Pandemics, including the COVID-19 pandemic, disrupt traditional health care operations by overwhelming system resource capacity. This article describes the development and rapid deployment of a virtual hospital program within a large health care system and their early caring for patients with COVID-19.
Abstract
Background:
Pandemics disrupt traditional health care operations by overwhelming system resource capacity but also create opportunities for care innovation.
Objective:
To describe the development and rapid deployment of a virtual hospital program, Atrium Health hospital at home (AH-HaH), within a large health care system.
Design:
Prospective case series.
Setting:
Atrium Health, a large integrated health care organization in the southeastern United States.
Patients:
1477 patients diagnosed with coronavirus disease 2019 (COVID-19) from 23 March to 7 May 2020 who received care via AH-HaH.
Intervention:
A virtual hospital model providing proactive home monitoring and hospital-level care through a virtual observation unit (VOU) and a virtual acute care unit (VACU) in the home setting for eligible patients with COVID-19.
Measurements:
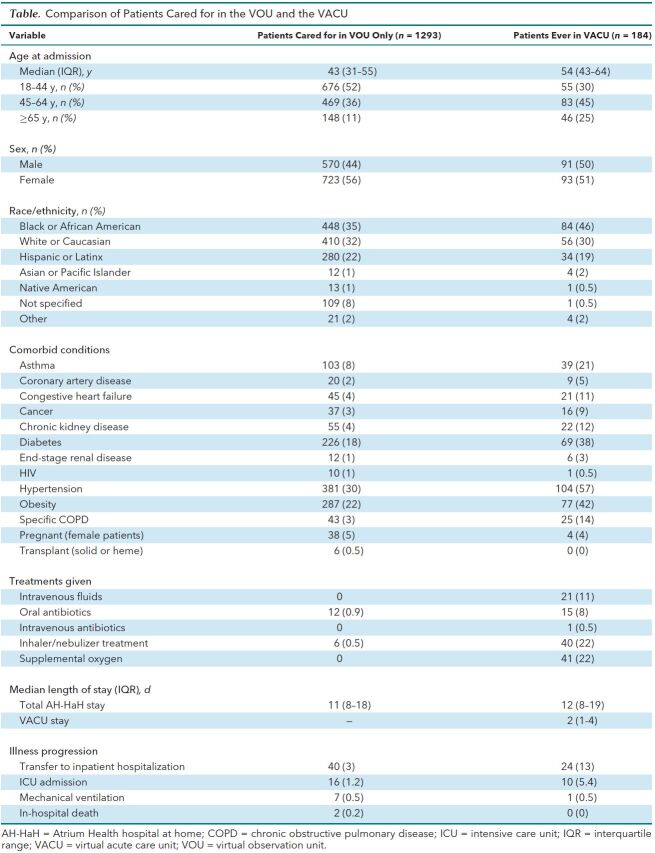
Patient demographic characteristics, comorbid conditions, treatments administered (intravenous fluids, antibiotics, supplemental oxygen, and respiratory medications), transfer to inpatient care, and hospital outcomes (length of stay, intensive care unit [ICU] admission, mechanical ventilation, and death) were collected from electronic health record data.
Results:
1477 patients received care in either the AH-HaH VOU or VACU or both settings, with a median length of stay of 11 days. Of these, 1293 (88%) patients received care in the VOU only, with 40 (3%) requiring inpatient hospitalization. Of these 40 patients, 16 (40%) spent time in the ICU, 7 (18%) required ventilator support, and 2 (5%) died during their hospital admission. In total, 184 (12%) patients were ever admitted to the VACU, during which 21 patients (11%) required intravenous fluids, 16 (9%) received antibiotics, 40 (22%) required respiratory inhaler or nebulizer treatments, 41 (22%) used supplemental oxygen, and 24 (13%) were admitted as an inpatient to a conventional hospital. Of these 24 patients, 10 (42%) required ICU admission, 1 (3%) required a ventilator, and none died during their hospital admission.
Limitation:
Generalizability is limited to patients with a working telephone and the ability to comply with the monitoring protocols.
Conclusion:
Virtual hospital programs have the potential to provide health systems with additional inpatient capacity during the COVID-19 pandemic and beyond.
Primary Funding Source:
Atrium Health.
