SUMMARY
The high transmissibility of SARS-CoV-2 before and shortly after the onset of symptoms suggests that only diagnosing and isolating symptomatic patients may not be sufficient to interrupt the spread of infection; therefore, public health measures such as personal distancing are also necessary. Additionally, it will be important to detect the newly infected individuals who remain asymptomatic, which may account for 50% or more of the cases. Molecular techniques are the “gold standard” for the diagnosis of SARS-CoV-2 infection. However, the massive use of these techniques has generated some problems. On the one hand, the scarcity of resources (analyzers, fungibles and reagents), and on the other the delay in the notification of results. These two facts translate into a lag in the application of isolation measures among cases and contacts, which favors the spread of the infection. Antigen detection tests are also direct diagnostic methods, with the advantage of obtaining the result in a few minutes and at the very “point-of-care”. Furthermore, the simplicity and low cost of these tests allow them to be repeated on successive days in certain clinical settings. The sensitivity of antigen tests is generally lower than that of nucleic acid tests, although their specificity is comparable. Antigenic tests have been shown to be more valid in the days around the onset of symptoms, when the viral load in the nasopharynx is higher. Having a rapid and real-time viral detection assay such as the antigen test has been shown to be more useful to control the spread of the infection than more sensitive tests, but with greater cost and response time, such as in case of molecular tests. The main health institutions such as the WHO, the CDC and the Ministry of Health of the Government of Spain propose the use of antigenic tests in a wide variety of strategies to respond to the pandemic. This document aims to support physicians involved in the care of patients with suspected SC2 infection, in the context of a growing incidence in Spain since September 2020, which already represents the second pandemic wave of COVID-19.
Key words: SARS-COV-2, COVID-19, diagnosis, antigenic test, PCR, primary care, pediatrics, nursing home and long-term facilities, emergency departments, microbiology
INTRODUCTION
Hand in hand with the increase in transmissibility, the request for diagnostic tests against SC2 has increased, for the study of cases and contacts. The need to measure the kinetics of transmission among contacts has also led to the use of telephone applications, which further increases the diagnostic demand in all health areas. Social and health centers require screening strategies that allow workers and residents to live together safely. Hospitals block or delay their activity because they do not have diagnostic techniques that allow a wide range of medical procedures to be safely performed. Microbiology laboratories have endured great work pressure for months and are rapidly consuming resources that will be needed shortly with the resurgence of the second epidemic wave we are now witnessing. The situation is further complicated by the imminent appearance of other seasonal respiratory viruses (influenza A and B, parainfluenza, syncytial respiratory virus, metapneumovirus, adenovirus, rhinovirus…) that overlap their symptoms with mild forms of SC2. The conclusion is that even with the continuous increase in the capacity and robotization of the microbiology laboratories in the Community of Madrid (CM), it is impossible to meet the diagnostic demand only with molecular techniques based on polymerase chain reaction (PCR) and transcription mediated amplification (TMA), which until now undoubtedly constitute the tests of reference. The action protocols recommended by the Ministry of Health in Spain propose home isolation for all cases and all contacts, with symptomatic treatment for the former [1]. However, the high level of demand, and economic and logistical limitations make it difficult to always comply with the aforementioned recommendations in time and form. Rapid antigenic tests (RAT) have recently been incorporated in an attempt to overcome the practical limitations of PCR or TMA, although a sufficient level of evidence on the former is still lacking. The objective of this document is to measure the current epidemiological and diagnostic problem, describe the advantages and disadvantages of diagnostic techniques to optimize them according to clinical contexts, and establish recommendations for common and practical use that allow us to manage clinical processes safely and efficiently.
METHODOLOGY
During the month of September 2020, the coordinating group (FJC, PB and JSR) selected experts from different scientific societies representing various health fields that support a greater demand for COVID-19 care (Primary Care, Pediatrics, Hospital Emergencies, Internal Medicine , Geriatrics, Infectious Diseases and Microbiology). Two face-to-face meetings were held two weeks apart. Before the first meeting, a script was sent to the experts to algorithmically discuss the diagnosis and management of the main clinical situations in their area of expertise. In the same way, the epigraphs of the document were distributed among the specialists, assigning a person in charge of writing and handing over to the coordinating group. In the second meeting, all the scenarios were shared with all the experts. A period of another week was subsequently left to clarify doubts of interpretation and to consult new recommendations from WHO, ECDC, CDC or other health institutions, which may have appeared within this period. The document and the recommendation algorithms were completed in the first week of October 2020. The sections developed were: i) situation and clinical-epidemiological concepts of SC2 infection in Spain and the Community of Madrid; ii) capacity and current value of the main microbiological techniques in the diagnosis of the disease: iii) procedure for collecting, transporting and storing the nasopharyngeal smear for the detection of SC2 (PCR, TMA and RAT); and iv) algorithms on the implementation of micro-biological techniques in the diagnosis of SC2 infection in different clinical contexts. The completed Document was sent for approval to the Vice-Ministry of Public Health and the COVID-19 Plan of the Community of Madrid.
CURRENT CLINICAL-EPIDEMIOLOGICAL SITUATION AND CONCEPTS OF SC2 INFECTION IN SPAIN AND IN THE COMMUNITY OF MADRID
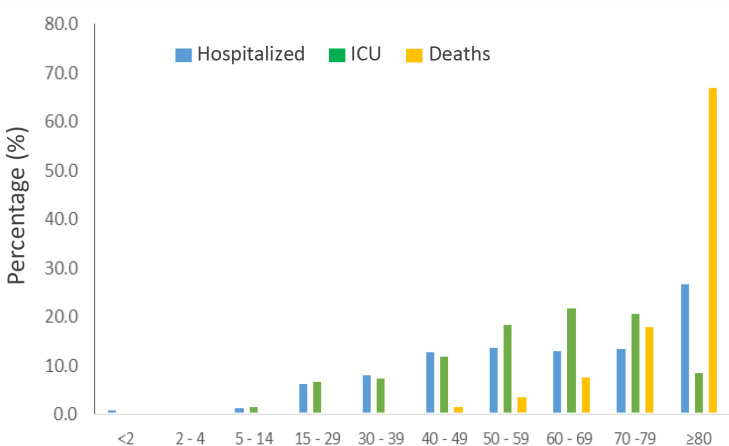
Since the last day of 2019, when the World became aware of the existence of the first cases of infection by SC2, until September 30th 2020, almost 33 million confirmed cases of this infection have been registered worldwide; these figures have been in Europe of more than 5 million, in Spain of almost 750,000 and in the CM of almost 237,000. The lockdown of the Spanish population established between March and May 2020 has divided the progression of new cases of SC2 infection into two pandemic waves, the first with a total of about 310,000 cases [2] and the second, in which we are now found, of around 460,000 cases throughout the national territory. In the second wave, 4.8% of the cases have been hospitalized, 0.4% have been admitted to the ICU (up to 7.4% of patients admitted to hospitals) and 0.6% have died. The highest proportion of COVID-19 cases now occurs in the 15-59 age group (making-up a 69% of the total), with the 15-29 age group being the most represented, with 23% of the cases. The percentage of hospitalizations and deaths by COVID-19 increases with age, now reaching 23.7% and 7.9% in those older than 79 years, respectively [3] (Table 1).
Table 1.
Comparison of demographics in first and second SC2 pandemic waves in Spain (data in the Community of Madrid) [2, 3].
| First wave (RENAVE 11-5-20) [2] |
Second wave (RENAVE 23-9-20) [3] |
|
|---|---|---|
| Cases below 30 years-old | 6.5% | 34% |
| Cases above 60 years-old | 51% | 18% |
| Asymptomatic cases | 50% | 50% (43%) |
| Contact with known COVID case | 53% | 60% (93%) |
| Hospitalized In ICU Deaths |
44% 5% 7.9% |
4.8% (3.7%) 7.4% (3.9%) 0.6% (0.5%) |
SC2: SARS-CoV-2
At this time, 50% of cases are diagnosed through the study of contacts, namely in asymptomatic people. An increase in the proportion of asymptomatic people between the first and second waves has been observed, which may be 40% before and 80% now, according to some studies in the USA [4].
Up to 40.7% of those diagnosed did not report known contact with a diagnosed case of COVID-19. The most frequent field of exposure is at home among cohabitants (33.8%). As high as 97.2% of recent diagnoses were made with molecular techniques, PCR in most cases.
