Abstract
Background & objectives
Polycystic ovary syndrome (PCOS) is the most common endocrinal disorder, and the greatest cause of infertility in women. Despite availability of individual data on impact of multiple endocrinal, reproductive and even metabolic factors in PCOS individuals, the data on the co-existence of BED and depression in PCOS patients with its relationship on the quality of life in Saudi Arabian females is not found. Hence this study is aimed to elucidate the implication of PCOS on eating behaviour, induction of depression and general health quality in Saudi Arabian population of Riyadh.
Materials and methods
This is a cross-sectional study carried out in multiple health facilities of Riyadh from January to March 2019. The study samples (494) were recruited by convenience sampling and administered validated questionnaire by trained research participants. The data obtained was analysed by binary logistic regression using SPSS-IBM 25.
Results
Of the total 494 women participated in the study, 23.48% (116) were PCOS individuals. The odds of developing abnormal health related quality of (HRQ) in patients with PCOS was significantly (P = 0.000, OR = 3.472) high when compared to non-PCOS participants. The odds of showing high binge eating disorder (BED, P = 0.007, OR = 2.856) and depression (P = 0.000, OR = 2.497) scores in PCOS participants were significantly more than patients who were not having PCOS. Out of the three parameters studied, abnormal health related quality of life possessed a higher influence of PCOS compared to depression and abnormal eating behavior.
Interpretation & conclusion
In conclusion, the present study shows that women with PCOS are at a significant risk for depressive disorders, disorganized eating behavior and impaired quality of life. Therefore, necessary care and screening is required to minimize the impact of PCOS on already burdened individuals.
Keywords: Polycystic ovary syndrome, Binge eating disorder, Health related quality of life, Depression disorder, Riyadh
1. Introduction
One of the most common endocrinal disorder seen during reproductive age (Bozdag et al., 2016) of women is polycystic ovary syndrome (PCOS) with high rate of infertility. As per the new Rotterdam criteria formulated by the European Society for Human Reproduction & Embryology and the American Society for Reproductive Medicine, PCOS is characterized by the presence of two of the three features of oligo/anovulation, hyperandrogenism or polycystic ovaries on ultrasound with exclusion of other etiologies such as congenital adrenal hyperplasia, androgen secreting tumors, Cushing syndrome, thyroid dysfunction and hyperprolactinemia (Teede et al., 2018). The other common clinical features of PCOS include: hirsutism, moderate to severe acne, irregular menses, obesity and metabolic syndrome (Elghblawi 2007).
Studies have reported an association of PCOS with multiple endocrinal, reproductive and even metabolic risks that reduces quality of life through the life cycle of the affected female (Dokras et al., 2011). Metabolic risks include impaired glucose tolerance, type II diabetes mellitus, dyslipidemia, breast cancer and cardiovascular complications which are mainly age-related existence of hypertension, and subtle endothelial and vascular changes. Reproductive risks include infertility, endometrial and ovarian cancer (Daniilidis and Dinas, 2009). In addition, PCOS patients are more likely to develop psychiatric disorders including depression and anxiety (Asdaq and Yasmin, 2020). Some reports have proposed that poor body image and enhanced body weight due to PCOS are contributory factors for mood disorders in these patients (Barry and Kuczmierczyk, 2011). A study showed a fall in quality of life in patients with PCOS probably due to PCOS induced obesity and infertility (Amiri et al., 2018). Some of the eating disorders like anorexia nervosa (AN), bulimia nervosa (BN) and binge eating disorder (BED) produces changes in the body image. The most common ED is BED, a 2% prevalence is reported in general public that increases to about 20% in adults seeking weight loss (Cossrow et al., 2016).
Since both, BED and PCOS, has been associated with diabetes mellitus, obesity, and hypertension (Dokras, 2013), it is worthwhile to investigate the status of BED in patients with PCOS. There is an independent relationship found between depression and eating disorder (ED) (Hudson et al., 2007) with an occurrence of major depression in 32% of BED patients. Also, there are individual reports of prevalence of BED and depression in PCOS, however, the data on the co-existence of BED and depression in PCOS patients is not yet reported. Hence, this study wss designed to explain the association of polycystic ovary syndrome (PCOS) with eating disorder, specifically, BED and depression as well as to determine the impact of these features on quality of life among women in Riyadh, Saudi Arabia.
