Abstract
Background
The SARS-CoV-2 pandemic has reached Poland on March 4th, 2020 and undoubtedly affected all areas of life and medical care, including bariatric care. The study was planned to identify the impact of the SARS-CoV-2 pandemic on bariatric care in Poland.
Methods
The online survey was designed and distributed to bariatric surgeons. The questionnaire was divided into three parts: demographic characteristics of participants and their bariatric centers, examining the impact of the pandemic on the bariatric care and last part with questions about planned care after the pandemic.
Results
49 surgeons participated in the survey. 27 (55%) participants worked in hospitals transformed into COVID-dedicated units. Only 9 (18%) respondents declared uninterrupted bariatric surgery during a pandemic. 91% of surgeons declared continuation of bariatric care with telemedicine techniques. All participants declared a high willingness to resume bariatric surgery after the SARS-CoV-2 pandemic and responded that bariatric procedures should resume immediately when World Health Organisation (WHO) announces the end of a pandemic regardless of oncological treatment. 90% of respondents believe that the pandemic will not affect the safety of bariatric procedures in the future.
Conclusions
Access to bariatric care during the pandemic is limited and redirected to telemedicine. Surgeons are ready to resume bariatric operations immediately after the pandemic, but its end is difficult to determine. In surgeons’ opinion pandemic will not affect the safety of bariatric surgery in the future. The extended waiting list and financial aspects will be the main issues after the pandemic.
Keywords: Bariatric surgery, COVID-19, SARS-CoV-2, Pandemic
Background
The demand for bariatric surgery in Poland is growing annually, despite a constant increase in the number of conducted surgeries. Currently, in Poland more than 30 surgical centers perform bariatric procedures, adding up to around 5000 procedures throughout the country annually [1].
In December 2019, China became the center of an outbreak of pneumonia caused by a new pathogen named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [2]. On March 11th, 2020 World Health Organization (WHO) declared coronavirus disease (COVID-19) global pandemic [3]. The virus has also reached Poland on March 4th, 2020, causing over 9,000 infections and over 350 deaths (Polish Ministry of Health, April 19th, 2020).
Obesity plays an important role in the development of a severe course of SARS-COV-2 infection and is considered as a very strong single risk factor for death [4]. International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) proposed recommendations for metabolic and bariatric surgery during the COVID-19 pandemic to minimizes risk for the patients and healthcare teams [5].
Currently, data on the impact of the pandemic on bariatric care is scarce. Furthermore, there is no information or any ideas about how to deal with bariatric patients after the SARS-CoV-2 pandemic dissipates.
Our objective was to identify the impact of the SARS-CoV-2 pandemic on bariatric care in Poland.
Methods
Study design
An anonymous, online, voluntary open-survey was designed and distributed by the mailing list to all bariatric surgeons associated with the Metabolic and Bariatric Chapter at the Association of Polish Surgeons (SCMiB). An invitation to the project was also published on the official website of SCMiB on April 8th, 2020. E-mail and invitations both included a link to the online form including the survey. The questionnaire was designed by the member of the science committee of the SCIMB. Technical functionality of the electronical questionnaire was tested prior to the study by bariatric surgeons working in first authors department. The survey was conducted between 8 and 15 April 8th and 15th, 2020. Comprehensive instructions on how to complete the survey were included at the beginning of the questionnaire and in the invitation to the project. The questionnaire included multiple choice and Likert scale questions. The order of questions was randomized in each part of the survey. Participants were not offered incentives to participate in the study. Adaptive questioning was not found to be necessary in this questionnaire. Each page included one question, therefore questionnaire included 44 pages. It was not possible to submit an incomplete survey, each question included a “Not applicable” answer. Respondents at any point were able to change their answers by using a “Back button”. Only completed questionnaires were analyzed. Our internet form service did not allow for recording unique site visitor, view rate and participation rate. Authors conducted a log-file analysis to prevent multiple entries from the same individual. The study was designed and described regarding all CHERRIES checklist points for reporting results from internet e-surveys [6].
Inclusion and exclusion criteria
The study group included surgeons and general surgery residents who are members of SCMiB working in bariatric centers. Both certified bariatric surgeons and non-certified were included in the study. We excluded retired surgeons, surgeons not performing bariatric procedures, and medical doctors who do not practice medicine during the pandemic (sick leave, vacation).
