Abstract
Variations in pulmonary venous anatomy (in the absence of any anomalous pulmonary venous connections) is not uncommon. Commonly occurring variations include presence of conjoined pulmonary veins (PV), supernumerary PVs and ostial PVs. Variant PV anatomy is often asymptomatic; however, it may assume importance in the pre-procedural planning prior to cardiothoracic surgeries and radiofrequency catheter-directed ablation for PV isolation. It is therefore important that the radiologist is aware of the conventional normal and variant PV anatomy in addition to obvious abnormalities like anomalous PV drainage or PV stenosis/ occlusion. Multidetector CT (MDCT) is often used as the first-line imaging modality for pre-procedural PV mapping as it provides high quality images with short acquisition times and availability of numerous post-processing tools.This pictorial review focusses on the MDCT-based PV imaging describing the reporting nomenclature, the conventional normal as well as non-anomalous variant PV anatomy along with their clinical significance.
Introduction
Pulmonary venous anatomy (in the absence of any anomalous pulmonary venous connections) is frequently variable with commonly observed variants including conjoined ostia of pulmonary veins (PV) or presence of supernumerary PVs and their numerous possible permutations and combinations. Variant anatomy of PVs, though often clinically silent, may assume importance in the pre-procedural planning in various thoracic and cardiac surgeries, including lung transplantation and oncological surgeries, as well as prior to radiofrequency catheter-directed ablation for isolating PVs in the management of arrhythmias. It is thus imperative to not only look for obvious abnormalities like anomalous PV drainage or PV stenosis/occlusion, but also be aware of the conventional normal anatomy as well as the non-anomalous variations in PV anatomy. It is therefore important for cardiac radiologists involved in the diagnosis of such patients to incorporate PV evaluation as part of their “routine search pattern” while evaluating cross-sectional imaging as these might be easily overlooked.1
The current pictorial review focusses on the multidetector CT (MDCT)-based imaging of the PVs including a brief description of the reporting nomenclature pertinent to PV imaging, the normal PV anatomy (conventional as well as non-anomalous variants) and their clinical implications, if any.
Pulmonary vein imaging
MDCT is frequently used a primary modality for the evaluation of PV anatomy, when required, and also often used as an educational tool for teaching normal and variant PV anatomy to trainees in the fields of anatomy, cardiology and cardiothoracic surgery, as it allows reconstruction of images in multiple planes along with availability of multiple post-processing features like volume rendering and generating surface shaded displays and endoluminal views. High quality images devoid of artIfacts are obtained with the use of MDCT owing to its high spatial and temporal resolution and short acquisition times. While MRI is being used at multiple centers for PV evaluation as it is ionizing radiation-free and can avoid use of iodinated contrast media, its limited availability, long scan times and frequent need for sedation precludes its widespread utilization for the same. Presence of cardiac implantable electronic devices, especially in patients with arrhythmias, is another contraindication for the use of MRI. Role of transesophageal echocardiography and conventional venography is often limited to intraprocedural delineation of PV anatomy.2
MDCT protocol
All the scans were performed on a third-generation dual source CT scanner (Somatom Force; Siemens Healthcare, Forchheim, Germany). The CT imaging protocol for dedicated imaging of pulmonary veinsand the post-processing tools employed are outlined in Table 1. It is prudent to mention that the variations, when detected incidentally, can be fairly evaluated on non-ECG gated scans as well.
Table 1.
