Abstract
Background
The aim of this systematic review is to assess if penalty-based pay-for-performance (P4P) programs are more effective in improving quality and cost outcomes compared to two other payment strategies (i.e., rewards and a combination of rewards and penalties) for surgical care in the United States. Penalty-based programs have gained in popularity because of their potential to motivate behavioral change more effectively than reward-based programs to improve quality of care. However, little is known about whether penalties are more effective than other strategies.
Materials and methods
A systematic literature review was conducted according to the PRISMA guideline to identify studies that evaluated the effects of P4P programs on quality and cost outcomes for surgical care. Five databases were used to search studies published from 2003 to March 1, 2020. Studies were selected based on the PRISMA guidelines. Methodological quality of individual studies was assessed based on ROBINS-I with GRADE approach.
Results
This review included 22 studies. Fifteen cross-sectional, 1 prospective cohort, 4 retrospective cohort, and 2 case-control studies were found. We identified 11 unique P4P programs: 5 used rewards, 3 used penalties, and 3 used a combination of rewards and penalties as a payment strategy. Five out of 10 studies reported positive effects of penalty-based programs, whereas evidence from studies evaluating P4P programs with a reward design or combination of rewards and penalties was little or null.
Conclusions
This review highlights that P4P programs with a penalty design could be more effective than programs using rewards or a combination of rewards and penalties to improve quality of surgical care.
Keywords: Pay-for-performance, Payment strategy, Quality, Cost, Value, Surgical care
Highlights
-
•
Evidence on the effectiveness of pay-for-performance programs in quality improvement is mixed.
-
•
Five out of 10 studies reported positive effects of penalty-based programs.
-
•
Evidence from studies evaluating P4P programs with a reward design or combination of rewards and penalties was little or null.
-
•
The increasing use of penalty-based pay-for-performance programs has the potential to improve surgical care quality.
-
•
Penalties may induce stronger provider and hospital behavioral change than other payment strategies.
1. Introduction
Over 17 million surgical procedures are performed at acute care hospitals in the United States annually, costing the nation approximately $400 billion per year and accounting for 30% of all health care spending and 50% of hospital costs [[1], [2], [3]]. Surgical complication rates can be as high as 17% depending on the procedure, with one study reporting increases in the costs of a patient stay of $6139–$17,850 [4]. One approach to improving surgical care quality and curbing cost are pay-for-performance (P4P) programs designed with the aim to incentivize providers and hospitals to deliver financially rewarding, high-quality care through linking payment strategies based on rewards or penalties to performance [[5], [6], [7]].
Numerous large-scale P4P programs have been launched by the Centers for Medicare and Medicaid Services (CMS) in inpatient settings over the past decade [8,9] and the number of P4P programs is rapidly expanding. While the greater focus of P4P has been on medical conditions, P4P programs are rapidly expanding in the surgical setting due to the strong potential for cost savings on post-operative care (e.g., complications, readmissions). Recently, programs using penalties have gained in popularity [10], because of their potential to affect behavioral change more effectively than reward-based programs. This is due to evidence showing that individuals, and perhaps organizations, tend to be more sensitive to losses than gains [11,12]. However, concerns exist that penalties could harm patients and hospitals by putting financial strain on those hospitals most in need of resources and care improvement [13]. The aim of this systematic review is to assess the current state of evidence on the impact of P4P penalty design on quality and cost outcomes for surgical care compared to two other payment strategies (i.e., reward and a combination of reward and penalty).
Despite the growth in penalty-based P4P programs, few studies have examined the effect of penalty designs compared to other types of payment designs. While several systematic reviews have examined the relationship between P4P program characteristics and their impact on rewards, such as optimal incentive levels and targets, little is known about how payment designs contribute to outcomes. The literature on P4P programs has grown considerably since the latest published systematic review (which searched through 2016) [14], and no studies have specifically focused on surgical care. Although most P4P programs initially targeted medical conditions (e.g., acute myocardial infarction and pneumonia), programs have expanded to target the surgical setting [15]. Given that surgery accounts for the highest inpatient costs with its high spending growth [16] and avoidable complication rates [17], it is important to understand whether penalties are more effective than other strategies in improving surgical care for patients, hospitals and health care delivery more broadly.
2. Methods
2.1. Protocol and registration
We developed a systematic review protocol in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Our study was registered in the Research Registry (registration number: reviewregistry944).
2.2. Systematic literature search
Five databases were used to conduct a systematic review of the effects of P4P payment design on the quality and cost of surgical care: PubMed, Embase, EconLit, the Database of Abstracts of Reviews of Effectiveness, and the Cochrane Database of Systematic Reviews. We supplemented this review with a Google Scholar search, reference list reviews, and a search for selected P4P researchers. Studies on P4P programs in hospitals gained attention over a decade ago [18]; therefore, the search was limited to studies published between 2003 and 2020, conducted on March 1, 2020. Multiple combinations of nine keywords—“pay for performance,” “financial,” “incentive,” “reward,” “bonus,” “penalty,” “reimburse,” “inpatient,” and “surgery”— were used to conduct literature searches in the selected databases. We used “OR” and “AND” as the search terms to include these keywords. We also used an advanced search combining a MeSH major topic, “reimbursement, incentive” and subheading “surgery” as well as a modified strategy employed in a 2014 RAND review of P4P publications [18] and a work by Milstein and Schreyoegg [7]. Using these strategies yielded more than 2800 articles from the five databases. The literature search terms used in each database and the corresponding results in detail are described in Table 1.
Table 1.
