Abstract
Objective
To assess the association between chemotherapy and prognosis of patients with breast cancer of luminal A subtype and lymph node-positive, luminal A subtype breast cancer
Methods
Articles published between January 1, 2010, and May 1, 2020, were collected from PubMed, Embase, and Web of Science databases. On the basis of a test for heterogeneity, we selected the random effects model or fixed effects model for meta-analysis. Article quality was evaluated by sensitivity analysis, and Begg’s and Egger’s tests were used to measure publication bias.
Results
Six eligible articles were identified. The hazard ratio of overall survival of luminal A breast cancer patients who received both chemotherapy and endocrine therapy was 1.73 (95% CI 1.23, 2.43). The hazard ratio of overall survival for lymph node-positive, luminal A breast cancer patients who received chemotherapy and endocrine therapy was 1.86 and 95% CI 1.26, 2.81. The hazard ratio of relapse-free survival to disease-free survival was 1.30 (95% CI 0.85, 1.77). Tumor size, vascular invasion, and age did not show significant correlations with breast cancer prognosis.
Conclusion
Compared with endocrine therapy alone, the addition of chemotherapy did not improve the prognosis of patients with luminal type A and lymph node positive cancer; instead, side effects of the additional chemotherapy may have negatively affected prognosis. Prospective studies are needed to determine whether the number of positive lymph nodes also correlates with efficacy of chemotherapy of luminal type A breast cancer.
Keywords: Luminal A, Lymph node-positive breast cancer, Prognosis, Meta-analysis
Introduction
Breast cancer is one of the most common cancers of women. In 2019, breast cancer accounted for 30% of female tumors, ranking first in morbidity; mortality was second for female tumors, accounting for about 26.8% [1].
To facilitate identification and treatment of breast cancer with different characteristics, investigators have classified tumors by subgroup according to the expression patterns of genes. This approach has technical limitations, and high cost prevents its wide use. Instead, clinicians more generally use immunohistochemical markers to classify tumors into subtypes [2]. The molecular subtypes recognized immunologically are the following: luminal A, luminal B, basal-like, and HER2 (human epidermis growth factor receptor-2). Molecular typing is related to the clinicopathological and prognostic characteristics of patients [3].
Luminal type A has better prognosis than other breast cancer subtypes. Oncologists define luminal A as estrogen receptor (ER) > 1%, progesterone receptor (PR) ≥ 20%, breast cancer with negative human epidermal growth factor receptor-2 (HER2), and Ki-67 < 14% of clinical cases [4]. Luminal A has high hormone receptor expression, negative HER2 expression, and a low proliferation rate, properties that contribute to its better prognosis [5].
There are three principal treatments for breast cancer: drug treatment, radiotherapy, and surgery. Drug treatment may also include endocrine therapy, drugs that target the HER2 receptor, and chemotherapy. For luminal type A, endocrine therapy is often more applicable [6]. However, there is still controversy about whether oncologists should include chemotherapy for luminal A, lymph node-positive breast cancer. Because lymph node-positive is a high-risk factor, breast cancer patients with positive luminal type A lymph node can benefit from chemotherapy [7, 8]. Other studies have failed to show benefit from chemotherapy for patients with luminal type A. Even in the case of positive lymph nodes, chemotherapy has not improved prognosis significantly [9, 10]. Therefore, it remains to be determined whether chemotherapy has clinical significance for luminal A type, especially for patients with positive lymph nodes. Coates et al. suggested that luminal A requires chemotherapy only when the number of positive lymph nodes is ≥ 4 [11]. The National Comprehensive Cancer Network guidelines recommend that patients with luminal A breast cancer and patients with positive lymph nodes should receive chemotherapy regardless of the number of nodes [12]. Considering this disparity in recommendations, and to identify factors that may affect prognosis, we have analyzed studies of lymph node-positive luminal A breast cancer patients who received chemotherapy. This analysis will provide ideas for clinical treatment plans and assessment of prognosis.
Methods
Search strategy
We searched the PubMed, Embase, and Web of Science databases for research articles published between January 1, 2010, and May 1, 2020. Keywords used in the search were the following: “luminal A”, “breast cancer”, “chemotherapy”, and “lymph node positive”. Eligible research articles must meet the following criteria: (1) research for breast cancer; (2) must include patients with breast type; (3) treatment methods must include chemotherapy and nonchemotherapy; (4) data must include either patient overall survival (OS), relapse-free survival (RFS), or disease-free survival (DFS). The indicator must be either relative risk (RR), odds ratio (OR), or risk ratio (RR) and contain the corresponding 95% confidence interval (CI). OS was defined as the time from the date of diagnosis of breast cancer to the time of death from any cause. The RFS/DFS ratio was defined as the time from the first treatment to progression, recurrence, and death of a patient with breast cancer. For meta-analysis, we used the principles of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Data extraction
The following information was extracted from each article included in the study: first author’s surname, study design, case origin or country in which the study was conducted, follow-up time, number of subjects, type of chemotherapy regimen, assessment outcome indicators and corresponding RR, OR, or HR, and 95% confidence interval. For each study, the treatment group that received only endocrine therapy was set as a reference (nonchemotherapy group). The chemotherapy group referred to the group that received both chemotherapy and endocrine therapy. Chemotherapy was used as the exposure factor. If the articles were grouped according to factors, such as the number of positive lymph nodes, the confidence interval and effect size (relative risk, odds ratio, or hazard ratio) in the groups were also extracted. We stored all extracted information in a well-structured table.