2. Methods
2.1. Sampling
The current study is a cross-sectional study carried out in multiple health centers (Prince Sultan Military City, King Saud Medical City, Prince Mohammed Bin Abdulaziz Hospital and King Salman bin Abdulaziz Hospital) of Riyadh, Saudi Arabia during January to March 2019. The study centers selected in this study were government tertiary care hospitals located in Riyadh with large number of daily patient flow to Gynecology and Obstetrics unit. Ethical approval to conduct this study was obtained from Institutional Review Committee of Al-Maarefa University, Riyadh (MCST (AU)-COP 1901/RC).
The sample size of the study participant was calculated based on the population size of Riyadh in the desired age group (20–54 years) based on specifications given in https://www.surveysystem.com/sscalc.htm. Considering 95% confidence level and 5% confidence interval and a female population of 1,806,309 in Riyadh (https://www.stats.gov.sa/en/5680), the sample required was 384. This study included 494 samples with 116 participants with confirmed PCOS and 378 participants considered as control.
The PCOS group consisted of female participants seeking management of PCOS in any of the study centers mentioned above with the diagnosis of PCOS based on Rotterdam criteria and confirmed by chart review. Participants of the study were recruited by convenient sampling when they visited the study centers for their regular follow ups. Women with confirmed pregnancy, postmenopausal or those diagnosed with adrenal or pituitary disorders or have any specific type of cancer were excluded from the study.
The control participants were patients presenting for general gynecologic care in the study centers in an age group of 20–54 years. All women who have severe physical illness, mentally handicapped, declined to participate as well as women coming for follow up for pregnancy were excluded from the group.
2.2. Study questionnaire
The questionnaire of this study was designed to achieve the desired objectives. Both face and content validity of the Arabic version of questionnaire was done prior to its administration. The questionnaire form had four major sections. Section number one dealt with questions related to sociodemographic information such as age (≤30 years/ greater than 30 years), education (high ≥ bachelor degree/ low ≤ secondary), employment (employed/not employed), social status (widow, married, divorced and single), PCOS prevalence (no/yes) and BMI (obese ≥ 30/non-obese < 30). The section two had questions about eating behavior in the past 14 days (2 weeks). The first three questions in this section were to explore general eating behavior whereas the next three questions were specifically to know the “binge eating”. It was mainly focused on eating what others would regard as an unusually large amount of food for the circumstances, accompanied by a sense of having lost control over eating (Fairburn and Beglin, 1994). The participants were requested to rate their experience of each item in a 4 point frequency scale (1 to 4) based on the level of their experience. The cutoff value for eating disorder was kept as 08/24.
The depression subscale from DASS 21 was used for the third section of this questionnaire (Lovibond and Lovibond, 1995). It measures low experience of positivity, hopelessness & reduced self-esteem. The participants were asked to rate their experience of each item during the last seven days in a 4-point frequency scales (0–3) based on the level of severity. The rating of ‘0’ represent 'Did not apply to me at all', while, ‘1’ Applied to me to some degree, whereas, ‘2’ applied to me to a considerable degree, and ‘3’ is an acknowledgement of 'Applied to me most of the time'. The scores of depression were added up and multiplied by 2 to get the actual score (Gomez, 2016). The cutoff value for depression was kept as 10 (Asdaq and Yasmin, 2020). The last section of the questionnaire was related to health related quality of life in the last 14 days. There were four questions in this section which mainly cover the overall health status, physical and mental health and their impact in daily activities (Palermo et al., 2008, Cronin et al., 1998). The participants were instructed to share their experience in a 4 point scale (1–4). The cutoff value for impairment in health related quality of life was 07/16.
2.3. Data collection
The female Pharm.D students of College of Pharmacy were given adequate training on the method of introduction of the questionnaire to the participants, presenting the survey form to them and gathering their responses. The nursing staff of the study centers also helped the data collection team in identifying the eligible surveyors. The participants who ought for help in filling their responses were provided necessary support through a face-to-face interview. The validated Arabic version of DASS-21 questionnaire was used in this study. The details of the participants were kept confidential and they were assured of anonymous processing of their response. They were informed about their right to refuse or withdraw at any time without any disadvantage or prejudice. The participants were briefed about the purpose, procedure and potential risk in Arabic language and they consented by ticking on the “agree to participate” column on the first page of questionnaire.
