Abstract
Background
This United States (U.S.) population study aimed to compare the incidence of neuroblastoma and outcomes in children, adolescents, and adults using the Surveillance, Epidemiology, and End Results (SEER) program database.
Material/Methods
Patients with neuroblastoma were identified in the SEER database from 1975 to 2013. According to the age at diagnosis, patients were divided into “Children” (≤14 years old) and “Adolescents/Adults” group (>14 years old). Then, comparisons in basic characteristics, incidence rates (IRs) and long-term survival outcomes between patients in 2 groups were made.
Results
A total of 4280 patients were identified, including 3998 children and 282 adolescent/adult patients. Adolescent/adult patients were more likely to have localized diseases than children and to be diagnosed with ganglioneuroblastoma (all P<0.05). The IR of neuroblastoma presented with upward and downward trends in children and adolescent/adult populations, respectively. Adolescents/adults had worse overall survival (OS) than children despite the earlier tumor stage. Lastly, multivariate Cox proportional hazards analyses showed that tumor stage, histology, sequence of primary malignancy, primary site, the administration of surgery, and treatment era were prognostic factors for children, and sequence of primary malignancy, primary site, undergoing surgery, and treatment era were tightly related to OS in adolescent/adult patients.
Conclusions
Analysis of the SEER program database between 1975 to 2013 showed that in the U.S., the incidence of neuroblastoma in children increased, but the incidence decreased in adolescents and adults. There was a trend for improved overall survival in all age groups despite the increased stage at presentation in children.
MeSH Keywords: Neuroblastoma, SEER Program, Epidemiology, Prognosis, Adolescent, Adult, Child
Background
Neuroblastoma, originating from nerve sympathetic cells, is the most common extracranial solid tumor in children worldwide [1,2]. Neuroblastoma accounts for about 8–10% [3] of all childhood cancer cases. The incidence rate of neuroblastoma is 11 to 13 per million children aged younger than 15 years old, and varies from 1 per million in children of 10–14 years old to 65 per million in children <1 year old [4–6]. It is typically a tumor of early childhood; the median age at diagnosis is 19 months [7] and more than 90% of all neuroblastoma cases are diagnosed before 10 years of age [8]. According to the SEER database, between 1975 to 1995, the percentage distribution of neuroblastoma and ganglioneuroblastoma among all cancers in the U.S. by age group were 14.0 (<5 years), 2.6 (5 to 9 years), 0.8 (10 to 14 years), and 0.3 (15 to 19 years) [9]. A previous Surveillance, Epidemiology, and End Results (SEER) population study [8] showed that the 3-year and 5-year survival rates for neuroblastoma were lowest in adult patients (45.9% and 36.3%, respectively), with survival being greatest for infants who had 86.0% 3-year overall survival and 84.6% 5-year overall survival. This previous study showed a decline in the incidence of adult neuroblastoma from 0.47 cases per million per year between 1973 to 1977, down to 0.12 cases per million per year between 1998 to 2002, with improved outcome during 3 decades, and heterogeneity of treatment has been shown in cases of childhood neuroblastoma within the U.S. [10]. Neuroblastoma in adults is rare, and little is known about the natural history of neuroblastoma patients in adults. It was reported that about 6.1% of all neuroblastoma patients were older than 20 years old, and only 0.9% for patients were ≥60 years old at diagnosis [11].
There have been few studies on adult neuroblastoma due to the extremely low incidence, and most of them were case reports [12–14] or reviews of large databases [8,15]. Mosse et al. [16] investigated the survival outcomes and genetic abnormalities of neuroblastoma in children, adolescents, and young adults using data from the International Neuroblastoma Risk Group (INRG) project. They found that older age at diagnosis was related to worse overall survival (OS), and unfavorable International Neuroblastoma Staging System (INNS) stage 4, MYCN amplification, and international neuroblastoma pathological classification (INPC) histology were prognostic factors for lower event-free survival and OS.
Previous studies had different definitions of the boundary between adult or adolescent and childhood patients. The authors of some studies believed that the boundary age should be 18 years old [1,12,17], while other studies considered that it should be 14 years old [18,19], 16 years old [20], or even 20 years old [20,21]. Furthermore, they had relatively little information on and conflicting comparisons of the treatment outcomes and clinical behavior of neuroblastoma in adults and children. Moreover, further subgroup analyses were limited in many studies due to the small sample size.
The SEER registry is a public registry supported by the National Cancer Institute (NCI). It currently collects and publishes outcomes of cancer incidence, mortality, and long-term follow-up covering 18 population-based cancer registries that represent approximately 30% of the population in the U.S. The SEER database is one of the largest databases, and it has become a useful tool for studying the incidence rate and prognosis of cancer patients, especially for rare cancers. Therefore, this U.S. population study was conducted to compare the incidence of neuroblastoma and outcomes in children, adolescents, and adults using the SEER program database.
Material and Methods
Database
In this study, all the data were downloaded from the SEER database (https://seer.cancer.gov). The SEER program consists of a consortium of 18 regional cancer registries. Histopathological type is based on the 2000 International Classification of Diseases for Oncology version 3 or ICD-O-3 (www.who.int/classifications/icd/adaptations/oncology). ICD-O-3 codes neuroblastoma as 9500/3 under the section of neuroepitheliomatous neoplasms 949–952. As of 2010, tumor grade, extension/metastasis, site-specific factors, and stage were captured based on version 7 of the American Joint Committee on Cancer (AJCC. www.cancerstaging.org). Before we began the present study, we signed the data agreement of the SEER registry with the username XXXXX. Use of public databases does not require Institutional Review Board (IRB) approval.
Primary cohort
To study the incidence rate (IR) trends of neuroblastoma in the past 4 decades, the age-adjusted IRs were extracted using the “Rate Session” tool in the SEER*Stat software (Version 8.3.6; National Cancer Institute, Bethesda, MD). SEER*Stat statistical software provides a convenient and intuitive mechanism for the analysis of the SEER database. It is a powerful tool for viewing personal cancer records and generating statistics to study the impact of cancer on the population. SEER 9 was utilized to extract IRs for patients from 1975 to 1991, SEER 13 for 1992 to 1999, and SEER 18 for 2000 to 2013. Moreover, annual percent change (APC) was calculated in all patients together and further stratified by age at diagnosis.