Multidetector CT imaging protocol and post-processing tools
| Parameter | Description |
|---|---|
| Image acquisition | |
| Cardiac gating | Retrospective ECG-gated scan |
| Contrast medium and dose | IV non-ionic iodinated contrast; 1.0 mL/kg body weight |
| Contrast injection and flow rate | Biphasic injection using dual head power injector via peripheral IV line; Contrast medium is injected at 4.0 ml s−1 followed by 50 ml saline chaser injected at 4.0 ml s−1 |
| Acquisition triggering | Bolus tracking method ROI placed in ascending aorta Contrast opacification threshold: 100 HU Automated triggering of CT acquisition when threshold reached in ROI on monitoring sequence |
| Scan range | From aortic arch cranially to the level of diaphragm caudally |
| Tube voltage and tube current | Automated tube voltage selection and automated tube current modulation enabled Based on body habitus of the patient |
| Image reconstruction | Slice reconstruction: 0.6 mm slice thickness at an increment of 0.4 mm Medium sharp kernel (Bv40) Model-based iterative reconstruction (strength: level 3) |
| Post-processing tools | |
| MPR | Sagittal and coronal reconstruction Double oblique reconstruction for measuring ostial diameters Curved MPR Vessel analysis using centerline: Reconstructed images along the cross-section and length of PV being evaluated |
| Epicardial VR | Including the LA and distal one-thirds of PVs Dorso-cranial view with RPO and LPO projection; Posterior projection Suited for: Evaluation of LA morphology Number of PVs including accessory veins Angulation of PV with respect to LA surface Location of ostial veins |
| Endocardial/ endoluminal VR | One view each for either side-including the ipsilateral ostia and the intervenous saddle Suited for: Evaluation of PV ostia and their orientation Geometry of ostial veins including distance from PV ostium Evaluation of common ostium in case of conjoined PVs |
HU: Hounsfield units; IV: intravenous; LA: left atrium; LPO: left posterior oblique; MPR: multiplanar reconstruction; PV: pulmonary vein; ROI: region of interest; RPO: right posterior oblique; VR: volume rendering
Relevant nomenclature
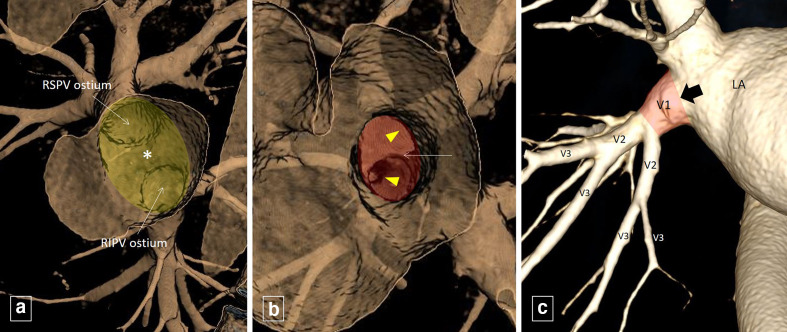
Radiologists should be aware of the accepted nomenclature of various parts of the distal PVs and adjacent left atrium (LA) to ensure standardized reporting and communication of the findings to their clinical counterparts (Figure 1).
Figure 1.
Endoluminal view (A) showing the RSPV and RIPV ostium with the interposed left atrial wall between the two ipsilateral ostia (intervenous saddle, indicated by *) forming the ‘right pulmonary venous inflow vestibule’ (shaded in yellow). Endoluminal view (B) of the RSPV ostium (shaded in red) show the venous wall (intravenous saddle, indicated by thin white arrow) interposed between the branches (arrowheads) of RSPV. Volume rendered image (C) shows the distal RIPV being divided into segments (labelled V1, V2 and so on in a sequential fashion) between its branch points, starting from the its ostium (thick black arrow) moving away from left atrium (LA). The V1 segment (shaded in red) is referred to as the pulmonary venous trunk. RIPV, right inferior pulmonary vein; RSPV, right superior pulmonary vein.
PV ostium
It represents the junction of the distal PV and the LA. Histologically, it may be identified as the point where the parietal pericardium reflects of the epicardial surface of the LA.2,3
PV trunk:
The distal (or central) PV comprises the part of the PV close to the LA. This distal PV is further divided into segments between its branch points, starting from the PV ostium moving away from the LA, and labelled V1, V2 and so on in a sequential fashion. The V1 segment which is the segment of distal PV between the PV ostium and its first branching point is called the PV trunk. The first branching point also anatomically marks the “last confluence” of PV branches.2,3
Intra- and intervenous saddle
While the venous wall between branches of a single PV is referred to as the “intravenous saddle”, the LA wall interposed between separate ipsilateral PVs is labelled the “inter venous saddle”.2,3
PV inflow vestibule:
The ipsilateral PV ostia along with the interposed LA wall, i.e. inter venous saddle constitutes the PV inflow vestibule.2
Posterior LA
The bilateral PV inflow vestibules along with the intervening posterior LA wall forms the posterior LA.3
Normal PV anatomy
“Normal” PV anatomy is frequently variable with multiple permutations and combinations of the number of PV ostia and their arrangements observed.1 While each of these configurations are non-anomalous and hence essentially normal (entire pulmonary venous return draining in the LA), for the purposes of this review, we would classify them on the basis of their commonality, with the commonest observed pattern labelled as “conventional normal PV anatomy” and the others comprising “variant PV anatomy”.
