Abstract
The MERCURY II study demonstrated the use of MRI-based risk factors such as extramural venous invasion (EMVI), tumor location, and circumferential resection margin (CRM) involvement to preoperatively predict pCRM (pathological CRM) outcomes for lower rectal tumors in a mixed group of upfront operated patients and patients who received neoadjuvant treatment. We aim to study the applicability of results of MERCURY II study in a homogeneous cohort of patients who received neoadjuvant chemoradiation (NACTRT) prior to surgery. After Institutional Review Board approval, post NACTRT restaging MRI of 132 patients operated for low rectal cancer between 2014 and 2018 were retrospectively reviewed by two radiologists for site of tumor, EMVI status, distance from anal verge (< 4 or > 4 cm), and mrCRM positivity. Findings were compared with post surgery pCRM outcomes using Fisher’s exact test. Only 9/132(7%) patients showed pCRM involvement on histopathology, 8 of them being CRM positive on MRI (p = 0.01). The positive predictive value (PPV) of mrCRM positive status and pCRM status was 12.7% (95% CI: 9.7–16.5%), while the negative predictive value was 98.5% (95% CI: 91.4–99.8%) (p = 0.01). EMVI positive and anteriorly located tumors showed higher incidence of pCRM positivity but were not found to be significant (15% vs 5.2% and p = 0.13 and 8.6% vs 2.1% and p = 0.28, respectively). Unsafe mrCRM was the only factor significantly associated with pCRM positivity on post neoadjuvant restaging MRI. Tumors less than 4 cm from anal verge, anterior tumor location, and mrEMVI positivity did not show statistically significant results to predict pCRM involvement.
Keywords: Magnetic resonance imaging (MRI), Circumferential resection margin (CRM), Neoadjuvant therapy, Low rectal carcinoma
Introduction
Low rectal cancer accounts for over a third of all rectal cancers [1–3]. Incomplete tumor resection, identified by pathological circumferential resection margin (pCRM) involvement, results in increased local recurrence and poor survival [4]. pCRM has been detected in 20–36% of lower rectal cancers, which is significantly worse than resection outcomes for upper rectal cancers [1, 2, 5]. This is due to the close relationship with adjacent structures such as prostate and vagina anteriorly, as also due to attempts at sphincter preservation [6, 7]. Surgical management of low rectal cancer thus remains a big challenge.
Rectal cancer treatment has undergone modification in recent years with chemoradiotherapy becoming standard practice preoperatively to downstage advanced tumors [8]. The prospective MERCURY II study has reported the utility of MRI findings to preoperatively assess the “tumor-mesorectal fascia relationship” and predict pCRM outcomes for lower rectal tumors. It concluded that the presence of extramural venous invasion on MRI (mrEMVI), tumors located < 4 cm from anal verge, and anteriorly located tumors are independent risk factors for pCRM positivity [1].
The MERCURY II study included a heterogeneous group of subjects, including both upfront operated patients (58.8%) and those who received neoadjuvant treatment prior to surgery (41.2%). However, the accuracy and purpose of performing MRI in the baseline and the post neoadjuvant therapy settings are quite different, and grouping them together for analysis may not be the optimal way to evaluate the role of MRI in these settings. Hence, it is not clear whether the results of MERCURY II can be applied to only one “pure” subset of patients (i.e., either upfront operated patients or those operated after neoadjuvant therapy). In our institution, the majority (> 75%) of rectal cancer patients have locally advanced tumors and receive neoadjuvant treatment prior to surgery to reduce tumor size and improve resectability [9]. We studied the applicability of results of MERCURY II study in a homogeneous cohort of patients undergoing surgery for rectal cancer following neoadjuvant therapy. The findings on post neoadjuvant therapy follow-up MRI imaging were compared with post surgery histopathology data for all subjects.
