Abstract
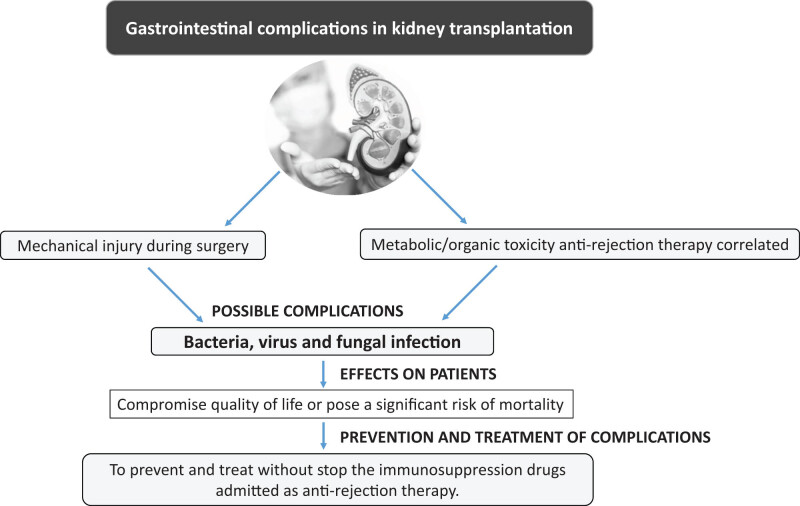
Kidney transplantation is the surgical operation by which one of the two original kidneys is replaced with another healthy one donated by a compatible individual. In most cases, donors are recently deceased. There is the possibility of withdrawing a kidney from a consenting living subject. Usually, living donors are direct family members, but they could be volunteers completely unrelated to the recipient. A much-feared complication in case of kidney transplantation is the appearance of infections. These tend to arise due to immune-suppressor drugs administered as anti-rejection therapy. In this review, we describe the gastrointestinal complications that can occur in subjects undergoing renal transplantation associated with secondary pathogenic microorganisms or due to mechanical injury during surgery or to metabolic or organic toxicity correlated to anti-rejection therapy. Some of these complications may compromise the quality of life or pose a significant risk of mortality; fortunately, many of them can be prevented and treated without the stopping the immunosuppression, thus avoiding the patient being exposed to the risk of rejection episodes.
Keywords: immunological and non-immunological complications, organ rejection, consequences of surgery, immunosuppressive therapy, infectious risk, development of neoplasms, gastrointestinal complications
Graphical abstract
1. Introduction
Organ transplantation is one of the greatest achievements of modern medicine and allows a person who has lost his or her native organ’s functions to regain them and in some cases allow the survival of the patient [1]. The first kidney transplants in humans were made in the 50s and 60s of the last century and since then this practice evolved to become the best therapy for advanced renal failure. Transplantation is a surgical operation during which a kidney obtained from a donor (cadaver or living) is implanted inside the recipient’s body. In this case, kidney transplantation is a heterotopic transplant, that is, an organ is placed in a different location with respect to the native organs, which therefore are not removed (with the exception like polycystic kidney disease). The kidney is placed in the iliac fossa unless there are anatomical particularities that prevent it. The graft’s arteries and veins are joined to the recipient’s vessels and the ureter to the bladder, but this is not enough because for the transplantation to work a therapy is needed that allows the organism not to reject the transplanted organ. Currently, many drugs prevent acute kidney rejection with an act on the immune system of the transplanted patient; and if on the one hand they prevent the body from attacking the kidney, on the other hand, they lower the immune defenses, making it more susceptible to severe infections and tumors [2]. The duration of the transplant is variable (<5 or 5–20 years) and depends on several factors (renal disease, the organ transplanted characteristics, effectiveness of immunosuppressive therapy, etc.). After transplantation, the patient must take immunosuppressive therapy, until the kidney continues to function. Furthermore, the patient should undergo periodic checks, which must be very frequent in the first months after transplantation and can then be reduced over time. In the first months after transplantation, due to the powerful immunosuppressive therapy, the patient must limit contacts with people as much as possible. To evaluate the eligibility for transplantation, patients must undergo numerous physical and psychological tests. The age of the transplant candidate is a very important factor and even if there are no defined age limits, older patients may have more difficulty in being transplanted due to the presence of multiple pathologies. For older patients, it is possible to use transplants from older donors and therefore of compatible age.
The condition of suitability for transplantation is subjected to continuous revision and immunological parameters are evaluated to identify the most suitable organ allocation to the patient s profile. Kidney transplantation in most cases is not a lifesaving transplant because dialysis allows survival of patients with renal failure. Compared to dialysis, transplantation is a therapeutic physiological alternative, especially in cases where the renal function returns to normal or close to normal. It allows people not to be dependent on dialysis and overcome the first months of isolation, so that they are able to move in full freedom and also re-enter fully into social and working life [3].
2. Types of renal transplantation
Kidney transplantation is the surgical procedure by which a kidney taken from a donor is placed in the body of a patient (recipient) with terminal renal insufficiency. There are several types of transplant, which can be classified according to the type of donor from which the organ originates.
2.1. Deceased donor kidney transplant
The organs destined to the donation are taken from patients whose death has been ascertained and with the consent or non-opposition of the family members. In order for an organ to be taken for a transplant, it is necessary that there are no serious diseases or conditions in the donor that could compromise the success of transplant or cause long-term complications for the recipient. Once the suitability of the donor has been ascertained, the organ is removed.
The following are the three types of cadaver donors:
-
(A)
Organs come from donors whose brain death has been ascertained. Death is identified with the irreversible cessation of all brain functions due to primary or secondary encephalic damage (traumatic, hemorrhagic, and anoxic). This means that all the nerve functions that supervise life have ceased and that only the cardiorespiratory activity is artificially supported to guarantee the blood supply to the organs to be taken.
-
(B)
Organs come from donors over 70 years old or over 60 years old with associated risk factors such as impaired renal function or presence of diseases (hypertension, diabetes, etc.). Once the suitability for the donation has been ascertained (renal tissue is evaluated), these organs are usually used for a double transplantation in a single recipient (also elderly).
-
(C)
Organs come from donors who died of cardiac death in which any attempt at resuscitation was useless. Death is identified with the irreversible cessation of all vital functions determined by cardiocirculatory arrest with consequent irreversible loss of all functions of the brain. Once the subject (consent or non-opposition of the family) becomes a donor, he or she is subjected to well-defined procedures designed to maintain the fitness of the organs for the purpose of transplantation.
2.2. Living donor kidney transplantation
This procedure requires that the organ to be transplanted comes from a subject still alive. The donor must be of legal age and may be a kinsman (family member), a non-consanguineous associate affective to the recipient or an unknown person. The act of donation is totally free, always revocable and without any kind of constraint/coercion (to be understood both physically and psychologically) toward the recipient. The risk of surgery for the donor is the same as any other surgery and it is now widely demonstrated that with a single kidney it is possible to lead a normal life. However, both the donor and the recipient must be aware of the limitations of transplant therapy and aware of all possible clinical complications for both possible personal consequences and psychological implications. For these reasons an explicit and informed consent must be expressed, one must undergo a psychological–psychiatric exam and further evaluation by a special commission is required as well as the clearance of the judicial authority. The living transplantation is beneficial due to the fact the evaluation process of the candidates can be followed so that both the donor and the recipient are in the best conditions of health and it is possible to program the surgery. Furthermore, by reducing the time between organ harvesting and transplantation, better results can be achieved in relation to functional recovery and organ survival. The kidney harvesting surgery is done using laparoscopy procedure, which consists of four holes in the abdomen through which the kidney is extracted. In the absence of complications, the length of hospital stay is 3–4 days. Particular situations may require the need to prepare specific therapeutic and surgical protocols; these may include cases of transplantation (patients with previous transplantation) and the so-called “hyperimmune” patients (who have antibodies circulating already before transplantation).
2.3. Non heart-beating donor (NHBD)
NHBD is a type of donation in which the donor suffered a cardiac death, unlike the best known and used donation from deceased donors following brain death, or donors to beating heart (HBD). The spread of this type of transplant has remained for a long time limited to few countries (Japan, Holland, Spain and England) The term “death due to cardiac arrest” refers to the death that occurs following the cessation of the body circulation for a period of time that determines the irreversible loss of all brain functions, which is ascertained by a doctor by detecting the absence of a heartbeat (asystole) with a 20-min electrocardiogram. The deceased donor for cardiac causes is suitable for the removal of all organs except the heart; the privileged organs are the ones most resistant to ischemic damage, in particular kidneys, liver, and pancreas. Cardiac arrest is the peculiarity but also the main criticality of this mode of donation. During the asystole condition, the kidney does not receive blood supply due to the interruption of the circulation, the refrigeration of the organ and the subsequent reperfusion after the transplant, causing a type of damage defined as ischemia–reperfusion that is potentially higher than that observed in the transplant from a standard donor. To minimize this damage, organ perfusion techniques are used before and after the explant. After the explants, the organs can be kept at 4°C in special storage solutions or positioned inside a dedicated machine that, depending on the model, allows the organ to be perfused in a pulsatile or continuous way with a specific preservation liquid. The latter is the storage method used in the case of NHBD donors (non-beating heart). It has been widely demonstrated that the use of this technique significantly reduces the risk of delay in post-transplant functional recovery (delayed graft function (DGF)), improving the survival of the organ as well as better storage, and it also allows an assessment of suitability before surgery. As in the case of HBDs, organs taken from NHBDs are also assessed on the basis of a series of criteria to establish their suitability before surgery; in order for this type of program to work optimally, the presence of a team is necessary, consisting of various specialized professionals trained to act in a very short time. The data collected so far show a greater number of cases in which there is a delay in functional recovery (DGF) for a prolonged ischemia time. However, the available data show that this event does not affect the long-term survival of the transplanted organ. NHBD is a valid alternative to heartbeat transplantation and an extra chance to receive an organ.
