Abstract
Superficial and life-threatening invasive Candida infections are a major clinical challenge in hospitalized and immuno-compromised patients. Emerging drug-resistance among Candida species is exacerbated by the limited availability of antifungals and their associated side-effects. In the current review, we discuss the application of probiotic yeasts as a potential alternative/ combination therapy against Candida infections. Preclinical studies have identified several probiotic yeasts that effectively inhibit virulence of Candida species, including Candida albicans, Candida tropicalis, Candida glabrata, Candida parapsilosis, Candida krusei and Candida auris. However, Saccharomyces cerevisiae var. boulardii is the only probiotic yeast commercially available. In addition, clinical studies have further confirmed the in vitro and in vivo activity of the probiotic yeasts against Candida species. Probiotics use a variety of protective mechanisms, including posing a physical barrier, the ability to aggregate pathogens and render them avirulent. Secreted metabolites such as short-chain fatty acids effectively inhibit the adhesion and morphological transition of Candida species. Overall, the probiotic yeasts could be a promising effective alternative or combination therapy for Candida infections. Additional studies would bolster the application of probiotic yeasts.
Keywords: Candida albicans, non-albicans Candida species, Candida auris, Saccharomyces boulardii, Saccharomyces cerevisiae, aromatic alcohols
1. Introduction
The fermented foods are a rich source of beneficial microorganisms, and they have a long history of exhibiting health benefits, particularly S. cerevisiae and lactic acid bacteria (LAB). Their safety is evidenced by consumption of fermented foods and beverages over centuries. Today, it is well accepted that the rich microbial profile of fermented food provides more than just nutrition. For example, functional activity of microorganisms in food helps enhance the bio-availability of micronutrients, improving the sensory quality and shelf life of the food, degrading anti-nutritive factors (such as trypsin inhibitors and phytate degradation), enriching antioxidant and antimicrobial compounds, and fortifying health-promoting bioactive compounds [1,2]. These attractive microbial activities in the fermented foods have been a draw in the field of probiotics.
Characteristics of bacterial strains such as Lactobacillus and Bifidobacterium species have been extensively studied and commercially available as probiotic supplements. Yeasts, which are also common in fermented foods, remain largely unexplored for probiotic potential. We and other researchers have observed that yeasts that originate from fermented sources such as apple cider, wine, fermented coconut palm, and fermented dairy products survive the harsh condition of the gastrointestinal (GI) tract and retain the ability to attach to intestinal epithelium [3,4,5]. More recently, live bacteria have been used in fecal transplants to prevent and/or treat several GI complications [6]. The probiotic bacteria, such as lactic acid bacteria (LAB) and Bifidobacterium species, have effectively treated several GI complications, including candidiasis [7,8]. However, other than Saccharomyces boulardii, potential probiotic yeasts such as S. cerevisiae and several other non-Saccharomyces yeasts are largely unexplored use as biotherapeutics, specifically for Candida infections. In reviewing the current literature here, we focus on the biotherapeutic potential and mechanism(s) of action of beneficial yeasts against Candida infections.
The vast majority of fungal infections are caused by Candida albicans, a polymorphic commensal yeast as well as some non-albicans Candida species. Disease range from superficial infections, such as cutaneous and mucosal, to life-threatening bloodstream infections (BSI), or invasive deep tissue infections. Superficial infections usually affect the nails, skin, and mucosal membrane of the host and are recalcitrant to treatment. For example, vulvovaginal candidiasis (VVC) has infected 75% of women population at least once in their lifetime. Furthermore, a small population (5–8%) suffers from at least four recurrent VVC per year [9].
Bloodstream infection (BSI) and other invasive Candida infections cause high morbidity and mortality especially among immune-compromised patients [10]. Candida species are the fourth-leading cause of nosocomial infections in the world, and Candida BSI attributes to 35% mortality rate in all the Candida associated infections [11]. Furthermore, the National Nosocomial Infection Surveillance System (NNIS), USA, has revealed total 27,200 nosocomial infections between January 1980 through April 1990, among these C. albicans and non-albicans Candida species were involved total 19,621 (72%) of the overall infections [12].
Though C. albicans is a major commensal yeast flora of the GI tract, non-albicans Candida species such as Candida glabrata, Candida tropicalis, Candida parapsilosis, and Candida krusei have been frequently identified in a healthy individual’s gut. On the other hand, among 15–20 pathogenic non-albicans Candida species, Candida glabrata, Candida tropicalis, Candida parapsilosis, and Candida krusei are predominant constituting 35–65% of the overall infections [13]. As an opportunistic pathogen, certain groups of immune-compromised individuals have a higher susceptibility towards Candida infection. Invasive Candida infections are also closely associated with advanced medical techniques such as medical implants and stents [14]. For instance, the patients who are on antibiotic therapy and chemotherapy, central venous catheters, total parenteral nutrition, extensive surgery, burns, renal failure and hemodialysis, or mechanical ventilation are at a major risk for superficial and invasive Candida infections [14].
2. Morphological Transition and Metabolic Flexibility Promote Virulence of Candida In Vivo
As a polymorphic yeast, C. albicans and few non-albicans Candida strains, such as C. tropicalis and C. glabrata, exhibit multiple morphological structures such as yeast form, germ tubes, pseudo-hyphae, and/or hyphae that play a key role in the infection. For example, filamentous morphology is well-known for epithelial invasion and is primarily involved in biofilm formation [15]. Yeast form cells are planktonic and are important for dissemination. Once they attach, they initiate germ tubes, pseudo-hyphae, and/or hyphae that enhance adhesion to surfaces. Attachment to abiotic surfaces initiates biofilm formation. Biofilms on implanted medical devises may lead to invasive fungal infections—a major risk factor for Candida infection-associated mortality [16]. Attachment to live cells (such as epithelium) causes damage, evokes an immune response and ultimately gains access to deeper tissues. Therefore, the polymorphism of Candida is an important consideration in its infectious outcomes.