Statistical analysis
We extracted the RR/HR/OR about the prognostic index of luminal A breast cancer from each study. Risk ratio and hazard ratio were regarded as equivalent measures of risk, and the odds ratio value was regarded as the hazard ratio [13, 14]. The heterogeneity of effects between different studies was assessed by an I2 statistical test or Q test, in which I2 < 50 or P < 0.1 of Q test indicated significant heterogeneity [15]. We selected the fixed effect model for meta-analysis according to the results of the test for heterogeneity. We also performed a sensitivity analysis by excluding one study at a time to determine whether the results changed significantly. In addition, we conducted a subgroup analysis to verify the influence of various factors on the relationship between chemotherapy and luminal type A breast cancer in the subgroup analysis. Lastly, we assessed publication bias by using Begg’s funnel plot and Egger’s linear regression. All statistical analyses were performed with Stata 14.0 (StataCorp, College Station, TX, USA).
Results
Literature search and study characteristics
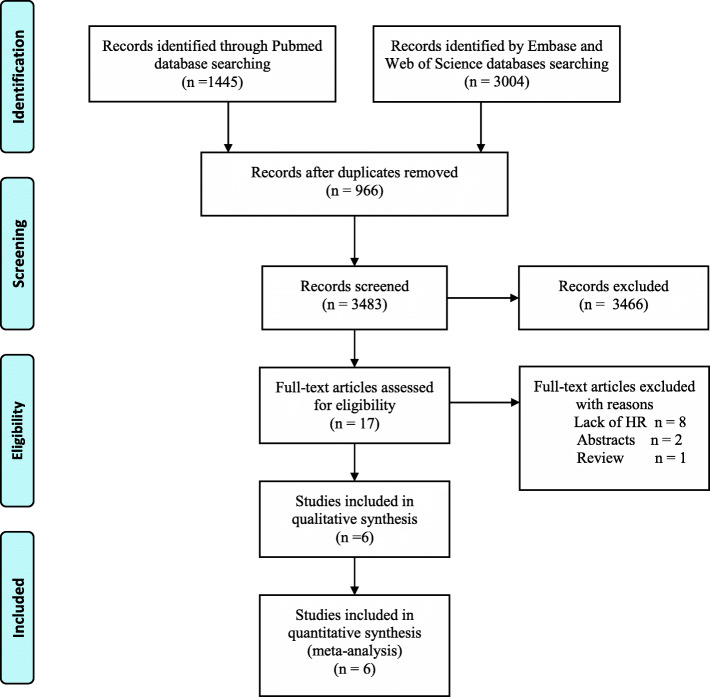
We used the keywords “luminal A”, “breast cancer”, “lymph node positive”, and “chemotherapy” to search the PubMed, Embase, and Web of Science databases. From 4449 articles, we removed 966 duplicates, and 3466 articles were excluded after reviewing the title or abstract (Fig. 1). We read the full text of 17 articles and finally included six articles [10, 16–20]. Table 1 shows the details of these publications.
Fig. 1.
A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of the selection procedure of studies to assess the relationship between chemotherapy and prognosis of luminal A breast cancer
Table 1.
Characteristics of articles in the meta-analysis on chemotherapy and luminal A breast cancer