Pandemics pose unique challenges to traditional health care delivery (1). What started in December 2019 as a local outbreak of viral pneumonia caused by a novel, severe acute respiratory coronavirus 2 (SARS-CoV-2) in Wuhan, China, has rapidly progressed to a once-in-a-century worldwide pandemic of coronavirus disease 2019 (COVID-19) (2, 3). As SARS-CoV-2 continues to spread, health systems face the ongoing risk for becoming overwhelmed by increases in COVID-19 cases. The strain on such resources as hospital and intensive care unit (ICU) bed capacity, ventilators, personal protective equipment, and health care staff threatens the quality and safety of care delivery (4, 5). To increase capacity during the pandemic and minimize SARS-CoV-2 exposures, health systems have relied heavily on leveraging telemedicine technology (6–9). One strategy to extend a hospital's bed capacity is the expansion of virtual care services that can be provided in patients' homes instead of a traditional hospital (9). Hospital at home (HaH), a care model that provides acute hospital-level care in patients' homes, has been well characterized (10–13). Controlled trials and subsequent meta-analyses have suggested the efficacy of HaH, demonstrating noninferior or even superior mortality, readmission, and length of stay outcomes compared with traditional hospitalization for heterogeneous patient populations (14–17). However, templates for how to effectively implement and rapidly scale virtual strategies for providing hospital-level care at home are lacking.
Emerging care models, such as HaH (18), face significant implementation challenges, with health systems struggling to adopt or scale these models as part of routine care or produce meaningful population outcomes. Reasons for low adoption include misaligned or lack of financial incentives and challenges inherent in implementing a complex intervention. For example, even when home hospitalization models have been implemented in the United States in study settings or those with aligned payment incentives, low participation rates have been ubiquitous (ranging from 7 to 15 patients per month) (11, 13–17, 19–21).
We describe how Atrium Health adapted a preexisting hospital transition program and telemedicine program into a virtual hospital that provided comprehensive services to almost two thirds of the health system's SARS-CoV-2–positive patient population. This virtual model, Atrium Health hospital at home (AH-HaH), enhanced existing primary care by providing daily telemonitoring by a nurse for all low-acuity patients to proactively identify disease progression and escalate care as needed. For higher-acuity patients who would otherwise be hospitalized, it provided the option for hospital-level care in the home by deploying a hybrid of virtual and in-person services. In the planning and execution of AH-HaH, we preemptively addressed challenges inherent to implementing innovative care models by focusing on 1) reliance on a virtual care platform; 2) data-driven patient identification; 3) a health information technology foundation and workflows that mirror routine inpatient care; 4) a health literate communication and marketing strategy to support informed decision making; 5) expansion of an existing community paramedicine and care management program to deliver in-person care and monitor patients; and 6) rapid deployment of inexpensive, low-tech remote monitoring kits. We present the strategy associated with the successful and rapid launch of AH-HaH to aid other health systems planning similar responses.
Methods
Setting
Atrium Health is one of the nation's largest integrated health care systems, organized as a not-for-profit academic learning health system spanning 3 states with 50 hospitals, 44 urgent care centers, 45 emergency departments, and 14 million patient encounters annually. Atrium Health had existing plans to deploy a multidisciplinary team to provide acute inpatient-level care to patients at their homes beginning later in 2020. In early March 2020, as it became clear that spread of COVID-19 across the United States was imminent, Atrium Health accelerated these plans so that the AH-HaH could become a reliable care option with significant capacity for patients with COVID-19.
At Atrium Health, AH-HaH is an extension of our hospital medicine division's existing transition services program. This multidisciplinary program, established 5 years ago, serves patients who are discharged from the hospital and are at high risk for readmission. A robust virtual care platform enables the team to deliver care to this vulnerable patient population through frequent paramedicine and virtual in-home visits with proactive escalation and de-escalation of care intensity. Patient management and accountability for AH-HaH are housed within a dedicated group of virtual hospital medicine providers and nurses, who provide 24/7 coverage and monitoring with other specialties linked as needed for virtual consultations. This foundational virtual infrastructure served as the basis for a hub-and-spoke virtual hospital model.
Development of AH-HaH
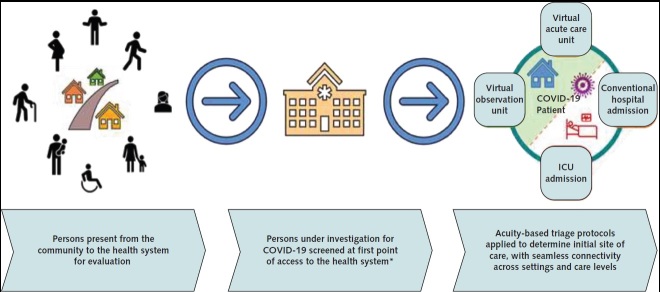
To plan, launch, and sustain the virtual hospital model, we collaborated with numerous stakeholders from hospital medicine, primary care, nursing, community paramedicine, pharmacy, care management, social work, information and analytic services, research, care transformation, innovation, and administrative leadership. Together, we developed templates for data-driven patient identification and eligibility assessments, patient- and provider-facing information, health information technology integration, and workflows to manage patients in AH-HaH that mirrored traditional inpatient care (Figure 1).
Figure 1. Seamless integrated workflow of the Atrium Health hospital at home.