Conventional normal PV anatomy
The commonest configuration observed comprises of four separate PV ostia in the ”posterior LA”. The two ostia on right side are commonly separated by the intervening LA wall and drain the right superior pulmonary vein (RSPV) and right inferior pulmonary vein (RIPV) respectively, while the two ostia on the left, usually with no intervening LA wall, drain the left superior pulmonary vein (LSPV) and left inferior pulmonary vein (LIPV) respectively.1,2,4,5 Table 2 summarizes the “normal” anatomy of the four veins outlining their course, relations to adjacent structures, tributaries, the segments of lung drained and the site of opening into LA.1,2,6,7
Table 2.
“Conventional” normal anatomy of pulmonary veins
| Pulmonary Vein | Part of lung drained | Draining tributaries | Orientation and course | Relation with adjacent structures | Site of opening in LA |
|---|---|---|---|---|---|
| RSPV | RUL and RML | Apical, anterior and posterior segmental veins of RUL join to form RSPV. Lateral and medial segmental veins of the RML join to form RMV which drains into the RSPV. |
Projects anteriorly and cephalad with respect to LA Has an oblique course caudally as it passes medially; more vertical compared to LSPV |
Courses posterior to SVC and anterior to RPA Further caudally, dives under the RPA and crosses posterior and inferior to the SVC-RA junction |
Most superior and right lateral aspect of LA |
| RIPV | RLL | Medial basal, anterior basal, lateral basal and posterior basal segmental veins of RLL join to form a common basal vein which unites with the superior segmental vein of the RLL to form the RIPV | Projects posteriorly and caudad with respect to LA Has a horizontal course centrally and vertical course peripherally |
Courses below the RSPV, albeit in a considerably posterior plane | Most inferior and right lateral aspect of LA |
| LSPV | LUL including lingula | Anterior and apico-posterior segmental veins of LUL join to form LSPV. Superior and inferior segmental veins of the lingula of LUL join to form lingular vein which drains into the LSPV. |
Projects anteriorly and cephalad with respect to LA Has an oblique course caudally as it passes medially; more horizontal compared to RSPV |
Courses superior and then anterior to LMB, anterior to LPA and inferior to MPA | Near LAA |
| LIPV | LLL | Antero medial basal, lateral basal and posterior basal segmental veins of LLL join to form a common basal vein which unites with the superior segmental vein of the LLL to form the LIPV | Projects posteriorly and caudad with respect to LA Has a horizontal course centrally and vertical course peripherally |
Courses anterior to the DTA and medial to LLL bronchus | Most inferior and left lateral aspect of LA, directly anterior to DTA |
DTA: descending thoracic aorta; LA: left atrium; LAA: left atrial appendage; LIPV: left inferior pulmonary vein; LLL: left lower lobe; LMB: left main bronchus; LPA: left pulmonary artery; LSPV: left superior pulmonary vein; LUL: left upper lobe; MPA: main pulmonary artery; RA: right atrium; RIPV: right inferior pulmonary vein; RML: right middle lobe; RMV: right middle vein; RPA: right pulmonary artery; RSPV: right superior pulmonary vein; RUL: right upper lobe; SVC: superior vena cava.
References: 1, 2, 6, 7
Variations in pulmonary venous drainage
Variations in PV drainage mainly relate to the presence of common or conjoined ostium of the PVs on either side, presence of separate direct drainage of a PV branch resulting in supernumerary ostia, or presence of early branching of the PVs. Table 3 summarizes the common variations observed.2,4
Table 3.
