Abstract
Background
Existing literatures demonstrated that meteorological factors could be of importance in affecting the spread patterns of the respiratory infectious diseases. However, how ambient temperature may influence the transmissibility of COVID-19 remains unclear.
Objectives
We explore the association between ambient temperature and transmissibility of COVID-19 in different regions across China.
Methods
The surveillance data on COVID-19 and meteorological factors were collected from 28 provincial level regions in China, and estimated the instantaneous reproductive number (Rt). The generalized additive model was used to assess the relationship between mean temperature and Rt.
Results
There were 12,745 COVID-19 cases collected in the study areas. We report the associated effect of temperature on Rt is likely to be negative but not of statistical significance, which holds for most Chinese regions.
Conclusions
We found little statistical evidence for that the higher temperature may reduce the transmissibility of COVID-19. Since intensive control measures against the COVID-19 epidemics were implemented in China, we acknowledge this may impact the underlying effect size estimation, and thus cautiousness should be taken when interpreting our findings.
Keywords: COVID-19, Ambient temperature, Transmissibility, Ecological association
Highlights
-
•
We explored the association between ambient temperature and COVID-19 in different regions across China.
-
•
To avoid the noncausal association on infectious disease, the R t is calculated to quantify the transmissibility of COVID-19.
-
•
We find little evidence that supports the association between temperature and the transmissibility of COVID-19.
-
•
It appears unlikely to mitigate the COVID-19 outbreaks relying on the change in temperature.
1. Introduction
Meteorological factors, e.g., ambient temperature, may be of importance in affecting the spread of infectious diseases. Dengue fever and malaria increase in morbidity as temperature rise around the world could be typical examples (Watts et al., 2019). The seasonal outbreaks of influenza in cold months also exemplify partly relationship between meteorological factors and infectious diseases (Lowen; et al., 2007). In the end of 2019, a new coronavirus caused by SARS-CoV-2 (or formerly, 2019-nCoV), can make humans suffer from atypical pneumonia, as one of the serious types of coronavirus disease 2019 (COVID-19) (Chen et al., 2020a; Lu et al., 2020). Compared to the severe acute respiratory syndrome (SARS) during 2002–03 (Drosten et al., 2003), COVID-19 shares genetic similarities with SARS but has stronger infectiousness and has been bringing about unprecedented damage globally. Motivated by the researchers found there was an inverse relationship between temperature and SARS (Cai et al., 2007), it is tempting to assume that such association could apply to COVID-19 as well, which may provide the region-specific prevention measures.
Earlier research on this issue in China including over 400 cities (Wang et al., 2020) found there was a non-linear relationship between temperature and cumulative number of cases, they found that as the temperature rise, the transmissibility rise first and then fall. Another study also found a non-linear relationship between temperature and daily cases of COVID-19, but they suggested that the infected cases would continue to increase in spite of rising temperature, which implies that the rising temperature may only reduce the growth rate of disease (Xie and Zhu, 2020). In addition, previous work investigated the association between the basic reproductive number and the weather conditions, however, they did not detect any evident association (Yao et al., 2020). Ran et al. (2020) explored the association between temperature and COVID-19 transmissibility with an ecological study design, and they found that the overall nonlinear association between basic reproductive number and temperature was of statistical significance. As such, how ambient temperature may influence the transmissibility of COVID-19 remains unclear.
Many studies on this issue considered the city of Wuhan (or Hubei province) as the target region, this may involve some bias in analysis. One of the main reasons is that there were numerous confirmed cases in Wuhan (or Hubei) compared to other Chinese regions, and such difference may affect the inference of role of temperature in COVID-19 transmission. In addition, the settings of medical resources and control interventions in Hubei and the other regions in China appear different, which may also affect the inference of association between air temperature and COVID-19 morbidity.
In this study, we aim to explore the association of temperatures with risks of transmissibility on COVID-19 outside Hubei in China. In view of the influence on different demographic and geographic characteristics, China was divided into seven regions according to Chinese Geographical Division. The generalized additive model was used to assess the relationship between mean temperature and reproductive number, R t. Furthermore, we perform the sensitivity analysis to test the robustness of the results. We further discussion the public health relevance of our estimates.