Material and Methods
Subjects
After approval by our Institutional Review Board, we retrospectively identified 190 consecutive patients who received neoadjuvant therapy for rectal cancer between 2014 and 2018 from the institutional database. All patients had a pathologically proven diagnosis of rectal adenocarcinoma and preoperative MRI for local staging performed at our institute. Out of this group of patients, the ones with low rectal tumors < 8 cm from the anal verge (henceforth referred to as lower rectal tumors) were selected for the study. All the patients in the selected subset were operated, after receiving neoadjuvant treatment in the form of chemoradiotherapy and presurgery MRI.
Clinical and Histopathologic Data
The demographic data, histopathology, and treatment details were extracted from the institutional electronic medical records. The histopathology was reported by a dedicated gastrointestinal oncopathologist in all cases. Presence or absence of positive (involved) pCRM status defined as tumor < 1 mm from the cut specimen margin was documented in all patients and correlated with MRI findings [10].
Imaging and Image Analysis
Post neoadjuvant therapy follow-up MRI study was available for all patients. MRI images were acquired on 1.5T (GE Healthcare, Milwaukee, USA), 1.5T (Philips Medical Systems, Eindhoven, Netherlands), or 3T (GE Healthcare, Milwaukee, USA) equipment in our institute using the institutional MRI rectal protocol. This included large FOV (field of view) T1W and T2W axial and T2W sagittal sequences of the pelvis, small FOV thin oblique axial and oblique coronal T2W sequences along the plane of the rectal tumor and axial diffusion weighted images (DWI). No intravenous contrast was administered in any of the patients.
The images were retrospectively and systematically reviewed on Centricity PACS (GE Healthcare, Milwaukee, USA) workstation by two oncoradiologists in consensus, with 10 and 5 years of experience respectively, who were blinded to the histopathologic findings. The senior oncoradiologist was fellowship trained in abdominal imaging and a dedicated colorectal and gastrointestinal radiologist.
The patients were stratified on the immediate pre-surgery MRI based on site of tumor (anterior or not anterior), EMVI status, distance of tumor from anal verge (less or more than 4 cm), and MRI CRM positivity (CRM threatened tumors were considered positive).
The distance from anal verge was determined by the distance between the inferior tumor edge and the anal verge on the sagittal MRI images. Tumor location between 10 and 2 o’clock on axial images was considered an anterior rectal location. Closest location of tumor or EMVI or malignant node within 1 mm from the mesorectal fascia or levator muscle was recorded as positive CRM [11]. CRM was also considered to be involved on MRI, if there was an invasion into the intersphincteric plane or beyond [1]. Extramural venous invasion was considered positive when the tumor signal intensity was expanding the mesorectal vessels [1].
The association between MRI findings and final pCRM status were evaluated using Fisher’s exact test.
Treatment
All the cases were discussed in the colorectal cancer multidisciplinary meetings held biweekly at our institute attended by surgeons, radiation oncologists, radiologists, and pathologists. Neoadjuvant chemoradiotherapy was decided based upon presence of imaging features that precluded upfront surgery in our treatment algorithm, namely, > T3 stage on MRI (tumor extension beyond the muscularispropria) CRM threatened or involved, node positivity on MRI, or internal sphincter involvement.
Patients with stage 3 and non-threatened CRM, N1 stage, or having lateral pelvic nodes were offered long-course or short-course radiotherapy [12].
The choice of surgery was decided based on the tumor stage on post-treatment MRI, which included abdominoperineal resection (APR), extralevator APR (ELAPE), low anterior resection, intersphincteric resection, pelvic exenteration, or extended TME (vascular approach sacrificing nerves, excision of seminal vesicles, prostate shave, vaginal excision). While the abdominal approach for extralevator APE stopped above at the level of S4, seminal vesicle, and laterally after taking middle rectal vessels, the perineal approach was performed in supine position using 2 large Devers and transection of coccyx. This technique has been described earlier by our group and adopted since 2015 [13, 14].
