Abstract
Background and Aims:
Spinal anaesthesia induced hypotension (SAIH) and bradycardia may prove deleterious to both parturient and baby, hence vasopressors play a vital role in their management. Recent studies on norepinephrine as rescue vasopressor during subarachnoid block (SAB) enlighten its role for SAIH. This randomised double-blind trial was conducted to compare the effect of intermittent intravenous boluses of norepinephrine and frequently used mephentermine for management of SAIH in caesarean section (CS) to prove whether norepinephrine produces comparable effects or superior to mephentermine.
Methods:
After approval from Institutional Ethics Committee and registration in Clinical Trials Registry India (CTRI/2019/06/019652), 256 parturients posted for elective CS under SAB were randomly allocated into Group-N and Group-M (n = 84) using chit system, who received boluses of intravenous norepinephrine 8μg and mephentermine 6mg for SAIH, respectively. Systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), Response%, Apgar score and maternal complications were analysed.
Results:
The changes in SBP and DBP were comparable in both the groups. It was significantly low after SAB compared to baseline and significantly high compared to 1st hypotensive value in both the groups throughout the study period (<0.0001). HR was comparable for initial 10 min, thereafter it was significantly high in Group-M (<0.0001) till 40 min. Response% after the first bolus was significantly high in Group-N (59.30n ± 29.21 vs 39.78 ± 25.6; P = <0.0001).
Conclusion:
Intravenous norepinephrine is better than mephentermine with respect to high response% and stable maternal HR although both are equally effective in maintaining blood pressure following SAIH during elective CS.
Keywords: Caesarean delivery, mephentermine, norepinephrine, spinal anaesthesia induced hypotension
INTRODUCTION
Spinal anaesthesia induced hypotension (SAIH) is reported in 80% parturients during caeserean section (CS) because of anaesthetic blockade up to T4 level. Severe and sustained SAIH is detrimental to both mother and baby.[1] The choice of the most effective management strategy for SAIH during CS continues to be one of the main challenges in obstetric anaesthesia. Many techniques and various vasopressors have been tried and studied for SAIH, but no single method was found to be adequate or superior.[2]
Mephentermine (a mixed sympathomimetic with mainly indirect β stimulation) is one of the most commonly used drugs in our institute and India. It has been shown to be as effective and safe as ephedrine for SAIH.[3] Norepinephrine, a potent α-agonist and a weak β-agonist, commonly used in septic shock has been showing promising results in many studies for SAIH with respect to maternal haemodynamic stability.[4]
However, looking at limited published literature on comparison of norepinephrine and mephentermine for management of SAIH, the present prospective, double-blind and randomised trial was conducted with the aim to assess whether intermittent intravenous boluses of norepinephrine were comparable or superior to intermittent boluses of mephentermine following SAIH in CS. The primary objective was to assess response percentage (response%) of the first dose of intravenous norepinephrine and mephentermine, and secondary objectives were to assess change in systolic blood pressure (SBP), diastolic blood pressure (DBP), maternal heart rate (HR), total number of boluses of norepinephrine and mephentermine required and Apgar score.
METHODS
The present prospective, double-blind and randomised study was conducted in a tertiary care teaching hospital after approval from the Institutional Ethics Committee and registration in Clinical Trials Registry of India (CTRI/2019/06/019652) within five months duration from June 2019 to November 2019. The study was conducted as per consort guidelines and followed ethical guidelines of the Declaration of Helsinki. After written informed consent to participate in the study, 297 parturients of 18-35 years of age, 50-100kg weight, 140-180cm height, American Society of Anaesthesiologists physical status (ASA)–II and singleton term pregnancy posted for elective CS under SAB were included in the study. Parturients with pre-existing pregnancy-induced hypertension, cardiovascular or cerebrovascular disease, hepato-renal disease, diabetes mellitus, allergy to study drugs, not required study drugs intraoperatively, intraoperative use of uterotonic other than oxytocin, known foetal abnormality, more than expected blood loss and contraindication to SAB were excluded from the study.
