Abstract
Early reports suggest that lockdown measures associated with the COVID-19 pandemic (e.g., social distancing) are having adverse consequences for people's mental health, including increases in maladaptive eating habits and body dissatisfaction. Certain groups, such as those with pre-existing mental health difficulties, may be especially at risk. The current study explored perceived changes in eating, exercise, and body image during lockdown within the United Kingdom, using an online survey (n = 264). There were large individual differences in perceived changes in eating, exercise, and body image in this period. Women were more likely than men to report increasing struggles with regulating eating, preoccupation with food and worsening body image. Those with a current/past diagnosis of eating disorders reported significantly greater difficulties in regulating eating, increased preoccupation with food, exercise thoughts and behaviours and concern about appearance, even when compared to those with other mental health and developmental disorders. Ongoing research to explore individual differences in the trajectories of change in eating, exercise and body image as lockdown measures ease will be important for understanding the full psychological impact of this pandemic and improve service and public health planning going forward.
Keywords: COVID-19, Eating disorders, Body image, Eating behaviour, Exercise, Survey
1. Background
In January 2020 the World Health Organisation declared Coronavirus disease 2019 (COVID-19) a Public Health Emergency of International Concern. The combination of significant morbidity and rapid spread of the virus has led to unprecedented public health measures on an international scale, resulting in significant restrictions to daily life. A high proportion of countries have implemented “lockdown”, involving restrictions on travel, social interaction and prohibition of public gatherings and social events. In the United Kingdom (UK) lockdown measures were imposed on March 26, 2020. This involved a “stay at home” directive where people were asked to only leave their home for essential purposes (e.g., keyworker roles, medical needs, to care for others, one form of exercise a day, and essential food purchases). This was accompanied by advice on “social distancing”, where people were required to maintain a distance of =two metres from each other, and “shielding” of physically vulnerable individuals by minimising social interaction with them. While essential to prevent transmission of the virus, evidence of a negative impact of these restrictions on mental health is emerging. The Institute of Fiscal Studies analysed longitudinal data and found a substantial deterioration in mental health during the period of COVD-19 lockdown in the UK, with women, young people and those with pre-existing mental health difficulties particularly affected (Banks & Xu, 2020). Furthermore, The UCL Covid-Social Study found that anxiety symptoms in the UK sample decreased after lockdown measures were implemented while depression scores rose, and that both anxiety and depression symptoms started to reduce further after lockdown began to ease (Fancourt, Bu, Mak, & Steptoe, 2020).
Due to the restrictions placed on people's movements, and changes to the accessibility of food throughout the day, lockdown may significantly influence people's eating habits, exercise behaviours, and body image. Some researchers have expressed concern about the potential for lockdown measures to increase sedentary behaviours and irregular eating patterns in the general population (Di Renzo et al., 2020; Naja & Hamadeh, 2020). At the same time, other researchers have voiced concern about the potential impact on vulnerable individuals, including those with pre-existing mental health difficulties (Holmes et al., 2020), and the development or exacerbation of pre-existing, eating disorder psychopathology (Touyz, Lacey, & Hay, 2020; Weissman, Bauer, & Thomas, 2020). Collective anxiety about weight gain during lockdown, and stigmatizing media messages about the dangers of higher body weight, might contribute to increased body shame and levels of disordered eating, especially in vulnerable populations such as those with a current or historic eating disorder.
Rodgers et al. (2020) outlined three potential pathways through which eating disorder symptomatology might develop or be exacerbated in those with existing difficulties during the pandemic. The first pathway suggests that disruptions to daily routines and restrictions to activities (e.g., limited exercise, grocery shopping and food insecurity, social distancing and/or isolation, reduced access to treatment or alternative coping strategies, irregular sleep) might increase eating disorder psychopathology. In the second pathway, increased consumption of media (particularly social media) due to social distancing measures could contribute to increased eating disorder psychopathology. This is through increased exposure to harmful eating and appearance-related content, as well as more general stressful or traumatic world events. The final pathway proposes that the fear of contagion may increase levels of stress and orthorexia-based cognitions, and subsequently increase the risk of disordered eating behaviours. Other authors also highlight the potential impact of food insecurity including financial ability to purchase binge foods (Touyz et al., 2020) and vulnerability to increased binge episodes as a result of stockpiling or hoarding food (Cooper et al., 2020; Termorshuizen et al., 2020). Recent findings of the You-COPE study also highlight the potential for emotional overeating, where one in two 16–24 year olds reported overeating in response to their mood during lockdown (Pascual-Sanchez et al., 2020).