Secondary cohort
In this section, patients diagnosed with neuroblastoma between 1975 and 2013 were extracted from the SEER 18 registry utilizing the “Case Listing Session” in SEER* Stat software. All the included cases had a known age and AYA site record of 9.1.2 Neuroblastoma (International Classification of Diseases for Oncology: 9490/3 for ganglioneuroblastoma and 9500/3 for neuroblastoma). All patients were diagnosed with positive pathology and those only with autopsy or death certificate were excluded.
Baseline data and clinical characteristics were extracted for each patient, including age at diagnosis, race, sex, year of diagnosis, primary site, histology record, stage, surgery, vital status, cause of death (COD), median household income, place of residence, and survival months. In this study, patients were divided into adolescents/adults (>14 years old) and children (≤14 years old) based on age at diagnosis. Tumor primary site was mainly classified into 6 groups: abdomen, mediastinum/thorax, head and neck, pelvis/extremities/vertebral, nerve system, and unknown. Year of diagnosis was categorized based on an interval of 10 years (1975–1984, 1985–1994, 1995–2004, and 2005–2013). Histological stage was grouped into 4 categories: “localized”, “regional”, “distant”, and “unknown”. Low and high levels of household income were determined by the median value, and place of residence was divided into urban and rural areas.
To investigate the overall and cancer-specific survival (OS and CSS) outcomes of neuroblastoma patients, Kaplan-Meier (KM) analyses and log-rank tests were performed to compare childhood and adolescent/adult patients. Multivariate Cox proportional hazards regression analyses were performed to explore the prognostic factors for OS in patients with neuroblastoma. Co-variates included age, sex, race, tumor stage, histology, primary site, surgery, treatment era, median household income, and place of residence.
Statistical analysis
Categorical data are shown as frequencies and percentages. Continuous data are expressed as median (interquartile range (IQR)) or mean±standard deviation values. We used the t test and chi-square test to make comparisons between adolescent/adult and childhood patients in continuous and categorical variables, respectively. Survival curves were created utilizing the KM method, and differences between groups were compared by log-rank test. Multivariable Cox proportional hazards regression analyses were performed to investigate the potential risk factors for CSS and OS in different populations. APCs of the IR were calculated and generated using the Joinpoint Regression Program (https://surveillance.cancer.gov/joinpoint/). Analyses were performed using R software (Version 3.4.1) and SPSS 23.0 software (SPSS Inc, Chicago, IL, USA). Two-sided P<0.05 was considered as statistically significant.
Results
Baseline characteristics
As shown in Table 1, a total of 4280 patients diagnosed with neuroblastoma with positive pathology were identified in the SEER 18 database from 1975 to 2013, including 3998 childhood patients and 282 adolescent/adult patients. The median (interquartile range (IQR)) age at diagnosis was 1 (0–4) year old. Most patients were white (78.67%), with distant diseases (46.94%), diagnosed in the last 2 decades (71.07%), and with the administration of surgery (73.41%). The abdomen was the most common primary site (63.27%), followed by mediastinum/thorax (16.29%). Most cases were detected in later treatment eras, perhaps because of the expanding coverage of the SEER registry.
Table 1.
Characteristics of patients with neuroblastoma, stratified by age group.
| Variables | Total | Children | Adolescents/adults | P value |
|---|---|---|---|---|
| N | 4,280 | 3,998 | 282 | |
| Age, year | <0.001 | |||
| Median (IQR) | 1 (0–4) | 1 (0–3) | 31 (20–53) | |
| Mean±SD | 4.43±10.28 | 2.15±2.735 | 36.77±19.463 | |
| Sex, n (%) | 0.768 | |||
| Male | 2,237 (52.27) | 2,092 (52.33) | 145 (51.42) | |
| Female | 2,043 (47.73) | 1,906 (47.67) | 137 (48.58) | |
| Race, n (%) | 0.172 | |||
| White | 3,367 (78.67) | 3,156 (78.94) | 211 (74.82) | |
| Black | 547 (12.78) | 499 (12.48) | 48 (17.02) | |
| Other | 324 (7.57) | 304 (7.60) | 20 (7.09) | |
| Unknown | 42 (0.98) | 39 (0.98) | 3 (1.06) | |
| SEER stage, n (%) | <0.001 | |||
| Localized | 861 (20.12) | 787 (19.68) | 74 (26.24) | |
| Regional | 999 (23.34) | 947 (23.69) | 52 (18.44) | |
| Distant | 2,009 (46.94) | 1,929 (48.25) | 80 (28.37) | |
| Unstaged/blank | 411 (9.60) | 335 (8.38) | 76 (26.95) | |
| Treatment era, n (%) | <0.001 | |||
| 1975–1984 | 556 (12.99) | 487 (12.18) | 69 (24.47) | |
| 1985–1994 | 682 (15.93) | 631 (15.78) | 51 (18.09) | |
| 1995–2004 | 1,338 (31.26) | 1,259 (31.49) | 79 (28.01) | |
| 2005–2013 | 1,704 (39.81) | 1,621 (40.55) | 83 (29.43) | |
| Surgery, n (%) | 0.208 | |||
| No/unknown | 1,138 (26.59) | 1,054 (26.36) | 84 (29.79) | |
| Yes | 3,142 (73.41) | 2,944 (73.64) | 198 (70.21) | |
| Median household income*, n (%) | 0.814 | |||
| Low | 2,305 (53.87) | 2,155 (53.92) | 150 (53.19) | |
| High | 1,974 (46.13) | 1,842 (46.08) | 132 (46.81) | |
| Histological stage, n (%) | 0.001 | |||
| Neuroblastoma | 3,580 (83.64) | 3,364 (84.14) | 216 (76.60) | |
| Ganglioneuroblastoma | 700 (16.36) | 634 (15.86) | 66 (23.40) | |
| Place of residence, n (%) | 0.556 | |||
| Urban | 3,488 (81.50) | 3,265 (81.67) | 223 (79.08) | |
| Rural | 713 (16.66) | 660 (16.51) | 53 (18.79) | |
| Missing/unknown | 79 (1.85) | 73 (1.83) | 6 (2.13) | |
| Primary site, n (%) | <0.001 | |||
| Abdomen | 2,708 (63.27) | 2,610 (65.28) | 98 (34.75) | |
| Mediastinum/thorax | 697 (16.29) | 674 (16.86) | 23 (8.16) | |
| Nerve system | 341 (7.97) | 248 (6.20) | 93 (32.98) | |
| Head and neck | 150 (3.50) | 122 (3.05) | 28 (9.93) | |
| Pelvis/extremities/vertebral | 150 (3.50) | 130 (3.25) | 20 (7.09) | |
| NOS, unknown | 234 (5.47) | 214 (5.35) | 20 (7.09) | |
| Primary malignancies, n (%) | ||||
| First primary | 4,245 (99.18) | 3,981 (99.57) | 264 (93.62) | <0.001 |
| 1 total | 4,164 (97.29) | 3,914 (97.90) | 250 (88.65) | <0.001 |
| 2 total | 100 (2.34) | 74 (1.85) | 26 (9.22) | |
| >2 total | 16 (0.37) | 610 (0.25) | 6 (2.13) | |
| Vital status, n (%) | <0.001 | |||
| Alive | 2,840 (66.36) | 2,754 (68.88) | 86 (30.50) | |
| Dead | 1,440 (33.64) | 1,244 (31.12) | 196 (69.50) | |
IQR – interquartile range, SD – standard deviation, SEER – Surveillance, Epidemiology and End Results.
