Abstract
Repetitive transcranial magnetic stimulation, as a relatively new type of rehabilitation treatment, is a painless and non-invasive method for altering brain excitability. Repetitive transcranial magnetic stimulation has been widely used in the neurorehabilitation of stroke patients. Here, we used CiteSpace software to visually analyze 315 studies concerning repetitive transcranial magnetic stimulation for stroke rehabilitation from 1999 to 2019, indexed by Web of Science, to clarify the research hotspots in different periods and characterize the gradual process of discovery in this field. We found that four main points were generally accepted: (1) repetitive transcranial magnetic stimulation has a positive effect on motor function recovery in patients with subcortical stroke; (2) it may be more advantageous for stroke patients to receive low-frequency repetitive transcranial magnetic stimulation in the unaffected hemispheres than to receive high-frequency repetitive transcranial magnetic stimulation in affected hemisphere; (3) low-frequency repetitive transcranial magnetic stimulation has become a potential therapeutic tool for patients with non-fluent aphasia after chronic stroke for neurological rehabilitation and language recovery; and (4) there are some limitations to these classic clinical studies, such as small sample size and low test efficiency. Our assessment indicates that prospective, multi-center, large-sample, randomized controlled clinical trials are still needed to further verify the effectiveness of various repetitive transcranial magnetic stimulation programs for the rehabilitation of stroke patients.
Keywords: data visualization, motor recovery, rehabilitation, repetitive transcranial magnetic stimulation, stroke, stroke rehabilitation, transcranial magnetic stimulation
Chinese Library Classification No. R459.9; R493; R743
Introduction
Magnetic signals can stimulate brain nerves through the skull without attenuation. Thus, transcranial magnetic stimulation (TMS) is considered to be a painless and non-invasive treatment method that has been extensively used in neurorehabilitation treatment of stroke patients (van Lieshout et al., 2019). Further, the emergence of continuously adjustable repetitive TMS (rTMS) has led to new applications in the fields of neurological diseases, rehabilitation, and the treatment of clinical mental illnesses (Hordacre et al., 2019). rTMS mainly uses different frequencies to achieve therapeutic purposes. High frequencies (> 1 Hz) mainly produce excitatory effects, and low frequencies (≤ 1 Hz) mainly produce inhibitory effects (Du et al., 2019; Zhang et al., 2019). rTMS affects local nerves by altering neural function at multiple sites through the connections and interactions between neural networks. To improve brain function in patients with various diseases, optimal therapeutic effects can be achieved by adjusting the stimulation intensity, frequency, site, and coil direction.
The purpose of this paper was to: (1) clarify the role and characteristics of rTMS in stroke rehabilitation, (2) perform a visual analysis of post-stroke rTMS rehabilitation studies using CiteSpace software, and (3) objectively clarify the time-series changes of research hotspots and dynamic frontiers in this field, with the goal of obtaining quantitative and objective data as well as key references.
Data and Methods
Retrieval strategy
The first author retrieved relevant studies addressing rTMS for stroke rehabilitation published from 1999 to 2019.
Data source
Web of Science (WOS) Core Collection Database.
Search terms
The search terms were as follows: (Repetitive Transcranial Magnetic Stimulation OR Transcranial Magnetic Stimulation OR Transcranial Magnetic) AND (Stroke* OR Cerebral Stroke* OR Cerebral Infarct* OR Cerebrovascular Accident) AND (Rehabilitation OR Stroke Rehabilitation).
Retrieval time
From 1999 to 2019.
Qualification
Full-text retrieval was performed.
Inclusion criteria
Studies related to the application of rTMS in stroke rehabilitation were selected after reading the title and abstract. The style of the study was not limited, such that we included any study describing a technical method for treating post-stroke rehabilitation, such as research originals, meta-analyses, reviews, commentaries, and case reports.
Number of studies included
A total of 315 studies were included, published before the deadline of December 30, 2019.
Methods
Software parameter settings
CiteSpace software was developed by Dr. Chaomei Chen, who is a scholar at Drexel University, USA. The software uses Java to conduct visual analyses of scientific references. The software uses co-occurrence and co-citation analyses of a large set of reference data in a given research field to objectively and quantitatively analyze and forecast research frontiers and development trends (Chen, 2004; Chen and Song, 2019).