| Author, year | Country, follow-up (median) | Study design | Sample size | Chemotherapy regimen | Outcome indicators |
|---|---|---|---|---|---|
| Uchida et al.2013 [10] | Japan, 3–113 (40) months | Retrospective study | 140 | FEC × 4/FEC × 4-docetaxel × 4 or paclitaxel × 4 | RFS, OS |
| Kwak et al. 2015 [16] | South Korea, 28–116 (61) months | Retrospective study | 879 | No detail description | DFS, OS |
| Han et al. 2015 [17] | China, 60–89 (67) months | Retrospective cohort study | 1580 | AC × 4/AC × 6 | DFS, OS |
| Nielsen et al. 2016 [18] | UK, 10 years (median) | Clinical trial | 1072 (luminal A n = 165) | C × 12/CMF × 12 | DFS, OS (not provided) |
| Alramadhan et al. 2016 [19] | South Korea, 51.3 ± 18.9(median) | Retrospective study | 406 | AC × 4/FAC × 4 | DFS, OS (not provided) |
| Herr et al. 2019 [20] | Multicenter, - | Retrospective multicenter Study | 1376 | A/AT | RFS, OS |
F fluorouracil, E epirubicin, C cyclophosphamide, A anthracycline, M methotrexate; T Taxane, RFS relapse-free survival, OS overall survival, DFS disease-free survival
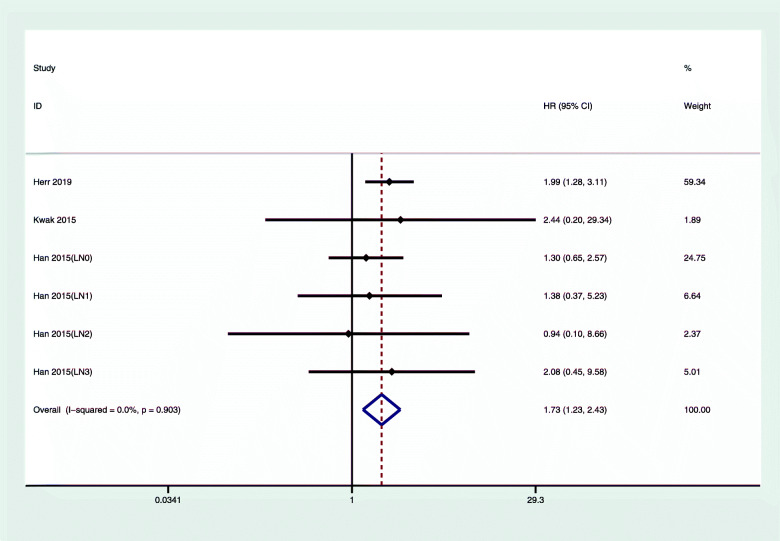
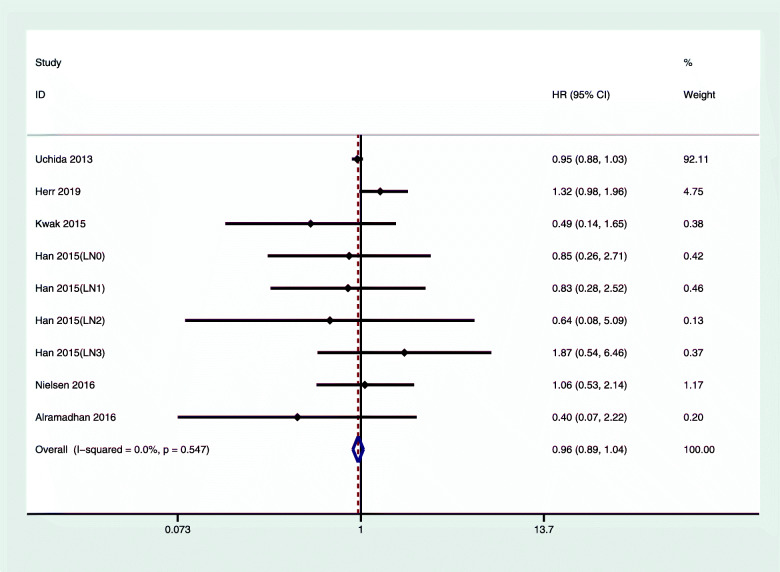
Summary hazard ratio for chemotherapy versus nonchemotherapy for luminal A breast cancer
Figure 2 shows the comparison between chemotherapy and nonchemotherapy treatment. Compared with the nonchemotherapy group, the hazard ratio of OS in luminal type A breast cancer for patients who received chemotherapy was 1.73 (95% CI 1.23, 2.43); we did not observe any obvious heterogeneity (I2 = 0%, P = 0.903). Figure 3 shows that the overall DFS/RFS hazard ratio of luminal type A breast cancer in the chemotherapy group and the nonchemotherapy group was 0.86 (95% CI 0.89, 1.04); we did not observe any obvious heterogeneity.
Fig. 2.
Multivariate-adjusted OS of luminal A breast cancer with chemotherapy versus nonchemotherapy. CI, confidence interval; HR, hazard ratio, OS, overall survival