2.4. Statistical analysis
The statistical analysis was done using SPSS IBM statistical package (version 25). The responses obtained in the survey for all the four sections were entered based on the explanation given above and description analysis was done to develop contingency table. Pearson Chi-square was done to check the statistical significance of differences among proportions of categorical data. The binary logistic regression analysis was done to obtain the odds ratios (ORs) and 95% CIs (confidence intervals) so as to determine the impact of PCOS on eating behavior, depression and health related quality of life. A P-value of less than 0.05 was considered significant.
3. Results
3.1. Sociodemographic description of the participants
Of the total 494 women participated in the study, 23.48% (116) of them were confirmed with PCOS and the remaining 76.51% (378) of the participants were recruited as non-PCOS participants. As depicted in Table 1, more than 65% of the study samples were in an age group of greater than 30 years and overall 55.66% of the participants were highly educated. Further, most of the recruiters of this study unemployed (66.80%) and divorced (56.27%). However, based on the personal declaration of the height and eight of the surveyors, large number of them were within the normal BMI range (<30).
Table 1.
Sociodemographic features and Binge eating disorder.
| Characteristics |
BED Frequency (percentage) |
P value* | Odds ratio | 95% Confidence interval |
|||
|---|---|---|---|---|---|---|---|
| Not present | Present | Total | Lower | Upper | |||
| Age | 0.950 | 1.017 | 0.606 | 1.706 | |||
|
26 (15.1) | 146 (84.9) | 172 (34.81) | ||||
|
48 (14.9) | 274 (85.1) | 322 (65.18) | ||||
| Total | 74 (15) | 420 (85) | 494 (100) | ||||
| Education | 0.187 | 0.717 | 0.437 | 1.177 | |||
|
36 (13.1) | 239 (86.9) | 275 (55.66) | ||||
|
38 (17.4) | 181 (82.6) | 219 (44.33) | ||||
| Total | 74 (15) | 420 (85) | 494 (100) | ||||
| Employment status | 0.079 | 0.603 | 0.342 | 1.064 | |||
|
18 (11.1) | 146 (89) | 164 (33.19) | ||||
|
56 (17) | 274 (83) | 330 (66.80) | ||||
| Total | 74 (15) | 420 (85) | 494 (100) | ||||
| Social status | 0.137 | Risk estimate statistics is not computed as it is not 2 × 2 table | |||||
|
4 (33.3) | 8 (66.7) | 12 (2.43) | ||||
|
7 (11.5) | 54 (88.5) | 61 (12.34) | ||||
|
37 (13.3) | 241 (86.7) | 278 (56.27) | ||||
|
26 (18.2) | 117 (81.8) | 143 (28.94) | ||||
| Total | 74 (15) | 420 (85) | 494 (100) | ||||
| PCOS status | 0.005 | 2.856 | 1.328 | 6.141 | |||
|
66 (17.5) | 312 (82.5) | 378 (76.51) | ||||
|
8 (6.9) | 108 (93.1) | 116 (23.48) | ||||
| Total | 74 (15) | 420 (85) | 494 (100) | ||||
| BMI | 0.045 | 1.733 | 1.008 | 2.979 | |||
|
53 (17.5) | 249 (82.5) | 302 (61.13) | ||||
|
21 (10.9) | 171 (89.1) | 192 (38.86) | ||||
| Total | 74 (15) | 420 (85) | 494 (100) | ||||
Pearson Chi-square test (2-sided).