The host’s innate immunity is a major factor in fungal clearance, normally through a process called phagocytosis where immune cells ingest and biochemically eliminate the pathogens [17]. However, the switch from yeast to filamentous form is a common escape mechanism of Candida species [18]. Therefore, C. albicans filament has less susceptibility for phagocytosis by innate immune cells than the yeast form [19]. In addition, metabolic flexibility of C. albicans facilitates colonization by adapting to varying nutritional availability [20]. For instance, in case of Candida meningoencephalitis (Candida infection in brain tissue), glucose and vitamins are the major nutrient sources for the pathogen, while in liver, it utilizes glycogen as a nutrient source [9]. A study revealed that adaptation to alternative carbon sources such as lactate and other nutrient sources increased environment stress response and virulence [21]. All of these attributes make C. albicans and non-albicans Candida species a unique pathogen among the microbial community.
3. Drug Resistance Is a Major Hurdle to Antifungal Therapy
Antifungal drugs used to treat Candida associated infections, work either by killing or inhibiting the growth of Candida species. A sparse number of antifungal classes such as polyenes, azoles, and echinocandins are used depending on conditions of invasive Candida infections [22]. Multiple Candida strains have already developed resistance to these drugs making this a public health threat [23]. For example, surveillance data from health-care facilities revealed widespread fluconazole resistance among clinical isolates of both C. albicans and non-albicans Candida strains [24,25,26]. Azoles such as fluconazole is a first-line antifungal drug that is used extensively for therapy and prophylaxis against Candida infections. Several resistant mechanisms have been connected to drug-resistant Candida species including overexpression of drug efflux pumps, alteration in drug targets, and changes in membrane sterol composition [22]. The structural heterogeneity of Candida biofilm has a major significance in clinical context due to higher resistance against most antifungal agents. Furthermore, these drugs can be toxic for the patients with several side effects that include GI disturbances, hepatotoxicity, and neurotoxicity due to their target resemblance to its host cell, antifungal metabolism in liver and cross drug interaction in the host [27,28].
More recently, multi-drug resistant Candida auris has emerged as a “super bug” posing significant clinical challenges and a major threat to public health. Candida auris, is often involved in the nosocomial bloodstream infection world-wide [29]. C. auris has been shown to last in the hospital settings and spread from person-to-person by direct contact or contaminated surfaces [23]. In addition, C. auris is closely related with Candida haemulonii and is often misidentified as such. This requires a specialized laboratory method for identification [23], further delaying implementation of infection control. Therefore, now more than ever, there is an urgent need for effective alternatives to conventional modes to treat Candida infections.
Some attempts have been made to using specific diets that avoid high sugar-containing food such as bakery products, milk, and dairy product. The claim is that it reduces Candida colonization of the GI tract [30]. Intestinal overgrowth of C. albicans contributes to Crohn’s disease that affects 1.6 million Americans [31,32]. C. albicans overgrowth is caused by an imbalance in the intestinal microbiota and host immune status. To restore the balance and modulate host immunity, foods rich in antioxidants and other nutritional supplements have been suggested [30,33]. More recently, studies on the human microbiome have opened new insight into the role of the resident gut microbiota in physical health and mental wellbeing. Applications of beneficial microbes as fecal transplants [34] or fermented milk products [35] for the treatment of irritable bowel syndrome (IBS) and irritable bowel disease (IBD) has gained traction. Here we discuss the potential of probiotic yeasts against Candida virulence and pathogenesis.
4. Use of Probiotics as Biotherapeutics
As stated by Hippocrates, “let food be thy medicine and medicine be thy food”. Today, the idea of food and/or diet is not just extended towards mere survival or hunger satisfaction. The health-conscious population deeply cares about additional aspects including health improvement and prevention of diseases. In this context, functional food plays a significant role where, the concept of food has not only intended to provide humans with necessary nutrients, but also to prevent diseases and increase physical and mental well-being. Probiotic, considered as a functional food, is mostly consumed in the form of traditional fermented food products such as milk products, fermented vegetables, and meats [36].
Probiotics are defined as “live microorganisms which, when consumed in adequate amounts, confer health benefits on the host” [37]. The archived scientific documents have explained the diverse positive effects of probiotics on a wide range of diseases and disorders including lactose indigestion, diarrhea, immune modulation, inflammatory bowel syndrome, constipation, infection, allergy, serum cholesterol, blood pressure, and reduction of urinary tract infections [38]. In addition, the Human Microbiome Project by National Institute of Health (NIH), USA, changed the views on beneficial microbial research; it exposed the influence of gut microbiome and human health during various infections and disease conditions including, mental health.
5. Interaction of Probiotics Yeast and Candida Species
Several reports suggest that probiotic bacteria are effective against GI complications such as diarrhea, leaky gut syndrome, as well as Helicobacter pylori and Clostridium difficile infections [39,40]. However, Saccharomyces cerevisiae var. boulardii is the only yeast currently available for human use as probiotics. Its efficacy against Candida has been explored previously. Specifically, pathogen-free mice that were infected with C. albicans and subsequently treated with S. boulardii prevented the translocation of Candida to internal organs [41,42,43]. These groups further confirmed that S. boulardii effectively reduced C. albicans translocation colonization and inflammation in in vivo models.
Clinical reports around the use of probiotic yeasts are limited. One study, reports that oral administration of S. boulardii to infants reduced the fungal colonization and invasive fungal infections [44]. Another study conducted in preteen children focused on the effects of probiotics against Candida infection. They used a probiotic cocktail of yeast and bacteria in combination with prebiotics and demonstrated a reduction in colonization of C. albicans [45].
6. Probiotic Yeasts Exhibit Multiple Inhibitory Mechanisms against Candida Species
Pre-clinical and/or clinical studies indicate that S. boulardii and other potential probiotic yeasts ameliorate complications associated with Candida infection by mechanisms outlined in Table 1. However, there was a lack of specific mechanistic insights on how these probiotic yeasts interact with Candida species especially in the context of a live host. Pathogens in GI tract induce necrosis and apoptosis of intestinal epithelia by reducing the production of mucin or its degradation. Pathogens also downregulate IgA and other proteins of the tight junction thereby increasing intestinal permeability [46,47]. S. boulardii has been shown to increase IgA production in Clostridium difficile colitis and antibiotic-associated diarrhea in mice model [48]. S. boulardii also decreases epithelial necrosis, apoptosis, and increases the production of antioxidant enzymes such as superoxide dismutase, catalase, and glutathione peroxidase in mouse models in necrotizing enterocolitis in mice [49]. In addition, S. boulardii activates the intestinal epithelial restoration in GI tract [50]. Together these cellular responses may contribute to its beneficial properties and prevent Candida infection.
