Abstract
Background
The intent of the Canadian Alliance for Healthy Hearts and Minds (CAHHM) cohort is to understand the early determinants of subclinical cardiac and vascular disease and progression in adults selected from existing cohorts—the Canadian Partnership for Tomorrow’s Health, the Prospective Urban and Rural Evaluation (PURE) cohort, and the Montreal Heart Institute Biobank. We evaluated how well the CAHHM-Health Services Research (CAHHM-HSR) subcohort reflects the Canadian population.
Methods
A cross-sectional design was used among a prospective cohort of community-dwelling adults aged 35-69 years who met the CAHHM inclusion criteria, and a cohort of adults aged 35-69 years who responded to the 2015 Canadian Community Health Survey-Rapid Response module. The INTERHEART risk score was calculated at the individual level with means and proportions reported at the overall and provincial level.
Results
There are modest differences between CAHHM-HSR study participants and the 2015 Canadian Community Health Survey-Rapid Response respondents in age (56.3 vs 51.7 mean years), proportion of men (44.9% vs 49.3%), and mean INTERHEART risk score (9.7 vs 10.1). Larger differences were observed in postsecondary education (86.8% vs 70.2%), Chinese ethnicity (11.0% vs 3.3%), obesity (23.2% vs 29.3%), current smoker status (6.1% vs 18.4%), and having no cardiac testing (30.4% vs 55.9%).
Conclusions
CAHHM-HSR participants are older, of higher socioeconomic status, and have a similar mean INTERHEART risk score, compared with participants in the Canadian Community Health Survey. Differing sampling strategies and missing data may explain some differences between the CAHHM-HSR cohort and Canadian community-dwelling adults and should be considered when using the CAHHM-HSR for scientific research.
Résumé
Contexte
L’étude Alliance canadienne cœurs et cerveaux sains (CAHHM) vise à mieux comprendre les facteurs déterminants précoces et la progression de l’atteinte cardiovasculaire subclinique chez des adultes sélectionnés au sein de cohortes existantes – soit celles de l’étude menée par le Partenariat canadien pour la santé de demain, de l’étude PURE (Prospective Urban and Rural Evaluation) et de la biobanque de l’Institut de cardiologie de Montréal. Nous avons évalué la mesure dans laquelle la sous-cohorte du volet de recherche sur l’utilisation des services de santé de la CAHHM (CAHHM-HSR) représente la population canadienne.
Méthodologie
Nous avons adopté une approche transversale pour étudier une cohorte prospective d’adultes vivant dans la communauté âgés de 35 à 69 ans et répondant aux critères d’inclusion de l’étude CAHHM, ainsi qu’une cohorte d’adultes âgés de 35 à 69 ans ayant participé au volet de réponse rapide de l’Enquête sur la santé dans les collectivités canadiennes (ESCC) de 2015. Le score de risque INTERHEART individuel des participants a été calculé à partir des moyennes et des proportions rapportées à l’échelle globale et à l’échelle provinciale.
Résultats
Les différences entre les participants du volet CAHHM-HSR et ceux du volet de réponse rapide de l’ESCC de 2015 étaient minimes quant à l’âge (56,3 ans vs 51,7 ans en moyenne), à la proportion d’hommes (44,9 % vs 49,3 %) et au score de risque INTERHEART moyen (9,7 vs 10,1). On a toutefois noté des différences plus importantes en ce qui concerne les caractéristiques suivantes : éducation postsecondaire (86,8 % vs 70,2 %), origine ethnique chinoise (11,0 % vs 3,3 %), obésité (23,2 % vs 29,3 %), tabagisme actuel (6,1 % vs 18,4 %) et absence d’antécédents d’examen cardiaque (30,4 % vs 55,9 %).
Conclusions
Les participants du volet CAHHM-HSR sont plus âgés et ont un statut socioéconomique plus élevé que ceux du volet de réponse rapide de l’ESCC, mais ont un score de risque INTERHEART moyen comparable. Les différences quant aux stratégies d’échantillonnage et des données manquantes pourraient expliquer certains des écarts observés entre la cohorte CAHHM-HSR et celle des adultes canadiens vivant dans la communauté; il conviendrait d’en tenir compte lorsqu’on utilise les données du volet CAHHM-HSR à des fins de recherche scientifique.
Cardiovascular disease is the leading cause of morbidity and mortality in Canada.1 Cardiovascular health is critical to prevent cardiac, vascular, and cognitive dysfunction, as well as ensure quality of life, longevity, and sustainable health care expenditures.2 Given the increasing prevalence of cardiovascular risk factors among Canadians, and the rising prevalence of obesity and the associated consequences, including hypertension and diabetes, it is of paramount importance to understand the early determinants of cardiac, vascular, and cognitive dysfunction and progression to clinical events.2 The Canadian Alliance for Healthy Hearts and Minds (CAHHM) was designed to address this knowledge gap.
