Abstract
Objectives
To assess physical activity (PA), mental health and well-being of adults in the United Kingdom (UK), Ireland, New Zealand and Australia during the initial stages of National governments’ Coronavirus disease (COVID-19) containment responses.
Design
Observational, cross-sectional.
Methods
An online survey was disseminated to adults (n = 8,425; 44.5 ± 14.8y) residing in the UK, Ireland, New Zealand and Australia within the first 2-6 weeks of government-mandated COVID-19 restrictions. Main outcome measures included: Stages of Change scale for exercise behaviour change; International Physical Activity Questionnaire (short-form); World Health Organisation-5 Well-being Index; and the Depression Anxiety and Stress Scale-9.
Results
Participants who reported a negative change in exercise behaviour from before initial COVID-19 restrictions to during the initial COVID-19 restrictions demonstrated poorer mental health and well-being compared to those demonstrating either a positive-or no change in their exercise behaviour (p < 0.001). Whilst women reported more positive changes in exercise behaviour, young people (18-29y) reported more negative changes (both p < 0.001). Individuals who had more positive exercise behaviours reported better mental health and well-being (p < 0.001). Although there were no differences in PA between countries, individuals in New Zealand reported better mental health and well-being (p < 0.001).
Conclusion
The initial COVID-19 restrictions have differentially impacted upon PA habits of individuals based upon their age and sex, and therefore have important implications for international policy and guideline recommendations. Public health interventions that encourage PA should target specific groups (e.g., men, young adults) who are most vulnerable to the negative effects of physical distancing and/or self-isolation.
Keywords: Coronavirus disease, pandemic, lifestyle behavior change, exercise, depression, sedentary time
1. Introduction
At the onset of the coronavirus disease 2019 (COVID-19) pandemic, governments in various countries implemented national containment strategies to limit the spread of the virus and reduce the risk of national healthcare systems becoming critically overburdened. Although physical distancing and self-isolation regulations aim to reduce person-to-person transmission of COVID-19, there are potentially significant public health implications from such measures. For example, a reduction in physical activity (PA) and an increase in sedentary behaviours may adversely affect immune function and enhance the risk for chronic health conditions.1
Physical activity is defined as any bodily movement produced by skeletal muscles that require energy expenditure, whereas exercise is a subcategory of PA that is planned, structured and repetitive, and aims to improve or maintain one or more components of physical fitness.2 Regular and adequate levels of PA is known for its beneficial effects on the immune system and for counteracting many comorbidities, such as obesity, diabetes, and mental health disorders.1, 3 Under non-pandemic circumstances, modern lifestyle behaviours encourage physical inactivity and sedentariness,4 but the evidence as to whether this is exacerbated by containment strategies during COVID-19 is still emerging. Physical inactivity is a term used to identify people who do not get the recommended level of regular PA,2 while sedentary behaviour is any waking behaviour characterized by an exergy expenditure ≤ 1.5 metabolic equivalents (METs, while in a sitting, reclining or lying position).5 Many opportunities to be physically active, such as participation in community- or hospital-based rehabilitation programmes, and use of fitness centres and public parks were prohibited or restricted for people of all ages as a result of the COVID-19 physical distancing and self-isolation directives. Indeed, recent research has shown a 29% increase in sitting time and more than a 30% decrease in PA during the initial stages of COVID-19 home confinement.6, 7, 8, 9 Furthermore, early COVID-19 reports from the United States of America (USA) suggested that individuals who did not meet recommended PA guidelines and engaged in greater screen time presented with higher depressive symptoms and stress than those who were more physically active.9 Due to the problematic psychological effects of containment and public health restrictions, engaging in regular PA throughout the duration of a pandemic may positively impact mental health and well-being.
Although containment strategies may have introduced new barriers to being physically active for some, a change in work and social patterns may have facilitated additional opportunities to engage in PA for others. For example, an increase in available time (e.g., reduced commute time) and access to various online platforms remotely delivering exercise classes (e.g., yoga/Pilates, high intensity interval training [HIIT]), may have provided individuals with opportunities to maintain or increase their PA during early COVID-19 restrictions. Indeed, despite strict government regulations in some countries, ‘daily exercise’ was one of the few reasons people could leave their homes and this may have been an incentive for some people to increase their PA.
While the types of COVID-19 restrictions implemented have been broadly similar globally, the timing and enforcement of these have differed considerably across countries. Differing government approaches likely contributed to the differences in COVID-19 infection and death rates, and may also have impacted on the behavioural, physical and mental health of individuals, in various countries. For example, a descriptive study with over 455,000 smartphone and app users from over 180 countries demonstrated regional differences in step counts within the first 30 days of the global declaration of the pandemic, likely reflecting the regional variation in COVID-19 timing, regional enforcement and behaviour change.8 Accordingly, the purpose of this study was to assess PA, mental health and well-being during initial COVID-19 restrictions between the United Kingdom [UK], Ireland [IRE], New Zealand [NZ], and Australia [AUS] populations. It was hypothesised that individuals who were physically active during COVID-19 restrictions would demonstrate better mental health and well-being than those who were not.
