult congenital heart disease? Cardiol Young. 2014;24:13–19. doi: 10.1017/S1047951113000747. [DOI] [PubMed] [Google Scholar]
- 11.Daliento L., Mapelli D., Russo G. Health related quality of life in adults with repaired tetralogy of Fallot: psychosocial and cognitive outcomes. Heart. 2005;91:213–218. doi: 10.1136/hrt.2003.029280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mackie A.S., Rempel G.R., Kovacs A.H. Transition intervention for adolescents with congenital heart disease. J Am Coll Cardiol. 2018;71:1768–1777. doi: 10.1016/j.jacc.2018.02.043. [DOI] [PubMed] [Google Scholar]
- 13.Saarijarvi M., Wallin L., Moons P., Gyllensten H., Bratt E.L. Transition program for adolescents with congenital heart disease in transition to adulthood: protocol for a mixed-method process evaluation study (the STEPSTONES project) BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-028229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Statistics Canada. https://www12.statcan.gc.ca/census-recensement/2011/as-sa/fogs-spg/Facts-pr-eng.cfm?Lang=Eng&GK=PR&GC=47 Available at: Accesed October 2, 2018.
- 15.Warnes C.A., Williams R.G., Bashore T.M. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease): developed in collaboration with the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society Of Thoracic Surgeons. Circulation. 2008;118:714–833. [Google Scholar]
- 16.Krantz D.S., Baum A., Wideman M.V. Assessment of preferences for self-treatment and information in health care. J Pers Soc Psychol. 1980;39:977–990. doi: 10.1037//0022-3514.39.5.977. [DOI] [PubMed] [Google Scholar]
- 17.Mackie A.S., Rempel G.R., Islam S. Psychosocial maturity, autonomy, and transition readiness among young adults with congenital heart disease or a heart transplant. Congenit Heart Dis. 2016;11:136–143. doi: 10.1111/chd.12300. [DOI] [PubMed] [Google Scholar]
- 18.Heery E., Sheehan A.M., While A.E., Coyne I. Experiences and outcomes of transition from pediatric to adult health care services for young people with congenital heart disease: a systematic review. Congenit Heart Dis. 2015;10:413–427. doi: 10.1111/chd.12251. [DOI] [PubMed] [Google Scholar]
- 19.Van Deyk K., Pelgrims E., Troost E. Adolescents’ understanding of their congenital heart disease on transfer to adult-focused care. Am J Cardiol. 2010;106:1803–1807. doi: 10.1016/j.amjcard.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 20.Clarizia N.A., Chahal N., Manlhiot C. Transition to adult health care for adolescents and young adults with congenital heart disease: perspectives of the patient, parent and health care provider. Can J Cardiol. 2009;25:e317–e322. doi: 10.1016/s0828-282x(09)70145-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khairy P., Ionescu-Ittu R., Mackie A.S. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56:1149–1157. doi: 10.1016/j.jacc.2010.03.085. [DOI] [PubMed] [Google Scholar]
- 22.Van De Bruaene A., Hickey E.J., Kovacs A.H. Phenotype, management and predictors of outcome in a large cohort of adult congenital heart disease patients with heart failure. Int J Cardiol. 2018;252:80–87. doi: 10.1016/j.ijcard.2017.10.086. [DOI] [PubMed] [Google Scholar]
- 23.Deng L.X., Khan A.M., Drajpuch D. Prevalence and correlates of post-traumatic stress disorder in adults with congenital heart disease. Am J Cardiol. 2016;117:853–857. doi: 10.1016/j.amjcard.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 24.Keir M., Bailey B., Lee A., Kovacs A., Roche S.L. Narrative analysis of adults with complex congenital heart disease: childhood experiences and their lifelong reverberations. Congenit Heart Dis. 2018;13:740–747. doi: 10.1111/chd.12647. [DOI] [PubMed] [Google Scholar]
- 25.Marelli A.J., Ionescu-Ittu R., Mackie A.S. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation. 2014;130:749–756. doi: 10.1161/CIRCULATIONAHA.113.008396. [DOI] [PubMed] [Google Scholar]
- 26.Dash J., Haller D.M., Sommer J., Junod Perron N. Use of email, cell phone and text message between patients and primary-care physicians: cross-sectional study in a French-speaking part of Switzerland. BMC Health Serv Res. 2016;16:549–555. doi: 10.1186/s12913-016-1776-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.