Commonly observed variations in pulmonary venous anatomy
| Sr. No. | Variations in pulmonary venous anatomy |
|---|---|
| 1 | Conjoined vein |
| RSPV and RIPV along with RMLV draining via single ostium | |
| LSPV and LIPV draining via single ostium | |
| Bilateral | |
| 2 | Supernumerary or accessory veins |
| Separate drainage of RML or superior segment of RLL | |
| Separate drainage of medial and lateral segment of the RML | |
| Separate drainage of all or part of lingula or superior segment of LLL | |
| Separate drainage of posterior segment of RUL | |
| Separate drainage of apico-posterior segment of LUL | |
| 3 | Early branching of pulmonary vein |
LIPV: left inferior pulmonary vein; LLL: left lower lobe; LSPV: left superior pulmonary vein; LUL: left upper lobe; RIPV: right inferior pulmonary vein; RLL: right lower lobe; RML: right middle lobe; RSPV: right superior pulmonary vein; RUL: right upper lobe.
References: 2, 4
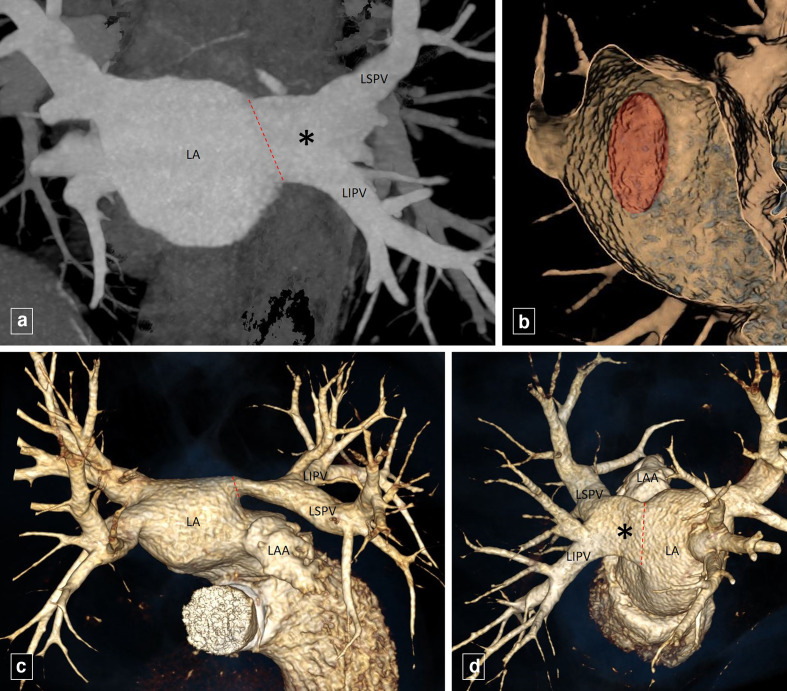
Conjoined pulmonary vein
A conjoined vein is observed when, instead of entering the LA through separate ostia, the superior and inferior PVs join each other forming a common channel before reaching the LA, resulting in a single pulmonary veno-atrial junction(Figures 2 and 3).8 It may be observed in 2.4–25% of population, more commonly seen on the left side than on the right side.2,4,6,9 Whenever present, a conjoined PV trunk has a significantly shorter length and a significantly larger diameter compared to the other PVs with a broad atriopulmonary venous junction.3,8
Figure 2.
Coronal maximum intensity projection image (A) shows the LSPV and IPV joining each other forming a common channel (*) before reaching the LA, resulting in a single pulmonary veno-atrial junction (dotted red line). Endoluminal view (B) shows the single ellipticalleft pulmonary venous ostium (shaded in red). Volume rendered images (C, D) depict the conjoined vein (*) draining the LSPV and LIPV into the LA. LAA, left atrial appendage; LIPV, left inferior pulmonary vein; LSPV, left superior pulmonary vein.
Figure 3.
Coronal maximum intensity projection image (A) and volume rendered image (B) shows theRSPV and RIPV joining each other forming a conjoined PV trunk (*, in B) having a significantly shorter length and a significantly larger diameter before reaching the LA. The red dashed line in A) represents the extrapolation of the shape of LA adjacent to the pulmonary venous ostia to define the expected atriopulmonary venous junction. Endoluminal view (C) shows the single broad right pulmonary venous ostium (shaded in yellow). LA, left atrium; RIPV, right inferior pulmonary vein; RSPV, right superior pulmonary vein.
