Abstract
Background: Despite the availability of effective drugs, blood pressure (BP) control rate is sub-optimal in individuals with hypertension in low- and middle-income countries (LMICs). The role of self-care in the management of BP is less studied in LMIC settings.
Methods: We conducted a community-based, cross-sectional study in individuals with hypertension in Kollam district, Kerala. A multistage cluster sampling method was used for the selection of study participants. We measured self-care by using an adapted Hypertension Self-Care Activity Level Effects (H-SCALE) scale. Descriptive statistics were used to summarise the data and logistic regression analysis was conducted to identify factors associated with BP control.
Results: In total, 690 individuals with hypertension (women=60%) and a mean age of 57±8 years participated in the study. More than half (54%) of the participants were adherent to anti-hypertensive medications. However, the adherence rate was much lower for the dietary approach to stop hypertension (DASH) diet (12.8%), recommended level of physical activity (24%) and weight management (11.4%). Overall BP control was achieved in two of five individuals (38.4%, 95% CI: 34.7-42.0%). Among self-care activities, adherence to medications (AOR: 1.8, 95% CI: 1.3-2.5), DASH diet (AOR: 1.5, 95% CI: 1.0-2.4), and non-smoking status (AOR: 3.3, 95% CI: 1.7-6.4) were associated with control of BP. Additionally, good family support to self-care (AOR: 1.9, 95% CI: 1.1-3.1) was associated with better control of BP.
Conclusion: In individuals with hypertension, the BP control rate is achieved in two of five individuals. Adoption of self-care activities are sub-optimal. Both family support and adherence to self-care activities are associated with BP control. Family based interventions to improve adherence to self-care activities could have a significant public health impact in achieving better population-level BP control rates in Kerala, India.
Keywords: Hypertension, blood pressure control, self-care, family support, India
Introduction
Globally, hypertension is a major cause of premature death and disability. Two of five adult individuals worldwide have raised blood pressure (BP) 1. Annually, more than 10 million deaths and 200 million disability adjusted life years (DALYs) are attributable to elevated BP 2. Hypertension is undoubtedly a major risk factor for stroke, heart failure, coronary heart disease and chronic kidney disease. More than half of the deaths due to cardiovascular disease (CVD) are linked to complications from hypertension 3. Hypertension is also a major public health problem in India, affecting almost one in three adult individuals 4. Additionally, high BP is attributable to more than 1.5 million deaths and 38 million DALYs in India 5.
Optimal BP control is essential to prevent the premature deaths and related disability attributable to hypertension. For example, a reduction of more than a third in the risk of stroke and a reduction of a quarter in the risk of myocardial infarction and heart failure are associated with optimal BP control in individuals with hypertension 6. However, BP control rates are abysmal in low- and middle-income countries (LMICs) even with the availability of effective drugs for management of hypertension 7. The disproportionately higher number of deaths from elevated BP in LMICs as compared to high-income regions is largely attributable to sub-optimal control of BP.
Hypertension is prevalent in two of five adult individuals in the state of Kerala, India 8. Despite the availability of a relatively strong public health system 9, BP control rate is poor in Kerala. For example, the BP control rate at the population level in adults over 18 years was less than 15% in a recent state-wide representative survey conducted in Kerala 8. In order to achieve optimal BP control, it is desirable to identify the major road blocks and target them with comprehensive health system approaches.
Comprehensive management of hypertension requires both pharmacological and lifestyle modification. Self-care has been recognised as an important determinant for achieving optimal BP control at the individual level. According to the World Health Organisation (WHO), self-care is defined as “the ability of individuals, families and communities to promote health, prevent disease, maintain health and to cope with illness and disability with or without the support of a healthcare provider” 10. Further, hypertension guidelines advise self-care activities such as self-monitoring of BP, reduction of dietary sodium intake, increase in physical activity, limiting alcohol intake, adoption of a dietary approach to stop hypertension (DASH) diet plan, weight management and abstinence from tobacco as lifestyle modification strategies to achieve optimal BP control 11. However, research in the areas of self-care practices and BP control are limited in LMICs. We aimed to assess hypertension self-care practices and its impact on BP control among adult individuals with hypertension in Kerala.
Methods
Ethical statement
The Institutional Ethics Committee of Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Kerala reviewed and approved the conduct of the study in Kerala (SCT/IEC/1450/NOVEMBER-2019). Written informed consent was obtained from all the study participants before administering the interview schedule. The participants had the freedom to refuse participation at the outset or during any stage of the study. There was no anticipated risk for participants by their involvement in the study. None of the selected participants refused participation.
Study design
We conducted a community based cross-sectional survey in Kollam District, Kerala, India.
Study setting
The study was conducted in five of eleven randomly selected ‘ block panchayats’ (panchayats are the lowest level of the three-tier local self-governance model in Kerala) of Kollam district, Kerala, India and the data collection took place between December 2019 to February 2020. The population size of Kollam district is 2.64 million, based on the 2011 census 12.