2. Materials and methods
2.1. Study regions
According to Chinese Geographical Division, China is divided into seven regions (Fig. 1 ), there are East China (Anhui, Fujian, Jiangsu, Jiangxi, Shandong, Shanghai, Taiwan and Zhejiang), North China (Beijing, Hebei, Inner Mongolia, Shanxi, and Tianjin), Central China (Henan, Hubei and Hunan), South China (Guangdong, Guangxi, Hainan, Hong Kong and Macao), Northeast China (Heilongjiang, Jilin and Liaoning), Northwest China (Gansu, Ningxia, Qinghai, Shannxi and Xinjiang), and Southwest China (Chongqing, Guizhou, Sichuan, Tibet and Yunnan).
Fig. 1.
Map of Chinese regions included or excluded in this study. Different colors represent different regions. White colors indicate that the data in these areas were not used. Tibet is classified in Southwest China. Hubei is classified in Central China. Hainan, Hong Kong and Macao are classified in South China. Taiwan is classified in East China.
We selected a total of 28 Chinese provincial regions as study place in this work. Since Wuhan (in Hubei province, China) was the epicenter of COVID-19 in China, where relatively intensive control measures were implemented, we avoid including COVID-19 data in Hubei province. Moreover, there were enormously larger number of cases in Wuhan than other cities, so it may be inappropriate for comparison among these regions. Besides, we excluded these cities from analysis, and they include Hong Kong, Hainan, and Taiwan for unavailable meteorological data, and Tibet for lack of COVID-19 case.
2.2. Data collection
The surveillance data of COVID-19 number of cases were collected from the reports released on the official websites of the Health Commissions. We collected case data from January 20 to February 29, 2020, for two reasons: (i) in almost all regions outside Hubei, the first case was reported in January 20, 2020, and nearly ended up in February 29, 2020 (Table S1), and (ii) to compare with the results from other similar studies that also choose this period of time (Ma et al., 2020; Oliveiros, 2020).
Meteorological data were collected from Houzhi Weather (see http://hz.zc12369.com) during the same time period for each city, including mean temperature (in °C), relative humidity (in %), air pressure (in hpa), and wind speed (in m per s, or m/s).
2.3. Transmissibility of COVID-19
We quantify the transmissibility of COVID-19 by using the number of incidences time series and serial interval (SI) that is defined as the time between the onset of symptoms in a primary case and the onset of symptoms of secondary cases (Cori et al., 2013, Fine, 2003). The statistical framework for estimating the instantaneous reproductive number R t at the t-th day has following formula (Ferretti et al., 2020; Thompson et al., 2019):
where is the confirmed case of COVID-19 at the t-th day, is the weighted sum of infection incidence up to the time step , and is the weighted function determined by the distribution of SI of COVID-19, and denotes the upper bound of the SI distribution (in days). The estimation of R t is conducted with a Poisson-distributed likelihood profile for the number of incidences. To set up the model, the distribution of SI used to estimate R t was approximated by a Gamma distribution with mean 5.5 days and standard deviation (SD) 3.3 days (Zhao, 2020).
2.4. Statistical analysis
Statistical analyses mainly consisting of the following two steps: (i) as (Zhao, 2020) pointed out that there may exist flawed analytical procedures by directly using the case number as response to modeling the temperature-morbidity relationship for infectious diseases, thus, we estimated instantaneous reproductive number (R t) as the proxy of the transmissibility of COVID-19. (ii) A generalized additive model (GAM) was built with log (R t) as a function of mean temperature (linear) and other meteorological variables (natural cubic spline) at city-specific level, then combining the city-level results to the region-level with meta-analysis, we calculated the relative risk (RR) of each region with different lag days. The model is described as follows:
| (1) |
where is the interception, is the mean temperature on the t-th day. The , and are relative humidity, air pressure and wind speed on the t-th day, respectively. The function denotes the natural cubic spline function with degrees of freedom (df) fixed at 3. The is the day of week, a categorical variable with coefficient γ. Considering the autocorrelation of time series data, we added the term to adjust for the autocorrelation.
The relative risk (RR) and its 95% confidence interval (95% CI) were employed to measure the association between temperature and the COVID-19 transmissibility (R t) by using the generalized additive model. We respectively calculated the effects of the current day, lag for 1 day, lag for 2 days, lag for 3 days and their moving averages by using generalized additive model.