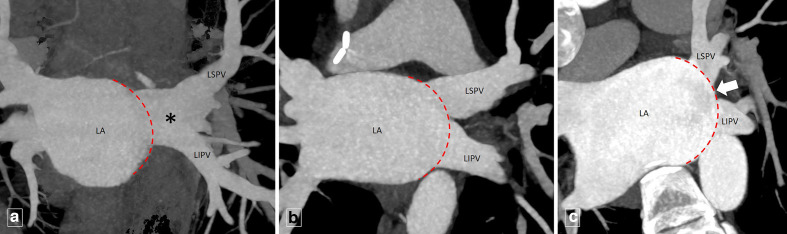
While it is easy to ascertain the presence or absence of a common ostium on the right side, a false positive diagnosis of the same on the left side is a distinct possibility as even “normally,” there is no intervening LA wall between the two adjacent ostia leading to potential confusion. An extrapolation of the shape of LA adjacent to the PV ostia to define the expected atriopulmonary venous junction should precede the diagnosis and PVs reaching up to the hypothetical atriopulmonary junction be treated as having “separate” ostia, while PVs joining before it be considered to have a “conjoined” ostium(Figures 3 and 4).1
Figure 4.
Coronal maximum intensity projection image (A, B, C) of different patients demonstrate the extrapolation of the LA shape adjacent to the left-sided pulmonary venous ostia to define the expected atriopulmonary venous junction (dashed red lines). (A) shows the (LSPV and LIPV joining each other (before reaching the dashed red lines) forming a conjoined vein (*). (B) shows separate LSPV and LIPV ostium with no intervening LA wall while (C) shows separate LSPV and LIPV ostium with intervening LA wall (thick white arrow). LA, left atrial; LIPV, left inferior pulmonary vein; LSPV, left superior pulmonary vein.
Supernumerary or accessory pulmonary veins
An accessory vein draining into the LA separate from the ipsilateral superior and inferior PV results in supernumerary ostia (Figures 5 and 6). Accessory PVs are usually named according to the pulmonary segment drained by them and are much more common on the right as compared to the left.2,4,8 Their reported incidences varies widely and can occur in up to approximately one-fourth of the population.8 When present, the accessory PV trunk is generally shorter in length and smaller in diameter compared to the other PVs and the vein may occasionally traverse across pulmonary fissures.2,8,10 Table 4 describes the morphological features of the commonly observed accessory veins.1,2,6,8,11 More than one accessory veins can co-exist resulting in multiple possible combinations and even up to seven separate PV ostia.2
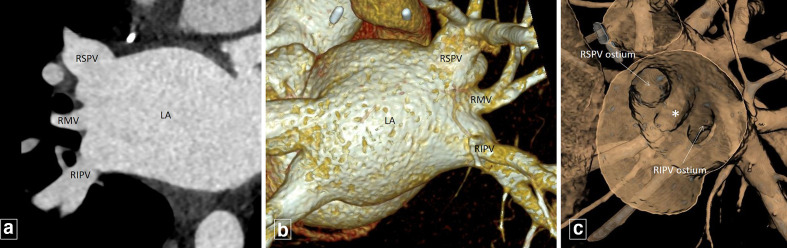
Figure 5.
Coronal oblique maximum intensity projection image(A) and volume rendered image (B) shows the right middle vein (RMV) draining directly into the LA, separate from the RSPV and RIPV. (B,) shows the veins draining the medial and lateral segment of right middle lobe joining to form the RMV. Endoluminal view (C) shows the supernumerary ostium (*) of RMV between the RSPV and RIPV ostium. LA, left atrium; RIPV, right inferior pulmonary vein; RSPV, right superior pulmonary vein.