3.2. Binge eating disorder and demographic features
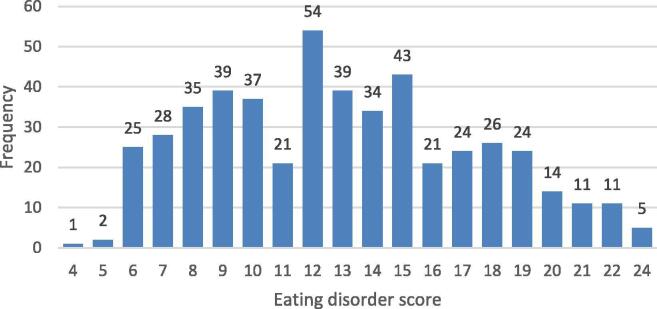
As shown in Table 1, significant (P = 0.005) correlation with high risk (OR = 2.856) of developing binge eating disorder (BED) in PCOS patients was found when compared to non-PCOS participants. Additionally, significantly (P = 0.045) higher number of participants with BED was found to have increased BMI and hence the estimated risk for developing obesity in individuals with BED was high (OR = 1.733) compared to non-BED individuals. However, no significant relationship was observed between occurrence of BED and age, educational level, employment and social status. Further, Fig. 1 shows the distribution of Binge eating score across the study participants. There is an approximate symmetrical distribution of curve where large number of the study samples scored average score with almost similar number of participants scoring on either side of the peak.
Fig. 1.
Distribution of study participants with Eating disorder score.
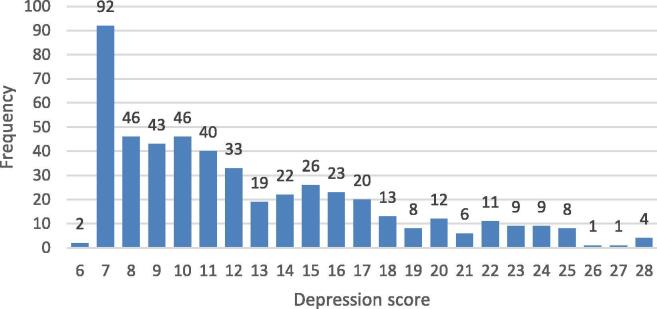
3.3. Depression and demographic features
Table 2 shows significant difference in occurrence of depression with respect to their educational status. Large proportion of less educated participants score high in depression scale compared to the cohort of highly educated ones (P = 0.007, OR = 1.634). Also, risk (OR = 2.497) of depression in PCOS individuals were significantly (P = 0.000) higher when compared to the non-PCOS persons. Although no significant difference was found on the basis of age, employment, social status and BMI for the prevalence of depression, there is a non-significant high risk noted. Overall, number of samples of this study scored (Fig. 2) almost equally on either side of cutoff score of 10 (45.7% Vs 54.3%).
Table 2.
Sociodemographic features and depression.
| Characteristics | Depression Frequency (percentage) |
P value | Odds ratio | 95% Confidence interval |
|||
|---|---|---|---|---|---|---|---|
| Not present | Present | Total | Lower | Upper | |||
| Age | 0.484 | 1.142 | 0.787 | 1.657 | |||
|
97 (56.4.1) | 75 (43.6.9) | 172 (34.81) | ||||
|
171 (53.1) | 151 (46.9) | 322 (65.18) | ||||
| Total | 268 (54.3) | 226 (45.7) | 494 (100) | ||||
| Education | 0.007 | 1.634 | 1.142 | 2.338 | |||
|
164 (59.6) | 111 (40.4) | 275 (55.66) | ||||
|
104 (47.5) | 115 (52.5) | 219 (44.33) | ||||
| Total | 268 (54.3) | 226 (45.7) | 494 (100) | ||||
| Employment status | 0.561 | 1.118 | 0.767 | 1.629 | |||
|
92 (56.1) | 72 (43.9). | 164 (33.19) | ||||
|
176 (53.3) | 154 (46.7) | 330 (66.80) | ||||
| Total | 268 (54.3) | 226 (45.7) | 494 (100) | ||||
| Social status | 0.499 | Risk estimate statistics is not computed as it is not 2 × 2 table | |||||
|
6 (50) | 6 (50) | 12 (2.43) | ||||
|
28 (45.9) | 33 (54.1) | 61 (12.34) | ||||
|
152 (54.7) | 126 (45.3) | 278 (56.27) | ||||
|
82 (57.3) | 61 (42.7) | 143 (28.94) | ||||
| Total | 268 (54.3) | 226 (45.7) | 494 (100) | ||||
| PCOS status | 0.000 | 2.497 | 1.625 | 3.834 | |||
|
225 (59.5) | 153 (40.5) | 378 (76.51) | ||||
|
43 (37.1) | 73 (62.9) | 116 (23.48) | ||||
| Total | 268 (54.3) | 226 (45.7) | 494 (100) | ||||
| BMI | 0.558 | 1.115 | 0.775 | 1.602 | |||
|
167 (55.3) | 135 (44.7) | 302 (61.13) | ||||
|
101 (52.6) | 91 (47.4) | 192 (38.86) | ||||
| Total | 268 (54.3) | 226 (45.7) | 494 (100) | ||||
Fig. 2.