Study population
Individuals in the age group of 30–70 years, diagnosed with hypertension for at least six months and started on at least one antihypertensive drug as part of initial management were eligible to be part of the study. Individuals who could not communicate and were unable to provide informed consent were excluded from the study. A multistage cluster sampling method was used to identify eligible participants for the cross-sectional survey conducted in Kollam district, Kerala. The primary sampling unit was ‘ block panchayats’. Initially, five of eleven ‘ block panchayats’ were randomly selected from Kollam District, Kerala using computer-generated random numbers. In the second stage of sampling, two primary health centres (PHCs: caters to a population of approximately 25,000–40,000) were identified by simple random sampling procedure from each ‘ block panchayat’. Additionally from each primary health centre, we randomly identified three sub-centres (sub-centres cater to a population of approximately 5,000 individuals) for the study using computer-generated random numbers. We obtained the listing of all individuals with hypertension in the selected sub-centres based on the population-based screening records held by the Accredited Social Health Activists (ASHA) in the respective areas. From the chosen sub-centres, we randomly selected 23 individuals with hypertension using computer-generated random numbers from the population-based listing of all individuals with diagnosed hypertension. Participants were approached in person at their residence by the researcher (SC) with the help of a local community health worker (ASHA). Participants were provided with an information sheet (see Extended data 13) in Malayalam language, which contains details about research aims, objectives, and information regarding study questionnaires.
Sample size
A sample size of 690 individuals with hypertension yields more than 80% power to estimate reliably a range of prevalence of self-care activities and BP control rate from 10% to 50% 8, 14 with an absolute precision of 2.5% (assuming an alpha error of 0.05 and a design effect of 1.5).
Study variables and data collection
The researcher (SC) collected the data in person by visting each study participant at their residence. We collected information regarding sociodemographic factors, health-seeking behaviour, details related to comorbidities, family support and self-care practices. Self-care activities were captured using the adapted version of Hypertension Self-care Activity Levels Effects (H-SCALE) developed by Jan Warren-Fellow and Seymour 15. The H-SCALE was modified to suit the cultural practices prevalent in Kerala. Questions related to intake of certain types of fruits and vegetables were modified and replaced with culturally relevant food items.A panel of experts with expertise in public health, epidemiology and clinical cardiology reviewed the face validity and content validity of the modified version of the questionnaire (see Extended data 16). The modified tool was translated into the local language (Malayalam, see Extended data 17), and piloted in five individuals with hypertension who were selected from Trivandrum district in Kerala. The piloting involved testing the wordings, possible responses, and clarity of instructions. The tool was finalised after an expert review of the responses received to each item of the scale in the piloting phase. Only minor changes to the wording of some of the items were introduced to improve clarity of the questions. We measured BP and heart rate of the study participants using a digital sphygmomanometer (OMRON HEM-7121). BP was measured after the individual was seated comfortably in an upright position with their arm rested and using an appropriate cuff-size. The BP was measured from the left arm as per the WHO guidelines. After obtaining the first reading, the cuff was deflated fully and the next measurement was conducted after three minutes. The measurement was repeated for the third time by following the same procedure. The mean of the consecutive three readings was obtained and recorded as the BP of the individual.
Definitions
Medication adherence: We used a three-item scale to measure how many days the person took the medication in a week at the recommended dosage and at the recommended time. The scores for each item were summed (range 0–21). A score of 21 was considered as good adherence.
Adherence to the DASH diet: We used an 11-item scale to assess the intake of healthy foods associated with the nutritional composition of the DASH diet. The scores for each item were summed. The possible range of scores for the DASH-Q scale was 0 to 77. A score of <32 was considered as low diet quality; a score between 33 and 51 was considered as medium quality, and scores of 52 or greater were considered as good adherence.
Physical activity engagement: A two-item scale measured the number of days of physical activity of at least 30 minutes for each participant. The scores on both items were summed (range 0-14). A score of eight or above was considered as good adherence to physical activity.
Smoking: The scores in a two-item scale were summed (range 0-14). Respondents who scored zero were considered as adherent to non-smoking.
Weight management: A 10-item scale measured weight management activities in the last month. The sum of the scores on all items ranged from 10-50. Individuals who scored above 40 were considered as adherent to weight management practices.
Alcohol use: Individuals who did not drink alcohol at all were considered as alcohol abstinent.
Family support: A 16- item scale measured the influence of family members on diet and other health behaviour. The average score on all items ranged from 0.94–2.56. We categorised family support into minimal, mild, moderate and strong based on quartiles of the observed score. A score of <1.37, 1.38–1.56, 1.57–1.68, and 1.69 or greater were considered as minimal, mild, moderate and strong support, respectively.
BP control: BP control was defined as a mean BP ≤140/90 mmHg in all individuals based on the average of three readings.