We used CiteSpace.5.6.R1 software to retrieve studies published from 1999 to 2019 with the ‘Time Slicing’ value set to 1 year. The subject heading was set to ‘Burst Term’.
The type of Node was selected according to the country, keyword, and category for co-occurrence analysis, and the reference and journal for co-citation analysis. CiteSpace software can be used to (1) generate a co-citation analysis map of a cited reference and cited journal; (2) generate a co-occurrence analysis map for a keyword, country, or category; and (3) generate a bibliographic coupling analysis map for a reference and an overlay map of a journal.
Burst detection is a form of topic detection. In CiteSpace, we used the algorithm proposed by Goldberg et al. (2002) to detect innovative topic hotspots.
Interpretation of the application of visualization map identification
Citation tree-rings: In a map drawn using Citespace, there is a circular region termed the citation ‘tree-rings’, which represents the citation history of a paper. The color of the most central citation tree-ring indicates the publication year.
Node circle: The size of the radius indicates the number of published papers in the author’s co-authored network and the institutional co-authored network, and also indicates how often the keywords appear in the keyword co-occurrence network.
Link between nodes: A link indicates the presence of co-authorship or a co-occurrence relationship. The node colors indicate different years, and gradually change from cold colors to warm colors such that blue represents earlier years and red represents later years.
Centrality: Centrality is a measure of the importance of nodes in the network. CiteSpace uses this index to find and measure the importance of references, and uses purple circle to mark the references (or authors, journals, and institutions). The nodes labeled with a purple circle have greater centrality (≥ 0.1), and the nodes labeled with red circle show greater burst intensity.
Cluster #: Cluster analysis is carried out on the generated map, and each cluster is labeled by citing the title, keywords, and subject headings in the abstract of the citing reference (each label can be divided into several categories, such as #0, #1, #2…).
Results
Research hotspots and hot journals for the application of rTMS in the field of stroke rehabilitation based on citation relationships
Burst analyses of cited journals revealed neuroscience journals with research hotspots
Journal co-citation analyses of references from 1991 to 2019 cited by 315 studies published from 1999 to 2019 found that among the earliest journals, BRAIN, J NEUROPHYSIOL, and NAT NEUROSCI had hotspots in 2004, and NAT NEUROSCI had hotspots for the longest time period, i.e., from 2004 to 2014. PLOS ONE and FRONT HUM NEUROSCI had the most recent frontier hotspot (Figure 1).
Figure 1.
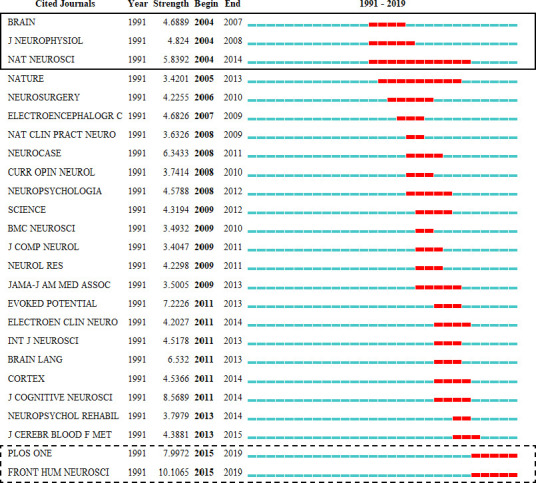
Top 25 cited journals with the strongest citation bursts among 315 studies published from 1999 to 2019.
(1) The Burst journals are the periodicals that were suddenly cited repeatedly at a certain time. (2) The figure shows the 25 most representative Burst journals covered by citations from 1991 to 2019 of 315 studies published from 1999 to 2019. (3) The red block represents a Burst year. The journals (solid line frame) with the earliest Bursts were BRAIN between 2004 and 2007, J NEUROPHYSIOL between 2004 and 2008, and NAT NEUROSCI between 2004 and 2014. Among them, NAT NEUROSCI spent the most time covering the research hotspot. In 2015–2019, the journals (virtual frame) with strong Bursts that appeared later were PLOS ONE and FRONT HUM NEUROSCI. (4) 1991 was the first year that a cited journal appeared. The strength represents the frequency intensity of the cited journal. ‘Begin’ and ‘End’ represent the time when the mutation of the cited journal began and ended, respectively.