Table 1.
List of probiotic yeasts and its mechanisms against virulence and pathogenesis of Candida species.
| Probiotic Yeast Strains | Mechanisms of Probiotic Yeasts against Candida Species Virulence and Pathogenesis |
|---|---|
| S. boulardii |
|
| S. cerevisiae * |
|
| I. occidentalis * |
|
* Potential probiotic yeast, not commercialized.
6.1. Immunogenic Response and Anti-Virulence Ability of Probiotic Yeasts
Since resistance to antifungal drugs has emerged as a significant problem, researchers have explored alternative means of treating recalcitrant fungal infections. Modulation of host immunity is one avenue that is being considered as an alternative [56,57]. For example, S. boulardii has been shown to reduce pro-inflammatory cytokines such as IL-1β and TNF, and increase anti-inflammatory cytokines IL-4 and IL-10 during Candida infection [42,58]. Other alternative therapies target virulence strategies such as adhesion and filamentation of C. albicans [59]. These maybe used to treat abiotic surfaces to deter microbes from binding. Probiotics also have the ability to inhibit virulence factors of the pathogen. We and others have demonstrated that cells, as well as the cell-free secretome of probiotic yeasts such as S. boulardii, S. cerevisiae, and a non-Saccharomyces yeast Issatchenkia occidentalis inhibit adhesion, filamentation, and biofilm development of C. albicans [52] and other non-albicans Candida species such as C. tropicalis, C. krusei, C. glabrata, and Candida parapsilopsis. Biofilms are complex multispecies structures that include C. albicans among other microbes [60,61]. Probiotics yeasts have been shown to be effective against fungal biofilms composed of C. albicans and non-albicans Candida species [53]; however, no studies have been focused on their efficacy on cross-kingdom biofilms. These studies implicated the involvement of yeast metabolite(s) in inhibiting adhesion and/ or morphological transition in vitro [53]. These studies also indicate that probiotic yeast affect a broad spectrum and not limited to C. albicans; rather, it can inhibit virulence across the Candida genus.
Cultured intestinal epithelial models such as Caco-2, Intestin 407 and HT-29 have been extensively used to study microbial interactions or host-microbe interactions. These cell lines recapitulate various features of the intestinal epithelial surface including the formation of villi, production of mucus, and antibodies such as IgA [62]. We and others have demonstrated that probiotic yeasts effectively reduce adhesion of C. albicans and non-albicans Candida species to these cultured epithelial cell lines [52,53]. In addition, yeast S. boulardii has been shown to pose a barrier and preserve the integrity of the epithelium by the reduction of pro-inflammatory cytokines in the intestine [40,52].
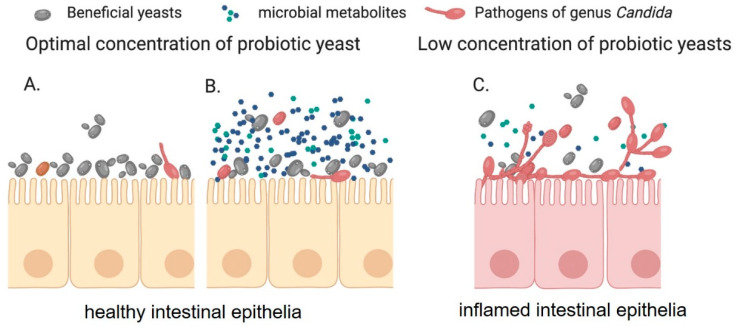
Even though live probiotic cells are known to play a significant role in preventing virulence of C. albicans, the role of exact cellular components involved are less investigated. For example, administration of cell wall components of S. cerevisiae reduced the Candida associated inflammation and colonization in animal models [55]. Interestingly, one of the four S. cerevisiae strains used in this study (strain Sc-4) increased the mortality and inflammation in the host, suggesting strain-specific effects of the probiotic yeasts against Candida species [55]. Such strain specificity as also been reported in the interaction of Lactobacillus strains with C. albicans [63]. Furthermore, heat-killed S. cerevisiae reduced the vaginal colonization of C. albicans when applied against vaginal candidiasis in a murine model [54]. These effects could either mediated by yeast cell wall components such as β-glucan or simply that the biomass of heat-inactivated probiotic cells form a physical barrier that occludes host factors that facilitate C. albicans attachment (Figure 1A) [54].
Figure 1.
Probiotic yeast either form a physical barrier on epithelial surfaces (A) or secretes bioactive metabolite (B) to inhibit the adhesion and morphological transition of Candida species on epithelial cells. Further, suitable probiotic yeasts cell number is required for the effective inhibition of Candida virulence in the host GI tract (C).
6.2. Role of Small Bioactive Metabolites in Probiotic Action
Beneficial microbes or probiotics in the intestine are thought to control pathogen overgrowth by competing for limited nutrients. There is a growing body of literature that supports the notion that inhibitory function is primarily mediated by secreted small molecules with suitable probiotic cell number (Figure 1B,C) [53,64]. Microorganisms produce metabolites that have been shown to alter the course of an infection by synergistic or antagonistic interactions with infectious agents. Such metabolites include hydrogen peroxide, bacteriocins, and organic acids that effectively inhibit the virulence and growth of various Candida species [64,65] (Table 2). On the other hand, few interesting microbial metabolites, such as tyrosol and indole-3 acetic acid, trigger the filamentation in C. albicans [66,67]. Small molecules derived from bacteria have been evaluated for activity against Candida virulence and pathogenesis. For example, lectins of lactobacilli and bifidobacterial strains isolated from humans have been shown to inhibit the growth of drug-resistant C. albicans [68]. The Gram-positive pathogenic bacteria, Enterococcus faecalis, produces a peptide called EntV which has been shown to reduce C. albicans virulence [69]. Furthermore, organic acids such as acetic acid and lactic acid have been shown to enhance antifungal treatment of C. albicans and C. glabrata [70]. Many Lactobacillus, Bifidobacterium, and yeasts strains produce these organic acids. S. boulardii produces several bioactive compounds such as Saccharomyces anti-inflammatory factor (SAIF), anti-toxin factors, short-chain fatty acids, bioactive proteins of 54 kDa, and 120 kDa which play a major role in preventing bacterial infections [38,71]. However, there has been very limited knowledge on probiotic yeast metabolites on Candida species. Recently a group showed that yeast S. boulardii metabolite capric acid (Decanoic acid)—a saturated fatty acid, inhibits the filamentation of C. albicans interaction [52].