Data analysis
We performed all data analysis in SPSS Version 25. Categorical variables were presented as frequencies and percentages. Continuous variables were presented as means with standard deviations. We performed multivariate logistic regression analysis to identify independent factors associated with BP control. All variables found to be statistically associated with BP control in the bivariate analyses at a higher p-value threshold of 0.1 were considered in the multivariate model.
Results
General characteristics of the study population
In total, 690 individuals (response rate = 100%) participated in the study. The age of participants ranged from 31 to 70 years with a mean age of 57±8 years ( Table 1). More than half of the participants (59.7%) were women. More than one-quarter (29%) of participants had primary or less than primary level of education. One in 10 women (10.7%) were living alone, while this was true for 3% of men. Below poverty level (BPL) ration cards were held by 44% of participants. Individual-level data for each participant are available as Underlying data 18.
Table 1. General characteristics of the study population.
| Characteristics | Men
N=278 |
Women
N=412 |
p-value |
|---|---|---|---|
| Age, mean (SD) | 57.40 (±8.91) | 56.93 (8.73) | 0.489 |
| Age group, n (%) | 0.520 | ||
| 31 - 40 | 16 (5.8) | 23 (5.6) | |
| 41-50 | 41 (14.7) | 78 (18.9) | |
| 51-60 | 109 (39.2) | 147 (35.7) | |
| 61-70 | 112 (40.3) | 164 (39.8) | |
| Marital status, n (%) | 0.0001 | ||
| Married | 249 (89.6) | 267 (64.8) | |
| Single /divorced | 29 (10.4) | 145 (35.2) | |
| Education, n (%) | 0.360 | ||
| Primary | 74 (26.6) | 127 (30.8) | |
| Secondary | 146 (52.5) | 213 (51.7) | |
| Higher secondary | 58 (20.9) | 72 (17.5) | |
| Occupation, n (%) | 0.001 | ||
| Self/formal employment | 89 (32.0) | 50 (12.1) | |
| Unemployed | 37 (13.3) | 27 (6.6) | |
| Retired | 45 (16.2) | 32 (7.8) | |
| Homemakers | 0 | 262 (63.6) | |
| Daily wages | 107 (38.5) | 41 (10.0) | |
| Living alone, n (%) | 0.001 | ||
| Yes | 9 (3.2) | 44 (10.7) | |
| No | 269 (96.8) | 368 (89.3) | |
| Income categories, n (%) | 0.262 | ||
| Below poverty line | 114 (41.0) | 188 (45.6) | |
| Above poverty line | 164 (59.0) | 224 (54.4) |
BP related characteristics of the study population
The mean age of diagnosis of hypertension was 50±9 years ( Table 2). Nearly three of five participants (59%) measured their BP at least once in a month. However, three-quarters (74.8%) of individuals were not aware of their last BP values. More than half (54%) were seeking treatment from public facilities. Similarly, more than half of the study participants (52.5%) visited a physician or health worker at least on a monthly basis. Only 10.8% and 7.3% of men and women were monitoring BP at home, respectively.
Table 2. Blood pressure, health seeking pattern and adherence to self-care components.
| Characteristics | Men | Women | p-value |
|---|---|---|---|
| Age at diagnosis, mean (SD) | 50.50 (9.5) | 50.62 (9.3) | 0.871 |
| Duration of hypertension, mean (SD) | 6.90 (6.6) | 6.31 (6.3) | 0.237 |
| Systolic BP (mmHg), mean (SD) | 142.55 (20.7) | 144.59 (19.4) | 0.186 |
| Diastolic BP (mmHg), mean (SD) | 87.55 (11.5) | 86.90 (11.3) | 0.465 |
| Health care facility, n (%) | 0.840 | ||
| Public | 150 (54.0) | 228 (55.3) | |
| Private | 84 (30.2) | 116 (28.2) | |
| Both | 44 (15.8) | 68 (16.5) | |
| Visit to a physician/health worker, n (%) | 0.433 | ||
| Weekly/monthly | 146 (52.5) | 198 (48.1) | |
| Twice/once in a year | 53 (19.1) | 79 (19.2) | |
| Rarely | 79 (28.4) | 135 (32.8) | |
| Home BP monitoring, n (%) | 0.142 | ||
| Yes | 30 (10.8) | 30 (7.3) | |
| No | 248 (89.2) | 382 (92.7) | |
| Awareness of last BP value, n (%) | 0.432 | ||
| Yes | 75 (27.0) | 99 (24.0) | |
| No | 203 (73.0) | 313 (76.0) | |
| Frequency of BP monitoring, n (%) | 0.220 | ||
| Monthly | 175 (62.9) | 232 (56.3) | |
| Twice/once in a year | 37 (13.3) | 65 (15.7) | |
| When symptoms occur/rarely | 66 (23.7) | 115 (28.0) | |
| Perceived BP control status, n (%) | 0.143 | ||
| Yes | 115 (41.4) | 195 (47.3) | |
| No | 163 (58.6) | 217 (52.7) | |
| Family support in self-care, n (%) | 0.065 | ||
| Minimal | 66 (23.7) | 118 (28.6) | |
| Mild | 82 (29.5) | 138 (33.5) | |
| Moderate | 55 (19.8) | 78 (18.9) | |
| Strong | 75 (27.0) | 78 (18.9) | |
| Self-care practices, n (%) | |||
| Medication adherence | 168 (60.4) | 210 (51.0) | 0.018 |
| DASH diet adherence | 40 (14.4) | 48 (11.7) | 0.347 |
| Physical activity adherence | 100 (36.0) | 65 (15.8) | <0.001 |
| Weight management adherence | 44 (15.8) | 37 (9.0) | 0.009 |
| Alcohol abstinence | 241 (86.7) | 412 (100.0) | <0.001 |
| Non-smoking | 215 (77.3) | 412 (100.0) | <0.001 |
BP, blood pressure; SD, standard deviation; DASH, dietary approach to stop hypertension.