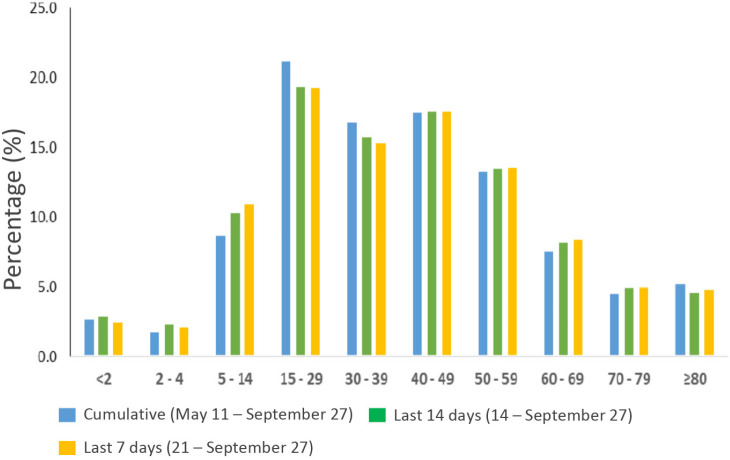
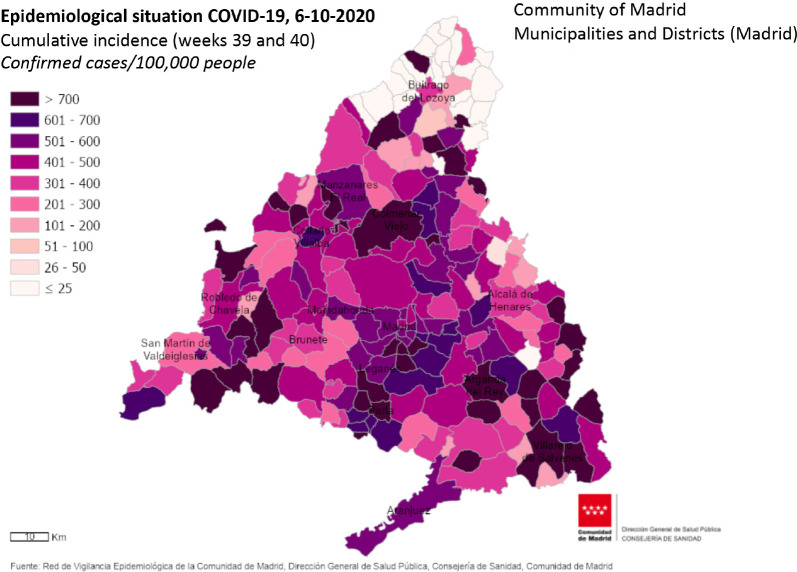
In the CM, the second epidemic wave has peaked to more than 165,000 cases, of which slightly more than 40% have been symptomatic. The distribution of cases by sex is homogeneous, and a third of infections occur in young people (between 15 and 59 years old) (Figure 1). As seen in the first wave, at this time advanced age continues to be a major risk factor for suffering more serious disease (Figure 2). The cumulative incidence rate in the region is 760 cases per 100,000 inhabitants in the previous 14 days, with important differences according to neighborhoods, health areas, and municipalities (Figure 3). In the first weeks of October a decrease in incidence rates has been observed in many areas of the CM. At the present time, about 12,000 patients with COVID are evaluated in the CM, of which 75% are treated in Primary Care and 25% in Hospitals in the region. The number of hospital admissions in the CM has been growing since the first week of August, although in the first weeks of October it seems to have stabilized at around 3,000 people, with a clear downward trend. The proportion of those admitted to ICU is 4% [5].
Figure 1.
Confirmed cases by age group along the second wave in he Community of Madrid (https://www.comunidad.madrid/servicios/salud/2019-nuevocoronavirus#situacion-epidemiologica-actual)
Figure 2.
Distribution of severe cases and deaths by age group in the Community of Madrid (https://www.comunidad.madrid/servicios/salud/2019-nuevocoronavirus#situacion-epidemiologica-actual).
Figure 3.
Cumulative incidence of confirmed cases in the previous 14 days in the Community of Madrid, as of October 6, 2020 (https://www.comunidad.madrid/servicios/salud/2019-nuevo-coronavirus#situacion-epidemiologica-actual).
In the pediatric setting and during the first wave of the pandemic, SC2 infections have accounted for no more than 1-2% of the cases diagnosed worldwide. In China, considering “cases” not only those diagnosed by PCR but also clinically probable, the figures reached 2% [6,7], while in the US according to the CDC, here only including confirmed diagnoses, they accounted for 1.7% [8]. These figures have been similar in Spain, with a proportion of pediatric cases of less than 1%, which has led to the accounting of around 1,300 children with confirmed PCR infection until May 2020, according to data from the Ministry of Health; 26% of these children required hospitalization and 14% of them were admitted to pediatric intensive care units (PICU) [9-10]. Mortality from COVID-19 has been very low (0.2% of children diagnosed). However, with the increase in diagnostic tests and contact screening in recent months, this situation has changed significantly; currently, children account for around 10% of the positive cases detected by PCR, so that between May 10 and the end of August 2020, more than 20,000 positive children have been identified in Spain. However, hospitalization rates have been much lower than in the first period, around 5%, and with admission to the PICU in less than 1% [3]. All of this shows that a very important percentage of detected cases corresponds to children either asymptomatic or with mild symptoms, mainly because of contact studies.
We are facing two challenges with uncertainty, the beginning of the school year and the beginning of autumn-winter, with the usual circulation of respiratory viruses in children. Pediatric services will be in a situation of stress, at a time of the year when the occupation of hospital beds and PICU it is usually complete.
The dynamics of SC2 transmission depends primarily on the concentration of virus in respiratory secretions. It is known that an infected person begins to shed significant amounts of virus from 3 days before of becoming symptomatic, with the maximum peak of viral load found throughout the 24 hours prior to clinical manifestations [11]. In asymptomatic people, it is estimated that the contagion period would be about 8 to 15 days after infection [12,13].
SC2 infection occurs in the majority of cases without symptoms, or as a mild picture affecting the general state and with respiratory or digestive manifestations, with an average incubation period of approximately 5 days (IC95%: 4.5-6 days), with a range of 1 to 14 days. Ninety-seven point five percent of those who develop symptoms will do so within 11.5 days on average (95% CI: 8-16 days) [14]. Only in a low percentage of infected people, particularly in the elderly or patients with other comorbidities, does COVID-19 have a serious course that may require hospital admission (in approximately 2-5% of cases) and cause the death of the patient (in approximately 0.5-1% of cases) [15-17].
Recommendations on periods of isolation in contacts and cases are based on the knowledge of the natural history of COVID-19 [1,18]:
• Study of contacts: risk of infection by SC2 should be considered whenever an undiagnosed person has had contact with another person diagnosed or under study of infection by SC2, if any of the following circumstances are met: i) having been face to face within 1 meter with a case, particularly if it was exposed to coughing or sneezing; ii) a conversation was held or there was physical contact; iii) having shared a small, closed area (room, vehicle, elevator, etc.) with a confirmed case; iii) remain in the same place as a case, at a distance of less than 2 meters and for more than 15 minutes, without protective measures such as a mask and hand washing by both. Symptomatic or asymptomatic persons can be excluded from the diagnostic process of contacts if, for no longer than three months, there is history of a serological test that indicates positive SC2-IgG or of positive SC2-PCR.
The main preventive action on contacts consists of quarantine for 10 days after the last contact with the case. If the contact occurred in the workplace with guarantees that the preventive measures (use of a mask and hand hygiene) were complied with, it is possible to de-isolate the contact if there is negative PCR during the aforementioned quarantine. If a contact develops symptoms during the quarantine period, they will be handled as a case, as indicated below. The period to consider for the study of contacts will be from 2 days before the onset of symptoms of the case until the moment in which the case is isolated. In asymptomatic cases confirmed by PCR, contacts will be sought from 2 days before the date of diagnosis. No special measures are necessary between partners or contacts of quarantined contacts, unless the contact develops symptoms and presents a positive diagnostic test for infection. If this circumstance occurs, the contact becomes a case and the partners or contacts will have to quarantine for 10 days as indicated above. For epidemiological purposes, it is recommended to carry out molecular tests on the contacts under study. As a general rule, it is not necessary to carry out a diagnostic test to confirm its negativity after successful quarantine.
• Case study: a suspected case of SC2 infection should be considered in any person with a clinical picture of respiratory infection (fever, cough, muscle aches, general malaise). Other suspected symptoms are a sore throat (odynophagia), loss of smell (anosmia), or loss of taste (ageusia). Contacts of cases who develop symptoms are also considered suspected cases.
The main preventive action on suspected or probable cases is isolation at home for ten days, and at least 3 days after the disappearance of symptoms. A viral detection diagnostic test should be proposed to confirm the infection whenever possible, to broaden the circle of isolation measures, and particularly in health or social health personnel, or in people who live with a vulnerable population. It is necessary to obtain a negative result in a molecular technique before health personnel, social health workers or people in contact with a vulnerable population come into contact with a population at risk.
Taking into account the knowledge generated about the COVID-19 pandemic, the diagnosis of the disease fulfills two functions, one aimed at the general population and the other at the patient. the first, with an epidemiological focus, to detect those infected and indicate the isolation measures that contain the expansion of the epidemic, and the second, of a more clinical nature, to identify the most serious cases and be able to make medical decisions (admission, treatment, prognosis) in addition to isolation. This distinction can also lead to consider that on the one hand there is the detection of infected people and, as a subgroup of these, the identification of those infected who are themselves infectious.
CAPACITY AND CURRENT VALUE OF THE MAIN MICROBIOLOGICAL TECHNIQUES IN THE DIAGNOSIS OF ACUTE DISEASE DUE TO SC2
Molecular techniques. To date, the gold standard tests for the virological diagnosis of SC2 infection are based on the detection of nucleic acids in nasopharyngeal secretions. The most widely used technique is PCR and TMA, that has subsequently been incorporated. The sensitivity and specificity of these techniques is very high, both around 99%, which makes them very useful for diagnosing infection [19].