2. Methods
This study was designed to collect cross-sectional data using online surveys during the initial government-mandated COVID-19 containment strategies (April/May, 2020). The overall programme of research, which also includes longitudinal components, received institutional ethical approval from University’s leading the study in the UK, IRE, NZ and AUS. Research was conducted in accordance with the Declaration of Helsinki. This study adhered to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.10 Study funders had no influence over data collection, analysis and/or interpretation, or in article preparation.
Sampling commenced between 10 days and 6 weeks of initial government-mandated COVID-19 restrictions (Table S1). Convenience sampling using mass emailing via collaborating author networks, social media and mass media engagement (radio, newspapers), and snowball sampling, were used for recruitment. English speaking adults (≥18 y) who were residing in the surveyed countries were eligible to participate. All participants provided informed consent.
The survey was administered using JISC (Bristol, UK) or Qualtrics (London, UK). Participants self-reported demographic information and completed questionnaires relating to PA (the International Physical Activity Questionnaire: Short Form [IPAQ-SF]),11 exercise behaviour change (Stages of Change scale),12 mental health (Depression Anxiety and Stress Scale-9 [DASS-9]),13 and well-being (World Health Organisation-5 Well-being Index [WHO-5]),14 and described their weekly PA (i.e., type of PA) using free-text responses. All measures were assessed during the initial COVID-19 restrictions with the exception of the Stages of Change scale and PA free-text responses, which also captured pre-COVID-19 restriction information. In addition, participants reported whether they met recommended guidelines for daily PA (≥150 minutes of moderate- to vigorous intensity PA each week) before the COVID-19 restrictions were imposed.15
Participants self-reported their exercise behaviour before and during initial COVID-19 restrictions based on one of the following statements from the Stages of Change scale: i) I currently do not exercise and do not intend to start in the next 6 months; ii) I currently do not exercise but I am thinking about starting in the next 6 months; iii) I currently exercise a little but not regularly; iv) I currently exercise regularly but have begun doing so in the last 6 months; or v) I currently exercise regularly and have done so for more than 6 months. These statements correspond with the Pre-contemplation, Contemplation, Preparation, Action, and Maintenance Stages of Change of the Transtheoretical Model of Behaviour Change, respectively. Changes in exercise intentions and behaviours were reported as no change, positive change (increased rating from pre- to during COVID-19 restrictions), or negative change (decreased rating from pre- to during COVID-19 restrictions).
The IPAQ-SF allows individuals to recall the previous week’s PA (days per week, total minutes per day), with regards to walking, and moderate- and vigorous-intensity activities, and average daily sitting time. The IPAQ-SF is a valid (r = 0.67) and reliable tool (rho = 0.77-1.00)16 that is acceptable for assessing PA in large populations across various age groups (e.g., 18-70 y).11 For the IPAQ-SF, results were reported as a continuous variable (MET·min–1·week–1) and in categories (low-, moderate- or high-PA levels).17
This study used the DASS-9, an empirically derived version based on the DASS-21.13 The DASS-9 consists of three subscales (depression, anxiety and stress) with three items each. Each item is scored on a scale from 0 (none of the time) to 3 (most of the time). The three subscales of the DASS-9 were each cumulatively scored between 0 and 9, with higher scores demonstrating poorer mental health.
The WHO-5 is a short global rating scale that measures subjective well-being.14 The WHO-5 includes the following items: i) ‘I have felt cheerful and in good spirits', ii) ‘I have felt calm and relaxed', iii) ‘I have felt active and vigorous', iv) ‘I woke up feeling fresh and rested' and v) ‘My daily life has been filled with things that interest me'. Each of the five items were scored from 0 to 5. The total raw score was translated into a percentage ranging from 0 (absence of well-being) to 100 (maximal well-being).
Free-text PA was thematically-coded by collaborating authors based upon the Compendium of Physical Activity,17 accounting for the type of activity in which participants engaged. Data was aggregated into 13 higher level activity groupings (Table S2). “Online” activity was categorised, and included non-face-to-face activities (YouTube videos, Zoom, etc.). Coding was checked by JF and W’OB.
Statistical analysis was primarily descriptive, with proportions reported for binary and categorical variables and means and standard deviations or medians and interquartile ranges reported for continuous variables. Data was checked for the assumptions of normality and homoscedasticity. For the IPAQ-SF classification, between group differences were explored using chi-squared tests. To explore changes in PA levels, multinomial logit models were used. For WHO-5, DASS-9 and IPAQ-SF, multivariable linear regression obtained the independent effect of each characteristic on the outcome. For multinomial logit models and multivariable linear regression, age, gender and ethnicity were included as covariates to control for their independent effects. Spearman’s correlation coefficient (rho) was used to quantify the association between PA with mental health and well-being. Statistical analysis was completed on Stata (version 16).