One patient was excluded because of the unknown median household income.
In the comparisons between adolescent/adult and childhood patients, we found a significantly higher proportion of childhood patients had the abdomen as the primary site compared to adolescent/adult patients (65.28% vs. 34.75%, P<0.001). A higher proportion of adolescent/adult patients (23.40%) were diagnosed with ganglioneuroblastoma compared to childhood patients (15.86%) (P=0.001). The percentage of localized diseases was significantly higher in adolescent/adult patients than in childhood patients (26.24% vs. 19.68%), while fewer distant cases were found in adolescent/adult patients (P<0.001). Considering the difference in age at diagnosis, neuroblastoma was more likely to be diagnosed as the first primary malignancy in childhood patients than in adolescent/adult patients (99.57% vs. 93.62%, P<0.001).
Incidence rate trends and annual percent changes
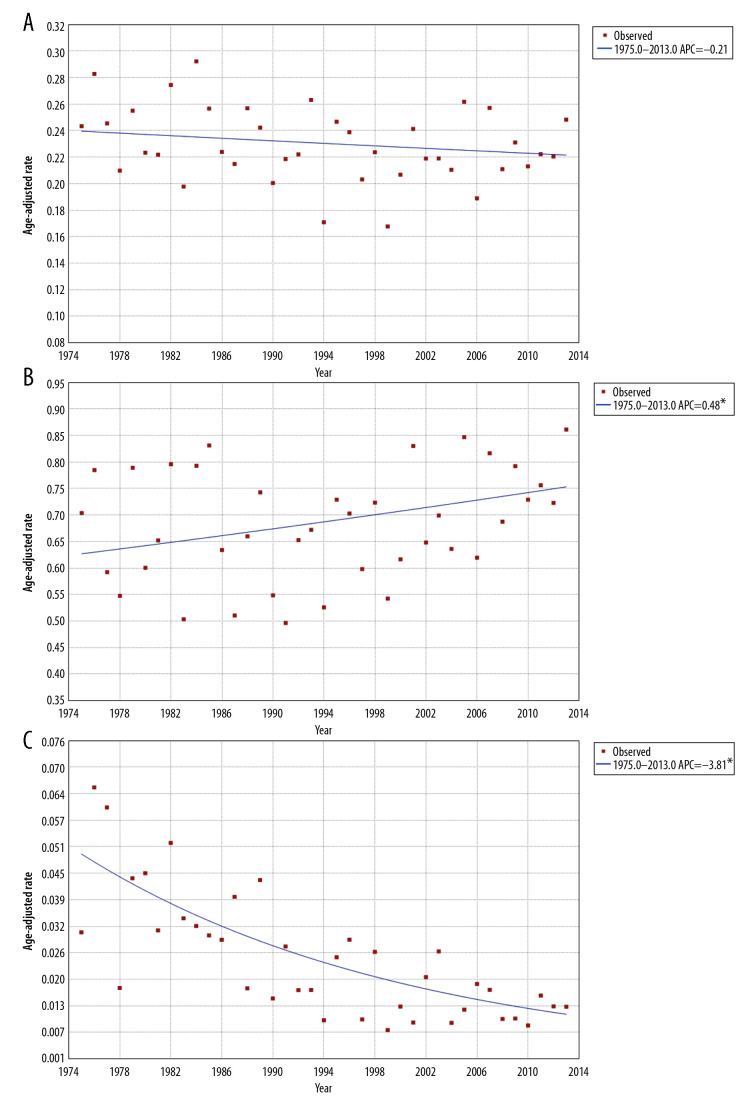
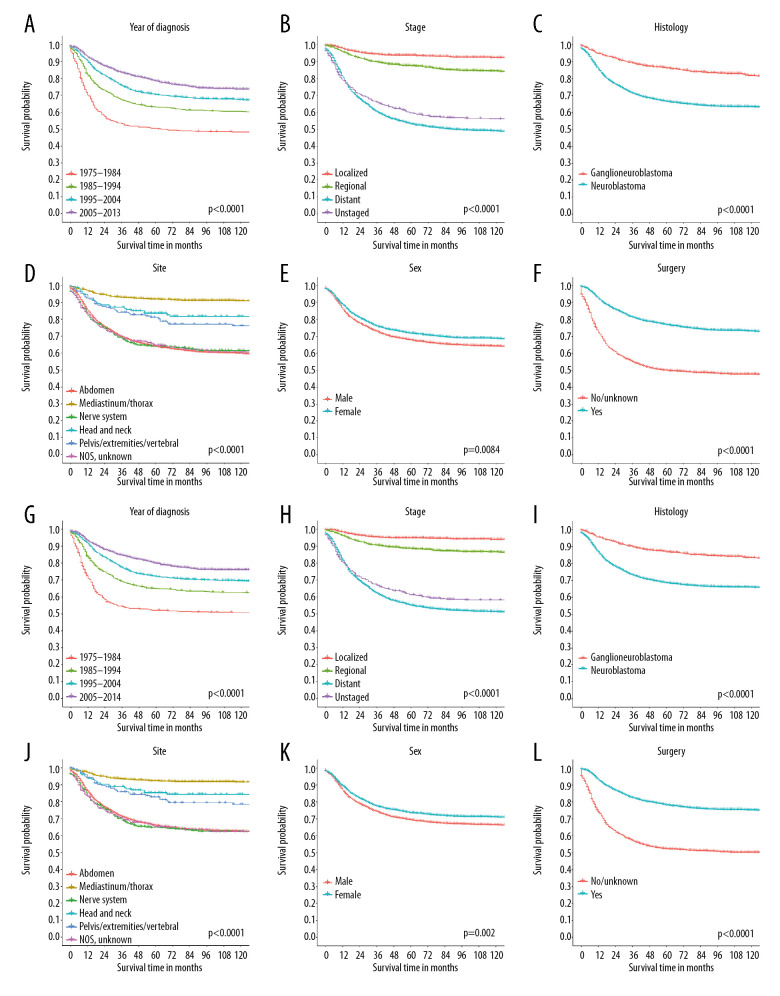
Overall, the IR of neuroblastoma has remained stable at 0.23 per 100 000 person-years since 1975. In adolescents/adults, the IR of neuroblastoma was extremely low, and declined from 0.05 to 0.01 per 100 000 person-years. Moreover, the rate in children was on the rise as a whole, from 0.50 to 0.85 per 100 000 person-years, with slight fluctuations (Figure 1). The APCs for childhood and adolescent/adult populations were −0.21 (P>0.05), 0.48 (P<0.05), and −3.81 (P<0.05), respectively (Figure 2).