Hypertension in isolation was present in 30% of the study population. Diabetes (39.1%) and dyslipidemia (32.2%) were the major comorbid conditions. The proportion of study participants with hypertension and one or two or more co-morbidities were 39% and 31.2%, respectively.
Self-care practices
The overall prevalence of medication adherence among study participants was 54.8% ( Table 2). The medication adherence was higher in men (60.4%) as compared to women (51%). Adherence to the DASH diet was very poor in both men (14.4%) and women (11.7%). Overall, 24% of participants were engaged in the recommended level of physical activity. Adherence to the recommended level of physical activity was very low in women (15.8%) as compared to men (36%). Nearly one-third (32.7%) of men were smokers. Alcohol use was prevalent in 13.3% of men. Overall, 11.4% of the individuals were adherent to weight management practices ( Table 2).
Family support in self-care
More than half (53.2 %) of men and 62.1% of women reported minimal to mild family support to self-care activities. Similarly, 47.6% and 37.7% of men and women reported moderate to strong family support to self-care activities related to hypertension management, respectively ( Table 2).
Factors associated with BP control
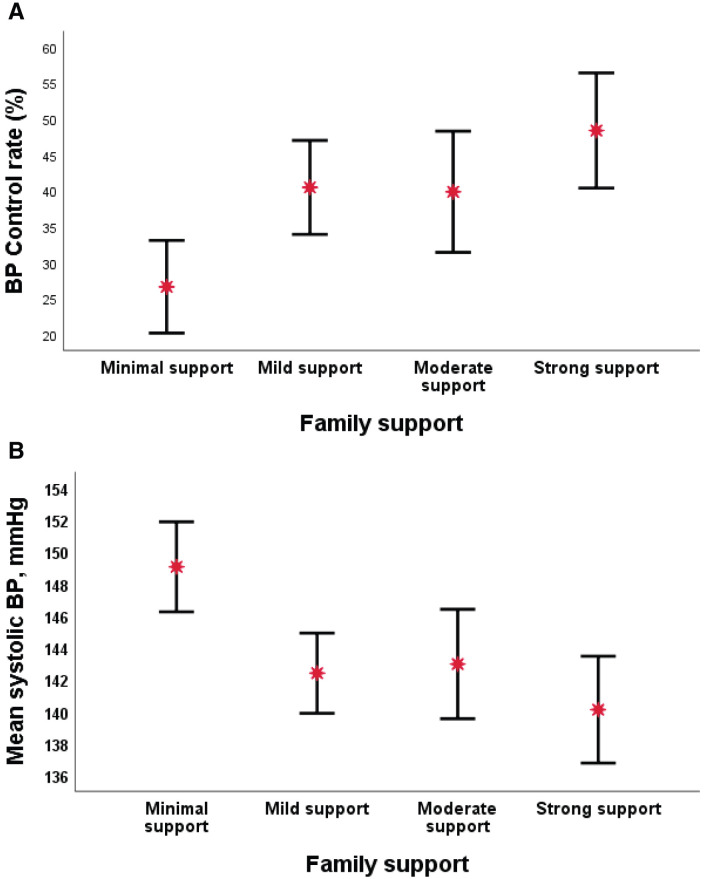
The proportion of individuals with controlled BP increased with the improvement in family support from minimal (26.6%) to strong support (48.8%). Similarly, the mean systolic BP was lowest in individuals with strong family support to self-care activities (140.10±2.82 mmHg) as compared to individuals with minimal family support (149.05±3.35mmHg) ( Figure 1).
Figure 1.
Panel A) Family support and blood pressure (BP) control rate. Panel B) Family support and mean systolic BP.