3. Results
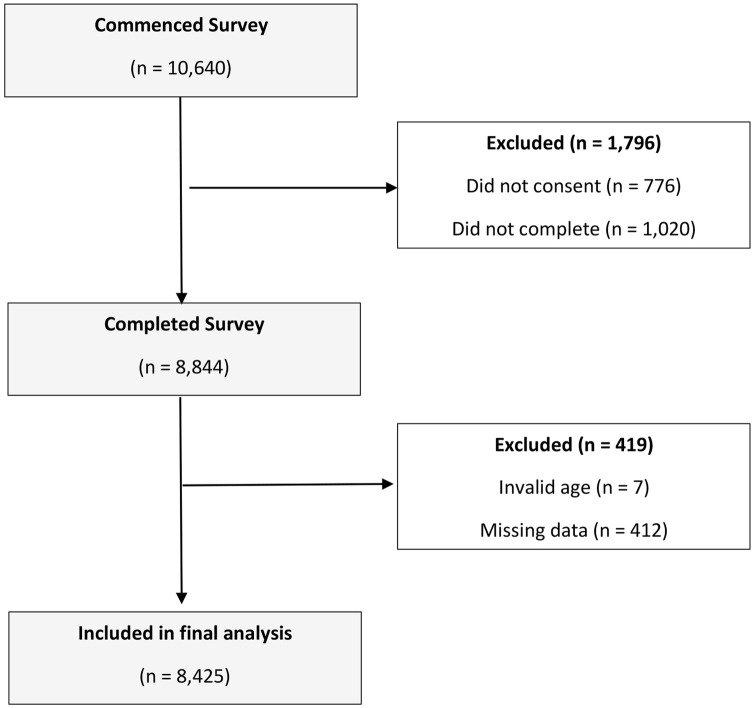
Of the 8,425 participants recruited (44.5 ± 14.8 y; 70.7% female; 93.8% white; see Table S3), 3,121 were residing in the UK, 4,007 in NZ, 903 in IRE and 394 in AUS (Figure S1). Only individuals who completed all survey items were included in the statistical analysis.
Fewer females met the recommended PA guidelines before initial COVID-19 restrictions compared to males (p < 0.001; 73% vs 81%, respectively; Table 1 ). During initial COVID-19 restrictions, there were no differences in PA between countries (p > 0.05; Table 1), although females engaged in less high-intensity PA than males (p < 0.001; 36% vs 41%, respectively), irrespective of country. Sitting time was lower for IRE compared to all other countries (p < 0.001), with no differences between the UK, NZ and AUS (p > 0.05). Depression, anxiety and stress were lower in NZ compared to UK, AUS and IRE (p < 0.001), whereas IRE reported higher scores than all other countries (p < 0.001; Table 1). Well-being was higher in NZ and AUS than the UK (p < 0.001), but there was no significant difference between the UK and IRE (p > 0.05; Table 1).
Table 1.
Pre- and during COVID-19 restrictions for physical activity instruments, WHO-5 and DASS
| UK | NZ | IRE | AUS | Total | ||
|---|---|---|---|---|---|---|
| Pre-COVID-19 restrictions | Met PA guidelines n (%) | |||||
| Males and females | 2,289 (73.3%) | 3,134 (78.2%) | 630 (69.7%) | 294 (74.4%) | 6,344 (75.3%) | |
| Males only | 816 (79.7%) | 901 (82.9%) | 182 (78.4%) | 72 (80.9%) | 1,971 (81%) | |
| Females only | 1,470 (70.2%) | 2,208 (76.5%) | 446 (66.7%) | 221 (72.7%) | 4,345 (73%)a | |
| Prefer not to say | 3 (100%) | 24 (70.6%) | 1 (100%) | 0 (0%) | 28 (68%) | |
| Stages of Change n (%) | ||||||
| 1. Precontemplation | 73 (2.3%) | 42 (1.1%) | 13 (1.4%) | 11 (2.8%) | 139 (1.7%) | |
| 2. Contemplation | 144 (4.6%) | 95 (2.4%) | 42 (4.7%) | 12 (3.1%) | 293 (3.5%) | |
| 3. Preparation | 519 (16.6%) | 735 (18.3%) | 187 (20.7%) | 59 (15.0%) | 1,500 (17.8%) | |
| 4. Action | 339 (10.9%) | 274 (6.8%) | 64 (7.1%) | 28 (7.1%) | 705 (8.4%) | |
| 5. Maintenance | 2046 (65.6%) | 2861 (71.4%) | 597 (66.1%) | 284 (72.1%) | 5,788 (68.7%) | |
| During COVID-19 restrictions | Stages of Change n (%) | |||||
| 1. Precontemplation | 57 (1.8%) | 31 (0.8%) | 14 (1.6%) | 1 (0.3%) | 103 (1.2%) | |
| 2. Contemplation | 195 (6.3%) | 131 (3.3%) | 45 (5.0%) | 36 (9.1%) | 407 (4.8%) | |
| 3. Preparation | 614 (19.7%) | 572 (14.3%) | 172 (19.1%) | 74 (18.8%) | 1,432 (17.0%) | |
| 4. Action | 533 (17.7%) | 699 (17.4%) | 176 (19.5%) | 54 (13.7%) | 1,482 (17.6%) | |
| 5. Maintenance | 1,702 (54.5%) | 2,574 (64.2%) | 496 (54.9%) | 229 (58.1%) | 5,001 (59.4%) | |
| IPAQ-SF | ||||||
| Total PA (MET·min–1·week–1) | 2,999 (2413) | 2,971 (2320) | 2,877 (2351) | 3,211 (2644) | 2,983 (2374) | |
| Sitting time (min) | 452 (220) | 450 (171) | 411 (177)b | 437 (167) | 446 (192) | |