However, the positivity of molecular techniques can extend for weeks, well beyond the infective period that is currently established at 10 days from the first positive molecular test in asymptomatic patients, or additionally three days without symptoms in patients with clinical manifestations. It can therefore be said that molecular techniques are “excessively sensitive” to establish infectivity, since they are capable of detecting very low viral loads, between 20 and 100 copies of RNA per mL according to the techniques [20], while sample infectivity is found in concentrations greater than 100 RNA copies/mL [21-23].
Taking into account that the risk of contagion is directly related to the viral concentration in the secretions, it has been proposed that the number of PCR cycles (Ct) necessary for the test to be positive would be inversely related to the infectivity of the sample [24]. In patients with a higher viral load, PCR positivity would be achieved with a lower number of cycles (around 20 cycles) than in patients with a lower viral load, who would give a positive result at higher cycles (greater than 30 cycles). Since the TMA technique is isothermal, it does not allow the estimation of viral concentration to be applied through the cycles.
This approximation by the Ct index to establish the degree of infectivity of the patient is subject to numerous factors of variability that make homogeneity of diagnostic criteria difficult: i) the quality of the sample obtained, ii) the presence of inhibitors, iii) the delay in processing, iv) the difference in the number of cycles that each commercialized system works with, and iv) differences in the cycle in which the various amplification targets, often two or three, are reached.
The delay in issuing results delays decisions about isolating infected people. This problem is exacerbated when the volume of tests requested increases and the laboratories are not able to absorb the demand within the usual deadlines. If this overload is associated with the growing problem in the supply of equipment, reagents or consumables, it is very possible that in a short time the indications of PCR and TMA will have to be restricted to most complex medical procedures (diagnostic techniques, hospitalization, admission to ICU, surgery) and may not be suitable in settings with less clinical severity, which are nevertheless those with the highest viral transmissibility.
Difficulties in carrying out molecular tests in the study of contacts and diagnosis of cases without or with few symptoms make it necessary to apply temporary criteria for isolation (10 days from contact, or at least 10 days from the onset of the clinical picture, always ensuring no symptoms for the last 3 days), which in many circumstances can cause personal and financial costs. These added burdens could be reduced if isolation periods are shortened after ruling out infection by viral screening tests.
Antigenic techniques. The limitations derived from the use of molecular techniques for the epidemiological and clinical purposes of the diagnosis of SC2 infection have recently led to the exploration of other alternatives. Antigen detection tests (ADT) are rapid diagnostic methods, based on lateral immuno-chromatography, already in use for other respiratory viruses (e.g. influenza virus, syncytial virus). Diagnostic capacity of ADT in these other viral processes is limited due to the low viral load in its acute phase. However, in the case of SC2, the viral load is high in the nasopharynx of infected patients within the first week of disease progression, which makes it possible to detect the virus with high sensitivity in this period. Throughout August 2020 the FDA has authorized the use of four trademarks based on various scientific evidences that are summarized below.
The sensitivity of the first antigenic tests was significantly lower than that detected by the nucleic acids (56.2% (IC95%: 29.5-79.8%)) with a comparable specificity (99.5% (IC95% (98.1%-99.9%)) [25]). However, the new generation of antigenic tests present, during the first week of infection, comparable values of sensitivity and specificity [26-28]. It has been shown that for viral loads below 2 log copies/mL the correlation between antigen and molecular techniques is 100%, while it drops to 60% with viral loads of 1-2 log copies/mL, and to 33% with viral loads <1 log copies/mL. As a consequence, other factors related to viral load can be used as surrogate markers of the validity of antigen tests: i) duration of infection: during the first week of symptoms the sensitivity of the ADT is on average 93.9% (95% CI: 86.5-97.4%) [28]; ii) Ct index: the sensitivity of ADT is 98% (95% CI: 90-100%) for Ct ≤25, and 57% (95% CI: 48-65%) for Ct ≥30 [26,27] . According to these data it can be affirmed that ADT have special clinical utility in suspected cases during the first 5-7 days of symptoms.
Having a test with high sensitivity and specificity are necessary, but not sufficient, conditions for an accurate individual diagnosis in environments such as COVID-19 with changing prevalence depending on the place and time. In settings in which the probability of SC2 infection is high, such as in community-transmission settings, high prevalence of COVID-19, or patients with compatible clinical symptoms or previously exposed to SC2, a positive result on the ADT probably indicates acute infection. However, in this same scenario, a negative result cannot be interpreted with equal certainty, so a second test would be necessary, either another ADT a few days later or a molecular test. On the contrary, in settings with a low prevalence or when there is little suspicion of SC2 infection, ADT are associated with a high negative predictive value, therefore they reliably rule out infection (Figure 4).
Figure 4.
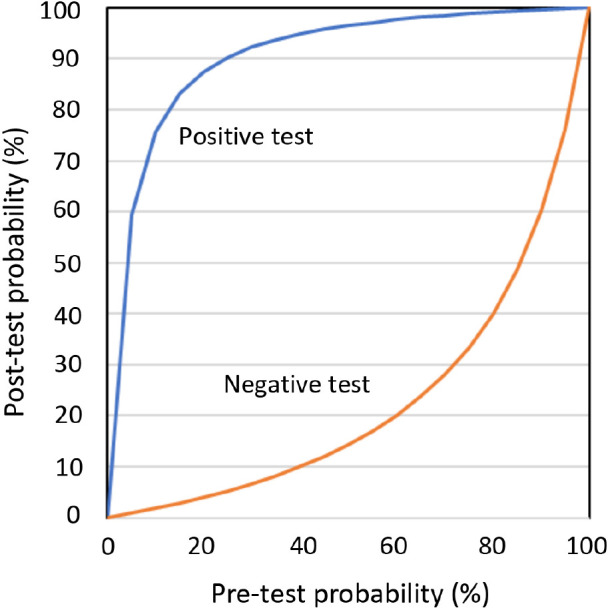
Pre-test and post-test probability of infection according to results of test with 83.8% sensitivity and 97% specificity
Apparently, ADT would not be suitable in the study of contacts or asymptomatic cases, since in general in this clinical context the levels of viral load are low. However, the simplicity and low cost of this test allow them to be repeated frequently, even daily. Having a viral detection analysis in real time and being able to confirm the negative result in the following days (antigen test), has proven more useful to control the spread of infection in closed populations than to perform a more sensitive test, but with longer delay time and cost (molecular test) [28].
PROCEDURE FOR COLLECTING, TRANSPORTING AND STORING THE NASOPHARYNGEAL SMEAR FOR THE DETECTION OF SC2 (MOLECULAR TECHNIQUE AND ANTIGENIC DETECTION)
A series of preconditions are necessary for performing the nasopharyngeal and oropharyngeal smear in the diagnosis of SC2 infection, by molecular technique or antigen detection: i) personal protective equipment, ii) ventilated and isolated space, iii) semi-flexible swabs with preservative medium for viruses, without inactivators (for molecular study), or without preservative medium (for antigen detection).
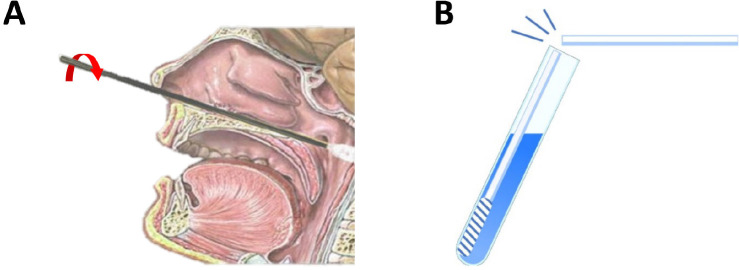
The procedure for collecting, transporting and storing clinical samples for SC2 is set out in numerous official documents [29-32]. Although the sample collection technique for PCR is simple, some experience is required to ensure that the exudate obtained is representative and is not artifacted by the presence of blood or other substances. The patient must enter the extraction point with an individual mask. The sample will be taken with the patient sitting and with his head tilted back, blowing his nose first to avoid traces of mucus in the sample. In the case of a nasopharyngeal smear, the swab will be introduced through a nostril, parallel to the floor of the nasal cavity. If any obstacles are encountered, the swab should be rotated slowly to proceed. Finally, the swab should reach the posterior wall of the nasopharynx or cavum. Once in this location, the swab should be rotated on its own axis to collect as many epithelial cells as possible (Figure 5A). Later, the swab will be removed and inserted through the other nostril with the same technique. For the oropharyngeal smear, the sample will be taken by introducing the swab through the mouth until it reaches the posterior wall of the pharynx, where it will be rotated several times to collect a sample of epithelial cells.
Figure 5.
Nasopharyngeal smear technique to perform the antigenic test against SARS-COV-2. A: The swab must reach the posterior wall of the nasopharynx or cavum. Once there, it should be turned on its own axis to collect as many epithelial cells as possible. B: The swab must be stirred well in order to get a good emulsion in the medium and break at the notch.