Age group, gender, educational level or occupation did not show any association with control of BP in the bivariate analysis ( Table 3). Similarly, duration of hypertension, home BP monitoring and frequency of BP monitoring were not associated with BP control. Only a quarter of patients living alone (24.5%) achieved BP control as compared to 40% in patients living with other family members (p = 0.04). Individuals seeking care from both private and public facilities were less likely to achieve BP control as compared to individuals seeking care from either private or public facilities. BP control rate improved with family support, adherence to medications and DASH diet. BP control rate was also better in those who were adherent to non-smoking practices as compared to smokers ( Table 3).
Table 3. Factors associated with blood pressure control.
| Variable | Controlled
n = 265 |
Uncontrolled
n = 425 |
p-value |
|---|---|---|---|
| Age group, n (%) | 0.429 | ||
| 31 - 40 | 18 (46.2) | 21 (53.8) | |
| 41 - 50 | 42 (35.3) | 77 (64.7) | |
| 51 - 60 | 105 (41.0) | 151 (59.0) | |
| 61 - 70 | 100 (36.2) | 176 (63.8) | |
| Gender, n (%) | 0.283 | ||
| Men | 114 (41.0) | 164 (59.0) | |
| Women | 151 (36.7) | 261 (63.3) | |
| Education level, n (%) | 0.730 | ||
| Up to primary | 78 (38.8) | 123 (61.2) | |
| Secondary | 141 (39.3) | 218 (60.7) | |
| Higher secondary and above | 46 (35.4) | 84 (64.6) | |
| Occupation, n (%) | 0.962 | ||
| Formal/self-employment | 56 (40.3) | 83 (59.7) | |
| Unemployed | 25 (39.1) | 39 (60.9) | |
| Retired | 27 (35.1) | 50 (64.9) | |
| Homemaker | 101 (38.5) | 161 (61.5) | |
| Daily wages | 56 (37.8) | 92 (62.2) | |
| Living alone, n (%) | 0.044 | ||
| Yes | 13 (24.5) | 40 (75.5) | |
| No | 252 (39.6) | 385 (60.4) | |
| Health care facility, n (%) | 0.006 | ||
| Public | 154 (40.7) | 224 (59.3) | |
| Private | 83 (41.5) | 117 (58.5) | |
| both | 28 (25.0) | 84 (75.0) | |
| Duration of hypertension, n (%) | 0.245 | ||
| <5 years | 136 (37.9) | 223 (62.1) | |
| 5-10 years | 74 (35.6) | 134 (64.4) | |
| <10 years | 55 (44.7) | 68 (55.3) | |
| Home BP monitoring, n (%) | 0.337 | ||
| Yes | 27 (45.0) | 33 (55.0) | |
| No | 238 (37.8) | 392 (62.2) | |
| Frequency of BP monitoring, n (%) | 0.922 | ||
| Monthly | 155 (38.1) | 252 (61.9) | |
| Twice/once in a year | 41 (40.2) | 61 (59.8) | |
| When symptoms occur/rarely | 69 (38.1) | 112 (61.9) | |
| Family support, n (%) | 0.001 | ||
| Minimal | 49 (26.6) | 135 (73.4) | |
| Mild | 89 (40.5) | 131 (59.5) | |
| Moderate | 53 (39.8) | 80 (60.2) | |
| Strong | 74 (48.4) | 79 (51.6) | |
| Medication adherence, n (%) | <0.001 | ||
| Adherent | 169 (44.7) | 209 (55.3) | |
| Non-adherent | 96 (30.8) | 216 (69.2) | |
| DASH diet adherence, n (%) | 0.071 | ||
| Adherent | 42 (47.7) | 46 (52.3) | |
| Non-adherent | 223 (37.0) | 379 (63.0) | |
| Physical activity adherence, n (%) | 0.261 | ||
| Adherent | 70 (42.4) | 95 (57.6) | |
| Non-adherent | 195 (37.1) | 330 (62.9) | |
| Weight management adherence, n (%) | 0.924 | ||
| Adherent | 32 (39.5) | 49 (60.5) | |
| Non-adherent | 233 (38.3) | 376 (61.7) | |
| Alcohol abstinence, n (%) | 0.552 | ||
| Adherent | 253 (38.7) | 400 (61.3) | |
| Non-adherent | 12 (32.4) | 25 (67.6) | |
| Non-smoking adherence, n (%) | 0.001 | ||
| Adherent | 253 (40.4) | 374 (59.6) | |
| Non-adherent | 12 (19.0) | 51 (81.0) |
BP, blood pressure; DASH, dietary approach to stop hypertension.
In the multivariate model ( Table 4), participants who were adherent to medication were approximately 1.5 times more likely to have controlled BP than non-adherent individuals (P = 0.009, OR = 1.5, 95% CI = 1.1-2.2). Individuals who were adherent to the DASH diet were 1.6 times more likely to have controlled BP as compared to the non-adherent group (P = 0.043, OR = 1.6, 95% CI = 1.0-2.6). Similarly, adherence to non-smoking improved the odds of BP control by almost three times (P = 0.001, OR = 3.1, 95% CI = 1.6-6.3).