Figure 1.
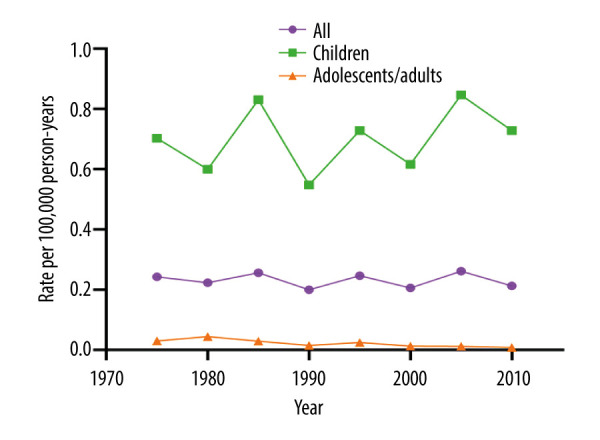
Evolution of the incidence rates of neuroblastoma by period and age group in the Surveillance, Epidemiology and End Results Program database from 1975 to 2013.
Figure 2.
Annual percentage change curves (incidence rate, per 100 000 person-years) for different populations: the general population (A), children (B), adolescents/adults (C). * Indicates that the Annual Percent Change (APC) is significantly different from zero at the alpha=0.05 level. Final Selected Model: 0 Joinpoints.
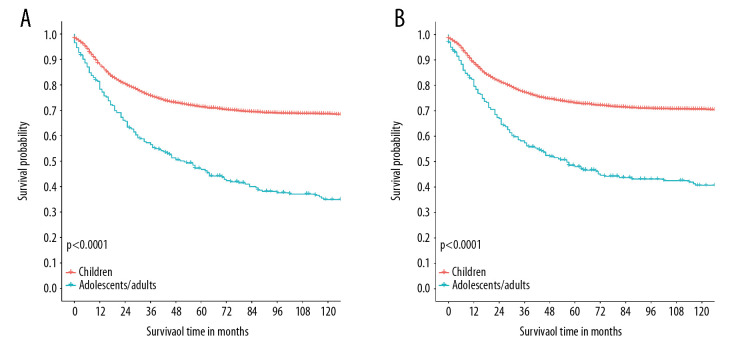
Survival outcomes
Overall, the prognosis of neuroblastoma patients has greatly improved in recent years (Figure 3A, 3G). Moreover, patients diagnosed with ganglioneuroblastoma had better OS and CSS (Figure 3C, 3I) than those diagnosed with neuroblastoma. Figure 3D and 3J shows that patients with the primary site of mediastinum/thorax had the best survival outcomes (both OS and CSS). Certainly, localized diseases (Figure 3B, 3H) and the administration of surgery (Figure 3F, 3L) resulted in better OS and CSS. Additionally, male patients had worse long-term survival than female patients (Figure 3E, 3K).
Figure 3.
Kaplan-Meier curves of overall survival (A–F) and cancer-specific survival (G–L) for neuroblastoma patients, stratified by year of diagnosis (A, G), stage (B, H), histology (C, I), primary site (D, J), sex (E, K), and the administration of surgery (C, L).