The goal of the CAHHM is to examine the associations among socio-environmental and contextual factors, activity, nutrition, and social and tobacco environments, as well as cardiovascular risk factors, subclinical vascular disease as measured by magnetic resonance imaging, and cardiovascular and other chronic disease outcomes.2,3 The CAHHM is a rich cohort platform to inform policy and population health interventions as well as determine markers of subclinical stages of cardiovascular disease.2
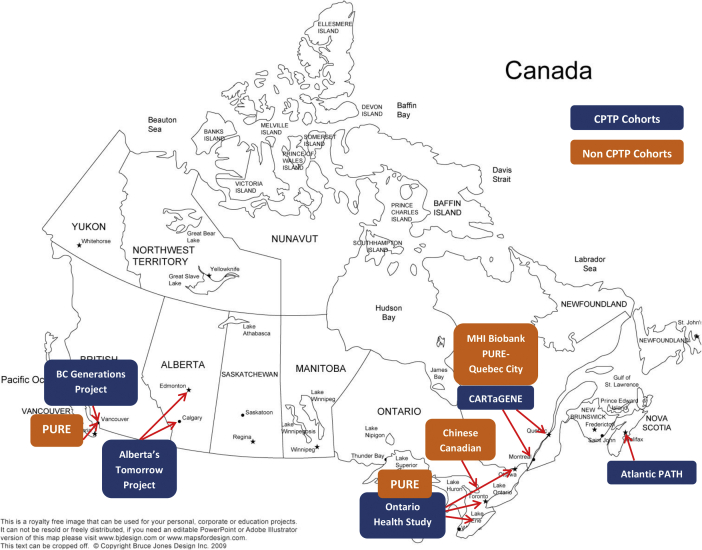
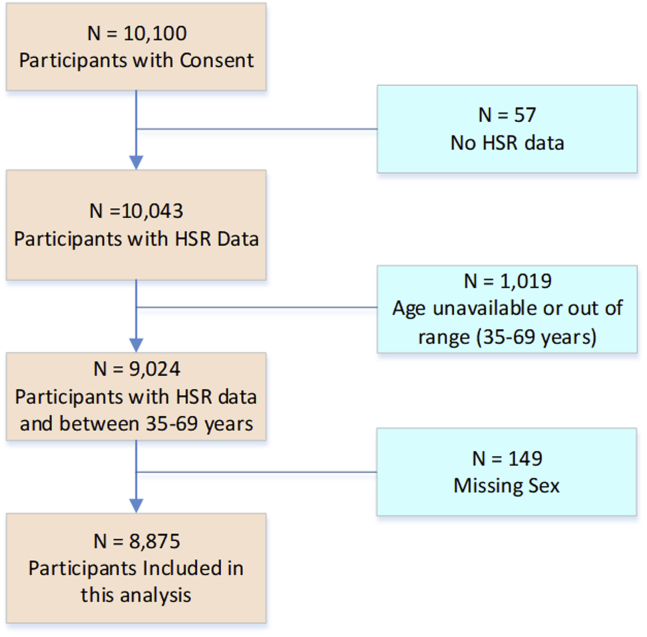
The CAHHM-Health Services Research (CAHHM-HSR) is a subcohort study of the CAHHM population with available HSR data among adults aged between 35 and 69 years. The cohorts for the CAHHM were largely recruited from participants in the Canadian Partnership for Tomorrow Project, which focused on individuals aged 35-69 years. The age group allows for understanding the early determinants of subclinical cardiac and vascular disease and progression. The CAHHM-HSR includes 8875 participants recruited from multiple sources, including existing cohorts as well as de novo. The 5 Canadian Partnership for Tomorrow’s Health cohorts (BC Generations Project, Alberta’s Tomorrow Project, Ontario Health Study, CARTaGENE, and Atlantic PATH), the Prospective Urban and Rural Evaluation (PURE) Canada cohort (from Vancouver, Quebec City, and Hamilton), and the Montreal Heart Institute Biobank (MHI-Biobank) invited their eligible participants to take part via e-mail, phone call, and in-person visits. Special efforts were made to recruit participants from ethnic minorities, by asking the partner cohorts to prioritize participants of South Asian, Chinese, and African ethnicity, as well as co-recruit South Asian participants from Ontario. Additional recruitment of a “new” Chinese cohort from the greater Toronto area was also undertaken as previously described.4 In parallel, a First Nations cohort was developed, and data from this cohort are not included in this analysis.5 The CAHHM cohort platform provides a large cohort of adults with extensive risk and contextual factor measurement, in-depth phenotyping, geographic and ethnic diversity, and the ability to link to health care service utilization and outcomes.2 The CAHHM-HSR subcohort includes individuals aged 35-69 years who had HSR data captured between 2014 and 2018 (Fig. 1). Given the extensive resources associated with the CAHHM, it is essential to describe the characteristics of the subcohort to inform and support researchers and promote broader uptake of this data source in accelerating future research into cardiac, vascular, and cognitive dysfunction and outcomes.2
Figure 1.
CAHHM-HSR participant selection by cohort. BC, British Columbia; CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CPTP, Canadian Partnership for Tomorrow Project; MHI, Montreal Heart Institute; PATH, Partnerships for Tomorrow’s Health; PURE, Prospective Urban and Rural Evaluation.
We aimed to assess the generalizability of the CAHHM-HSR cohort to Canadians selected for the 2015 Canadian Community Health Survey—Rapid Response (CCHS-RR) module and residing in the same provinces as the CAHHM-HSR participants. Specifically, the objectives of this study were as follows: (i) to describe the CAHHM-HSR cohort ; (ii) to compare the CAHHM-HSR cohort to the CCHS-RR cohort. This comparison is 2-fold, focusing first on population health and health services indicators, including rates of smoking, diabetes, hypertension, obesity, myocardial infarction (MI), and stroke, as well as diabetes screening, lipid screening, electrocardiograms, cardiac stress tests, and echocardiograms. The second area of focus covers the regional variation across Canada in rates of cardiac disease, access to care, screening rates, prevalence of risk factors, cardiac testing, and INTERHEART risk score results. Based on the above findings, we discuss the generalizability of the CAHHM-HSR cohort to the Canadian population.
Materials and Methods
Data sources
CAHHM-HSR
The CAHHM-HSR is a derived prospective cohort of adults from existing cohorts in the Canadian Partnerships for Tomorrow Project.6 The specific cohorts included the following: (i) CARTaGENE in Quebec7; (ii) Ontario Health Study in Ontario (OHS), (iii) British Columbia Generations Project (BCGP)8; (iv) Atlantic Partnership for Tomorrow’s Health (PATH) in Nova Scotia9; (v) Alberta’s Tomorrow Project10; (vi) the Prospective Urban Rural Epidemiological Study (PURE—Canada) in Hamilton, Vancouver, and Quebec City11; (vii) the Montreal Heart Institute—MHI BioBank in Montreal (see Fig. 1), and a new Chinese cohort of adults recruited from the greater Toronto area. All cohorts with the exception of the OHS, had a maximum of 20% of participants with a history of MI, stroke, cancer, percutaneous transluminal coronary angioplasty, or coronary artery bypass graft (CABG) surgery. The OHS participant selection criteria excluded subjects with history of MI, stroke, CABG surgery, angioplasty, congestive heart failure, or cancer.
Details of the CAHHM design and methodology have been described elsewhere.2 In brief, the CAHHM study selected adults aged 35-69 years at the time of entry into their respective Canadian Partnership for Tomorrow’s Health cohorts that were willing to undergo a magnetic resonance imaging scan through a quasi-random process. Recruitment was targeted to allow over-recruiting of high-risk ethnic minorities of South Asian, Chinese, and African descent, as well as achieve equal representation of male and female participants and ensure that we have a predominantly healthy cohort with at most 20% with known cardiovascular disease (MI, stroke, percutaneous transluminal coronary angioplasty, CABG) across 3 age groupings: 35-45, 46-55, and 56-69 years.2 Consecutive participants from the PURE—Canada, and the MHI BioBank cohorts, were selected.2 At the time of the analyses (November 2018), there were 8875 participants, with most participants (∼80%) providing the HSR information in 2015 and 2016, and with Ontario participants representing 49%, Quebec 24%, British Columbia 11%, Nova Scotia 10%, and Alberta 7% of the cohort (Fig. 2).