Distribution of study participants with depression score.
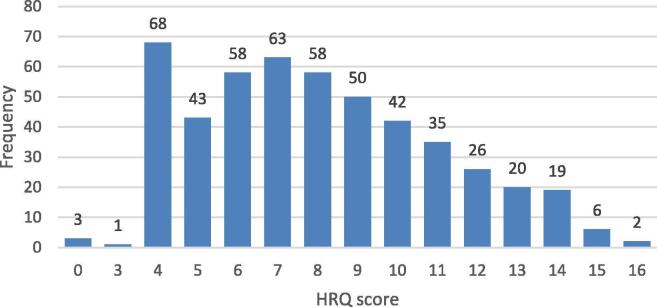
3.4. Abnormal health related quality of life (HRQ) and demographic factors
Table 3 illustrates the significant (P = 0.000) relationship between abnormal HRQ with the presence of PCOS (OR = 3.472). There was no significant influence of age, educational level, employment status, social status and BMI was seen on the development of abnormal HRQ scores, however, all these factors possess estimated risk. Overall, Fig. 3 shows high percentage of the participants of this study have abnormal HRQ score, 65.2% against 34.8%.
Table 3.
Sociodemographic features and Abnormal Health related quality of life (HRQ).
| Characteristics | Abnormal HRQ-Frequency (percentage) |
P value | Odds ratio | 95% Confidence interval |
|||
|---|---|---|---|---|---|---|---|
| Not present | Present | Total | Lower | Upper | |||
| Age | 0.311 | 1.221 | 0.830 | 1.795 | |||
|
65 (37.8) | 107 (62.2) | 172 (34.81) | ||||
|
107 (33.2) | 215 (66.9) | 322 (65.18) | ||||
| Total | 172 (34.8) | 322 (65.2) | 494 (100) | ||||
| Education | 0.537 | 1.634 | 1.142 | 2.338 | |||
|
99 (36) | 176 (64) | 275 (55.66) | ||||
|
73 (33.3) | 146 (66.7) | 219 (44.33) | ||||
| Total | 172 (34.8) | 322 (65.2) | 494 (100) | ||||
| Employment status | 0.673 | 0.919 | 0.619 | 1.363 | |||
|
55 (33.5) | 109 (66.5). | 164 (33.19) | ||||
|
117 (35.5) | 213 (64.5) | 330 (66.80) | ||||
| Total | 172 (34.8) | 322 (65.2) | 494 (100) | ||||
| Social status | 0.318 | Risk estimate statistics is not computed as it is not 2 × 2 table | |||||
|
2 (16.7) | 10 (83.3) | 12 (2.43) | ||||
|
17 (27.9) | 44 (72.1) | 61 (12.34) | ||||
|
100 (36) | 178 (64) | 278 (56.27) | ||||
|
53 (37.1) | 90 (62.9) | 143 (28.94) | ||||
| Total | 172 (34.8) | 322 (65.2) | 494 (100) | ||||
| PCOS status | 0.000 | 3.472 | 2.038 | 5.915 | |||
|
153 (40.5) | 225 (59.5) | 378 (76.51) | ||||
|
19 (16.4) | 97 (83.6) | 116 (23.48) | ||||
| Total | 172 (34.8) | 322 (65.2) | 494 (100) | ||||
| BMI | 0.869 | 1.032 | 0.706 | 1.510 | |||
|
106 (35.1) | 196 (64.9) | 302 (61.13) | ||||
|
66 (34.4) | 126 (65.6) | 192 (38.86) | ||||
| Total | 172 (34.8) | 322 (65.2) | 494 (100) | ||||
Fig. 3.
Distribution of study participants with Abnormal HRQ score.
