Abstract
Takotsubo syndrome is a well described clinical phenomenon that often mimics acute coronary syndrome. We present an atypical case of Takotsubo syndrome, characterized by delayed troponin elevation and electrocardiogram changes suggestive of acute coronary syndrome, but a normal coronary angiogram. We describe the integration of cardiac magnetic resonance imaging to identify syndrome overlap, and discuss the utilization of diagnostic modalities beyond coronary angiogram if clinical equipoise exists, including B-type natriuretic peptide/troponin ratio, intravascular coronary imaging, and cardiac magnetic resonance imaging.
Résumé
Le syndrome de Takotsubo est un phénomène clinique bien connu qui se présente souvent comme un syndrome coronarien aigu. Nous rapportons un cas atypique de syndrome de Takotsubo caractérisé par une élévation tardive du taux de troponine et par un tracé électrocardiographique évoquant un syndrome coronarien aigu, alors que la coronarographie ne révèle aucune anomalie. Nous décrivons comment utiliser l’imagerie par résonance magnétique cardiaque pour évaluer le chevauchement des deux syndromes et nous présentons l’utilisation des outils diagnostiques autres que la coronarographie en cas d’incertitude clinique absolue, notamment le rapport peptide natriurétique de type B/troponine, l’imagerie endocoronaire et l’imagerie par résonance magnétique cardiaque.
A 66-year-old woman presented for evaluation of back pain. The back pain was constant in nature, without a positional component, and not relieved by nitroglycerin or morphine. Her medical history included right-sided breast cancer (triple positive 2-mm invasive ductal carcinoma, with 1.2-cm ductal carcinoma in situ) diagnosed 12 months prior to the inciting event, following a right-breast lumpectomy, and treated with tamoxifen oral therapy. Adjuvant radiotherapy was completed 8 months prior to the inciting event. The patient did not smoke or consume alcohol, and there were no additional cardiovascular risk factors or known cardiac disease. The patient’s husband had passed away 1 week prior to presentation. There was no history of recent illness, immobilization, surgery, or travel. Heart rate and blood pressure were 70 beats per minute and 150/84 mm Hg, respectively. Physical examination was within normal limits.
High-sensitivity troponin was elevated at 244 ng/L (upper limit of normal: 30 ng/L) on presentation. All other laboratory investigations were within normal limits. Chest radiograph was normal. Computed tomography of the chest excluded pulmonary embolism and aortic dissection. An electrocardiogram (Fig. 1) did not demonstrate ischemic changes. Repeat troponin measurement, approximately 6 hours after presentation, was 3739 ng/L. B-type natriuretic peptide was not measured.
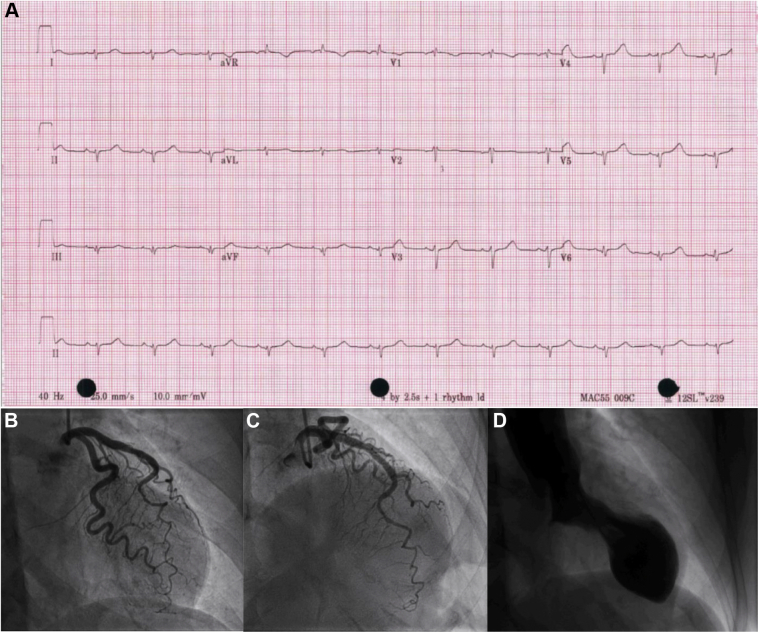
Figure 1.