Table 2.
Microbial metabolites and its functions against Candida species.
| Microbial Strains | Bioactive Metabolite | Functions |
|---|---|---|
| S. boulardii [52] | Short-chain fatty acids (capric acid) | Filamentation inhibition, and antifungal activity against C. albicans |
| S. cerevisiae [53,54] | Unknown | Adhesion and filamentation inhibition |
| I. occidentalis [53] | Unknown | Adhesion and filamentation inhibition |
| Lactobacillus acidophilus, L. crispatus, L. vaginalis [65,68] | Lectins, hydrogen peroxide, lactic acid |
Inhibit cell growth of C. albicans |
| Bifidobacterium adolescentis, B. bifidum, B. gallinarum [68] | Lectins | Inhibit cell growth of C. albicans |
| Enterococcus faecalis [69] | Peptide EntV | Filamentation inhibition |
| Pseudomonas aeruginosa [75,79] | Phenazine, 3-oxo-C12 homoserine lactone | Filamentation inhibition |
| Salmonella typhimurium [72] | Unknown | Inhibit cell growth and filamentation |
| Streptococcus mutants [73] | Unknown | Inhibit cell growth and filamentation |
In natural habitats, potential interaction of microbial communities has been a key element for the ecological dynamics. Bacteria and eukaryotic microorganisms exhibit both symbiotic and/or antagonistic interaction in the natural environment. In fact, C. albicans co-exists with other non-albicans Candida species or bacteria in the biofilm as well as the human GI tract. These inter-species interactions between C. albicans and other microbes typically affect filamentation of C. albicans. For instance, certain secretory molecules of Salmonella typhimurium and Streptococcus mutants inhibit cell growth and filamentation of C. albicans in the co-culture conditions [72,73]. Another well studied bacterium is Pseudomonas aeruginosa, where bacterial toxin phenazine inhibits the filamentation of C. albicans [74,75].
The morphological transition of yeast has been controlled by cell density and/or quorum sensing molecules. Apart from bacteria, the quorum sensing mechanism is also well studied in yeast such as C. albicans and S. cerevisiae. Farnesol and tyrosol are known cell density molecules in C. albicans which controls the morphological transition. Similarly, yeasts such as S. cerevisiae and other many non-Saccharomyces yeast produce alcoholic signaling molecules called phenylethanol and tryptophol. An abundant usage and availability of well-curated genetic database indicate that S. cerevisiae has gained more attention on quorum sensing mechanisms than the non-Saccharomyces yeast strains. There are few studies claiming that factors such as low nitrogen content and cell density play a significant role in the production of phenylethanol and tryptophol in S. cerevisiae and regulates its morphological transition mechanism [76]. Furthermore, these signal molecules are controlled by the expression of ARO8, ARO9, and ARO10, where ARO8 and ARO9 encode the aromatic aminotransferases and ARO10 encodes the aromatic decarboxylase reaction [77,78].
Several research groups have predicted and/or observed an antagonistic nature of aromatic alcohols, phenylethanol, and tryptophol against fungi. Winters et al., (2019) reported that high concentrations of S. cerevisiae inhibited non-Saccharomyces strains in mixed cultures and under fermentation conditions [78]. Although there were direct evidence of inhibition due to these secondary metabolites, commercially procured phenylethanol and tryptophol have been shown to inhibit filamentation of C. albicans [77]. This result is bolstered by the observation that administration of tryptophol enhances survival of Galleria mellonella larval that are infected with Candida [80]. Furthermore, a cocktail of phenylethanol, isoamyl alcohol, E-nerolidol, and farnesol provides protection against Candida infection in a murine model of infection [81]. Together these studies establish a paradigm for inhibition of fungal virulence that is mediated by aromatic alcohols.
7. Gaps in our Understanding of Biotherapeutic Application of Probiotics for Candida Infection
Probiotic yeasts yield several positive outcomes in in vitro, ex vivo, and in vivo readouts during colonization of Candida species. Information about their effect during systemic infection is an area that needs further investigation. Numerous animal and handful of clinical experiments have revealed that probiotics and metabolites such as short-chain fatty acids, tryptophol and phenylethanol play an abundant role in human health and diseases. However, the origin of these metabolites is ill-defined and their effects on clinical manifestations of Candida infection need further investigation. These studies would provide substantive information to improve biotherapeutic properties of beneficial microbes against Candida infections.
Emergence of drug resistance and complications associated with side effects have sparked interest in alternative therapies. Applications of food-derived yeasts have been shown to have positive outcomes against C. albicans and non-albicans Candida species virulence and infection in pre-clinical and clinical settings. Food-derived beneficial yeasts are also generally safe and pose an effective alternative to traditional antifungals. They may also be used in combination therapy with conventional antifungal drugs since the synergistic effect of probiotics and antifungal agents would prevent emergence of drug resistance.
Acknowledgments
We thank the Director, CSIR-Central Food Technological Research Institute (CFTRI) for encouragement and research support. This work is partially supported by NIH-NCCIH 1R15AT009926-01 grant to RPR. LK is grateful to the INSPIRE program, Department of Science and Technology, Government of India and Fulbright-Nehru doctoral fellowship, United States–India Education Foundation (USIEF), India for the financial support for his doctoral research.