The tumor extent and predicted margin involvement on MRI was used to decide the surgical approach between total mesorectal excision (TME) and beyond TME surgery.
Results
We identified consecutive 190 cases in which neoadjuvant therapy for rectal cancer was administered. Forty-five out of 190 had high rectal tumor location on MRI and were excluded from the study. Of the remaining 145 patients, 13 did not have post neoadjuvant MRI scans in our system and were hence excluded. The remaining 132 patients were included in our study cohort (Fig. 1). The median patient age was 52 years. There were 72 males and 60 females in the study.
Fig. 1.
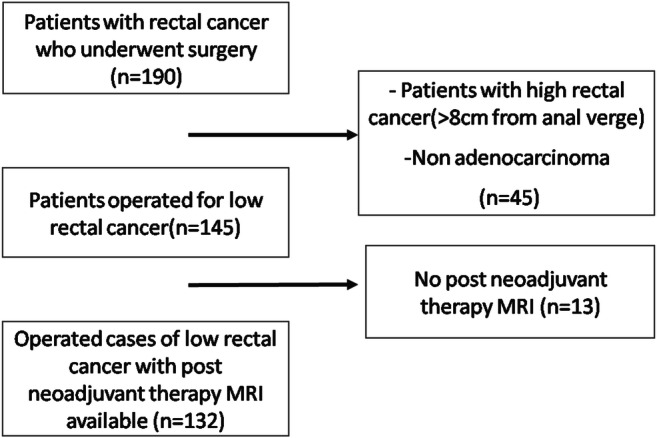
Consort diagram for enrollment of patients
MRI Findings
The tumor characteristics on MRI and pathology findings are summarized in Tables 1 and 2. Overall, 93/132 (70%) patients had anterior tumor location, with 54/132 (41%) having a tumor <4 cm from the anal verge. Sixty-three out of 132 (48%) tumors were CRM positive on the pre-surgical MRI, with mrEMVI being present in 20/132 (15%) patients.
Table 1.
The proportion of low rectal cancer cases with pCRM involvement according to MRI assessed tumor characteristics
| Tumor characteristics on MRI | Number of cases (out of 132) | pCRM involvement | PPV (95% CI) | NPV (95% CI) | p Value |
|---|---|---|---|---|---|
| Quadrant of tumor invasion | 8.6% (6.8–10.9%) | 97.4% (85.5–9.6%) | p = 0.28 | ||
| Anterior | 93 (70) | 8 (8.6) | |||
| Others | 39 (30) | 1 (2.5) | |||
| mrEMVI status | 15% (6–32.9%) | 94.6% (91.7–6.6%) | p = 0.13 | ||
| Positive | 20 (15) | 3 (15) | |||
| Negative | 112 (85) | 6 (5.3) | |||
| Height (from the anal verge) | 7.4% (3.6–14.6%) | 93.6% (88.9–6.4%) | p = 1 | ||
| < 4 cm | 54 (41) | 4 (7.4) | |||
| > 4 cm | 78 (49) | 5 (6.4) | |||
| MrCRM status | 12.7% (9.7–6.5%) | 98.5% (91.4–9.8%) | p = 0.01 | ||
| Positive | 63 (48) | 8 (12) | |||
| Negative | 69 (52) | 1 (1.4) | |||
Table 2.