| IPAQ-SF Classifications n (%) | ||||||
| Low | 283 (9.1%) | 305 (7.6%) | 80 (8.9%) | 39 (9.9%) | 707 (8.4%) | |
| Moderate | 1,649 (52.8%) | 2,181 (54.4%) | 497 (55.0%) | 194 (49.1%) | 4,521 (53.7%) | |
| High | 1,189 (38.1%) | 1,521 (38.0%) | 326 (36.1%) | 162 (41.0%) | 3,198 (37.9%) | |
| WHO-5 | ||||||
| WHO-5 score | 52.08 (21.77) | 57.78 (20.76)d | 53.06 (20.56) | 54.41 (20.77)d | 55.00 (21.28) | |
| DASS | ||||||
| Depression | 2.63 (2.23) | 2.05 (1.85)b | 2.89 (2.26)c | 2.42 (1.98) | 2.37 (2.07) | |
| Anxiety | 0.95 (1.62) | 0.56 (1.16)b | 1.13 (1.77)c | 0.88 (1.40) | 0.78 (1.44) | |
| Stress | 2.58 (2.10) | 1.95 (1.71)b | 2.79 (2.12)c | 2.62 (2.01) | 2.31 (1.95) | |
Significant difference between sex (p < 0001).
Significantly lower than all other countries (p < 0.001).
Significantly higher than all other countries (p < 0001).
Significantly higher than the UK (p < 0001).
Using combined data from all four countries, Spearman’s correlation coefficient (rho[95%CI]) demonstrated moderate positive correlations between PA and WHO-5 scores (rho = 0.35 [0.33, 0.37]; p < 0.001) and negative correlations between PA and depression (rho = -0.24 [-0.26,-0.22]; p < 0.001), anxiety (rho = -0.13 [-0.15,-0.11]; p < 0.001) and stress (rho = -0.13 [-0.14,-0.10] p < 0.001) during the initial COVID-19 restrictions. Longer sitting times were negatively correlated with the WHO-5 (rho = -0.20 [-0.22,-0.18]; p < 0.001), but positively correlated with depression (rho = 0.18 [0.16,0.20]), anxiety (rho = 0.08 [0.05,0.10]) and stress (rho = 0.08 [0.06,0.10]) (all p < 0.001).
The UK and AUS reported the greatest negative change in exercise behaviour (21.3% & 22.6% respectively; p < 0.001; Table S4). NZ demonstrated the least change in exercise behaviour during early COVID-19 restrictions (12.6%). Females reported more positive changes in their exercise behaviour compared to males (16.4% vs. 12.1%, respectively; p < 0.001; Table S5), while younger people (18-29 y) reported more negative changes (26.1%) than all other age groups (between 11.1% and 19.1%; p < 0.001; Table S5). Individuals with self-reported comorbidity were more likely to change their exercise behaviour than those without (p < 0.001), with a similar percentage reporting a positive (17.8%) or negative (17.3%) change in exercise behaviour. When adjusted for age, gender, and ethnicity, individuals who demonstrated a negative change in exercise behaviour had significantly higher DASS-9 scores and significantly lower WHO-5 scores compared to those who had either a positive change- or no change in their exercise behaviour (all p < 0.001; Table 2 ). Individuals who did not meet recommended guidelines for daily PA before COVID-19 restrictions were more likely to exhibit a positive change (74.1%) in their exercise behaviour during initial COVID-19 restrictions (Table S6).
Table 2.