Search terms used in hospital setting pay-for-performance for surgical care literature review.
| Database/Searching Engine | Search Terms | Results |
|---|---|---|
| PubMed | (“pay for performance”[tiab] OR P4P[tiab] OR “pay for value”[tiab] OR “financial penalties” OR “financial incentive” OR ((bonus[tiab] OR reward[tiab] OR penalty[tiab] OR nonpayment[tiab]) AND (payment[tiab] OR reimburse*[tiab] OR incentive*[tiab] OR penalty*[tiab] OR nonpayment*[tiab]) AND (quality[tiab] OR value[tiab])) AND (hospital[tiab] OR inpatient[tiab]) AND (surgery[tiab] OR perioperative[tiab]) | 116 |
| Embase | ‘pay for performance':ab,ti OR p4p:ab,ti OR ′pay for value':ab,ti OR ‘nonpayment':ab,ti AND ′hospital patient’ AND [2003–2020]/py | 147 |
| EconLit | (ab(‘pay for performance’) OR ab(p4p) OR ab(incentive) OR ab(penalty) OR ab(nonpayment)) AND ab(inpatient) | 72 |
| DARE | ‘pay for performance’ and MeSH DESCRIPTOR Reimbursement, Incentive EXPLODE ALL TREES | 21 |
| CDSR | “pay for performance” in Title, Abstract, Keywords or “nonpayment” in Title, Abstract, Keywords or “incentive” in Title, Abstract, Keywords or “penalty” in Title, Abstract, Keywords and “inpatient” in Title, Abstract, Keywords, Publication Year from 2003 to 2020 | 73 |
| Selected P4P researcher search (PubMed & Google Scholar) | Researcher list: Andrew Ryan, Adams Dudley, Howard Beckman, Kathleen Curtin, Larry Casalino, Tim Doran, Ashish Jha, Laura Petersen, Martin Roland, Meredith Rosenthal, Eric Schneider, Rachel Werner, Cheryl Damberg |
2383 |
| •PubMed search term: (Last Name, First Name [Author]) •Google Scholar search term: allintitle: ‘pay for performance’ OR ‘hospital’; author: “First name Last name” |
||
| Other Sources | CMS, RAND, Commonwealth Fund, Kaiser Permanente, and Reference list review | 31 |
Note: DARE = Database of Abstracts of Reviews of Effectiveness. CDSR = Cochrane Database of Systematic Reviews, CMS = Centers for Medicare and Medicaid Services.
2.3. Study selection
Only studies that met all of the following criteria were included: (a) full text available in English, (b) published between 2003 and 2020, (c) evaluated P4P solely implemented in the hospital sector, (d) analyzed the effects of P4P for surgical care, (e) assessed a P4P that used a financial strategy targeting providers and hospitals (as opposed to targeting patients), and (f) demonstrated either quantitative or qualitative empirical analysis, or both.
The study selection process followed protocols under the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). One researcher (K.K.) conducted the database search, and two researchers (K.K. and U.M.) independently reviewed the titles and abstracts of all studies identified in the initial search and selected articles for the primary review following the selection criteria.
2.4. Data extraction and analysis
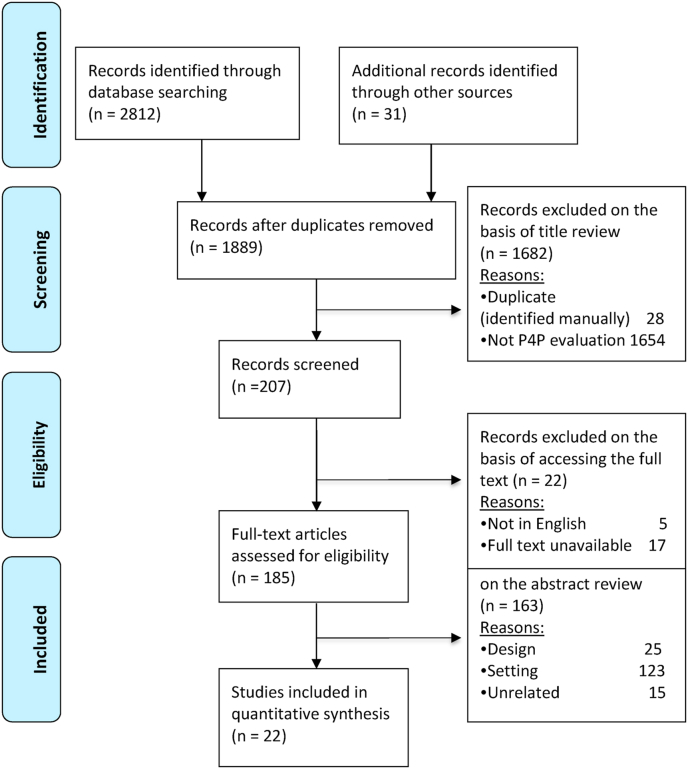
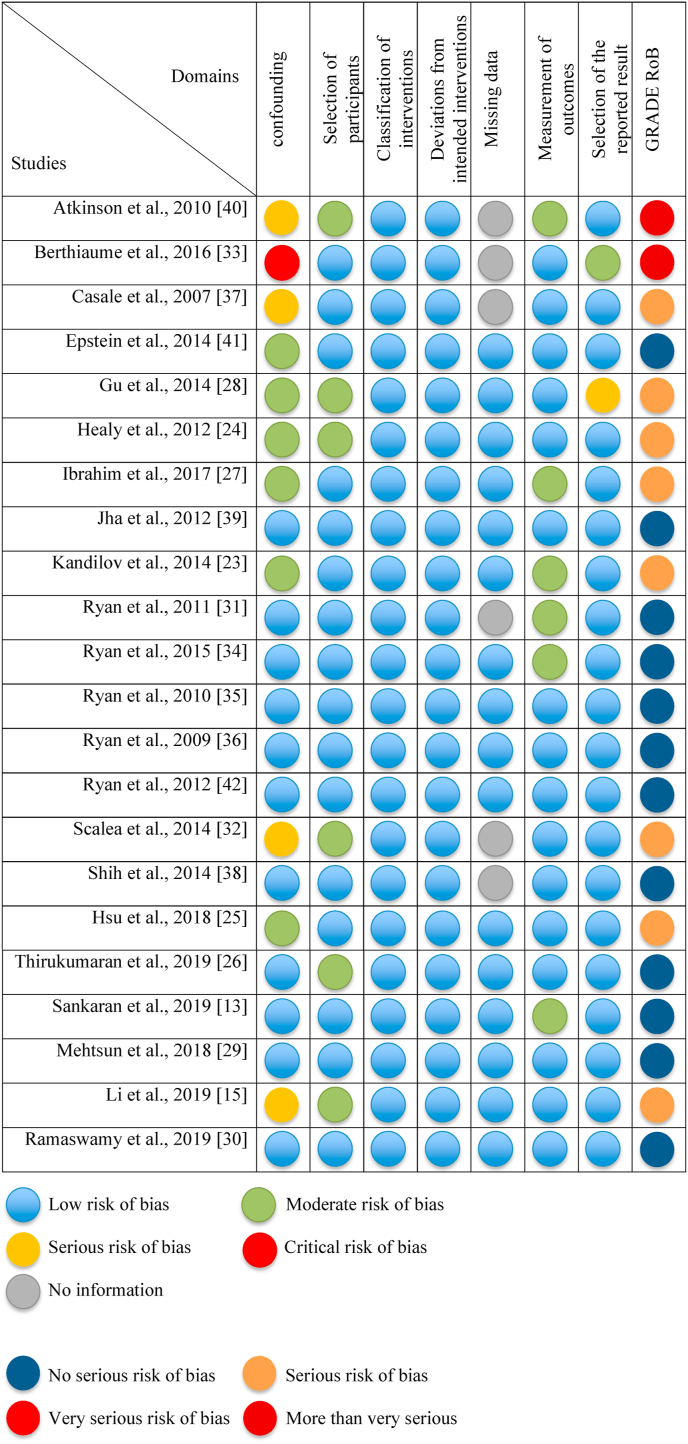
The full-text articles were obtained, and two researchers (K.K. and U.M.) independently reviewed all studies to determine eligibility for final inclusion in this review. Any disagreements were resolved by consensus. Any P4P programs that target surgical care and that are explicitly framed as reward, penalty, or combination of both in the United States were considered. The primary outcomes of interest were quality and cost because these outcomes directly demonstrate the ultimate outcome that matters to patients and society [19]. Fig. 1 presents the study selection process based on the PRISMA flow diagram [20]. The quality of the included studies was evaluated using the modified Oxford Centre for Evidence-Based Medicine [21]. We assessed the risk of bias using the risk of bias in non-randomized studies of interventions tool with GRADE approach [22] and summarized this in Fig. 2.