Fig. 3.
Multivariate-adjusted DFS/RFS of luminal A breast cancer with chemotherapy versus nonchemotherapy. CI, confidence interval; HR, hazard ratio; RFS, relapse-free survival; DFS, disease-free survival
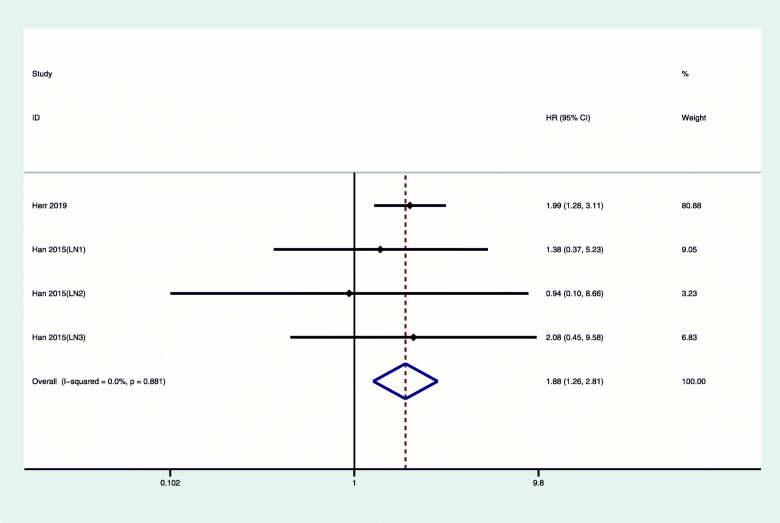
Summary hazard ratio for chemotherapy versus nonchemotherapy for lymph node-positive luminal A breast cancer
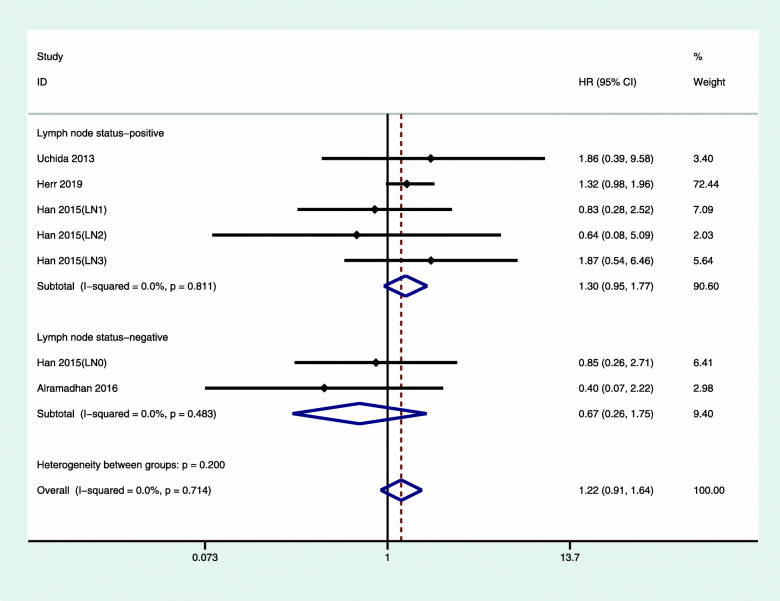
We also analyzed the relationship between chemotherapy and the prognosis of patients with luminal A type breast cancer with positive lymph nodes (Fig. 4). The overall hazard ratio of OS for lymph node-positive luminal A with chemotherapy was 1.86 (95% CI 1.26, 2.81). We did not observe any obvious heterogeneity (I2 = 0%, P = 0.881). Figure 5 shows that the overall hazard ratio of DFS/RFS for lymph node-positive breast cancer treated with chemotherapy was 1.30 (95% CI 0.85, 1.77). For luminal type A, lymph node-negative breast cancer, the overall hazard ratio of DFS/RFS was 0.67, (95% CI 0.85, 1.77), and there was no obvious heterogeneity.
Fig. 4.
Multivariate-adjusted OS of luminal A, lymph node-positive breast cancer with chemotherapy versus nonchemotherapy. CI, confidence interval; HR, hazard ratio, OS, overall survival
Fig. 5.
Multivariate-adjusted DFS/RFS of luminal A breast cancer with chemotherapy versus nonchemotherapy, sorted by lymph node status. CI, confidence interval; HR, hazard ratio; RFS, relapse-free survival; DFS, disease-free survival
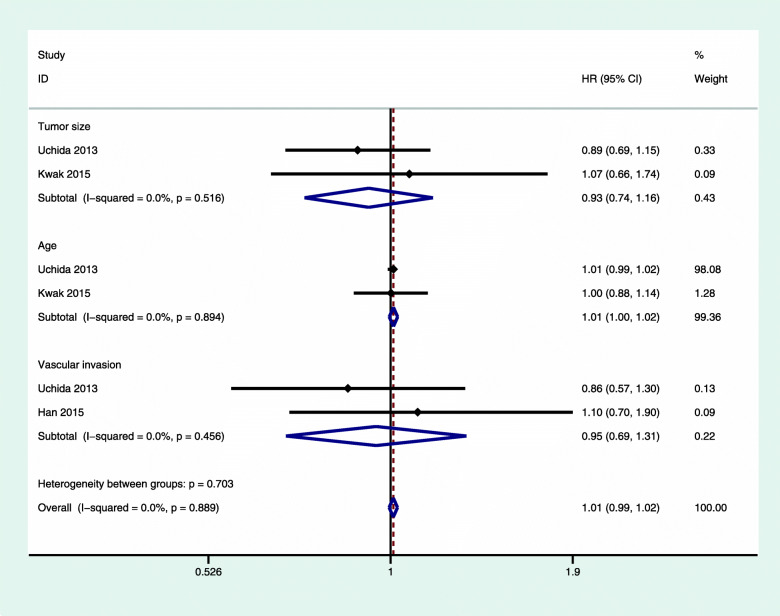
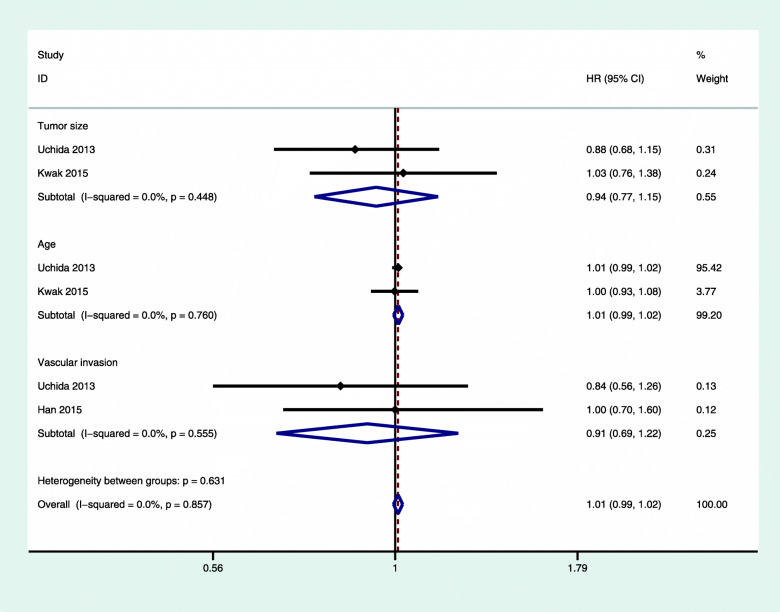
Subgroup analysis of other factors
We also performed a subgroup analysis for the following factors: age, tumor size, and vascular invasion. We did not find a significant correlation in any of these analyses, and we did not observe any significant heterogeneity (Figs. 6 and 7).