For sample size calculation, data of the study by Ngan Kee WD was used. He found the response on SBP of 8μg intravenous norepinephrine to be 74.2 ± 34.5%.[5] As the study on response percentage of mephentermine was not available, a pilot study was conducted in our institute in 10 parturients to observe the response of mephentermine 6mg on SBP that was 49.08 ± 31.71%. Taking these into consideration, the difference between these two means with confidence level and power 99% each, a minimum sample size of 84 per group was required to compare the effect of both the drugs as calculated by Epitool in stat software.
A total of 297 parturients were screened and 41 parturients were excluded on the basis of exclusion criteria. Randomisation was done by sealed envelope technique with an allocation ratio of 1:1 into 2 groups by a resident anaesthesiologist who was not involved in the intraoperative management. For that, 168 slips labelled with either norepinephrine or mephentermine (n = 84) were sealed with an adhesive and placed in a container. If particular participant was excluded after randomisation because of any reason mentioned above, then that slip was again dropped into the container. Epinephrine 8 μg/ml or mephentermine 6 mg/ml was prepared in two separate 10 ml syringes labelled as vasopressor by same resident anaesthesiologist. This resident held the code for randomisation and group allocation. Group-N and Group-M received bolus intravenous norepinephrine 8μg and mephentermine 6mg for the maintenance of intraoperative systolic blood pressure, respectively. Participants and anaesthesiologist involved in intraoperative management were blinded to the type of vasopressor used and group allocation.
All participants were kept nil per oral for 6 hours prior to operation. On arrival to the operation theatre, 18-gauge intravenous cannula was accessed and multipara monitor was attached and baseline systolic blood pressure(SBP), diastolic blood pressure (DBP), heart rate (HR), peripheral oxygen saturation (SpO2) and electrocardiogram (ECG) were recorded. All participants were premedicated with intravenous metoclopramide 10mg and pantoprazole 40mg. They were preloaded with 500ml ringer lactate. Subarachnoid space was accessed under all aseptic precautions through L3-L4 or L4-L5 intervertebral space using 25-gauge Quincke's spinal needle in the left lateral decubitus position. After confirmation of free flow of cerebrospinal fluid, 2ml hyperbaric bupivacaine 0.5% (w/v) was administered in subarachnoid space to achieve block up to T4. HR, SBP and DBP were recorded at every 2 min interval till 20 min and thereafter at every 5 min interval till the completion of surgery. Bolus intravenous injection of study drug was given through vasopressor labelled syringe on development of hypotension, (i.e., decrease in SBP to less than 80% of baseline value) as per group assigned. To see response%, SBP was recorded at 1 minute after the first bolus of vasopressor. Response of drug on blood pressure was defined according to the equation: 'Response% = [C-B/A-B] × 100'. Where, A: Baseline SBP, B: SBP at first episode of hypotension and C: SBP at 1 minute after the first injection of vasopressor.[5]
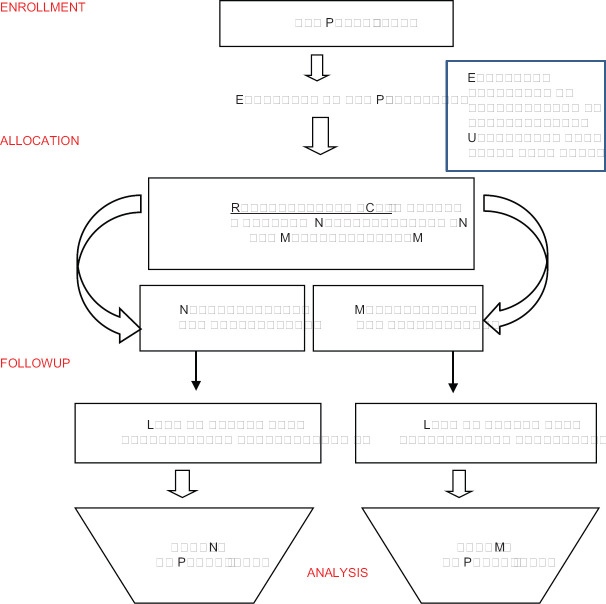
Bradycardia (a fall in heart rate below 50 per minute) was treated with intravenous atropine 0.6mg. Nausea, vomiting and other maternal undesired effects were noted and managed accordingly. Neonatal outcome was assessed by Apgar score at the 1st min and 5th min. Parturients who received more than expected blood loss, parturients received atropine and uterotonic agents other than oxytocin were also excluded from the study. Finally, data of 84 parturients in Group-N and 84 parturients in Group- M were recorded and analysed [Figure 1].