Fig. 1.
PRISMAa flow diagram for selected studies in the systematic literature review.
Fig. 2.
Risk of bias assessment of included studies using the risk of bias in non-randomized studies of interventions tool with GRADE approach.
3. Results
3.1. Characteristics of eligible studies
This review included 22 studies that met the inclusion criteria. The majority of the studies were published after 2010. The study population included inpatient surgical patients for the following procedures: coronary artery bypass graft [CABG] (ten studies), trauma (one study), bariatric surgery (two studies), orthopedic surgery (nine studies), vascular surgery (one study), obstetrics (one study), and general surgical care (five studies). Some studies evaluated more than one surgical procedure. Twelve studies included patients who underwent surgery for non-targeted conditions or patients in non-P4P program-participating hospitals as the control group. The other ten studies did not have a control group. Two studies used propensity score matching, eight a difference-in-differences (DD) or difference-in-difference-in-differences (DDD) design, two used the DD with a propensity score matched sample, four studies applied an interrupted time series analysis, and one used a regression discontinuity design. The average quality rating of the studies based on the Oxford Centre for Evidence-Based Medicine criteria was 3 (range 2–4), where level 2 studies represent those yielding the highest level of individual studies. We assessed that 12 (55%), 8 (36%), and 2 (9%) of the 22 studies had no serious, serious, and more than very serious risk of bias, respectively, mainly due to confounding factors and measurement of outcomes. (See S1 Table for an overview of studies analyzed, including sample, design, outcomes, results and other study characteristics).
3.2. Key features of the P4P programs
Key features of the P4P programs (i.e., program name, implementation year, target procedures, payment design, payment size, number of participating hospitals, and other important features) are presented in Table 2. Eleven specific P4P programs were included in this review. We classified P4P programs into three categories of payment design: penalties, rewards, and a combination of both. Three programs used penalties; five P4P programs used rewards; and three P4P programs used a combination of both. Six of 11 programs were initiated by CMS. The majority of targeted surgical procedures of P4P programs in the studies were CABG, hip fracture, THA, and TKA. Table 3 shows the summary characteristics of P4P programs included in this review, with substantial variability across programs. The majority of programs aimed at hospitals (n = 9, 82%). All Mandatory P4P programs were introduced by CMS. The first penalty-, reward-, and combination of reward and penalty programs were implemented in 2008, 2001, and 2004, respectively.
Table 2.
Key Features of P4P programs Targeted Surgical Care in the Systematic Review.