Data from non-clinical samples suggest that people commonly perceive changes to their eating and exercise behaviours during lockdown. In a survey of over 3500 respondents during Italian lockdown (Di Renzo et al., 2020), more than half of the participants reported a change in their hunger and satiety perception (17% reporting reduced appetite, 34% increased appetite) and most participants reported a change in their consumption of “healthy” foods during lockdown (37% reported eating more, and 36% eating less). Despite this, 48% of the sample perceived that they had gained weight during lockdown. There was no significant change in activity levels during lockdown for participants who reported that they did not engage in any exercise before; however, for participants who already engaged in exercise, the frequency of training increased during lockdown. Notably, the percentage of participants that reported engaging in high levels of exercise (at least five times per week) significantly increased from 6% before lockdown to 16% during lockdown. A recent large-scale Australian survey (Phillipou et al., 2020) saw variations in exercise behaviours, with 35% of the general population sample (n = 5289) reporting more exercise than before the pandemic, but almost half (43%) reporting less exercise. Therefore, there is clear evidence that lockdown has impacted on perceived changes in eating and exercise behaviours internationally in the general population. However, individual differences in response suggest a more complex picture than that perceived and communicated by the media.
There is also preliminary evidence of an increase in disordered eating. In the Australian survey by Phillipou et al. (2020), the majority of the general population reported no change in disordered eating during lockdown; however, 27% reported a greater level of food restriction than before COVID-19 and 34% reported increased binge eating behaviours, despite reporting no previous eating disorder history. In a small-scale study from Spain (Fernández-Aranda et al., 2020), one third of individuals with an eating disorder reported a deterioration in eating disorder symptoms. Similarly, a significant proportion of people with an eating disorder (n = 180) within the Australian study reported an exacerbation of restricting, binge eating, purging and exercise behaviours, relative to before COVID-19 (Phillipou et al., 2020). Therefore, there is some evidence to suggest that eating disorder psychopathology may worsen in people with eating disorders, alongside the potential development of disordered eating behaviours within the general population. Further evidence is required to determine who is at most risk for these changes.
The aim of the current study was therefore to explore the perceived impact of the COVID-19 related lockdown in the UK on people's eating, exercise and body image. Specifically, we explored the following research questions (RQ):
-
1.
To what extent do people perceive changes in being able to regulate eating, preoccupation with food, exercise behaviour, thinking about exercise and appearance concerns during lockdown?
-
2.
Do these perceived changes vary by gender, age group, living circumstances, and pre-existing mental health conditions and developmental disorders, including eating disorders?
-
3.
To what extent are perceived changes in eating, exercise and body image associated with psychological distress?
2. Methods
2.1. Study design
The current study draws on data collected as part of an ongoing longitudinal survey exploring the impact of COVID-19 on eating, exercise and body image.
2.2. Participants
Adults (18 years or older) living in the UK were invited to take part in a study on the impact of lockdown on body image and eating behaviours. Participants were recruited online between May and June 2020 using advertisements shared on social media by the research team. Additionally, a Facebook targeted advertisement was run for one week (June 15–22) in attempt to increase the number of male participants. A total of 404 unique respondents entered the survey between 11th May and 26th June 2020. Of these, 87 did not consent to take part and four were not living in the UK. From the remaining 313, we only used data from those who had answered the set of questions about how they had been affected by the COVID-19 lockdown. This gave a total of 264 respondents for this study.
2.3. Measures
2.3.1. Demographic information
Participants were asked to provide a range of demographics including their age, gender (man, woman, other), ethnicity (White; Black, African, Caribbean, Black British; Asian, Asian British; mixed/multiple ethnic groups; other), and education level (secondary school or equivalent, college/vocational training/apprenticeship; undergraduate degree, postgraduate degree, other). For analysis, age was categorised into <30 years vs. 30+ years to capture potential differences for participants during the period of emerging adulthood, which is often operationalised as 18 years to mid-late 20s (Arnett, 2000).