2.4. Living donor kidney transplantation
Living donor transplantation is the best alternative in case of terminal chronic renal failure [4]. In fact, it has many advantages compared to the deceased donor transplantation such as a better degree of donor–recipient compatibility, a shorter waiting time and a reduction in damage related to organ preservation. In USA and in Japan, the percentage of living donor donation is very high; in Italy, on the other hand, there is little information concerning the living transplant, which unfortunately represents only 10% of the transplants performed. The law states that the spontaneous nature of the donation must always be ascertained to exclude any form of trade. In addition, the potential donor must be competent, aged no more than 75–80 years and “healthy”. In fact, although the focus is often on restoring health to the recipient, an equally important goal is to make sure that the donor can maintain his or her state of health after the donation. However, the assessment of eligibility requires a clinical evaluation and specific laboratory and instrumental tests. The donor is subjected to cardiological, vascular, pneumological, gastroenterological and hemocoagulative evaluation in order to exclude risks related to surgery, to nephrological exam to exclude that the removal of a kidney does not negatively affect survival or residual renal function and to immunological tests that highlight the degree of compatibility between donor and recipient; in addition, the presence of neoplasms or infections, such as hepatitis B, hepatitis C or HIV infection, which can be transmitted to the recipient, must be excluded. The candidate is subjected to a psychological evaluation in order to investigate the motivations that lead him or her to donate, the knowledge of possible risk factors and the anxieties about the success of the transplant; a more thorough psychological evaluation is made in case of altruistic donation, that is, to an unknown person. The kidney withdrawal surgery takes the name of nephrectomy and can be done in two ways: the laparoscopic procedure which consists of making four holes in the abdomen through which the laparoscopic instruments are inserted and a small incision through which the kidney is extracted or the laparotomic mode which consists of opening of the abdomen and is a little more invasive. In the absence of complications, the length of hospital stay is 3–4 days. The main risks of donation are related to surgery. The mortality of the donor linked to perioperative cardiovascular complications is however very modest and corresponds to an incidence of 0.03–0.05%, equaling to that reported in the most common surgical procedures. With regard to the long-term risks, careful selection of the donor allows the consequences to be very low; donors have a survival comparable to that of the general population. A fundamental advantage of living transplantation is related to time before the transplant; in fact, the longer you stay in dialysis, the lower the survival of patients after transplantation. The availability of a living transplant can reduce the stay in dialysis or even avoid it: in fact, a living donor transplant can be performed before the start of dialysis treatment (preemptive transplantation). The main obstacles to living donation are the presence of ABO blood group incompatibility between the donor and the recipient and the presence of antibodies in the recipient against the donor. In order to cope with these obstacles and therefore increase the possibility of donations from living donors, kidney transplantation can be performed between incompatible ABO subjects, treating the recipient with desensitization therapies about 1 month before and by plasmapheresis a few days earlier in order to eliminate antibodies against the donor. Since the organ demand is much higher than the supply of kidneys from a deceased donor, the living donor transplant represents a valid therapeutic option; i.e., being able to have a living donor allows a quick and safe transplantation without particular risks for the donor.
3. Complications related to kidney transplantation
Complications after a transplant can be related to the surgery itself (infection or abscess) or immunosuppressive therapy that the patient must continue for the life (cytomegalovirus [CMV] or viral infections) [5,6,7,8]. Several authors also reported in this setting of patients the risk of developing neoplasms like lung carcinoma and renal cell carcinoma [2,9] and lymphomas [10,11,12] (Table 1). Immunosuppressive therapy significantly reduces defenses against infections, so it is necessary to exclude any infectious or inflammatory condition before surgery. This therapy promotes the reduction in the body’s ability to control and eliminate cancer cells, so before receiving the organ it is necessary to exclude any condition of neoplasia or pre-cancerous disease in progress.
Table 1.
The complications in kidney transplantation
| Etiology | |
|---|---|
| Systemic infection | Candida spp., Cryptococcus neoformans, Pneumocystis carinii, cytomegalovirus |
| Gastrointestinal complications: | |
| Esophagus–gastric infections | CMV, Herpes simplex virus (HSV) and C. albicans, C. krusei, C. tropicalis, C. parapsilosis, Torulopsis glabrata |
| Bacterial infection | Helicobacter pylori, Clostridium difficile, Campylobacter jejuni, Salmonella spp. |
| Viral infections | CMV, HSV, Epstein-Barr virus. |
| Diarrheal episodes | Bacterial, viral and parasitic (Caliciviruses spp., HSV, Clostridium difficile, Salmonella spp., Campylobacter jejuni, and CMV) |
| Immunosuppressive drugs | Gastroduodenal ulcer and gastroduodenitis |
| Complications related to kidney transplantation: | |
| Early complications | Viral infections, abscess, colonic ischemia, pseudomembranous colitis, hemorrhages and infections related to treatment of acute rejection |
| Complications after 1 year post-transplantation | Diverticular disease, intestinal occlusion, colitis or neoplasms and intestinal perforation |
| Transplantation and risk of cancer | Lung carcinoma, renal cell carcinoma, lymphomas and leukemia |
In particular, gastrointestinal complications can occur in many kidney transplant recipients. Such complications may be secondary to pathogenic microorganisms but may also be induced by mechanical or metabolic causes or by immunosuppressive drugs. Although this type of complication can compromise the quality of life of the transplant or be responsible for mortality, it can generally be prevented or treated without interfering with immunosuppression. Gastrointestinal complications are among the major causes of morbidity and mortality in immunosuppressed subjects [13,14,15] (Table 1). The digestive sphere represents, in fact, one of the privileged targets of clinical manifestations in patients with congenital immunodeficiency, in those subjected to organ transplantation or bone marrow or to immunosuppressive therapy for neoplasm or autoimmune disease [16,17]. This is may be due to the lymphoid tissue (macrophages and lymphocytic cells) localized in the chorion of the digestive mucosa. The onset of gastrointestinal infections in these subjects depends on the time from transplantation, age, the presence of chronic viral infections and pathologies present before transplantation (diverticular disease of the colon, peptic ulcer disease, diabetes, etc.), on the use prolonged of certain techniques (nasogastric tube), on exposure to pathogenic germs in community or hospital and on immunosuppressive therapy [18,19,20,21,22,23,24]. Budiño et al. [24] found that the main causes of death in 156 transplant recipients subjected to autopsy are infections, with a percentage ranging from 21 in heart transplant patients to 63 in those receiving a lung transplant [25]. Regarding the temporal appearance of gastrointestinal complications, in the first 30 days after transplantation, candida esophagitis or herpes simplex virus (HSV) and Clostridium difficile (CD) infection represent the most common pathologies. From 1 to 6 months after transplantation, viral and opportunistic infections occur, mainly from CMV; while after 6 months, 80% of patients are susceptible to infections for pathogens acquired in the community [26].
4. Esophagus–gastric infections
The esophagus is the organ most frequently affected by gastrointestinal complications in subjects receiving immunosuppressive therapy. The use of different prophylactic strategies, especially in the early phase of post-transplantation, has dramatically decreased esophageal and gastric infections. The most commonly implicated pathogens are CMV, HSV and Candida [27,28,29,30,31,32,33,34] (Table 1). Clinically, the most frequent symptom is dysphagia. Other modes of presentation of esophago-gastric lesions are the following: painful sensation during swallowing (odinophagia), retrosternal pain, dyspepsia, oral ulceration, and epigastralgia. In other studies, transplanted patients underwent endoscopy, with the identification of opportunistic infections in 64% of subjects with dysphagia, 39% with dyspepsia and 17% with hemorrhage; less common symptoms reported are nausea, vomiting, anorexia, hiccups and obstruction [35,36]. Most of these infections occur 2–6 months after transplantation, with a prevalence of 5% in kidney transplant recipients [37]. Candidiasis is the most common opportunistic infection in transplant patients, and Cryptococcus neoformans and Pneumocystis carinii can also be observed. Predisposing factors for infection are neoplasms, especially lymphomas and leukemia, organ transplants, prolonged therapy with antibiotics or corticosteroids, malnutrition, diabetes, and immunosuppressive therapy. Clinically esophageal candidiasis is diagnosed because of dysphagia, as the lesion of the mucosa is little or not ulcerated and the other symptoms, above all the painful ones (odynophagia, retrosternal pains, or epigastralgia) are rare. Nausea and hiccups or even asymptomatic forms are also observed [38]. Complications are rare and consist of hemorrhage, pseudotumoral stenosis, perforation or fistulization in the bronchi or mediastinum, while distant dissemination is exceptional. Therefore, the importance of esophageal candidiasis is not related to complications but to the possible repercussions on nutrition, and in the majority of cases, subjects already defected. Endoscopy is the examination of choice to obtain a diagnosis of certainty (Table 1). It can be postponed when the symptoms are striking and there is a diagnosis of esophageal candidiasis. In these cases, the probability of a relapse is so high that ex-juvantibus therapy is justified without further investigation [38]. Typical endoscopic manifestations are white-yellowish membranes or plates scattered on the esophageal mucosa, sometimes confluent, which can form longitudinal striae with a track-like appearance. The mucosa can be completely covered by pseudomembrane; and in some cases, the lumen can be obstructed. Membranes can rarely be blackish, while they are often easily detachable from the underlying mucosa, which may have a normal, erythematous, erosive or hemorrhagic appearance. In the case of descending candidiasis, i.e., starting from the oral cavity, the upper part of the esophagus is most frequently affected. The endoscopic aspect is so typical that biopsies are not indispensable and because of these lesions, differential diagnosis is not a problem. In uncertain cases, especially when the lesions are minimal, the diagnosis of certainty is evidenced by yeasts and filaments of mycetes, or by the cultivation of fungi from the biopsy samples. The culture test must be carried out when there is resistance to antifungal therapy in order to characterize the species of candida involved and provide an antifungigram. In fact, although Candida albicans is the most common species, infections are also caused by C. krusei, C. tropicalis, C. parapsilosis, Torulopsis glabrata, etc. (Table 1). Systemic antifungal therapy is used. Symptomatological improvement is usually rapid in 3–5 days. The duration of treatment ranges from 10 to 15 days [39]. The prophylaxis of fungal infections is different depending on the programs of the different transplant centers [40].