Survey
The questionnaire was divided into three parts: demographic characteristics of participants and their bariatric centers, examining the impact of the pandemic on the bariatric care and last part with questions about planned care after the pandemic.
First part gathered data on age, sex, stage of surgical training—resident/specialist/ certificated bariatric surgeon, type of hospital—academic/state hospital/municipal hospital, numbers of bariatric procedures performed in 2019, number of bariatric surgeries performed in 2020 before the outbreak of SARS-CoV-2, actual status of the hospital during pandemic—COVID dedicated hospital/COVID non-dedicated hospital, and information if COVID-19 patients were treated in the hospital.
Questions in the second part concerned the impact of the pandemic on bariatric care. They asked about the level of current bariatric care, still performed bariatric procedures, numbers of postponed surgeries, reasons for cancellation, the ability to provide the emergency procedure in bariatric patients. Survey included questions about telemedicine and possible application in bariatric care during pandemic, acceptance of this form of patient-doctor communication, and satisfaction with this kind of medium. Roles of surgeon, dietitian, psychologist, and patient organizations online support during pandemic were evaluated with the numeric linear scale (1–10).
The third part of the survey requested information on bariatric care after pandemic: impact of the pandemic on patients’ waiting list, plans on how to resolve the problem with a large number of suspended surgeries, willingness to resume bariatric surgery after pandemic (scale 1–10). Next questions regarded when bariatric procedures should be resumed, and how to reconcile them with oncological procedures waiting list. At the end of the survey, there were questions about the impact of SARS-CoV-2 on future qualification rules, type of performed bariatric surgery proposed to the patients and their safety after the pandemic.
The questionnaire was developed for this study and it is presented in Additional file 1.
Ethical considerations
The designed survey was fully anonymous. Personal data of participants collected during study, was not disclosed at any stage. Participants were informed about the length of time of the survey, range of data, that were stored and where and for how long, the name of the primal investigator and the purpose of the study. The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments (Fortaleza). Participants were informed about the aim of the study and informed consent was obtained electronically prior to the beginning of the survey. The study was approved by the Bioethics Committee of the Jagiellonian University (1072.6120.103.2020).
Statistical analysis
Results are presented as numbers with percentages, means with standard deviation or medians with interquartile range, when appropriate.
Results
Participants
Overall, 49 surgeons and surgical residents participated in our survey, which constitutes 60% of a total number of SCMiB members (82). Completion rate was 100%. The study group included 41 (84%) males and 8 (16%) females. The mean age was 43 ± 10 years. The group of respondents included 19 (39%) surgeons with bariatric certificate, 19 (39%) surgeons and 11 (22%) residents (Table 1).
Table 1.
Basic characteristics
| All | |
|---|---|
| n (%) | 49 (100%) |
| Mean age, years ± SD | 43 ± 10 |
| Males/females, n (%) | 41/8 (84%/16%) |
| Stage of surgical training | |
| Specialist surgeons with SCMiB certificate, n (%) | 19 (39%) |
| Specialist surgeons, n (%) | 19 (39%) |
| Residents, n (%) | 11 (22%) |
| Type of hospital | |
| University hospital, n (%) | 22 (45%) |
| Voivodship specialist hospital, n (%) | 9 (18%) |
| District hospital/city hospital, n (%) | 18 (37%) |
| COVID status | |
| COVID-dedicated hospital | 27 (55%) |
| Non-COVID dedicated hospital | 22 (45%) |
| Numbers of bariatric procedures | |
| Median number of bariatric procedures in 2019 (January, February), n (IQR) | 27 (22–50) |
| Median number of bariatric procedures in 2020 until pandemic (January, February), n (IQR) | 30 (24–50) |
Hospitals
Most of the participants worked in academic hospitals—22 (45%), 18 (37%) worked in district/city hospitals and 9 (18%) in state departments. 27 (55%) of participants worked in hospitals transformed into COVID-dedicated units. 28 (57%) participants declared that patients with SARS-CoV-2 were treated in their hospitals. Median number of bariatric procedures in 2019 (January, February) was 27 (22–50). Median number of bariatric procedures in 2020 until pandemic (January, February) was 30 (24–50) (Table 1).