(A) 12-lead electrocardiogram on admission. (B, C) Angiographic appearances of left anterior descending artery. (D) Ventriculographic appearance showing end-systole. aVF, augmented vector foot; aVL, augmented vector left; aVR, augmented vector right; V1-V6, precordial leads; I-III, limb leads.
The patient was advanced for coronary angiography, which demonstrated a normal dominant right coronary artery, mild plaque and ectasia in the mid-left anterior descending artery, but no obstructive coronary disease (Fig. 1). The left ventricular (LV) ejection fraction by ventriculography was estimated at 35%-49%, with basal segments contracting normally, but the mid-anterior wall, apex, and inferior segments were dyskinetic (Fig. 1). LV end diastolic pressure was 18-19 mm Hg. Echocardiography demonstrated an LV ejection fraction of 58%, with akinetic apical segments, normal LV wall thickness, and no evidence of LV thrombus (Videos 1-3
 , view videos online). Overall, preliminary findings were suggestive of stress-induced or typical Takotsubo syndrome.
, view videos online). Overall, preliminary findings were suggestive of stress-induced or typical Takotsubo syndrome.
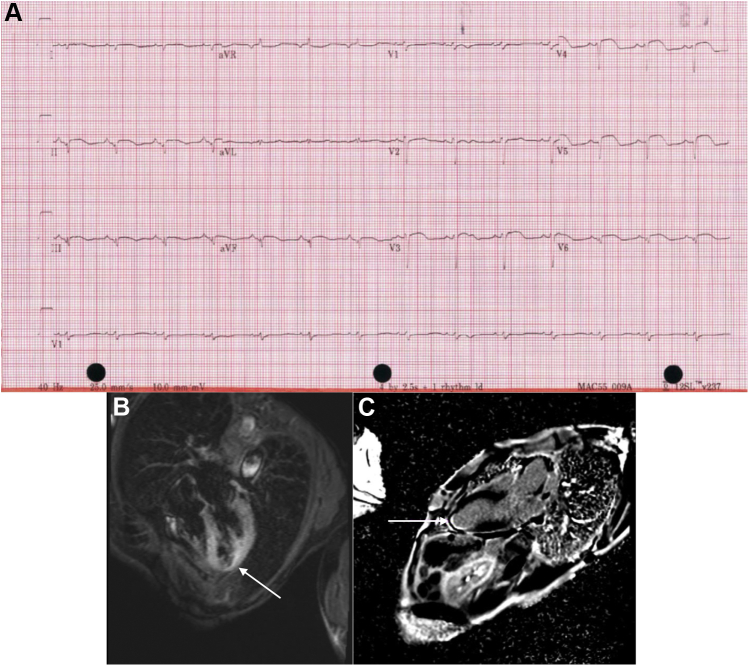
The following day, the patient reported a recurrence of back pain. Electrocardiogram results demonstrated new, profound ST-segment elevation in the inferior and posterior limb leads (Fig. 2). Despite previously trending down to 3068 ng/L, troponin now exhibited a further elevation to 5377 ng/L. The interventional cardiologist felt that ST-elevation myocardial infarction was unlikely, so a repeat coronary angiography was not performed. Echocardiography, with contrast study and agitated saline, demonstrated an LV ejection fraction of 46%, with akinetic distal apical segments, normal LV wall thickness, and no evidence of intracardiac shunt or LV thrombus. Given diagnostic uncertainty, cardiac magnetic resonance imaging (MRI; Fig. 2) was performed, demonstrating myocardial edema in the mid to apical LV segments, consistent with Takotsubo syndrome morphology. Edema in the mid to apical LV segments was assessed utilizing Hounsfield units (HU), and region of interest computing. Mean HU of the mid compared with the apical myocardium were not significantly different—HU 82 vs HU 85, respectively. Although there was LV apical hypokinesis, there was also subendocardial late-gadolinium enhancement, which is not a typical finding of Takotsubo syndrome but rather is suggestive of concomitant myocardial infarction.
Figure 2.