Funding
This research was funded by NIH-NCCIH, grant number NIH-NCCIH 1R15AT009926-01, DST-INSPIRE program, Department of Science and Technology, Government of India, award number DST/INSPIRE Fellowship/2013/553 and Fulbright-Nehru doctoral fellowship, United States–India Education Foundation (USIEF), India, award number 2310/DR/2018-2019.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Tamang J.P., Shin D.H., Jung S.J., Chae S.W. Functional Properties of Microorganisms in Fermented Foods. Front. Microbiol. 2016;7:578. doi: 10.3389/fmicb.2016.00578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nkhata S.G., Ayua E., Kamau E.H., Shingiro J.B. Fermentation and germination improve nutritional value of cereals and legumes through activation of endogenous enzymes. Food Sci. Nutr. 2018;6:2446–2458. doi: 10.1002/fsn3.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lohith K.A., Anu-Appaiah K.A. In vitro probiotic characterization of yeasts of food and environmental origin. Int. J. Probiotics Prebiotics. 2014;9:1–6. [Google Scholar]
- 4.Lohith K.A., Anu-Appaiah K.A. Antagonistic effect of Saccharomyces cerevisiae KTP and Issatchenkia occidentalis ApC on hyphal development and adhesion of Candida albicans. Med. Mycol. 2018;56:1023–1032. doi: 10.1093/mmy/myx156. [DOI] [PubMed] [Google Scholar]
- 5.Kumura H., Tanoue Y., Tsukahara M., Tanaka T., Shimazaki K. Screening of dairy yeast strains for probiotic applications. J. Dairy Sci. 2004;87:4050–4056. doi: 10.3168/jds.S0022-0302(04)73546-8. [DOI] [PubMed] [Google Scholar]
- 6.Gupta S., Allen-Vercoe E., Petrof E.O. Fecal microbiota transplantation: In perspective. Ther. Adv. Gastroenterol. 2016;9:229–239. doi: 10.1177/1756283X15607414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verna E.C., Lucak S. Use of probiotics in gastrointestinal disorders: What to recommend? Ther. Adv. Gastroenterol. 2010;3:307–319. doi: 10.1177/1756283X10373814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagner R.D., Pierson C., Warner T., Dohnalek M., Farmer J., Roberts L., Hilty M., Balish E. Biotherapeutic effects of probiotic bacteria on candidiasis in immunodeficient mice. Infect. Immun. 1997;65:4165–4172. doi: 10.1128/IAI.65.10.4165-4172.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mayer F.L., Wilson D., Hube B. Candida albicans pathogenicity mechanisms. Virulence. 2013;4:119–128. doi: 10.4161/viru.22913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delaloye J., Calandra T. Invasive candidiasis as a cause of sepsis in the critically ill patient. Virulence. 2014;5:161–169. doi: 10.4161/viru.26187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calderone R.A., Fonzi W.A. Virulence factors of Candida albicans. Trends Microbiol. 2001;9:327–335. doi: 10.1016/S0966-842X(01)02094-7. [DOI] [PubMed] [Google Scholar]
- 12.Jarvis W.R. Epidemiology of nosocomial fungal infections, with emphasis on Candida species. Clin. Infect. Dis Off. Publ. Infect. Dis. Soc. Am. 1995;20:1526–1530. doi: 10.1093/clinids/20.6.1526. [DOI] [PubMed] [Google Scholar]
- 13.Pappas P.G., Lionakis M.S., Arendrup M.C., Ostrosky-Zeichner L., Kullberg B.J. Invasive candidiasis. Nat. Rev. Dis. Prim. 2018;4:18026. doi: 10.1038/nrdp.2018.26. [DOI] [PubMed] [Google Scholar]
- 14.Spampinato C., Leonardi D. Candida infections, causes, targets, and resistance mechanisms: Traditional and alternative antifungal agents. BioMed Res. Int. 2013;2013:204237. doi: 10.1155/2013/204237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson D. Candida albicans. Trends Microbiol. 2019;27:188–189. doi: 10.1016/j.tim.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Taff H.T., Mitchell K.F., Edward J.A., Andes D.R. Mechanisms of Candida biofilm drug resistance. Future Microbiol. 2013;8:1325–1337. doi: 10.2217/fmb.13.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Munoz J.F., Delorey T., Ford C.B., Li B.Y., Thompson D.A., Rao R.P., Cuomo C.A. Coordinated host-pathogen transcriptional dynamics revealed using sorted subpopulations and single macrophages infected with Candida albicans. Nat. Commun. 2019;10:1607. doi: 10.1038/s41467-019-09599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudbery P., Gow N., Berman J. The distinct morphogenic states of Candida albicans. Trends Microbiol. 2004;12:317–324. doi: 10.1016/j.tim.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Wartenberg A., Linde J., Martin R., Schreiner M., Horn F., Jacobsen I.D., Jenull S., Wolf T., Kuchler K., Guthke R., et al. Microevolution of Candida albicans in macrophages restores filamentation in a nonfilamentous mutant. PLoS Genet. 2014;10:e1004824. doi: 10.1371/journal.pgen.1004824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lorenz M.C., Fink G.R. The glyoxylate cycle is required for fungal virulence. Nature. 2001;412:83–86. doi: 10.1038/35083594. [DOI] [PubMed] [Google Scholar]
- 21.Ene I.V., Adya A.K., Wehmeier S., Brand A.C., MacCallum D.M., Gow N.A., Brown A.J. Host carbon sources modulate cell wall architecture, drug resistance and virulence in a fungal pathogen. Cell. Microbiol. 2012;14:1319–1335. doi: 10.1111/j.1462-5822.2012.01813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berman J., Krysan D.J. Drug resistance and tolerance in fungi. Nat. Rev. Microbiol. 2020;18:319–331. doi: 10.1038/s41579-019-0322-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention (CDC) Candida auris. [(accessed on 22 July 2020)]; Available online: https://www.cdc.gov/fungal/candida-auris/candida-auris-qanda.html.