2.5. Sensitivity analysis
To test the robustness of the results, we performed the sensitivity analyses as follows: (i) We used daily maximum and minimum temperatures as the interested indicators to explore the temperature-disease relationships, respectively. (ii) The model is also applied for the whole studied areas by using mean, maximum and minimum temperature, respectively. (iii) We extended the endpoint of study period from February 29, 2020 to April 30, 2020. (iv) Additionally, considering the Baidu Index (BDI) may be an effective proxy to measure public awareness, which may affect public behavior (Zhao et al., 2020), we used BDI as a covariate in model (1) to adjust the potential effect of human behavior (public awareness). The more details with respect to BDI were given in the supplementary materials.
Data analyses were conducted in R statistical software (version 4.0.2).
3. Results
During the study period, there were 12,745 COVID-19 cases collected in total, among which the most cases existed in East China (5150), and were roughly 10 times of the cases in Northwest China that had the least number of cases (503). The two warmest regions were South China and Southwest China, which the average daily mean temperatures exceeded 10 °C (16.0 and 10.4, respectively). The coldest region was Northeast China (−8.4). For other regions, the temperatures from high to low followed by East (8.4), Central (7.5), North (−0.7) and Northwest (−1.3). Details of statistics of confirmed cases of COVID-19 and other meteorological variables shows in Table 1 .
Table 1.
Summary of meteorological variables, released COVID-19 cases in different regions of China.
| Region | City | Cum. Of Cases | Average temperature (°C) |
Relative humidity (%) |
Wind speed (m/s) |
Air pressure (hpa) |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| East China | Anhui | 990 | 6.5 (3.4) | 78.2 (12.4) | 2.4 (0.9) | 1007.6 (4.5) |
| Fujian | 296 | 14.1 (3.5) | 72.6 (12.6) | 1.5 (0.4) | 1007.2 (3.9) | |
| Jiangsu | 631 | 6.8 (3.0) | 74.4 (12.8) | 2.0 (0.8) | 1024.1 (4.8) | |
| Jiangxi | 935 | 10.5 (4.0) | 78.6 (11.6) | 1.4 (0.5) | 1011.9 (4.6) | |
| Shandong | 756 | 3.4 (3.5) | 65.4 (12.1) | 2.3 (0.7) | 1006.8 (5.0) | |
| Shanghai | 337 | 8.1 (3.3) | 76.6 (13.7) | 2.0 (0.9) | 1025.4 (4.7) | |
| Zhejiang | 1205 | 9.7 (3.3) | 76.5 (12.8) | 1.7 (0.7) | 1021.3 (4.6) | |
| Regional cases | 5150 | |||||
| North China | Beijing | 413 | 0.8 (2.9) | 55.3 (17.8) | 1.4 (0.9) | 1022.9 (5.5) |
| Hebei | 318 | 1.1 (3.0) | 60.9 (13.0) | 1.6 (0.6) | 1007.3 (5.5) | |
| Inner Mongolia | 75 | −7.4 (4.6) | 55.1 (7.5) | 2.1 (0.6) | 916.4 (4.5) | |
| Shanxi | 133 | 0.3 (2.9) | 54.1 (15.0) | 1.6 (0.8) | 926.9 (4.6) | |
| Tianjin | 136 | 1.5 (3.0) | 64.7 (16.0) | 1.8 (1.1) | 1026.6 (5.8) | |
| Regional cases | 1075 | |||||
| Central China | Henan | 1272 | 5.4 (3.3) | 66.9 (16.5) | 2.0 (0.6) | 1007.2 (5.3) |
| Hunan | 1018 | 9.5 (3.9) | 81.7 (12.4) | 1.4 (0.8) | 1003.5 (4.9) | |