Table 4. Strength of association of self-care and control of blood pressure.
| Variable | Unadjusted OR
(95% CI) |
p-value | Adjusted OR
(95% CI) |
p-value |
|---|---|---|---|---|
|
Living alone
Yes No |
Reference 2.0 (1.1-3.9) |
0.034 |
Reference 1.7 (0.8-3.5) |
0.116 |
|
Family support
Minimal Mild Moderate Strong |
Reference 1.9 (1.2-2.9) 1.8 (1.1-2.9) 2.6 (1.6-4.0) |
0.004 0.013 <0.001 |
Reference 1.4 (0.9-2.2) 1.3 (0.8-2.8) 1.9 (1.1-3.1) |
0.124 0.218 0.013 |
|
Health care facility
Public Private Both |
Reference 1.0 (0.7-1.5) 0.5 (0.3-0.8) |
0.860 0.003 |
Reference 0.9 (0.6-1.3) 0.5 (0.3-0.8) |
0.648 0.005 |
|
Adherence to home BP monitoring
No Yes |
Reference 1.3 (0.8-2.3) |
0.273 |
* |
|
|
Medication adherence
Adherent Non-adherent |
1.8 (1.3-2.5) Reference |
<0.001 |
1.5 (1.1-2.2) Reference |
0.009 |
|
DASH diet adherence
Adherent Non-adherent |
1.5 (1.0-2.4) Reference |
0.056 |
1.6 (1.0-2.6) Reference |
0.043 |
|
Physical activity adherence
Adherent Non-adherent |
1.2 (0.9-1.8) Reference |
0.224 |
* |
|
|
Weight management adherence
Adherent Non-adherent |
1.1 (0.7-1.7) Reference |
0.828 |
* |
|
|
Non-smoking adherence
Adherent Non-adherent |
3.3 (1.7-6.4) Reference |
<0.001 |
3.1 (1.6-6.3) Reference |
0.001 |
|
Alcohol abstinence
Adherent Non-adherent |
1.3 (0.7-2.7) Reference |
0.444 |
* |
BP, blood pressure; OR, odds ratio; CI, confidence interval; DASH, dietary approach to stop hypertension.
* Not included in multivariate analysis
Discussion
BP control is an important treatment goal for prevention of cardiovascular disease and related complications in individuals with hypertension. Self-care practices are sub-optimal and they are strongly associated with BP control in individuals with hypertension in Kerala. Additionally, family support enhances adherence to self-care practices related to BP management.
The overall BP control rate in our study population is higher than the data reported in previous studies from Kerala. For example, a large cross-sectional survey conducted in Kerala observed that BP control is only achieved in less than 15% of individuals with hypertension 8. As a standard practice in community-based surveys on hypertension prevalence, the above cited study included all individuals with elevated BP above the hypertension threshold of 140/90 mmHg in the ‘uncontrolled BP’ category. Hence, even the individuals with a first time diagnosis of hypertension based on a single visit BP measurement are labelled as ‘uncontrolled hypertension’. However, we have included those who were diagnosed with hypertension for at least six months, started on at least one antihypertensive drug as part of initial management, and had a BP above the hypertension threshold in the ‘uncontrolled BP’ category in our study. Therefore, the control rate observed in our study is among individuals who were formally diagnosed and treated for hypertension. Unlike other facility-based surveys, our results are based on a representative community-based sample of individuals with diagnosed hypertension.
Self-care practice was less than optimal in our study population. Despite the prescription of treatment and the follow-up by ASHA workers, only 55% were adherent to the medications. Additionally, adherence to DASH diet components were only observed in less than 15% of the study population. Our study demonstrates that self-care practices are very important in achieving optimal control of BP. We show that those who were adherent to drugs, the DASH diet and non-smoking achieved better BP control than the non-adherent group. Consistent findings on adherence to medication and BP control are reported in other studies 19– 21.
BP control in individuals with hypertension often requires adherence to self-care activities beyond medications. However, self-care activities related to diet and smoking are often ignored. Clinical trial evidence suggests that a low sodium DASH diet improves the control of BP and reduces cardiovascular risk in individuals with hypertension 11. In the PREMIER trial, the DASH diet and other lifestyle practices together reduced BP and cardiovascular events 22. Despite the known benefits of a low sodium DASH diet, adherence to DASH diet components were abysmally poor in our study. Community-based strategies to improve adherence to DASH diet components 23 and policy initiatives promoting low sodium salt 24 may improve the BP control rate at the population level. Prescribing mandatory targets for the food industry, front of pack labelling, food procurement policies and taxation are some additional policy initiatives to reduce population level salt consumption 25.