Among the top 10 cited journals among 315 studies published from 1999 to 2019, STROKE was the most frequently cited
STROKE was cited 253 times; CLIN NEUROPHYSIOL was cited 232 times; and NEUROLOGY was cited 219 times (Figure 2).
Figure 2.
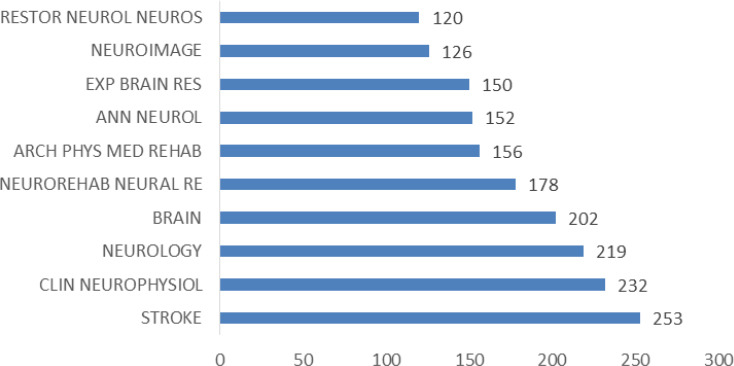
Top 10 most cited journals among 315 studies published from 1999 to 2019.
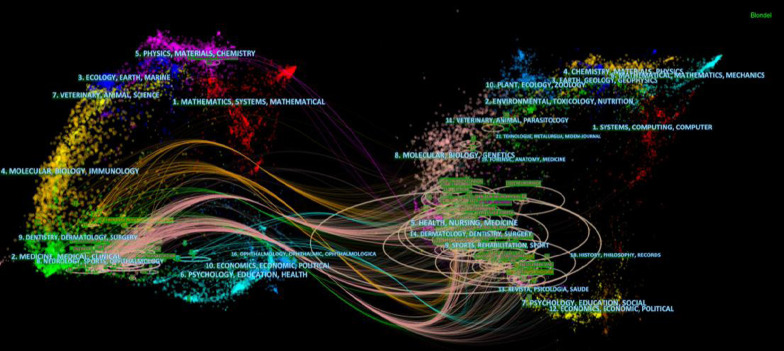
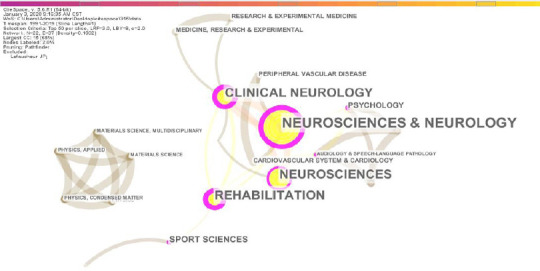
Dual-map overlays showed that hot cited journals were mainly in the fields of rehabilitation medicine and neuroscience
CiteSpace.5.6.R1 software provided basic reference data, and the basic map resource data regarding dual-map overlays were sourced from Journal Citation Reports 2011. The results of the dual-map overlays, shown in Figure 3, confirmed that the application of rTMS in post-stroke rehabilitation is still a current research hotspot, covered by major neuroscience journals such as STROKE and J NEUROSCI. Based on the Bblondel algorithm, the map of dual-map overlays among 315 studies is displayed in Figure 3: The left side of the figure shows the journal distribution of citing journals, and the right side shows the journal distribution of cited journals (Chen et al., 2014). The citing journals of the 315 studies are mainly from the fields of neurology, sports, medical science, medicine, and rehabilitation medicine. The cited journals of the 315 studies are mainly from the fields of health, nursing care, medical science, skin, oral health, surgery, sports, and rehabilitation medicine. Among them, rehabilitation medicine was most concentrated in the cited journals (shown in the center of the circle on the right), and is the hotspot of current research on rTMS.
Figure 3.
Visualization of dual-map overlays of citing journals and cited journals of 315 studies published from 1999 to 2019.
The colored curve indicates the path of citation, which originates from 11 fields of the citing journals on the left and points to 14 fields of the cited journals on the right.