COVID-19 = coronavirus disease 2019; ICU = intensive care unit.
* Primary care clinics (in person or virtual), urgent care, emergency departments, or external testing sites.
Within AH-HaH, we created 2 virtual “floors” defined by the level of acuity. These floors are staffed with separate care teams that include physicians, advanced practice providers (APPs), registered nurses (RNs), pharmacists, social workers, and community paramedics. The “first floor,” or virtual observation unit (VOU), is designed for low-acuity patients who can be managed remotely with daily telemedicine-supported symptom monitoring by RNs. The “second floor,” or virtual acute care unit (VACU), is designed for patients who would otherwise have been admitted to a traditional brick-and-mortar hospital providing inpatient care, such as oxygen, medical treatments, daily virtual physician rounds, vital sign monitoring, twice-daily nursing assessments, and daily paramedic visits. We primarily focus on describing the AH-HaH VACU because it most closely resembles other frameworks for home-based hospital-level care.
Screening for Program Eligibility
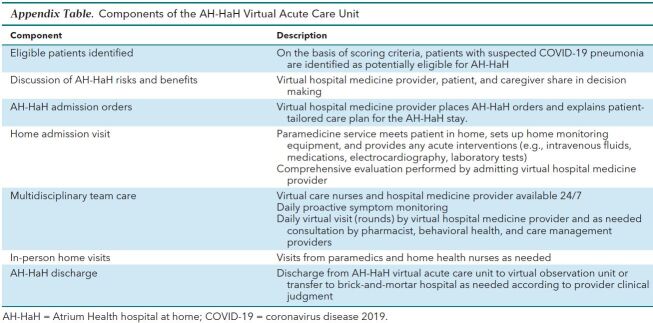
Adoption of new care models is often challenged by unfamiliarity with program eligibility, services, and logistics, leading most providers to default to the care option with which they are most familiar—in this case, traditional hospitalization (22). To overcome this implementation barrier, we embedded evidence-based scoring algorithms directly within the electronic health record (EHR) workflow for COVID-19 testing. This point-of-care decision support created a standardized process, which allowed every patient tested at Atrium Health's mobile COVID-19 test sites, urgent cares, and emergency departments to be evaluated for AH-HaH eligibility (23, 24) (Appendix Table, available at Annals.org).
Appendix Table. Components of the AH-HaH Virtual Acute Care Unit.
To consider patients for traditional hospitalization, VOUa, or VACU, we used prespecified thresholds in 2 well-known pneumonia severity scoring tools: the modified DSCRB-65 (comorbid disease, oxygen saturation, confusion, respiratory rate ≥30 breaths/min, systolic blood pressure <90 mm Hg or diastolic blood pressure ≤60 mm Hg , age ≥65 years) (25) and the American Thoracic Society/Infectious Diseases Society of America Major and Minor Criteria for Severe Pneumonia (26) (Figure 2). All patients who were not living in an institutional setting and who had a positive SARS-CoV-2 test and a DSCRB-65 score of 0 to 2 were offered enrollment into the VOU. Patients with a DSCRB-65 score greater than 2 and no major and 3 or fewer minor criteria for severe pneumonia were considered by the testing provider for VACU admission. In addition to standard provider education (e-mailed instructions and group meetings), the EHR included a reminder for the provider that AH-HaH was an available care option. As with any clinical decision support, a provider's judgment always superseded the scoring triage system.
Figure 2. Initial risk scoring of COVID-19 for appropriate patient placement.
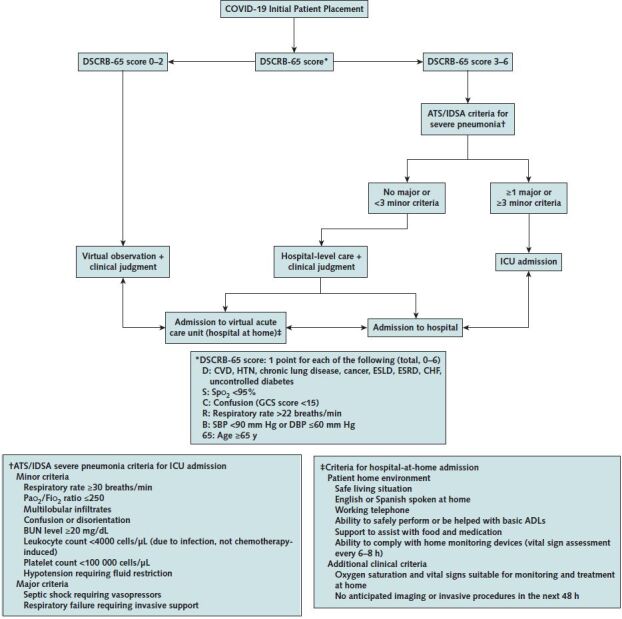
ADL = activity of daily living; ATS/IDSA = American Thoracic Society/Infectious Diseases Society of America; BUN = blood urea nitrogen; CHF = congestive heart failure; COVID-19 = coronavirus disease 2019; CVD = cardiovascular disease; DBP = diastolic blood pressure; ESLD = end-stage liver disease; ESRD = end-stage renal disease; GCS = Glasgow Coma Scale; HTN = hypertension; ICU = intensive care unit; SBP = systolic blood pressure.