Figure 2.
CAHHM-HSR study cohort. CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds-Health Services Research.
CAHHM-HSR participant sociodemographic factors were obtained from their original cohort study data, and all participants who consented to CAHHM-HSR completed a detailed self-administered Health Services Questionnaire (HSR) (online or mailed) to obtain information on cardiovascular risk factors, health behaviours, access to care and cardiac diagnostic testing, and information needed to calculate the non-lab INTERHEART risk score—a validated score for quantifying risk-factor burden without the use of laboratory testing.12 The score range is 0-49, with a higher score, the greater the modifiable cardiovascular risk-factor burden, and when categorized, a score between 0 and 9 is considered low risk; 10-15 is medium risk, and 16-49 is a high risk factor burden.8 The HSR contained questions similar to those administered in the 2015 CCHS-RR module (see Supplemental Appendix S1).
CCHS-RR module
The CCHS is a national cross-sectional survey conducted by Statistics Canada that has collected demographic, health status, health care utilization, and determinants of health information on ∼130,000 community-dwelling Canadians annually since 2007.13 Data collection in the 110 health regions is conducted through random selection of telephone numbers to conduct interviews with a randomly selected respondent per household, and planned oversampling of youths will result in a second member of certain households being interviewed.13
An investigator (JVT), in collaboration with Statistics Canada, developed the 15-question Rapid Response Module to capture supplemental cardiac health information on the 2015 CCHS (CCHS-RR; see Supplemental Appendix S2). The CCHS-RR was administered to a subset of the CCHS respondents between July and December 2015. From the CCHS-RR we created a subcohort of adults aged 35-69 years and excluded respondents from Saskatchewan, Manitoba, New Brunswick, Prince Edward Island, and Newfoundland, and indigenous respondents to mirror the CAHHM-HSR cohort participants, resulting in 10,395 respondents, representing 14,439,126 Canadian adults between aged 35 and 69 years residing in British Columbia, Alberta, Ontario, Quebec, and Nova Scotia. The CCHS-RR cohort represents over 80% of Canada’s 35-69-year-old population, and its regional distribution reflects Canada’s regional population distribution with the exception of Ontario, where the CCHS-RR cohort is ∼5% lower.14
The collection of data from the CAHHM- HSR, in addition to data from the CCHS-RR, enabled examination of differences on the cardiac risk factors, outcomes, and utilization of preventive health care services in communities across Canada.
Analysis
Pairwise deletion was used in all analyses (ie, records were excluded only when the variable of interest was missing). See Supplemental Table S1 for variable percentage of missing records for variables used in this study. Means for continuous measures and proportions for categorical measures were calculated. Means and proportions were age/sex standardized based on the 2011 Canada Census using the following age groupings: 35-49, 50-59, and 60-69 years. CCHS-RR results were weighted using Statistics Canada survey weights.13
Results
Table 1 compares the sociodemographic characteristics of the CCHS-RR and CAHHM-HSR cohorts. Compared to the CCHS-RR participants, CAHHM-HSR study participants are older (aged 56.3 vs 51.7 years), have a lower prevalence of men (44.9% vs 49.3%) and widowers (1.8% vs 2.4%), and a higher prevalence of participants with postsecondary education (86.8% vs 70.2%) and Chinese ethnic background (11.0% vs 3.3%).
Table 1.
Self-reported prevalence of sociodemographic characteristics in the CCHS-RR and CAHHM-HSR cohorts
| Characteristic | CCHS-RR |
CAHHM-HSR |
|---|---|---|
| (N = 14,439,126) | (N = 8875) | |
| Age (mean), y | 51.7 | 56.3 |
| Sex, male | 49.3 | 44.9 |
| Marital status∗ | ||
| Divorced/separated | 11.4 | 12.0 |
| Married/common-law | 74.6 | 74.7 |
| Single | 11.6 | 11.5 |
| Widowed | 2.4 | 1.8 |
| Highest level of education∗ | ||
| Less than secondary school | 9.1 | 0.6 |
| Secondary school | 20.7 | 12.7 |
| Postsecondary or university degree | 70.2 | 86.8 |
| Canadian born∗ | 70.3 | 73.5 |
| Racial/ethnic background∗ | ||
| White only | 79.2 | 80.1 |
| South Asian only | 4.7 | 4.2 |
| Chinese only | 3.3 | 11 |
| Black only | 2.7 | 1.3 |
| Other/multiple | 10.0 | 3.4 |
Values are %, unless otherwise indicated.
CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response.
Among those not missing data.
Table 2 compares the differences in prevalence of cardiovascular risk factors, conditions, and comorbidities between the CAHHM-HSR and the CCHS-RR. The CAHHM-HSR participants have a higher prevalence of cardiovascular disease (3.7% vs 2.5%), a much higher prevalence of hypertension (26.1% vs 18.1%), hypercholesterolemia (32.7% vs 14.6%), asthma (12.8% vs 7.5%), and paternal family history of heart attack (17.4% vs 10.4%), but a lower prevalence of obesity, diabetes, and chronic obstructive pulmonary disease (23.2% vs 29.3%, 5.8% vs 7.4%, and 0.7% vs 3.5%, respectively), compared with the general Canadian adult population in the same age range (ages 35-69 years). As well, the CAHHM-HSR cohort participants are more likely to report having a regular health care provider than the CCHS-HSR cohort (94.3% vs 86.6%).
Table 2.
Age- and sex-standardized self-reported prevalence of cardiovascular risk factors, conditions, and comorbidities in the CCHS-RR and CAHHM-HSR cohorts∗
| Cardiovascular risk factors | CCHS-RR | CAHHM-HSR |
|---|---|---|
| Diabetes | 7.4 | 5.8 |
| Hypertension | 18.1 | 26.1 |
| High cholesterol | 14.6 | 32.7 |
| Obesity† | 29.3 | 23.2 |
| Family history, mother | 5.4 | 4.8 |
| Family history, father | 10.4 | 17.4 |
| Smoking status | ||
| Current | 18.4 | 6.1 |
| Former | 29.2 | 29.3 |
| Experimental or abstainer | 52.4 | - |
| Ate salty foods in the past week | 78.6 | 30.8 |
| Ate meat in the past week | 95.9 | 34.6 |
| Deep fried foods in the past week | 53.8 | 13.7 |
| Cardiovascular conditions and comorbidities | ||
| Cardiovascular disease | ||
| Atrial fibrillation | 0.7 | 1.3 |
| Heart attack | 1.0 | 0.9 |
| Stroke | 0.8 | 0.4 |
| Angina | 0.8 | 0.8 |
| Heart failure | 0.3 | 0.1 |
| Aortic stenosis | 0.4 | 0.2 |
| Peripheral vascular disease | 0.4 | 0.1 |
| PCI or CABG | 1.4 | 1.3 |
| Any cardiovascular disease‡ | 2.5 | 3.7 |
| Comorbidities | ||
| Asthma | 7.5 | 12.8 |
| Chronic obstructive pulmonary disease | 3.5 | 0.7 |
| Has a regular health care provider | 86.6 | 94.3 |
CABG, coronary artery bypass graft; CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response; PCI, percutaneous coronary intervention.