Risk in numbers and percentage (in brackets) of pCRM involvement in patients with low rectal cancer, according to the four preoperative factors assessed on MRI
| mrEMVI status | Tumor site | MRI predicted CRM SAFE UNSAFE Distance from anal verge > 4 cm < 4 cm > 4 cm < 4 cm |
|||
|---|---|---|---|---|---|
| Negative | Not Anterior | 0/16 | 0/9 | 0/6 | 1/4 (25) |
| Negative | Anterior | 0/21 | 1/19 (5) | 2/19(10) | 2/18 (11) |
| Positive | Not Anterior | 0/1 | 0/0 | 0/3 | 0/0 |
| Positive | Anterior | 0/2 | 0/1 | 3/10 (30) | 0/3 |
Treatment
Surgical treatment was planned in the multidisciplinary tumor boards in consultation with the radiologist in all cases, with the type and extent of surgery decided based on the post-treatment restaging MRI findings. Sixty-one patients underwent abdominoperineal resection (extralevator), and 50 underwent low anterior resection (TME or extended TME). Pelvic exenteration was performed for 10 and intersphincteric resection for 11 patients. Out of the 9 patients who had pCRM involvement, 7 had undergone ELAPE, and pelvic exenteration was performed in the remaining 2 patients.
Histopathological Correlation
Only 9/132 (7%) patients had pCRM involvement on histopathology, with eight of these being CRM positive on MRI (p = 0.01). The positive predictive value (PPV) of mrCRM positive status and pCRM status was 12.7% (95% CI: 9.7–16.5%), while the negative predictive value (NPV) was 98.5% (95% CI: 91.4–99.8%) (p = 0.01). Ninety-three out of 132 (70%) tumors were anteriorly located, with eight of them (8.6%) having positive CRM on MRI. Similarly, 20/132 (15%) had EMVI positive status on MRI, with three of them (15%) having pCRM positivity. Finally, 54/132 (41%) tumors were less than 4 cm from the anal verge, with four of them (7.4%) being CRM positive on pathology.
Overall, EMVI positive tumors had a higher incidence of pCRM positivity (15% vs 5.2%). Similarly, anteriorly located tumors had a higher incidence of pCRM positive status (8.6% vs 2.1%). However, these were not found to be statistically significant.
Discussion and Conclusion
Rectal cancer in India has low prevalence and is seen in younger population (median age 46 years) with a higher percentage of signet ring tumors. It may account for a higher proportion of locally advanced stage at presentation [9]. The restaging MRI (performed after neoadjuvant treatment) is used in our institute for response assessment and to give a surgical roadmap to help decide on standard TME or extended TME approaches. These patients may also receive salvage chemotherapy in our institute if they remain CRM positive after chemoradiation. Our institution is a high volume center with more than 60 APRs performed annually in a standardized supine extralevator pattern by two experienced faculty, which has led to low perforation rates and acceptable positive CRM rates. Extended resection for anterior tumors with excision of seminal vesicles, posterior exenteration, or pelvic exenteration is based on the restaging MRI.
Simpson et al., in a retrospective study, reported 88/169 (52%) patients having baseline CRM positivity on MRI and who received neoadjuvant chemoradiation, after which 18/88 (20%) patients remained CRM positive on MRI, with 7/88 (8%) of these having positive CRM margins on pathology after resection [15]. On the other hand, out of the 70/88 patients who became CMR negative on MRI after neoadjuvant chemoradiation, 5/88 (6%) underwent margin positive resection. Our prior prospective institutional data showed that a relatively higher 39% of locally advanced rectal cancers remained CRM positive on MRI, but with an overall pathological CRM positivity rate of 5% after surgery [16].
In the current study, we found that out of the parameters already identified in MERCURY II study, mrCRM positivity was the only factor significantly associated with pCRM positivity when applied to this homogeneous cohort of post neoadjuvant therapy patients. Negative mrCRM also had a high negative predictive value in ruling out pCRM involvement. These findings are consistent with previously published literature.
The MERCURY study demonstrated that preoperative mrCRM assessment gave an accurate prediction of the pCRM and local recurrence. The accuracy for prediction of a clear margin in 97 patients was 77% (75/97, 69–86%CI) and negative predictive value of 98% (58/59) [2]. Ma et al. in their study of 203 patients found good accuracy of mrCRM for predicting involvement of pCRM of 84.2%, with sensitivity 50%, specificity 86.8%, NPV 95.9%, and PPV 21.9% (p < 0.0002) [17]. In the MERCURY II study, 25/279 post-treatment cases showed pCRM involvement, out of which 17 were mrCRM unsafe. Hence, post-treatment unsafe mrCRM cases had higher rates of pCRM involvement, 19.3% vs 4% (p < 0.001) [1].