Patients identified as potentially eligible for VACU on the basis of these clinical triage scores were then evaluated by the testing site provider for additional AH-HaH patient environmental criteria (ability to comply with home monitoring devices for assessment of vital signs every 6 to 8 hours, ability to safely perform or be helped with basic activities of daily living, safe living situation, English or Spanish spoken by the patient or someone at home, a working phone, the support necessary to assist with food and medication administration) and clinical criteria (for example, no anticipated need for imaging or invasive procedures in the next 48 hours). The AH-HaH “quarterback” physician was readily available to review cases or questions through provider to provider phone calls.
Atrium Health Hospital at Home Interventions
Every patient admitted to the VACU is provided with a home monitoring kit that includes a blood pressure cuff, pulse oximeter, and thermometer. Along with the medical equipment, all patients are given written instructions in English or Spanish on how to use each device and a phone number to call for help. These devices are delivered to the patient at the first in-home mobile clinician visit. Given the large geographic footprint of Atrium Health, storage and retrieval of the medical device kits is facilitated with a central distribution center in the region and managed within the existing storage, supply chain, and distribution network.
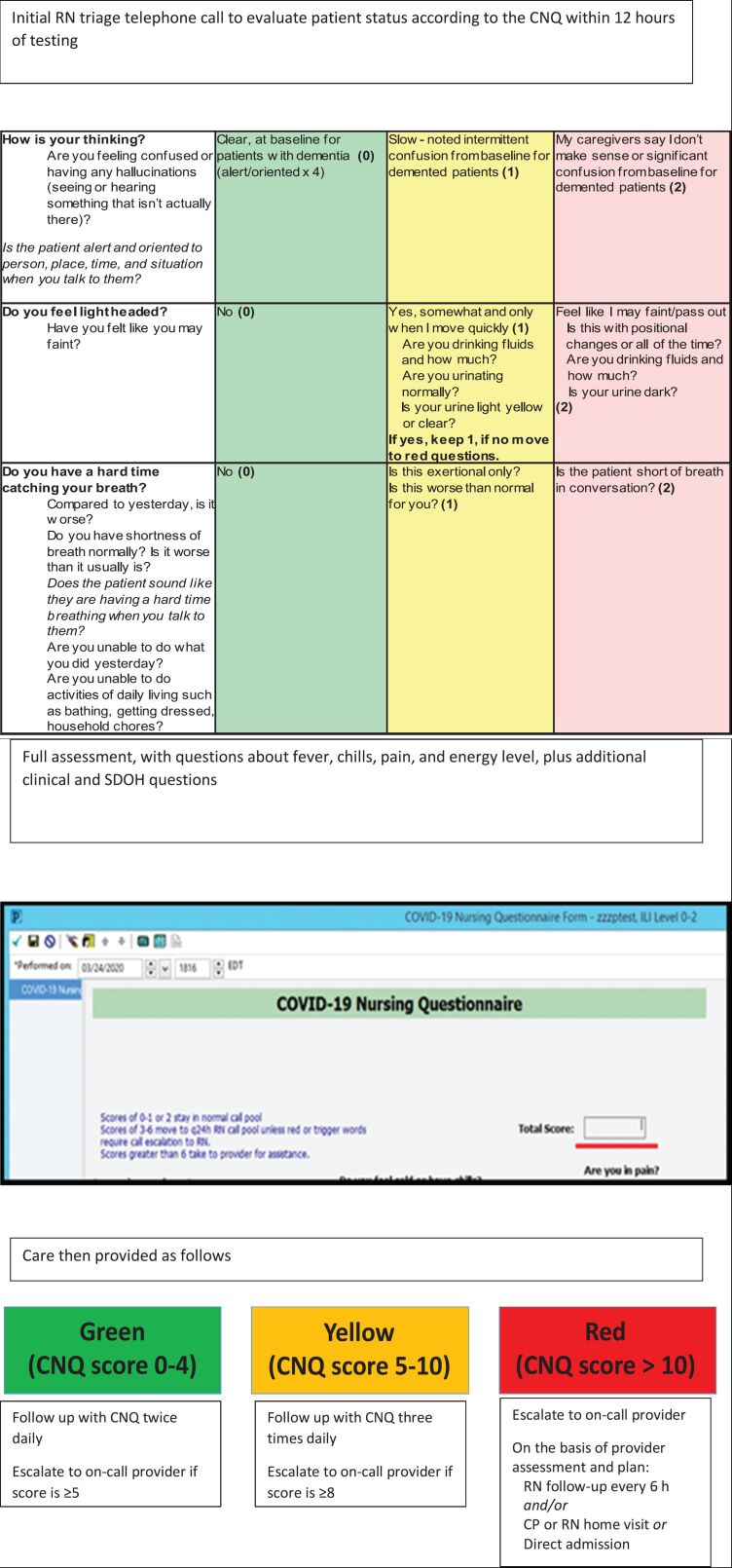
Implementation of a telemedicine mobile app interface allows patients to immediately escalate their concerns 24 hours a day through telephone calls directly to RNs or point-to-point messaging, guided by predefined symptom algorithms with temperature and pulse oximetry cutoffs. The virtual health care team follows up within 12 hours of VACU admission and telephones the patient to administer a 12-question structured COVID-19 nursing questionnaire (CNQ) evaluation in a Cerner EHR PowerForm developed to capture data, evaluate disease progression, and dictate a pathway of standardized care escalation and de-escalation. The CNQ is then readministered on the basis of the case progression and patient answers (Appendix Figure 1, available at Annals.org).