Additionally, in relation to COVID-19 specific circumstances, participants were asked to indicate their current country of residence (England, Scotland, Wales, Northern Ireland, other), and current living arrangements (living alone, living with family, living with friend/s, living with romantic partner/s, living with roommate/s, living with stranger/acquaintances in short-term/temporary housing, other).
2.3.2. Mental health and developmental disorder history
Participants were asked several questions about mental health diagnoses. First, they were asked if they had ever been diagnosed with an eating disorder, another mental health disorder, or developmental disorder (yes, no, I'm not sure). Where participants indicated that they had an eating disorder diagnosis, mental health or developmental disorder diagnosis, they were also asked to specify the diagnosis.
2.3.3. Perceived changes in eating, exercise and body image
As participants' eating attitudes and behaviour, exercise behaviours and body image were unknown before the UK lockdown, we developed a measure to capture perceived changes in behaviour specifically for this study. The measure consisted of nine statements set in the timeframe of ‘since the lockdown began’. Five of these items are the focus of the current study: “I have found it more difficult to regulate or control my eating”; “I have become more preoccupied with food/eating”; “I have been exercising more”, “I have been thinking about exercise more”, and “I've been more concerned about the way that I look”.1 All questions were answered using a 5-point Likert scale, from strongly disagree (1) to strongly agree (5).
2.3.4. Psychological distress
Psychological distress was captured using the 4-item version of the Patient Health Questionnaire (PHQ-4) (Kroenke, Spitzer, Williams, & Löwe, 2009). This measure asks about symptoms of anxiety and depression in the past 2 weeks. The total score is a composite of the 4 items, with a possible range of 0–12. The PHQ-4 has demonstrated excellent psychometric properties in both clinical samples and the general population (Kroenke et al., 2009; Löwe et al., 2010).
2.4. Procedure
The project received ethical approval from the University of Edinburgh (Ref: STAFF181, 05/06/20). The survey was hosted online using Qualtrics, to which participants were directed through a link on the study advertisements. After following the link, participants were presented with further information about the study aims, use of their data and their rights. Participants were required to consent to take part before entering the main body of the survey. In this main part of the survey, participants were asked to provide demographic information, to complete a range of standardised measures related to dieting, disordered eating and mood, as well as perceived changes in exercise, eating behaviour and body image since the lockdown began. At the end of the survey, participants were thanked for their time, informed that they would be contacted again for a follow up survey, and provided with the researchers’ contact details. As the survey had asked questions about coping with the lockdown and mental health, online resources for support were signposted.
2.5. Data analysis
There were minimal missing data (n < 3 for all variables, other than past/present mental health diagnosis, in which n = 11 were missing). Given this, we used pairwise deletion meaning n varies slightly between analyses.
We used descriptive statistics and histograms to explore the extent to which people reported perceived changes in eating, exercise and body image during lockdown (RQ1). Given the single item ordinal scales, we compared the extent of perceived changes by age (under 30 years vs. 30+ years), gender (male vs. female), living circumstances (living alone vs. not living alone), and current or past diagnosis (dx) of mental health condition or developmental disorder (No dx vs. current/past ED dx vs. current/past other disorder dx) using Kruskal-Wallis tests. In all cases of significant differences, post hoc pairwise comparisons were Bonferroni-adjusted for multiple tests, and the reported p values reflect the adjusted p value (RQ2). Spearman's rank correlation coefficients (with Bonferroni-adjusted p values) were used to explore the association between extent of perceived changes and psychological distress (RQ3). In all analyses, alpha was set to 0.05.
3. Results
3.1. Sample characteristics
The sample was predominantly women (78.0%, n = 206), of White ethnicity (92.0%, n = 243), with an undergraduate degree (81.4%, n = 215). Age ranged from 18 to 79 years, with 42% (n = 111) aged 18–29 years, and 58% (n = 151) aged 30+ years (2 participants did not provide their age). The majority of the sample were living with other people (friends, family, flatmates) during lockdown (85.23%, n = 225), with only 15% living alone (n = 39). Thirty-five (13.8%) participants reported a current or past diagnosis of an eating disorder, 93 (36.8%) reported a current or past diagnosis of another mental health condition or developmental disorder, with half reporting no current or past diagnoses (n = 125, 49.4%) (11 participants either did not provide a response or said they did not know if they had every received a diagnosis of a mental health/developmental disorder). Based on the PHQ-4 measure, 19% (n = 50) reported psychological distress in the low/mild range, and 11% (n = 30) reported distress in the moderate/severe range.