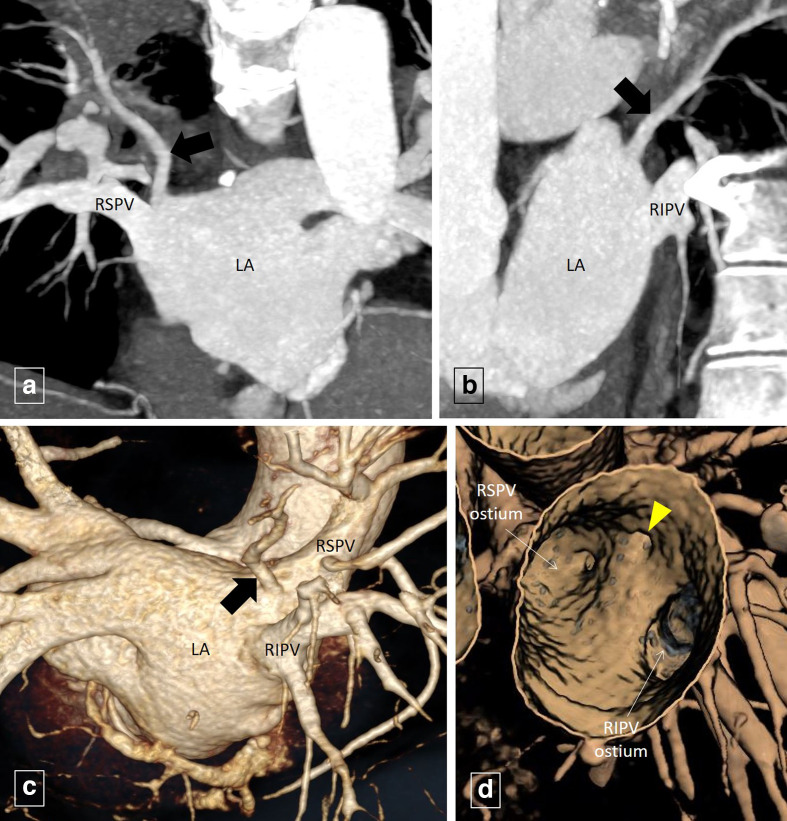
Figure 6.
Coronal oblique (A) and sagittal oblique (B) maximum intensity projection imagesand volume rendered image (C) shows the right “top” vein (thick black arrow) draining directly into the LA, separate from the RSPV and RIPV. Endoluminal view (D) shows the supernumerary ostium (arrowhead) of the right “top” vein supero-medial to the RSPV ostium. LA, left atrium; RIPV, right inferior pulmonary vein; RSPV, right superior pulmonary vein.
Table 4.
Commonly observed accessory pulmonary veins and their characteristics
| Accessory vein | Incidence | Course | Part of lung drained | Site of entry into LA |
|---|---|---|---|---|
| RMV (Figure 5) | 9 to 26.6% | Projects anteriorly | Commonly drains the RML; medial and lateral segment of RML may drain separately resulting in two RMVs May drain superior segment of RLL |
Between ostia of RSPV and RIPV |
| Right “top” vein (Figure 6) | 0.3 to 9.3% | Tortuous course Traverses posterior and medial to BI |
Posterior segment of RUL or superior segment of RLL | Supero-medial to RSPV ostium |
| Left “top” vein | Uncommon | Tortuous course Traverses posterior and medial to LMB |
Apico-posterior segment of LUL | Supero-medial to LSPV ostium |
| LMV | 0.1 to 0.5% | Projects anteriorly | Commonly drains all or part of lingula May drain superior segment of LLL |
Between ostia of LSPV and LIPV |
BI: bronchus intermedius; LA: left atrium; LIPV: left inferior pulmonary vein; LLL: left lower lobe; LMV: left middle vein; LSPV: left superior pulmonary vein; LUL: left upper lobe; RIPV: right inferior pulmonary vein; RLL: right lower lobe; RML: right middle lobe; RMV: right middle vein; RSPV: right superior pulmonary vein; RUL: right upper lobe.