The sample swab will be inserted into the vial containing the virus preservative medium. The swab must be stirred well into the medium to achieve a good emulsion, and then broken at the notch (Figure 5B). Subsequently, the vial is closed with a screw cap to prevent leakage. The samples must be placed in triple biological safety containers or similar, and kept at 4ºC until collected. The samples must be correctly identified with the patient data. In the same way, they must be sent with the corresponding petitioner leaflet containing the complete demographic data of the patient, as well as the origin of the petitioner.
The nasopharyngeal smear procedure for antigenic study is very similar to that described above. The precautions and biosafety requirements are the same and the collection of the sample will be carried out in a similar way, but using the swabs that incorporate the commercial tests. The swab should be processed immediately, by placing it in a tube with extraction buffer. If sample processing cannot be done immediately after collection, the swab can be stored in the collection tube at room temperature for up to 2 hours.
It is necessary to establish a computerized system in the laboratory of microbiology for recording the sampling and results also for antigenic tests, regardless of the place where they were carried out, outpatient setting, emergency room or hospitalization. The versatility of ADT lends itself to the fact that the results may not be adequately recorded, which generates errors in patient management and additional costs.
If there is needed to store or transport the samples to another institution, since blows or spills may occur, they must be treated as potentially infectious (category B), therefore they must be transported in triple packaging (UN3373 standard). It is not essential that the transport of clinical samples with SC2 be carried out by specialized companies. Packing of the samples shall be carried out in accordance with the packing instruction P650 of the ADR agreement, which applies to the UN3373 standard for the packing of hazardous substances (the packing instruction P650 is equivalent to the IATA instruction 650).
The package must consist of three layers. A first container or tube, which will contain the infectious substance, which must be airtight and impermeable to the substance it contains. There will be a second hermetic and impermeable container (plastic bag with the corresponding marks and pocket for the petition flyer), spill-proof and with sufficient absorbent material in case of breakage or leakage. Finally, a third layer or packaging, which will be used to protect the secondary containers or plastic bags from physical damage during transport, if necessary.
There are a series of criteria for acceptance or rejection of samples to guarantee the traceability, quality, conservation and representativeness of the sample received in the laboratory, since all these factors affect the results of the sample and have a clinical and epidemiological impact.
The most frequent incidents in the arrival of a sample to the microbiology laboratory are listed below:
• Poorly identified sample: an unidentified, misidentified or sample in which the identification of the request leaflet does not coincide with that of the sample should not be accepted. In any case, the requesting service will be contacted to inform them of the need for them to proceed with the correct identification of the sample. If possible, the error will be corrected or the sample will be collected again.
• Spilled or deteriorated samples: spilled samples will not be accepted, a new sample will be requested. If it is not possible to obtain a new sample, an attempt will be made to clean the outside of the container with antiseptic in order to then obtain the best possible sample, leaving a record of the status of the sample upon arrival at the laboratory.
• Inappropriate transport or storage: if the above-mentioned transport and storage requirements are not met, a new sample will be requested. In the case of samples that cannot be collected again, you can choose to process them by informing the requesting service in writing of the incident that affects the sample, and warning that the results obtained must be interpreted with the corresponding caution.
ALGORITHMS ON THE IMPLEMENTATION OF MICROBIOLOGICAL TECHNIQUES IN THE DIAGNOSIS OF ACUTE INFECTION BY SC2 IN DIFFERENT CLINICAL CONTEXTS
Primary Care (PC)
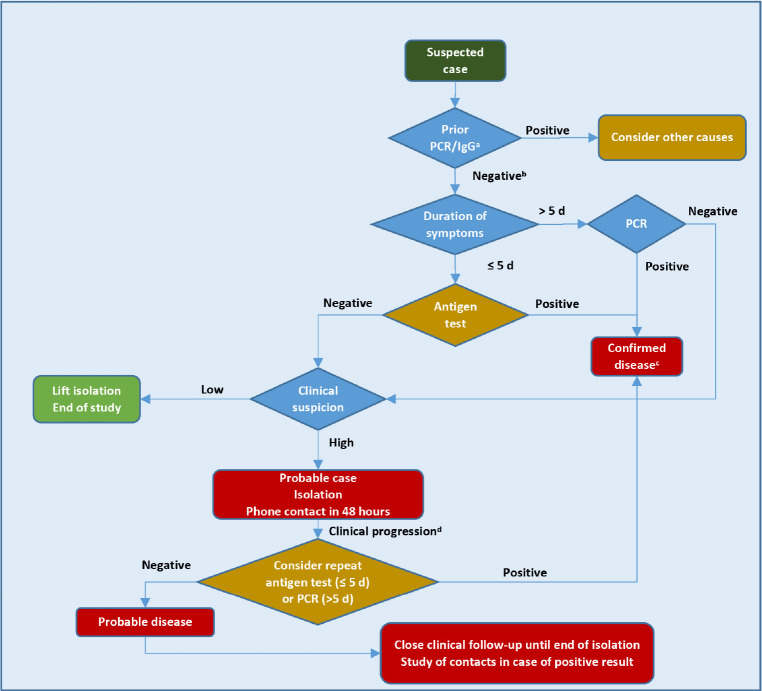
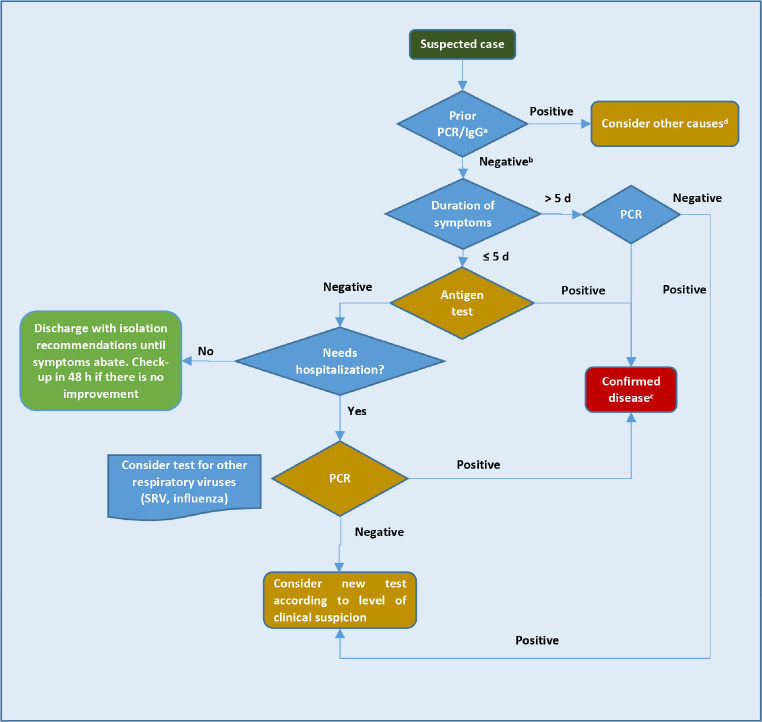
a) Suspected case of SC2 infection (Figure 6)
Figure 6.
Work-up algorithm for the study of suspected cases of acute SC2 infection in Primary Care.
aDone in the previous 3 months, except in special cases; bOr not done; cPositive antigen test does not require confirmation with PCR; dNew symptoms or worsening of previous ones, without severity criteria (severe dyspnea, tachypnea ≥30 rpm, Sat O2≤93%, and/or pulmonary infiltrates ≥50%) [34]
Antigen detection (ADT) or genetic (PCR or TMA) tests will be carried out on all persons aged 14 years and over if considered suspected cases of SC2 infection (see definition above). There is not enough evidence at the moment about the possibility of SC2 reinfections (32), so in people with a history of COVID-19 in the previous 3 months it is necessary to consider other diagnostic possibilities before considering antigen or molecular tests for SC2.
The choice of technique (ADT, PCR, TMA) will depend on the time elapsed since the onset of symptoms. In patients with symptoms of 5 or less days of evolution, ADT will be preferred. Any positive result in ADT, PCR or TMA should be treated as a confirmed case, indicating home isolation, study of close contacts and clinical follow-up. If there is not a high suspicion of COVID-19, if there is a negative result in these tests, infection with SC2 will be ruled out, and the isolation may be interrupted. If the suspicion of COVID-19 is still high (typical symptoms -ageusia or anosmia-, analytical parameters or compatible radiological findings, recent contact with a confirmed case, etc.) the patient will be considered as a probable case, therefore isolation and study of contacts will be indicated. Although there are no specific symptoms and signs of SC2 infection, the frequency of clinical manifestations in the different published series makes it possible to classify the symptoms and signs that in adults better predict the probability of positivity in a screening test for SC2 (Table 2) [33,34].
Table 2.