Current status of bariatric care
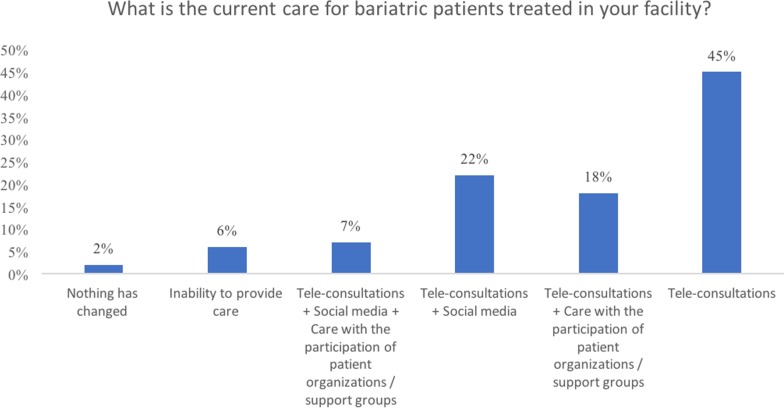
Only 9 (19%) respondents declared uninterrupted bariatric service during pandemic, all of whom worked in non-COVID dedicated hospitals. In 100% of COVID-dedicated hospitals, bariatric surgeries have been suspended. Median number of postponed procedures per centre was 23 (18–32). In 40 (81%) respondents the cessation of these surgical procedures was dictated by the hospital management, 8 (16%) by internal arrangements in the surgery department, and 1 (2%) by independent decision of the surgeon. All respondents declare that the limitation of bariatric surgery during pandemic is necessary, median score was 10 (8–10). In the part dedicated to the current care for bariatric patients, 3 (6%) respondents declared inability to provide any care, 1 (2%) respondent declared that nothing has changed, 45 (92%) declared individual phone contact, e-mail, teleconsultations, and social media as an actual way of caring for bariatric patients (Fig. 1). 11 (23%) participants performed full outpatient bariatric service, 38 (77%) performed only follow-up after surgery without qualification of new patients. All respondents consider it necessary to continue providing remote care for bariatric patients. The majority, 45 (93%) respondents, believe that patients have limited access to diagnostic tests ordered by the attending surgeon required before the surgery and during follow-up. During any type of contact with patients, 37 (75%) surgeons informed patients about obesity being a risk factor for a severe course of COVID-19 and death. Only 18 (37%) participants recommend changes in diet, physical activity, and psychological support during pandemic. 43 (87%) surgeons declare that hospital is ready in case of emergency in bariatric patients.
Fig. 1.
The current care for bariatric patients
Bariatric care after pandemic
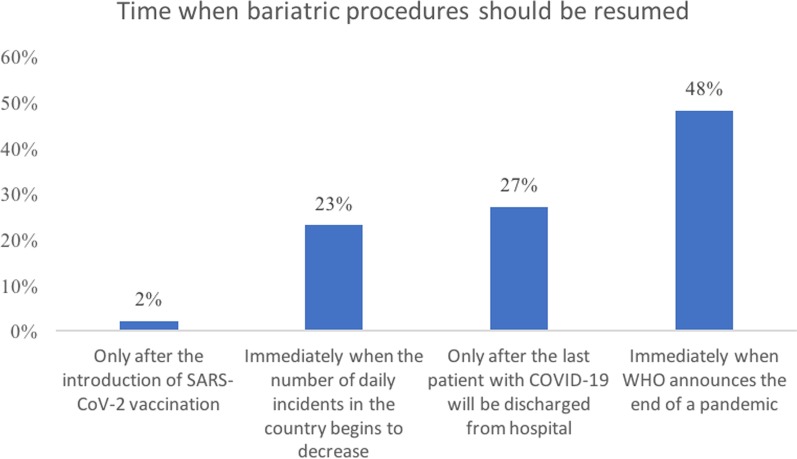
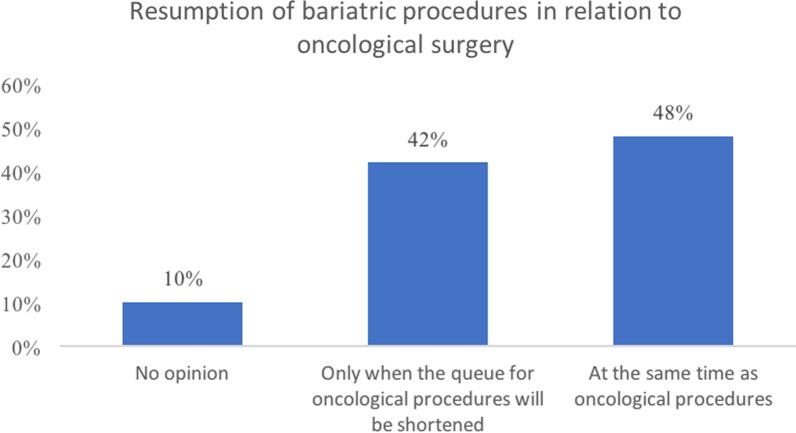
In the opinion of 40 (81%) respondents, the current situation will affect future work after a pandemic and prolong waiting list for bariatric procedures. Only 9 (19%) participants declared prepared plan for post-pandemic bariatric care, 22 (45%) are currently working on it, 18 (36%) do not resolve this issue yet. Surgeons are worried about the financial aspect of bariatric procedures after pandemic—46 (94%), 3 (6%) believe that a pandemic will not affect bariatrics funding. All participants declared a high willingness to resume bariatric surgery after the SARS-CoV-2 pandemic, median score 10 (10–10). Asked when bariatric procedures should resume, respondents answered: immediately when WHO announces the end of a pandemic—24 (48%), after the last patient with COVID-19 was discharged from hospital—13 (27%), immediately when the number of daily new infections in the country starts to decrease—11 (23%), after the introduction of SARS-CoV-2 vaccination—1 (2%) (Fig. 2). In the context of oncological treatment bariatric surgery should resume in parallel—24 (48%), after managing oncological queue—20 (42%), 5 (10%) participants had no opinion (Fig. 3). 34 (69%) surgeons believed that pandemic will not affect qualification rules or types of surgery proposed to the patients in the future. The majority of participants, 44 (90%), believe that the pandemic will not affect the safety of bariatric procedures. In opinion of 10% sleeve gastrectomy will be the safest procedure after the pandemic.