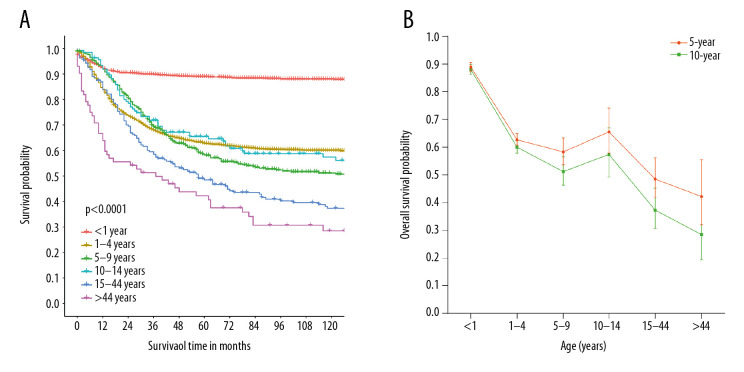
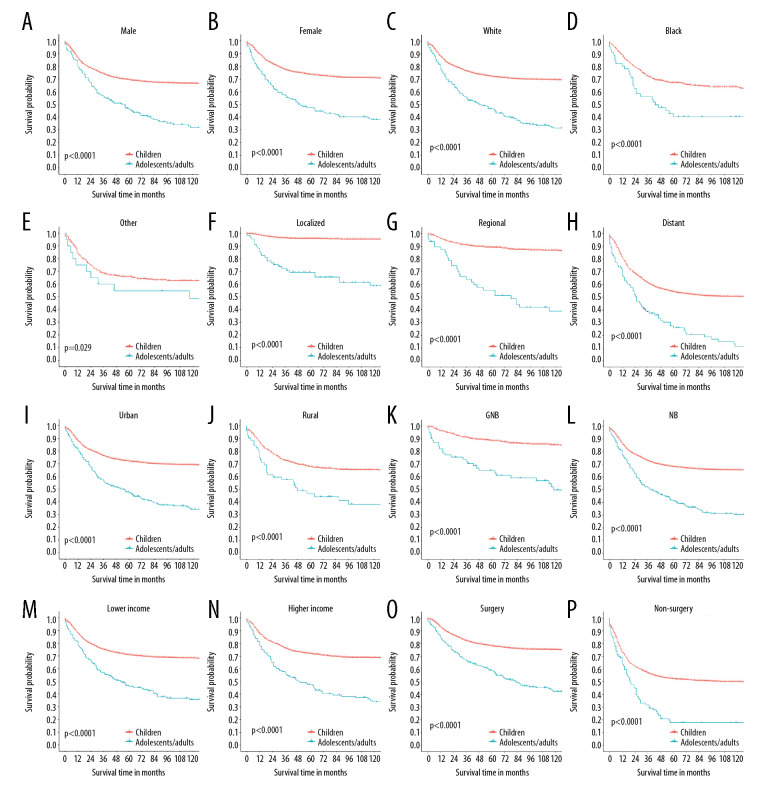
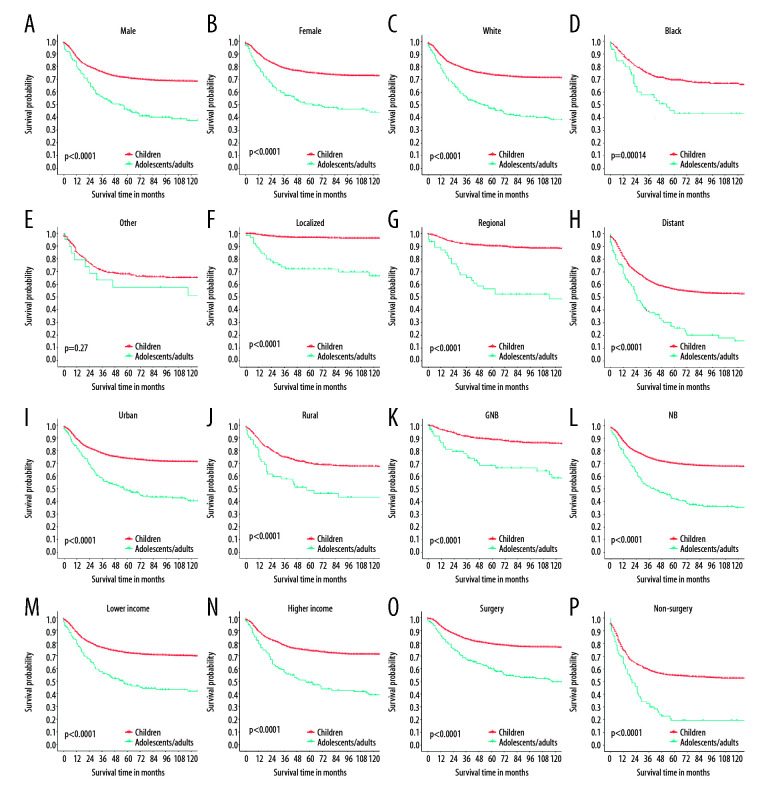
Figure 4 reveals that childhood patients had superior OS and CSS than adolescent/adult patients (P<0.001). Generally, with increasing of age at diagnosis, the OS of neuroblastoma patients decreased (Figure 5A, P<0.001). The 5- and 10-year OS rates were 88.9% (95% CI=87.2–90.6%) and 88.0%, respectively, (95% CI=86.2–89.8%) for patients young than 1 year old, and 42.2% (95% CI=32.1–55.5%) and 28.5%, respectively, (95% CI=19.3–42.2%) for patients aged over 44 years old (Figure 5B). Furthermore, we found that the prognosis of adolescent/adult patients was worse than childhood patients regardless of subgroup (Figures 6, 7).
Figure 4.
Kaplan-Meier curves of overall survival (A) and cancer-specific survival (B) for the 3998 children with neuroblastoma compared with the 282 adolescents/adults with neuroblastoma.
Figure 5.
Kaplan-Meier curves of overall survival for all patients, stratified by age at diagnosis (A), and the 5- and 10-year survival probabilities by age group (B).
Figure 6.
Kaplan-Meier curves of overall survival for adolescents/adults and children with neuroblastoma, stratified by different variables: sex (A, B), race (C–E), stage (F–H), place of residence (I, J), histology (K, L), median household income (M, N), and the administration of surgery (O, P).
Figure 7.
Kaplan-Meier curves of cancer-specific survival for adolescents/adults and children with neuroblastoma, stratified by different variables: sex (A, B), race (C–E), stage (F–H), place of residence (I, J), histology (K, L), median household income (M, N), and the administration of surgery (O, P).
Finally, multivariate Cox analyses (Table 2) showed that age at diagnosis, stage, histology, primary site, the administration of surgery, sequence of primary malignancy, treatment era, and place of residence (all P<0.05) were prognostic factors for OS in patients with neuroblastoma. In childhood patients, the risk factors were stage, histology, sequence of primary malignancy, primary site, the administration of surgery, and treatment era (all P<0.05). Furthermore, in adolescent/adult patients, sequence of primary malignancy, primary site, the administration of surgery, and treatment era (all P<0.05) were significantly associated with OS.
Table 2.