Probability of COVID-19 according to presenting symptoms [Modified from reference 33]
| Symptoms with high predictive value | Symptoms with low predictive value |
|---|---|
|
Type A (acute in the lower respiratory tract): Dry or productive cough, dyspnea with no other cause |
Type C: Throat ache, intestinal symptoms (nausea, vomits, diarrhea), nasal symptoms (congestion, runny nose, sneezing), ocular symptoms (red eyes, dry eyes, foreign body sensation). |
|
Type B: Fever (Temp ≥38˚C) o high temperature (Temp ≥37.5˚C) with/without chills, myalgia/arthromyalgia, asthenia, headache, hyposmia-anosmia, hypogeusia-dysgeusia | |
| High probability of SC2 infection | Low probability of SC2 infection |
| Any type A symptom, with/without type B or C symptoms ≥2 type B symptoms, with/without type C symptoms ≥3 type C symptoms |
Type C symptoms, without type A or B symptoms |
SC2: SARS-CoV-2
Clinical monitoring from PC will be carried out, whenever possible, in a non-face-to-face way (by telephone or telematics), to reduce the risk of contagion of health care personnel. A SC2 test will be repeated if 48 hours after the first test was done the patient presents clinical progression (worsening or the appearance of new symptoms). The choice of the diagnostic test will depend on the time elapsed since the beginning of symptoms. A positive microbiological result will definitely confirm the case; if the result is negative, since the clinical suspicion of COVID-19 remains high, isolation will be maintained until 3 days after the resolution of the fever and the significant improvement in the clinical picture, with a minimum of 10 days from the onset of symptoms. It will not be necessary to perform a microbiological technique to finalize the isolation. Both in the case of positive and negative microbiological results, in patients with symptoms clinical follow-up will continue from PC.
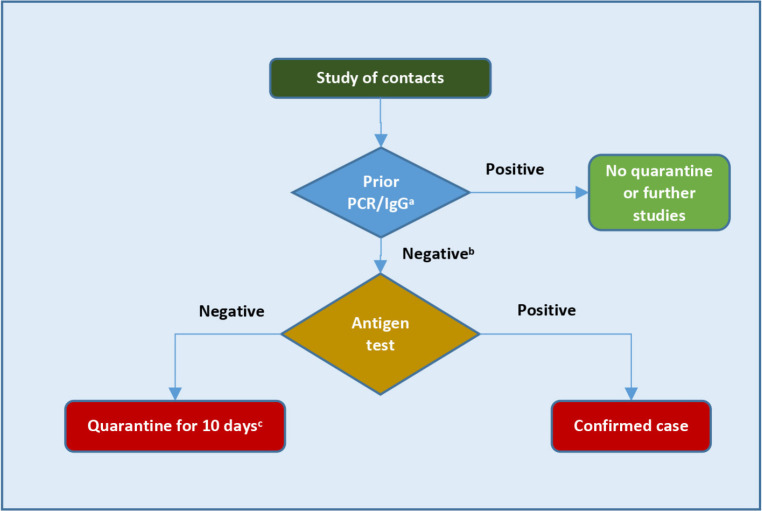
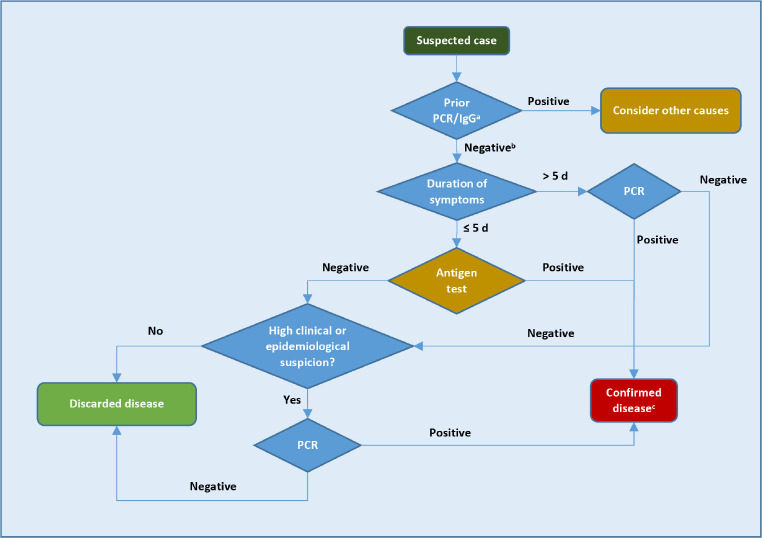
b) Close contact with infected with SC2 (Figure 7)
Figure 7.
Work-up algorithm for the study of close contacts of SC2 infection in Primary Care.
aDone in the previous 3 months, except in special cases; bOr not done; cConsider PCR in health or social care personnel
Any person considered close contact will be studied and monitored at PC. People with a history of SC2 infection in the previous 3 months, confirmed by serological, molecular or antigen tests, can be excluded from the contact study. Surveillance and home quarantine will be indicated for all close contacts of a confirmed case for 10 days after the last contact. In addition, with the main objective of detecting new positive cases of COVID-19 in asymptomatic phase, an ADT or a PCR or TMA will be performed after the identification of the contact. PCR or TMA are preferable in people who may be at higher risk of evolving into serious, critical or fatal disease (Table 3) [35-40], their caregivers and partners, and in health workers, or workers in social health centers or essential services. In the rest of the cases ADT may be of choice. Any positive result of any of the mentioned tests must be treated as a confirmed case. If the result is negative, the home quarantine will also continue until day 10.
Table 3.
Factors related with poorer COVID-19 outcome [Modified from references 35-40]
| Comorbidities | Other factors |
|---|---|
| Severe cardiovascular disease (heart failure, ischemic heart, myocardiopathies) HBP Diabetes Mellitus COPD Autoimmune disease Immunodepression (HIV infection, solid organ or bone marrow transplant, corticoids or other immune suppressive drugs) Sickle cell disease Obesity (BMI>30) Solid organ or blood cancer Chronic liver or kidney disease Alzheimer’s disease Depression |
Greater than 70 years old Greater than ≥60 years old with ≥1 comorbidities Any age with ≥2 comorbidities Institutionalized people |
If during the follow-up period the contact develops symptoms, this person will be considered as a suspected case and the SC2 detection test will be repeated. The choice of technique will be made based on the time elapsed since the initial exposure to the case. Taking into account the average incubation period for SC2 (4-5 days) and that from the theoretical point of view the viral load levels are lower in asymptomatic patients, ADT should be used within the first 7 days from the initial exposure to the case, and provided that the duration of the symptoms is less than 5 days. Outside of these periods, a molecular technique will be used. Any positive result of molecular or antigenic tests should be treated as a confirmed case. Despite the result of the SC2 detection tests were negative, the quarantine will continue until day 10.
Pediatric field
Pediatric cases have been described in all age groups, although the median age is around 8 years and without a clear predominance of sex [7,41-42]. The incubation period is similar in children to that of adults, although the majority of pediatric cases are asymptomatic or have mild symptoms, and may manifest as an upper respiratory infection or a gastrointestinal infection. The most frequent symptoms of COVID-19 in children are fever and cough, which are observed in around 50% of symptomatic cases. Minors can also present odynophagia, rhinorrhea and diarrhea, as well as more nonspecific symptoms such as myalgia, fatigue or abdominal pain. Anosmia and ageusia are less common in children and adolescents [43]. In nurslings COVID-19 can present as a fever without a source.
It has been considered that isolated rhinorrhea may be attributable to a multitude of viriasis; in the case of SC2 infection, it should be assessed whether this symptom is associated with other symptoms more characteristic of COVID-19, leaving open the possibility of not performing an SC2 test; each case will be assessed individually, taking into account the epidemiological context.
The clinical picture associated with greater severity and the need for intensive care is the pediatric multisystemic inflammatory syndrome (MIS-C) linked to SC2 [44-46], which could correspond to a late inflammatory response infection and which has accounted for around 17 % of hospitalizations in PICU in Spain [47].
Among the most frequent radiographic findings are patchy infiltrates and bilateral ground glass opacities on chest X-rays, although other radiographic patterns are possible [48]. Regarding admissions, children under one year of age are the group with the highest incidence of hospitalization. Severity risk factors are age less than 1 year or greater than 10 years, in addition to the presence of comorbidities and obesity [7]. Data on the possible vertical transmission of SC2 are still limited, although it seems highly unlikely [49].
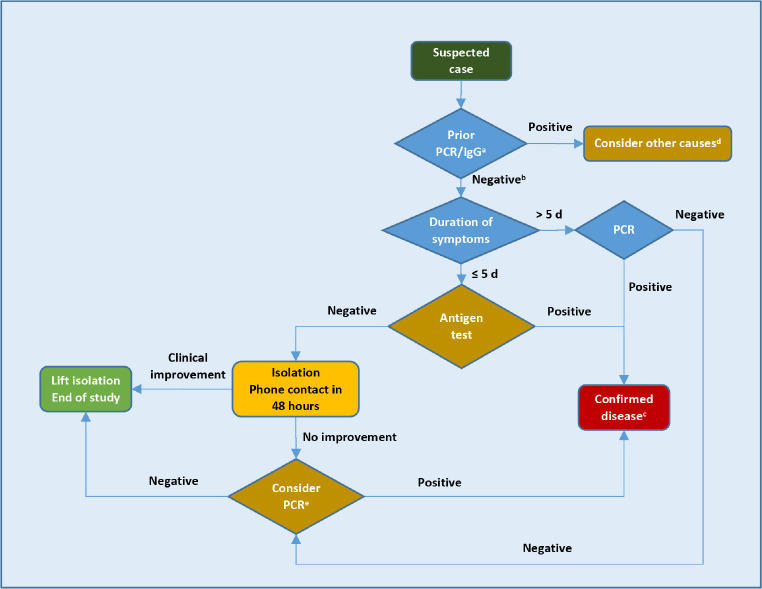
In the pediatric area we consider three situations that include the care of the child with suspected SC2 infection in PC (Figure 8), in Hospital Emergencies (Figure 9) and the study of contacts, including the school setting (Figure 10). In the algorithm, we highlight that when evaluating a child, the family epidemiologic environment is important, since at home transmission is especially relevant, with around 70% of intra-family cases [42,50].
