Background: The coronavirus disease 2019 (COVID-19) pandemic has had far-reaching effects on health care delivery in the United States, ranging from postponement of elective care (1) to increases in the use of telemedicine (2). However, little is known about how the pandemic has affected the treatment of behavioral and psychiatric conditions.
Objective: To characterize quarterly telemedicine and office-based visits from the first quarter of 2018 (2018Q1) through the second quarter of 2020 (2020Q2).
Methods and Findings: We used IQVIA's National Disease and Therapeutic Index—a proprietary, 2-stage, stratified (by specialty and geographic area), nationally representative audit of ambulatory care in the United States—to characterize quarterly telemedicine and office-based visits from 2018Q1 through 2020Q2. Telemedicine visits included those taking place by telephone as well as through web-based platforms. The National Disease and Therapeutic Index involves approximately 4800 physicians who use an electronic form to record details of all patient contacts during 2 consecutive workdays per quarter and generates more than 350 000 annual contact records. Reporting days are randomly assigned to ensure that all workdays in a report period are covered; Saturdays, Sundays, and holidays are assigned as reporting days to physicians practicing on those days. We restricted our analyses to primary care and psychiatric visits and focused on care for 6 of the most prevalent behavioral and psychiatric conditions in the United States: anxiety, depression, overactivity, bipolar disorder, insomnia, and opioid use disorder (3).
Total visits across settings for the 6 conditions decreased from an average of 15.9 million during the first quarter of 2018 and 2019 (2018/2019Q1) to 13.0 million in 2020Q1 (percentage change, −18%) before increasing to 15.8 million in 2020Q2, which is near the 2018/2019Q2 average of 15.7 million (Figure and Table). Office-based visits decreased from an average quarterly volume of 15.5 million before 2020 to 11.9 million in 2020Q1 and 5.3 million in 2020Q2. During the same period, telemedicine visits accounted for fewer than 3% of visits before 2020 (approximately 0.4 million), 9% during 2020Q1 (1.1 million), and 66% during 2020Q2 (10.5 million). Generally, there were no significant variations in patients' sex or race/ethnicity during the same period; however, patients who had telemedicine visits were younger, especially in 2020Q2. Most visits were subsequent rather than new visits, even after the shift to telemedicine starting in 2020 (Figure), suggesting that telemedicine served primarily to accommodate persons already established in care.
Figure. Quarterly trends in telemedicine and office-based visits for behavioral and psychiatric conditions in the United States, 2018–2020 (.
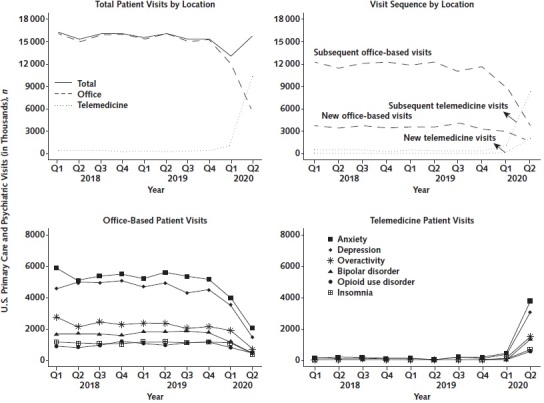
n = 16 067 unweighted total visits). Q = quarter. Source: IQVIA's National Disease and Therapeutic Index, 2018–2020, based on a sampling frame of more than 500 000 physicians from the American Medical Association and the American Osteopathic Association master lists. Estimates are weighted based on survey weights provided by the National Disease and Therapeutic Index. Conditions were defined on the basis of having International Classification of Diseases, Ninth Revision codes listed from a visit. Data were based on primary care (family practice, general practice, geriatrics, internal medicine, and pediatrics) and psychiatrist visits.
Table. Telemedicine and Office-Based Visits for Behavioral and Psychiatric Conditions in the United States During the First Two Quarters of 2018–2020 (n = 9540 Unweighted Total Visits)*.