5. Viral infections
CMV infection is the most frequent, but other viruses such as HSV and Epstein–Barr virus can be due to serious esophagogastric complications [41] (Table 1). Helicobacter pylori (H. pylori) plays an important role in the pathogenesis of antral gastritis and peptic ulceration in the general population. H. pylori infection can be diagnosed by invasive methods, requiring endoscopy and biopsy sampling (histological examination, rapid urease test, culture, polymerase chain reaction) and non-invasive techniques such as urea breath test (breath test), the search for bacterium antigens on fecal samples or the search for specific antibodies in the blood and urine [42,43,44,45,46,47]. (Table 1). Among the non-invasive tests, only the breath test or the search for antigens of the bacterium in the stool allow to identify the infection in place and that is why they are called direct. The search for specific antibodies both in the blood and in the urine, on the contrary, represents only an index of successful exposure to H. pylori (immunological memory) but not of infection in progress and therefore are defined indirect tests. The prevalence of H. pylori is reported 70% in hemodialysed subjects and 60% in those undergoing kidney transplantation. Gastritis was found in 65% of kidney transplant patients and only in 19% of hemodialysis patients, suggesting that other factors contribute to the onset of gastric lesions [41]. Teenan et al. [40] performed endoscopy in 33 patients, 2–4 months after kidney transplantation, and identified 16 cases of duodenitis, 10 of gastritis and 4 of gastric ulcer. H. pylori was detected in 48% of cases of antrum gastritis; no association was observed between H. pylori infection and plasma levels of cyclosporine or corticosteroids [40].
6. Cytomegalovirus infections
CMV infections are mostly esophagitis. Unlike HSV, CMV can cause systemic symptoms such as fever and weight loss. Being an immunomodulatory virus, other pathogens such as Aspergillus may cause disease [48] (Table 1). CMV seems to facilitate the onset of bacterial, fungal and viral infections, through a direct immunosuppressive effect. The lesions can arise due to a reactivation of the latent virus or a primary infection. The reactivation of CMV occurs 1–4 months after organ transplantation. Immunosuppressive anti-rejection therapy can prolong this period of high susceptibility to infection; only rapamycin is associated with a low incidence of CMV infections [49]. Symptoms that are often painful are represented, in order of frequency, by odynophagia, retrosternal pains, and dysphagia. Endoscopy is essential for diagnosis [50], more frequently the lesions are located in the lower half of the esophagus (Table 1). The most typical aspect is that of ulcerations excavated in irregular margins, sometimes covered by fibrin, rarely hemorrhagic; it is also possible to observe only an erythema of mucosa, or an erythema with erosions and some pseudotumoral forms have been observed too. Deep biopsies must be performed on the bottom of the crater and on the margins (the viral particles are localized in the chorion) to highlight the characteristic intranuclear inclusions in the connective cells. If inclusions are not visible, one should systematically perform an immunohistochemical study associated with standard methods for detecting viral particles. The therapy is based on virostatic agents to be used in environments specialized for their toxicity. At the gastric level, CMV is found more rarely and manifests itself with epigastralgias [49,51]. The diagnosis is made with endoscopy showing the typical appearance of ulcerative gastritis, of unique or numerous mold ulcerations, or with the less typical appearance of erythematous gastritis. CMV inclusions are also present in biopsy samples of healthy mucosa, so sometimes the clinician faces the problem, not indifferent considering the toxicity of effective drugs, of deciding whether to treat asymptomatic subjects.
CMV is usually localized in the colon, both segmentally and widespread. Ileal lesions that determine a very serious necrotic enterocolitis have also been described. Diarrhea is associated with abdominal pain, while systemic symptoms such as fever are rare. Gastrointestinal hemorrhages, perforations and toxic megacolon are possible in patients with preexisting gastroenterological diseases. The virus can proliferate in vascular endothelial cells causing vasculitis, thrombotic phenomena and local ulcerations. When the damage is very extensive, an ischemic colitis may occur, which may be an early complication in the first 4 months after kidney transplantation [52]. The most frequently involved segments are terminal ileum, cecum and ascending colon up to hepatic flexure [53]. Colitis from CMV occurs in transplanted patients with isolated, wide and molded ulcerations prevailing in the right colon, and the clinical picture is often characterized by hemorrhagic manifestations. CMV infection usually occurs in the first 6 months after transplantation [54,55]. Diagnosis of infection is made with colonoscopy with deep biopsy samples that show typical nuclear inclusions [50]. The virostatic drugs are intravenously effective but do not protect against relapse [56]. CMV causes bloody diarrhea and ulcerative lesions in the colonic mucosa. They have been identified as pathogens of enteritis especially in transplant patients [25]. Nosocomial outbreaks are reported in patients undergoing solid organ transplants or with cancer [57].
7. Other gastrointestinal complications
Diarrhea is one of the most frequent post-transplant complications and may result in discontinuity of immunosuppressive therapy. Usually supported by bacterial, viral and parasitic causes, the onset can also be determined by drugs used in the post-transplantation period. Caliciviruses can cause a prolonged diarrhea that resolves by reducing the dosage of immunosuppressive drugs. HSV is a rare cause of colitis in transplant recipients (Table 1). Colonoscopy can detect erythema, fragility of the mucosa, aphthous ulcers and necrotic ulcerative lesions. The defined diagnosis is based on the isolation of the virus after culturing the biopsy specimens [58].
The incidence of diarrheal episodes is 12.6%, with 41.5% of cases related to infectious episodes and 34% correlated to drugs [59]. The average period of onset of diarrhea was about 10 months after transplantation (2–12 years). Furthermore, while 12% of the episodes occurred in the first month, 22% were diagnosed around 1–6 months post-transplant and 66% in the late period (after 6 months) [59].
The CD is responsible for about 50% of diarrheal episodes associated with antibiotic treatment (Table 1). The mode of presentation varies from asymptomatic pictures, to febrile enterocolitis, to toxic megacolon. It is common in patients with transplantation and often occurs in semiepidemic or endemic form, with transmission from person to person and with spores that persist on the surfaces of the environments.
Another infectious cause of post-transplant diarrhea is Salmonella infection, which has a clinical syndrome characterized by febrile diarrhea, with or without polymorphonuclear leukocytes in the feces. Bacteremia is common in patients transplanted with salmonella gastroenteritis: approximately 20–30% compared to 3–4% of non-transplant recipients [22]. Campylobacter jejuni is the most commonly reported bacterial cause of foodborne infection which causes gastroenteritis and diarrhea. The epidemiology is similar to that of Salmonella and the clinical syndrome is characterized by febrile diarrhea with nausea and vomiting, and about 70–85% of patients present leukocytes and blood in the stool. CMV causes a febrile syndrome with diarrhea, which can be associated with bleeding, possible perforation, ischemic colitis and/or toxic megacolon [22,60]. In a study evaluating gastrointestinal complications in 580 kidney transplant patients, six cases of CMV colitis were detected, with death in two patients [27]. In addition to the infectious causes, diarrhea can also be correlated with some immunosuppressive drugs that are able to alter the transit time or interfere with the complex system of the intestinal flora [61,62,63].
8. Gastrointestinal perforations
Colorectal complications after renal transplantation can occur both early and after transplantation and are a direct consequence of the biological modifications produced by immunosuppressive therapy [64] (Table 1). Early complications such as colonic ischemia, pseudomembranous colitis, hemorrhages or infections may be related to treatment of acute rejection. Complications at a distance from transplantation include diverticular disease, intestinal occlusion, colitis or neoplasms. Diverticular disease is the most common source of gastrointestinal complications, with most cases occurring after 1 year post-transplantation but has also been reported in the early post-operative phase. In particular, diverticulitis complicated by intestinal perforations, abscesses, phlegm or fistulas has been reported in approximately 1.1% of kidney transplant patients [65]. An increase in the incidence of diverticular disease and intestinal perforation has also been reported, without a clear explanation, in patients undergoing kidney transplantation with polycystic kidney disease [66,67].
9. Transplantation and risk of cancer
Undergoing an organ transplant can save lives, but it can also increase the risk of cancer [68,69,70,71,72,73,74,75,76,77,78]. Among patients who have undergone a solid organ transplant, the risk of getting cancer is 50% [79] (Table 1). Other diseases, incorrect lifestyles and anti-rejection drugs, are among the main responsible. The incidence of 12.6% of colorectal neoplasms has been observed in kidney transplant patients. The risk factors identified are age at transplantation, pre-transplant splenectomy, a history of pre-transplantation neoplasia and cigarette smoking [80]. Vera et al. [81] showed a significant increase in colorectal neoplasms after liver transplantation in subjects with primary sclerosing cholangitis and ulcerative colitis. The risk factors for the development of colorectal neoplasia have been colonic dysplasia after transplantation (p < 0.00003), duration of colitis for more than 10 years (p < 0.002) and pancolitis (p < 0.0004). In these settings, a follow-up with a colonoscopy is recommended [81].
10. Immunosuppressive drugs and gastroenterological complications
As stated previously, complications after a transplant can be immunological and non-immunological (Table 1). The most important immunological complication of renal transplantation is the rejection that can be acute or chronic. To prevent or mitigate the recipient’s immunological response, it is subjected to a scheme of immunosuppressive therapy with the intake of one or more drugs that limit host defense responses, modulating one or more stages of rejection. The transplanted patient, subjected to immunosuppressive therapy, can present some specific complications. In fact, immune-suppressor drugs with their intrinsic toxicity are also responsible for multiple complications involving the digestive system. Sirolimus is an immunosuppressive drug used to prevent rejection in kidney transplants. The effect of sirolimus on causing oral ulcers is known [82,83]. Three cases of gastroduodenal ulcer bleeding are reported in patients receiving sirolimus [83]. The causes of ulcer in these patients are multifactorial and sirolimus has certainly played an important role in slowing the tissue-healing processes despite ongoing anti-secretory therapy. In the literature is reported a case of abdominal pain caused by gastroduodenitis from leukocytoclastic vasculitis in a kidney transplant patient on sirolimus. Both the symptomatology reported by the patient and the histological lesion on the antral level regressed after the suspension of the sirolimus [84].