Figure 8.
Work-up algorithm for the study of suspected cases of acute SC2 infection in Primary Pediatric Care.
aDone in the previous 3 months, except in special cases; bOr not done; cWith positive antigenic test no PCR confirmation is required. The presence of fever, cough, odynophagia, respiratory distress, ageusia, anosmia, gastrointestinal symptoms are considered suggestive symptoms of COVID-19. Isolated rhinorrhea would not be considered clinically suggestive (also take into account the family epidemic environment and context); dIf the patient already had an infection confirmed by PCR or presents positive SC2-IgG in the previous 3 months, it is not recommended to perform the antigenic test or PCR, except in special cases (immunosuppressed or at-risk cohabitants or need for admission); eConsider PCR if there is no improvement, persisting clinical or epidemiological suspicion.
Figure 9.
Work-up algorithm for the study of suspected cases of acute SC2 infection in Pediatric Emergency Room.
aDone in the previous 3 months, except in special cases; bOr not done; cWith positive antigenic test, no PCR confirmation is required. The presence of fever, cough, odynophagia, respiratory distress, ageusia, anosmia, and gastrointestinal symptoms are considered suggestive symptoms of COVID-19. Isolated rhinorrhea would not be considered clinically suggestive (also take into account the family epidemic environment and context); dIf the patient already had a confirmed infection by PCR or presents positive SC2-IgG in the previous 3 months, it is not recommended to perform the antigenic test or PCR, except in special cases (immunosuppressed or cohabitants at risk or need for admission).
Figure 10.
Work-up algorithm for the study of close contacts of SC2 infection in the pediatric field, including schools.
aDone in the previous 3 months, except in special cases; bOr not done; cPositive antigenic test does not require PCR confirmation;dIf the patient already had a confirmed infection by PCR or presents positive SC2-IgG in the previous 3 months, it is not recommended to perform the antigenic test or PCR, except in special cases (immunosuppressed or cohabitants at risk or need for admission). In case of close contact at school test not generally indicated, but a test is to be done if the patient develops symptoms during quarantine, vulnerable people according to the criteria of their pediatrician or family doctor, or in situations of special risk, prior public health indication.
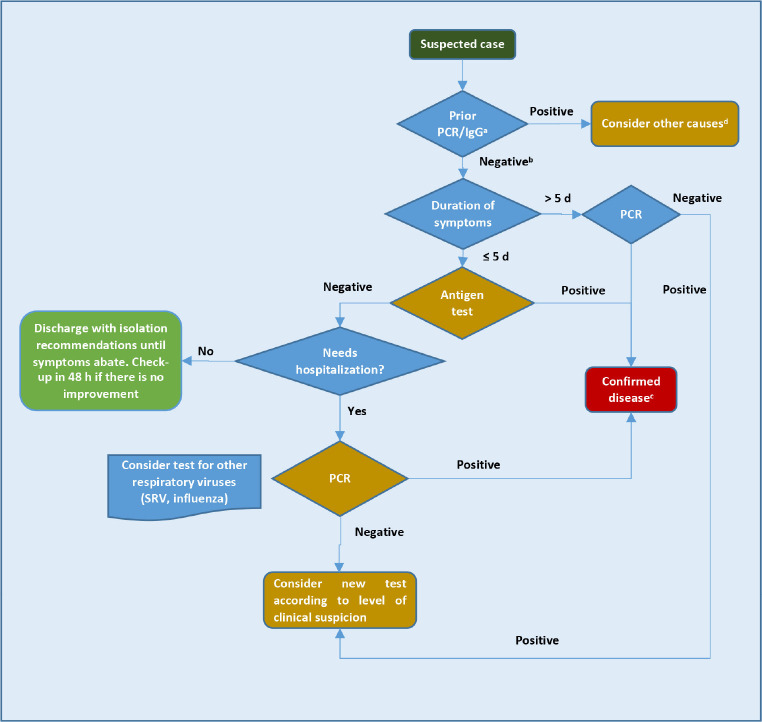
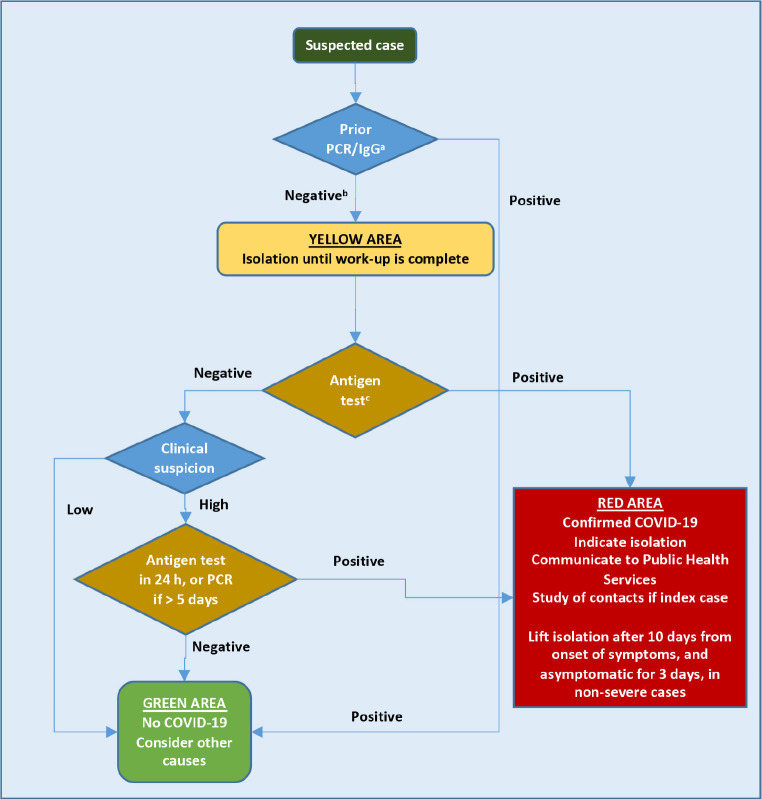
Hospital emergency
The criteria shown in the corresponding algorithm (Figure 11) to carry out the ADT for SC2 in the adult emergency department are proposed in accordance with international recommendations [51-53]. We must take into account a series of considerations: i) if a patient has suffered from COVID-19 in the last 3 months, according to molecular technique (PCR or TMA positive) or positive SC2-IgG, other diagnostic alternatives should be considered before requesting any diagnostic test for SC2 (molecular or antigenic). In the emergency services, the performance of any type of screening test for SC2 in the nasopharynx (antigenic or molecular) will be considered indistinctly, availability, experience in use and care overload will be taken into account. ADT will be recommended preferentially in patients who come to the emergency room without hospitalization criteria with symptoms for 5 or less days.
Figure 11.
Work-up algorithm for the study of suspected cases of acute SC2 infection in Emergency Services.
aDone in the previous 3 months, except in special cases; bOr not done; cPositive antigenic test does not require PCR confirmation.
A positive ADT result confirms COVID-19; if the ADT is negative and the patient does not have criteria for hospital admission, active infection will be considered reasonably ruled out, especially in patients with mild symptoms. In a population like in the CM, with a prevalence of infection that ranges between 10% and 30%, the positive predictive value of ADT is between 97.2% and 99.3%, and the negative predictive value is between 94.5% and 98.5%. If the ADT result is negative, the patient has hospital admission criteria and there is a high clinical or epidemiological suspicion of SC2 infection, a molecular technique should be repeated in nasopharyngeal exudate (PCR or TMA). If the duration of symptoms is greater than 5 days, a molecular technique will be preferred. At the present time, ADT are not indicated in symptomatic patients with more than 5 days of evolution or as a screening of patients treated in the Emergency Department for a pathology other than COVID-19.
Sociosanitary Centers
To carry out ADT for SC2 in the field of social health centers, the procedure shown in the algorithms in Figures 12, 13 and 14 will be followed depending on whether it is the study of a suspected case, of a close contact or of the screening of a worker [1,18]. A suspected case will be defined as any person with a clinical picture of respiratory infection of any severity, which, depending on the symptoms, can be graded as follows: i) high clinical suspicion: if they present two or more typical symptoms (fever, cough, dyspnea , odynophagia, anosmia, ageusia, myalgia, diarrhea, chest pain or headache); ii) low clinical suspicion: if it presents only a typical symptom or presents with atypical symptoms for an SC2 infection (general malaise, fall, asthenia, confusional syndrome) [54]. A patient will be defined as having a documented history of SC2 infection if they present in the last 3 months positive SC2-IgG and / or a positive SC2 PCR or TMA. So far there is no evidence on the possibility of reinfection by SC2, however, in the event that a patient presents symptoms highly compatible with COVID-19 and a documented history of SC2 infection, an expert should be consulted to study the possibility remote reinfection [32].
Figure 12.
Work-up algorithm for the study of suspected cases of acute SC2 infection in sociosanitary centers (residents or professionals).
aDone in the previous 3 months, except in special cases; bOr not done; cPositive antigenic test does not require PCR confirmation.