| Regional cases | 2290 | |||||
| South China | Guangdong | 1349 | 16.6 (3.6) | 75.4 (12.2) | 1.7 (0.6) | 1014.5 (3.6) |
| Guangxi | 249 | 15.4 (4.3) | 75.4 (14.2) | 1.9 (0.6) | 1006.2 (4.1) | |
| Total case | 1598 | |||||
| Northeast China | Heilongjiang | 480 | −13.0 (4.5) | 63.2 (6.3) | 1.9 (0.6) | 999.9 (5.1) |
| Jilin | 93 | −9.0 (5.8) | 65.7 (7.6) | 1.7 (0.7) | 997.1 (5.2) | |
| Liaoning | 122 | −3.3 (4.7) | 58.8 (11.7) | 2.3 (1.0) | 1016.7 (5.2) | |
| Regional cases | 695 | |||||
| Northwest China | Gansu | 91 | −0.7 (3.6) | 42.3 (11.1) | 1.6 (0.5) | 855.6 (3.8) |
| Ningxia | 73 | −0.3 (3.9) | 42.2 (12.4) | 1.6 (0.9) | 876.8 (4.4) | |
| Qinghai | 18 | −1.5 (3.6) | 36.8 (12.0) | 1.9 (0.7) | 789.8 (3.5) | |
| Shannxi | 245 | 3.2 (3.2) | 52.3 (15.6) | 1.8 (0.7) | 944.9 (5.4) | |
| Xinjiang | 76 | −7.1 (5.5) | 68.2 (6.7) | 1.0 (0.3) | 964.2 (4.9) | |
| Regional cases | 503 | |||||
| Southwest China | Chongqing | 576 | 10.7 (2.0) | 80.0 (10.3) | 0.7 (0.6) | 991.4 (5.2) |
| Guizhou | 146 | 9.2 (3.7) | 78.5 (6.5) | 1.2 (0.4) | 891.2 (3.7) | |
| Sichuan | 538 | 10.3 (2.3) | 73.5 (9.2) | 1.0 (0.4) | 965.1 (4.7) | |
| Yunnan | 174 | 10.5 (2.5) | 61.8 (6.6) | 1.5 (0.2) | 821.3 (2.5) | |
| Regional cases | 1434 | |||||
| Total cases | 12,745 | |||||
As Table 2 shows, the estimated reproductive number ranges from 1.1 to 1.5 across Chinese regions, and the virus was more infectious in East China, while in the North China was weaker.
Table 2.
Summary of estimated instantaneous reproductive number (Rt) in different regions, China from January 2020 to February 2020.
| Chinese Region | Mean | 25% percentile | Median | 75% percentile |
|---|---|---|---|---|
| East | 1.5 | 0.5 | 0.7 | 1.7 |
| North | 1.3 | 0.4 | 0.8 | 1.6 |
| Central | 1.3 | 0.2 | 0.6 | 1.6 |
| South | 1.2 | 0.3 | 0.6 | 1.8 |
| Northeast | 1.2 | 0.4 | 0.7 | 2.2 |
| Northwest | 1.1 | 0.3 | 0.7 | 1.4 |
| Southwest | 1.2 | 0.4 | 0.7 | 1.4 |
There were some estimated results of the reproductive number of COVID-19 of China recently. For example, Ran et al. (2020) estimated the reproductive number for the 154 cities (15 inside Hubei and 139 outside Hubei) from December 2019 to February 2020 have a mean ± standard deviation of 1.4 ± 0.3. Yao et al. (2020) also given an estimation of the reproductive number in 62 Chinese cities was 1.4 ± 0.3. Thus, our estimated reproductive number of COVID-19 was largely consistent with these reported works.
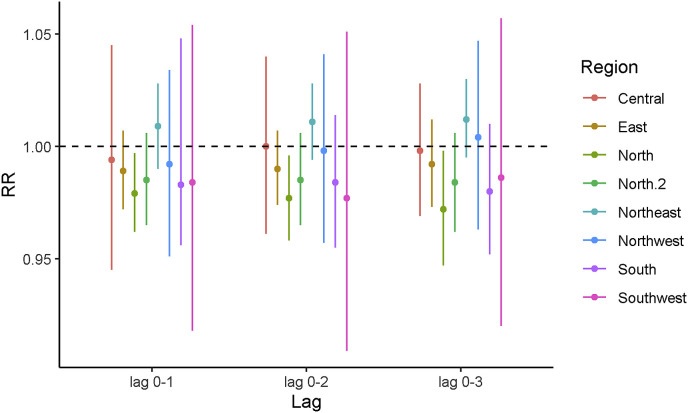
Table 3 shows the delayed effects of mean temperature on the transmissibility of COVID-19. Almost all the estimated RR in different regions (except North China) with different lag days were nearly 1, and their estimated confidence intervals crossed 1. While in North China, the weak effect was found at lag 1 day (RR: 0.981, 95% CI: 0.964–0.999) and lag 2 day (RR: 0.982, 95% CI: 0.965–0.999). These results indicated that the association between the mean temperature and transmissibility of COVID-19 is not statistically clear.