Multivariate Cox proportional hazards regression analyses evaluating factors influencing overall survival in patients with neuroblastoma.
| Variables | All patients | Childhood patients | Adolescent/adult patients | ||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | HR | 95% CI | P | |
| Age category | <0.001 | ||||||||
| Children | Reference | ||||||||
| Adolescents/adults | 3.417 | 2.811–4.154 | <0.001 | ||||||
| Sex | 0.301 | 0.204 | 0.660 | ||||||
| Male | Reference | Reference | Reference | ||||||
| Female | 0.941 | 0.838–1.056 | 0.301 | 0.924 | 0.817–1.044 | 0.204 | 0.919 | 0.631–1.339 | 0.660 |
| Race | 0.117 | 0.143 | 0.758 | ||||||
| White | Reference | Reference | Reference | ||||||
| Black | 1.181 | 1.003–1.391 | 0.046 | 1.185 | 0.995–1.412 | 0.057 | 1.124 | 0.682–1.851 | 0.646 |
| Other | 1.094 | 0.877–1.364 | 0.427 | 1.090 | 0.867–1.371 | 0.461 | 1.341 | 0.551–3.264 | 0.517 |
| Sequence | <0.001 | 0.003 | <0.001 | ||||||
| First primary | Reference | Reference | Reference | ||||||
| Not first primary | 4.092 | 2.472–6.772 | <0.001 | 3.824 | 1.574–9.291 | 0.003 | 4.725 | 2.323–9.656 | <0.001 |
| SEER stage | <0.001 | <0.001 | 0.052 | ||||||
| Localized | Reference | Reference | Reference | ||||||
| Regional | 1.756 | 1.316–2.344 | <0.001 | 2.504 | 1.703–3.680 | <0.001 | 1.422 | 0.834–2.425 | 0.196 |
| Distant | 5.803 | 4.497–7.490 | <0.001 | 9.266 | 6.520–13.168 | <0.001 | 1.879 | 1.130–3.124 | 0.015 |
| Histology | 0.013 | 0.012 | 0.540 | ||||||
| Ganglioneuro-blastoma | Reference | Reference | Reference | ||||||
| Neuroblastoma | 1.306 | 1.058–1.611 | 0.013 | 1.365 | 1.071–1.741 | 0.012 | 1.159 | 0.723–1.859 | 0.540 |
| Primary site | <0.001 | <0.001 | 0.004 | ||||||
| Abdomen | Reference | Reference | Reference | ||||||
| Mediastinum/thorax | 0.347 | 0.268–0.451 | <0.001 | 0.347 | 0.264–0.458 | <0.001 | 0.300 | 0.127–0.710 | 0.006 |
| Nerve system | 1.108 | 0.855–1.436 | 0.439 | 0.984 | 0.708–1.367 | 0.921 | 1.564 | 0.919–2.664 | 0.099 |
| Head and neck | 0.679 | 0.462–1.000 | 0.050 | 0.573 | 0.336–0.978 | 0.041 | 0.786 | 0.423–1.460 | 0.445 |
| Pelvis/extremities/vertebral | 0.545 | 0.372–0.799 | 0.002 | 0.542 | 0.339–0.868 | 0.011 | 0.439 | 0.212–0.910 | 0.027 |
| Surgery | <0.001 | <0.001 | 0.002 | ||||||
| No/unknown | Reference | Reference | Reference | ||||||
| Yes | 0.658 | 0.581–0.746 | <0.001 | 0.662 | 0.581–0.755 | <0.001 | 0.468 | 0.293–0.749 | 0.002 |
| Treatment era | <0.001 | <0.001 | 0.001 | ||||||
| 1975–1984 | Reference | Reference | Reference | ||||||
| 1985–1994 | 0.646 | 0.530–0.787 | <0.001 | 0.629 | 0.510–0.776 | <0.001 | 0.608 | 0.311–1.189 | 0.146 |
| 1995–2004 | 0.496 | 0.414–0.593 | <0.001 | 0.472 | 0.390–0.572 | <0.001 | 0.400 | 0.224–0.712 | 0.002 |
| 2005–2013 | 0.348 | 0.289–0.419 | <0.001 | 0.338 | 0.278–0.412 | <0.001 | 0.287 | 0.157–0.522 | <0.001 |
| Median household income | 0.229 | 0.222 | 0.620 | ||||||
| Low-level | Reference | Reference | Reference | ||||||
| High-level | 0.926 | 0.817–1.049 | 0.229 | 0.921 | 0.808–1.051 | 0.222 | 1.117 | 0.721–1.731 | 0.620 |
| Place of residence | 0.033 | 0.061 | 0.145 | ||||||
| Urban | Reference | Reference | Reference | ||||||
| Rural | 1.188 | 1.014–1.392 | 0.033 | 1.173 | 0.993–1.386 | 0.061 | 1.496 | 0.870–2.570 | 0.145 |
HR – hazard ratio, CI – confidence interval.
Discussion
This study was conducted to compare the IR of neuroblastoma and survival outcomes in children, adolescents, and adults using the SEER program database. In the past 40 years, the incidence of neuroblastoma in the general population has been relatively stable, maintaining at around 0.23 per 100 000 person-years. The IR in adolescents/adults showed a descending tendency, while it was on the rise in children. For survival outcomes, significantly better OS were found in childhood patients when compared with adolescent/adult patients, regardless of sex, race, tumor site, stage, place of residence, and so on. Moreover, some prognostic factors for OS in different populations were identified.
We found that the IRs had remained stable with sight fluctuations since 1975 for the general population, and presented with upward and downward trends in childhood and adolescent/adult populations, respectively. In the study conducted by Tas et al. [22], the overall IR for children aged 0–17 years ranged from 0.62 to 0.95 per 100 000 person-years between 1990 to 2014, which was comparable with the results of our study (0.50–0.85 per 100 000 person-years for childhood patients). Furthermore, the average APC in patients aged 0–17 years old was statistically significant (P=0.01). In our study, the APC for childhood patients from 1975 to 2013 was 0.48 (P<0.05). Georgakis et al. [23] compared the SEER registry with the Southern and Eastern European (SEE) cancer registries, showing that the geographical differences in IRs of neuroblastoma were possibly associated with underdiagnosis or overdiagnosis in low-income or high-income areas. Moreover, close monitoring of IR and mortality are needed to avoid unnecessary treatment while ensuring the best possible outcome for patients. Esiashvili et al. [8] investigated the IR and prognosis of neuroblastoma in adults on the basis of SEER data. They found that there was a steady decline in the IR of neuroblastoma in adults (20 years or older) from 1973–1977 to 1998–2002. Similar conclusions were drawn in the study of Ries et al. [9]. In our study, in the past 40 years, the incidence of adult neuroblastoma has shown a significant downward trend with an APC value of statistical significance.