| P4P program | Ref# | Implement years & Other features | What to incentivize |
Who to incentivize |
How to incentivize |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome vs.Input | Specific vs.broad target conditions | Individual providers vs.hospital | Reward vs.penalty vs. withholding | Absolute vs.relative performance | Payment size | Voluntary vs. Mandatory | Numbers of participating hospitals | |||||||
| FIP | [32] | •Feb 2013 – Unclear (Results reported through Dec 2013) •A single hospital initiative |
Outcome | Trauma | Provider | Reward | Absolute | Certified registered nurse anesthetist: $100–200/2weeks Registered nurse: $50–120/2weeks Scrub technician: $40–80/2weeks |
Voluntary | 1 | ||||
| HAC-POA | [23, 24, 25, 26] |
•Q4 2008 – Present • CMS initiative • Claim basis |
Outcome | SSI following CABG, orthopedics (spine, neck, shoulder, elbow), and bariatric surgery, DVT &PE following THA or TKA | Hospital | Penalty | Absolute | No payment for hospital acquired conditions | Mandatory | 3203 (FY 2017) | ||||
| HACRP | [13] | • Q4 2014 – Present – Present • CMS initiative • Claim basis |
Outcome | Hospital-associated infections including surgical site infection following abdominal hysterectomy and colon procedures | Hospital | Penalty | Relative | 1% payment reduction | Mandatory | 3306 (FY 2017) | ||||
| HQSR | [33] | •2001 – Present •Payer initiative |
Process & Outcome | Surgical and obstetrical procedures | Hospital | Reward | Relative | Varies by hospitals (reward size depends on hospital's share of the total Hawaii Medical Service Association payout ($9 million in sum in 2004) | Voluntary | 17 | ||||
| HRRP | [15,[27], [28], [29], [30]] | •Q4 2012 – Present • CMS initiative • Payment adjustment to all Medicare discharges |
Outcome | THA, TKA, CABG |
Hospital | Penalty | Absolute | Up to 3% [Base DRG payment amount * readmissions adjustment factor] - Base operating DRG payment amount | Mandatory | 3129 (FY 2020) | ||||
| HVBP | [34] | • Q4 2012 – Present • CMS initiative • Budget neutral (all withheld monies are paid out as rewards) |
Process & Outcome | Surgical cases | Hospital | Withholding & Incentive |
Relative | 2% | Mandatory | 2955 (FY 2017) | ||||
| Long Island Provider Initiated P4P | [40] | •2004 – Present • Provider initiative |
Process & Outcome | Patient satisfaction, Patient safety, Hospital quality for conditions including, but are not limited to hip fracture, and other surgical procedures | Hospital | Reward & Penalty |
Relative | 50% of at-risk amount for each hospital | Voluntary | 10 | ||||
| Mass Health |
[31] | •FY 2008 – Present • MA State initiative • Medicaid patients • Greater incentive than PHQID |
Process & outcome (health disparity) | SSI | Hospital | Reward | Relative (1) Perform-ance above median performance of all hospitals (2)Top decile to earn maximum (3)Improve-ment from previous year |
$25,000,000 (Rate year 2017) If divided equally among the 66 hospitals, this allocation would have exceeded $370,000 per hospital |
Voluntary | 66 | ||||
| PHQID | Phase I [35,36] | •Phase I Q4 2004 – Q3 2006 • CMS initiative |
CABG, THA, TKA | Hospital | Reward | Relative | Reward (1) 2% for the top decile (2) 1% for the second decile |
Voluntary | 265 | |||||
| PHQID | Phase II [38, 39, 41, 42] |
•Phase II Q4 2006 – Q3 2009 • CMS initiative |
CABG, THA, TKA | Hospital | Reward & Penalty |
Relative | Reward (1) top 20% (2) composite score exceeded the median from all the participating hospitals two years prior to the current year (3) composite score exceeded the current year's median and in the top 20 percentile for improvement Penalty the lowest two deciles of performance in the third year |
Voluntary | 233 | |||||
| Proven care | [38] | • Feb 2006 – Present • Provider initiative |
Process | CABG, PCI, Cataract, THA, TKA, hip fracture, bariatric, and low back surgeries and perinatal | Provider | Reward | Absolute | 100% | Voluntary | 740 physicians at 3 hospitals and 40 primary care clinics covered by Geisinger Health Plan | ||||
Table 3.
Summary Characteristics of P4P Programs Included in the Systematic Review. Rows may not add to 100% due to the programs targeted multiple surgical procedures.
| Characteristics of P4P programs | No. of P4P programs/Total No. of P4P programs (%) |
|---|---|
| Payment Strategy | |
| Penaltiesa | 3/11 (27%) |
| Rewardsb | 5/11 (45%) |
| Combination of rewards and penaltiesc | 3/11 (27%) |
| Targeted Surgical Procedures | |
| All surgical procedures | 5/11 (45%) |
| Cardiac proceduresd | 4/11 (36%) |
| Orthopedic procedurese | 4/11 (36%) |
| Othersf | 2/11 (18%) |
| Targets | |
| Providers | 2/11 (18%) |
| Hospitals | 9/11 (82%) |
| Initiator | |
| Payerg | 7/11 (63%) |
| Hospital/Provider | 3/11 (27%) |
| State | 1/11 (9%) |
| Earliest Program Implementation years | |
| Penalty | 2008 |
| Reward | 2001 |
| Combination of reward and penalty | 2004 |
| Median (Interquartile range) | |
| Participating Hospitals | 233 (10–3129) |
Penalty-based programs included in this review are: hospital acquired conditions presented on admission, hospital acquired condition reduction program, and hospital readmission reduction program.
Reward-based programs are: financial incentive program, hospital quality service and recognition, MassHealth, the first phase of the premier hospital quality incentive demonstration (PHQID), and ProvenCare
Combination of rewards and penalty programs are: hospital value-based purchasing program, Long Island provider-initiated P4P, and the second phase of the PHQID.
Cardiac procedures include coronary artery bypass graft and percutaneous transluminal coronary angioplasty.
Orthopedic procedures include spine, shoulder, elbow, knee, hip, and trauma surgeries.
Others include trauma, vascular, and obstetrics procedures.
Payers include the Centers for Medicare & Medicaid Services and a private health insure.
Note: Surgical procedures are in italics. AMI: acute myocardial infarction, CABG: coronary artery bypass graft, CAUTI: catheter-associated urinary tract infections, CDI: clostridium difficile Infection, CHF: congestive heart failure, CLABSI: central line–associated bloodstream infections, DVT: deep vein thrombosis, CMS: Centers for Medicare and Medicaid Services, FIP: financial incentive program, HAC-POA: hospital acquired conditions presented on admission, FY: fiscal year, HACRP: hospital acquired condition reduction program, HQSR: hospital quality service and recognition, HRRP: hospital readmission reduction program, HVBP: hospital value-based purchasing program, MA: Massachusetts, MRSA: methicillin-resistant staphylococcus aureus, PCI: Percutaneous Coronary Intervention, PE: pulmonary embolism, PHQID: premier hospital quality incentive demonstration, PN: pneumonia, SSI: surgical site infection, THA: total hip arthroplasty, TKA: total knee arthroplasty, VCAI: vascular catheter-associated infections.