Co-occurrence of WOS categories of 315 studies published from 1999 to 2019 shows that neurology and rehabilitation are the most important fields in the application of rTMS
The 315 included studies are from various fields, such as neuroscience, neurology, clinical neurology, rehabilitation, and sports science (Figure 4).
Figure 4.
Co-occurrence analysis of web of science categories of the 315 included studies.
References are organized by year from left to right, and the color is arranged from cold in 1999 to warm in 2019. The color of the most central citation tree-ring represents the publication year of the reference.
Co-citation of hot rTMS references based on cited references of 315 included studies
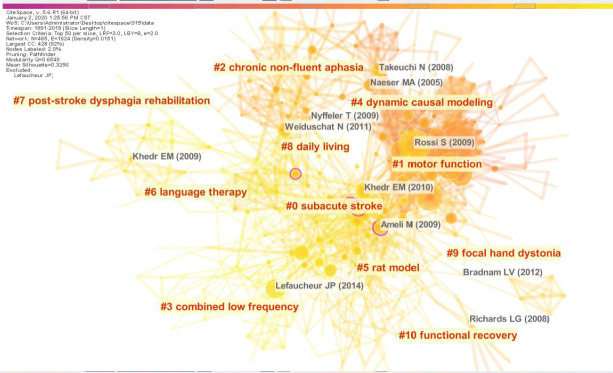
Eleven categories of cited references of 315 studies published from 1999 to 2019
The landscape generated using the clusters of co-cited references is exhibited in Figure 5. The top 100 references with the highest number of citations in each year were selected to build a co-cited network. After synthesizing the network for each year, the network was found to contain a total of 1624 citations and 465 nodes. The clustered research categories were divided into 11 groups (#0–10). Each cluster was labeled according to the title, keywords, and subject headings in the abstracts of the citing references that cited the clustered citation (Chen et al., 2014).
Figure 5.
Analysis of cited references in keyword clusters.
The color of a cluster block indicates the year in which the co-citation relationship in the cluster first occurred. The occurrence in the blue block is earlier than that in green block, and that in the yellow block is later than that in the green block. By analogy, the size of a node represents the number of citations of a reference, journal, or author, and the color of the line represents the time of the first citation. The citation time color is from 1999 to 2019, from left to right. There are 11 types of clusters (#0–10).
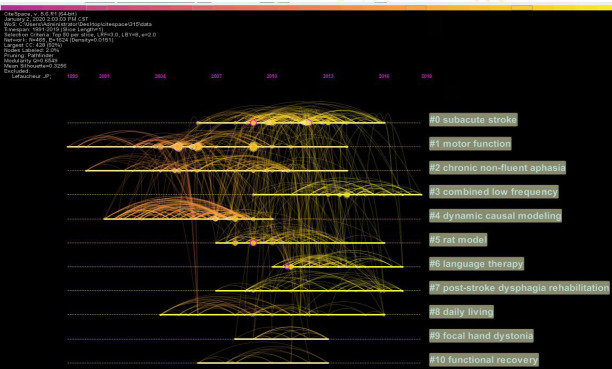
Time trends for the cited references of the 315 included studies
After generating the co-cited cluster map, the timeline map of the co-citation network could be obtained using the cluster number as the Y-axis and the publication year of the citation as the X-axis. The timeline view shows the time span and research progress of the development and evolution of each cluster sub-domain.
Figure 6 presents the characteristics of the time-span citation information for the 11 cluster domains. Taking the field represented by cluster #0 at the top of the figure (#0 subacute stroke) as an example, the time span is from 2006 to 2016. Moreover, there are a series of important landmark achievements between 2009 and 2012. For example, (1) Khedr et al. (2009) compared the long-term effects of 1 Hz and 3 Hz rTMS therapies (five daily sessions) on motor function recovery from acute stroke. This paper was cited 28 times. (2) Khedr et al. (2010) evaluated the effect of rTMS at two different frequencies on cortical excitability up to one year after motor function recovery and treatment, and this paper was cited 33 times. (3) Avenanti et al. (2012) observed the effects of regular rTMS and physical therapy combined with interventions for long-term behavioral and neurophysiological changes in patients with chronic mild stroke-induced dyskinesia, and this paper was cited 30 times. (4) Sasaki et al. (2013) elucidated the mechanisms of rTMS, and found it to be favorable for treating upper limb hemiplegia early after stroke. This paper was cited 26 times. (5) Du et al. (2016) compared the effects of high-frequency rTMS and low-frequency rTMS on early motor function recovery after stroke, and this paper was cited 8 times.