11. Kidney transplantation and nutritional status
A concept that is emerging strongly in the field of clinical nutrition is the possibility of improving the course of a disease in different and serious conditions, thanks to the modulation of the diet. The state of nutrition can influence the trend, the prevalence of complications and the prognosis of many diseases and is variously compromised during illnesses. Dialysis patients are subject to profound metabolic and nutritional changes that modify the energy balance in a chronic and persistent form. Following the diet is essential for patients, regardless of the method adopted: the food plan makes the dialysis treatment more effective and improves the state of nutrition of the subject. Since the uremic condition is not perfectly correct by the dialysis methods, malnutrition in dialysis is present from 18% to 75% depending on the method used for the assessment of the state of nutrition and is one of the factors responsible for high mortality. On the other hand, also from this point of view, kidney transplantation represents the best substitution therapy for patients with chronic renal failure in terms of survival, quality of life and sensation of subjective well-being. Furthermore, transplantation represents the possibility of liberalizing the diet after the limitations imposed by conservative therapy and dialysis. However, most of the patients who have undergone renal transplantation tend to be overweight because the use of immunosuppressive and corticosteroids, generating among other side effects the increase in appetite, fat mass and retention of sodium and water. This increase will lead to higher calorie needs than the actual energy needs.
The outcome of kidney transplantation can be influenced by the patient’s nutritional status. Malnutrition, obesity and other metabolic complications can be prevented or corrected by appropriate food interventions. Weight control therefore plays a fundamental role in therapy and lifestyle. Furthermore, as described above, gastrointestinal complications can occur in many subjects undergoing transplantation. The first tool to be used is proper nutrition, supported by any nutritional approaches, to reduce the symptoms of gastroesophageal pathologies [14]. The diet to be followed will not be very different from that of an individual who is not transplanted and will be much easier to follow than that prescribed during dialysis. Currently, only a few randomized clinical trials on the best nutritional treatment after kidney transplantation are available. Furthermore, it is important to develop guidelines for optimizing the nutritional status of patients with chronic kidney disease at all stages and for the management of patients undergoing kidney transplantation. In the future, further studies should be performed to evaluate the effect of nutritional manipulation in kidney transplant patients and to provide data for a structured, multidisciplinary dietary approach to post-transplant nutritional care.
12. Conclusions
Organ transplantation represents one of the most important clinical achievements of the second millennium due to the positive clinical implications in the treatment of numerous unfavorable and not effectively treatable diseases. In recent years, several therapeutic protocols have been developed and perfected, which more specifically seek to inhibit rejection, trying to safeguard at least in part a residual capacity of the immune system to defend the organism with the reduction in the side effects related to the chronic use of drugs. Currently, the 5-year survival from kidney transplantation is more than 90% in transplant recipients. However, the anti-rejection immunosuppressive drugs necessary for the success of the transplant and for the patient’s survival are directly associated with an increased frequency of infections and tumors associated with viral infections, which are the main causes of morbidity and mortality in people undergoing kidney transplantation; in terms of incidence this risk is quantifiable by about 2- to 3-fold increase in developing any post-transplant de novo tumor. Prolonged exposure to immunosuppressive drugs, in fact, seems to negatively influence the ability of antiviral and antitumor immunosurveillance and to enhance the carcinogenic effect of some risk factors, such as ultraviolet rays and some drugs, that seems to promote carcinogenesis through mechanisms independent of the immunosuppressive mechanism. These evidences indicate the need to prepare appropriate screening/surveillance models in these patients to prevent or at least anticipate the diagnosis of post-transplant tumors. In this context, even the correct eating habits can represent an optimal secondary prevention strategy in reducing the risks of transplant rejection due to non-immunological reasons and morbidity and mortality from post-transplant complications.
Footnotes
Conflict of interest: All the authors of the manuscript declare no conflict of interest in connection with this article.
References
- [1].Lechler RI, Sykes M, Thomson AW, Turka LA. Organ transplantation – how much of the promise has been realized? Nat Med. 2005;11(6):605–13. [DOI] [PubMed]; Lechler RI, Sykes M, Thomson AW, Turka LA. Organ transplantation – how much of the promise has been realized? Nat Med. 2005;11(6):605–13. doi: 10.1038/nm1251. [DOI] [PubMed] [Google Scholar]
- [2].Santangelo ML, Criscitiello C, Renda A, Federico S, Curigliano G, Dodaro C, et al. Immunosuppression and multiple primary malignancies in kidney-transplanted patients: a single-institute study. Biomed Res Int. 2015;2015:183523. 10.1155/2015/183523. [DOI] [PMC free article] [PubMed]; Santangelo ML, Criscitiello C, Renda A, Federico S, Curigliano G, Dodaro C. et al. Immunosuppression and multiple primary malignancies in kidney-transplanted patients: a single-institute study. Biomed Res Int. 2015;2015:183523. doi: 10.1155/2015/183523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–109. [DOI] [PubMed]; Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D. et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–109. doi: 10.1111/j.1600-6143.2011.03686.x. [DOI] [PubMed] [Google Scholar]
- [4].Davis CL, Delmonico FL. Living-donor kidney transplantation: a review of the current practices for the live donor. J Am Soc Nephrol. 2005;16(7):2098–110. [DOI] [PubMed]; Davis CL, Delmonico FL. Living-donor kidney transplantation: a review of the current practices for the live donor. J Am Soc Nephrol. 2005;16(7):2098–110. doi: 10.1681/ASN.2004100824. [DOI] [PubMed] [Google Scholar]
- [5].Calogero A, Sagnelli E, Creta M, Angeletti S, Peluso G, Incollingo P, et al. Eradication of HCV infection with the direct-acting antiviral therapy in renal allograft recipients. BioMed Res Int. 2019;2019:4674560. 10.1155/2019/4674560. Erratum to “Eradication of HCV infection with the direct-acting antiviral therapy in renal allograft recipients,” BioMed Res Int. 2019:8797329. doi: 10.1155/2019/8797329. [DOI] [PMC free article] [PubMed]; Calogero A, Sagnelli E, Creta M, Angeletti S, Peluso G, Incollingo P. et al. Eradication of HCV infection with the direct-acting antiviral therapy in renal allograft recipients. BioMed Res Int. 2019;2019:4674560. doi: 10.1155/2019/4674560. Erratum to “Eradication of HCV infection with the direct-acting antiviral therapy in renal allograft recipients,” BioMed Res Int. 2019:8797329, doi: 10.1155/2019/8797329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Coppola N, Pisaturo M, Guastafierro S, Tonziello G, Sica A, Sagnelli C, et al. Absence of occult hepatitis C virus infection in patients under immunosupressive therapy for oncohematological diseases. Hepatology. 2011;54(4):1487–9. [DOI] [PubMed]; Coppola N, Pisaturo M, Guastafierro S, Tonziello G, Sica A, Sagnelli C. et al. Absence of occult hepatitis C virus infection in patients under immunosupressive therapy for oncohematological diseases. Hepatology. 2011;54(4):1487–9. doi: 10.1002/hep.24436. [DOI] [PubMed] [Google Scholar]
- [7].Coppola N, Pisaturo M, Guastafierro S, Tonziello G, Sica A, Iodice V, et al. Increased hepatitis C viral load and reactivation of liver disease in HCV RNA-positive patients with onco-haematological disease undergoing chemotherapy. Dig Liv Dis. 2012;44(1):49–54. [DOI] [PubMed]; Coppola N, Pisaturo M, Guastafierro S, Tonziello G, Sica A, Iodice V. et al. Increased hepatitis C viral load and reactivation of liver disease in HCV RNA-positive patients with onco-haematological disease undergoing chemotherapy. Dig Liv Dis. 2012;44(1):49–54. doi: 10.1016/j.dld.2011.07.016. [DOI] [PubMed] [Google Scholar]