Mean (SD) WHO-5 and DASS-9 scores for positive, negative and no change in exercise behaviours. Mean difference (± 95% CI) reported when comparing no change and positive exercise behaviour with negative change in exercise behavior.
| Negative change | No change |
Positive change |
|||
|---|---|---|---|---|---|
| x (SD) | x (SD) | Mean difference compared to negative change (95% CI) | x (SD) | Mean difference compared negative change (95% CI) | |
| WHO-5 score | 40.52 (19.97)a | 58.48 (20.45) | 16.2 (15.0, 17.3) | 55.53 (19.54) | 14.3 (12.9, 15.8) |
| DASS-9 | |||||
| Depression | 3.65 (2.39)b | 2.09 (1.89) | −1.3 (-1.5, -1.2) | 2.22 (1.94) | −1.3 (-1.5, -1.2) |
| Anxiety | 1.24 (1.85)b | 0.65 (1.30) | −0.5 (-0.5, -0.4) | 0.84 (1.44) | −0.3 (-0.4, -0.2) |
| Stress | 3.03 (2.21)b | 2.13 (1.85) | −0.7 (-0.8, -0.5) | 2.26 (1.92) | −0.7 (-0.8, -0.5) |
Significantly lower than either positive or no change in exercise behaviour (p < 0.001).
Significantly higher than positive or no change in exercise behaviour (p < 0001).
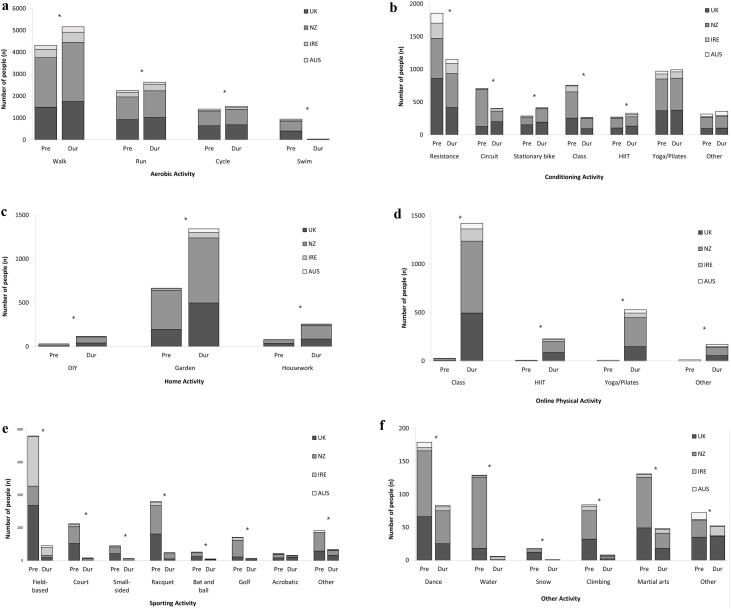
The type of PA participants engaged in before and during initial COVID-19 restrictions are presented in Fig. 1 and Tables S7 and S8.
Fig. 1.
Number of people taking part in activities before (pre) and during initial COVID-19 restrictions: 1a) Aerobic activities, 1b) Conditioning activities, 1c) Online activities, 1d) Home activities, 1e) Sporting activities, and 1f) Other activities.
*Significant difference between pre- and during COVID-19 restrictions (p < 0.001).
4. Discussion
This study demonstrated that individuals who had a negative change in their exercise behaviour between before and during initial COVID-19 restrictions reported poorer mental health and well-being; a relationship that was evident across all countries investigated. Whilst females reported more positive changes in exercise behaviour compared to males, younger adults reported more negative changes in exercise behaviour compared to all other age groups. Between countries, there were no differences in the amount of PA people engaged in during COVID-19 restrictions, however, there were differences in mental health and well-being, with those in NZ reporting better outcomes than those in the UK, IRE or AUS. These findings have important implications for policy and guideline recommendations to encourage people to be physically active, and thus promote better mental health and well-being, throughout the ongoing COVID-19 pandemic and the subsequent recovery period.
A potential implication of physical distancing is that poor lifestyle behaviours may be intensified, including decreases in PA and increases in sedentary behaviours.3 A large descriptive study with nearly 500,000 participants has demonstrated a 5.5% and 27.3% decrease in mean steps within 10 and 30 days, respectively, of the start of the COVID19 pandemic.8 In our study, the government containment strategies did allow for individuals to engage in differing daily PA and/or exercise, which afforded the opportunity for people to meet the recommended PA guidelines of 150 minutes of moderate to vigorous intensity PA each week. It is interesting to report that 74% of the study sample that exhibited a positive change in exercise behaviour were individuals who did not meet recommended PA guidelines before COVID-19 (Table S6). This suggests that during national containment responses to COVID-19, there are opportunities for individuals who do not normally partake in PA to instigate important changes in their behaviour to engage in exercise, which in-turn, could lead to long-term health benefits. Furthermore, in this study, individuals (83% of sample) who reported no change or a positive change in exercise behaviour from pre- to during COVID-19 restrictions reported better mental health (lower DASS-9 scores) compared to individuals who reported a negative change in their exercise behaviour. Similarly, individuals who reported a negative exercise behaviour change exhibited a substantially lower WHO-5 score compared to people who reported no changes (95%CI: 15.0 to 17.3 points lower) or a positive change (95%CI: 12.9 to 15.8 points lower) in exercise behaviour. As the threshold for a clinically relevant change on the WHO-5 is 10 points,18 these findings further substantiate the beneficial effects of PA on mental health and well-being.