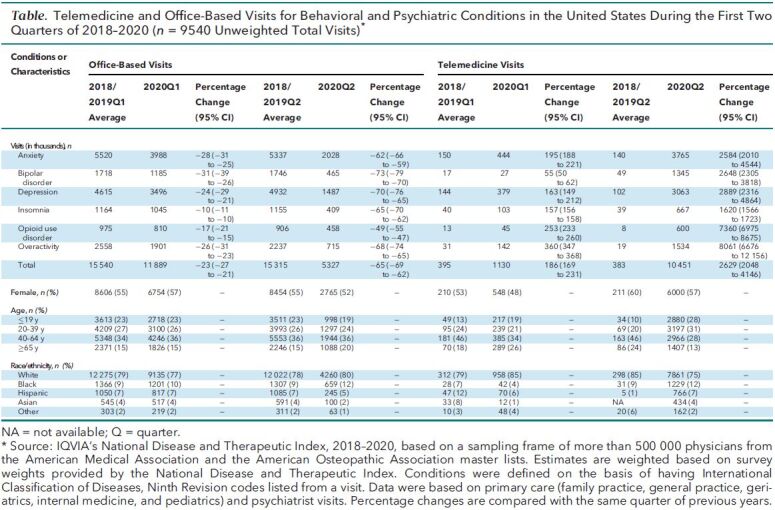
From 2018/2019Q1 to 2020Q1, there were decreases of 17% to 31% in office-based visits across the 6 conditions (Figure and Table). Office-based visits decreased further, by 49% (opioid use disorder) to 73% (bipolar disorder), between 2018/2019Q2 and 2020Q2. By contrast, telemedicine visits increased by 55% (bipolar disorder) to 360% (overactivity) between 2018/2019Q1 and 2020Q1 and by 1620% (insomnia) to 8061% (overactivity) between 2018/2019Q2 and 2020Q2.
Discussion: The COVID-19 pandemic has been associated with large decreases in office-based visits for behavioral and psychiatric conditions, although by 2020Q2 these had been offset by large increases in telemedicine visits among the conditions examined. Given concerns about the potential deleterious effects of the pandemic on the behavioral and psychiatric needs of vulnerable populations as well as the implementation of policies to mitigate such harms (4), the increases in telemedicine visits are noteworthy. However, further work is needed to establish how effectively telemedicine can reduce logistic and social barriers to mental health care. It is also unclear if the increases we note are sufficient to address the increased prevalence of depressive and anxiety symptoms as a result of the COVID-19 pandemic (5).
Despite our analyses' insights, they provide a snapshot of dynamic processes and, like all surveys, may be prone to measurement error and bias. These limitations notwithstanding, our findings suggest profound shifts in care patterns for common behavioral and psychiatric illnesses in the United States and underscore the importance of further work to assess how different treatment settings, including the delivery of care through telemedicine platforms, may affect patients' experiences and health outcomes.
Footnotes
This article was published at Annals.org on 17 November 2020
References
- 1.Cutler D. How will COVID-19 affect the health care economy? JAMA Forum. 9 April 2020. Accessed at https://jamanetwork.com/channels/health-forum/fullarticle/2764547 on 2 June 2020. [DOI] [PubMed]
- 2. Alexander GC , Tajanlangit M , Heyward J , et al. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3:e2021476. [PMID: ] doi: 10.1001/jamanetworkopen.2020.21476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ashman JJ , Rui P , Okeyode T . Characteristics of office-based physician visits, 2016. NCHS Data Brief. 2019:1-8. [PMID: ] [PubMed] [Google Scholar]
- 4. Alexander GC , Stoller KB , Haffajee RL , et al. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19 [Editorial]. Ann Intern Med. 2020;173:57-58. doi: 10.7326/M20-1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Amsalem D , Dixon LB , Neria Y . The coronavirus disease 2019 (COVID-19) outbreak and mental health: current risks and recommended actions. JAMA Psychiatry. 2020. [PMID: ] doi: 10.1001/jamapsychiatry.2020.1730 [DOI] [PubMed] [Google Scholar]