As the anterior aspect of the mesorectum is disproportionately small, the resection margin for anterior tumors is closer to the mesorectal fascia, leading to a higher potential risk of CRM positivity [18]. We observed that the rate of pCRM involvement was higher for anterior tumors (8.6%) than non-anterior (2.5%) tumors, but this was not statistically significant. This could be due to the overall low pCRM positive patients. Other studies have observed a correlation of anterior tumor location with pCRM positivity or higher recurrence. Mo et al. retrospectively studied pathology slides of 58 patients who underwent total mesorectal excision for mid and low rectal cancer to study the impact of circumferential tumor location on CRM status. They found that pCRM positivity was more frequently observed in anterior tumors than in non-anterior tumors (41.1% vs 10.3%, p < 0.007) [18]. Chan et al. [19] reported that patients with anterior tumors had a higher recurrence rate (5-year LR 15.9% vs 5.8%, p < 0.009) than patients with non-anterior tumors. The MERCYRY II study showed that pCRM involvement was 2.8-fold more likely in the 35% (99/279) of tumors with anterior quadrant invasion risk (95% CI, 1.1–6.8, p < 0.027) [1].
Through many independent series, EMVI is known to be associated with worse overall outcomes and increased likelihood of disease recurrence [20–22]. Talbot et al. followed up 684 operated cases of rectal cancers and found that in the presence of mrEMVI, the 5-year survival rate was decreased to 33% (p < 0.001) as against 73% when venous invasion was not demonstrated [23]. Few studies have assessed the relationship between the EMVI status and pCRM involvement. In our study, pCRM involvement was more common in mrEMVI-positive patients (15%) than in EMVI-negative patients (5.2%). However, this was not statistically significant. As reported in previous studies, the higher rate of pCRM involvement in EMVI positive group could be due to mrEMVI being the reason for mrCRM positivity and inadequate downstaging of EMVI following neoadjuvant therapy [1, 24]. In a study of 133 cases, Smith et al. recorded that EMVI-positive tumors were significantly more likely to have positive CRM (18.7% vs 3.9%, p < 0·013) [21]. Similarly, according to the MERCURY II study, mrEMVI (19%, 54/279) was associated with a 3.8-fold increased risk of pCRM involvement [1]. These differed from the results of our study.
We observed no significant difference in pCRM involvement between tumor less than 4 cm from the anal verge and those more than 4 cm. There is variability in the published literature regarding this. In contrast to our results, in a study of 149 patients by Amir et al., compared with patients with mid-/upper rectal cancer, patients with low rectal cancers (< 5 cm) showed significantly higher rates of pathological positive circumferential resection margin involvement (14.1 vs 7.1%; p = 0.047) [5]. The MERCURY II study found that the tumors less than 4 cm from the anal verge carry a 3.4-fold increased pCRM involvement risk (95% CI 1.3–8.8, p < 0.006) [1]. However, a study by Bhanguet al. reported no significant difference in the positive pCRM rate between low (< 5 cm) and mid- to upper rectal tumors (3.4% vs 2.9%, p = 1.0) [25]. Similarly, Poulsen et al. also found that the correlation between mrMRF (mesorectal fascia) and pCRM was not influenced by tumor height [26].
Thus, overall, our findings were slightly different from the MERCURY II study. A reason for the discordance could be due to the fact that only 41.2% patients in the MERCURY II study received neoadjuvant treatment. MRI risk factors such as EMVI and mrCRM involvement could change and indeed resolve after neoadjuvant treatment, leading to the difference in findings.