Appendix Figure 1. Atrium Health hospital at home telephone monitoring protocol and COVID-19 Nursing Questionnaire (CNQ).
COVID-19 = coronavirus disease 2019; CP = community paramedic; RN = registered nurse; SDOH = social determinants of health.
After VACU admission, a team of mobile clinicians (paramedics and RNs) visits the patient's home within the first 24 hours. The actual timing is based on the patient's condition to enable a secure virtual visit with the covering physician by using Vidyo videoconferencing software. Our mobile clinicians have a formulary of therapies available, including intravenous fluids, intravenous and oral antiemetics, respiratory medications, and other medications to treat VACU patients as needed per standing protocols or provider orders. The mobile clinicians also can perform electrocardiography, blood samples for laboratory tests, and other tests if needed. The mobile clinicians also provide support and human touch for patients during an otherwise isolating and vulnerable time. These mobile clinician and virtual provider visits continue daily until a patient's clinical condition improves to the point of de-escalation to the VOU for ongoing mobile app-driven symptom monitoring and telephonic CNQ nurse follow-up.
Staff Structure of the AH-HaH
Initially, AH-HaH utilized existing staff who were redeployed from their usual duties owing to the pandemic, but over time it has transitioned to reliance on newly created, dedicated roles. Staffing levels for the AH-HaH service depended on the daily patient census. In the VACU, there was a daily census of 20 to 30 patients, and we targeted staffing around 12 to 13 patients per virtual rounding physician, 1 quarterback physician dedicated to evaluating patient eligibility and admissions, 1 covering nocturnist physician, 1 nocturnist RN, 2 or 3 daytime RNs, and 10 to 12 community paramedics. In addition, on Monday through Friday, 1 pharmacist, 1 social worker, 1 palliative care APP, and 1 behavioral health APP were available for virtual consultation. The VOU was staffed only by virtual RNs (day) and certified medical assistants (night); availability of a virtual primary care physician was scheduled each day and night to be available for questions from the care team.
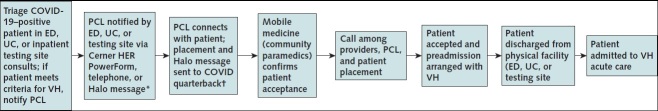
Integration of Health Information
To match patient volume with the correct health care delivery capacity to provide in-home visits across the broad geography of Atrium Health using our mobile clinician team, we recognized the need to eliminate confusing back-and-forth communications from the emergency department and urgent care admission sites. We developed a COVID-19 transfer PowerForm within the EHR that securely transferred both patient demographic data and contact information for the patient's recovery location to our Atrium Health centralized patient transfer and coordination center (Appendix Figure 2, available at Annals.org). Utilizing a secure communications platform workflow (Halo Health, Inc.), immediate messaging to the AH-HaH quarterback physician relayed the patient data to the virtual health care team to determine mobile resource availability in real time. Efficient management of the distribution of mobile clinicians is achieved using GPS-enabled, web-based fleet management software (Geotab, Inc.). If mobile health care resources were available, the admitting emergency department or urgent care setting would then be connected via the centralized patient transfer and coordination center to the AH-HaH admitting physician to discuss the patient's clinical and environmental factors to ensure that patient could be safely managed in the AH-HaH (Figure 3). When AH-HaH mobile health care resources were not available for that specific patient, then the admitting emergency department or urgent care provider would be connected to the admitting physician at the brick-and-mortar hospital in standard fashion; however, we never had to do this, owing to adequate availability of resources.
Appendix Figure 2. Atrium Health hospital at home virtual acute care unit PowerForm for transfer of patients with coronavirus disease 2019.