Among those not missing data .
Body mass index ≥ 30.
Defined as reporting any of the following: atrial fibrillation, heart attack, stroke, angina, heart failure, aortic stenosis, peripheral vascular disease, PCI, CABG.
Although the CAHHM-HSR participants had the same prevalence of former smokers as the CCHS-RR participants (29.3% vs 29.2%), the prevalence of current smokers was 3 times lower among the CAHHM-HSR participants than among CCHS-RR participants aged 35-69 years (6.1% vs 18.4%). There were large differences in the reported consumption of salty, deep-fried foods, and meat or poultry between the CAHHM-HSR and CCHS-RR participants (30.8% vs 78.6%, 13.7% vs 53.8%, and 34.6% vs 95.9%, respectively).
Table 3 compares the proportion of CAHHM-HSR and CCHS-RR participants exposed to cardiac testing and screening. The CAHHM-HSR participants had a higher prevalence of cardiac-specific testing compared with the general Canadian population, but they had a similar frequency of blood pressure screening (80.4% vs 79.3%) and a lower blood lipid–screening frequency (56.3% vs 66.1%).
Table 3.
Age- and sex-standardized self-reported prevalence of cardiac testing, screening, and medication in the CCHS-RR and CAHHM-HSR cohorts∗
| Cardiac testing | CCHS-RR | CAHHM-HSR |
|---|---|---|
| Electrocardiogram | 39.3 | 58.4 |
| Stress test | 17.7 | 31.0 |
| Echocardiogram | 17.6 | 20.4 |
| Cardiac MRI | — | 4.8 |
| Heart CT | — | 3.8 |
| Holter monitor | — | 15.2 |
| Other | — | 3.4 |
| None | 55.9 | 30.4 |
| Screening† | ||
| Blood pressure measured (≤ 1 y) | 79.3 | 80.4 |
| Lipids measured (≤ 1 y) | 66.1 | 56.3 |
| Medication | ||
| Lipid-lowering medication | 13.3 | 13.9 |
| Aspirin | 12.7 | 10.9 |
CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response; CT, computed tomography; MRI, magnetic resonance imaging.
Excludes those who did not respond.
CAHHM-HSR screening values measured at <1 year.
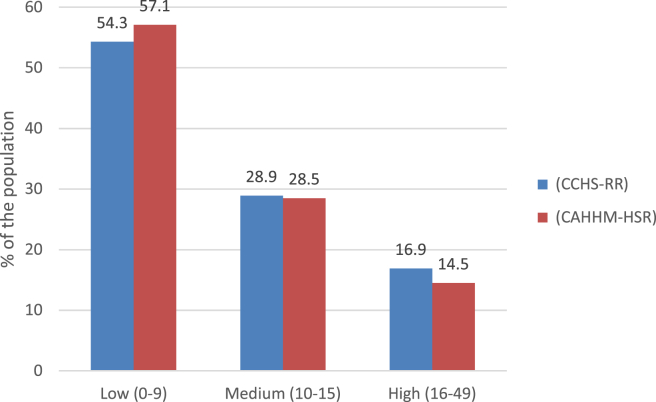
Table 4 and Figure 3 illustrate the overall difference in INTERHEART risk score between the CAHHM-HSR and CCHS-RR participants. Overall, CAHHM-HSR participants had mean INTERHEART scores similar to those in the general Canadian population aged 35-69 years (9.7 vs 10.1; see Table 4). Among the CAHHM-HSR participants, 14.5% were considered to have a high risk-factor burden (score 16-49), compared to 16.9% of the CCHS-RR participants.
Table 4.
Age- and sex-standardized regional variation in mean INTERHEART risk score∗ in the CCHS-RR vs CAHHM-HSR cohorts
| Cohort | BC | AB | ON | QC | NS | Overall |
|---|---|---|---|---|---|---|
| CCHS-RR | 8.7 | 9.9 | 10.3 | 10.6 | 11.5 | 10.1 |
| CAHHM-HSR | 8.8 | 9.1 | 10.0 | 9.7 | 10.1 | 9.7 |
AB, Alberta; BC, British Columbia; CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response; NS, Nova Scotia; ON, Ontario; QC, Quebec
Calculated among those with complete data needed to calculate the score.
Figure 3.
Overall age- and sex-standardized proportions of INTERHEART risk-score categories (calculated among those with complete data needed to calculate the score) for CCHS-RR and CAHHM-HSR. CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response.