- [8].Ciccozzi M, Lai A, Zehender G, Borsetti A, Cella E, Ciotti M, et al. The phylogenetic approach for infectious disease evolution and epidemiology: an updating review. J Med Virol. 2019;91(10):1707–24. 10.1002/jmv.25526. [DOI] [PubMed]; Ciccozzi M, Lai A, Zehender G, Borsetti A, Cella E, Ciotti M. et al. The phylogenetic approach for infectious disease evolution and epidemiology: an updating review. J Med Virol. 2019;91(10):1707–24. doi: 10.1002/jmv.25526. [DOI] [PubMed] [Google Scholar]
- [9].Engels EA, Pfeiffer RM, Fraumeni JF, Kasiske BL, Israni AK, Snyder JJ, et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA. 2011;306(17):1891–901. [DOI] [PMC free article] [PubMed]; Engels EA, Pfeiffer RM, Fraumeni JF, Kasiske BL, Israni AK, Snyder JJ. et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA. 2011;306(17):1891–901. doi: 10.1001/jama.2011.1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Fernberg P, Edgren G, Adami J, Ingvar Å, Bellocco R, Tufveson G, et al. Time trends in risk and risk determinants of non-Hodgkin lymphoma in solid organ transplant recipients. Am J Transplant. 2011;11(11):2472–82. [DOI] [PubMed]; Fernberg P, Edgren G, Adami J, Ingvar Å, Bellocco R, Tufveson G. et al. Time trends in risk and risk determinants of non-Hodgkin lymphoma in solid organ transplant recipients. Am J Transplant. 2011;11(11):2472–82. doi: 10.1111/j.1600-6143.2011.03704.x. [DOI] [PubMed] [Google Scholar]
- [11].Creta M, Calogero A, Sagnelli C, Peluso G, Incollingo P, Candida M, et al. Donor and recipient outcomes following robotic-assisted laparoscopic living donor nephrectomy: a systematic review. Biomed Res Int. 2019;2019:1729138. 10.1155/2019/1729138. [DOI] [PMC free article] [PubMed]; Creta M, Calogero A, Sagnelli C, Peluso G, Incollingo P, Candida M. et al. Donor and recipient outcomes following robotic-assisted laparoscopic living donor nephrectomy: a systematic review. Biomed Res Int. 2019;2019:1729138. doi: 10.1155/2019/1729138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Viscardi G, Zanaletti N, Ferrara MG, Sica A, Falcone U, Guastafierro S, et al. Atypical haemolytic-uraemic syndrome in patient with metastatic colorectal cancer treated with fluorouracil and oxaliplatin: a case report and a review of literature. ESMO Open. 2019;4(5):e000551. 10.1136/esmoopen-2019-000551. [DOI] [PMC free article] [PubMed]; Viscardi G, Zanaletti N, Ferrara MG, Sica A, Falcone U, Guastafierro S. et al. Atypical haemolytic-uraemic syndrome in patient with metastatic colorectal cancer treated with fluorouracil and oxaliplatin: a case report and a review of literature. ESMO Open. 2019;4(5):e000551. doi: 10.1136/esmoopen-2019-000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Fishman JA, Rubin RH. Infection in organ-transplant recipients. New England J Med. 1998;338(24):1741–51. [DOI] [PubMed]; Fishman JA, Rubin RH. Infection in organ-transplant recipients. New England J Med. 1998;338(24):1741–51. doi: 10.1056/NEJM199806113382407. [DOI] [PubMed] [Google Scholar]
- [14].Langella C, Naviglio D, Marino M, Calogero A, Gallo M. New food approaches to reduce and/or eliminate increased gastric acidity related to gastroesophageal pathologies. Nutrition. 2018;54:26–32. [DOI] [PubMed]; Langella C, Naviglio D, Marino M, Calogero A, Gallo M. New food approaches to reduce and/or eliminate increased gastric acidity related to gastroesophageal pathologies. Nutrition. 2018;54:26–32. doi: 10.1016/j.nut.2018.03.002. [DOI] [PubMed] [Google Scholar]
- [15].Yolken RH, Bishop CA, Townsend TR, Bolyard EA, Bartlett J, Santos GW, et al. Infectious gastroenteritis in bone-marrow-transplant recipients. New England J Med. 1982;306(17):1009–12. [DOI] [PubMed]; Yolken RH, Bishop CA, Townsend TR, Bolyard EA, Bartlett J, Santos GW. et al. Infectious gastroenteritis in bone-marrow-transplant recipients. New England J Med. 1982;306(17):1009–12. doi: 10.1056/NEJM198204293061701. [DOI] [PubMed] [Google Scholar]
- [16].Dryden MS, Shanson DC. The microbial causes of diarrhoea in patients infected with the human immunodeficiency virus. J Infect. 1988;17(2):107–14. [DOI] [PubMed]; Dryden MS, Shanson DC. The microbial causes of diarrhoea in patients infected with the human immunodeficiency virus. J Infect. 1988;17(2):107–14. doi: 10.1016/s0163-4453(88)91515-0. [DOI] [PubMed] [Google Scholar]
- [17].Simon D, Brandt LJ. Diarrhea in patients with the acquired immunodeficiency syndrome. Gastroenterology. 1993;105(4):1238–42. [DOI] [PubMed]; Simon D, Brandt LJ. Diarrhea in patients with the acquired immunodeficiency syndrome. Gastroenterology. 1993;105(4):1238–42. doi: 10.1016/0016-5085(93)90972-f. [DOI] [PubMed] [Google Scholar]
- [18].Sica A, Vitiello P, Papa A, Sagnelli C, Calogero A, Casale D, et al. Use of rituximab in NHL Malt type pregnant in I° trimester for two times. Open Med (Wars). 2019;14:757–60. 10.1515/med-2019-0087. [DOI] [PMC free article] [PubMed]; Sica A, Vitiello P, Papa A, Sagnelli C, Calogero A, Casale D. et al. Use of rituximab in NHL Malt type pregnant in I° trimester for two times. Open Med (Wars) 2019;14:757–60. doi: 10.1515/med-2019-0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Zaia JA. Infections in organ transplant recipients. Clinical Virology. Churchill Livingston, on CD ROM, 2009.; Zaia JA. Infections in organ transplant recipients. Clinical Virology. 2009. . Churchill Livingston, on CD ROM,
- [20].Sagnelli C, Pisaturo M, Calò F, Martini S, Sagnelli E. Reactivation of HBV infection in patients with hemo-lymphoproliferative diseases, and its prevention C. World J Gastroenterol. 2019;25(26):3299–312. [DOI] [PMC free article] [PubMed]; Sagnelli C, Pisaturo M, Calò F, Martini S, Sagnelli E. Reactivation of HBV infection in patients with hemo-lymphoproliferative diseases, and its prevention C. World J Gastroenterol. 2019;25(26):3299–312. doi: 10.3748/wjg.v25.i26.3299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Sagnelli C, Sagnelli E. Towards the worldwide eradication of HBV infection; a combination of prophylactic and therapeutic factors. World J Clin Infect Dis. 2019;9(2):11–22. 10.5495/wjcid.v9.i2.11 [DOI]; Sagnelli C, Sagnelli E. Towards the worldwide eradication of HBV infection; a combination of prophylactic and therapeutic factors. World J Clin Infect Dis. 2019;9(2):11–22. doi: 10.5495/wjcid.v9.i2.11. [DOI] [Google Scholar]
- [22].Rubin RH. Gastrointestinal infectious disease complications following transplantation and their differentiation from immunosuppressant-induced gastrointestinal toxicities. Clin Transplant. 2001;15(S4):11–22. [DOI] [PubMed]; Rubin RH. Gastrointestinal infectious disease complications following transplantation and their differentiation from immunosuppressant-induced gastrointestinal toxicities. Clin Transplant. 2001;15(S4):11–22. doi: 10.1111/j.1399-0012.2001.00011.x. [DOI] [PubMed] [Google Scholar]
- [23].Logan AJ, Morris-Stiff GJ, Bowrey DJ, Jurewicz WA. Upper gastrointestinal complications after renal transplantation: a 3-year sequential study. Clin Transplant. 2002;16(3):163–7. [DOI] [PubMed]; Logan AJ, Morris-Stiff GJ, Bowrey DJ, Jurewicz WA. Upper gastrointestinal complications after renal transplantation: a 3-year sequential study. Clin Transplant. 2002;16(3):163–7. doi: 10.1034/j.1399-0012.2002.01012.x. [DOI] [PubMed] [Google Scholar]
- [24].Budiño BS, Martul EV, Díaz SP, Barreiro AV, Rey EC, Reboredo JM. Autopsy-determined causes of death in solid organ transplant recipients. Transplant Proc. 2004;36(3):787–9. [DOI] [PubMed]; Budiño BS, Martul EV, Díaz SP, Barreiro AV, Rey EC, Reboredo JM. Autopsy-determined causes of death in solid organ transplant recipients. Transplant Proc. 2004;36(3):787–9. doi: 10.1016/j.transproceed.2004.03.044. [DOI] [PubMed] [Google Scholar]
- [25].Thom K, Forrest G. Gastrointestinal infections in immunocompromised hosts. Curr Opin Gastroenterol. 2006;22(1):18–23. [DOI] [PubMed]; Thom K, Forrest G. Gastrointestinal infections in immunocompromised hosts. Curr Opin Gastroenterol. 2006;22(1):18–23. doi: 10.1097/01.mog.0000196149.29077.0d. [DOI] [PubMed] [Google Scholar]
- [26].McDonald GB, Sharma P, Hackman RC, Meyers JD, Thomas ED. Esophageal infections in immunosuppressed patients after marrow transplantation. Gastroenterology. 1985;88(5):1111–7. [DOI] [PubMed]; McDonald GB, Sharma P, Hackman RC, Meyers JD, Thomas ED. Esophageal infections in immunosuppressed patients after marrow transplantation. Gastroenterology. 1985;88(5):1111–7. doi: 10.1016/s0016-5085(85)80068-8. [DOI] [PubMed] [Google Scholar]
- [27].Ponticelli C, Passerini P. Gastrointestinal complications in renal transplant recipients. Transplant Int. 2005;18(6):643–50. [DOI] [PubMed]; Ponticelli C, Passerini P. Gastrointestinal complications in renal transplant recipients. Transplant Int. 2005;18(6):643–50. doi: 10.1111/j.1432-2277.2005.00134.x. [DOI] [PubMed] [Google Scholar]