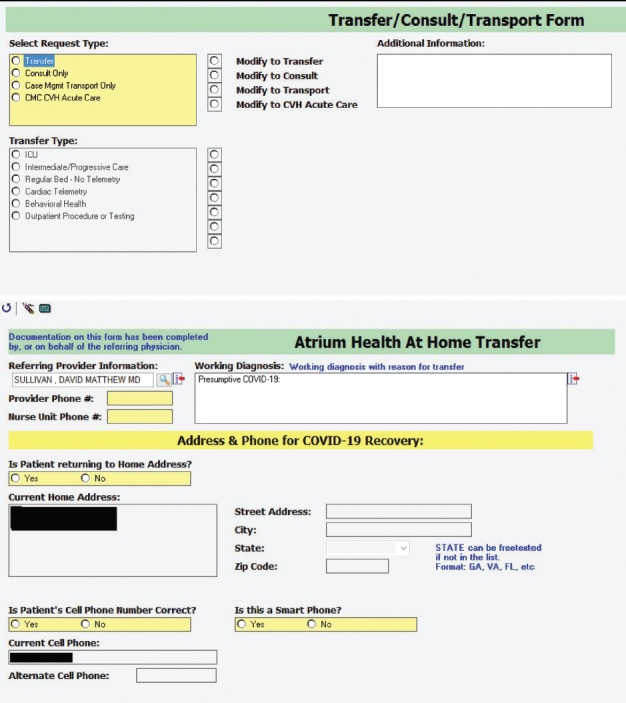
Figure 3. Atrium Health hospital at home virtual acute care unit admission process.
Halo is the secure messaging service used at Atrium Health; the PCL is the centralized communication center for health care staff regarding patient transfers. ED = emergency department; HER = electronic health record; PCL = physician connection line; UC = urgent care; VH = virtual hospital.
The EHR workflow was integrated into the AH-HaH by creating a virtual facility location within the system's EHR, so that the look, feel, and background functionality mirrored that of brick-and-mortar facilities. This allows for a seamless interface for patient care across encounters; creates a familiar structure for patients to be admitted, discharged, and transferred to other care locations from the AH-HaH; and allows our Atrium Health virtual care team to use standard physician, APP, and nurse workflows for patient assignment, patient tracking, clinical documentation, and ordering despite the patient's home location. In line with COVID-19 disease progression, the option exists within the EHR workflows to escalate the patient from the VOU or VACU via direct admission to our brick-and-mortar hospital beds and to transfer patients from VACU to the VOU for ongoing, less acute telephonic monitoring. The care teams used daily proactive telemonitoring software (GetWellNetwork, Inc.), which generated frequent reminders for patients to report signs and symptoms to the virtual RN and facilitated direct communications from the patient to the care team to assist in clinical management.
Data Collection
We collected data from the EHR to describe patients with COVID-19 who received care through AH-HaH. Patient characteristics included age, gender, race/ethnicity, and comorbid health conditions at the time of AH-HaH admission. Potential treatments received through AH-HaH VACU included intravenous fluids, antibiotics, oxygen, and respiratory therapies. We evaluated transfer to inpatient care and hospital outcomes, including length of stay, ICU admission, mechanical ventilation, and hospital mortality.
Statistical Analysis
Univariate statistics were calculated for continuous (median [interquartile range]) and categorical (number [percentage]) variables to describe AH-HaH patients and their outcomes.
Role of the Funding Source
This project was sponsored by Atrium Health. No other sponsors were involved in the design or conduct of the study, analysis of the data, or the decision to submit the manuscript for publication.
Results
Between 23 March and 7 May 2020, 2299 patients tested positive for COVID-19 in our health system and 1477 patients received care in the AH-HaH (64%). Of these 1477 patients, 1293 received all of their care (limited to RN telemonitoring) in the VOU and 184 received hospital-level care in the VACU (Table). The median age of patients was 43 years in the VOU and 54 years in the VACU. In both groups, most patients were female and African American. Patients who received care in the VACU had a higher proportion of comorbid conditions at baseline than patients in the VOU; these conditions included asthma, congestive heart failure, diabetes, hypertension, chronic obstructive pulmonary disease, and obesity. The median total length of stay in the AH-HaH was 11 days for patients in the VOU and 12 days for patients ever admitted to the VACU.
Table. Comparison of Patients Cared for in the VOU and the VACU.