References: 1, 2, 6, 8, 11
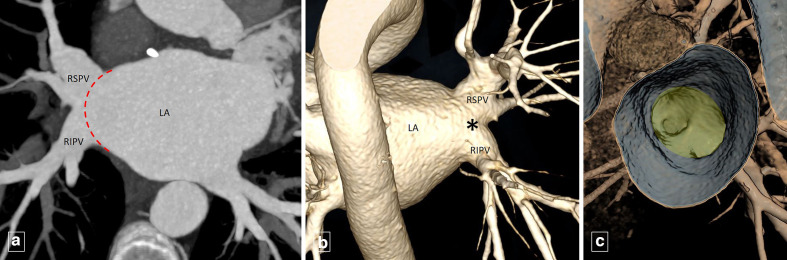
Early branching of pulmonary vein
Early branching denotes presence of a PV branch within 5 mm of the pulmonary veno-atrial junction, thus reducing the V1 segment to less than 5 mm in length. Thus, while this branch does not have its separate ostium, it drains very close to the PV ostium and is, therefore, referred to as an ”ostial vein.”2,3,8 Common examples include early branching of the right middle lobe vein from the RSPV and superior segmental branch of right lower lobe from the RIPV, within 5 mm of their respective ostia (Figures 7 and 8).2
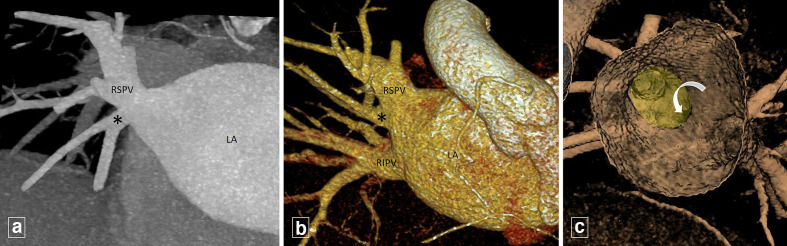
Figure 7.
Coronal oblique maximum intensity projection image (A) and volume rendered image (B) shows early branching of the right middle lobe vein (*) from the RSPV within 5 mm of the RSPV ostium. Endoluminal view (C) shows the right middle lobe vein ostium (curved arrow) within 5 mm of the RSPV ostium (shaded in yellow). LA, left atrium; RIPV, right inferior pulmonary vein.
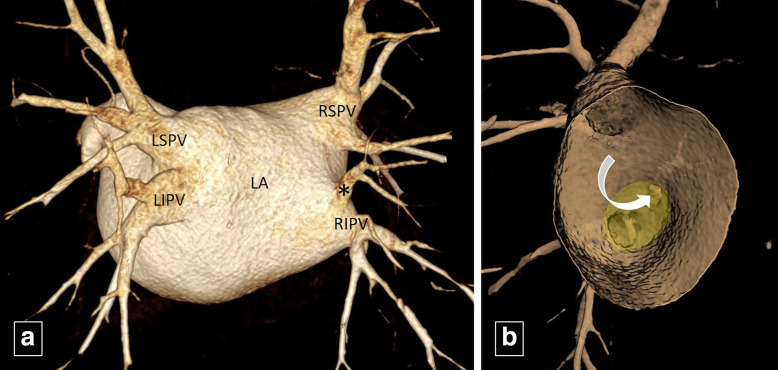
Figure 8.
Volume rendered image (A) shows early branching of the superior segmental branch of right lower lobe (*) from the RIPV within 5 mm of the RIPV ostium. Endoluminal view (B) shows its ostium (curved arrow) within 5 mm of the RIPV ostium (shaded in yellow). RIPV, right inferior pulmonary vein.
Clinical relevance
The myocardial sleeves extending from the LA into the distal segments of PVs, across the PV–LA junction, are believed to be electrically active and having arrhythmogenic potential.2,3 Isolating these arrhythmogenic foci from the LA using radiofrequency catheter-directed ablation is the current focus of treatment.2 The site of treatment has gradually evolved from ablation of the foci in the PVs, to the PV ostia and more recently, to the PV inflow vestibule.2,3 To avoid PV injury and subsequent PV stenosis, ablation is done within 5 mm of all the PV ostia.6 It thus becomes imperative to identify any variations in the number and branching of PVs to ensure all potential foci are ablated as well as delineate the ostial orientation and identify any ostial veins to avoid branch PV stenosis post-ablation.2
Conclusion
Variations in PV anatomy are not uncommon. Although frequently asymptomatic, knowledge of these variations is important in while planning cardiothoracic surgeries and PV isolation. MDCT can provide high quality images, owing to very short acquisition times and availability of multiple post-processing tools, and thus has become a first-line imaging modality for pre-procedural PV mapping.