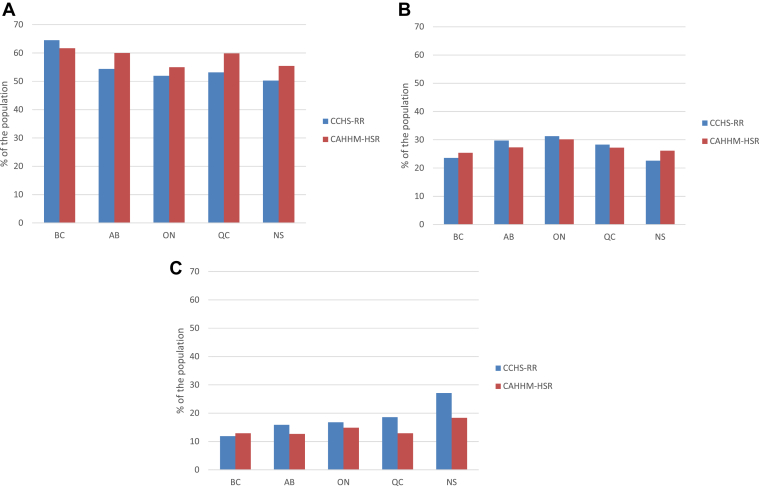
Regional variation
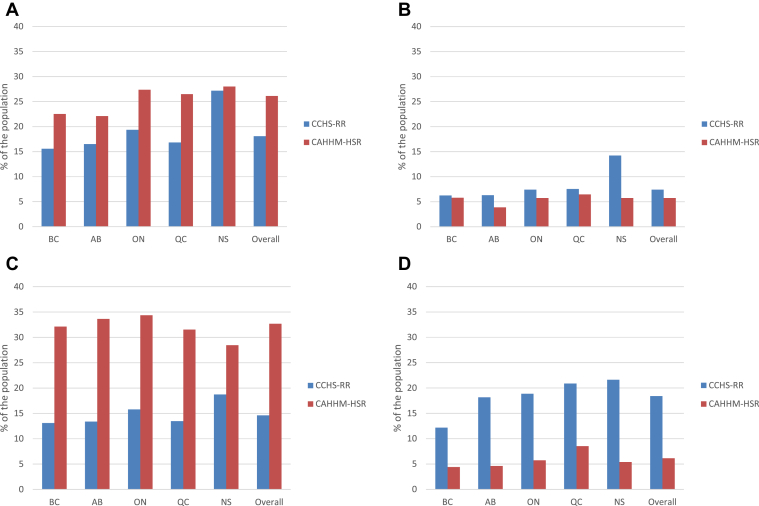
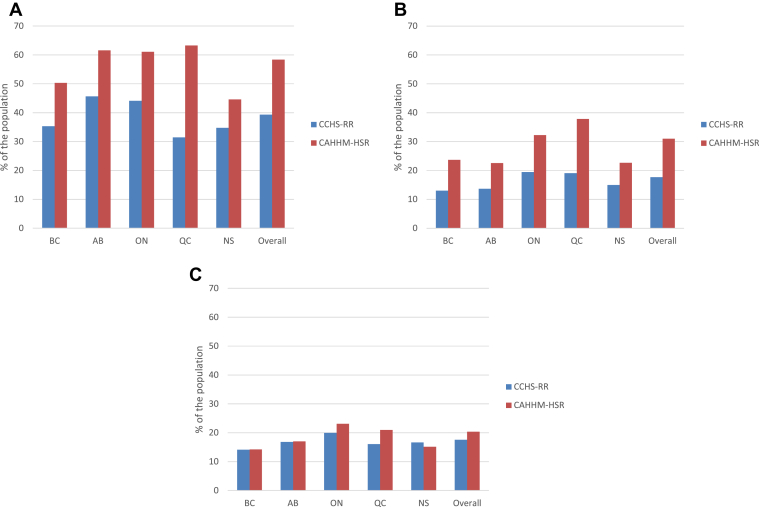
Figure 4, A-C shows the provincial variation in the proportion of respondents with low, moderate, and high INTERHEART risk scores. In British Columbia, the frequencies of INTERHEART risk-score categories (low/medium/high) are very similar in the CAHHM-HSR and CCHS-RR cohorts. However, in most of the other provinces, the CAHHM-HSR cohort has a higher proportion of participants in the low INTERHEART risk-score category, and a lower proportion of participants in the high INTERHEART risk-score category, compared with the CCHS-RR cohort. There is also a west-to-east gradient in the mean INTERHEART risk scores among CCHS-RR respondents, with the mean INTERHEART risk scores monotonically increasing, moving from the western to the eastern region of Canada, that does not appear in the CAHHM-HRS cohort (see Table 4). Figure 5, A-D illustrates the variation in risk-factor frequency across Canada in the CCHS-RR and CAHHM-HSR cohorts. Again, the west-to-east gradient of cardiovascular risk-factor frequency among the CCHS-RR cohort was not observed in the CAHHM-HSR cohort, except for hypertension. Across all regions, the CAHHM-HSR cohort has a lower prevalence of diabetes and a much lower prevalence of current smokers compared to the CCHS-RR cohort. Conversely, the CAHHM-HSR cohort had a higher prevalence of hypertension and hypercholesterolemia across all regions.
Figure 4.
(A-C) Age- and sex-standardized prevalence of CAHHM-HSR and CCHS-RR participants with a low (0-9), medium (10-15), and high (16-49) INTERHEART risk score (calculated among those with complete data needed to calculate the score), by region. AB, Alberta; BC, British Columbia; CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response; NS, Nova Scotia; ON, Ontario; QC, Quebec.
Figure 5.
(A-D) Prevalence of age- and sex-standardized cardiovascular risk factors (hypertension, diabetes, high cholesterol, current smoker) across regions in the CAHHM-HSR and CCHS-RR cohorts (calculated among those with complete data needed to calculate). AB, Alberta; BC, British Columbia; CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response; NS, Nova Scotia; ON, Ontario; QC, Quebec.
Figure 6, A-C illustrates that the CAHHM-HSR cohort has higher rates of cardiac testing than the CCHS-RR cohort across all regions with electrocardiogram and stress-testing rates much higher across all regions for the CAHHM-HSR cohort than the CCHS-RR cohort. The 2 cohorts differed in echocardiogram testing in Quebec and Ontario, with the CAHHM-HSR cohort having higher rates (21.0% vs 16.1% and 23.1% vs 20.0%, respectively), but it had lower rates in Nova Scotia (15.2% vs 16.7%) than the CCHS-RR cohort.
Figure 6.
(A-C). Prevalence of age- and sex-standardized cardiac testing (electrocardiogram, stress test, echocardiogram) across regions in the CCHS-RR and CAHHM-HSR cohorts (calculated among those with complete data needed to calculate ). AB, Alberta; BC, British Columbia; CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response; NS, Nova Scotia; ON, Ontario; QC, Quebec.