Figure 1.
Consort Flow Chart
Statistical analysis was done by applying Graph-pad in stat software. The numerical variables were compared between the groups by Student's unpaired t-test and within the group by Student's paired t-test. Categorical data were compared between the groups by Chi-square test. P value ≤0.05 was considered as significant.
RESULTS
Demographic data of parturients, duration of surgery and Apgar score of neonates were statistically comparable between the groups. [Table 1] Level of block was T4-T5 in all parturients.
Table 1.
Demographic profile, duration of surgery and Apgar score
| Parameters | Group N (n=84) (mean±SD) | Group M (n=84) (mean±SD) | P |
|---|---|---|---|
| Age (years) | 24.36±3.21 | 24.8±3.94 | 0.4286 |
| Height (cm) | 155.43±3.32 | 154.5±3.087 | 0.0618 |
| Weight (kg) | 63.33±4 | 63.93±4.296 | 0.3502 |
| Duration of surgery (min) | 46.74±3.82 | 46.15±3.262 | 0.2833 |
| Apgar Score | |||
| At 1st min | 7.64±0.65 | 7.65±0.63 | 0.9195 |
| At 5th min | 9.68±0.52 | 9.67±0.55 | 0.9038 |
After 1st bolus of vasopressors, rise in SBP was observed in both the groups. However, rise in SBP and response% was significantly high in Group-N as compared to Group-M [(SBP: 103.87 ± 8.90 mmHg vs 98.63 ± 7.31 mmHg, P = <0.0001) and (response%: 59.30 ± 29.21% vs 39.78 ± 25.6%; P = <0.0001)]. HR after 1st bolus of vasopressor was significantly high in Group-M as compare to Group-N (87.33 ± 9.01/min vs. 95.37 ± 11.75/min, P = <0.0001).
The changes in SBP and DBP were comparable in both the groups throughout the study period. In intragroup comparison, SBP and DBP were significantly low after SAB compared to baseline and significantly high compared to 1st hypotensive value in both the groups throughout the study period (<0.0001) [Figure 2].
Figure 2.
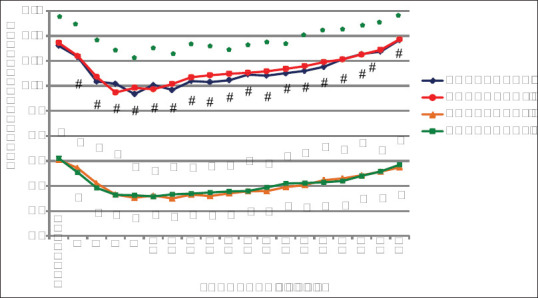
Mean systolic blood pressure (SBP) mmHg and diastolic blood pressure (DBP) mmHg.* Denotes P value > 0.05 of SBP between Group-N and Group-M. # denotes P value < 0.001 for SBP of Group-N and Group-M when compared with the value of the first episode of hypotension.^ denotes P value > 0.05 of DBP between Group-N and Group-M. $ denotes P value < 0.001 for DBP of Group-N and Group-M when compared with the value of the first episode of hypotension
HR was comparable at baseline and for initial 10 min after SAB between the groups. Thereafter, it was statistically higher in Group-M as compare to Group-N until 40 min (p < 0.0001). Though in intragroup comparison, it was decreased significantly as compared to HR at the time of hypotension in both the groups throughout the study period (p < 0.001). However, in the majority of times, intraoperative HR was less than the baseline value in Group-N and more than the baseline value in Group-M [Figure 3].