3.2. To what extent do people perceive changes in being able to regulate eating, preoccupation with food, exercise behaviour, thinking about exercise and appearance concerns during lockdown?
Table 1 shows the frequencies with which people agreed with each statement regarding changes in eating, exercise and body image during lockdown. There were clear individual differences across each of the domains, with the sample endorsing the full range of response options. Just over half of the sample reported that it was more difficult to regulate or control their eating, with 60% reporting that they were more preoccupied with food/eating. Half the sample reported exercising more during lockdown, and over two thirds reported thinking more about exercise. Just under half agreed that they had been more concerned about their appearance during lockdown.
Table 1.
Frequencies of response options for perceived changes in eating, exercise and body image.
| Strongly Disagree N (%) |
Disagree N (%) |
Neutral N (%) |
Agree N (%) |
Strongly Agree N (%) |
|
|---|---|---|---|---|---|
| More difficult to control or regulate eating | 42 (16.0%) | 49 (18.7%) | 32 (12.2%) | 77 (29.4%) | 62 (23.7%) |
| More preoccupied with food/eating | 25 (9.5%) | 37 (14.1%) | 44 (16.8%) | 99 (37.8%) | 57 (21.8%) |
| Exercising more | 45 (17.2%) | 51 (19.5%) | 34 (13.0%) | 66 (25.2%) | 66 (25.2%) |
| Thinking about exercise more | 20 (7.6%) | 29 (11.0%) | 36 (13.7%) | 86 (32.7%) | 92 (35.0%) |
| More concerned about the way I look | 28 (10.6%) | 56 (21.2%) | 52 (19.7%) | 56 (21.2%) | 72 (27.3%) |
3.3. Do these perceived changes vary by gender, age group, living circumstances, and pre-existing mental health conditions?
Table 2 shows the results of the Kruskal-Wallis tests comparing perceived changes by demographic characteristics. In general, women reported greater perceived changes than men, specifically being more likely to report finding it more difficult to control or regulate eating, being more preoccupied with food/eating, exercising more, and having increasing concerns about their appearance.
Table 2.
Results of Kruskal-Wallis (KW) tests comparing perceived changes in eating, exercise and body image by demographic characteristics.
| Gender | Age | Living circumstances | Mental health | ||
|---|---|---|---|---|---|
| More difficult to control or regulate eating | KW Test | X2 (1) = 13.93, p < 0.001 | X2 (1) = 1.18, p = 0.27 | X2 (1) = 0.45, p = 0.50 | X2 (2) = 13.75, p = 0.001 |
| Post hoc comparisons | Female > Male | N/A | N/A | ED > No Dx | |
| More preoccupied with food/eating | KW Test | X2 (1) = 14.00, p < 0.001 | X2 (1) = 2.43, p = 0.12 | X2 (1) = 0.23, p = 0.63 | X2 (2) = 25.78, p < 0.001 |
| Post hoc comparisons | Female > Male | N/A | N/A | ED > No Dx ED > Other Dx Other Dx > No Dx |
|
| Exercising more | KW Test | X2 (1) = 4.21, p < 0.04 | X2 (1) = 1.59, p = 0.21 | X2 (1) = 0.93, p = 0.34 | X2 (2) = 12.30, p = 0.002 |
| Post hoc comparisons | Female > Male | N/A | N/A | ED > No Dx ED > Other Dx |
|
| Thinking about exercise more | KW Test | X2 (1) = 3.01, p = 0.08 | X2 (1) = 12.20, p < 0.001 | X2 (1) = 0.33, p = 0.57 | X2 (2) = 14.34, p < 0.001 |
| Post hoc comparisons | N/A | Younger > Older | N/A | ED > No Dx ED > Other Dx |
|
| More concerned about the way I look | KW Test | X2 (1) = 14.03, p < 0.001 | X2 (1) = 12.57, p < 0.001 | X2 (1) = 0.02, p = 0.88 | X2 (2) = 21.71, p < 0.001 |
| Post hoc comparisons | Female > Male | Younger > Older | N/A | ED > No ED > Other Dx |
Age was also associated with differential perceived changes, although across fewer domains. Specifically, younger people (i.e. those aged <30 years) were more likely to report thinking more about exercise and also having increasing concerns about their appearance during lockdown. In contrast, there were no differences by age group in perceived changes to eating.