Effects of P4P programs on quality and cost of surgical care.
Twenty-one of the 22 studies evaluated quality outcomes associated with P4P programs using penalty (10), reward (7), or a combination of reward and penalty (4). Four of the 22 studies evaluated the cost of care related to P4P programs using penalty (1), reward (2), and the combination of both (1). Table 4 summarizes the number of studies by payment design of P4P programs (i.e., penalty, reward, or the combination of both) and the direction of effects (i.e., positive, negative, null, or mixed). The quality outcomes assessed in these P4P programs varied among studies and included mortality, readmissions, length of stay (LOS), number of procedures, number of complications, composite quality process score, operating room (OR) turnover time, and on-time start of the first surgery of the day. The cost outcomes evaluated in these programs include program operation costs, Medicare costs, and payments received by hospitals.
Table 4.
Summary of the effects of P4P programs included in the systematic review.
| Payment design |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Penalty |
Reward |
Combination of Reward and Penalty |
||||||||||
| Direction of Effect | Direction of Effect | Direction of Effect | ||||||||||
| Measurement of Effects of P4P programs | ↑ | ↓ | Ø | ↑↓ | ↑ | ↓ | Ø | ↑↓ | ↑ | ↓ | Ø | ↑↓ |
| No. of studies | No. of studies | No. of studies | ||||||||||
| Quality of Surgical Care | ||||||||||||
| Composite quality process score | 2 | 1 | ||||||||||
| Number of complications/Complication rates | 2 | 2 | 1 | 1 | ||||||||
| Length of stay | 1 | 2 | 1 | |||||||||
| Mortalitya | 1 | 1 | 2 | |||||||||
| Readmissionb | 3 | 2 | 1 | |||||||||
| Othersc | 2 | 1 | 1 | 1 | 1 | 1 | ||||||
| Cost of Surgical Cared | 1 | 1 | 1 | 1 | ||||||||
Mortality includes 30-day mortality and operative mortality.
Readmission include 30-day readmission, 90-day readmission, and readmission to ICU.
Others include operating room turnover time, operating room on time 1st case start, patient experience, access to care (i.e., number of patients who have undergone CABG procedure and the rate at which patients undergo CABG procedure), use of skilled nursing facilities, use of blood products, reintubation during hospital stay, total ventilation hours, percentage of hospitals that received incentives, and spillover effect to nontargeted procedures or other payers. These were grouped because only one study examined these outcomes.
The measures of surgical care cost include Medicare payment, hospital payment, physician payment, post-acute acre payment, home health agency payment, the program's potential savings, and payment received across incentivized conditions.
Multiple outcomes were evaluated in 12 out of 22 studies. Thus, the numbers may not sum to the total numbers of studies. ↑ indicates that the P4P improved the outcomes; ↓ indicates that the P4P worsened the outcomes; Ø indicates a null effect; and ↑↓ indicates inconsistent findings (i.e., some outcomes improved with the P4P, whereas others showed no improvement, or improvement was also reported in the control group in the same study) or that no conclusion can be drawn. See S2 Table for the references.
3.3. Quality of surgical care for penalty-based programs
Ten studies examined outcomes of penalty based P4P programs on the quality of surgical care [13,15,23] [[13], [15], [23], [24], [25], [26], [27], [28], [29], [30]] [[13], [15], [23], [24], [25], [26], [27], [28], [29], [30]], with the majority showing that penalty designs were effective [24,26,27,29,30]. Although six out of 10 studies reported improved quality in surgical care, we conclude that one study did not congruently show a positive effect of P4P programs due to lack of comparison to the pre-policy period [23]. Two studies observed a positive spillover effect of a penalty based P4P program for nontargeted procedures [27] or non-Medicare patients [24].
3.4. Quality of surgical care for reward-based programs
The seven studies evaluating the effect of P4P with reward design had mixed results [[31], [32], [33], [34], [35], [36], [37]]. Two of the seven studies found a significant effect of P4P implementation on at least one of the outcomes; one found a positive effect [32], while the other study found a negative effect [35]. Positive effects included reduced turnover time in the OR and improved on-time first case starts while negative effects included reduced access to surgical care for non-White, Black, or Hispanic cardiac patients. Two of the seven studies reported improvements related to P4P program implementation [33,37], but the results were based on the pre-post comparison or lacked details on statistical methods, and consequently no conclusion can be drawn.
3.5. Quality of surgical care for combined reward and penalty-based programs
The four studies that evaluated the effects of P4P with combined payment design did not show any significant results [[38], [39], [40], [41]]. Three of the studies that evaluated the PHQID, using reward payment in the first phase and a combined reward and penalty payment for the second phase, did not observe a significant improvement or a negative impact on patient outcomes [38,39,41]. The fourth study found a decreased LOS and an improved quality of care [40]. However, this study was descriptive, and no statistical significance was reported.
3.6. Cost of surgical care
Four of the 22 studies investigated the effect of P4P on the cost of surgical care using a penalty [23], reward [32,36], and the combination of reward and penalty [42]. One study evaluated a single hospital-initiated P4P program with a reward for providers and reported improved efficiency in the OR and estimated savings [32]. Three studies that examined CMS-initiated P4P programs reported mixed effects [23,36,42]. One of the three studies investigated P4P with rewards and found no evidence for a reduction in costs for CABG patients [36]. Another study consisted of a descriptive analysis of surgical care costs after implementation of the CMS P4P that utilizes a penalty design and was not a comparison of the pre- and post-implementation [23]. Therefore, this study did not provide evidence for improvement in the costs of care related to the P4P program. The other study compared the effect of a P4P payment program that used a combined reward and penalty design with different incentive sizes based on quality outcomes post implementation [42]. They found that hospitals with larger shares of socioeconomically disadvantaged patients received more incentives. However, this was due to an incentive size change that was introduced towards the later phase of the program, not due to a quality improvement. We conclude from these studies that evidence regarding the effects of P4P programs on cost is limited and remains largely unknown.