Figure 3.
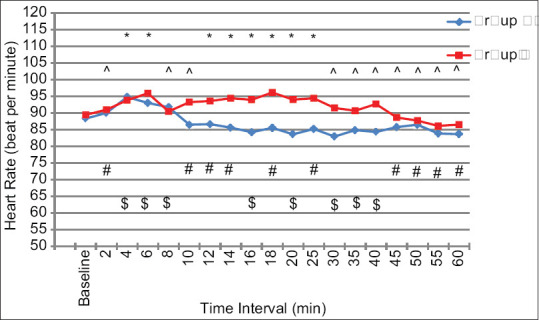
Mean heart rate (beat per minute). *Denotes P value < 0.05 for HR of Group-M when compared with the baseline HR. ^denotes P value > 0.05 for HR of Group-M when compared with the baseline HR. #denotes P value > 0.05 for HR of Group-N when compared with the baseline HR. $denotes P value < 0.05 for HR of Group-N when compared with the baseline HR
Maximum number of parturients required three boluses of norepinephrine to treat SAIH in Group-N as compared to single bolus of mephentermine in Group-M [36 parturients (42.86%) vs 38 parturients (45.24%)), respectively]. In Group-N, 4 parturients (4.76%) and 2 parturients (2.38%) required five and six boluses of norepinephrine respectively while in Group-M maximum numbers of boluses required were four [Table 2].
Table 2.
Parturients distribution as per number of boluses of norepinephrine and mephentermine administered (Number and Percentage)
| Frequency | Group-N (n=84) | Group-M (n=84) | P |
|---|---|---|---|
| One time | 3 (3.57%) | 38 (45.24%) | <0.0001 |
| Two times | 24 (28.57%) | 28 (33.33%) | 0.5059 |
| Three times | 36 (42.86%) | 11 (13.09%) | <0.0001 |
| Four times | 16 (19.04%) | 7 (8.33%) | 0.0441 |
| Five times | 4 (4.76%) | 0 (0%) | 0.0436 |
| Six times | 2 (2.38%) | 0 (0%) | 0.1561 |
The incidence of maternal adverse events such as nausea/vomiting, shivering and headache were comparable between the groups. None of the parturients in either group had an episode of hypertension, high spinal or total spinal. [Table 3] Apgar score at the 1st and 5th minute was also comparable between the groups and no statistical difference was observed (p = 0.9195 and 0.9038) [Table 1].
Table 3.
Incidence of adverse events
| Adverse Events | Group N (number and percentage) (n=84) | Group M (number and percentage) (n=84) | P |
|---|---|---|---|
| Nausea/Vomiting | 7 (8.33%) | 8 (9.5%) | 0.7908 |
| Shivering | 9 (10.7%) | 9 (10.7%) | 1.000 |
| Headache | 6 (7.14%) | 5 (5.95%) | 0.7559 |
| High Spinal/Total Spinal | 0 | 0 | |
| Hypertension | 0 | 0 |
DISCUSSION
The results of the study showed that both norepinephrine and mephentermine maintained blood pressure effectively following SAIH in CS. Statistically significant rise in blood pressure (systolic and diastolic) and fall in HR were recorded throughout the study period after administration of vasopressors compared to first hypotensive value in both the groups (p < 0.001). Though changes in SBP and DBP were comparable between the groups, HR was significantly high compared to baseline after mephentermine administration after 10 mins of hypotension. Furthermore, the response percentage of the 1st bolus of norepinephrine was significantly high, though significantly more number of boluses were required to manage SAIH compare to mephentermine.