Fig. 2.
Time when bariatric procedures should be resumed
Fig. 3.
Resumption of bariatric procedures in relation to oncological surgery
Discussion
The presented study is a result of a national survey that was dedicated for bariatric surgeons. Survey shows COVID negative impact on bariatric care in Poland. As a result of the pandemic, most bariatric procedures were postponed which is officially recommended [5, 7]. Data from around the world indicate this affects all types of surgery, including oncology [8]. This pandemic definitely represents significant harm for bariatric patients. Difficulties also arise in the functioning of the bariatric outpatient clinic. Telemedicine techniques have undoubtedly become preferred. Digital healthcare provides a necessary solution in this time of unprecedented medical crisis [9]. Our survey shows that telemedicine is possible and well suited to provide bariatric care during the pandemic.
Survey also shows how, in surgeons' opinion, SARS-CoV-2 will affect bariatric care when pandemic ends. The study showed that bariatric surgeons are ready to resume bariatric surgery as soon as possible after the pandemic. They also consider patients with different diseases who will be negatively affected during the pandemic and after it. Most healthcare systems are prioritizing surgical care for oncological patients, emergency surgery and other elective surgeries. When we combine it with the expected problems with public finances, possibly decreased reimbursement, there is a concern that bariatric patients’ treatment may have to be postponed even further [10]. Survey respondents consider that the COVID-19 pandemic will not affect the safety of future bariatric procedures.
Limitations
This study is associated with several limitations. Multiple accesses to the questionnaire by respondents were potentially possible. To avoid the bias Authors have conducted a log-file analysis aimed to identify potential multiple entries from the same individual. Unfortunately, there still was a possibility of multiple entries from a single respondent. However, we have additionally included an instruction at the beginning of the survey and there was no incentive for sending multiple responses. The overall number of respondents is relatively low. It is important to notice, that sample size was limited only to surgeons, that are members of the Bariatric Chapter at the Association of Polish Surgeons, in which response rate has reached 60%. This constitutes a high score when compared with available literature including online-survey based studies [11–14]. Therefore, low number of respondents resulted from a limited target group of potential subjects. Moreover, we concentrated only on Polish bariatric departments, so it may be difficult to extrapolate our results to other countries, however, we expect that most bariatric surgeons have similar problems.