We show that smoking status is independently associated with BP control. Consistent findings are reported in the national health survey in England 26. Available evidence also shows that nicotine in cigarettes acts as an adrenergic agonist and mediates release of catecholamines, which affects BP levels and heart rate 27. Alcohol abstinence is also an important self-care practice that plays a significant role in the control of BP. In our study, alcohol use was not associated with BP control. However, the amount of alcohol consumption should be taken into consideration while exploring the association with BP control. In the INTERSALT study, a significant reduction in BP was observed in people who had limited their alcohol consumption 28. The potentially causal relationship between alcohol abstinence and BP reduction in the INTERSALT study provides further evidence to recommend alcohol reduction to control BP in hypertensive individuals.
Family support of self-care activities is a key factor associated with BP control in our study. Better family support acts through improvements in the adherence to self-care activities and thereby improves BP control. The positive association between BP control and perceived family support emphasizes the need for health care providers to assess the available family support when managing individuals with hypertension. Further, it calls for innovative family-based models such as the Programme of Lifestyle Intervention in Families (PROLIFIC study) in managing BP 29. The PROLIFIC model vouches for a family centred strategy for lifestyle changes and self-care for cardiovascular risk reduction. In a family centred approach, the proposed lifestyle changes and self-care strategies are more achievable and sustainable for the individuals and their family members 30.
Strengths and limitations
The study sample was representative of the population of Kollam District in Kerala. To the best of our knowledge, the impact of self-care activities on BP control is not studied in detail in community settings in India. Due to the self-reported nature of adherence pattern, the study is prone to recall and response bias. The associations observed in our study may not infer causality due to the cross-sectional nature of the study.
Conclusion
Overall, BP control is achieved in two of five participants with diagnosed hypertension and on treatment in Kerala at the community level. Further, compliance to self-care practices are less than optimal in the study population. Optimal adherence to self-care strategies is important in improving BP control rate in individual with hypertension. Family support is key to improving adherence to self-care practices and thereby facilitates individuals with hypertension to achieve improved BP control. Interventions to improve family support for self-care activities could have a significant public health impact in achieving better population-level BP control rates in Kerala, India.
Data availability
Underlying data
Figshare: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala. https://doi.org/10.6084/m9.figshare.12616325.v1 18.
This project contains the following underlying data:
-
-
Dataset.csv (raw individual level data for each participant)
-
-
Codes used in dataset.docx
Extended data
Figshare: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala. https://doi.org/10.6084/m9.figshare.12616214.v4 16.
This project contains the following extended data:
-
-
Interview schedule English version.pdf
Figshare: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala. https://doi.org/10.6084/m9.figshare.12662042.v2 17.
This project contains the following extended data:
-
-
Interview schedule malayalam version.pdf
Figshare: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala. https://doi.org/10.6084/m9.figshare.12662357.v1 13.
This project contains the following extended data:
-
-
Participant information sheet english version.pdf
-
-
Participant information sheet malayalam version 2.pdf
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0).
Acknowledgements
We gratefully acknowledge the time and effort given by all the participants. We also acknowledge the support of ASHA workers in identifying the participants.
Funding Statement
This work was supported by the Wellcome Trust through a Wellcome Trust/DBT India Alliance Clinical and Public Health Intermediate Fellowship to Panniyammakal Jeemon [IA/CPHI/14/1/501497].
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; peer review: 2 approved]
References
- 1. WHO: Global status report on noncommunicable diseases 2010. WHO. Reference Source [Google Scholar]
- 2. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators: Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990– 2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lawes CMM, Vander Hoorn S, Rodgers A, et al. : Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–8. 10.1016/S0140-6736(08)60655-8 [DOI] [PubMed] [Google Scholar]
- 4. Anchala R, Kannuri NK, Pant H, et al. : Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170–7. 10.1097/HJH.0000000000000146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Global Burden of Disease Visualisations: Compare. (accessed June 24, 2020). Reference Source [Google Scholar]