It is thus important to not extrapolate such mixed data on to the post-treatment patient group completely. Importantly, the main goal of post-treatment MRI is to provide a surgical roadmap so that the surgeon can obtain R0 resections by modifying their surgeries accordingly. This seemed to be served, with only 7% patients having pCRM involvement, although mrCRM positivity was present in 48% tumors.
Our study has certain limitations. It is a retrospective study, with assessment of only the post neoadjuvant therapy MRI performed; the baseline MRI was not assessed. There was a possible selection bias due to ours being a tertiary care cancer center, with a potentially higher number of complex and advanced cases. Also, there was a low overall incidence of events (pCRM involvement), which could be responsible for our observations regarding anterior tumor location and EMVI positivity not reaching statistical significance. While a GI oncopathologist reported all the surgical specimens, all 26 participating centers in the Mercury trial had dedicated colorectal pathologists who also participated in pathology workshops and could dedicate much more time with each specimen [1]. It is possible that their evaluation may be stringent to detect even minor pCRM positivity. This may be one reason for low pCRM positivity in our study. Overall, the findings need to be further evaluated with a larger study for validation.
In conclusion, unsafe mrCRM was the only factor significantly associated with pCRM positivity on post neoadjuvant restaging MRI. Tumors less than 4 cm from anal verge, anterior tumor location, and mrEMVI positivity did not show statistically significant results to predict pCRM involvement.
Authors’ Contributions
Patra A, Baheti AD, Ankathi SK: radiologists who performed data collection, MRI analysis, and review of literature. The manuscript was primarily written by Dr. Patra and Dr. Baheti. Desouza A, Engineer R, Ostwal V, Ramaswamy A, Saklani A: data collection, review of literature, clinical details, and manuscript edits. All authors read and approved the final manuscript.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Battersby NJ, How ÃP, Moran ÃB, Bchir MB, Stelzner S, West NP, et al. Prospective validation of a low rectal cancer magnetic resonance imaging staging system and development of a local recurrence risk stratification model. : the MERCURY II study. Ann Surg 2016;263(4) [DOI] [PubMed]
- 2.Group MS Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ. 2006;333(7572):779. doi: 10.1136/bmj.38937.646400.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marr R, Birbeck K, Garvican J, Mapstone NP, Sebag-montefiore D. The modern abdominoperineal excision. Ann Surg. 2005;242(1):74–82. doi: 10.1097/01.sla.0000167926.60908.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor FGM, Quirke P, Heald RJ, Moran BJ, Blomqvist L, Swift IR. Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence : 5- year follow-up results of the MERCURY study. J Clin Oncol. 2014;32:34–43. doi: 10.1200/JCO.2012.45.3258. [DOI] [PubMed] [Google Scholar]
- 5.Amir M, Khan S, Ang CW, Hakeem AR, Scott N, Saunders RN, et al. The impact of tumour distance from the anal verge on clinical management and outcomes in patients having a curative resection for rectal Cancer. J Gastrointest Surg. 2017;21(12):2056–2065. doi: 10.1007/s11605-017-3581-0. [DOI] [PubMed] [Google Scholar]