SAB has been the preferred anaesthesia technique for caesarean section due to awake post-operative state for early mother-baby bonding, early initiation of breastfeeding, faster recovery of gastrointestinal functions after surgery, better postoperative analgesia, early mobilisation and lower risk of placental drug transfer.[1] However, associated sympatholysis induces a decrease in systemic vascular resistance and activates Bezold-Jarisch reflex, leading to vasodilation, bradycardia and hypotension which may be deleterious to both parturient and baby. This is further aggravated by aortocaval compression. Severe and sustained SAIH not only increases the risk of nausea-vomiting, aspiration, acute renal failure and altered mental status in parturients but also compromises uteroplacental circulation with consecutive foetal hypoxia, bradycardia, acidosis and neurological injury.[3,5,6,7,8] Various measures have been used in clinical practice for prevention and control of SAIH, such as preloading/co-loading with crystalloid/colloid infusion, wrapping lower limbs with compression stockings, left tilt, administering an optimal local anaesthetic to obtain an optimal height and administering vasopressor/inotropes. Vasopressors are effective in preventing and treating SAIH but the choice of vasopressor has been debated.
Mephentermine has been widely used in India because of its safety, ready availability, and familiarity to most anaesthesiologists. It acts mainly by indirect action (release of norepinephrine) causing an increase in myocardial contractility and HR, and hence cardiac output; it also causes peripheral vasoconstriction and raises the blood pressure by direct action on α and β receptors.[1,3,9,10,11] Recent studies also showed a promising role of norepinephrine in SAIH for maintaining blood pressure with less negative effects on HR and cardiac output because of a potent α-agonist and a weak β-agonist property.[4,12,13,14,15,16,17,18,19,20]
Ngan Kee et al.[17] compared the prophylactic continuous intravenous norepinephrine infusion (2.5 μg/min) with a bolus of 5μg norepinephrine and revealed the superiority of continuous norepinephrine infusion over the intermittent intravenous boluses. In our study, intermittent i.v. boluses were chosen because of its familiarity.
Ngan Kee et al.[5] compared norepinephrine to phenylephrine for maintaining SBP under spinal anaesthesia in CS with a computer-controlled closed-loop feedback system and noted higher response% which is well correlated with our finding. The higher response percentage with norepinephrine and requirement of frequent boluses in our study could be because of the faster onset of action and shorter half-life of norepinephrine compared to mephentermine.
Onwochei et al.[19] studied the effect of different intermittent i.v. boluses of norepinephrine to prevent SAIH in cesarean delivery. The results obtained were feasible and were not associated with significant maternal or fetal adverse effects that coincide with the results of our study.
Amira Abo Elnasr Awad[20] and El Shafei MM, et al.[13] compared 5μg norepinephrine with 5mg ephedrine to prevent SAIH in lower limb orthopaedic surgery and coronary artery disease patients undergoing knee arthroscopy. They found that norepinephrine is more effective compared with ephedrine in the maintenance of blood pressure and has less adverse effects on HR in patients. These results are in agreement with the results obtained in our study although we conducted our study in parturients.
Modak A, et al.[11] compared the boluses of phenylephrine and mephentermine for maintenance of arterial pressure during spinal anaesthesia in CS and found a significant increase in HR after bolus dose of mephentermine as compare to phenylephrine till the end of surgery when compared with the values at the onset of hypotension due to its β-agonist property.
As per the electronic search, norepinephrine and mephentermine have never been compared for management of SAIH, thus potency ratio of them was uncertain. So equipotent doses were calculated on the basis of the evidence available in the literature. Mohta et al.[9] suggested the potency ratio of phenylephrine: mephentermine of 11.9:1. Ngan Kee[5] conducted comparative dose-response analysis and revealed relative potency for norepinephrine: phenylephrine when given as a bolus for restoring BP in SAIH in obstetric patients to be 13.1:1.0 and found that phenylephrine 100μg was equivalent to norepinephrine 8 μg, although in the previous dose-finding study bolus injection of 6μg norepinephrine was reported effective. Therefore, we derived the relative potency of norepinephrine vs. mephentermine and used 8μg norepinephrine and 6mg mephentermine as equipotent doses.