Figure 6.
Timeline view of co-citation analysis.
(1) The timeline view shows the way that references are co-cited over time. (2) Different years correspond to different colors, and the longer the color line segment, the larger the time span of the citation. (3) The node represents the reference name. Larger nodes indicate higher frequencies of the citations. The lines represent the connections between the references. (4) The longer the color line segment, the larger the time span of the citation. (5) The cluster label on the right is the category of research hotspots involved in the citation.
From 1999 to 2014, the cluster categories with the largest time span for the cited references are #1 motor function and #2 chronic non-fluent aphasia. The most frequently cited cluster categories are #0 subacute stroke and #1 motor function. In recent years, the cluster categories of the most concentrated citations were #3 combined low frequency and #6 language therapy.
Analysis of representative cited references in the 315 included studies
Content and perspective analysis: Reference information for the cited references of the 315 included studies is summarized in Table 1. The studies by Rossi et al. (2009) and Lefaucheur et al. (2014) are considered to be references regarding the guidelines for efficacy and safety, and are cited frequently. The studies by Takeuchi et al. (2015), Fregni et al. (2006), Khedr et al. (2005), and Avenanti et al. (2012) are randomized controlled trials. A study by Takeuchi et al. (2015) focused on hand function recovery. A study by Fregni et al. (2006) focused on the effect of rTMS on stroke patients. A study by Khedr et al. (2005) focused on the effects of real rTMS and sham rTMS on the recovery of neurological function in stroke patients. A study by Avenanti et al. (2012) focused on the effect of physical therapy combined with rTMS on motor function recovery in affected limbs. A study by Mansur et al. (2005) was a cross-controlled study focusing on the effect of low-frequency rTMS on improving motor function in stroke patients. A study by Kim et al. (2006) focused on the effects of high-frequency rTMS on exercise performance in patients with chronic stroke. A study by Hsu et al. (2012) was a meta-analysis. Hsu et al. (2012) concluded that the effect of rTMS varied according to the stimulation site. Particularly, low-frequency rTMS on the unaffected hemisphere may be more beneficial than high-frequency rTMS on the affected hemisphere. Although these concepts are generally well accepted, further verification via large-scale randomized controlled studies is required to clarify the different roles of various rTMS schemes in stroke treatment.
Table 1.
Ten representative studies on rTMS and post-stroke rehabilitation among the cited references of the included 315 studies
| Study | Citation counts | Design or type of articls | Sample size | Intervention | Outcomes | Highlights |
|---|---|---|---|---|---|---|
| Rossi et al. (2009) | 54 | Safety guideline | – | – | – | The present updated guidelines review issues of risk and safety of conventional transcranial magnetic stimulation (TMS) protocols. |
| Takeuchi et al. (2015) | 49 | Randomized controlled trial | 20 | Real versus sham rTMS in stroke patients | Amplitude of motor-evoked potentials in contralesional M1 and the transcallosal inhibition (TCI) duration | A disruption of the TCI by the contralesional M1 virtual lesion caused a paradoxical functional facilitation of the affected hand in stroke patients; this suggests a new neurorehabilitative strategy for stroke patients. |
| Fregni et al. (2006) | 45 | Randomized, sham-controlled, phase II trial | 15 | Fifteen patients with chronic stroke were randomized to receive active or sham rTMS of the unaffected hemisphere. | Motor function and corticospinal excitability at baseline, during and after 2 weeks of treatment | These results support and extend the findings of previous studies on rTMS in stroke patients because five consecutive sessions of rTMS increased the magnitude and duration of the motor effects. Furthermore, this increased dose of rTMS is not associated with cognitive adverse effects and/or epileptogenic activity. |