Fig. 6.
Subgroup analysis of OS of luminal A breast cancer with chemotherapy versus nonchemotherapy. OS, overall survival; CI, confidence interval; HR, hazard ratio
Fig. 7.
The subgroup analysis of the DFS/RFS of luminal A breast cancer with chemotherapy versus nonchemotherapy. CI, confidence interval; HR, hazard ratio; RFS, relapse-free survival; DFS, disease-free survival
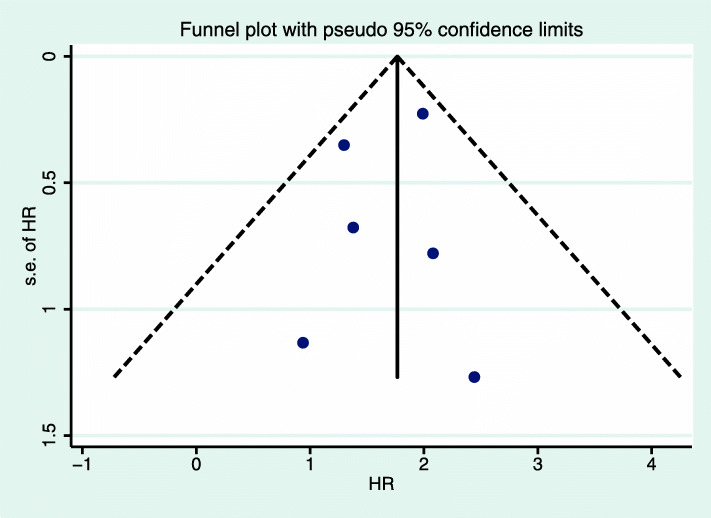
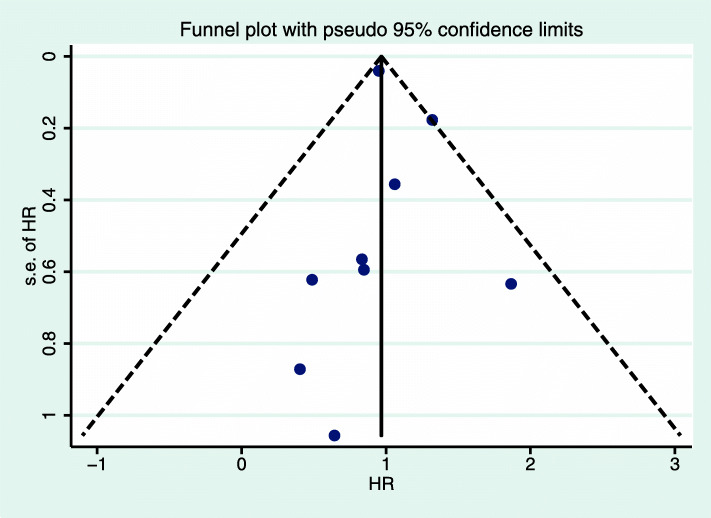
Sensitivity analysis and publication bias
We conducted a sensitivity analysis and found that no study had an excessive effect on the relationship between the prognosis of luminal A breast cancer and chemotherapy. The funnel chart (Figs. 8 and 9) shows that the prognosis of luminal A breast cancer patients was related to chemotherapy (OS: Egger, P = 0.70; Begg, P = 0.61; DFS/RFS: Egger, P = 0.70; Begg, P = 0.75). The analysis did not reveal any publication bias.
Fig. 8.
Funnel plot of OS of luminal A breast cancer with pseudo 95% confidence limits. HR, hazard ratio; OS, overall survival
Fig. 9.
Funnel plot of DFS/RFS of luminal A breast cancer with pseudo 95% confidence limits. HR, hazard ratio; RFS, relapse-free survival; DFS, disease-free survival
Discussion
Chemotherapy is an important treatment for breast cancer. Adjuvant chemotherapy can reduce the recurrence rate [21]. However, because of tumor heterogeneity, chemotherapy of different breast cancer molecular subtypes has different effects [3]. We found that chemotherapy did not improve the OS of patients with luminal A subtype breast cancer (1.73, 95% CI 1.23, 2.43). Interestingly, patients who received only endocrine therapy had better prognosis compared with patients who received both chemotherapy and endocrine therapy, regardless of whether the lymph nodes metastasized (Figs. 2 and 4). The RFS/DFS of luminal A breast cancer patients did not show significant associations, which indicated that chemotherapy did not reduce the risk of disease recurrence.