Of the 1293 (88%) patients who were admitted to the VOU only, 40 required escalation of care from the VOU to inpatient hospitalization. Among those 40 transferred patients, 16 required ICU admission, 7 required mechanical ventilation, and 2 died during their hospital admission. Of the 184 (12%) patients ever admitted to the VACU, 21 required IVF, 16 received antibiotics (intravenous in 1 patient and oral in 15 patients), 40 required respiratory inhaler or nebulizer medications, and 41 used supplemental oxygen 1 to 4 L/min during the VACU stay. None of the patients in the VACU received noninvasive ventilation because they were escalated to higher level in-hospital care at the point of requiring greater than 4 L of oxygen. A total of 24 patients required transfer from the VACU to an inpatient hospital, of whom 10 required ICU admission, 1 required mechanical ventilation, and none died during their hospital admission.
Discussion
We describe the rapid implementation of a virtual hospital for patients with COVID-19. The purpose of the AH-HaH is to provide patients with COVID-19 with high-quality daily medical care and monitoring while limiting exposure to other patients and providers and allow for the expansion of the health system's acute-care capacity. The program was planned and launched within 2 weeks, successfully keeping most patients in their home setting; only 3% of VOU patients and 13% of VACU patients required admission to a brick-and-mortar hospital. In the absence of VACU availability, all 160 VACU patients who did not require transfer to a brick-and-mortar hospital can be viewed by extension as traditional hospital beds saved. The AH-HaH maintained a consistent patient census for the first 6 weeks as COVID-19 cases spread locally, with built-in capacity to expand its census by another 10-fold as a safety net for the system.
We recognized and overcame inherent challenges to implementing new care models. First, we built a scalable, EHR-centered platform that mandated a data-informed patient eligibility assessment. Second, we used a virtual telemedicine platform to maximize provider scalability. Finally, we operationalized a patient- and resource-centric communication strategy and provided daily electronic monitoring with an overlay of telephonic nurse-to-patient structured proactive communication and monitoring.
Our virtual care model includes several additional benefits specific to the COVID-19 pandemic. By “forward triaging” (8) patients with virtual assessments and directly admitting patients from satellite testing centers to the AH-HaH, we kept patients out of the emergency department, thus minimizing exposure of health care staff and other patients in the traditional hospital setting. In addition, minimizing health care staff exposure meant that less personal protective equipment was needed at a time of scant resources. Most of the team was virtual and centrally located; this care model allows virtual redeployment of health care provider staff with high-risk comorbid conditions or immunosuppression, who would otherwise be unable to safely work. Finally, we expect to realize the potential long-term benefits a virtual hospital may provide in terms of reduced health care costs, reduced readmissions, and improved patient health outcomes for non–COVID-19 diagnoses (17).
Our implementation of the AH-HaH has limitations. First, our eligibility criteria are intentionally broad, but they require patients to have a working telephone, English or Spanish spoken by someone at home if the patient does not, and the ability to comply with the monitoring protocols. Second, our AH-HaH implementation was facilitated in part by the existing infrastructure and collaborative culture developed through prior adoption of other transitional and virtual care programs in our system; thus, generalizability may be limited by requirements for a robust technology platform, a supply of mobile health care clinicians (such as community paramedics), home monitoring equipment, and an interoperable EHR. Yet, our description provides a framework for other health systems to examine adaptation of virtual care delivery to best fit within diverse local contexts. Finally, the sustainability of novel care delivery options such as AH-HaH will be threatened without permanent insurance reimbursement solutions to cover hospital care delivered in a home setting. Value-based payment models may serve to keep forward momentum for virtual hospital care until there is broader payment reform (22, 27, 28).
In conclusion, we found that a virtual hospital can be a viable part of a health system's surge planning and provides an important alternative strategy to care for patients with COVID-19 by mitigating some risks associated with traditional inpatient management. Our framework leveraging a virtual platform, health IT, and data-informed decision making can overcome the challenges inherent to implementing a novel care model. This framework can guide other health systems as they innovate to care for their communities and may also serve as the basis for the new paradigm of medicine beyond the COVID-19 pandemic.
Footnotes
This article was published at Annals.org on 11 November 2020
References
- 1. Rebmann T. Infectious disease disasters: bioterrorism, emerging infections, and pandemics. APIC Text of Infection Control and Epidemiology. 5 March 2020. Accessed at https://text.apic.org/toc/community-based-infection-prevention-practices/infectious-disease-disasters-bioterrorism-emerging-infections-and-pandemics on 4 November 2020.