Living alone versus living with other people was not associated with differences in rates of perceived changes to eating, exercise or body image.
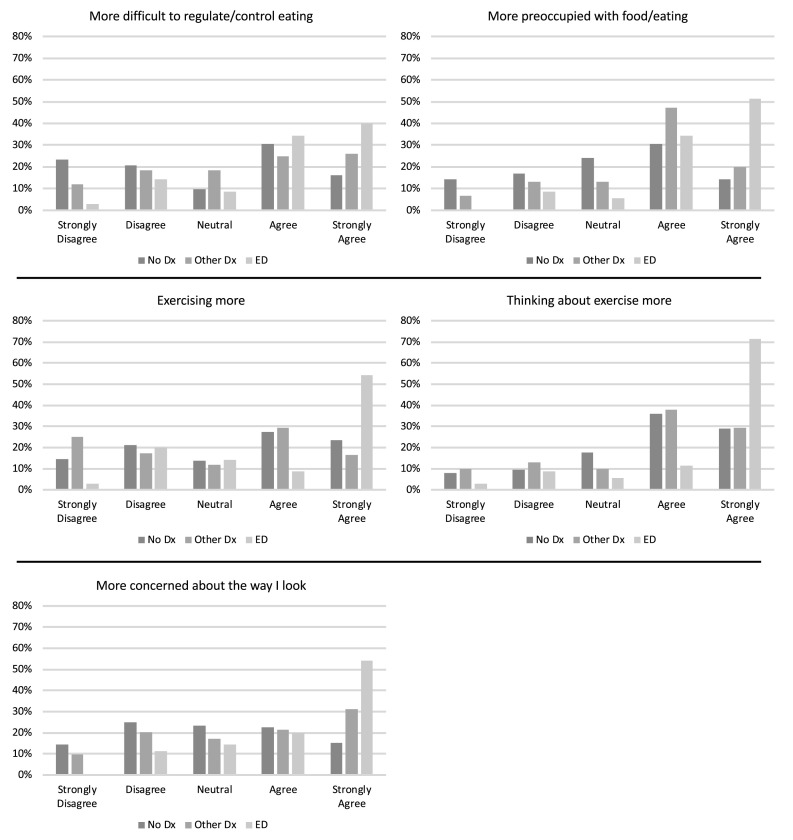
Finally, pre-existing diagnoses of mental health and developmental disorders were associated with differential rates in perceived changes across all domains (illustrated in Fig. 1 ). Specifically, compared to those without a history of mental health problems or developmental disorders, those with a current or past diagnosis of an ED were significantly more likely to report increased difficulties in controlling/regulating eating, increased preoccupation with food, increased exercise thoughts and behaviours, and increased concerns about appearance. In all domains except regulation of eating, those with ED also reported significant increases compared to those with other mental health conditions or developmental disorders.
Fig. 1.
Bar charts showing extent of perceived changes in eating, exercise and body image, by mental health history.
3.4. To what extent are perceived changes in eating, exercise and body image associated with psychological distress?
There was a significant correlation between psychological distress and finding it more difficult to control/regulate one's eating (rs = 0.36, p < 0.001, n = 262), being more preoccupied with food/eating (rs = 0.29, p < 0.001, n = 262), thinking more about exercise (rs = 0.17, p = 0.02, n = 262) and being more concerned about one's appearance (rs = 0.41, p < 0.001, n = 264). In contrast, there was no significant association between psychological distress and perceived changes in exercise (rs = −0.14, p = 0.10, n = 262). Note that all reported p values are Bonferroni-adjusted.
4. Discussion
This study explored perceived changes in body image, eating and exercise behaviours within the general population of the UK during the early stages of the COVID-19 pandemic-related ‘lockdown’ measures. Consistent and regular media messages throughout this period have focused on the potential negative impact of increased sedentary lifestyle and dysregulated eating behaviours within the general population. Our study suggests a more complex picture, with large individual differences in perceived impact, and differential rates of perceived change based on demographic characteristics and pre-existing mental health conditions, particularly eating disorders.