We analyzed the reasons for these results from several aspects. First, not all lymph node-positive luminal A subtype breast cancer patients are suitable for chemotherapy. The American Society of Clinical Oncology guidelines indicate that low-risk, node-negative breast cancer patients will not benefit from chemotherapy [22]. In addition, Han et al. reported that when the number of positive lymph nodes was ≥ 4 patients should receive chemotherapy [17]. Herr et al. verified this conclusion. When the number of lymph node positives was ≥ 4, the OS of patients after chemotherapy improved, whereas 1–3 lymph node-positive patients with luminal A breast cancer did not have improved prognosis after chemotherapy [20]. The National Surgical Adjuvant Breast and Bowel Project B20 and Southwest Oncology Group 8814 found that not all patients with lymph node-positive luminal A subtype breast cancer benefited from chemotherapy. Both studies showed that Oncotype DX 21-gene recurrence score determined whether chemotherapy was needed [23, 24]. The Southwest Oncology Group 8814 study showed that postmenopausal women with lymph node-positive luminal A subtype breast cancer with low (< 18) or moderate (18 < RS < 31) recurrence scores did not benefit from chemotherapy [23]. Park et al. reported that chemotherapy did not significantly improve the prognosis of patients with luminal A, lymph node-positive breast cancer [25].
Second, the side effects of chemotherapy negatively affect prognosis. Older patients have diminished tolerance to chemotherapy. In a clinical trial, Muss et al. showed that, compared with patients aged ≤ 50 years (< 0.001), patients aged > 65 years who received chemotherapy had higher likelihoods of developing grade 4 hematologic toxicity [26]. Older patients have a higher prevalence of comorbidities and functional decline. These conditions impair survival, especially survival of patients who received chemotherapy [27, 28]. For elderly patients, the side effects of chemotherapy cancel the benefits.
Regarding the relationship between lymph node positivity and breast cancer prognosis, in some cases, lymph node positivity will affect the prognosis of breast cancer. For example, when the lymph node is positive, extra-lymph node invasion is an important factor that affects prognosis. Some investigators found that the poor prognosis may be related to the invasion of tumor cells into adipose tissue around lymph nodes [29–31]. In addition, tumor markers can also predict the prognosis of lymph node metastasis in breast cancer. The silent mating type information regulation 2 homolog 1, a tumor suppressor, can inhibit lymph node metastasis by activating cysteine aspartate protease 3 [32]. However, breast cancer prognosis is not always related to lymph node positivity. Shigematsu et al. found that when the sentinel lymph node metastasis was detected in patients with cT1-2N0M0 lymph node metastasis did not affect the RFS [33].
Age is a factor in the treatment of breast cancer because age is associated with the effectiveness and tolerance of chemotherapy drugs. Delgado-Ramos et al. showed that chemotherapy could be used effectively in older women with early-stage breast cancer, and chemotherapy was well-tolerated, with few life-threatening or fatal toxic reactions [27]. Haque et al. found that people aged > 50 were more likely to benefit from chemotherapy and have longer OS [34]. Contrary to the Delgado-Ramos study, we found that age did not affect the relationship between prognosis of luminal A, lymph node-positive patients and chemotherapy. This difference may be related to molecular typing, and we need more research to test that idea.
Tumor size is often associated with prognosis. Kustic et al. showed that, in nonluminal A breast cancer, large tumor size was associated with poor prognosis and adversely affected DFS and OS [35]. In luminal type A breast cancer, many studies have failed to find association between tumor size and prognosis, regardless of lymph node positivity [10, 19, 20]. Similarly, we did not find association between tumor size and prognosis.
Vascular invasion is another factor that influences the course of breast cancer. In a meta-analysis, Zhang et al. showed that lymphatic vessel invasion was a predictor of lymph node metastasis, and peritumoral vessels and lymphatic vessels were important means of lymph node metastasis [36]. We assessed vascular invasion and found that, in luminal A, lymph node-positive breast cancer, vascular invasion did not significantly affect the relationship between chemotherapy and breast cancer prognosis.
Our study had some limitations. Although we checked for heterogeneity and publication bias to ensure the accuracy of the study, more research is needed because of the small number of articles that we surveyed. In addition, we did not analyze the effect of the number of positive lymph nodes on prognosis. Further study is needed on this issue as well.
Conclusion
We found that chemotherapy for luminal type A, lymph node-positive breast cancer did not improve OS or RFS/DFS. Instead, the side effects of additional chemotherapy may jeopardize prognosis. Whether the number of positive lymph nodes also affects the outcome of chemotherapy remains to be assessed with prospective studies.
Acknowledgments
The authors thank AiMi Academic Services (www.aimieditor.com) for English language editing and review services.
Abbreviations
- ER
Estrogen receptor
- PR
Progesterone receptor
- HER2
Human epidermis growth factor receptor-2
- NCCN
The National Comprehensive Cancer Network
- OS
Overall survival
- RFS
Relapse-free survival
- DFS
Disease-free survival
- RR
Relative risk
- HR
Hazard ratio
- OR
Odds ratio
- CI
Confidence interval
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- F
Fluorouracil
- E
Epirubicin
- C
Cyclophosphamide
- A
Anthracycline
- M
Methotrexate
- T
Taxane
- SIRT1
The silent mating type information regulation 2 homolog 1
Authors’ contributions
Conceptualization: Li Ma, Yilun Li. Data curation: Yilun Li, Li Ma. Project administration: Yilun Li, Li Ma. Writing-original draft: Yilun Li, Li Ma Writing-review and editing: Li Ma. The authors read and approved the final manuscript.