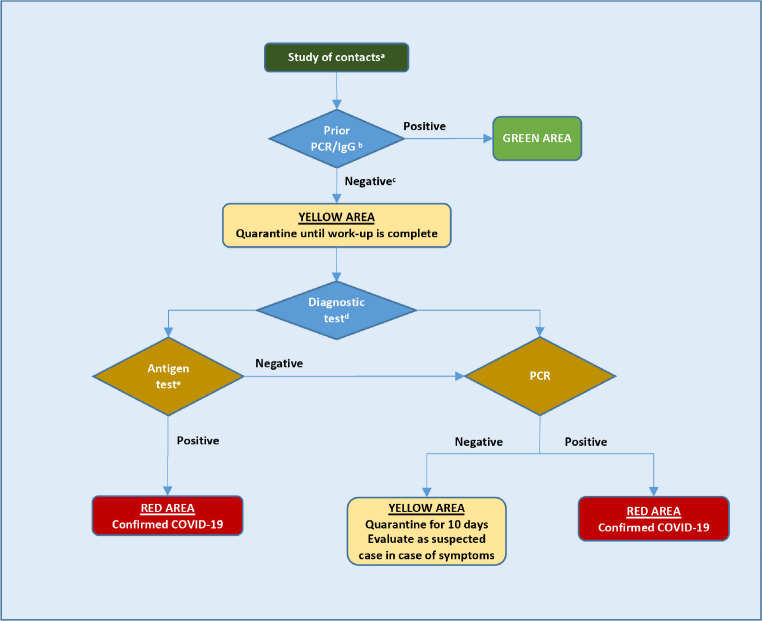
Figure 13.
Work-up algorithm for the study of close contacts of SC2 infection in sociosanitary centers.
aDocumented history of COVID-19 in the previous 3 months; bDone in the previous 3 months, except in special cases; cOr not done; dAntigenic test or PCR depending on the availability of the tests. If the lag for PCR result is expected to be less than 24 hours, it is preferable to perform a baseline PCR. Otherwise, it will be preferable to chose antigen test, having to confirm negative results with PCR; ePositive antigenic test does not require PCR confirmation.
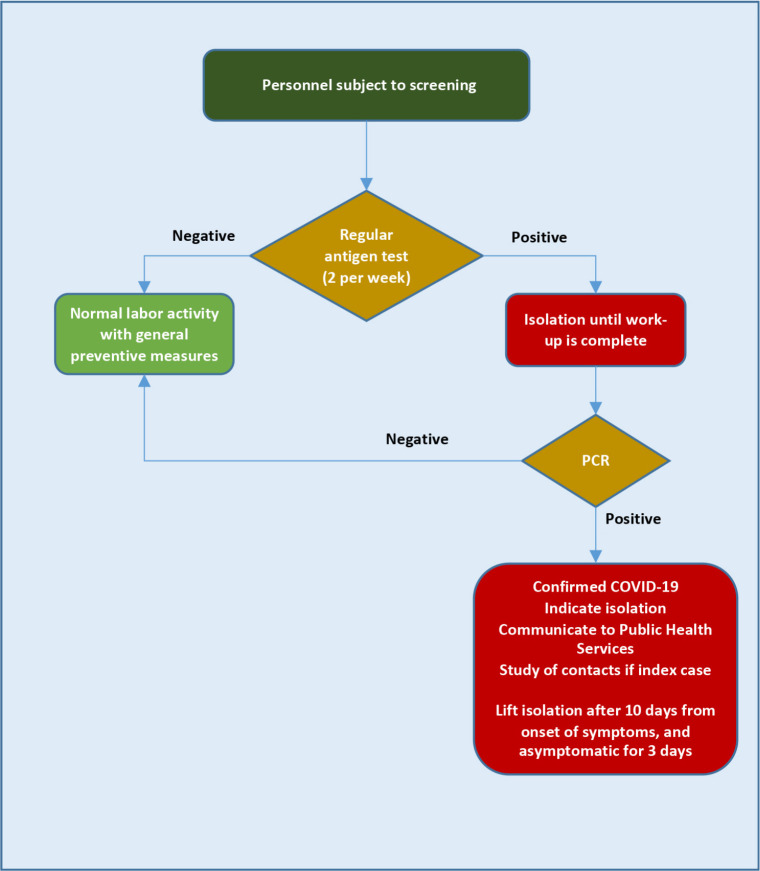
Figure 14.
Work-up algorithm for the screening of SC2 infection in personnel in sociosanitary centers.
Close patient-in-residence contacts will be considered to be any person who has provided care (health or social-health personnel, family members or people who have other similar types of physical contact) to a confirmed case without adequate protection measures, or to any person who has been in the same place as a case at a distance of less than 2 meters and for more than 15 minutes. The period to be considered will be from 2 days before the onset of symptoms of the case until the moment in which the case is isolated. In asymptomatic cases confirmed by PCR, contacts will be sought from 2 days before the date of diagnosis.
Antigenic vs PCR test will be chosen depending on the availability of the tests. If the waiting time for the PCR result is expected to be less than 24 hours, it is preferable to perform an initial PCR. Otherwise, the antigen test will be preferred and negative results will have to be confirmed by PCR.
The screening of workers in social health centers (Figure 14) will be considered in residences that have a seroprevalence (percentage of IgG+) among residents of less than 50%, have nursing staff, and are not in the active outbreak phase.
The antigenic tests could not be suitable in the study of asymptomatic cases, since in this clinical context it is not possible to specify the age and the nasopharyngeal viral load could already be low. However, the simplicity and low cost of this test allows to repeat them frequently (twice a week). Having a viral detection test in real time, and being able to confirm the negative result in the following days, has been shown to be even more useful to control the expansion of the infection in closed populations than performing a more sensitive test, but with a longer delay and higher cost (molecular test) [28].
References
- 1.Instituto de Salud Carlos III. Estrategia de detección precoz, vigilancia y control de COVID-19. 25 de septiembre de 2020. Disponible en (consultado el 1 de octubre de 2020): https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/COVID19_Estrategia_vigilancia_y_control_e_indicadores.pdf
- 2.Instituto de Salud Carlos III. Informe nº 30. Situación de COVID-19 en España. 11 de mayo de 2020. Disponible en (consultado el 29/09/2020): https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20n%C2%BA%2030.%20Situaci%C3%B3n%20de%20COVID-19%20en%20Espa%C3%B1a%20a%2011%20de%20mayo%20de%202020.pdf
- 3.Instituto de Salud Carlos III. Informe nº 47. Situación de COVID-19 en España. Casos diagnosticados a partir 10 de mayo. 7 de octubre de 2020. Disponible en (consultado el 10/10/2020): https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20n%C2%BA%2045.%20Situaci%C3%B3n%20de%20COVID-19%20en%20Espa%C3%B1a%20a%2023%20de%20septiembre%20de%202020.pdf
- 4.Gandhi M, Rutherford G. Facial Masking for Covid-19. Potential for “variolation” as we await a vaccine. N Eng J Med 2020. doi: 10.1056/NEJMp2026913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Red de Vigilancia Epidemiológica de la CM. Semana 39. Infección por el nuevo coronavirus COVID-19 (Datos provisionales). 29 de septiembre de 2020: Disponible en (consultado el 29/09/2020): https://www.comunidad.madrid/sites/default/files/doc/sanidad/epid/informe_epidemiologico_semanal_covid.pdf
- 6.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323:1239-1242. doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 7.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z. et al. . Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics 2020; 145:e20200702. doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control. Coronavirus disease 2019 in children-United States. MMWR Morb Mortal Wkly Rep 2020; 69:422-426 doi: 10.15585/mmwr.mm6914e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tagarro A, Epalza C, Santos M, Sanz-Santaeuremia FJ, Otheo E, Moraleda C, et al. . Screening and severity of COVID-19 in children in Madrid, Spain. JAMA Pediatr 2020; e201346. doi: 10.1001/jamapediatrics.2020.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Ceano-Vivax M, Martín-Espín I, del Rosal T, Bueno-Barriocanal M, Plata-Gallardo M, Ruiz-Dominguez JA, et al. . SARS-CoV-2 infection in ambulatory and hospitalized Spanish children. Arch Dis Child 2020. 105:808-809. doi: 10.1136/archdischild-2020-319366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He X, Lau E, Wu P, et al. . Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med 2020; 26:672-5. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 12.Aguirre-Duarte N. Can people with asymptomatic or pre-symptomatic COVID-19 infect others? : a systematic review of primary data. medRxiv 2020. doi: 10.1101/2020.04.08.20054023 [DOI] [Google Scholar]
- 13.Sakurai A, Sasaki T, Kato S, et al. . Natural History of Asymptomatic SARS-CoV-2 Infection. N Engl J Med 2020; 383:885-6. doi: 10.1056/NEJMc2013020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lauer S, Grantz K, Bi Q, et al. . The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020; 172:577-82. doi: 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen N, Zhou M, Dong X, et al. . Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395:507-13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang D, Hu B, Hu C, et al. . Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus infected pneumonia in Wuhan, China. JAMA 2020; 323:1061–9. doi: 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guan W, Ni Z, Hu Y, et al. . Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020; 382:1708-20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Consejería de Sanidad. Estrategia de detección precoz, vigilancia y control de COVID-19 adaptada a la Comunidad de Madrid, 14 de agosto 2020. Disponible en (consultado el 29/9/2020): https://www.comunidad.madrid/sites/default/files/doc/sanidad/epid/estrategia_vigilancia_y_control_adaptada_cm_agosto_2020_v2.pdf
- 19.Smith E, Zhen W, Manji R, Schron D, Duong S, Berry G. Analytical and clinical comparison of three nucleic acid amplification tests for SARS-CoV-2 detection. J Clin Microbiol 2020; 58:e01134-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vogels C, Brito A, Wyllie A, et al. . Analytical sensitivity and efficiency comparisons of SARS-CoV-2 qRT-PCR assays. Nat Microbiol 2020; 5:1299-1305. doi: 10.1038/s41564-020-0761-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quicke K, Gallichote E, Sexton N, Young M, Janich A, Gahm G, et al. . Longitudinal surveillance for SARS-CoV-2 RNA among asymptomatic staff in five Colorado skilled nursing facilities: epidemiologic, virologic and sequence analysis. medRxiv 2020. doi: 10.1101/2020.06.08.20125989 [DOI] [Google Scholar]
- 22.Wölfel R, Corman V, Guggemos W, et al. . Virological assessment of hospitalized patients with COVID-2019. Nature 2020; 581:465–9. doi: 10.1038/s41586-020-2196-x [DOI] [PubMed] [Google Scholar]