During the initial COVID-19 restrictions, females engaged in less high-intensity PA (e.g., running, cycling, resistance exercises) than males, but more low-intensity activity (walking, yoga/Pilates; Table S6). More positive changes in exercise behaviour were also shown for females compared to males. In females, the largest increases were found for online exercise classes (0.4% vs. 21.2%, respectively) and online yoga/Pilates classes (0.1% vs. 8.2%, respectively). In contrast, for males, online exercise classes increased from 0.1% to 6.5%, and from 0% to 1.5% for online yoga/Pilates classes (for pre- and during COVID-19 restrictions, respectively). Self-efficacy, social support, and motivation are empirically substantiated factors that impact on PA levels among women more than men.19 Little is known, however, about the impact of this pandemic on these factors or even whether such influential factors are altered during a pandemic. Our longitudinal design will provide data to help explore the barriers, facilitators and adherence to PA for both females and males, as the COVID-19 pandemic continues across the globe
In line with our findings, a study with 1,854 young adult workers (21-40 y) in Singapore reported a 42% reduction in PA within 6 weeks of the global declaration of the COVID-19 pandemic.7 Furthermore, the least active group of their study sample comprised of younger and predominantly single individuals. In our study, individuals aged 18-29 years reported the largest negative change (26.1%) in exercise behaviour between before and during initial COVID-19 restrictions for all age groups assessed. Previous research has shown that individuals aged 16-34 years typically engage in more aerobic, strength, and sporting activities than people of an older age.20 In the current study, 18-29 year-olds engaged in less resistance-based exercise (35.2% vs. 19.4% for pre- and during COVID-19 restrictions, respectively) and sporting activities (23.8% vs. 3.6% for pre- and during COVID-19 restrictions, respectively), most likely due to the closure of gyms/fitness centres and the cancellation of all structured team and individual sporting activities (Fig. 1; Table S8). As re-commencing a previously broken PA habit can be challenging, in accordance with the ‘relapse’ stage of the Transtheoretical Model of Behaviour Change, the changes observed in this study when extrapolated to the general population could indeed be detrimental to long-term public health.
In our study, 17.8% of individuals with a self-reported chronic condition reported a positive change in their exercise behaviour between pre- and during early COVID-19 restrictions. Increases in PA may help mitigate the effects of COVID-19 on this subgroup of ‘higher risk’ individuals by boosting immune function, which is vital to control and eliminate COVID-19,21 and counteract prevalent comorbidities such as obesity, diabetes, hypertension and vascular conditions.3, 4 However, 17.3% of individuals with a self-reported chronic condition reported a negative change in their exercise behaviour. Indeed, a negative change may promote the development and/or progression of many chronic diseases, which may contribute to potentially poorer outcomes in those who contract COVID-19.2 Accordingly, individuals with comorbidity are an important group to consider when designing and delivering guideline recommendations to encourage PA during periods of physical distancing and self-isolation.
The World Health Organisation reports a higher prevalence of depressive and anxiety disorders in NZ (5.4%, 7.3%, respectively) and AUS (5.9%, 7.0%, respectively), compared to the UK (4.5%, 4.2%, respectively) or IRE (4.8%, 6.3%, respectively).22 In the present study, however, the NZ population demonstrated better mental health and well-being during COVID-19 restrictions than all other countries surveyed. In our study, a greater proportion of the NZ study population maintained their pre-COVID-19 exercise behaviour (72.2%) compared to the UK, IRE or AUS (63.7%, 65.3% and 64.2%, respectively). Furthermore, NZ demonstrated statistically fewer negative changes in exercise behaviour (12.6%) compared to the other countries surveyed (UK: 21.3%; IRE: 17.7%; AUS: 22.6%). It is widely accepted that PA is associated with a reduced risk of depression and anxiety.23, 24 A recent study in the USA demonstrated that reduced PA and increased screen time during the early COVID-19 restriction period were associated with poorer mental health outcomes.9 Similarly, our correlational findings demonstrated that longer sitting times were associated with poorer mental health and well-being. IRE reported the lowest daily sitting time but comparable PA levels to other countries, suggesting that participants in IRE may have been undertaking greater incidental PA. Despite incidental PA being suggested to have numerous practical and physiological health benefits,25 as well as potential to improve mood and well-being,26 in this study, IRE reported statistically poorer mental health compared to the other countries surveyed. It is plausible that the COVID-19 pandemic adds additional complexity to such a relationship, and further research into incidental PA and mental health is warranted.