3.5. Impact of PCOS on BED, depression and HRQ using binary regression analysis
Table 4 explains the binary logistic regression analysis of PCOS on BED, depression and HRQ. The odds of developing abnormal health related quality of (HRQ) in patients with PCOS was significantly (P = 0.000, OR = 3.472) high when compared to non-PCOS participants. The odds of showing high BED (P = 0.007, OR = 2.856) and depression (P = 0.000, OR = 2.497) scores in PCOS participants were significantly more than patients who were not having PCOS. Out of the three parameters studied, abnormal health related quality of life possessed a higher influence of PCOS compared to depression and abnormal eating behavior.
Table 4.
Impact of PCOS on BED, depression and abnormal HRQ using Binary regression analysis.
| Variable | Odds ratio | 95% Confidence Interval |
P Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Binge Eating disorder: | ||||
|
2.856 | 1.328 | 6.141 | 0.007 |
| Depression status: | ||||
|
2.497 | 1.625 | 3.834 | 0.000 |
| Abnormal HRQ | ||||
|
3.472 | 2.038 | 5.915 | 0.000 |
4. Discussion
This study was done to elucidate the impact of polycystic ovary sysndrome (PCOS) on eating behavior, depression and health related quality of life. Around 23% of the participants recruited in several study centers by convinient sampling were found to have PCOS.
In keeping with the existing literature (Jeanes et al., 2017), women with PCOS have shown higher proportion of BED than the controls. Disorganized dietary habits has been reported as contributory factor for increasing body weight, hence a significant correlation was found between BED and PCOS by linear regression analysis, wherein binge eating disorder increases the body weight and increase in body weight further aggravate disorganized eating tendencies. An increase in body weight is one of the secondary feature of PCOS (Emeksiz and Bideci, 2018) and thus increase in BMI is the predictor of established PCOS.
Without binding to BED, any eating disorders in PCOS population may pose a significant problem as it may lead to excess body weight which may have profound effect to cause increase insulin resistance, hyperandrogonism and ovulatory dysfunction. Therefore counseling of PCOS individuals is necessary to cut down the extra weight by avoiding BED. However, it has to be delicately manage as subjects with BED have less weight loss (Sherwood et al., 1999), more rapid weight regain (Yanovski et al., 1994), and more attrition from weight loss treatments (Sherwood et al., 1999) than those without BED, and this is especially true in those who have depression as a concurrent psychological illness. Therefore reducing body weight is not easy in woman who have both depression and BED during PCOS.
With diagnosis of any disorder, disease, or syndrome it is reasonable to say that a patient may have abnormal psychological status (Damone et al., 2019). The causes of this added abnormality in life is most attributable to hirsutism, irregular menses, and infertility. There is a direct relationship reported between PCOS and development of depression (Sadeeqa et al., 2018). The fluctuation in mood may be due to PCOS mediated hyperandrogonism that may alter monoamine balance and probably leads to depression in PCOS cases (Kocelak et al., 2012). Our findings are similar to earlier reports of increased risk of depression in PCOS women (Hollinrake et al., 2007). A systemic review of 14 studies (Araujo et al., 2010) supports our results.
Infertility is one of the common features of PCOS and that is associated with low social status and high divorce rate (Paulson et al., 1988). However, the participants of this study reported a very high divorce rate that is indistinguishable whether their separation is due to PCOS or non-PCOS issues. An increase in divorce rate together with high proportion of employed participants in PCOS patients is another reason to advocate and initiate self-sufficient skills in the young females of Riyadh.
Besides that, we found that PCOS has a significant negative impact on health related quality of life (HRQ). A study showed negative impact of PCOS on HRQ including psychological, physical and sexual domains (Upadhya and Trent, 2007). Our findings are also in line with other reports that explained the inverse correlation of depression and BED on health related quality of life (Aliasghari et al., 2017). High scores for abnormal eating is also associated with fall in quality of life scores as well as worsening the psychological illness. Therefore it is imperative to take necessary steps to neutralize the eating behavior together with controlling all comorbid features to improve the quality of life of PCOS patients.
Although our research accomplished its aims, the study has also number of limitations. First, the result was based on self-reported questionnaire. Therefore, there is potential for reporting bias, or misunderstanding of the questions. Second, our questionnaire includes statements about feeling and ability of doing some works by participants during the last 2 weeks, consequently relies on the ability to recall, which is not consistent across all individuals. The incidence of depression is generally higher during young reproductive age, it is not clear whether the depression found in PCOS was solely due to PCOS or other concurrent factors, more comprehensive data sheet would have answered this. Finally, there is a possibility of other contributory factors for the development of abnormal eating habits, induction of depression and impairment in quality of life than only PCOS.