In this study, in terms of survival, the OS and CSS rates of patients diagnosed in recent years were better than those diagnosed many years ago. Moreover, younger age at diagnosis, administration of surgery, localized stage, histological type of ganglioneuroblastoma, and primary site of mediastinum/thorax were tightly associated with better survival outcomes. Panagopoulou et al. [24] found that patients diagnosed in 2006–2008 had better OS than those diagnosed in 2000–2002 and 2003–2005. We attribute the improved survival outcomes to the advanced methods of treatment, including targeted therapy [25] and immunotherapy [26]. Ali et al. [27] reported that Wilms disease patients diagnosed in 1999–2007 had better survival outcomes than those diagnosed in 1973–1981. Additionally, in the comparisons between adolescent/adult and childhood patients, significantly better OS was detected in childhood patients regardless of race, sex, stage, place of residence, surgery, histological type, and median household income. Additionally, Esiashvili et al. [16628557] demonstrated that adults with neuroblastoma have worse prognosis than children, and infants had the best survival outcomes. Lu et al. [28] hypothesized that the higher OS in childhood patients may due to the complex heterogeneous nature of neuroblastoma with variable prognosis. The disease itself tends to spontaneously regress in pediatric patients, especially in infants, and is more likely to have metastatic status in adult patients.
Based on the results of multivariate Cox regression analyses, several risk factors for OS were identified in childhood and adolescent/adult patients. Generally, primary site, surgery, sequence of primary malignancy, stage, and treatment era were recognized as prognostic factors in all age groups. Interestingly, we noted that patients in rural areas had significantly worse OS when compared with those in urban areas (P=0.033). Lu et al. [28] considered younger age, ganglioneuroblastoma subtype, surgery, and limited lesion were significantly associated with better survival in patients with primary central nervous system neuroblastoma. However, gene-related prognostic factors were not included in our study due to the limitations of the database itself. In previous studies, many genes have been recognized to be associated with the progression and prognosis of neuroblastoma. The oncogenic role of the anaplastic lymphoma receptor tyrosine kinase (ALK) gene has already been reported because of the high protein expression levels [29]. Moreover, X-linked alpha-thalassemia/mental retardation (ATR-X) syndrome mutations in neuroblastoma have been proven to be associated with age at diagnosis, especially in MYCN non-amplified stage 4 patients over 12 years old [30]. In addition, many other genes have been shown to be associated with adverse outcomes [2].
The present study has certain limitations that should be considered. This is a U.S. population database that includes approximately 30% of all cancer cases, with incomplete individual-level data on specific cancer risk and individual treatment. In addition, there may be inaccuracies in data collection for any registry. Co-morbidities and preventive treatments are not included in SEER. Because data on tumor recurrence are not currently collected, progression-free survival (PFS) and the outcome from salvage therapies cannot be assessed. Survival outcome data may be affected by curative and palliative therapy, duration of chemotherapy, and the use of other treatments, and these were not considered in the database. Finally, patient follow-up may end if the patient moves to a different region in the U.S. where SEER data are not collected.
Conclusions
Analysis of the SEER program database between 1975 to 2013 showed that in the U.S., the incidence of neuroblastoma in children increased, but the incidence decreased in adolescents and adults. There was a trend of improved overall survival in all age groups despite the increased stage at presentation in children. However, further prospective, well-designed studies are needed to better define the clinical and genetic characteristics of neuroblastoma.
Footnotes
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors. We received permission to obtain the data from the SEER database (reference number 10977-Nov2019).
Source of support: Departmental sources
References
- 1.Suzuki M, Kushner BH, Kramer K, et al. Treatment and outcome of adult-onset neuroblastoma. Int J Cancer. 2018;143:1249–58. doi: 10.1002/ijc.31399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmed AA, Zhang L, Reddivalla N, et al. Neuroblastoma in children: Update on clinicopathologic and genetic prognostic factors. Pediatr Hematol Oncol. 2017;34:165–85. doi: 10.1080/08880018.2017.1330375. [DOI] [PubMed] [Google Scholar]
- 3.Smith MA, Seibel NL, Altekruse SF, et al. Outcomes for children and adolescents with cancer: Challenges for the twenty-first century. J Clin Oncol. 2010;28:2625–34. doi: 10.1200/JCO.2009.27.0421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xie L, Onysko J, Morrison H. Childhood cancer incidence in Canada: Demographic and geographic variation of temporal trends (1992–2010) Health Promot Chronic Dis Prev Can. 2018;38:79–115. doi: 10.24095/hpcdp.38.3.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaatsch P, Steliarova-Foucher E, Crocetti E, et al. Time trends of cancer incidence in European children (1978–1997): Report from the Automated Childhood Cancer Information System project. Eur J Cancer. 2006;42:1961–71. doi: 10.1016/j.ejca.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 6.Hsieh MH, Meng MV, Walsh TJ, et al. Increasing incidence of neuroblastoma and potentially higher associated mortality of children from nonmetropolitan areas: Analysis of the surveillance, epidemiology, and end results database. J Pediatr Hematol Oncol. 2009;31:942–46. doi: 10.1097/MPH.0b013e3181bcc809. [DOI] [PubMed] [Google Scholar]