| Mansur et al. (2005) | 44 | Crossover, sham stimulation-controlled, double-blind study | 16 | Participants received three sessions of rTMS (1 Hz, 100% of motor threshold, 600 pulses) to the unaffected hemisphere over the primary motor (real or sham rTMS) and over the premotor cortex (real rTMS). | Simple reaction time (sRT), four-choice reaction time (cRT), Purdue Pegboard Test, and finger tapping. | The authors investigated the use of slow-frequency rTMS to the unaffected hemisphere to decrease interhemispheric inhibition of the lesioned hemisphere and improve motor function in patients within 12 months of a stroke. |
| Kim et al. (2006) | 38 | Single-arm, case analysis | 15 | Fifteen patients with chronic hemiparetic stroke practiced a complex, sequential finger motor task using their paretic fingers either after 10 Hz or sham rTMS over the contralateral primary motor cortex (M1). | MEP amplitude, and the plastic change | High-frequency rTMS of the affected motor cortex can facilitate practice-dependent plasticity and improve the motor learning performance in chronic stroke victims. |
| Khedr et al. (2005) | 35 | Randomized controlled trial | 52 | Patients were randomly assigned to real or sham rTMS. | Three clinical rating scales plus measures of MEPs evoked in muscles on the hemiplegic side. | Disability scales measured before rTMS, at the end of the last rTMS session, and 10 days later showed that real rTMS improved patients’ scores more than sham. |
| Lefaucheur et al. (2014) | 35 | Guidelines on the therapeutic use | – | – | – | The effects of rTMS in a number of indications reach level C (possible efficacy), including LF-rTMS of the left temporoparietal cortex in tinnitus and auditory hallucinations. |
| Khedr et al. (2010) | 33 | Randomized controlled trial | 48 | Forty-eight patients with acute ischemic stroke were randomly classified into three groups. The first two groups received real rTMS over motor cortex (3 and 10 Hz respectively) of the affected hemisphere and the third group received sham stimulation of the same site, daily for five consecutive days. | Disability and cortical excitability | Real rTMS over motor cortex can enhance and maintain recovery and may be a useful add on therapy in treatment of acute stroke patients. |
| Hsu et al. (2012) | 32 | Meta-analysis | 18 studies, 392 patients. | meta-analysis | The mean effect size and a 95% CI were estimated for the motor outcome and motor threshold using fixed and random effect models. | rTMS has a positive effect on motor recovery in patients with stroke, especially for those with subcortical stroke. Low-frequency rTMS over the unaffected hemisphere may be more beneficial than high-frequency rTMS over the affected hemisphere. |
| Avenanti et al. (2012) | 30 | Double-blind, randomized, single-center clinical trial | 30 | Patients received 10 daily sessions of 1 Hz rTMS over the intact motor cortex. In different groups, stimulation was either real (rTMS(R)) or sham (rTMS(S)) and was administered either immediately before or after PT. | Dexterity, force, interhemispheric inhibition, and corticospinal excitability | This interventional study provides Class I evidence that time-locked rTMS before or after physical therapy improves measures of dexterity and force in the affected limb in patients with chronic deficits more than 6 months poststroke. |
MEP: Motor evoked potential; rTMS: repetitive transcranial magnetic stimulation.
Analyzing the degree of innovation
According to the formula for calculating Sigma given by Professor Chen Chaomei (Chen et al, 2010), Sigma = (centrality+1)burstness (burstness on the index), the Sigma value is composed of two indicators: the intermediary centrality and the burst value. This formula can be used to identify innovative references and thus identify innovative topics. We have summarized the top 3 innovative references (Table 2). A study by Ameli et al. (2009) was a case analysis that confirmed the effectiveness of 10 Hz rTMS in the treatment of stroke. A study by Khedr et al. (2009) was a randomized controlled trial that found that 1 Hz rTMS in the unaffected hemisphere or 3 Hz rTMS in the affected hemisphere could promote functional recovery after stroke. A study by Barwood et al. (2011) was a case study that highlighted the potential effect of rTMS on language rehabilitation after stroke.
Table 2.