- 6.Helewa RM, Park J. Surgery for locally advanced T4 rectal cancer : strategies and techniques. Clin Colon Rectal Surg. 2016;29(2):106–113. doi: 10.1055/s-0036-1580722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart DB, Dietz DW. Total mesorectal excision : what are we doing ? Clin Colon Rectal Surg. 2007;20(3):190–202. doi: 10.1055/s-2007-984863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mcbrearty A, Mccallion K, Rj M, Mcallister I, Mulholland K, Gilliland R, et al. Re-staging following long-course chemoradiotherapy for rectal cancer : does it influence management ? Ulster Med J. 2016;85(3):178–181. [PMC free article] [PubMed] [Google Scholar]
- 9.Patil PS, Saklani A, Mehta S, De Souza A, Bal M. Colorectal cancer in India: an audit from a tertiary center in a low prevalence area. Indian J Surg Oncol. 2017;8(4):484–490. doi: 10.1007/s13193-017-0655-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-sukhni E, Attwood K, Gabriel E, Nurkin SJ. Predictors of circumferential resection margin involvement in surgically resected rectal cancer : a retrospective review of 23 , 464 patients in the US National Cancer Database. Int J Surg. 2016;28:112–117. doi: 10.1016/j.ijsu.2016.01.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nougaret S, Reinhold C, Mikhael HW, Rouanet P, Bibeau F, Brown G. The use of MR imaging in treatment planning for patients with rectal carcinoma: have you checked the “DISTANCE”? Radiology. 2013;268(2):330–344. doi: 10.1148/radiol.13121361. [DOI] [PubMed] [Google Scholar]
- 12.Bujko K, Wyrwicz L, Rutkowski A, Malinowska M, Pietrzak L, Kryński J, Michalski W, Olędzki J, Kuśnierz J, Zając L, Bednarczyk M, Szczepkowski M, Tarnowski W, Kosakowska E, Zwoliński J, Winiarek M, Wiśniowska K, Partycki M, Bęczkowska K, Polkowski W, Styliński R, Wierzbicki R, Bury P, Jankiewicz M, Paprota K, Lewicka M, Ciseł B, Skórzewska M, Mielko J, Bębenek M, Maciejczyk A, Kapturkiewicz B, Dybko A, Hajac Ł, Wojnar A, Leśniak T, Zygulska J, Jantner D, Chudyba E, Zegarski W, Las-Jankowska M, Jankowski M, Kołodziejski L, Radkowski A, Żelazowska-Omiotek U, Czeremszyńska B, Kępka L, Kolb-Sielecki J, Toczko Z, Fedorowicz Z, Dziki A, Danek A, Nawrocki G, Sopyło R, Markiewicz W, Kędzierawski P, Wydmański J, Albiński J, Banaś R, Chmielowska E, Bal W, Baszczyk-Mnich J, Bialas M, Borowiec T, Bujko M, Cencelewicz A, Chomik K, Chwaliński M, Ciepela I, Dupla D, Florek A, Górnicki A, Jeziorski K, Józwicki W, Kobiela J, Koda M, Kołodziej P, Kruszewski P, Kryj M, Kuciel-Lisiecka G, Kwiatkowski R, Lachowski A, Liszka-Dalecki P, Majewski A, Majewski W, Majsak T, Maka D, Malka M, Mazurkiewicz A, Morawiec J, Nogal E, Olejniczak M, Olkowski D, Ostrowska-Cichocka K, Pietruszka M, Piotrkowski G, Plewicka M, Porzuczek-Zuziak D, Reszke J, Rychter A, Sadowski J, Salata A, Serkies K, Srutek E, Szóstak B, Tuziak T, Tyralik D, Skoczylas J, Wachua E, Wandzel P, Winkler-Spytkowska B, Wojtasik P, Wroński K, Zemal M, Zygulski I. Long-course oxaliplatin-based preoperative chemoradiation versus 5 x 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: results of a randomized phase III study. Ann Oncol. 2016;27:834–842. doi: 10.1093/annonc/mdw062. [DOI] [PubMed] [Google Scholar]
- 13.Jain K, Sasi S, Saklani AP, Kumar S. Short term outcomes following prone versus supine extra-levator abdominoperineal resection (ELAPR) for rectal cancer in a tertiary care cancer centre. Conference: Abstracts of the 14th Scientific and Annual Meeting of the European Society of Coloproctology, Austria Centre, 25–27 September 2019, Vienna. Color Dis 21(S3):76–77