The study findings should be contextualised in light of methodological limitations and strengths. The predominant ethnicity and sex of the respondents were white females which may not reflect the total population of the countries surveyed. Further investigation of the relationship between PA and mental health should consider that racial and/or ethnic disparities may impact the burden of COVID-19 related outcomes.27 Furthermore, 75% of participants reported meeting PA guidelines of engaging in ≥150 minutes of moderate- to vigorous intensity PA each week, which is higher than the population average of the countries surveyed.28, 29 Finally, our study did not capture the public health restrictions participants were following at the time the survey was completed (i.e., quarantine, physical distancing, social isolation). This would be a worthwhile line of investigation, particularly for older adults and extremely clinical vulnerable individuals, due to the variance in public health approaches nationally and globally. Strengths of this study include the sample size and the speed with which the surveys were implemented within all four countries. This ensured that the population response to the respective government-mandated containment strategies was captured at similar levels of restriction across all countries, and facilitated our planned longitudinal study design.
In countries where physical distancing (e.g., working from home) is likely to feature to a greater or lesser extent in the short- to medium-term, the potential impact of PA and changes in exercise behaviour on mental health and well-being is significant. Marginalizing PA during these uncertain times could have paramount negative implications for public health and thus attention must be paid to help promote and support people to engage in PA. Differing health promotion strategies may be required to facilitate engagement from specific groups (e.g., males, younger adults, individuals with comorbidity). These findings have important implications for policy and guideline recommendations and may assist in refining government strategies concerning physical distancing and self-isolation.
5. Conclusion
During early COVID-19 restrictions, a negative change in exercise behaviour compared to pre- COVID-19 restrictions was associated with poorer mental health and wellbeing. Whilst females reported more positive changes in exercise behaviour, young people (18-29 y) reported more negative changes. PA was comparable between the UK, NZ, IRE and AUS, however, people in NZ reported better mental health and well-being. Our findings will assist in the development of targeted interventions to encourage greater PA participation while individuals continue to physical distance, self-isolate, or ‘work from home’ for extended periods. Due to the uncertainty surrounding the long-term effects of the COVID-19 pandemic, longitudinal studies are needed to explore the relationships between PA and mental health and well-being.
Practical implications
-
•
During the COVID-19 pandemic and recovery period, physical activity should be encouraged to promote better mental health and well-being.
-
•
These findings have important implications for policy and guideline recommendations, particularly for males, younger adults and individuals with co-morbidities.
-
•
Our findings will assist in the development of targeted interventions to encourage greater PA participation while individuals continue to physical distance, self-isolate, or ‘work from home’ for extended periods.
Author Contributors
JF, DL, JB, W’OB, BM and DW designed the study. All authors contributed to survey dissemination and preliminary data preparation. BS analysed the data. JF and DL wrote the main draft of the manuscript and all authors contributed to manuscript revision and approved the final version.
Ethical approval
The overall program of research received institutional ethical approval in the UK (Faculty of Health and Wellbeing Ethics Committee, University of Winchester, UK; HWB/REC/20/04), Ireland (Dublin City University Research Ethics Committee; DCUREC/2020/089), New Zealand (Massey University Human Ethics Committee; 4000022445) and Australia (University of the Sunshine Coast Human Research Ethics Committee; A201381).
Transparency statement
JF confirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned (and, if relevant, registered) have been explained.
Funding
Research and statistical funding support was provided by the Institute for Life Sciences, and Higher Education Innovation Fund, University of Southampton, UK.
Competing interests
None to declare
Data Sharing
Data are available upon request.
Acknowledgements
Due to the journals Double Blind Peer Review policy, details of the ethical approval, funding and author contributors are presented on the uploaded Title Page (with author details) file.
There are no further acknowledgements to include.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jsams.2020.11.016.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Sallis J.F., Adlakha D., Oyeyemi A., et al. An international physical activity and public health research agenda to inform coronavirus disease-19 policies and practices. J Sport Health Sci. 2020;9:328–334. doi: 10.1016/j.jshs.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. Physical Activity. Available from: https://www.who.int/health-topics/physical-activity#tab=tab_1 [Accessed 24th October 2020].