- 24.Shi C., Liu J., Li W., Zhao Y., Meng L., Xiang M. Expression of fluconazole resistance-associated genes in biofilm from 23 clinical isolates of Candida albicans. Braz. J. Microbiol. 2019;50:157–163. doi: 10.1007/s42770-018-0009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rybak J.M., Muñoz J.F., Barker K.S., Parker J.E., Esquivel B.D., Berkow E.L., Lockhart S.R., Gade L., Palmer G.E., White T.C., et al. Mutations in tac1b: A novel genetic determinant of clinical fluconazole resistance in Candida auris. mBio. 2020;11:e00365-20. doi: 10.1128/mBio.00365-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Castanheira M., Deshpande L.M., Messer S.A., Rhomberg P.R., Pfaller M.A. Analysis of global antifungal surveillance results reveals predominance of Erg11 Y132F alteration among azole-resistant Candida parapsilosis and Candida tropicalis and country-specific isolate dissemination. Int. J. Antimicrob. Agents. 2020;55:105799. doi: 10.1016/j.ijantimicag.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Lewis R.E. Current concepts in antifungal pharmacology. Mayo Clin. Proc. 2011;86:805–817. doi: 10.4065/mcp.2011.0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang J.L., Chang C.H., Young-Xu Y., Chan K.A. Systematic review and meta-analysis of the tolerability and hepatotoxicity of antifungals in empirical and definitive therapy for invasive fungal infection. Antimicrob. Agents Chemother. 2010;54:2409–2419. doi: 10.1128/AAC.01657-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ben-Ami R., Berman J., Novikov A., Bash E., Shachor-Meyouhas Y., Zakin S., Maor Y., Tarabia J., Schechner V., Adler A., et al. Multidrug-Resistant Candida haemulonii and Candida auris, Tel Aviv, Israel. Emerg. Infect. Dis. 2017;23:195. doi: 10.3201/eid2302.161486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martins N., Ferreira I.C., Barros L., Silva S., Henriques M. Candidiasis: Predisposing factors, prevention, diagnosis and alternative treatment. Mycopathologia. 2014;177:223–240. doi: 10.1007/s11046-014-9749-1. [DOI] [PubMed] [Google Scholar]
- 31.Loftus E.V., Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–1517. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 32.Molodecky N.A., Soon S., Rabi D.M., Ghali W.A., Ferris M., Chernoff G., Benchimol E.I., Panaccione R., Ghosh S., Barkema H.W., et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54 e42. doi: 10.1053/j.gastro.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 33.Rehaume L.M., Jouault T., Chamaillard M. Lessons from the inflammasome: A molecular sentry linking Candida and Crohn’s disease. Trends Immunol. 2010;31:171–175. doi: 10.1016/j.it.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Xu D., Chen V.L., Steiner C.A., Berinstein J.A., Eswaran S., Waljee A.K., Higgins P.D., Owyang C. Efficacy of fecal microbiota transplantation in irritable bowel syndrome: A systematic review and meta-analysis. Am. J. Gastroenterol. 2019;114:1043–1050. doi: 10.14309/ajg.0000000000000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Simren M., Ohman L., Olsson J., Svensson U., Ohlson K., Posserud I., Strid H. Clinical trial: The effects of a fermented milk containing three probiotic bacteria in patients with irritable bowel syndrome—A randomized, double-blind, controlled study. Aliment. Pharmacol. Ther. 2010;31:218–227. doi: 10.1111/j.1365-2036.2009.04183.x. [DOI] [PubMed] [Google Scholar]
- 36.Suryabhan P., Lohith K., Anu-Appaiah K.A. Sucrose and sorbitol supplementation on maltodextrin encapsulation enhance the potential probiotic yeast survival by spray drying. LWT. 2019;107:243–248. doi: 10.1016/j.lwt.2019.03.002. [DOI] [Google Scholar]
- 37.Morelli L., Capurso L. FAO/WHO guidelines on probiotics: 10 years later. J. Clin. Gastroenterol. 2012;46:S1–S2. doi: 10.1097/MCG.0b013e318269fdd5. [DOI] [PubMed] [Google Scholar]
- 38.Vandenplas Y., Brunser O., Szajewska H. Saccharomyces boulardii in childhood. Eur. J. Pediatr. 2009;168:253–265. doi: 10.1007/s00431-008-0879-7. [DOI] [PubMed] [Google Scholar]
- 39.Tung J.M., Dolovich L.R., Lee C.H. Prevention of Clostridium difficile infection with Saccharomyces boulardii: A systematic review. Can. J. Gastroenterol. J. Can. Gastroenterol. 2009;23:817–821. doi: 10.1155/2009/915847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Terciolo C., Dapoigny M., Andre F. Beneficial effects of Saccharomyces boulardii CNCM I-745 on clinical disorders associated with intestinal barrier disruption. Clin. Exp. Gastroenterol. 2019;12:67–82. doi: 10.2147/CEG.S181590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jawhara S., Poulain D. Saccharomyces boulardii decreases inflammation and intestinal colonization by Candida albicans in a mouse model of chemically-induced colitis. Med. Mycol. 2007;45:691–700. doi: 10.1080/13693780701523013. [DOI] [PubMed] [Google Scholar]
- 42.Algin C., Sahin A., Kiraz N., Sahinturk V., Ihtiyar E. Effectiveness of bombesin and Saccharomyces boulardii against the translocation of Candida albicans in the digestive tract in immunosuppressed rats. Surg. Today. 2005;35:869–873. doi: 10.1007/s00595-005-3049-9. [DOI] [PubMed] [Google Scholar]
- 43.Berg R., Bernasconi P., Fowler D., Gautreaux M. Inhibition of Candida albicans translocation from the gastrointestinal tract of mice by oral administration of Saccharomyces boulardii. J. Infect. Dis. 1993;168:1314–1318. doi: 10.1093/infdis/168.5.1314. [DOI] [PubMed] [Google Scholar]