Table 3.
Summary of the relative risks (RR) and 95% confidence intervals (CI) for COVID-19 associated with one unit increase in mean temperatures at different lag days in different regions of China.
| Chinese Region | RR (95% CI) |
|||
|---|---|---|---|---|
| Lag 0 | Lag 1 | Lag 2 | Lag 3 | |
| East | 0.988 (0,970, 1.006) | 0.996 (0.983, 1.009) | 0.996 (0.981, 1.011) | 0.994 (0.964, 1.026) |
| North | 0.981 (0.964, 0.999) | 0.982 (0.965, 0.999) | 0.987 (0.972, 1.002) | 0.989 (0.973, 1.004) |
| Central | 0.995 (0.947, 1.046) | 0.999 (0.968, 1.030) | 1.001 (0.998, 1.014) | 0.997 (0.985, 1.010) |
| South | 0.984 (0.956, 1.012) | 0.990 (0.970, 1.011) | 0.997 (0.981, 1.013) | 0.993 (0.974, 1.011) |
| Northeast | 1.002 (0.980, 1.023) | 1.000 (0.996, 1.002) | 1.009 (0.997, 1.022) | 0.991 (0.953, 1.030) |
| Northwest | 0.988 (0.949, 1.029) | 0.998 (0.969, 1.027) | 1.007 (0.986, 1.028) | 1.005 (0.988, 1.022) |
| Southwest | 0.988 (0.932, 1.047) | 0.988 (0.933, 1.047) | 0.933 (0.963, 1.023) | 1.005 (0.973, 1.038) |
Fig. 2 shows the temperature moving average effect. Similar as in Table 2, the significant result only found in North China. However, the correlation of temperature and COVID-19 becomes insignificant when we excluded Inner Mongolia (The corresponding values of RR and their 95% CI, see Table S5).
Fig. 2.
Relative risks (point) and 95% confidence intervals (bar) for COVID-19 associated with different moving average, per one unit (in °C) increase in temperature. The label ‘North.2’ indicates North China without Inner Mongolia.
For sensitivity analysis, the results were similar in term of the effect size of statistical significance, when we replaced mean temperature with maximum and minimum temperature, respectively (see Table S2; Table S3; Figure S1; Figure S2). When all regions were analyzed as a whole, the results also suggested that the association between temperature and COVID-19 is insignificant (Table S4). Hence, we consider our estimates with higher confidence, and unlikely to be altered by different meteorological indicators or varying the study period.
4. Discussion
COVID-19 has been widely spread in China and overseas and caused severe health burden around the world, and the peak of the outbreak in most cities in China was in February. This study explored the association between ambient temperature and COVID-19 transmissibility in different regions in China. However, there was no apparent effect between temperature and transmissibility of COVID-19 in our study.
Previous studies on this topic in China suggested a slightly nonlinear or linear relationship between temperature and cases (Ma et al., 2020; Oliveiros et al., 2020; Wang et al., 2020; Xie and Zhu, 2020). The study conducted by Islam (Islam et al. (2020) also suggested that higher daily maximum temperature decreased the incidence rate ratio of COVID-19 at the current day.