- 3.Woods J., Hutchinson N.T., Powers S.K., et al. The COVID-19 Pandemic and physical activity. Sport Med Health Sci. 2020;2:55–64. doi: 10.1016/j.smhs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Narici M., De Vito G., Franchi M., et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur J Sport Sci. 2020;12:1–22. doi: 10.1080/17461391.2020.1761076. [DOI] [PubMed] [Google Scholar]
- 5.Tremblay M.S., Aubert S., Barnes J.D., et al. SBRN Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ammar A., Brach M., Trabelsi K., et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ong J.L., Lau T., Massar S.A.A., Chong Z.T., Ng B.K.L., Koek D., Zhao W., Yeo B.T., Cheong B.K.L., Chee M.W.L. COVID-19-related mobility reduction: heterogenous effects on sleep and physical activity rhythms. Sleep. 2020 doi: 10.1093/sleep/zsaa179. zsaa179. Available from: https://doi.org/10.1093/sleep/zsaa179 [Accessed 24th October 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tison G.H., Avram R., Kuhar P., Marcus G.M., Pletcher M.J., Olgin J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Annals of Internal Medicine. 2020 doi: 10.7326/M20-2665. Available from: https://doi.org/10.7326/M20-2665 [Accessed 24th October 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meyer J., McDowell C., Lansing J., et al. Changes in physical activity and sedentary behaviour due to the COVID-19 outbreak and associations with mental health in 3,052 US adults. Int J Environ Res Public Health. 2020;17:6469. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 11.The International Physical Activity Questionnaire . 2005. Guidelines for Data Processing and Analysis of the International Physical Activity (IPAQ) [Internet]http://www.ipaq.ki.se Available from: [Google Scholar]
- 12.Beiner L., Abrams D.B. The contemplation ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- 13.Youssof M.S.B. Psychometric Properties of the Depression Anxiety Stress Scale in a Sample of Medical Degree Applicants. Int Med J. 2013;20:295–300. [Google Scholar]
- 14.Topp C.W., Østergaard S.D., Søndergaard S., et al. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother Psychosom. 2015;84:167–176. doi: 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- 15.Piercy K.L., Troiano R.P., Ballard R.M., et al. The physical activity guidelines for Americans. JAMA. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Craig C.L., Marshall A.L., Sjostrom M., et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2011;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 17.Ainsworth B.E., Haskell W.L., Herrmann S.D., et al. Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 18.Bech P., Lunde M., Bech-Andersen G., et al. Psychiatric outcome studies (POS): does treatment help the patients? A Popperian approach to research in clinical psychiatry. Nord J Psychiatry. 2007;61:4–34. doi: 10.1080/08039480601151238. [DOI] [PubMed] [Google Scholar]
- 19.Edwards E.S., Sackett S.C. Psychosocial Variables Related to Why Women are Less Active than Men and Related Health Implications. Clinical Medicine Insights: Women’s Health. 2016;S1:47–56. doi: 10.4137/CMWH.S34668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.NHS Digital. Health Survey for England . 2016. physical activity in adults. Available from: http://healthsurvey.hscic.gov.uk/media/63730/HSE16-Adult-phy-act.pdf [Accessed1st July 2020] [Google Scholar]
- 21.Nieman D.C. Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society. J Sport Health Sci. 2020;9:293–301. doi: 10.1016/j.jshs.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organisation . World Health Organisation; Geneva: 2017. Depression and other common mental disorders: Global Health estimates. License: CC BY-NC-SA 3.0 IGO. Available From: https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/ [Accessed 20th June 2020] [Google Scholar]
- 23.Schuch F.B., Vancampfort D., Firth J., Rosenbaum S., Ward P.B., Silva E.S., Hallgren M., Ponce De Leon A., Dunn A.L., Deslandes A.C., Fleck M.P. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175:631–648. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- 24.McDowell C.P., Dishman R.K., Gordon B.R., Herring M.P. Physical activity and anxiety: a systematic review and meta-analysis of prospective cohort studies. Am J Prev Med. 2019;57:545–556. doi: 10.1016/j.amepre.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 25.Stamatakis E., Johnson N.A., Powell L., et al. Short and sporadic bouts in the 2018 US physical activity guidelines: is high intensity incidental physical activity the new HIIT? Br J Sports Med. 2019;53:1137–1139. doi: 10.1136/bjsports-2018-100397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teychenne M., White R.L., Richards J., et al. Do we need physical activity guidelines for mental health: What does the evidence tell us? Ment Health Phys. 2020;18 [Google Scholar]
- 27.Hooper M.W., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial / ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ministry of Health. Annual Data Explorer 2018/19: New Zealand health survey [Data File]. Available from: https://minhealthnz.shinyapps.io/nz-health-survey-2018-19-annual-data-explorer/ [Accessed 1st July 2020].
- 29.NHS Digital (Great Britain). Statistics on obesity, physical activity and diet, England, 2019: Main report. Dandy Booksellers Limited. Available from: https://digital.N.H.S.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2019 [Accessed 1st July 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.