5. Conclusion
In conclusion, the present study shows that women with PCOS are at a significant risk for depressive disorders, disorganized eating behavior and impaired quality of life. Therefore, additional care and services have to be developed to minimize the impact of PCOS on already burdened individuals.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors are indebted to the support provided by the physicians and nursing staff of OBGYN Clinic at study centers of Riyadh, Saudi Arabia. The authors would like to thank the AlMaarefa University for financial support given for publication of this research.
Footnotes
Peer review under responsibility of King Saud University.
References
- Aliasghari F., Mirghafourvand M., Charandabi S.M., Lak T.B. The predictors of quality of life in women with polycystic ovarian syndrome. Int. J. Nurs. Pract. 2017;23(3):e12526. doi: 10.1111/ijn.12526. [DOI] [PubMed] [Google Scholar]
- Amiri M., Bidhendi Yarandi R., Nahidi F., Tohidi M., Ramezani Tehrani F. The relationship between clinical and biochemical characteristics and quality of life in patients with polycystic ovary syndrome. Clin. Endocrinol. (Oxf.) 2019;90(1):129–137. doi: 10.1111/cen.13858. Epub 2018 Oct 17. [DOI] [PubMed] [Google Scholar]
- Araujo D.M., Santos G.F., Nardi A.E. Binge eating disorder and depression: a systematic review. World J. Biol. Psychiatry. 2010;11(2–2):199–207. doi: 10.3109/15622970802563171. [DOI] [PubMed] [Google Scholar]
- Asdaq S.M., Yasmin F. Risk of psychological burden in polycystic ovary syndrome: A case control study in Riyadh, Saudi Arabia. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.05.086. [DOI] [PubMed] [Google Scholar]
- Barry J.A., Kuczmierczyk A.R., Hardiman P.J. Anxiety and depression in polycystic ovary syndrome: a systematic review and meta-analysis. Hum. Reprod. 2011;26:2442–2451. doi: 10.1093/humrep/der197. [DOI] [PubMed] [Google Scholar]
- Bozdag G., Mumusoglu S., Zengin D., Karabulut E., Yildiz B.O. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum. Reprod. 2016;31(12):2841–2855. doi: 10.1093/humrep/dew218. [DOI] [PubMed] [Google Scholar]
- Cossrow N., Pawaskar M., Witt E.A., Ming E.E., Victor T.W., Herman B.K. Estimating the prevalence of binge eating disorder in a community sample from the United States: comparing DSM-IV-TR and DSM-V criteria. J. Clin. Psychiatry. 2016;77:e968–e974. doi: 10.4088/JCP.15m10059. [DOI] [PubMed] [Google Scholar]
- Cronin L., Guyatt G., Griffith L., Wong E., Azziz R., Futterweit W., Cook D., Dunaif A. Development of a health-related quality-of-life questionnaire (PCOSQ) for women with polycystic ovary syndrome (PCOS) J. Clin. Endocrinol. Metabol. 1998;83(6):1976–1987. doi: 10.1210/jcem.83.6.4990. [DOI] [PubMed] [Google Scholar]
- Damone A.L., Joham A.E., Loxton D., Earnest A., Teede H.J., Moran L.J. Depression, anxiety and perceived stress in women with and without PCOS: a community-based study. Psychol. Med. 2019;49(9):1510–1520. doi: 10.1017/S0033291718002076. [DOI] [PubMed] [Google Scholar]
- Daniilidis A., Dinas K. Long term health consequences of polycystic ovarian syndrome: a review analysis. Hippokratia. 2009;13(2):90. [PMC free article] [PubMed] [Google Scholar]
- Dokras A., Clifton S., Futterweit W., Wild R. Increased risk for abnormal depression scores in women with polycystic ovary syndrome: a systematic review and meta-analysis. Obstet. Gynecol. 2011;117(1):145–152. doi: 10.1097/AOG.0b013e318202b0a4. [DOI] [PubMed] [Google Scholar]
- Dokras A. Cardiovascular disease risk in women with PCOS. Steroids. 2013;78:773–777. doi: 10.1016/j.steroids.2013.04.009. [DOI] [PubMed] [Google Scholar]