- [28].Graham SM, Flowers JL, Schweitzer E, Bartlett ST, Imbembo AL. Opportunistic upper gastrointestinal infection in transplant recipients. Surg Endosc. 1995;9(2):146–50. [DOI] [PubMed]; Graham SM, Flowers JL, Schweitzer E, Bartlett ST, Imbembo AL. Opportunistic upper gastrointestinal infection in transplant recipients. Surg Endosc. 1995;9(2):146–50. doi: 10.1007/BF00191955. [DOI] [PubMed] [Google Scholar]
- [29].Sagnelli C, Fumagalli L, Prigitano A, Baccari P, Magnani P, Lazzarin A. Successful voriconazole therapy of disseminated Fusarium verticillioides infection in an immunocompromised patient receiving chemotherapy. J Antimicrob Chemother. 2006;57(4):796–8. [DOI] [PubMed]; Sagnelli C, Fumagalli L, Prigitano A, Baccari P, Magnani P, Lazzarin A. Successful voriconazole therapy of disseminated Fusarium verticillioides infection in an immunocompromised patient receiving chemotherapy. J Antimicrob Chemother. 2006;57(4):796–8. doi: 10.1093/jac/dkl016. [DOI] [PubMed] [Google Scholar]
- [30].Smyth RL, Higenbottam TW, Scott JP, Wreghitt TG, Stewart S, Clelland CA, et al. Herpes simplex virus infection in heart–lung transplant recipients. Transplantation. 1990;49(4):735–9. [DOI] [PubMed]; Smyth RL, Higenbottam TW, Scott JP, Wreghitt TG, Stewart S, Clelland CA. et al. Herpes simplex virus infection in heart–lung transplant recipients. Transplantation. 1990;49(4):735–9. doi: 10.1097/00007890-199004000-00016. [DOI] [PubMed] [Google Scholar]
- [31].Washington K, Gottfried MR, Wilson ML. Gastrointestinal cryptococcosis. Modern Pathol. 1991;4(6):707–11. [PubMed]; Washington K, Gottfried MR, Wilson ML. Gastrointestinal cryptococcosis. Modern Pathol. 1991;4(6):707–11. [PubMed] [Google Scholar]
- [32].Walsh TJ, Belitsos NJ, Hamilton SR. Bacterial esophagitis in immunocompromised patients. Arch Intern Med. 1986;146(7):1345–8. [PubMed]; Walsh TJ, Belitsos NJ, Hamilton SR. Bacterial esophagitis in immunocompromised patients. Arch Intern Med. 1986;146(7):1345–8. [PubMed] [Google Scholar]
- [33].Farrell JJ, Cosimi AB, Chung RT. Idiopathic giant esophageal ulcers in a renal transplant patient responsive to steroid therapy. Transplantationc. 2000;70(1):230–2. [PubMed]; Farrell JJ, Cosimi AB, Chung RT. Idiopathic giant esophageal ulcers in a renal transplant patient responsive to steroid therapy. Transplantationc. 2000;70(1):230–2. [PubMed] [Google Scholar]
- [34].Agha FP, Lee HH, Nostrant TT. Herpetic esophagitis: a diagnostic challenge in immunocompromised patients. Am J Gastroenterol. 1986;81(4):246–52. [PubMed]; Agha FP, Lee HH, Nostrant TT. Herpetic esophagitis: a diagnostic challenge in immunocompromised patients. Am J Gastroenterol. 1986;81(4):246–52. [PubMed] [Google Scholar]
- [35].McBane RD, Gross JB. Herpes esophagitis: clinical syndrome, endoscopic appearance, and diagnosis in 23 patients. Gastroint Endosc. 1991;37(6):600–3. [DOI] [PubMed]; McBane RD, Gross JB. Herpes esophagitis: clinical syndrome, endoscopic appearance, and diagnosis in 23 patients. Gastroint Endosc. 1991;37(6):600–3. doi: 10.1016/s0016-5107(91)70862-6. [DOI] [PubMed] [Google Scholar]
- [36].Patterson JE. Epidemiology of fungal infections in solid organ transplant patients. Transplant Infect Dis. 1999;1(4):229–36. [DOI] [PubMed]; Patterson JE. Epidemiology of fungal infections in solid organ transplant patients. Transplant Infect Dis. 1999;1(4):229–36. doi: 10.1034/j.1399-3062.1999.010402.x. [DOI] [PubMed] [Google Scholar]
- [37].Odds FC. Candida and candidosis: a review and bibliography. London, UK: Bailliere Tindall; 1988.; Odds FC. Candida and candidosis: a review and bibliography. London, UK: Bailliere Tindall; 1988. [Google Scholar]
- [38].López-Dupla M, Mora Sanz P, Pintado García V, Ortega EV, Uriol PL, Khamashta MA, et al. Clinical, endoscopic, immunologic, and therapeutic aspects of oropharyngeal and esophageal candidiasis in HIV-infected patients: a survey of 114 cases. Am J Gastroenterol. 1992;87(12):1771–6. [PubMed]; López-Dupla M, Mora Sanz P, Pintado García V, Ortega EV, Uriol PL, Khamashta MA. et al. Clinical, endoscopic, immunologic, and therapeutic aspects of oropharyngeal and esophageal candidiasis in HIV-infected patients: a survey of 114 cases. Am J Gastroenterol. 1992;87(12):1771–6. [PubMed] [Google Scholar]
- [39].Helderman JH, Goral S. Gastrointestinal complications of transplant immunosuppression. J Am Soc Nephrol. 2002;13(1):277–87. [DOI] [PubMed]; Helderman JH, Goral S. Gastrointestinal complications of transplant immunosuppression. J Am Soc Nephrol. 2002;13(1):277–87. doi: 10.1681/ASN.V131277. [DOI] [PubMed] [Google Scholar]
- [40].Teenan RP, Burgoyne M, Brown IL, Murray WR. Helicobacter pylori in renal transplant recipients. Transplantation. 1993;56(1):100–3. [DOI] [PubMed]; Teenan RP, Burgoyne M, Brown IL, Murray WR. Helicobacter pylori in renal transplant recipients. Transplantation. 1993;56(1):100–3. doi: 10.1097/00007890-199307000-00018. [DOI] [PubMed] [Google Scholar]
- [41].Ozgür O, Boyacioğlu S, Ozdoğan M, Gür G, Telatar H, Haberal M. Helicobacter pylori infection in haemodialysis patients and renal transplant recipients. Nephrol Dial Transplant. 1997;12(2):289–91. [DOI] [PubMed]; Ozgür O, Boyacioğlu S, Ozdoğan M, Gür G, Telatar H, Haberal M. Helicobacter pylori infection in haemodialysis patients and renal transplant recipients. Nephrol Dial Transplant. 1997;12(2):289–91. doi: 10.1093/ndt/12.2.289. [DOI] [PubMed] [Google Scholar]
- [42].Buommino E, D’Abrosca B, Donnarumma G, Parisi A, Scognamiglio M, Fiorentino A, et al. Evaluation of the antioxidant properties of carexanes in AGS cells transfected with the Helicobacter pylori’s protein HspB. Microb Pathog. 2017;108:71–7. 10.1016/j.micpath.2017.05.007. [DOI] [PubMed]; Buommino E, D’Abrosca B, Donnarumma G, Parisi A, Scognamiglio M, Fiorentino A. et al. Evaluation of the antioxidant properties of carexanes in AGS cells transfected with the Helicobacter pylori’s protein HspB. Microb Pathog. 2017;108:71–7. doi: 10.1016/j.micpath.2017.05.007. [DOI] [PubMed] [Google Scholar]
- [43].De Falco M, Lucariello A, Iaquinto S, Esposito V, Guerra G, De Luca A. Molecular mechanisms of Helicobacter pylori pathogenesis. J Cell Physiol. 2015;230(8):1702–07. [DOI] [PubMed]; De Falco M, Lucariello A, Iaquinto S, Esposito V, Guerra G, De Luca A. Molecular mechanisms of Helicobacter pylori pathogenesis. J Cell Physiol. 2015;230(8):1702–07. doi: 10.1002/jcp.24933. [DOI] [PubMed] [Google Scholar]
- [44].Coppola N, De Stefano G, Marrocco C, Scarano F, Scolastico C, Tarantino L, et al. Helicobacter spp. and liver diseases. Infez Med. 2003;11(4):201–7. [PubMed]; Coppola N, De Stefano G, Marrocco C, Scarano F, Scolastico C, Tarantino L. et al. Helicobacter spp. and liver diseases. Infez Med. 2003;11(4):201–7. [PubMed] [Google Scholar]
- [45].De Luca A, De Falco M, Manente L, Dattilo D, Lucariello A, Esposito V, et al. Helicobacter pylori heat shock protein B (HspB) localizes in vivo in the gastric mucosa and MALT lymphoma. J Cell Physiol. 2008;216:78–82. [DOI] [PubMed]; De Luca A, De Falco M, Manente L, Dattilo D, Lucariello A, Esposito V. et al. Helicobacter pylori heat shock protein B (HspB) localizes in vivo in the gastric mucosa and MALT lymphoma. J Cell Physiol. 2008;216:78–82. doi: 10.1002/jcp.21376. [DOI] [PubMed] [Google Scholar]
- [46].Manente L, Perna A, Buommino E, Altucci L, Lucariello A, Citro G, et al. The Helicobacter pylori’s protein VacA has direct effects on the regulation of cell cycle and apoptosis in gastric epithelial cells. J Cell Physiol. 2008;214:582–7. [DOI] [PubMed]; Manente L, Perna A, Buommino E, Altucci L, Lucariello A, Citro G. et al. The Helicobacter pylori’s protein VacA has direct effects on the regulation of cell cycle and apoptosis in gastric epithelial cells. J Cell Physiol. 2008;214:582–7. doi: 10.1002/jcp.21242. [DOI] [PubMed] [Google Scholar]
- [47].Buommino E, Donnarumma G, Manente L, De Filippis A, Francesco Silvestri F, Iaquinto S, et al. The Helicobacter pylori protein HspB interferes with Nrf2/Keap-1 pathway altering the antioxidant response of AGS cells. Helicobacter. 2012;17:417–25. [DOI] [PubMed]; Buommino E, Donnarumma G, Manente L, De Filippis A, Francesco Silvestri F, Iaquinto S. et al. The Helicobacter pylori protein HspB interferes with Nrf2/Keap-1 pathway altering the antioxidant response of AGS cells. Helicobacter. 2012;17:417–25. doi: 10.1111/j.1523-5378.2012.00973.x. [DOI] [PubMed] [Google Scholar]
- [48].Chatterjee SN, Fiala M, Weiner J, Stewart JA, Stacey B, Warner N. Primary cytomegalovirus and opportunistic infections. JAMA. 1978;240(22):2446. [PubMed]; Chatterjee SN, Fiala M, Weiner J, Stewart JA, Stacey B, Warner N. Primary cytomegalovirus and opportunistic infections. JAMA. 1978;240(22):2446. [PubMed] [Google Scholar]