4. Discussion
This systematic review evaluated the effects of different P4P payment designs. We found mixed evidence on the effectiveness of P4P in quality improvement. However, with five out of 10 studies reporting positive effects of penalty-based programs, and studies evaluating P4P programs with a reward design or a combination of rewards and penalties showing little or null effects, penalty-based payment design emerged as a potentially more effective strategy than reward-based programs or programs using rewards and penalties in combination.
One explanation for why penalty-based P4P programs might be more effective than other designs is the tendency for people and organizations to respond to losses more than to gains, a behavior explained by the theory of loss aversion [43]. Supported by behavioral economics and psychology, this theory postulates that penalties may induce stronger provider and hospital motivation to improve quality. Subjecting hospitals to payment reductions on TKA, THA, and CABG alone, which are the most frequently targeted surgical procedures by P4P programs with over 1.5 million procedures performed annually [2], likely incentivizes change in behavior.
We found inter- and intra-program variations. Regarding inter-program variations within the same penalty-based payment design, the hospital readmission reduction program was shown to be more likely to have positive impacts on improving quality of care. This might be related to the penalty size. The hospital readmission reduction program imposes up to 3% penalties for each patient if hospitals have a higher number of 30-day readmissions for the targeted conditions, which has impacted 83% hospitals [44]. Intra-program variations were also found. Whereas some studies evaluated effects over at least 5 years and showed positive effects of the hospital readmission reduction program on decreasing readmissions, others evaluated the effects over a short period and found no significant effect. This suggests the importance of long-term program evaluation because it could take years for hospitals to change their practices and to observe improvements in quality [39].
Our review shows the small number of studies that have evaluated the impact of P4P on cost outcomes for surgical care, although one of the main purposes of P4P is cost reduction. One reason for the lack of studies focusing on cost outcomes could be an uneasiness in the United States to ration health care based on cost [45]. Some policymakers argue against using cost-effectiveness as a reason to cut expensive yet effective treatments [46]. The Patient-Centered Outcomes Research Institute [47] also prohibits the use of a dollar-per-quality-outcome measurement in establishing treatment recommendations [48]. Despite the ethical complexities of health care rationing that underline these recommendations, payers and many other policymakers have had a substantial interest in implementing P4P programs to curb vast health expenditures in resource-scarce settings [49].
With the continued growth of P4P programs utilizing penalties, the number of studies evaluating penalty-based P4P programs have increased. We did not find randomized controlled trials (RCTs), as RCTs are rarely used to evaluate P4P programs due to the high costs of RCTs [50]. However, recent studies have used advanced analytic methods, such as a DD or DDD model, interrupted time series, and propensity score matching, to overcome the limitations of observational data. These studies have produced robust results regarding the effects of P4P, which allowed us to conclude that penalty designs could improve the quality of surgical care more effectively than other payment designs. Future studies with methodologically rigorous designs are needed to verify the potential of penalty-based P4P programs over other types of payment design programs.
This review has three notable limitations. First, a meta-analysis could not be conducted because of the lack of studies evaluating the same outcomes. If future studies become available, a meta-analysis may be able to produce quantifiable summary data on the effectiveness of specific payment designs. Second, studies examined P4P programs with substantially varied design features, as described. The aim of this review was to evaluate the variation in quality and cost outcomes of surgical care as attributable to P4P payment designs, thus we compared findings across studies solely focused on the type of payment strategy and did not analyze heterogeneity across other features, such as incentive size and mandatory versus voluntary participation. Third, our findings may not be generalizable to all surgical procedures because the majority of studies examined P4P programs that targeted CABG, THA, or TKA only.
5. Conclusion
Results of this systematic review suggest that P4P programs utilizing penalties could be more effective than those utilizing rewards or a combination of both to improve the quality of surgical care. P4P has been used as a tool to improve quality at a reduced cost since the early 2000s and will likely function as an important policy tool for the foreseeable future. With the growing volume and high costs of surgical procedures, P4P initiatives are increasingly popular in surgical settings. Considering that over 4400 surgeries per 100,000 people are performed annually at acute care hospitals [2], the implications of improving surgical care quality are significant.
Funding/support
The research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
This is a review article and received an exemption of review.
Consent
n/a
Author contribution
K Kim: conceptualization, study design, data collection, data analysis, writing – original draft and review & editing.
W Max: conceptualization, study design, writing – review and editing.
J White: conceptualization, study design, writing – review and editing.
S Chapman: conceptualization, study design, writing – review and editing.
U Muench: conceptualization, study design, data analysis, writing – review and editing.
Registration of Research Studies
Name of the registry: Research Registry
Unique Identifying number or registration ID: reviewregistry944
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry#registryofsystematicreviewsmeta-analyses/registryofsystematicreviewsmeta-analysesdetails/5effa270994afe001534394b/
Guarantor
K Kim
U Muench
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2020.11.060.
Contributor Information
Kyung Mi Kim, Email: kyungkim@stanford.edu, kyungkim@stanford.edu.
Wendy Max, Email: wendy.max@ucsf.edu.
Justin S. White, Email: justin.white@ucsf.edu.
Susan A. Chapman, Email: susan.chapman@ucsf.edu.