(A) Delayed 12-lead electrocardiogram, with ST-segment elevation in V3-V6. (B) Cardiac magnetic resonance imaging 4-chamber slice utilizing fluid-sensitive sequence (TIRM—turbo inversion recovery magnitude) demonstrating high signal (relative to skeletal muscle) within the mid to apical myocardium consistent with myocardial edema; note relative sparing of basal myocardium (white arrow). (C) Cardiac magnetic resonance imaging with delayed gadolinium sequence, 2-chamber view. The white arrow indicates the left ventricular apex with subendocardial enhancement. aVF, augmented vector foot; aVL, augmented vector left; aVR, augmented vector right; V1-V6, precordial leads; I-III, limb leads.
The patient was observed in-hospital for further episodes of discomfort, which did not occur. We hypothesized, given the information available, that the patient may have developed a missed LV thrombus in the context of Takotsubo syndrome, with coronary embolization. Following clinical stability and with planned follow-up, the patient was discharged on therapeutic anticoagulation in addition to a beta-blocker, statin, and an angiotensin-converting enzyme inhibitor. Repeat echocardiography 2 months after discharge demonstrated improvement of LV ejection fraction to 67%, with normal wall thickness and no evidence of LV thrombus. Although most of the prior regional wall motional abnormalities exhibited improvement, a small area of distal apical dyskinesis persisted, suggesting a diagnosis of Takotsubo syndrome with myocardial infarction overlap.
Discussion
The differential diagnosis for the area of infarction included small-vessel coronary artery disease, coronary vasospasm, spontaneous coronary artery dissection, left anterior descending artery plaque erosion, cardioembolic phenomena in the context of a missed LV thrombus, or atypical presentation of Takotsubo syndrome. Given clinical equipoise, we opted for a noninvasive approach with cardiac MRI. However, alternative diagnostic and imaging modalities can be used for such cases. B-type natriuretic peptide was not measured, and recent literature suggests that this biomarker may be further elevated in Takotsubo syndrome vs acute myocardial infarction alone, with a B-type natriuretic peptide/troponin ratio >1272 providing high specificity (95%) but low sensitivity for Takotsubo syndrome.1 Further, the magnitude of troponin elevation in this case is more likely to be associated with myocardial infarction than with Takotsubo syndrome alone.1 Intravascular ultrasound at the time of coronary angiography was not performed, but it may have allowed comment on spontaneous coronary artery dissection or vulnerable lesions and their precursors in the left anterior descending artery, potentially resulting in acute coronary syndrome (ACS) and stunning of the myocardium.2
In the acute setting, coronary angiography remains the gold-standard test to differentiate between Takotsubo syndrome and ACS.3 In a recent cohort study of patients admitted with suspected ST-elevation myocardial infarction who were advanced for percutaneous coronary intervention, 0.9% of patients were diagnosed with Takotsubo syndrome. Of this subset, the majority were women, with a mean age of 69 years; mean troponin elevation was 921 ng/L.4 Although ST-elevation is common at the time of presentation in patients who are diagnosed with Takotsubo syndrome, delayed ST-elevation is uncommon. As observed in this case, the two diagnoses are not mutually exclusive, and prior case reports have described ACS leading to Takotsubo syndrome, or ACS as a consequence of Takotsubo syndrome.5,6 Although there are proposed mechanisms linking these two diagnoses, such as somatic stress, it remains unclear in most cases whether Takotsubo syndrome is a cause or consequence of ACS.6,7
The role of cardiac MRI has been explored for such cases when there is diagnostic uncertainty. In Takotsubo syndrome, common imaging findings include cardiac edema within the LV wall without a vascular distribution.8 In an acute myocardial infarction, myocardial edema may be present but has a vascular distribution.8 Takotsubo syndrome typically presents without late gadolinium enhancement on delayed contrast sequences, as this would indicate myocardial necrosis.8 In this case, cardiac MRI served as an important tool for narrowing the differential diagnosis and forming a treatment plan.