The results should be interpreted with cautions. First, the contribution of temperature in explaining the variation in COVID-19's transmissibility appears low (Oliveiros et al., 2020; Prata et al., 2020; Wang et al., 2020), which means that if there exists real relationship, temperature may only explain a minor part of the transmissibility. Other factors, such as geographical characteristics (Sajadi et al., 2020), individual behavior (Anderson et al., 2020), population mobility (Sam Engle et al., 2020; Sirkeci and Yucesahin, 2020), control measures (Nussbaumer-Streit et al., 2020), may largely influence the epidemic of infectious diseases. The association between temperature and COVID-19 is insignificant based on our model (1), a nonlinear association may exist (Ran et al., 2020). Second, the most important and cannot be ignored issue is related to the particularity of infectious diseases. That is, the number of incidences for infectious diseases is determined by transmissibility (Wallinga and Lipsitch, 2007). Unlike non-communicable diseases (NCD), using case number as response modeling the relationship between infectious disease and environmental factors may produce non-causal associations (Zhao, 2020). In China, quarantine measures are the most stringent in the world, as well as earliest, the whole city of Wuhan was lockdown on January 23 (Tian et al., 2020), followed by Hubei and the other provinces. During policy implementation period, most people stay at home during the outbreak and maintain social distance outside, which could effectively reduce the spread of COVID-19 (Zhao et al., 2020). Thus, from January to February, the rising temperature in China may lead to a non-causal association to the morbidity related to COVID-19. Besides, a counterexample that raises suspicion is that there are some countries more warmer and the prevention measures more looser than China during the same period (Qasim Bukhari and Jameel, 2020), such as India and Brazil (Kumar, 2020; Prata et al., 2020), the epidemic situation is not more optimistic than China. Third, we should point out that our analysis found insignificant association between the ambient temperature and the transmission of COVID-19, but the RR estimation results (see Table 3) suggested that there likely exists a negative correlation between temperature and the transmission of COVID-19. By using global data, Chen et al. (2020b) lately examined the relationship between temperature and the spread of COVID-19, and found that there is a robust and significant negative association between COVID-19 transmissibility and ambient temperature at the country level. Ran et al. (2020) observed that the ambient temperature was found to have a nonlinear negative association with COVID-19 transmissibility based on the discontinuity regression method. Inconsistent results may be due to the different model frameworks, thus, more multi-data evidences might be needed to further test the association between ambient temperature and COVID-19 transmissibility.
According to the study by (Zhao, 2020), the instantaneous reproductive number R t could be more representative for the transmissibility of COVID-19. In our study, we used R t in place of daily confirmed cases, and did not find the significant association between temperature and COVID-19. This result is in agreement with the study conducted by Yao et al. (2020), they found temperature and ultraviolet radiation have no significant effects on COVID-19 transmission. Similar results were also found in Canada and Spain (Briz-Redon and Serrano-Aroca, 2020; To et al., 2020). A study in Iran (Ahmadi et al., 2020) suggested the population density and intra-provincial movement were the most important factors affecting the COVID-19 outbreak rate, and high solar radiation was a protective factor, but the temperature is unlikely.
A special case is that in North China, we found slightly significant negative association between temperature and R t. However, when we re-estimated the relationship without Inner Mongolia, the weak correlation was disappeared, which indicate this association appears not sufficiently stable. The reason why Inner Mongolia was an exception in our analysis is not clear as the weather-diseases relationship is more complicated and easily affected by the other non-meteorological factors, thus, this phenomenon may need further research. We still prefer to believe that the effect of temperature on COVID-19 is weak in that the exception of one city may not be convinced.
Our study has some advantages. First, the association between ambient temperature and transmissibility of COVID-19 in different regions across China was studied. A total of 28 Chinese provincial regions were included in this study, which may be benefit to obtain a reliable conclusion. Second, for aggregated data, the instantaneous reproductive number was used to avoid the noncausal association between environmental factor and COVID-19. This result was different with that obtained by using the infected cases data. Third, compared to the SARS, the association between temperature and COVID-19 is insignificant across China, which is of important reference value for specific public health strategy.
Our study also has some limitations. First, there was a time-series ecological study, it is difficult to check the causal relationship between temperature and transmissibility of COVID-19. Second, it is difficult to obtain the meteorological data at the individual level. Third, there are some other important factors such as air pollution, medical resources, governmental interventions may also affect the transmissibility of COVID-19. Third, with increase of the intervention prevention and control strategy of China, the effect size estimated in this study might be in small scale, and thus the true association between temperature and COVID-19 may be affected through the under controlled infected cases of COVID-19. Last, due to lack of information, our estimation of R t neglected the difference between local and imported cases. We remark the analytical framework adopted in this study can be extended to address this limitation with cases’ import or local status available. These issues should be addressed in future.
5. Conclusions
We found little statistical evidence for that the higher temperature may reduce the transmissibility of COVID-19. Since intensive control measures against the COVID-19 epidemics were implemented in China, we acknowledge this may impact the underlying effect size estimation, and thus cautiousness should be taken when interpreting our findings.