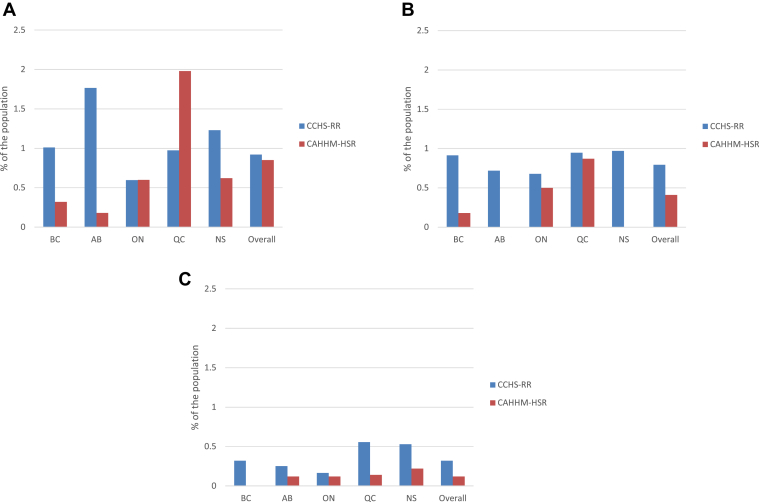
Figure 7, A-C illustrates the regional variation in cardiac disease in the CCHS-RR and CAHHM-HSR cohorts. Generally, the prevalence of cardiac disease across the regions was lower in the CAHHM-HSR cohort than in the CCHS-RR cohort. The exception was in Ontario where the CCHS-RR and CAHHM-HSR cohorts had a similar prevalence of MI, and in Quebec, the MI frequency in the CAHHM-HSR cohort was double the frequency in the CCHS-RR cohort (1.98% vs 0.97%).
Figure 7.
(A-C) Prevalence of age- and sex-standardized cardiac disease (heart attack, stroke, heart failure) across regions in the CCHS-RR and CAHHM-HSR cohorts (calculated among those with complete data needed to calculate). AB, Alberta; BC, British Columbia; CAHHM-HSR, The Canadian Alliance for Healthy Hearts and Minds—Health Services Research; CCHS-RR, Canadian Community Health Survey—Rapid Response; NS, Nova Scotia; ON, Ontario; QC, Quebec.
Discussion
The CAHHM-HSR cohort is the first study in Canada of cardiovascular risk factors including modifiable risk factors. The CAHHM-HSR participants are, on average, older, more likely to be women, and more highly educated compared with the general Canadian community-dwelling adults aged 35-69 years included in the CCHS-RR. There are also differences in cardiovascular risk factors; specifically, CAHHM-HSR participants were more likely to have a diagnosis of hypertension and hypercholesterolemia, but less likely to be considered current smokers, obese, or diagnosed with diabetes compared with the general Canadian population. The 2017 Canadian Tobacco, Alcohol and Drugs study revealed a higher prevalence of current smokers (15.1%) among the Canadian population aged 15 years or older, than among the CAHHM-HSR cohort, supporting our finding of a much healthier CAHHM-HSR cohort, compared with the Canadian population.15 Similarly, the obesity and diabetes prevalence—26.7% and 10%, respectively, in Canada during the study period, as reported by Diabetes Canada, also suggests a healthier CAHHM-HSR cohort.16 The higher prevalence of hypertension and hypercholesterolemia is not surprising given that over 90% of CAHHM-HSR participants reported that they had a regular health care provider. Higher rates of cardiovascular risk factor screening and monitoring have been observed when individuals have a regular health care provider.17 Despite the differences in demographics, cardiovascular risk, and history of cardiovascular disease between the CAHHM-HSR and CCHS-RR cohorts, we observed similar frequencies between the 2 of a history of MI and angina, and small differences in the overall mean INTERHEART risk score (9.7 vs 10.1), but larger differences in the proportions of respondents in the low and high INTERHEART risk-score categories: low risk—57.1% vs 54.3%; medium risk—28.5% vs 28.8%; and high risk—14.5% vs 16.9%, respectively, indicating better cardiovascular health status of the CAHHM-HSR cohort. However, both the CAHHM-HSR and the CCHS-RR cohorts report a lower prevalence of age–sex standardized MI (0.9%,1.0% vs 2.0%, respectively) and heart failure (0.1%, 0.3% vs 3.4%, respectively) than observed in the general Canadian population aged >20 years, based on administrative databases.18 This information should be considered when analyzing data from CAHHM.
Strengths
One strength of this study is that it provides an example of the value of the 2015 CCHS-RR as a rich data source representative of the Canadian population aged 35-69 years. Cardiovascular health researchers should consider using it to evaluate the representativeness of their study cohorts because it contains information beyond sociodemographic characteristics available in census data. Specifically, the CCHS-RR captures cardiovascular risk-factor, screening, and cardiac testing, as well as data needed to calculate the INTERHEART risk score, and it can assist in determining the generalizability of relevant study populations.
The CAHHM-HSR cohort leverages several cohorts across Canada and provides a rich data source, including phenotype and modifiable risk-factor information, to study national and regional cardiovascular disease development and benchmarking for future CAHHM research. It also includes oversampling of participants of Chinese ethnicity to allow for robust subpopulation cardiovascular disease development studies.
Limitations
Selection, recall, and social desirability bias are always a concern in any survey-based study. The quality of self-reported conditions, medications, and diagnostic testing is dependent upon having been diagnosed, prescribed, or referred by a physician and reporting accurately in the survey. Ideally, the data would have been verified through linkage to health administrative data or collection of physical or clinical measures to mitigate potential misclassification.
The observed differences between the CAHHM-HSR and CCHS-RR participants may also be explained by the different recruitment strategies. The sampling frame CAHHM-HSR used included several cohorts that employed recruiting incentives that resulted in a selected group of participants enrolled who are healthier in general (current smokers 6.1% vs 18.4% in the CCHS-RR; obesity 23.2% vs 29.3% in the CCHS-RR) and have higher education and time to travel to central urban sites for in-depth investigations and measurements.19 Unlike the CCHS, which is a telephone survey designed to be representative of the Canadian population, recruitment strategies for the cohorts within the CAHHM-HSR increased the chances of a nonrepresentative sample. For example, there was a concerted effort to prioritize recruitment of Chinese-, South Asian–, and African-origin participants, and recruitment of a separate Chinese cohort given the higher risk for cardiovascular morbidity observed in these ethnic groups. Although we show that the CAHHM-HSR cohort is not a clear representation of the general Canadian population aged 35-69 years in British Columbia, Alberta, Ontario, Quebec, and Nova Scotia, limiting generalizability, the CAHHM-HSR cohort recruitment and survey instrument was consistent, and hence subcohort comparisons (ie, provincial comparisons) are unlikely to be affected by differential misclassification (ie, when comparing groups with different data sources, the accuracy may be better in one group, resulting in differential misclassification).
Given the differing sampling strategies employed in the 2 cohorts, it is unclear how to best formally test differences between them. The CAHHM-HSR is a convenience sample without weights but allows for conventional statistical methods for making inferences. In contrast, it is uncertain if applying the CCHS bootstrap weights in conjunction with bootstrap resampling methodology to the CCHS-RR respondents to construct confidence intervals is appropriate. Furthermore, it is unclear how to compare the 2 cohorts, one of which requires the use of bootstrap weights for inference (CCHS-RR), and one of which permits the use of conventional methods for statistical inference (CAHHM-HSR). However, our intent was to illustrate the similarities and differences between cohorts, not to draw formal conclusions nor formally test statistical hypotheses about differences.