This case highlights the challenge in differentiating syndrome overlap, and it may serve as an educational tool for the choice and integration of diagnostic modalities beyond coronary angiogram. The resurgence of back pain, further troponin elevation, and profound electrocardiogram changes were suggestive of an ischemic event. However, known coronary anatomy could not explain the electrocardiogram findings. Without intravascular coronary imaging, we acknowledge the preliminary coronary angiogram may have missed left anterior descending artery plaque rupture, a precursor to a vulnerable coronary lesion such as a thin-cap fibrous atheroma, or spontaneous coronary artery dissection.2 If clinical equipoise exists, exploring the use of advanced diagnostic modalities such as cardiac MRI or intravascular ultrasound may assist clinical decision-making. In this case, the utilization of cardiac MRI prompted our service to consider syndrome overlap, rather than a single diagnosis, which carried important implications for patient care, such as the choice of an oral anticoagulant vs dual antiplatelet therapy, and will serve as an educational piece for our institution.
Novel Teaching Points.
-
•
Takotsubo syndrome and ACS are not always mutually exclusive, and there are proposed mechanisms linking the 2 diagnoses.
-
•
Biochemical markers, including B-type natriuretic peptide and B-type natriuretic peptide/troponin ratio may help narrow the differential diagnosis.
-
•
Intravascular coronary imaging may be considered at the time of coronary angiogram to identify vulnerable coronary lesions.
-
•
Cardiac MRI is a noninvasive tool that can add valuable information when there is diagnostic uncertainty, and it carries the potential to differentiate between Takotsubo syndrome and ACS.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 725 for disclosure information.
Ethics Statement: Research reported has adhered to the relevant ethical guidelines. Informed consent was obtained prior to sharing clinical information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2020.08.001.
Supplementary Material
Two-dimensional transthoracic echocardiogram, apical three-chamber view, with akinetic apical segments, normal LV wall thickness, and no evidence of LV thrombus.
Two-dimensional transthoracic echocardiogram, apical four-chamber view, with akinetic apical segments, normal LV wall thickness, and no evidence of LV thrombus.
Two-dimensional transthoracic echocardiogram, parasternal short-axis view.
References
- 1.Randhawa M.S., Dhillon A.S., Taylor H.C., Sun Z., Desai M.Y. Diagnostic utility of cardiac biomarkers in discriminating takotsubo cardiomyopathy from acute myocardial infarction. J Card Fail. 2014;20:2–8. doi: 10.1016/j.cardfail.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Alfonso C.E. Takotsubo cardiomyopathy and coronary artery disease: a meaningful coincidence? J Am Heart Assoc. 2016;5:1–3. doi: 10.1161/JAHA.116.005131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lyon A.R., Bossone E., Schneider B. Current state of knowledge on Takotsubo syndrome: a position statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2016;18:8–27. doi: 10.1002/ejhf.424. [DOI] [PubMed] [Google Scholar]
- 4.Showkathali R., Patel H., Ramoutar A. Typical takotsubo cardiomyopathy in suspected ST elevation myocardial infarction patients admitted for primary percutaneous coronary intervention. Eur J Intern Med. 2014;25:132–136. doi: 10.1016/j.ejim.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Hurtado Rendón I.S., Alcivar D., Rodriguez-Escudero J.P., Silver K. Acute myocardial infarction and stress cardiomyopathy are not mutually exclusive. Am J Med. 2018;131:202–205. doi: 10.1016/j.amjmed.2017.07.039. [DOI] [PubMed] [Google Scholar]
- 6.Redfors B., Råmunddal T., Shao Y., Omerovic E. Takotsubo triggered by acute myocardial infarction: a common but overlooked syndrome? J Geriatr Cardiol. 2014;11:171–173. doi: 10.3969/j.issn.1671-5411.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ezad S., McGee M., Boyle A.J. Takotsubo syndrome associated with ST elevation myocardial infarction. Case Rep Cardiol. 2019;2019:1–6. doi: 10.1155/2019/1010243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernández-Pérez G.C., Aguilar-Arjona J.A., De La Fuente G.T. Takotsubo cardiomyopathy: assessment with cardiac MRI. Am J Roentgenol. 2010;195:W139–W145. doi: 10.2214/AJR.09.3369. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two-dimensional transthoracic echocardiogram, apical three-chamber view, with akinetic apical segments, normal LV wall thickness, and no evidence of LV thrombus.
Two-dimensional transthoracic echocardiogram, apical four-chamber view, with akinetic apical segments, normal LV wall thickness, and no evidence of LV thrombus.
Two-dimensional transthoracic echocardiogram, parasternal short-axis view.