Credit author statement
Qingan Wang, Writing – original draft, Formal analysis. Yu Zhao, Writing – review & editing, Methodology, Funding acquisition. Yajuan Zhang, Data curation, Visualization. Jiangwei Qiu, Investigation. Juan Li, Investigation. Ni Yan, Investigation. Nan Li, Investigation. Jiaxing Zhang, Investigation. Di Tian, Investigation. Xiaolan Sha, Investigation. Jinyun Jing, Investigation. Chan Yang, Investigation. Kairong Wang, Investigation. Rongbin Xu, Methodology. Yuhong Zhang Supervision, Funding acquisition. Huifang Yang, Funding acquisition, Project administration. Shi Zhao, Methodology, Writing – review & editing, Validation. Yi Zhao Conceptualization, Project administration, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported by Ningxia Key Research and Development Plan Science and Technology Support Project (2020GZBD0004), National Natural Science Foundation of China (81860603, 12061058), and Natural Science Foundation of Ningxia (2020AAC03188).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110576.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ahmadi M. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729:138705. doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R.M. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briz-Redon A., Serrano-Aroca A. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukhari Qasim, Jameel Y. Will coronavirus pandemic diminish by summer? SSRN. 2020 doi: 10.2139/ssrn.3556998. [DOI] [Google Scholar]
- Cai Q.C. Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Publ. Health. 2007;121:258–265. doi: 10.1016/j.puhe.2006.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S. Revisiting the association between temperature and COVID-19 transmissibility across 117 countries. ERJ Open Res. 2020;6 doi: 10.1183/23120541.00550-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cori A. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am. J. Epidemiol. 2013;178:1505–1512. doi: 10.1093/aje/kwt133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drosten C. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- Engle Sam. Staying at home mobility effects of COVID-19. Covid Econ.: Vetted and Real-Time Pap. 2020;4:86–102. [Google Scholar]
- Ferretti L. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;10:1126. doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine P.E. The interval between successive cases of an infectious disease. Am. J. Epidemiol. 2003;158:1039–1047. doi: 10.1093/aje/kwg251. [DOI] [PubMed] [Google Scholar]
- Islam N. Temperature, humidity, and wind speed are associated with lower Covid-19 incidence. medRxiv. 2020 doi: 10.1101/2020.03.27.20045658. [DOI] [Google Scholar]
- Kumar S. Effect of meteorological parameters on spread of COVID-19 in India and air quality during lockdown. Sci. Total Environ. 2020;745:141021. doi: 10.1016/j.scitotenv.2020.141021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A.C. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:e151. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J. Med. Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaumer-Streit B. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst. Rev. 2020;4 doi: 10.1002/14651858.CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveiros B. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. medRxiv. 2020 doi: 10.1101/2020.03.05.20031872. [DOI] [Google Scholar]
- Prata D.N. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran J. A re-analysis in exploring the association between temperature and COVID-19 transmissibility: an ecological study with 154 Chinese cities. Eur. Respir. J. 2020;56 doi: 10.1183/13993003.01253-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi Mohammad M. SSRN; 2020. Temperature, humidity, and latitude analysis to predict potential spread and seasonality for COVID19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirkeci I., Yucesahin M.M. Coronavirus and migration: analysis of human mobility and the spread of covid-19. Mig. Let. 2020;17:379–398. [Google Scholar]
- Thompson R.N. Improved inference of time-varying reproduction numbers during infectious disease outbreaks. Epidemics. 2019;29:100356. doi: 10.1016/j.epidem.2019.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H. medRxiv; 2020. Early Evaluation of Transmission Control Measures in Response to the 2019 Novel Coronavirus Outbreak in China. [DOI] [Google Scholar]
- To T. Correlation of ambient temperature and COVID-19 incidence in Canada. Sci. Total Environ. 2020;750 doi: 10.1016/j.scitotenv.2020.141484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallinga J., Lipsitch M. How generation intervals shape the relationship between growth rates and reproductive numbers. Proceed. Royal Soc. B. 2007;274:599–604. doi: 10.1098/rspb.2006.3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M. Temperature Significantly Change COVID-19 Transmission in 429 Cities. MedRxiv. 2020 doi: 10.1101/2020.02.22.20025791. [DOI] [Google Scholar]
- Watts N. The 2019 report of the Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836–1878. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55 doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao S. To avoid the noncausal association between environmental factor and COVID-19 when using aggregated data: simulation-based counterexamples for demonstration. Sci. Total Environ. 2020;748 doi: 10.1016/j.scitotenv.2020.141590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y. Analysis of the transmissibility change of 2019-novel coronavirus pneumonia and its potential factors in China from 2019 to 2020. BioMed Res. Int. 2020;2020 doi: 10.1155/2020/3842470. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.