- Elghblawi E. Polycystic ovary syndrome and female reproduction. Br. J. Nurs. 2007;16(18):1118–1121. doi: 10.12968/bjon.2007.16.18.27504. [DOI] [PubMed] [Google Scholar]
- Emeksiz H.C., Bideci A., Nalbantoğlu B., Nalbantoğlu A., Celik C., Yulaf Y., Çamurdan M.O., Cinaz P. Anxiety and depression states of adolescents with polycystic ovary syndrome. Turk. J. Med. Sci. 2018;48(3):531–536. doi: 10.3906/sag-1708-131. [DOI] [PubMed] [Google Scholar]
- Fairburn C.G., Beglin S.J. Assessment of eating disorders: interview or self-report questionnaire? Int. J. Eat. Disord. 1994;16:363–370. [PubMed] [Google Scholar]
- Gomez F. Central and Eastern Sydney Primary Health Networks; 2016. A Guide to the Depression, Anxiety and Stress Scale (DASS 21) [Google Scholar]
- Hollinrake E., Abreu A., Maifeld M., Van Voorhis B.J., Dokras A. Increased risk of depressive disorders in women with polycystic ovary syndrome. Fertil Steril. 2007;87:1369–1376. doi: 10.1016/j.fertnstert.2006.11.039. [PubMed: 17397839] [DOI] [PubMed] [Google Scholar]
- Hudson J.I., Hiripi E., Pope H.G., Jr, Kessler R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry. 2007;1:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeanes Y.M., Reeves S., Gibson E.L., Piggott C., May V.A., Hart K.H. Binge eating behaviours and food cravings in women with polycystic ovary syndrome. Appetite. 2017;1(109):24–32. doi: 10.1016/j.appet.2016.11.010. [DOI] [PubMed] [Google Scholar]
- Kocelak P., Chudek J., Naworska B. Psychological disturbance and quality of life in obese and infertile women and men. Int. J. Endocrinol. 2012;2014:14. doi: 10.1155/2012/236217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. second ed. Psychological Foundation; Sydney: 1995. Manual for the Depression Anxiety Stress Scales. [Google Scholar]
- Palermo T.M., Long A.C., Lewandowski A.S., Drotar D., Quittner A.L., Walker L.S. Evidence-based assessment of health-related quality of life and functional impairment in pediatric psychology. J. Pediatr. Psychol. 2008;33:983–996. doi: 10.1093/jpepsy/jsn038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulson J.D., Haarmann B.S., Salerno R.L., Asmar P. An investigation of the relationship between emotional maladjustment and infertility. Fertil. Steril. 1988;49(2):258–262. doi: 10.1016/s0015-0282(16)59712-x. [DOI] [PubMed] [Google Scholar]
- Sadeeqa S., Mustafa T., Latif S. Polycystic ovarian syndrome–related depression in adolescent girls: a review. J. Pharm. Bioallied Sci. 2018;10(2):55. doi: 10.4103/JPBS.JPBS_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood N.E., Jeffery R.W., Wing R.R. Binge status as a predictor of weight loss treatment outcome. Int. J. Obes. Relat. Metab. Disord. 1999;23:485–493. doi: 10.1038/sj.ijo.0800846. [DOI] [PubMed] [Google Scholar]
- Teede H.J., Misso M.L., Costello M.F., Dokras A., Laven J., Moran L., Piltonen T., Norman R.J. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum. Reprod. 2018;33(9):1602–1618. doi: 10.1093/humrep/dey256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upadhya K., Trent M. Effects of polycystic ovary syndrome on health-related quality of life. Expert Rev. Pharmacoecon. Outcomes Res. 2007;7(6):597–603. doi: 10.1586/14737167.7.6.597. [DOI] [PubMed] [Google Scholar]
- Yanovski S.Z., Gormally J.F., Leser M.S., Gwirtsman H.E., Yanovski J.A. Binge eating disorder affects outcome of comprehensive very-low-calorie diet treatment. Obes. Res. 1994;2:205–212. doi: 10.1002/j.1550-8528.1994.tb00049.x. [DOI] [PubMed] [Google Scholar]