Three innovative studies about rTMS and post-stroke rehabilitation among the cited references of the included 315 studies
| Study | Sigma* | Design or type | Sample size (n) | Intervention | Outcomes | Highlights |
|---|---|---|---|---|---|---|
| Ameli et al. (2009) | 0.16 | Single-arm, case analysis | 29 | Pateints received 1 session of 10 Hz rTMS (5-second stimulation, 25-second break, 1,000 pulses, 80% of the resting motor threshold) applied over: 1) ipsilesional M1 and 2) vertex (control stimulation). | Motor function of the affected hand; neural activity in ipsilesional M1 | The beneficial effects of 10 Hz repetitive transcranial magnetic stimulation (rTMS) over ipsilesional M1 on motor function of the affected hand depend on the extension of MCA stroke. Neural activity in ipsilesional M1 may serve as a surrogate marker for the effectiveness of facilitatory rTMS. |
| Khedr et al. (2009) | 0.14 | Randomized controlled trial | 36 | The patients were randomly assigned into one of three groups; the first and second groups received real rTMS; 1 and 3 Hz and third group received sham stimulation, daily for 5 days. | Motor disability and cortical excitability | These results confirm that five daily sessions of rTMS over motor cortex using either 1 Hz over the unaffected hemisphere or 3 Hz over the affected hemisphere can enhance recovery. |
| Barwood et al. (2011) | 0.14 | Single-arm, case analysis | 12 | Low-frequency (1 Hz) rTMS was applied to six real stimulation and six sham placebo patients for 20 min per day, for 10 days | Behavioural language outcome measures | Considerable evidence to support the theory of rTMS modulating mechanisms of transcallosal disinhibition in the aphasic brain and highlight the potential clinical applications for language rehabilitation post-stroke. |
*Sigma = (centrality+1)burstness (burstness on the index) to identify innovative references (Chen et al., 2010).
Keywords for hotspots based on a co-occurrence analysis of keywords for the 315 included studies
The co-occurrence analysis of all the keywords in the 315 studies revealed 183 keyword nodes and 826 connection lines.
Hot word clusters revealed by the cluster analysis chart
The keyword clusters were divided into eight categories (#0–7) (Figure 7). The main three categories were: (1) #0: daily living, with 30 keywords; (2) #1 subacute stroke, with 26 keywords; (3) #2: chronic motor deficit, with 26 keywords (Figure 8).
Figure 7.
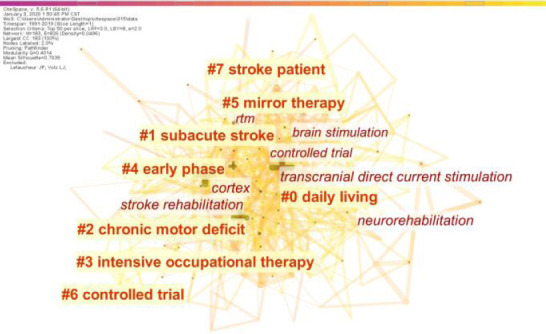
Cluster of keywords from 315 included studies.
The keyword clusters (LLR algorithm) were divided into eight categories (#0–7). Those without ‘#’ are high-frequency keywords.
Figure 8.
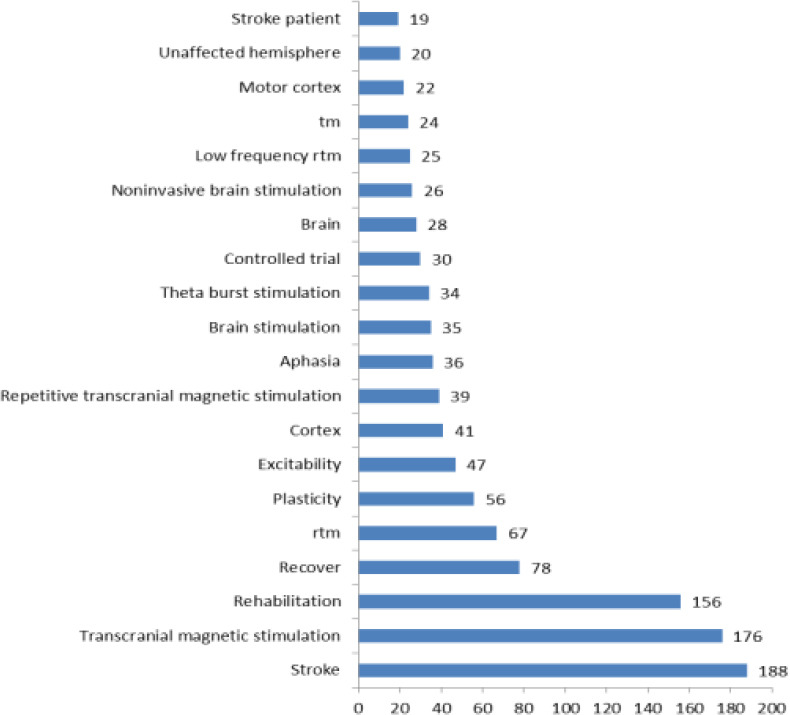
Frequency of the top 20 keywords.