- 23.La Scola B, Le Bideau M, Andreani J, et al. . Viral RNA load as determined by cell culture as a management tool for discharge of SARSCoV-2 patients from infectious disease wards. Eur J Clin Microb Infect Dis 2020; 39:1059-61. doi: 10.1007/s10096-020-03913-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tom M, Mina M. To interpret the SARS-CoV-2 test, consider the cycle threshold value. Clin Infect Dis 2020; May 21;ciaa619. doi: 10.1093/cid/ciaa619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dinnes J, Deeks J, Adriano A, et al. . Rapid, point-of-care antigen and molecular-based tests for diagnosis of SARS-2 infection. Cochrane Database Sys Rev 2020; Aug 26;8:CD013705. doi: 10.1002/14651858.CD013705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Porte L, Legarraga P, Vollrath V, et al. . Evaluation of novel antigen-based rapid detection test for the diagnosis of SARS-CoV-2 in respiratory samples. Intern J Infect Dis 2020. 99:328-333. doi: 10.1016/j.ijid.2020.05.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirotsu Y, Maejima M, Shibusawa M, et al. . Comparison of automated SARS-CoV-2 antigen test for COVID19 infection with quantitative RT-PCR using 313 nasopharyngeal swabs including from 7 serially followed patients. Int J Infect Dis 2020; 99:397-402. doi: 10.1016/j.ijid.2020.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larremore D, Wilder B, Lester E, et al. . Test sensitivity is secondary to frequency and turnaround time for covid-19 surveillance. medRxiv 2020. doi: 10.1101/2020.06.22.20136309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.García-Lechuz JM, González JJ, Orta N, Sánchez MI. Recogida, transporte y procesamiento general de las muestras en el Laboratorio de Microbiología. Procedimientos en Microbiología Clínica. Cercenado E, Cantón Moreno R (editores). Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica, 2017. Disponible en (consultado el 29/9/2020): https://seimc.org/contenidos/documentoscientificos/procedimientosmicrobiologia/seimc-procedimientomicrobiologia1b.pdf
- 30.Centers for Disease Control. Interim guidelines for collecting, handling, and testing clinical specimens from persons for coronavirus disease 2019 (COVID-19), 8 de octubre 2020. Disponible en (consul-tado el 29/9/2020): https://www.cdc.gov/coronavirus/2019-ncov/lab/guidelines-clinical-specimens.html
- 31.World Health Organization. Antigen-detection in the diagnosis of SARS-CoV-2 infection using rapid immunoassays, 11 de septiembre 2020. Disponible en (consultado el 29/9/2020): https://www.who.int/publications/i/item/antigen-detection-in-the-diagnosis-ofsars-cov-2infection-using-rapid-immunoassays
- 32.Kang H, Wang Y, Tong Z, Liu X. Retest positive for SARS-CoV-2 RNA of “recovered” patients with COVID-19: Persistence, sampling issues, or re-infection? J Med Virol 2020; June 3; 10.1002/jmv.26114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clemency BM, Varughese R, Scheafer DK, et al. . Symptom criteria for COVID-19 testing of heath care workers. Acad Emerg Med 2020; 27:469-474. doi: 10.1111/acem.14009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lan FY, Filler R, Mathew S, et al. . COVID-19 symptoms predictive of healthcare workers’ SARS-CoV-2 PCR results. PLoS One 2020; 15:e0235460. doi: 10.1371/journal.pone.0235460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control. Evidence used to update the list of underlying medical conditions that increase a person’s risk of severe illness from COVID-19, 6 octubre 2020. Disponible en (consul-tado el 10/10/2020): https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html
- 36.Sisó-Almirall A, Kostov B, Mas-Heredia M, et al. . Prognostic factors in Spanish COVID-19 patients: A case series from Barcelona. PLoS ONE 2020; 15:e0237960. doi: 10.1371/journal.pone.0237960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gil-Rodrigo A, Miró Ò, Piñera P, et al. . Analysis of clinical characteristics and outcomes in patients with COVID-19 based on a series of 1000 patients treated in Spanish emergency departments. Evaluación de las características clínicas y evolución de pacientes con COVID-19 a partir de una serie de 1000 pacientes atendidos en servicios de urgencias españoles. Emergencias 2020; 32:233-241. PMid: [PubMed] [Google Scholar]
- 38.Casas-Rojo JM, Antón-Santos JM, Millán-Núñez-Cortés J, et al. . Características clínicas de los pacientes hospitalizados con COVID-19 en España: resultados del Registro SEMI-COVID-19. Rev Clin Esp 2020; Jul 19;S0014-2565(20)30206-X. doi: 10.1016/j.rce.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vageesh J, Yuan JM. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health 2020; 65:533-546. doi: 10.1007/s00038-020-01390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guan W, Liang W, Zhao Y, et al. . Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J 2020; 55:2000547. doi: 10.1183/13993003.00547-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hoang A, Chorath K, Moreira A, et al. . COVID-19 in 7780 pediatric patients: A systematic review. EClin Med 2020; 24:100433. doi: 10.1016/j.eclinm.2020.100433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu X, Zhang L, Du H, et al. . SARS-CoV-2 infection in children. N Engl J Med 2020; 382:1663-1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mak PQ, Chung KS, Wong JS, Shek CC, Kwan MY. Anosmia and ageusia: not an uncommon presentation of COVID-19 infection in children and adolescents. Pediatr Infect Dis J 2020; 39:e199-e200. doi: 10.1097/INF.0000000000002718. [DOI] [PubMed] [Google Scholar]
- 44.Feldstein LR, Rose EB, Horwitz SM, et al. . Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med 2020; 383:334-346. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiang L, Tang K, Levin M, et al. . COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis 2020; 17:S1473-3099. doi: 10.1016/S1473-3099(20)30651-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gruber C, Patel R, Trachtman R, et al. . Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C). Cell 2020; 183:1-14. doi: 10.1016/j.cell.2020.09.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moraleda C, Serna-Pascual M, Soriano-Arandes A, et al. . Multi-inflammatory syndrome in children related to SARS-CoV-2 in Spain. Clin Infect Dis 2020; Jul 25;ciaa1042. doi: 10.1093/cid/ciaa1042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Posfay-Barbe KM, Wagner N, Gauthey M, et al. . COVID-19 in children and the dynamics of Infection in families. Pediatrics 2020; 146:e20201576. doi: 10.1542/peds.2020-1576 [DOI] [PubMed] [Google Scholar]
- 49.Dong L, Tian J, He S, et al. . Possible vertical transmission of SARSCoV-2 from an infected mother to her newborn. JAMA 2020; 323:1846-1848. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liguoro I, Pilotto C, Bonanni M, et al. . SARS-CoV-2 infection in children and newborns: a systematic review. Eur J Pediatr 2020; 179:1029-1046. doi: 10.1007/s00431-020-03684-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.European Center for Disease Control. Latest evidence on COVID-19: diagnostic testing and screening for SARS-CoV-2. Disponible en (consultado el 29/9/2020): https://www.ecdc.europa.eu/en/covid-19/latest-evidence/diagnostic-testing
- 52.Centers for Disease Control. Standard operating procedure (SOP) for triage of suspected COVID-19 patients in non-US healthcare settings: early identification and prevention of transmission during triage, 11 de septiembre 2020. Disponible en (consultado el 29/9/2020): https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/sop-triage-prevent-transmission.html
- 53.World Health Organization. Country & Technical Guidance- Coronavirus disease (COVID-19): public health surveillance for COVID-19: interim guidance, 7 de Agosto de 2020. Disponible en (consultado el 29/9/2020): https://www.who.int/publications/i/item/who-2019-nCoV-surveillanceguidance-2020.7
- 54.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect 2020; 80:e14-18. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]