- [49].Lautenschlager I. Cytomegalovirus and solid organ transplantation: an update. Curr Opin Org Transplant. 2003;8(4):269–75.; Lautenschlager I. Cytomegalovirus and solid organ transplantation: an update. Curr Opin Org Transplant. 2003;8(4):269–75. [Google Scholar]
- [50].Péter A, Telkes G, Varga M, Sárváry E, Kovalszky I. Endoscopic diagnosis of cytomegalovirus infection of upper gastrointestinal tract in solid organ transplant recipients: Hungarian single-center experience. Clin Transplant. 2004;18(5):580–4. [DOI] [PubMed]; Péter A, Telkes G, Varga M, Sárváry E, Kovalszky I. Endoscopic diagnosis of cytomegalovirus infection of upper gastrointestinal tract in solid organ transplant recipients: Hungarian singlecenter experience. Clin Transplant. 2004;18(5):580–4. doi: 10.1111/j.1399-0012.2004.00230.x. [DOI] [PubMed] [Google Scholar]
- [51].Lowance D, Neumayer HH, Legendre CM, Squifflet JP, Kovarik J, Brennan PJ, et al. Valacyclovir for the prevention of cytomegalovirus disease after renal transplantation. N Engl J Med. 1999;340(19):1462–70. [DOI] [PubMed]; Lowance D, Neumayer HH, Legendre CM, Squifflet JP, Kovarik J, Brennan PJ. et al. Valacyclovir for the prevention of cytomegalovirus disease after renal transplantation. N Engl J Med. 1999;340(19):1462–70. doi: 10.1056/NEJM199905133401903. [DOI] [PubMed] [Google Scholar]
- [52].Foucar E, Mukai K, Foucar K, Sutherland DE, Van Buren CT. Colon ulceration in lethal cytomegalovirus infection. Am J Clin Pathol. 1981;76(6):788–801. [DOI] [PubMed]; Foucar E, Mukai K, Foucar K, Sutherland DE, Van Buren CT. Colon ulceration in lethal cytomegalovirus infection. Am J Clin Pathol. 1981;76(6):788–801. doi: 10.1093/ajcp/76.6.788. [DOI] [PubMed] [Google Scholar]
- [53].Dee SL, Butt K, Ramaswamy G. Intestinal ischemia: a significant early postoperative complication after renal transplantation. Arch Pathol Lab Med. 2002;126(10):1201–04. [DOI] [PubMed]; Dee SL, Butt K, Ramaswamy G. Intestinal ischemia: a significant early postoperative complication after renal transplantation. Arch Pathol Lab Med. 2002;126(10):1201–04. doi: 10.5858/2002-126-1201-II. [DOI] [PubMed] [Google Scholar]
- [54].Boobes Y, Al Hakim M, Dastoor H, Bernieh B, Abdulkhalik S. Late cytomegalovirus disease with atypical presentation in renal transplant patients. Transplant Proc. 2004;36(6):1841–3. [DOI] [PubMed]; Boobes Y, Al Hakim M, Dastoor H, Bernieh B, Abdulkhalik S. Late cytomegalovirus disease with atypical presentation in renal transplant patients. Transplant Proc. 2004;36(6):1841–3. doi: 10.1016/j.transproceed.2004.07.017. [DOI] [PubMed] [Google Scholar]
- [55].Shapiro AM, Bain VG, Preiksaitis JK, Ma MM, Issa S, Kneteman NM. Ogilvie’s syndrome associated with acute cytomegaloviral infection after liver transplantation. Transplant Int. 2000;13(1):41–5. [DOI] [PubMed]; Shapiro AM, Bain VG, Preiksaitis JK, Ma MM, Issa S, Kneteman NM. Ogilvie’s syndrome associated with acute cytomegaloviral infection after liver transplantation. Transplant Int. 2000;13(1):41–5. doi: 10.1007/s001470050006. [DOI] [PubMed] [Google Scholar]
- [56].Rotterdam H, Tsang P. Gastrointestinal disease in the immunocompromised patient. Hum Pathol. 1994;25(11):1123–40. [DOI] [PubMed]; Rotterdam H, Tsang P. Gastrointestinal disease in the immunocompromised patient. Hum Pathol. 1994;25(11):1123–40. doi: 10.1016/0046-8177(94)90029-9. [DOI] [PubMed] [Google Scholar]
- [57].Peigue-Lafeuille H, Henquell C, Chambon M, Gazuy N, De Champs C, Cluzel R. Nosocomial rotavirus infections in adult renal transplant recipients. J Hospital Infect. 1991;18(1):67–70. [DOI] [PubMed]; Peigue-Lafeuille H, Henquell C, Chambon M, Gazuy N, De Champs C, Cluzel R. Nosocomial rotavirus infections in adult renal transplant recipients. J Hospital Infect. 1991;18(1):67–70. doi: 10.1016/0195-6701(91)90095-p. [DOI] [PubMed] [Google Scholar]
- [58].Kaufman SS, Chatterjee NK, Fuschino ME, Magid MS, Gordon RE, Morse DL, et al. Calicivirus enteritis in an intestinal transplant recipient. Am J Transplant. 2003;3(6):764–8. [DOI] [PubMed]; Kaufman SS, Chatterjee NK, Fuschino ME, Magid MS, Gordon RE, Morse DL. et al. Calicivirus enteritis in an intestinal transplant recipient. Am J Transplant. 2003;3(6):764–8. doi: 10.1034/j.1600-6143.2003.00112.x. [DOI] [PubMed] [Google Scholar]
- [59].Altıparmak MR, Trablus S, Pamuk ÖN, Apaydın S, Sarıyar M, Öztürk R, et al. Diarrhoea following renal transplantation. Clin Transplant. 2002;16(3):212–6. [DOI] [PubMed]; Altıparmak MR, Trablus S, Pamuk ÖN, Apaydın S, Sarıyar M, Öztürk R. et al. Diarrhoea following renal transplantation. Clin Transplant. 2002;16(3):212–6. doi: 10.1034/j.1399-0012.2002.01129.x. [DOI] [PubMed] [Google Scholar]
- [60].Chang HR, Lian JD, Chan CH, Wong LC. Cytomegalovirus ischemic colitis of a diabetic renal transplant recipient. Clin Transplant. 2004;18(1):100–4. [DOI] [PubMed]; Chang HR, Lian JD, Chan CH, Wong LC. Cytomegalovirus ischemic colitis of a diabetic renal transplant recipient. Clin Transplant. 2004;18(1):100–4. doi: 10.1046/j.0902-0063.2003.00108.x. [DOI] [PubMed] [Google Scholar]
- [61].Pirsch JD, Miller J, Deierhoi MH, Vincenti F, Filo RS. A comparison of tacrolimus (fk506) and cyclosporine for immunosuppression after cadaveric renal transplantation 1. Transplantation. 1997;63(7):977–83. [DOI] [PubMed]; Pirsch JD, Miller J, Deierhoi MH, Vincenti F, Filo RS. A comparison of tacrolimus (fk506) and cyclosporine for immunosuppression after cadaveric renal transplantation 1. Transplantation. 1997;63(7):977–83. doi: 10.1097/00007890-199704150-00013. [DOI] [PubMed] [Google Scholar]
- [62].Mayer AD, Dmitrewski J, Squifflet JP, Besse T, Grabensee B, Klein B, et al. Multicenter randomized trial comparing Tacrolimus (FK506) and Cyclosporine in the prevention of renal allograft rejection1: a report of the European Tacrolimus multicenter renal study group. Transplantation. 1997;64(3):436–43. [DOI] [PubMed]; Mayer AD, Dmitrewski J, Squifflet JP, Besse T, Grabensee B, Klein B. et al. Multicenter randomized trial comparing Tacrolimus (FK506) and Cyclosporine in the prevention of renal allograft rejection1: a report of the European Tacrolimus multicenter renal study group. Transplantation. 1997;64(3):436–43. doi: 10.1097/00007890-199708150-00012. [DOI] [PubMed] [Google Scholar]
- [63].Maes BD, Lemahieu W, Kuypers D, Evenepoel P, Coosemansc W, Pirenne J, et al. Differential effect of diarrhea on FK506 versus cyclosporine A trough levels and resultant prevention of allograft rejection in renal transplant recipients. Am J Transplant. 2002;2(10):989–92. [DOI] [PubMed]; Maes BD, Lemahieu W, Kuypers D, Evenepoel P, Coosemansc W, Pirenne J. et al. Differential effect of diarrhea on FK506 versus cyclosporine A trough levels and resultant prevention of allograft rejection in renal transplant recipients. Am J Transplant. 2002;2(10):989–92. doi: 10.1034/j.1600-6143.2002.21018.x. [DOI] [PubMed] [Google Scholar]
- [64].Parnaby CN, Barrow EJ, Edirimanne SB, Parrott NR, Frizelle FA, Watson AJM. Colorectal complications of end-tage renal failure and renal transplantation: a review. Colorectal Dis. 2012;14(4):403–15. [DOI] [PubMed]; Parnaby CN, Barrow EJ, Edirimanne SB, Parrott NR, Frizelle FA, Watson AJM. Colorectal complications of end-tage renal failure and renal transplantation: a review. Colorectal Dis. 2012;14(4):403–15. doi: 10.1111/j.1463-1318.2010.02491.x. [DOI] [PubMed] [Google Scholar]
- [65].Lederman ED, Conti DJ, Lempert N, Singh TP, Lee EC. Complicated diverticulitis following renal transplantation. Dis Colon Rect. 1998;41(5):613–8. [DOI] [PubMed]; Lederman ED, Conti DJ, Lempert N, Singh TP, Lee EC. Complicated diverticulitis following renal transplantation. Dis Colon Rect. 1998;41(5):613–8. doi: 10.1007/BF02235270. [DOI] [PubMed] [Google Scholar]
- [66].Andreoni KA, Pelletier RP, Elkhammas EA, Davies EA, Bumgardner GL, Henry ML, et al. Increased incidence of gastrointestinal surgical complications in renal transplant recipients with polycystic kidney disease 1. Transplantation. 1999;67(2):262–6. [DOI] [PubMed]; Andreoni KA, Pelletier RP, Elkhammas EA, Davies EA, Bumgardner GL, Henry ML. et al. Increased incidence of gastrointestinal surgical complications in renal transplant recipients with polycystic kidney disease 1. Transplantation. 1999;67(2):262–6. doi: 10.1097/00007890-199901270-00013. [DOI] [PubMed] [Google Scholar]
- [67].Fernandez ED, Albrecht KH, Heemann U, Kohnle M, Erhard J, Stöblen F, et al. Prevalence of diverticulosis and incidence of bowel perforation after kidney transplantation in patients with polycystic kidney disease. Transplant Int. 1998;11(1):28–31. [DOI] [PubMed]; Fernandez ED, Albrecht KH, Heemann U, Kohnle M, Erhard J, Stöblen F. et al. Prevalence of diverticulosis and incidence of bowel perforation after kidney transplantation in patients with polycystic kidney disease. Transplant Int. 1998;11(1):28–31. doi: 10.1007/s001470050098. [DOI] [PubMed] [Google Scholar]