Apgar score at the 1st and 5th minute in our study was >7 in both the groups. The incidence of maternal adverse events was also comparable between both the groups. Bradycardia was not considered as an adverse event/complication in our study. Parturients with bradycardia were excluded from the study as they were treated with injection atropine, which may have affected the blood pressure and may have confounded our results. Hypotension was also not mentioned as adverse event/complication as all parturients included in the study had hypotension. The incidence of adverse events of our study is not consistent with most of the reviewed studies as they included all participants as denominator or patients with bradycardia were part of the denominator to calculate the incidence of adverse events/complications.
The limitations of our study were that we had limited the study duration till end of surgery that should be extended till the passing off effect of SAB. Umbilical blood analysis was not studied to evaluate neonatal outcome.
In future, the same study could be extended to include umbilical blood analysis to know the effect of studied drugs on neonates. The study can be conducted among non-parturient patients undergoing surgical procedures under spinal anaesthesia to know the equipotent doses of norepinephrine and mephentermine for the management of SAIH.
CONCLUSION
Intravenous norepinephrine is more effective than mephentermine in terms of response percentage of first dose and maintaining stable maternal heart rate without any untoward effect on Apgar score following spinal anaesthesia induced hypotension in elective caesarean section. Although intravenous boluses of both norepinephrine and mephentermine are equally effective in maintaining systolic blood pressure, more number of boluses of norepinephrine are required compared to mephentermine.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ganeshanavar A, Ambi US, Shettar AE, Koppal R, Ravi R. Comparison of bolus phenylephrine, ephedrine and mephentermine for maintenance of arterial pressure during spinal anaesthesia in caesarean section. J Clin Diagn Res. 2011;5:948–52. [Google Scholar]
- 2.Cyna AM, Andrew M, Emmett RS, Middleton P, Simmons SW. Techniques for preventing hypotension during spinal anaesthesia for caesarean section (Review) Cochrane Database Syst Rev. 2006;4:1–235. doi: 10.1002/14651858.CD002251.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Kansal A, Mohta M, Sethi AK, Tyagi A, Kumar P. Randomised trial of intravenous infusion of ephedrine or mephentermine for management of hypotension during spinal anaesthesia for caesarean section. Anaesthesia. 2005;60:28–34. doi: 10.1111/j.1365-2044.2004.03994.x. [DOI] [PubMed] [Google Scholar]
- 4.Carvalho B, Dyer RA. Norepinephrine for spinal hypotension during cesarean delivery another paradigm shift? Anesthesiology. 2015;122:728–30. doi: 10.1097/ALN.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 5.Ngan Kee WD. A random-allocation graded dose-response study of norepinephrine and phenylephrine for treating hypotension during spinal anesthesia for cesarean delivery. Anesthesiology. 2017;127:934–41. doi: 10.1097/ALN.0000000000001880. [DOI] [PubMed] [Google Scholar]
- 6.Gandhi KA, Jain K. Management of anaesthesia for elective, low-risk (Category 4) caesarean section. Indian J Anaesth. 2018;62:27–34. doi: 10.4103/ija.IJA_459_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fakherpour A, Ghaem H, Fattahi Z, Zaree S. Maternal and anaesthesia-related risk factors and incidence of spinal anaesthesia-induced hypotension in elective caesarean section: A multinomial logistic regression. Indian J Anaesth. 2018;62:44–54. doi: 10.4103/ija.IJA_416_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasanin A, Mokhtar AM, Badawy AA, Fouad R. Post-spinal anesthesia hypotension during cesarean delivery, a review article. Egypt J Anaesth. 2017;33:189–93. [Google Scholar]