Funding
Not applicable
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the published articles cited in the text.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors report no conflicts of interest regarding the content herein.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Callagy G, Cattaneo E, Daigo Y, Happerfield L, Bobrow LG, Pharoah PD, Caldas C. Molecular classification of breast carcinomas using tissue microarrays. Diagn Mol Pathol. 2003;12:27–34. doi: 10.1097/00019606-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ. Strategies for subtypes--dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–1747. doi: 10.1093/annonc/mdr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, Senn HJ. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24:2206–2223. doi: 10.1093/annonc/mdt303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stenmark Tullberg A, Lundstedt D, Olofsson Bagge R, Karlsson P. Positive sentinel node in luminal A-like breast cancer patients - implications for adjuvant chemotherapy? Acta Oncol. 2019;58:162–167. doi: 10.1080/0284186X.2018.1533647. [DOI] [PubMed] [Google Scholar]
- 6.Al-Mahayri ZN, Patrinos GP, Ali BR. Toxicity and pharmacogenomic biomarkers in breast cancer chemotherapy. Front Pharmacol. 2020;11:445. doi: 10.3389/fphar.2020.00445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Twelves C, Jove M, Gombos A, Awada A. Cytotoxic chemotherapy: still the mainstay of clinical practice for all subtypes metastatic breast cancer. Crit Rev Oncol Hematol. 2016;100:74–87. doi: 10.1016/j.critrevonc.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 8.Sun Y, Liu X, Cui S, Li L, Tian P, Liu S, Li Y, Yin M, Zhang C, Mao Q, Wang J. The inconsistency of molecular subtypes between primary foci and metastatic axillary lymph nodes in luminal A breast cancer patients among Chinese women, an indication for chemotherapy? Tumour Biol. 2016;37:9555–9563. doi: 10.1007/s13277-016-4844-1. [DOI] [PubMed] [Google Scholar]
- 9.Taskaynatan H, Kucukzeybek Y, Alacacioglu A, Yildiz Y, Salman T, Oflazoglu U, Varol U, Bolat Kucukzeybek B, Kemal Atahan M, Oktay Tarhan M. Is adjuvant chemotherapy necessary for luminal A-like breast cancer? J buon. 2018;23:877–882. [PubMed] [Google Scholar]
- 10.Uchida N, Suda T, Ishiguro K. Effect of chemotherapy for luminal a breast cancer. Yonago Acta Med. 2013;56:51–56. [PMC free article] [PubMed] [Google Scholar]
- 11.Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, Thürlimann B, Senn HJ. Tailoring therapies--improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015;26:1533–1546. doi: 10.1093/annonc/mdv221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gradishar WJ, Anderson BO, Abraham J, Aft R, Agnese D, Allison KH, Blair SL, Burstein HJ, Dang C, Elias AD, et al. Breast cancer, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18:452–478. doi: 10.6004/jnccn.2020.0016. [DOI] [PubMed] [Google Scholar]
- 13.Bradburn MJ, Deeks JJ, Berlin JA, Russell Localio A. Much ado about nothing: a comparison of the performance of meta-analytical methods with rare events. Stat Med. 2007;26:53–77. doi: 10.1002/sim.2528. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li XJ, Ren ZJ, Qin JW, Zhao JH, Tang JH, Ji MH, Wu JZ. Coffee consumption and risk of breast cancer: an up-to-date meta-analysis. PLoS One. 2013;8:e52681. doi: 10.1371/journal.pone.0052681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwak HY, Chae BJ, Eom YH, Hong YR, Seo JB, Bae JS, Jung SS, Song BJ. Is adjuvant chemotherapy omissible in women with T1-2 stage, node-positive, luminal A type breast cancer? J Chemother. 2015;27:290–296. doi: 10.1179/1973947815Y.0000000015. [DOI] [PubMed] [Google Scholar]
- 17.Han Y, Li Q, Xu BH, Zhang P, Yuan P, Wang JY, Ma F, Cai RG, Fan Y. Adjuvant chemotherapy may improve survival of patients with luminal A breast cancer and positive lymph nodes. Genet Mol Res. 2015;14:8563–8573. doi: 10.4238/2015.July.31.4. [DOI] [PubMed] [Google Scholar]
- 18.Nielsen TO. Jensen MB, Burugu S, Gao D, Jørgensen CL, Balslev E, Ejlertsen B. High-risk premenopausal luminal A breast cancer patients derive no benefit from adjuvant cyclophosphamide-based chemotherapy: results from the DBCG77B clinical trial. Clin Cancer Res. 2017;23:946–953. doi: 10.1158/1078-0432.CCR-16-1278. [DOI] [PubMed] [Google Scholar]