Ulrike Muench, Email: ulrike.muench@ucsf.edu.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Muñoz E., Muñoz W., III, Wise L. National and surgical health care expenditures. 2005–2025: Ann. Surg. 2010;251:195–200. doi: 10.1097/SLA.0b013e3181cbcc9a. [DOI] [PubMed] [Google Scholar]
- 2.McDermott K.W., Freeman W.J., Elixhauser A. Agency for Healthcare Research and Quality; 2017. Overview of Operating Room Procedures during Inpatient Stays in U.S. Hospitals, 2014. [PubMed] [Google Scholar]
- 3.Steiner C.A., Karaca Z., Moore B.J., Imshaug M., Pickens G. 2014. Surgeries in Hospital-Based Ambulatory Surgery and Hospital Inpatient Settings. 2017. [PubMed] [Google Scholar]
- 4.Healy M.A., Mullard A.J., Campbell D.A., Dimick J.B. Hospital and payer costs associated with surgical complications. JAMA Surg. 2016;151:823. doi: 10.1001/jamasurg.2016.0773. [DOI] [PubMed] [Google Scholar]
- 5.Busse R. Pay-for-performance: time to act but also to provide further evidence. Health Pol. 2016;120:1123–1124. doi: 10.1016/j.healthpol.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Dudley R.A. Pay-for-performance research: how to learn what clinicians and policy makers need to know. J. Am. Med. Assoc. 2005;294:1821–1823. doi: 10.1001/jama.294.14.1821. [DOI] [PubMed] [Google Scholar]
- 7.Milstein R., Schreyoegg J. Pay for performance in the inpatient sector: a review of 34 P4P programs in 14 OECD countries. Health Pol. 2016;120:1125–1140. doi: 10.1016/j.healthpol.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Kondo K.K., Damberg C.L., Mendelson A., Motu’apuaka M., Freeman M., O'Neil M. Implementation processes and pay for performance in healthcare: a systematic review. J. Gen. Intern. Med. 2016;31:61–69. doi: 10.1007/s11606-015-3567-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryan A.M., Blustein J. Making the best of hospital pay for performance. N. Engl. J. Med. 2012;366:1557–1559. doi: 10.1056/NEJMp1202563. [DOI] [PubMed] [Google Scholar]
- 10.Kristensen S.R. Financial penalties for performance in health care. Health Econ. 2017;26:143–148. doi: 10.1002/hec.3463. [DOI] [PubMed] [Google Scholar]
- 11.Abdellaoui M., Bleichrodt H., Paraschiv C. Loss aversion under prospect theory: a parameter-free measurement. Manag. Sci. 2007;53:1659–1674. doi: 10.1287/mnsc.1070.0711. [DOI] [Google Scholar]
- 12.Rouyard T., Attema A., Baskerville R., Leal J., Gray A. Risk attitudes of people with ‘manageable’ chronic disease: an analysis under prospect theory. Soc. Sci. Med. 2018;214:144–153. doi: 10.1016/j.socscimed.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Sankaran R., Sukul D., Nuliyalu U., Gulseren B., Engler T.A., Arntson E. Changes in hospital safety following penalties in the US Hospital Acquired Condition Reduction Program: retrospective cohort study. BMJ. 2019 doi: 10.1136/bmj.l4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mendelson A., Kondo K., Damberg C., Low A., Motúapuaka M., Freeman M. The effects of pay-for-performance programs on health, health care use, and processes of care: a systematic review. Ann. Intern. Med. 2017;166:341. doi: 10.7326/M16-1881. [DOI] [PubMed] [Google Scholar]
- 15.Li B.Y., Urish K.L., Jacobs B.L., He C., Borza T., Qin Y. Inaugural readmission penalties for total hip and total knee arthroplasty procedures under the hospital readmissions reduction program. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.16008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.2017 reportHealth Care Cost and Utilization Report. Health Care Cost Institute; 2019.
- 17.Healey M.A., Shackford S.R., Osler T.M., Rogers F.B., Burns E. Complications in surgical patients. Arch. Surg. 2002;137:8. doi: 10.1001/archsurg.137.5.611. [DOI] [PubMed] [Google Scholar]
- 18.Damberg C.L., Sorbero M.E., Lovejoy S.L., Martsolf G.R., Raaen L., Mandel D. RAND Corporation; Santa Monica, CA: 2014. Measuring Success in Health Care Value-Based Purchasing Programs: Findings from an Environmental Scan, Literature Review, and Expert Panel Discussions. [PMC free article] [PubMed] [Google Scholar]
- 19.Porter M.E., Larsson S., Lee T.H. Standardizing patient outcomes measurement. N. Engl. J. Med. 2016;374:504–506. doi: 10.1056/NEJMp1511701. [DOI] [PubMed] [Google Scholar]
- 20.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 21.OCEBM Levels of Evidence Working Group. Oxford 2011 levels of evidence n.d.