Differences in the percentage of missing data may also explain the observed differences between the CCHS-RR and CAHHM-HSR cohorts. The range of missing data in the CCHS-RR varied from 0% for age and sex data to 22% for the INTERHEART risk score, which includes several cardiovascular risk factors. In the CAHHM-HSR, the level of missing data varied from 0% for age and sex data to 40% for a history of stroke. The extent of missing data on cardiac testing, and of data needed to calculate the INTERHEART risk score in the CAHHM-HSR, was close to half the missing data in the CCHS-RR (7% vs 15% and 13% vs 22%, respectively). Conversely, for smoking status and obesity, the extent of missing data in the CAHHM-HSR was more than double that in the CCHS-RR (13% vs <5%; 13% vs 4%, respectively; see Supplemental Table S1). Finally, the questionnaires used by the CCHS-RR vs CAHHM-HSR were very similar but not identical for all questions. Examples are the time frame used to ask about most-recent screening tests, and the response options available for the dietary questions. For the dietary questions, responses were analyzed to allow for harmonization of the dietary questions between the 2 cohorts and are therefore unlikely to explain the observed large differences in dietary risk factors. However, in the CCHS-RR, the dietary question was posed as “In the past week, how many times did you eat salty foods or snacks such as prepared soups, lunch meat and potato chips?” Thus, it provides examples, whereas in the CAHHM-HSR, the question was simply “Do you eat salty food or snacks one or more times a day?” The examples provided in the CCHS-RR may have introduced recall bias, and furthermore, there may have been social desirability bias among the CAHHM-HSR participants, contributing to the large differences reported between the 2 cohorts.
Conclusions
Compared with the CCHS-RR, the CAHHM-HSR cohort is older, of higher socioeconomic status, and has differing individual INTERHEART cardiovascular risk-score frequencies (low/medium/high), although the mean INTERHEART risk score is similar. These differences should be considered when using the CAHHM-HSR data for scientific research.
Acknowledgements
The authors thank Tara O’Neill for creating the figures and tables, as well as formatting the manuscript for publication, and Dr Peter Austin for his statistical advice. The authors are indebted to Dr Jack V. Tu (deceased May 30, 2018), who was a Co-Principle Investigator on the Canadian Alliance for Healthy Hearts and Minds study and contributed to the early work of this paper.
Steering Committee: S. Anand (Chair), M.G. Friedrich (Co-Chair), Douglas Lee (Co-Chair), J. Tu (former Co-Chair), P. Awadalla (OHS), T. Dummer (BCGP), J. Vena (Alberta Tomorrow Project), P. Broet (CARTaGENE), J. Hicks (Atlantic Partnership for Tomorrow's Health), J-C. Tardif (MHI Biobank), K. Teo (PURE-Central), B-M. Knoppers (Ethics Legal Social Implications).
Project office staff at Population Health Research Institute (PHRI): D. Desai, S. Nandakumar (Ex), M. Thomas (Ex), S. Zafar.
Statistics/biometrics programmer team at PHRI: K. Schulze, L. Dyal, A. Casanova, S. Bangdiwala, C. Ramasundarahettige, K. Ramakrishnana, Q. Ibrahim.
Central operations leads: D. Desai (PHRI), H. Truchon (Montreal Heart Institute), N. Tusevljak (Institute for Clinical Evaluative Sciences).
Cohort operations research personnel: K. McDonald (OHS), N. Noisel (CARTaGene), J. Chu (BCGP), J. Hicks (Atlantic Partnership for Tomorrow's Health), H. Whelan (Alberta Tomorrow Project), S. Rangarajan (PURE), D. Busseuil (MHI Biobank).
Site investigators and staff: (site112) J.Leipsic, S.Lear, V.deJong; (site 306) M. Noseworthy, K. Teo, E. Ramezani, N. Konyer; (site 402) P. Poirier, A-S. Bourlaud, E. Larose, K Bibeau; (site 512) J. Leipsic, S. Lear, V. deJong; (site 609) E. Smith, R. Frayne, A. Charlton, R. Sekhon; (site 703) A. Moody, V. Thayalasuthan; (site 704) A. Kripalani, G. Leung; (site 706) M. Noseworthy, S. Anand, R..deSouza, N. Konyer, S. Zafar; (site 707) G. Paraga, L. Reid; (site 714) A. Dick, F. Ahmad; (site 799) D. Kelton, H. Shah; (site 801) F. Marcotte, H. Poiffaut; (site 802) M. Friedrich, J. Lebel; (site 817) E. Larose, K. Bibeau; (site 913) R. Miller, L. Parker, D. Thompson, J. Hicks; (site 1001) J-C. Tardif, H. Poiffaut; (site1103) J. Tu, K. Chan, A. Moody, V. Thayalasuthan.
MRI working group and core lab investigators/staff: Chair: M. Friedrich; Brain Core Lab: E. Smith, C. McCreary, S.E. Black, C. Scott, S. Batool, F. Gao; Carotid Core Lab: A. Moody, V. Thayalasuthan; Abdomen: E. Larose, K. Bibeau; Cardiac: F. Marcotte, F. Henriques.
Contextual working group: R. de Souza, S. Anand, G. Booth, J. Brook, D. Corsi, L. Gauvin, S. Lear, F. Razak, S.V. Subramanian, J. Tu.
CAHHM Founding Advisory Group: Jean Rouleau, Pierre Boyle, Caroline Wong, Eldon Smith; CAHHM Scientific Review Board: Bob Reid, Ian Janssen, Amy Subar, Rhian Touyz.
Research Data
Data were harmonized by Maelstrom Research, and access policies and procedures were developed by the Centre of Genomics and Policy in collaboration with the cohorts.
The data set from this study is held securely in coded form at ICES. Although data-sharing agreements prohibit ICES from making the data set publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at www.ices.on.ca/DAS. The full data set creation plan and underlying analytic code are available from the authors upon request, with the understanding that the programs may rely upon coding templates or macros that are unique to ICES.
Funding Sources
This study was supported by the Canadian Institutes of Health Research–Foundation Scheme (grant no. FDN 143313) awarded to the Cardiovascular Health in Ambulatory Care Research Team (CANHEART). The Canadian Alliance for Healthy Hearts and Minds cohort study (CAHHM) was funded by the Canadian Partnership Against Cancer (CPAC), the Heart and Stroke Foundation of Canada (HSF-Canada), and the Canadian Institutes of Health Research (CIHR). This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC).
