Abstract
Studies that focus on disparities in care should aim to discern differences both within their communities and also among larger populations to improve the applicability of important findings. Such work should attempt to discern what factors may be influential in creating or contributing to racial inequities
Keywords: Race, Racial disparities, Healthcare disparities
Quality of life with fertility preservation
Gonadotoxic cancer treatments can limit or prematurely end the reproductive lifespan. The threat of infertility due to cancer treatments has been associated with increased distress and anxiety [1]. Fortunately, with the advent of gamete cryopreservation, it is possible for cancer survivors to maintain some aspect of fertility. The first step in fertility preservation is counseling. Survivors who receive adequate counseling often experience less regret and an improved quality of life [2]. Moreover, patients value not just counseling but also access to fertility preservation services in a timely fashion [3]. Medically indicated fertility preservation is a critical component of comprehensive cancer care but may not be equally accessed by all people in need.
Health care disparities in fertility care
Disparities in access to fertility services have existed since the advent of assisted reproductive technologies. In particular, women of color have consistently participated less in fertility evaluation and services compared with White women [4]. In addition, several studies have demonstrated racial differences in ART outcomes [5, 6]. Generally speaking, women of color tend to have lower implantation and pregnancy rates [7]. Black women may present at an older age for treatment and certainly have a higher incidence of fibroids—both factors that may potentially influence success with ART treatment [8]. Recent data suggests that differences in sex-steroid hormone levels differ by race and may also be associated with pregnancy outcomes [9]. Importantly, limited data suggest that there are racial differences in medically indicated fertility preservation counseling although the influence of other sociodemographic factors are conflicting [10, 11].
Potential disparities in access to medically indicated fertility preservation
The authors of “Equal opportunity for all? An analysis of race and ethnicity in fertility preservation in a major American city” described their population of patients seeking medically indicated fertility preservation for cancer and compared them to an expected distribution of patients that should be seeking or completing treatment based upon New York City census data. They demonstrated significant inequity in the uptake of fertility preservation services by race.
Understanding the reasons why patients decline care is critical to improving the quality of life among cancer survivors. First, an accurate assessment of where and how patients access fertility preservation services at the local and national level is important to determining whether or not gaps in access to care exist. For instance, it is conceivable that patients in a predominantly African American community who are counseled by oncologists and reproductive endocrinologists in their community may not decline care at the same rates as patients in a community where Black people are considered a minority group. Without reliable data on the uptake of fertility preservation at the local, national, and global levels, it is difficult to target interventions to close perceived healthcare caps.
Second, beyond defining the disparities in access to care, we should seek to understand if socioeconomic factors influence the reasons that patients decline care. Although race and socioeconomic status in the USA are often linked, there may be additional mediators and confounders that might result in the disparities seen by the authors of this study. Parity, marital status, or religious beliefs may influence one’s decision to pursue fertility preservation and should be accounted for in any studies that examine the utilization of fertility preservation.
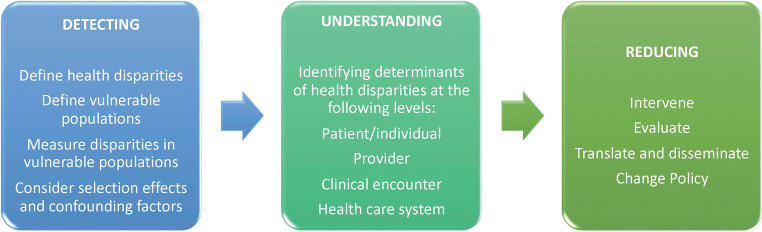
Defining inequities and influential factors that may impact access to care are the first steps in a framework proposed by Kilbourne et al. to close health care caps. Following knowledge acquisition, it is important to understand the determinants of such disparities and finally reduce the disparity through interventions, education, and policy changes (Fig. 1) [12]. The authors should be commended for their investigation which contributes to defining the potential disparity in access to medically indicated fertility preservation. Future studies on disparities in the utilization of fertility preservation should continue to define the affected populations and seek to understand the underlying reasons why such disparities occur. To close the gap in both access and opportunity for fertility preservation, studies should capture the barriers that people of color face when contemplating whether or not to freeze oocytes or embryos.
Fig. 1.
Framework for a health disparity research agenda. Adapted from Kilbourne et al. Advancing Health Disparities Research within the. Health Care System: A conceptual Framework AM J Public Health 2006 Dec; 96(12): 2113-2121
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lawson AK, Klock SC, Pavone ME, Hirshfeld-Cytron J, Smith KN, Kazer RR. Psychological counseling of female fertility preservation patients. J Psychosoc Oncol. 2015;33(4):333–353. doi: 10.1080/07347332.2015.1045677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, Melisko ME, Cedars MI, Rosen MP. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012;118(6):1710–1717. doi: 10.1002/cncr.26459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anazodo A, Laws P, Logan S, Saunders C, Travaglia J, Gerstl B, Bradford N, Cohn R, Birdsall M, Barr R, Suzuki N, Takae S, Marinho R, Xiao S, Qiong-Hua C, Mahajan N, Patil M, Gunasheela D, Smith K, Sender L, Melo C, Almeida-Santos T, Salama M, Appiah L, Su I, Lane S, Woodruff TK, Pacey A, Anderson RA, Shenfield F, Ledger W, Sullivan E. How can we improve oncofertility care for patients? A systematic scoping review of current international practice and models of care. Hum Reprod Update. 2019;25(2):159–179. doi: 10.1093/humupd/dmy038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chandra A, Copen CE, Stephen EH. Infertility service use in the United States: data from the National Survey of Family Growth, 1982-2010. Natl Health Stat Rep. 2014;73:1–21. [PubMed] [Google Scholar]
- 5.Fujimoto VY, Luke B, Brown MB, Jain T, Armstrong A, Grainger DA, Hornstein MD, Society for Assisted Reproductive Technology Writing Group Racial and ethnic disparities in assisted reproductive technology outcomes in the United States. Fertil Steril. 2010;93(2):382–390. doi: 10.1016/j.fertnstert.2008.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Humphries LA, Chang O, Humm K, Sakkas D, Hacker MR. Influence of race and ethnicity on in vitro fertilization outcomes: systematic review. Am J Obstet Gynecol. 2016;214(2):212.e1–212.e17. doi: 10.1016/j.ajog.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Quinn MM, Fujimoto VY. Racial and ethnic disparities in assisted reproductive technology access and outcomes. Fertil Steril. 2016;105(5):1119–1123. doi: 10.1016/j.fertnstert.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Missmer SA, Seifer DB, Jain T. Cultural factors contributing to health care disparities among patients with infertility in Midwestern United States. Fertil Steril. 2011;95(6):1943–1949. doi: 10.1016/j.fertnstert.2011.02.039. [DOI] [PubMed] [Google Scholar]
- 9.Hill MJ, Royster GD, Taneja M, Healy MW, Zarek SM, Christy AY, et al. Does elevated progesterone on day of oocyte maturation play a role in the racial disparities in IVF outcomes? Reprod BioMed Online. 2017;34(2):154–161. doi: 10.1016/j.rbmo.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodman LR, Balthazar U, Kim J, Mersereau JE. Trends of socioeconomic disparities in referral patterns for fertility preservation consultation. Hum Reprod. 2012;27(7):2076–2081. doi: 10.1093/humrep/des133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Letourneau JM, Smith JF, Ebbel EE, Craig A, Katz PP, Cedars MI, Rosen MP. Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer: fertility preservation disparities. Cancer. 2012;118(18):4579–4588. doi: 10.1002/cncr.26649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96(12):2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]