- 9.Mohta M, Sai Janani S, Sethi AK, Agarwal D, Tyagi A. Comparison of phenylephrine hydrochloride and mephentermine sulphate for prevention of post spinal hypotension. Anaesthesia. 2010;65:1200–5. doi: 10.1111/j.1365-2044.2010.06559.x. [DOI] [PubMed] [Google Scholar]
- 10.Das S, Potli S, Madhusudhana R, Krishnamurthy D. A Comparative Study of Phenylephrine, Ephedrine and Mephentermine for Maintenance of Arterial Pressure during Spinal Anaesthesia in Caesarean Section IOSR-JDMS. 2015;14((Issue 1, ver VII)):80–5. [Google Scholar]
- 11.Modak A, Saranya R. Comparison of bolus phenylephrine and mephentermine for maintenance of arterial pressure during spinal anaesthesia in caesarean section. Int J Sci Res. 2016;5:142–4. [Google Scholar]
- 12.Mets B. Should norepinephrine, rather than phenylephrine, be considered the primary vasopressor in anesthetic practice? Anesth Analg. 2016;122:1707–14. doi: 10.1213/ANE.0000000000001239. [DOI] [PubMed] [Google Scholar]
- 13.El Shafei MM, El Gendy HA, El Fawy DM. Norepinephrine versus ephedrine for the prevention of spinal anesthesia-induced hypotension in coronary artery disease patients undergoing knee arthroscopy. Ain-Shams J Anaesthesiol. 2015;8:424–8. [Google Scholar]
- 14.Sharkey AM, Siddiqui N, Downey K, Ye XY, Guevara J, Carvalho JC. Comparison of intermittent intravenous boluses of phenylephrine and norepinephrine to prevent and treat spinal-induced hypotension in cesarean deliveries: Randomized controlled trial. Anesth Analg. 2019;129:1312–8. doi: 10.1213/ANE.0000000000003704. [DOI] [PubMed] [Google Scholar]
- 15.Puthenveettil N, Sivachalam SN, Rajan S, Paul J, Kumar L. Comparison of norepinephrine and phenylephrine boluses for the treatment of hypotension during spinal anaesthesia for caesarean section – A randomised controlled trial. Indian J Anaesth. 2019;63:995–100. doi: 10.4103/ija.IJA_481_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohta M, Dubey M, Malhotra RK, Tyagi A. Comparison of the potency of phenylephrine and norepinephrine bolus doses used to treat post-spinal hypotension during elective caesarean section. Int J Obstet Anesth. 2019;38:25–31. doi: 10.1016/j.ijoa.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Ngan Kee WD, Lee SWY, Tan PE. Randomized double-blinded comparison of norepinephrine and phenylephrine for maintenance of blood pressure during spinal anesthesia for cesarean delivery. Anesthesiology. 2015;122:736–45. doi: 10.1097/ALN.0000000000000601. [DOI] [PubMed] [Google Scholar]
- 18.Elnabtity AM, Selim MF. Norepinephrine versus ephedrine to maintain arterial blood pressure during spinal anesthesia for cesarean delivery: A prospective double-blinded trial. Anesth Essays Res. 2018;12:92–7. doi: 10.4103/aer.AER_204_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Onwochei DN, Ngan KW, Fung L, Downey K, Xiang YY, Carvalho JC. Norepinephrine intermittent intravenous boluses to prevent hypotension during spinal anesthesia for cesarean delivery: A sequential allocation dose finding study. Anesth Analg. 2017;125:212–8. doi: 10.1213/ANE.0000000000001846. [DOI] [PubMed] [Google Scholar]
- 20.Awad AAE. Administration of ephedrine versus norepinephrine for management of post-spinal hypotension during lower limb orthopedic surgery. Clin Pract. 2019;8:1–9. [Google Scholar]