- 44.Demirel G., Celik I.H., Erdeve O., Saygan S., Dilmen U., Canpolat F.E. Prophylactic Saccharomyces boulardii versus nystatin for the prevention of fungal colonization and invasive fungal infection in premature infants. Eur. J. Pediatr. 2013;172:1321–1326. doi: 10.1007/s00431-013-2041-4. [DOI] [PubMed] [Google Scholar]
- 45.Kumar S.B.A., Chakrabarti A., Singhi S. Evaluation of efficacy of probiotics in prevention of Candida colonization in a PICU—A randomized controlled trial. Crit. Care Med. 2013;41:565–572. doi: 10.1097/CCM.0b013e31826a409c. [DOI] [PubMed] [Google Scholar]
- 46.Zeng Q., He X., Puthiyakunnon S., Xiao H., Gong Z., Boddu S., Chen L., Tian H., Huang S.H., Cao H. Probiotic mixture golden bifido prevents neonatal Escherichia coli K1 translocation via enhancing intestinal defense. Front. Microbiol. 2017;8:1798. doi: 10.3389/fmicb.2017.01798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allert S., Förster T.M., Svensson C.M., Richardson J.P., Pawlik T., Hebecker B., Rudolphi S., Juraschitz M., Schaller M., Blagojevic M., et al. Candida albicans-Induced Epithelial Damage Mediates Translocation through Intestinal Barriers. mBio. 2018;9:e00915-18. doi: 10.1128/mBio.00915-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Qamar A., Aboudola S., Warny M., Michetti P., Pothoulakis C., LaMont J.T., Kelly C.P. Saccharomyces boulardii stimulates intestinal immunoglobulin A immune response to Clostridium difficile toxin A in mice. Infect. Immun. 2001;69:2762–2765. doi: 10.1128/IAI.69.4.2762-2765.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang Y., Li Y., Chen C., Zhang Y., Li J., Fan Y., Chen X., Wang S., Wang J. Saccharomyces boulardii exerts anti-apoptosis and anti-necroptosis effects on neonatal mice necrotizing enterocolitis by increasing reactive oxygen species consumption. Int. J. Clin. Exp. Med. 2019;12:10019–10028. [Google Scholar]
- 50.Canonici A., Siret C., Pellegrino E., Pontier-Bres R., Pouyet L., Montero M.P., Colin C., Czerucka D., Rigot V., André F. Saccharomyces boulardii improves intestinal cell restitution through activation of the alpha2beta1 integrin collagen receptor. PLoS ONE. 2011;6:e18427. doi: 10.1371/journal.pone.0018427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murzyn A., Krasowska A., Augustyniak D., Majkowska-Skrobek G., Łukaszewicz M., Dziadkowiec D. The effect of Saccharomyces boulardii on Candida albicans-infected human intestinal cell lines Caco-2 and Intestin 407. FEMS Microbiol. Lett. 2010;310:17–23. doi: 10.1111/j.1574-6968.2010.02037.x. [DOI] [PubMed] [Google Scholar]
- 52.Murzyn A., Krasowska A., Stefanowicz P., Dziadkowiec D., Lukaszewicz M. Capric acid secreted by S. boulardii inhibits C. albicans filamentous growth, adhesion and biofilm formation. PLoS ONE. 2010;58:e12050. doi: 10.1371/journal.pone.0012050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kunyeit L., Kurrey N.K., Anu-Appaiah K.A., Rao R.P. Probiotic yeasts inhibit virulence of non-albicans Candida species. mBio. 2019;10:e02307-19. doi: 10.1128/mBio.02307-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pericolini E., Gabrielli E., Ballet N., Sabbatini S., Roselletti E., Cayzeele Decherf A., Pélerin F., Luciano E., Perito S., Jüsten P., et al. Therapeutic activity of a Saccharomyces cerevisiae-based probiotic and inactivated whole yeast on vaginal candidiasis. Virulence. 2017;8:74–90. doi: 10.1080/21505594.2016.1213937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jawhara S., Habib K., Maggiotto F., Pignede G., Vandekerckove P., Maes E., Dubuquoy L., Fontaine T., Guerardel Y., Poulain D. Modulation of intestinal inflammation by yeasts and cell wall extracts: Strain dependence and unexpected anti-inflammatory role of glucan fractions. PLoS ONE. 2012;7:e40648. doi: 10.1371/journal.pone.0040648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vylkova S., Nayyar N., Li W., Edgerton M. Human beta-defensins kill Candida albicans in an energy-dependent and salt-sensitive manner without causing membrane disruption. Antimicrob. Agents Chemother. 2007;51:154–161. doi: 10.1128/AAC.00478-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Edgerton M., Koshlukova S.E., Araujo M.W., Patel R.C., Dong J., Bruenn J.A. Salivary histatin 5 and human neutrophil defensin 1 kill Candida albicans via shared pathways. Antimicrob. Agents Chemother. 2000;44:3310–3316. doi: 10.1128/AAC.44.12.3310-3316.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fidan I., Kalkanci A., Yesilyurt E., Yalcin B., Erdal B., Kustimur S., Imir T. Effects of Saccharomyces boulardii on cytokine secretion from intraepithelial lymphocytes infected by Escherichia coli and Candida albicans. Mycoses. 2009;52:29–34. doi: 10.1111/j.1439-0507.2008.01545.x. [DOI] [PubMed] [Google Scholar]
- 59.Fazly A., Jain C., Dehner A.C., Issi L., Lilly E.A., Ali A., Cao H., Fidel P.L., Rao R.P., Kaufman P.D. Chemical screening identifies filastatin, a small molecule inhibitor of Candida albicans adhesion, morphogenesis, and pathogenesis. Proc. Natl. Acad. Sci. USA. 2013;110:13594–13599. doi: 10.1073/pnas.1305982110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harriott M.M., Noverr M.C. Importance of Candida-bacterial polymicrobial biofilms in disease. Trends Microbiol. 2011;19:557–563. doi: 10.1016/j.tim.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coco B.J., Bagg J., Cross L.J., Jose A., Cross J., Ramage G. Mixed Candida albicans and Candida glabrata populations associated with the pathogenesis of denture stomatitis. Oral Microbiol. Immunol. 2008;23:377–383. doi: 10.1111/j.1399-302X.2008.00439.x. [DOI] [PubMed] [Google Scholar]