- 7.London WB, Castleberry RP, Matthay KK, et al. Evidence for an age cutoff greater than 365 days for neuroblastoma risk group stratification in the Children’s Oncology Group. J Clin Oncol. 2005;23:6459–65. doi: 10.1200/JCO.2005.05.571. [DOI] [PubMed] [Google Scholar]
- 8.Esiashvili N, Goodman M, Ward K, et al. Neuroblastoma in adults: Incidence and survival analysis based on SEER data. Pediatr Blood Cancer. 2007;49:41–46. doi: 10.1002/pbc.20859. [DOI] [PubMed] [Google Scholar]
- 9.Ries L, Smith MA, Gurney J. Cancer incidence and survival among children and adolescents: United States SEER program 1975–1995, national cancer institute SEER program NIH Pub N99-4649. Bethesda, MD: National Cancer Institute; 1999. pp. 1–182. [Google Scholar]
- 10.Coughlan D, Gianferante M, Lynch CF, et al. Treatment and survival of childhood neuroblastoma: Evidence from a population-based study in the United States. Pediatr Hematol Oncol. 2017;34:320–30. doi: 10.1080/08880018.2017.1373315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogowitz E, Babiker HM, Kanaan M, et al. Neuroblastoma of the elderly, an oncologist’s nightmare: Case presentation, literature review and SEER database analysis. Exp Hematol Oncol. 2014;3:20. doi: 10.1186/2162-3619-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duan K, Dickson BC, Marrano P, et al. Adult-onset neuroblastoma: Report of seven cases with molecular genetic characterization. Genes Chromosomes Cancer. 2020;59:240–48. doi: 10.1002/gcc.22826. [DOI] [PubMed] [Google Scholar]
- 13.Malik D, Jois A, Singh H, et al. Metastatic neuroblastoma in adult patient, presenting as a super scan on 68Ga-DOTANOC PET/CT imaging. Clin Nucl Med. 2017;42:697–99. doi: 10.1097/RLU.0000000000001749. [DOI] [PubMed] [Google Scholar]
- 14.Kaye JA, Warhol MJ, Kretschmar C, et al. Neuroblastoma in adults. Three case reports and a review of the literature. Cancer. 1986;58:1149–57. doi: 10.1002/1097-0142(19860901)58:5<1149::aid-cncr2820580529>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 15.Platek ME, Merzianu M, Mashtare TL, et al. Improved survival following surgery and radiation therapy for olfactory neuroblastoma: Analysis of the SEER database. Radiat Oncol. 2011;6:41. doi: 10.1186/1748-717X-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mosse YP, Deyell RJ, Berthold F, et al. Neuroblastoma in older children, adolescents and young adults: A report from the International Neuroblastoma Risk Group project. Pediatr Blood Cancer. 2014;61:627–35. doi: 10.1002/pbc.24777. [DOI] [PubMed] [Google Scholar]
- 17.Conter HJ, Gopalakrishnan V, Ravi V, et al. Adult versus Pediatric Neuroblastoma: The M.D. Anderson Cancer Center Experience. Sarcoma. 2014;2014 doi: 10.1155/2014/375151. 375151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berlanga P, Vicente ML, Canete A, et al. Cancer in children and adolescents in Spain: Incidence, treatment setting and provider specialty. Clin Transl Oncol. 2016;18:27–32. doi: 10.1007/s12094-015-1330-y. [DOI] [PubMed] [Google Scholar]
- 19.Panagopoulou P, Skalkidou A, Marcotte E, et al. Parental age and the risk of childhood acute myeloid leukemia: Results from the Childhood Leukemia International Consortium. Cancer Epidemiol. 2019;59:158–65. doi: 10.1016/j.canep.2019.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sultan I, Rodriguez-Galindo C, Al-Sharabati S, et al. Salivary gland carcinomas in children and adolescents: A population-based study, with comparison to adult cases. Head Neck. 2011;33:1476–81. doi: 10.1002/hed.21629. [DOI] [PubMed] [Google Scholar]
- 21.Piscitelli P, Marino I, Falco A, et al. Hospitalizations in pediatric and adult patients for all cancer type in Italy: The EPIKIT study under the E.U. COHEIRS project on environment and health. Int J Environ Res Public Health. 2017;14 doi: 10.3390/ijerph14050495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tas ML, Reedijk AMJ, Karim-Kos HE, et al. Neuroblastoma between 1990 and 2014 in the Netherlands: Increased incidence and improved survival of high-risk neuroblastoma. Eur J Cancer. 2020;124:47–55. doi: 10.1016/j.ejca.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 23.Georgakis MK, Dessypris N, Baka M, et al. Neuroblastoma among children in Southern and Eastern European cancer registries: Variations in incidence and temporal trends compared to US. Int J Cancer. 2018;142:1977–85. doi: 10.1002/ijc.31222. [DOI] [PubMed] [Google Scholar]
- 24.Panagopoulou P, Georgakis MK, Baka M, et al. Persisting inequalities in survival patterns of childhood neuroblastoma in Southern and Eastern Europe and the effect of socio-economic development compared with those of the US. Eur J Cancer. 2018;96:44–53. doi: 10.1016/j.ejca.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 25.Duong C, Yoshida S, Chen C, et al. Novel targeted therapy for neuroblastoma: Silencing the MXD3 gene using siRNA. Pediatr Res. 2017;82:527–35. doi: 10.1038/pr.2017.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jabbari P, Hanaei S, Rezaei N. State of the art in immunotherapy of neuroblastoma. Immunotherapy. 2019;11:831–50. doi: 10.2217/imt-2019-0018. [DOI] [PubMed] [Google Scholar]
- 27.Ali AN, Diaz R, Shu HK, et al. A Surveillance, Epidemiology and End Results (SEER) program comparison of adult and pediatric Wilms’ tumor. Cancer. 2012;118:2541–51. doi: 10.1002/cncr.26554. [DOI] [PubMed] [Google Scholar]
- 28.Lu X, Zhang X, Deng X, et al. Incidence, treatment, and survival in primary central nervous system neuroblastoma. World Neurosurg. 2020;140:e61–72. doi: 10.1016/j.wneu.2020.04.145. [DOI] [PubMed] [Google Scholar]
- 29.Passoni L, Longo L, Collini P, et al. Mutation-independent anaplastic lymphoma kinase overexpression in poor prognosis neuroblastoma patients. Cancer Res. 2009;69:7338–46. doi: 10.1158/0008-5472.CAN-08-4419. [DOI] [PubMed] [Google Scholar]
- 30.Cheung NK, Zhang J, Lu C, et al. Association of age at diagnosis and genetic mutations in patients with neuroblastoma. JAMA. 2012;307:1062–71. doi: 10.1001/jama.2012.228. [DOI] [PMC free article] [PubMed] [Google Scholar]