- 14.Martijnse IS, Dudink RL, West NP, Wasowicz D, Nieuwenhuijzen GA, van Lijnschoten I, Martijn H, Lemmens VE, van de Velde CJ, Nagtegaal ID, Quirke P, Rutten HJ. Focus on extralevator perineal dissection in supine position for low rectal cancer has led to better quality of surgery and oncologic outcome. Ann Surg Oncol. 2012;19(3):786–793. doi: 10.1245/s10434-011-2004-9. [DOI] [PubMed] [Google Scholar]
- 15.Simpson GS, Eardley N, McNicol F, Healey P, Hughes M, Rooney PS. Circumferential resection margin (CRM) positivity after MRI assessment and adjuvant treatment in 189 patients undergoing rectal cancer resection. Int J Color Dis. 2014;29(5):585–590. doi: 10.1007/s00384-014-1846-6. [DOI] [PubMed] [Google Scholar]
- 16.Chandarana M, Arya S, de Menezes J-L, Engineer R, Ostwal V, Patil P, et al. Can CRM status on MRI predict survival in rectal cancers: experience from the Indian subcontinent. Indian J Surg Oncol. 2019;10(2):364–371. doi: 10.1007/s13193-019-00894-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma X, Li X, Xu L, Shi D, Tong T, Huang D, et al. (2015) Characteristics and prognostic significance of preoperative magnetic resonance imaging-assessed circumferential margin in rectal cancer. Gastroenterol Res Pract, vol [DOI] [PMC free article] [PubMed]
- 18.Mo B, Park Y, Jin S, Yeon K, Woo C, Lee S. ScienceDirect does circumferential tumor location affect the circumferential resection margin status in mid and low rectal cancer ? Asian J Surg. 2018;41(3):257–263. doi: 10.1016/j.asjsur.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Chan CLH, Bokey EL, Chapuis PH, Renwick AA, Dent OF Local recurrence after curative resection for rectal cancer is associated with anterior position of the tumour. Br J Surg. 1990;2006:105–112. doi: 10.1002/bjs.5212. [DOI] [PubMed] [Google Scholar]
- 20.Chand M, Siddiqui MRS, Swift I, Brown G, Chand M, Siddiqui MRS, et al. Systematic review of prognostic importance of extramural venous invasion in rectal cancer. World J Gastroenterol. 2016;22(4):1721–1726. doi: 10.3748/wjg.v22.i4.1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith NJ, Barbachano Y, Norman AR, Swift RI, Abulafi AM, Brown G. Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. Br J Surg. 2008;95:229–236. doi: 10.1002/bjs.5917. [DOI] [PubMed] [Google Scholar]
- 22.Bugg WG, Andreou AK, Biswas D, Toms AP, Williams SM. The prognostic significance of MRI-detected extramural venous invasion in rectal carcinoma. Clin Radiol. 2014;69(6):619–623. doi: 10.1016/j.crad.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 23.Talbot IC, Ritchie S, Leighton MH, Hughes AO, Bussey HJ, Morson BC. The clinical significance of invasion of veins by rectal cancer. Br J Surg. 1980;67:439–442. doi: 10.1002/bjs.1800670619. [DOI] [PubMed] [Google Scholar]
- 24.Yu SKT, Tait D, Chau I, Brown G (2013) MRI predictive factors for tumor response in rectal cancer following neoadjuvant chemoradiation therapy - implications for induction chemotherapy ? Radiat Oncol Biol [DOI] [PubMed]
- 25.Bhangu A, Rasheed S, Brown G, Tait D, Cunningham D, Tekkis P. Does rectal cancer height influence the oncological outcome ? Color Dis. 2014;16(10):801–808. doi: 10.1111/codi.12703. [DOI] [PubMed] [Google Scholar]
- 26.Poulsen LØ, Yilmaz MK, Oddershede L, Holt G, Eld M, Ljungmann K, et al. Is the accuracy of preoperative MRI stage in rectal adenocarcinoma influenced by tumour height ? Acta Oncol. 2018;57(6):728–734. doi: 10.1080/0284186X.2018.1433319. [DOI] [PubMed] [Google Scholar]