Conclusions
The SARS-CoV-2 pandemic resulted in canceling or postponing of bariatric procedures in Poland. Access to bariatric care during the pandemic is limited and redirected to telemedicine. Surgeons are ready to resume bariatric operations immediately after the pandemic, but its end is difficult to determine. In the surgeons’ opinion, the pandemic will not affect the safety of bariatric surgery in the future. The extended waiting list and financial aspects will be the main issues after the pandemic. Guidelines about post-pandemic bariatric care organization plans are yet to be established.
Supplementary Information
Acknowledgements
Study was conducted in collaboration with Metabolic and Bariatric Chapter at Association of Polish Surgeons (SCMiB).
Abbreviations
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- WHO
World Health Organization
- COVID-19
Coronavirus disease
- IFSO
International Federation for the Surgery of Obesity and Metabolic Disorders
- SCMiB
Metabolic and Bariatric Chapter at the Association of Polish Surgeons
Authors’ contributions
PMaj: conceptualization, methodology, formal analysis, investigation and writing—original draft, visualization and project administration. TS, MW, PMał and AR: formal analysis, investigation and writing—review and editing. MPS, JS, MP: conceptualization, methodology, investigation, writing—review and editing, supervision. All authors have read and approved the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was anonymous, performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments (Fortaleza). Participants were informed about the aim of the study and informed consent was obtained electronically prior to the beginning of the survey. The study was approved by the Bioethics 297 Committee of the Jagiellonian University (1072.6120.103.2020).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12893-020-00990-7.
References
- 1.Waledziak M, Rozanska-Waledziak AM, Kowalewski PK, Janik MR, Bragoszewski J, Pasnik K, et al. Present trends in bariatric surgery in Poland. Wideochirurgia i inne Tech maloinwazyjne = Videosurgery other miniinvasive Tech. 2019;14:86–89. doi: 10.5114/wiitm.2018.77707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet (London, England) 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Director-General’s opening remarks at WHO characterizes COVID-19 as a pandemic.
- 4.Kassir R. Risk of COVID-19 for patients with obesity. Obes Rev. 2020;21:e13034. doi: 10.1111/obr.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang W, Wang C, Shikora S, Kow L. Recommendations for metabolic and bariatric surgery during the COVID-19 pandemic from IFSO. Obes Surg. 2020;30:1–3. doi: 10.1007/s11695-020-04578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES) J Med Internet Res. 2004;6:1–6. doi: 10.2196/jmir.6.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American College of Surgeons. COVID-19: Recommendations for management of elective surgical procedures 2020.
- 8.Indini A, Aschele C, Cavanna L, Clerico M, Daniele B, Fiorentini G, et al. Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: a nationwide Italian survey. Eur J Cancer Engl. 2020;132:17–23. doi: 10.1016/j.ejca.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Kapoor A, Guha S, Kanti Das M, Goswami KC, Yadav R. Digital healthcare: the only solution for better healthcare during COVID-19 pandemic? Indian Heart J. 2020;72:61–64. doi: 10.1016/j.ihj.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tyagi SK, Singhal R. Bariatric surgery in the times of corona. Obes Surg. 2020;30:2807. doi: 10.1007/s11695-020-04589-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307:1805–1806. doi: 10.1001/jama.2012.3532. [DOI] [PubMed] [Google Scholar]
- 12.Agresta F, Campanile FC, Podda M, Cillara N, Pernazza G, Giaccaglia V, et al. Current status of laparoscopy for acute abdomen in Italy: a critical appraisal of 2012 clinical guidelines from two consecutive nationwide surveys with analysis of 271,323 cases over 5 years. Surg Endosc. 2017;31:1785–1795. doi: 10.1007/s00464-016-5175-4. [DOI] [PubMed] [Google Scholar]
- 13.Iversen HH, Holmboe O, Bjertnaes O. Patient-reported experiences with general practitioners: a randomised study of mail and web-based approaches following a national survey. BMJ Open. 2020;10:e036533. doi: 10.1136/bmjopen-2019-036533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shih T-H, Fan X. Comparing response rates in e-mail and paper surveys: a meta-analysis. Educ Res Rev. 2009;4:26–40. doi: 10.1016/j.edurev.2008.01.003. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.