Firstly, women (and to some extent young people) were disproportionately more likely to report changes in thoughts and behaviours, including finding it more difficult to regulate eating, being more preoccupied with food and having increasing concerns around appearance. This finding mirrors other studies showing a disproportionate negative mental health impact of COVID-19 on women (Banks & Xu, 2020; Pierce et al., 2020). Further work will be needed to understand mechanisms underpinning these changes, but potential explanations could include heightened levels of stress and anxiety (Murray, Byrne, & Rieger, 2011) resulting from increased caregiving responsibilities, exposure to increased weight stigma via public health and social media messaging regarding obesity and COVID-19 (Pearl, 2020), as well as increased saliency of food and eating as a result of shopping restrictions and changes to daily routines.
Interestingly, women and younger people also reported exercising more during lockdown. This could represent an improvement in health behaviours, or reflect more compulsive behavioural changes driven by heightened anxiety and weight and shape concerns (Meyer, Taranis, Goodwin, & Haycraft, 2011). Physical activity may also improve mood and mental health (Liao, Shonkoff, & Dunton, 2015; Schuch & Stubbs, 2019) and thus might be used as a coping strategy. Interestingly though, in the current study distress was associated only with thinking about exercise more, and not a perceived increase in exercise behaviour. This could signal that exercise-related thoughts were driven more by appearance concerns than physical benefits, or simply that during lockdown it was not possible for people to visit gyms or engage in their usual levels of physical activity.
Body dissatisfaction and cognitive biases are important risk and maintenance factors for disordered eating (e.g. Neumark-Sztainer, Story, Faibisch, Ohlson, & Adamiak, 1999; Williamson, White, York-Crowe, & Stewart, 2004). Therefore, these findings may provisionally support concerns that COVID-19 lockdown may be a catalyst for the development of these difficulties (e.g., Rodgers et al., 2020), with women potentially being at greater risk. Following the trajectories of these groups as lockdown measures ease will be vital in determining any longer-term implications of these perceived changes.
Second, those with past or current eating disorders showed particularly elevated rates of perceived change in body image, eating and exercise. It has been noted that measures associated with lockdown (e.g., social isolation, restricted food shopping) may present particular challenges to those with eating disorders (Rodgers et al., 2020; Touyz et al., 2020), and this is supported by our findings. Notably, perceived increases in being preoccupied with food, thoughts about exercise and appearance concerns were greater in those with eating disorders, even compared to those with a history of other mental health conditions or developmental disorders. This suggests deterioration in the specific pathology associated with eating disorders that should be considered.
These findings indicate that we may see an increase in demand for UK eating disorder services as existing service users may experience more severe symptoms, and there is potential for an increase in new disordered eating presentations. This appears to be provisionally supported by UK-based third sector organisations seeing significant increase in demand for services during lockdown (Turnbridge, 2020). This would have implications for health services at a critical point of COVID-related restructuring and associated social distancing constraints on the delivery of traditional interventions (Davis et al., 2020; Touyz et al., 2020; Weissman et al., 2020), alongside an increase in weight- and diet-orientated media messages, as a result of the launch of Public Health England's Obesity Strategy (Department of Health and Social Care, 2020). Increasing freely available self-help resources, digital delivery and investment in early intervention approaches should be promoted at this time, alongside careful consideration of any risks associated with obesity related public health messages.
A third key finding was that greater perceived changes in eating and body image (and to a lesser extent exercise) were significantly associated with elevated psychological distress. Given the cross-sectional nature of these baseline data, it is not possible to determine whether increased distress during lockdown might be driving more disordered eating thoughts and behaviours, or whether those who were already distressed may be using eating as a new coping mechanism when constrained in other coping skills. Given that overall levels of psychological distress in this study were in line with norms reported prior to the pandemic (Löwe et al., 2010), the latter may be more probable. Future longitudinal work will be needed to explore this further, and this may have significant implications for our understanding of the relationship between significant psychosocial stressors and eating behaviours across the population. By understanding underpinning mechanisms associated with these eating behaviours we may begin to develop more targeted, and potentially more effective, public health approaches to weight management.