- 22.Schünemann H.J., Cuello C., Akl E.A., Mustafa R.A., Meerpohl J.J., Thayer K. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. J. Clin. Epidemiol. 2019;111:105–114. doi: 10.1016/j.jclinepi.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kandilov A., Coomer N., Dalton K. The impact of hospital-acquired conditions on Medicare program payments. Medicare Medicaid Res. Rev. 2014;4:E1–E23. doi: 10.5600/mmrr.004.04.a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Healy D., Cromwell J. Centers for Medicare and Medicaid Services; 2012. Hospital-acquired Conditions – Present on Admission: Examination of Spillover Effects and Unintended Consequences. [Google Scholar]
- 25.Hsu H.E., Kawai A.T., Wang R., Jentzsch M.S., Rhee C., Horan K. The impact of the Medicaid healthcare-associated condition program on mediastinitis following coronary artery bypass graft. Infect. Control Hosp. Epidemiol. 2018;39:694–700. doi: 10.1017/ice.2018.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thirukumaran C.P., Glance L.G., Rosenthal M.B., Temkin-Greener H., Balkissoon R., Mesfin A. Impact of medicare's nonpayment program on venous thromboembolism following hip and knee replacements. Health Serv. Res. 2018;53:4381–4402. doi: 10.1111/1475-6773.13013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ibrahim A.M., Nathan H., Thumma J.R., Dimick J.B. Impact of the hospital readmission reduction program on surgical readmissions among medicare beneficiaries. Ann. Surg. 2017;266:617–624. doi: 10.1097/SLA.0000000000002368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gu Q., Koenig L., Faerberg J., Steinberg C.R., Vaz C., Wheatley M.P. The Medicare Hospital Readmissions Reduction Program: potential unintended consequences for hospitals serving vulnerable populations. Health Serv. Res. 2014;49:818–837. doi: 10.1111/1475-6773.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mehtsun W.T., Papanicolas I., Zheng J., Orav E.J., Lillemoe K.D., Jha A.K. National trends in readmission following inpatient surgery in the hospital readmissions reduction program era. Ann. Surg. 2018;267:599–605. doi: 10.1097/SLA.0000000000002350. [DOI] [PubMed] [Google Scholar]
- 30.Ramaswamy A., Marchese M., Cole A.P., Harmouch S., Friedlander D., Weissman J.S. Comparison of hospital readmission after total hip and total knee arthroplasty vs spinal surgery after implementation of the hospital readmissions reduction program. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.4634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ryan A.M., Blustein J. The effect of the MassHealth hospital pay-for-performance program on quality. Health Serv. Res. 2011;46:712–728. doi: 10.1111/j.1475-6773.2010.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scalea T.M., Carco D., Reece M., Fouche Y.L., Pollak A.N., Nagarkatti S.S. Effect of a novel financial incentive program on operating room efficiency. JAMA Surg. 2014;149:920–924. doi: 10.1001/jamasurg.2014.1233. [DOI] [PubMed] [Google Scholar]
- 33.Berthiaume J.T., Chung R.S., Ryskina K.L., Walsh J., Legorreta A.P. Aligning financial incentives with quality of care in the hospital setting. J. Health C Qual. 2006;28(36–44):51. doi: 10.1111/j.1945-1474.2006.tb00601.x. [DOI] [PubMed] [Google Scholar]
- 34.Ryan A.M., Burgess J.F.J., Pesko M.F., Borden W.B., Dimick J.B. The early effects of Medicare's mandatory hospital pay-for-performance program. Health Serv. Res. 2015;50:81–97. doi: 10.1111/1475-6773.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ryan A.M. Has pay-for-performance decreased access for minority patients? Health Serv. Res. 2010;45:6–23. doi: 10.1111/j.1475-6773.2009.01050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ryan A.M. Effects of the premier hospital quality incentive demonstration on Medicare patient mortality and cost. Health Serv. Res. 2009;44:821–842. doi: 10.1111/j.1475-6773.2009.00956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Casale A.S., Paulus R.A., Selna M.J., Doll M.C., Bothe A.E.J., McKinley K.E. “ProvenCareSM”: a provider-driven pay-for-performance program for acute episodic cardiac surgical care. Ann. Surg. 2007;246:613–621. doi: 10.1097/SLA.0b013e318155a996. discussion 621-623. [DOI] [PubMed] [Google Scholar]
- 38.Shih T., Nicholas L.H., Thumma J.R., Birkmeyer J.D., Dimick J.B. Does pay-for-performance improve surgical outcomes? An evaluation of phase 2 of the premier hospital quality incentive demonstration. Ann. Surg. 2014;259:677–681. doi: 10.1097/SLA.0000000000000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jha A.K., Joynt K.E., Orav E.J., Epstein A.M. The long-term effect of premier pay for performance on patient outcomes. N. Engl. J. Med. 2012;366:1606–1615. doi: 10.1056/NEJMsa1112351. [DOI] [PubMed] [Google Scholar]
- 40.Atkinson J.G., Masiulis K.E., Felgner L., Schumacher D.N. Provider-initiated pay-for-performance in a clinically integrated hospital network. J. Health C Qual. 2010;32:42–50. doi: 10.1111/j.1945-1474.2009.00063.x. quiz 50. [DOI] [PubMed] [Google Scholar]
- 41.Epstein A.M., Jha A.K., Orav E.J. The impact of pay-for-performance on quality of care for minority patients. Am. J. Manag. Care. 2014;20:e479–486. [PubMed] [Google Scholar]
- 42.Ryan A.M., Blustein J., Doran T., Michelow M.D., Casalino L.P. The effect of Phase 2 of the Premier Hospital Quality Incentive Demonstration on incentive payments to hospitals caring for disadvantaged patients. Health Serv. Res. 2012;47:1418–1436. doi: 10.1111/j.1475-6773.2012.01393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kahneman D., Tversky A. Choices, values, and frames. Am. Psychol. 1984;39:341–350. [Google Scholar]
- 44.Rau J. Kaiser Health News; 2019. New Round of Medicare Readmission Penalties Hits 2,583 Hospitals.https://khn.org/news/hospital-readmission-penalties-medicare-2583-hospitals/ accessed. [Google Scholar]
- 45.Kim J.J. The role of cost-effectiveness in US vaccination policy. N. Engl. J. Med. 2011;365:1760–1761. doi: 10.1056/NEJMp1110539. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein M.C., Skinner J.A. Comparative effectiveness and health care spending - implications for reform. N. Engl. J. Med. 2010;362:460–465. doi: 10.1056/NEJMsb0911104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patient-Centered Outcomes Research Institute. 2019. https://www.pcori.org/ accessed.
- 48.Social Security Administration O. 2018. Limitations on Certain Uses of Comparative Clinical Effectiveness Research.https://www.ssa.gov/OP_Home/ssact/title11/1182.htm accessed. [Google Scholar]
- 49.James J. Health Affairs; 2012. Health Policy Brief: Pay-For-Performance. [Google Scholar]
- 50.Mullen K., Frank R., Rosenthal M. Can you get what you pay for? Pay-for-performance and the quality of healthcare providers. Rand J. Econ. 2010;vol. 41:64–91. doi: 10.1111/j.1756-2171.2009.00090.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.