Contributor Information
Niraj Nirmal Pandey, Email: nirajpandey2403@gmail.com.
Sanjeev Kumar, Email: sanjeevradio@gmail.com.
REFERENCES
- 1.Hassani C, Saremi F. Comprehensive cross-sectional imaging of the pulmonary veins. Radiographics 2017; ; 37: 1928–54Nov-Dec. doi: 10.1148/rg.2017170050 [DOI] [PubMed] [Google Scholar]
- 2.Rajiah P, Kanne JP. Computed tomography of pulmonary venous variants and anomalies. J Cardiovasc Comput Tomogr 2010; ; 4: 155–63May-Jun. doi: 10.1016/j.jcct.2010.01.016 [DOI] [PubMed] [Google Scholar]
- 3.Lacomis JM, Wigginton W, Fuhrman C, Schwartzman D, Armfield DR, Pealer KM. Multi-detector row CT of the left atrium and pulmonary veins before radio-frequency catheter ablation for atrial fibrillation. Radiographics 2003; 23 Spec No : S35–48Oct;23 Spec No:S35-48; discussion. doi: 10.1148/rg.23si035508 [DOI] [PubMed] [Google Scholar]
- 4.Marom EM, Herndon JE, Kim YH, McAdams HP. Variations in pulmonary venous drainage to the left atrium: implications for radiofrequency ablation. Radiology 2004; 230: 824–9. doi: 10.1148/radiol.2303030315 [DOI] [PubMed] [Google Scholar]
- 5.Ho SY. Pulmonary vein ablation in atrial fibrillation: does anatomy matter? J Cardiovasc Electrophysiol 2003; 14: 156–7. doi: 10.1046/j.1540-8167.2003.02551.x [DOI] [PubMed] [Google Scholar]
- 6.Cronin P, Sneider MB, Kazerooni EA, Kelly AM, Scharf C, Oral H, et al. Mdct of the left atrium and pulmonary veins in planning radiofrequency ablation for atrial fibrillation: a how-to guide. AJR Am J Roentgenol 2004; 183: 767–78. doi: 10.2214/ajr.183.3.1830767 [DOI] [PubMed] [Google Scholar]
- 7.Choi SI, Seo JB, Choi SH, Lee SH, KH D, SM K, et al. Variation of the size of pulmo- nary venous ostia during the cardiac cycle: optimal reconstruction window at ECG gated multidetector row CT. EurRadiol 2005; 15: 1441–5. [DOI] [PubMed] [Google Scholar]
- 8.Stojanovska J, Cronin P. Computed tomography imaging of left atrium and pulmonary veins for radiofrequency ablation of atrial fibrillation. Semin Roentgenol 2008; 43: 154–66. doi: 10.1053/j.ro.2008.01.010 [DOI] [PubMed] [Google Scholar]
- 9.Scharf C, Sneider M, Case I, Chugh A, Lai SWK, Pelosi F, et al. Anatomy of the pulmonary veins in patients with atrial fibrillation and effects of segmental ostial ablation analyzed by computed tomography. J Cardiovasc Electrophysiol 2003; 14: 150–5. doi: 10.1046/j.1540-8167.2003.02444.x [DOI] [PubMed] [Google Scholar]
- 10.Cronin P, Kelly AM, Desjardins B, Patel S, Gross BH, Kazerooni EA, et al. Normative analysis of pulmonary vein drainage patterns on multidetector CT with measurements of pulmonary vein ostial diameter and distance to first bifurcation. Acad Radiol 2007; 14: 178–88. doi: 10.1016/j.acra.2006.11.004 [DOI] [PubMed] [Google Scholar]
- 11.Cronin P, Kelly AM. Pulmonary venous abnormalities encountered on pre-radiofrequency ablation mapping multidetector computed tomography. S. Afr. j. radiol. 2017; 21: a1189. doi: 10.4102/sajr.v21i1.1189 [DOI] [Google Scholar]