There are some limitations of the current study that should be considered. First, our recruitment strategy relied on people self-selecting to take part, which may mean that our sample is biased towards those interested in health behaviours. Our participants were recruited through social media platforms, and the survey was hosted online. Therefore, our sample is likely to be biased towards individuals with internet access and who actively use social media. For some analyses, we had small and unequal group sample size, especially in the ED group, meaning it was not possible to differentially explore current vs past diagnosis of an ED participants, nor between specific diagnoses in the comparator group (e.g., depression, anxiety). Second, because of the lockdown timing we were unable to obtain a baseline measures of body image, exercise and eating, and therefore were reliant on self-reported changes using an unvalidated measure; this limitation also affects other studies conducted during the lockdown period (e.g. Di Renzo et al., 2020). Although we only required participants to report change rather than actual eating or eating behaviour, we cannot objectively validate the accuracy of these data. Third, the cross-sectional nature of the study means we can only establish relationships between variables, rather than temporality or causality. As the study will involve follow-up rounds, we can examine temporal relationships between variables in more detail and the longer-term impact of changes within groups in later survey sweeps. Finally, our findings do not address the nature of the mechanisms underlying the perceived changes in eating and exercise behaviours. These mechanisms need to be investigated further to identify why some individuals experienced greater changes than others, to inform prevention and intervention strategies.
In conclusion, adults in the UK report a wide range of changes to their eating- and exercise-related thoughts and behaviours, as well as their body image, during the lockdown associated with this pandemic. Growing challenges with regulating food consumption, being more preoccupied with food and worsening body image are all linked with psychological distress. Importantly, some groups appear to be more susceptible to these changes, with women, young people and those with pre-existing mental health problems – especially eating disorders – being at heightened risk. Ongoing research to explore the full range of experiences and individual differences in the trajectories of change in eating, exercise and body image as lockdown measures ease will be important for understanding the full psychological impact of this pandemic and improve service and public health planning going forward.
Author contributions
MR, EN and HS conducted data preparation and analysis. All authors conceived of the study and contributed to writing the manuscript. All authors have reviewed and approved the final article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
Ethical approval for this study provided by the University of Edinburgh School of Health in Social Science Research Ethics Committee. (Ref: STAFF181, 05/06/20). All participants provide informed consent prior to taking part in this study.
Acknowledgements
We are very grateful to all participants who volunteered to take part in this study.
Footnotes
The remaining four items were excluded from this study as they were only applicable to people who were dieting: “I have found it more difficult to eat according to my rules”, “I have found it easier to avoid eating food(s) I shouldn't eat”, “I have found it more difficult to resist temptations (avoid “cheating” on my diet)”, “I have become more rigid in sticking to rules about what, when, and how much I eat”.
References
- Arnett J.J. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55(5):469. doi: 10.1037/0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- Banks J., Xu X. 2020. The mental health effects of the first two months of lockdown and social distancing during the Covid-19 pandemic in the UK. Institute for Fiscal Studies Working Paper W20/16.https://www.ifs.org.uk/publications/14874 [Google Scholar]
- Cooper M., Reilly E.E., Siegel J.A., Coniglio K., Sadeh-Sharvit S., Pisetsky E. Eating disorders during the COVID-19 pandemic: An overview of risks and recommendations for treatment and early intervention. Eating Disorders. 2020 doi: 10.1080/10640266.2020.1790271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C., Chong N.K., Oh J.Y., Baeg A., Rajasegaran K., Chew C.S.E. Caring for children and adolescents with eating disorders in the current COVID-19 pandemic: A Singapore perspective. Journal of Adolescent Health. 2020 doi: 10.1016/j.jadohealth.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Social Care Tackling obesity: Empowering adults and children to live healthier lives. 2020. https://www.gov.uk/government/publications/tackling-obesity-government-strategy
- Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attinà A., Cinelli G.…Scerbo F. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. Journal of Translational Medicine. 2020;18(1):1–15. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Bu F., Mak H.W., Steptoe A. Covid-19 social study. Results release 22. 2020. https://b6bdcb03-332c-4ff9-8b9d-28f9c957493a.filesusr.com/ugd/3d9db5_636933e8191d4783866c474fab3ca23c.pdf
- Fernández-Aranda F., Casas M., Claes L., Bryan D.C., Favaro A., Granero R.…Le Grange D. COVID‐19 and implications for eating disorders. European Eating Disorders Review. 2020;28(3):239. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L.…Everall I. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Liao Y., Shonkoff E.T., Dunton G.F. The acute relationships between affect, physical feeling states, and physical activity in daily life: A review of current evidence. Frontiers in Psychology. 2015;6:1975. doi: 10.3389/fpsyg.2015.01975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K.…Brähler E. A 4-item measure of depression and anxiety: Validation and standardization of the patient health questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders. 2010;122(1–2):86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- Meyer C., Taranis L., Goodwin H., Haycraft E. Compulsive exercise and eating disorders. European Eating Disorders Review. 2011;19(3):174–189. doi: 10.1002/erv.1122. [DOI] [PubMed] [Google Scholar]
- Murray K.M., Byrne D.G., Rieger E. Investigating adolescent stress and body image. Journal of Adolescence. 2011;34(2):269–278. doi: 10.1016/j.adolescence.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Naja F., Hamadeh R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. European Journal of Clinical Nutrition. 2020:1–5. doi: 10.1038/s41430-020-0634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D., Story M., Faibisch L., Ohlson J., Adamiak M. Issues of self-image among overweight African-American and caucasian adolescent girls: A qualitative study. Journal of Nutrition Education. 1999;31(6):311–320. doi: 10.1016/S0022-3182(99)70484-X. [DOI] [Google Scholar]
- Pascual-Sanchez A., Nicholls D., Patalay P., Crosby L., McColoud T., Hudson L.…Viner R. You-COPE. Mental health consequences experienced by young people aged 16-24 during first months of the COVID-19 lockdown. 2020. https://www.ucl.ac.uk/child-health/sites/child-health/files/youcope_briefing_mental_health_impact_final_version.pdf
- Pearl R.L. Obesity; 2020. Weight stigma and the “quarantine‐15”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipou A., Meyer D., Neill E., Tan E.J., Toh W.L., Van Rheenen T.E. Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: Initial results from the COLLATE project. International Journal of Eating Disorders. 2020 doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A.…McManus S. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers R.F., Lombardo C., Cerolini S., Franko D.L., Omori M., Fuller‐Tyszkiewicz M.…Guillaume S. The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders. 2020 doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch F.B., Stubbs B. The role of exercise in preventing and treating depression. Current Sports Medicine Reports. 2019;18(8):299–304. doi: 10.1249/JSR.0000000000000620. [DOI] [PubMed] [Google Scholar]
- Termorshuizen J.D., Watson H.J., Thornton L.M., Borg S., Flatt R.E., MacDermod C.M.…Bulik C.M. Early impact of COVID-19 on individuals with self-reported eating disorders: A survey of ~1,000 individuals in the United States and The Netherlands. International Journal of Eating Disorders. 2020 doi: 10.1002/eat.23353. n/a(n/a) [DOI] [PubMed] [Google Scholar]
- Touyz S., Lacey H., Hay P. Eating disorders in the time of COVID-19. Journal of eating disorders. 2020;8(19) doi: 10.1186/s40337-020-00295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbridge S. Eating disorder chairty sees 70% increase in calls for help during lockdown. Huffington post. 2020. https://www.huffingtonpost.co.uk/entry/eating-disorder-coronavirus-lockdown-beat_uk_5f0c605ac5b6480493d2fe80?guccounter=1&guce_referrer=aHR0cHM6Ly93d3cuZ29vZ2xlLmNvbS8&guce_referrer_sig=AQAAAIzPJ0rq2YcAA_lBX5Eu0PawFR39l3KIje7Lbi1ekGLdA3eYYmQNSN6ZdZqHlQiPJ6ZFjQsvMRXG_afT_MUEU8GAR2lvF_NA66zgsSW3uMjBxQ_psirhQrksg28m-pbAQ1O8RdoBfw0B9pv_6yL9xBJLOkL_sCslgd9ROTEKA0-v
- Weissman R.S., Bauer S., Thomas J.J. Access to evidence‐based care for eating disorders during the COVID‐19 crisis. International Journal of Eating Disorders. 2020;53(5):639–646. doi: 10.1002/eat.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson D.A., White M.A., York-Crowe E., Stewart T.M. Cognitive-behavioral theories of eating disorders. Behavior Modification. 2004;28(6):711–738. doi: 10.1177/0145445503259853. [DOI] [PubMed] [Google Scholar]