Financial contributions were also received from the PHRI and CIHR Foundation Grant no. FDN-143255 to S.S. Anand, and FDN 154317 to E.E.S. In-kind contributions were received from A.R.M. and S.E.B. from Sunnybrook Hospital, Toronto for MRI reading costs, and Bayer AG for provision of IV contrast. The Canadian Partnership for Tomorrow’s Health (CanPath, formerly The Canadian Partnership for Tomorrow Project) is funded by the Canadian Partnership Against Cancer, BC Cancer, Genome Quebec, Ontario Institute for Cancer Research, Alberta Health, and the Alberta Cancer Foundation. The PURE Study was funded by multiple sources. The Montreal Heart Institute Biobank is funded by Mr. André Desmarais and Mrs. France Chrétien-Desmarais and the Montreal Heart Institute Foundation. S.S.A. was supported by a Tier 1 Canada Research Chair in Ethnicity and Cardiovascular Disease and Heart and Stroke Foundation Chair in Population Health. P.A. was supported by a Ministry of Research and Innovation of Ontario Investigator Award. S.E.B. was supported by the Hurvitz Brain Sciences Research Program, Sunnybrook Research Institute, and the Department of Medicine, Sunnybrook Health Sciences Centre, University of Toronto. J.-C.T. holds the Tier 1 Canada Research Chair in Translational and Personalized Medicine, and the Université de Montréal Pfizer Endowed Research Chair in Atherosclerosis.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: ICES is an independent, non-profit research institute funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). As a prescribed entity under Ontario’s privacy legislation, ICES is authorized to collect and use healthcare data for the purposes of health system analysis, evaluation and decision support. Secure access to these data is governed by policies and procedures that are approved by the Information and Privacy Commissioner of Ontario. Research ethics board approval was obtained from each CAHHM-HSR participating centre, and all participants signed consent forms prior to beginning the study.
See page 608 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2020.07.013.
Supplementary Material
References
- 1.Tu J.V., Nardi L., Fang J. Canadian cardiovascular outcomes research: national trends in rates of death and hospital admissions related to myocardial infarction, heart failure and stroke 1994-2004. CMAJ. 2009;180:E118–E125. doi: 10.1503/cmaj.081197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anand S.S., Tu J.V., Awadalla P. Rationale, design and methods for Canadian alliance for healthy hearts and minds cohort study (CAHHM)—a Pan Canadian cohort study. BMC Public Health. 2016;16:650. doi: 10.1186/s12889-016-3310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.deSouza R.J., Arora R., Gauvin L. Development of an on-line interactive map to display environmental health assessments of Canadian communities: knowledge translation to support collaborations for health. J Cities Health. 2018;2:123–129. [Google Scholar]
- 4.Anand S.S., Tu J.V., Desai D. Cardiovascular risk scoring and magnetic resonance imaging detected subclinical cerebrovascular disease. Eur Heart J—Cardiovasc Imaging. 2020;21:692–700. doi: 10.1093/ehjci/jez226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anand S.S., Abonyi S., Arbour L. Canadian Alliance for Healthy Hearts and Minds: First Nations cohort study rationale and design. Prog Community Health Partnersh. 2018;12:55–64. doi: 10.1353/cpr.2018.0006. [DOI] [PubMed] [Google Scholar]
- 6.Dummer T.J.B., Awadalla P., Boileau C. The Canadian Partnership for Tomorrow Project: a pan-Canadian platform for research on chronic disease prevention. CMAJ. 2018;190:E710–E717. doi: 10.1503/cmaj.170292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Awadalla P., Boileau C., Payette Y. Cohort profile of the CARTaGENE study: Quebec’s population-based biobank for public health and personalized genomics. Int J Epi. 2013;42:1285–1299. doi: 10.1093/ije/dys160. [DOI] [PubMed] [Google Scholar]
- 8.Dhalla A., McDonald T.E., Gallagher R.P. Cohort profile: The British Columbia Generations Project (BCGP) Int J Epidemiol. 2019;48 doi: 10.1093/ije/dyy160. 377-8k. [DOI] [PubMed] [Google Scholar]
- 9.Sweeney E., Cui Y., DeClercq V. Cohort profile: The Atlantic Partnership for Tomorrow's Health (Atlantic PATH) Study. Int J Epidemiol. 2017;46 doi: 10.1093/ije/dyx124. 1762-3i. [DOI] [PubMed] [Google Scholar]
- 10.Ye M., Robson P.J., Eurich D.T. Cohort profile: Alberta’s Tomorrow Project. Int J Epidemiol. 2017;46 doi: 10.1093/ije/dyw256. 1097-8l. [DOI] [PubMed] [Google Scholar]
- 11.Teo K., Chow C.K., Vaz M. Am Heart J. 2009;158:1–7. doi: 10.1016/j.ahj.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 12.McGorrian C., Yusuf S., Islam S. Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART modifiable risk score. Eur Heart J. 2011;32:581–589. doi: 10.1093/eurheartj/ehq448. [DOI] [PubMed] [Google Scholar]
- 13.Statistics Canada. https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226&Item_Id=144171&lang=en Available at:
- 14.Statistics Canada Population estimates on July 1st, by age and sex. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501 Available at:
- 15.Statistics Canada Serving Canadians while Navigating a Path to Recovery. https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2017-summary/2017-detailed-tables.html#t2 Available at: Accessed June 17, 2020.
- 16.Diabetes Canada Diabetes in Canada. https://www.diabetes.ca/DiabetesCanadaWebsite/media/Advocacy-and-Policy/Backgrounder/2020_Backgrounder_Canada_English_FINAL.pdf Available at: Accessed June 17, 2020.
- 17.Tom Xu K. Usual source of care in preventative service use: a regular doctor versus a regular site. Health Serv Res. 2002;37:1509–1529. doi: 10.1111/1475-6773.10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Public Health Agency of Canada (PHAC) PHAC; 2018. Report from the Chronic Disease Surveillance System: Heart Disease in Canada.https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/diseases-conditions/report-heart-disease-canada-2018/pub1-eng.pd Available at: [Google Scholar]
- 19.Borugian M.J., Robson P., Fortier I. The Canadian Partnership for Tomorrow Project: building a pan-Canadian research platform for disease prevention. CMAJ. 2010;182:1197–1201. doi: 10.1503/cmaj.091540. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.