- 6. Law MR, Morris JK, Wald NJ: Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009(accessed July 6, 2020);338:b1665. 10.1136/bmj.b1665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Irazola VE, Gutierrez L, Bloomfield G, et al. : Hypertension Prevalence, Awareness, Treatment, and Control in Selected LMIC Communities: Results From the NHLBI/UHG Network of Centers of Excellence for Chronic Diseases. Glob Heart. 2016;11(1):47–59. 10.1016/j.gheart.2015.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sarma PS, Sadanandan R, Thulaseedharan JV, et al. : Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open. 2019;9(11):e027880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thankappan KR, Valiathan MS: Health at low cost - The Kerala model. Lancet. 1998;351(9111):1274–5. Reference Source [Google Scholar]
- 10. Organization WH, Asia RO for S-E: Self care for health. WHO Regional Office for South-East Asia.2014; (accessed June 1, 2020). Reference Source [Google Scholar]
- 11. Chobanian AV, Bakris GL, Black HR, et al. : The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureThe JNC 7 Report. JAMA. 2003;289(19):2560–2560. 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 12. Census of India: Primary Census Abstract. (accessed July 16, 2020). Reference Source [Google Scholar]
- 13. Chacko S, Jeemon P: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala.2020; published online July 16. 10.6084/m9.figshare.12662357.v1 [DOI] [PMC free article] [PubMed]
- 14. Saju MD, Allagh KP, Scaria L, et al. : Prevalence, Awareness, Treatment, and Control of Hypertension and Its Associated Risk Factors: Results from Baseline Survey of SWADES Family Cohort Study. Int J Hypertens. 2020;2020:e4964835. 10.1155/2020/4964835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Warren-Findlow J, Basalik DW, Dulin M, et al. : Preliminary validation of the Hypertension Self-Care Activity Level Effects (H-SCALE) and clinical blood pressure among patients with hypertension. J Clin Hypertens (Greenwich). 2013;15(9):637–43. 10.1111/jch.12157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chacko S, Jeemon P: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala.2020; published online July 6. 10.6084/m9.figshare.12616214.v4 [DOI] [PMC free article] [PubMed]
- 17. Chacko S, Jeemon P: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala.2020; published online July 16. 10.6084/m9.figshare.12662042.v2 [DOI] [PMC free article] [PubMed]
- 18. Chacko S, Jeemon P: Role of family support and self-care practices in blood pressure control in individuals with hypertension; results from a cross sectional study in Kollam District, Kerala.2020; published online July 6. 10.6084/m9.figshare.12616325.v1 [DOI] [PMC free article] [PubMed]
- 19. Matsumura K, Arima H, Tominaga M, et al. : Impact of antihypertensive medication adherence on blood pressure control in hypertension: the COMFORT study. QJM. 2013;106(10):909–14. 10.1093/qjmed/hct121 [DOI] [PubMed] [Google Scholar]
- 20. Dennis T, Meera NK, Binny K, et al. : Medication adherence and associated barriers in hypertension management in India. CVD Prev Control. 2011;6(1):9–13. 10.1016/j.cvdpc.2010.11.001 [DOI] [Google Scholar]
- 21. Morgado M, Rolo S, Macedo AF, et al. : Predictors of uncontrolled hypertension and antihypertensive medication nonadherence. J Cardiovasc Dis Res. 2010;1(4):196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Appel LJ, Champagne CM, Harsha DW, et al. : Effects of Comprehensive Lifestyle Modification on Blood Pressure Control: Main Results of the PREMIER Clinical Trial. JAMA. 2003;289(16):2083–93. 10.1001/jama.289.16.2083 [DOI] [PubMed] [Google Scholar]
- 23. Lin PH, Appel LJ, Funk K, et al. : The PREMIER intervention helps participants follow the Dietary Approaches to Stop Hypertension dietary pattern and the current Dietary Reference Intakes recommendations. J Am Diet Assoc. 2007;107(9):1541–51. 10.1016/j.jada.2007.06.019 [DOI] [PubMed] [Google Scholar]
- 24. Bernabe-Ortiz A, Sal Y Rosas VG, Ponce-Lucero V, et al. : Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat Med. 2020;26(3):374–8. 10.1038/s41591-020-0754-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Trieu K, Neal B, Hawkes C, et al. : Salt Reduction Initiatives around the World - A Systematic Review of Progress towards the Global Target. PLoS One. 2015;10(7):e0130247. 10.1371/journal.pone.0130247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Primatesta P, Falaschetti E, Gupta S, et al. : Association between smoking and blood pressure: evidence from the health survey for England. Hypertension. 2001;37(2):187–93. 10.1161/01.hyp.37.2.187 [DOI] [PubMed] [Google Scholar]
- 27. Lee DH, Ha MH, Kim JR, et al. : Effects of smoking cessation on changes in blood pressure and incidence of hypertension: a 4-year follow-up study. Hypertension. 2001;37(2):194–8. 10.1161/01.hyp.37.2.194 [DOI] [PubMed] [Google Scholar]
- 28. Marmot MG, Elliott P, Shipley MJ, et al. : Alcohol and blood pressure: the INTERSALT study. BMJ. 1994;308(6939):1263–7. 10.1136/bmj.308.6939.1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jeemon P, Harikrishnan S, Sanjay G, et al. : A PROgramme of Lifestyle Intervention in Families for Cardiovascular risk reduction (PROLIFIC Study): design and rationale of a family based randomized controlled trial in individuals with family history of premature coronary heart disease. BMC Public Health. 2017;17(1):10. 10.1186/s12889-016-3928-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Joseph LM, Lekha TR, Boban D, et al. : Perceived facilitators and barriers of enrolment, participation and adherence to a family based structured lifestyle modification interventions in Kerala, India: A qualitative study [version 2; peer review: 3 approved]. Wellcome Open Res. 2019;4:131. 10.12688/wellcomeopenres.15415.2 [DOI] [PMC free article] [PubMed] [Google Scholar]