- 19.Alramadhan M, Ryu JM, Rayzah M, Nam SJ, Kim SW, Yu J, Lee SK, Bae SY, Park S, Paik HJ, Lee JE. Goserelin plus tamoxifen compared to chemotherapy followed by tamoxifen in premenopausal patients with early stage-, lymph node-negative breast cancer of luminal A subtype. Breast. 2016;30:111–117. doi: 10.1016/j.breast.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 20.Herr D, Wischnewsky M, Joukhadar R, Chow O, Janni W, Leinert E, Fink V, Stüber T, Curtaz C, Kreienberg R, et al. Does chemotherapy improve survival in patients with nodal positive luminal A breast cancer? A retrospective multicenter study. PLoS One. 2019;14:e0218434. doi: 10.1371/journal.pone.0218434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717. [DOI] [PubMed]
- 22.Burstein HJ, Lacchetti C, Griggs JJ. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline update on ovarian suppression summary. J Oncol Pract. 2016;12:390–393. doi: 10.1200/JOP.2016.011239. [DOI] [PubMed] [Google Scholar]
- 23.Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, Cronin M, Baehner FL, Watson D, Bryant J, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–3734. doi: 10.1200/JCO.2005.04.7985. [DOI] [PubMed] [Google Scholar]
- 24.Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh IT, Ravdin P, Bugarini R, Baehner FL, Davidson NE, et al. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010;11:55–65. doi: 10.1016/S1470-2045(09)70314-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park S, Lee SK, Paik HJ, Ryu JM, Kim I, Bae SY, Yu J, Kim SW, Lee JE, Nam SJ. Adjuvant endocrine therapy alone in patients with node-positive, luminal A type breast cancer. Medicine (Baltimore) 2017;96:e6777. doi: 10.1097/MD.0000000000006777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muss HB, Berry DA, Cirrincione C, Budman DR, Henderson IC, Citron ML, Norton L, Winer EP, Hudis CA. Toxicity of older and younger patients treated with adjuvant chemotherapy for node-positive breast cancer: the Cancer and Leukemia Group B Experience. J Clin Oncol. 2007;25:3699–3704. doi: 10.1200/JCO.2007.10.9710. [DOI] [PubMed] [Google Scholar]
- 27.Delgado-Ramos GM, Nasir SS, Wang J, Schwartzberg LS. Real-world evaluation of effectiveness and tolerance of chemotherapy for early-stage breast cancer in older women. Breast Cancer Res Treat. 2020;182:247–258. doi: 10.1007/s10549-020-05684-5. [DOI] [PubMed] [Google Scholar]
- 28.Read WL, Tierney RM, Page NC, Costas I, Govindan R, Spitznagel EL, Piccirillo JF. Differential prognostic impact of comorbidity. J Clin Oncol. 2004;22:3099–3103. doi: 10.1200/JCO.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 29.van la Parra RF, Peer PG, Ernst MF, Bosscha K. Meta-analysis of predictive factors for non-sentinel lymph node metastases in breast cancer patients with a positive SLN. Eur J Surg Oncol. 2011;37:290–299. doi: 10.1016/j.ejso.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 30.Shigematsu H, Taguchi K, Koui H, Ohno S. Clinical significance of extracapsular invasion at sentinel lymph nodes in breast cancer patients with sentinel lymph node involvement. Ann Surg Oncol. 2015;22:2365–2371. doi: 10.1245/s10434-014-4269-2. [DOI] [PubMed] [Google Scholar]
- 31.Verheuvel NC, van den Hoven I, Ooms HW, Voogd AC, Roumen RM. The role of ultrasound-guided lymph node biopsy in axillary staging of invasive breast cancer in the post-ACOSOG Z0011 trial era. Ann Surg Oncol. 2015;22:409–415. doi: 10.1245/s10434-014-4071-1. [DOI] [PubMed] [Google Scholar]
- 32.Kim H, Lee KH, Park IA, Chung YR, Im SA, Noh DY, Han W, Moon HG, Jung YY, Ryu HS. Expression of SIRT1 and apoptosis-related proteins is predictive for lymph node metastasis and disease-free survival in luminal A breast cancer. Virchows Arch. 2015;467:563–570. doi: 10.1007/s00428-015-1815-7. [DOI] [PubMed] [Google Scholar]
- 33.Shigematsu H, Nishina M, Yasui D, Hirata T, Ozaki S. Minimal prognostic significance of sentinel lymph node metastasis in patients with cT1-2 and cN0 breast cancer. World J Surg Oncol. 2019;17:41. doi: 10.1186/s12957-019-1585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haque W, Verma V, Hatch S, Klimberg VS, Butler EB, Teh BS. Omission of chemotherapy for low-grade, luminal A N1 breast cancer: patterns of care and clinical outcomes. Breast. 2018;41:67–73. doi: 10.1016/j.breast.2018.06.014. [DOI] [PubMed] [Google Scholar]
- 35.Kustic D, Lovasic F, Belac-Lovasic I, Avirovic M, Ruzic A, Petretic-Majnaric S. Impact of HER2 receptor status on axillary nodal burden in patients with non-luminal A invasive ductal breast carcinoma. Rev Med Chil. 2019;147:557–567. doi: 10.4067/S0034-98872019000500557. [DOI] [PubMed] [Google Scholar]
- 36.Zhang S, Zhang D, Yi S, Gong M, Lu C, Cai Y, Tang X, Zou L. The relationship of lymphatic vessel density, lymphovascular invasion, and lymph node metastasis in breast cancer: a systematic review and meta-analysis. Oncotarget. 2017;8:2863–2873. doi: 10.18632/oncotarget.13752. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the published articles cited in the text.