- 62.Lea T. Epithelial Cell Models; General Introduction. In: Verhoeckx K., Cotter P., Lopez-Exposito I., Kleiveland C., Lea T., Mackie A., Requena T., Swiatecka D., Wichers H., Cham C.H., editors. The Impact of Food Bioactives on Health: In Vitro and Ex Vivo Models. Springer International Publishing; Cham, Switzerland: 2015. pp. 95–102. [PubMed] [Google Scholar]
- 63.Strus M., Kucharska A., Kukla G., Brzychczy-Włoch M., Maresz K., Heczko P.B. The in vitro activity of vaginal Lactobacillus with probiotic properties against Candida. Infect. Dis. Obstet. Gynecol. 2005;13:69–75. doi: 10.1080/10647440400028136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ohshima T., Kojima Y., Seneviratne C.J., Maeda N. Therapeutic application of synbiotics, a fusion of probiotics and prebiotics, and biogenics as a new concept for oral candida infections: A Mini Review. Front. Microbiol. 2016;7:10. doi: 10.3389/fmicb.2016.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Parolin C., Marangoni A., Laghi L., Foschi C., Ñahui Palomino R.A., Calonghi N., Cevenini R., Vitali B. Isolation of vaginal lactobacilli and characterization of anti-Candida activity. PLoS ONE. 2015;10:e0131220. doi: 10.1371/journal.pone.0131220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rao R.P., Hunter A., Kashpur O., Normanly J. Aberrant synthesis of indole-3-acetic acid in Saccharomyces cerevisiae triggers morphogenic transition, a virulence trait of pathogenic fungi. Genetics. 2010;185:211–220. doi: 10.1534/genetics.109.112854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen H., Fujita M., Feng Q., Clardy J., Fink G.R. Tyrosol is a quorum-sensing molecule in Candida albicans. Proc. Natl. Acad. Sci. USA. 2004;101:5048–5052. doi: 10.1073/pnas.0401416101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lakhtin M., Alyoshkin V., Lakhtin V., Afanasyev S., Pozhalostina L., Pospelova V. Probiotic Lactobacillus and Bifidobacterial lectins against Candida albicans and Staphylococcus aureus clinical strains: New Class of the Pathogen Biofilm Destructors. Probiot. Antimicrob. Proteins. 2010;2:186–196. doi: 10.1007/s12602-010-9046-3. [DOI] [PubMed] [Google Scholar]
- 69.Graham C.E., Cruz M.R., Garsin D.A., Lorenz M.C. Enterococcus faecalis bacteriocin EntV inhibits hyphal morphogenesis, biofilm formation, and virulence of Candida albicans. Proc. Natl. Acad. Sci. USA. 2017;114:4507–4512. doi: 10.1073/pnas.1620432114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lourenco A., Pedro N.A., Salazar S.B., Mira N.P. Effect of Acetic Acid and Lactic Acid at Low pH in Growth and Azole Resistance of Candida albicans and Candida glabrata. Front. Microbiol. 2018;9:3265. doi: 10.3389/fmicb.2018.03265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Czerucka D., Piche T., Rampal P. Review article: Yeast as probiotics–Saccharomyces boulardii. Aliment. Pharmacol. Ther. 2007;26:767–778. doi: 10.1111/j.1365-2036.2007.03442.x. [DOI] [PubMed] [Google Scholar]
- 72.Tampakakis E., Peleg A.Y., Mylonakis E. Interaction of Candida albicans with an intestinal pathogen, Salmonella enterica serovar Typhimurium. Eukaryot. Cell. 2009;8:732–737. doi: 10.1128/EC.00016-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shareck J., Belhumeur P. Modulation of Morphogenesis in Candida albicans by Various Small Molecules. Eukaryot. Cell. 2011;10:1004–1012. doi: 10.1128/EC.05030-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Morales D.K., Grahl N., Okegbe C., Dietrich L.E., Jacobs N.J., Hogan D.A. Control of Candida albicans metabolism and biofilm formation by Pseudomonas aeruginosa phenazines. mBio. 2013;4:e00526-12. doi: 10.1128/mBio.00526-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hogan D.A., Kolter R. Pseudomonas-Candida interactions: An ecological role for virulence factors. Science. 2002;296:2229–2232. doi: 10.1126/science.1070784. [DOI] [PubMed] [Google Scholar]
- 76.Wuster A., Babu M.M. Transcriptional control of the quorum sensing response in yeast. Mol. bioSyst. 2010;6:134–141. doi: 10.1039/B913579K. [DOI] [PubMed] [Google Scholar]
- 77.Chen H., Fink G.R. Feedback control of morphogenesis in fungi by aromatic alcohols. Genes Dev. 2006;20:1150–1161. doi: 10.1101/gad.1411806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Winters M., Arneborg N., Appels R., Howell K. Can community-based signalling behaviour in Saccharomyces cerevisiae be called quorum sensing? A critical review of the literature. FEMS Yeast Res. 2019;19 doi: 10.1093/femsyr/foz046. [DOI] [PubMed] [Google Scholar]
- 79.Hogan D.A., Vik A., Kolter R. A Pseudomonas aeruginosa quorum-sensing molecule influences Candida albicans morphology. Mol. Microbiol. 2004;54:1212–1223. doi: 10.1111/j.1365-2958.2004.04349.x. [DOI] [PubMed] [Google Scholar]
- 80.Singkum P., Muangkaew W., Suwanmanee S., Pumeesat P., Wongsuk T., Luplertlop N. Suppression of the pathogenicity of Candida albicans by the quorum-sensing molecules farnesol and tryptophol. J. Gen. Appl. Microbiol. 2019;65:277–283. doi: 10.2323/jgam.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 81.Martins M., Lazzell A.L., Lopez-Ribot J.L., Henriques M., Oliveira R. Effect of exogenous administration of Candida albicans autoregulatory alcohols in a murine model of hematogenously disseminated candidiasis. J. Basic Microbiol. 2012;52:487–491. doi: 10.1002/jobm.201100158. [DOI] [PubMed] [Google Scholar]