- [68].Carlomagno N, Duraturo F, Candida M, De Rosa M, Varone V, Ciancia G, et al. Multiple splenic hamartomas and familial adenomatous polyposis: a case report and review of the literature. J Med Case Rep. 2015;9:154. 10.1186/s13256-015-0627-3. [DOI] [PMC free article] [PubMed]; Carlomagno N, Duraturo F, Candida M, De Rosa M, Varone V, Ciancia G. et al. Multiple splenic hamartomas and familial adenomatous polyposis: a case report and review of the literature. J Med Case Rep. 2015;9:154. doi: 10.1186/s13256-015-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Grifasi C, Calogero A, Esposito A, Dodaro C. Perioperative care of elderly outpatient: a review. Ann Ital Chir. 2014;85(ePub):S2239253X14022403. [PubMed]; Grifasi C, Calogero A, Esposito A, Dodaro C. Perioperative care of elderly outpatient: a review. Ann Ital Chir. 2014;85 ePub: S2239253X14022403. [PubMed] [Google Scholar]
- [70].Carlomagno N, Santangelo ML, Mastromarino R, Calogero A, Dodaro C, Renda A. Rare multiple primary malignancies among surgical patients – a single surgical unit experience. Ecancermedicalscience. 2014;8:438. 10.3332/ecancer.2014.438. [DOI] [PMC free article] [PubMed]; Carlomagno N, Santangelo ML, Mastromarino R, Calogero A, Dodaro C, Renda A. Rare multiple primary malignancies among surgical patients – a single surgical unit experience. Ecancermedicalscience. 2014;8:438. doi: 10.3332/ecancer.2014.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Calogero A, Sagnelli C, Carlomagno N, Tammaro V, Candida M, Vernillo A, et al. Familial polyposis coli: the management of desmoid tumor bleeding. Open Med (Wars). 2019;14:572–6. 10.1515/med-2019-0064. [DOI] [PMC free article] [PubMed]; Calogero A, Sagnelli C, Carlomagno N, Tammaro V, Candida M, Vernillo A. et al. Familial polyposis coli: the management of desmoid tumor bleeding. Open Med (Wars) 2019;14:572–6. doi: 10.1515/med-2019-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Dodaro CA, Calogero A, Tammaro V, Pellegrino T, Lionetti R, Campanile S, et al. Colorectal cancer in the elderly patient: the role of neo-adjuvant therapy. Open Med (Wars). 2019;14:607–12. 10.1515/med-2019-0068. [DOI] [PMC free article] [PubMed]; Dodaro CA, Calogero A, Tammaro V, Pellegrino T, Lionetti R, Campanile S. et al. Colorectal cancer in the elderly patient: the role of neo-adjuvant therapy. Open Med (Wars) 2019;14:607–12. doi: 10.1515/med-2019-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Carlomagno N, Santangelo ML, Amato B, Calogero A, Saracco M, Cremone C, et al. Total colectomy for cancer: analysis of factors linked to patients’ age. Int J Surg. 2014;12(Suppl 2):S135–S139. 10.1016/j.ijsu.2014.08.363. [DOI] [PubMed]; Carlomagno N, Santangelo ML, Amato B, Calogero A, Saracco M, Cremone C. et al. Total colectomy for cancer: analysis of factors linked to patients’ age. Int J Surg. 2014;12(Suppl 2):S135–S139. doi: 10.1016/j.ijsu.2014.08.363. [DOI] [PubMed] [Google Scholar]
- [74].Merli M, Frigeni M, Alric L, Visco C, Besson C, Mannelli L, et al. Direct-acting antivirals in hepatitis C virus-associated diffuse large B-cell lymphomas. Oncologist. 2019;24(8):e720–e729. 10.1634/theoncologist.2018-0331. [DOI] [PMC free article] [PubMed]; Merli M, Frigeni M, Alric L, Visco C, Besson C, Mannelli L. et al. Direct-acting antivirals in hepatitis C virus-associated diffuse large B-cell lymphomas. Oncologist. 2019;24(8):e720–e729. doi: 10.1634/theoncologist.2018-0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Tonziello G, Pisaturo M, Sica A, Ferrara MG, Sagnelli C, Pasquale G, et al. Transient reactivation of occult hepatitis B virus infection despite lamivudine prophylaxis in a patient treated for non-Hodgkin lymphoma. Infection. 2013;41(1):225–9. 10.1007/s15010-012-0305-y. [DOI] [PubMed]; Tonziello G, Pisaturo M, Sica A, Ferrara MG, Sagnelli C, Pasquale G. et al. Transient reactivation of occult hepatitis B virus infection despite lamivudine prophylaxis in a patient treated for non-Hodgkin lymphoma. Infection. 2013;41(1):225–9. doi: 10.1007/s15010-012-0305-y. [DOI] [PubMed] [Google Scholar]
- [76].Peluso G, Incollingo P, Calogero A, Tammaro V, Rupealta N, Chiacchio G, et al. Current tissue molecular markers in colorectal cancer: a literature review. Biomed Res Int. 2017;2017:2605628. 10.1155/2017/2605628. [DOI] [PMC free article] [PubMed]; Peluso G, Incollingo P, Calogero A, Tammaro V, Rupealta N, Chiacchio G. et al. Current tissue molecular markers in colorectal cancer: a literature review. Biomed Res Int. 2017;2017:2605628. doi: 10.1155/2017/2605628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Nardelli C, Iaffaldano L, Pilone V, Labruna G, Ferrigno M, Carlomagno N, et al. Changes in the microRNA profile observed in the subcutaneous adipose tissue of obese patients after laparoscopic adjustable gastric banding. J Obes. 2017;2017:6754734. 10.1155/2017/6754734. [DOI] [PMC free article] [PubMed]; Nardelli C, Iaffaldano L, Pilone V, Labruna G, Ferrigno M, Carlomagno N. et al. Changes in the microRNA profile observed in the subcutaneous adipose tissue of obese patients after laparoscopic adjustable gastric banding. J Obes. 2017;2017:6754734. doi: 10.1155/2017/6754734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Sciuto A, Merola G, De Palma GD, Sodo M, Pirozzi F, Bracale UM, et al. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol. 2018;24(21):2247–2260. 10.3748/wjg.v24.i21.2247. [DOI] [PMC free article] [PubMed]; Sciuto A, Merola G, De Palma GD, Sodo M, Pirozzi F, Bracale UM. et al. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol. 2018;24(21):2247–2260. doi: 10.3748/wjg.v24.i21.2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Hall EC, Pfeiffer RM, Segev DL, Engels EA. Cumulative incidence of cancer after solid organ transplantation. Cancer. 2013;119(12):2300–8. [DOI] [PMC free article] [PubMed]; Hall EC, Pfeiffer RM, Segev DL, Engels EA. Cumulative incidence of cancer after solid organ transplantation. Cancer. 2013;119(12):2300–8. doi: 10.1002/cncr.28043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Danpanich E, Kasiske BL. Risk factors for cancer in renal transplant recipients 1. Transplantation. 1999;68(12):1859–64. [DOI] [PubMed]; Danpanich E, Kasiske BL. Risk factors for cancer in renal transplant recipients 1. Transplantation. 1999;68(12):1859–64. doi: 10.1097/00007890-199912270-00008. [DOI] [PubMed] [Google Scholar]
- [81].Vera A, Gunson BK, Ussatoff V, Nightingale P, Candinas D, Radley S, et al. Colorectal cancer in patients with inflammatory bowel disease after liver transplantation for primary sclerosing cholangitis. Transplantation. 2003;75(12):1983–8. [DOI] [PubMed]; Vera A, Gunson BK, Ussatoff V, Nightingale P, Candinas D, Radley S. et al. Colorectal cancer in patients with inflammatory bowel disease after liver transplantation for primary sclerosing cholangitis. Transplantation. 2003;75(12):1983–8. doi: 10.1097/01.TP.0000058744.34965.38. [DOI] [PubMed] [Google Scholar]
- [82].Montalbano M, Neff GW, Yamashiki N, Meyer D, Bettiol M, Slapak-Green G, et al. A retrospective review of liver transplant patients treated with sirolimus from a single center: an analysis of sirolimus-related complications. Transplantation. 2004;78(2):264–8. [DOI] [PubMed]; Montalbano M, Neff GW, Yamashiki N, Meyer D, Bettiol M, Slapak-Green G. et al. A retrospective review of liver transplant patients treated with sirolimus from a single center: an analysis of sirolimus-related complications. Transplantation. 2004;78(2):264–8. doi: 10.1097/01.tp.0000128628.31556.b1. [DOI] [PubMed] [Google Scholar]
- [83].van Gelder T, ter Meulen CG, Hené R, Weimar W, Hoitsma A. Oral ulcers in kidney transplant recipients treated with sirolimus and mycophenolate mofetil. Transplantation. 2003;75(6):788–91. [DOI] [PubMed]; van Gelder T, ter Meulen CG, Hené R, Weimar W, Hoitsma A. Oral ulcers in kidney transplant recipients treated with sirolimus and mycophenolate mofetil. Transplantation. 2003;75(6):788–91. doi: 10.1097/01.TP.0000056639.74982.F9. [DOI] [PubMed] [Google Scholar]
- [84].Smith AD, Bai D, Marroquin CE, Tuttle-ewhall JE, Desai DM, Collins BH, et al. Gastrointestinal hemorrhage due to complicated gastroduodenal ulcer disease in liver transplant patients taking sirolimus. Clin Transplant. 2005;19(2):250–4. [DOI] [PubMed]; Smith AD, Bai D, Marroquin CE, Tuttle-Newhall JE, Desai DM, Collins BH. et al. Gastrointestinal hemorrhage due to complicated gastroduodenal ulcer disease in liver transplant patients taking sirolimus. Clin Transplant. 2005;19(2):250–4. doi: 10.1111/j.1399-0012.2005.00332.x. [DOI] [PubMed] [Google Scholar]