- 2. Cucinotta D , Vanelli M . WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157-160. [PMID: ] doi: 10.23750/abm.v91i1.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Spinelli A , Pellino G . COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;107:785-787. [PMID: ] doi: 10.1002/bjs.11627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fauci AS , Lane HC , Redfield RR . Covid-19—navigating the uncharted [Editorial]. N Engl J Med. 2020;382:1268-1269. [PMID: ] doi: 10.1056/NEJMe2002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ranney ML , Griffeth V , Jha AK . Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382:e41. [PMID: ] doi: 10.1056/NEJMp2006141 [DOI] [PubMed] [Google Scholar]
- 6. Carenzo L , Costantini E , Greco M , et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020;75:928-934. [PMID: ] doi: 10.1111/anae.15072 [DOI] [PubMed] [Google Scholar]
- 7. Verelst F , Kuylen E , Beutels P . Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, March 2020. Euro Surveill. 2020;25. [PMID: ] doi: 10.2807/1560-7917.ES.2020.25.13.2000323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hollander JE , Carr BG . Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679-1681. [PMID: ] doi: 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 9. Grabowski DC , Joynt Maddox KE . Postacute care preparedness for COVID-19: thinking ahead. JAMA. 2020;323:2007-2008. [PMID: ] doi: 10.1001/jama.2020.4686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leff B , Burton L , Bynum JW , et al. Prospective evaluation of clinical criteria to select older persons with acute medical illness for care in a hypothetical home hospital. J Am Geriatr Soc. 1997;45:1066-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 11. Federman AD , Soones T , DeCherrie LV , et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018;178:1033-1040. [PMID: ] doi: 10.1001/jamainternmed.2018.2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leff B . Defining and disseminating the hospital-at-home model. CMAJ. 2009;180:156-7. [PMID: ] doi: 10.1503/cmaj.081891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Leff B , Burton L , Mader SL , et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005;143:798-808 [DOI] [PubMed] [Google Scholar]
- 14. Shepperd S , Iliffe S , Doll HA , et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9:CD007491. [PMID: ] doi: 10.1002/14651858.CD007491.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shepperd S , Iliffe S . Hospital at home versus in-patient hospital care. Cochrane Database Syst Rev. 2005:CD000356. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 16. Shepperd S , Doll H , Angus RM , et al. Avoiding hospital admission through provision of hospital care at home: a systematic review and meta-analysis of individual patient data. CMAJ. 2009;180:175-82. [PMID: ] doi: 10.1503/cmaj.081491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Levine DM , Ouchi K , Blanchfield B , et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172:77-85. doi: 10.7326/M19-0600 [DOI] [PubMed] [Google Scholar]
- 18. Leff B , Burton L , Guido S , et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999;47:697-702. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 19. Mader SL , Medcraft MC , Joseph C , et al. Program at home: a Veterans Affairs Healthcare Program to deliver hospital care in the home. J Am Geriatr Soc. 2008;56:2317-22. [PMID: ] doi: 10.1111/j.1532-5415.2008.02006.x [DOI] [PubMed] [Google Scholar]
- 20. Klein S, Hostetter M, McCarthy D. The hospital at home model: bringing hospital-level care to the patient. Commonwealth Fund. 22 August 2016. Accessed at www.commonwealthfund.org/publications/case-study/2016/aug/hospital-home-model-bringing-hospital-level-care-patient on 5 May 2020.
- 21. Cryer L , Shannon SB , Van Amsterdam M , et al. Costs for ‘hospital at home’ patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood). 2012;31:1237-43. [PMID: ] doi: 10.1377/hlthaff.2011.1132 [DOI] [PubMed] [Google Scholar]
- 22. Gupta DM , Boland RJ Jr , Aron DC . The physician's experience of changing clinical practice: a struggle to unlearn. Implement Sci. 2017;12:28. [PMID: ] doi: 10.1186/s13012-017-0555-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McWilliams A , Roberge J , Anderson WE , et al. Aiming to improve readmissions through InteGrated hospital transitions (AIRTIGHT): a pragmatic randomized controlled trial. J Gen Intern Med. 2019;34:58-64. [PMID: ] doi: 10.1007/s11606-018-4617-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kowalkowski M , Chou SH , McWilliams A , et al. Atrium Health ACORN Investigators. Structured, proactive care coordination versus usual care for Improving Morbidity during Post-Acute Care Transitions for Sepsis (IMPACTS): a pragmatic, randomized controlled trial. Trials. 2019;20:660. [PMID: ] doi: 10.1186/s13063-019-3792-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dwyer R , Hedlund J , Henriques-Normark B , et al. Improvement of CRB-65 as a prognostic tool in adult patients with community-acquired pneumonia. BMJ Open Respir Res. 2014;1:e000038. [PMID: ] doi: 10.1136/bmjresp-2014-000038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Metlay JP , Waterer GW , Long AC , et al. Diagnosis and treatment of adults with community-acquired pneumonia. an official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45-e67. [PMID: ] doi: 10.1164/rccm.201908-1581ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Centers for Medicare & Medicaid Services. Medicare telemedicine health care provider fact sheet. CMS.gov. 17 May 2020. Accessed at www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet on 5 May 2020.
- 28. Liao JM , Navathe A , Press MJ . Hospital-at-home care programs-is the hospital of the future at home. JAMA Intern Med. 2018;178:1040-1041. [PMID: ] doi: 10.1001/jamainternmed.2018.2566 [DOI] [PubMed] [Google Scholar]