Three stages of keyword mutations for the 315 included studies
Figure 9 shows the years when hot keywords began to appear and ended. An analysis of the year in which the keywords began (“Begin” in Figure 9) indicated two main points. (1) In the first stage, the primary motor cortex (2007–2010) was the first hot keyword, mainly describing the relationship between TMS and the primary motor cortex in stroke patients. (2) In the second stage, unaffected hemisphere (2008–2010), upper extremity function (2009–2012), aphasia (2009–2015), language (2011–2013), and hemispatial neglect (2012–2015) were the hot keywords, mainly describing the effects of rTMS on the unaffected hemisphere, hemispatial neglect, upper limb function, and speech function in patients with stroke. (3) In the third stage, noninvasive brain stimulation (2014–2019) and motor function recovery (2016–2017) were the latest hot words, reflecting the finding that a noninvasive brain stimulation method can promote the recovery of motor function after stroke. The ending years of the above highlighted keywords are shown in Figure 9.
Figure 9.
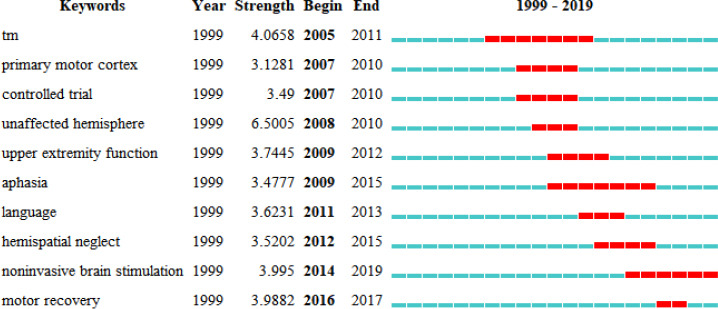
Top 10 keywords with the strongest citation bursts of the 315 included studies published from 1999 to 2019.
“Unaffected hemisphere” was the keyword with the highest burst intensity. The year represents the earliest year of the keyword appearance. The strength stands for the citation strength. ‘Begin’ and ‘End’ represent the start and end time of the mutation, respectively.
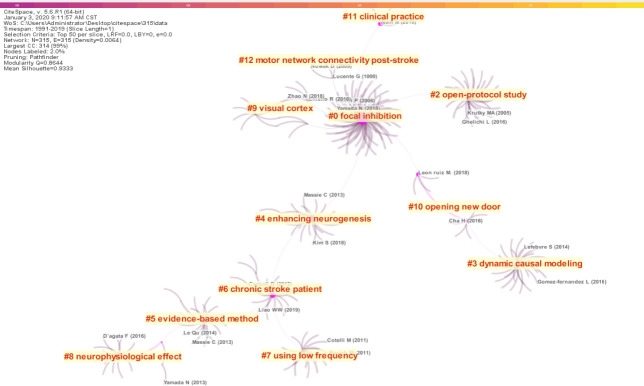
Bibliographic coupling analysis of 13 academic hotspots among the 315 included studies
Among the 315 studies, if two or more studies cited a reference together, then these two or more studies constituted a coupling relationship. Cluster analysis of the coupled references yielded 13 categories (#0–12). The hottest words in the largest coupling area were #0 focal inhibition and #1 open-protocol trial (Figure 10).
Figure 10.
Bibliographic coupling of the 315 included studies (cluster #0–12).
The 13 categories were obtained via cluster analysis of the coupled references.
Analysis of authoritative authors, institutions, and countries in the application of rTMS in post-stroke rehabilitation
Authoritative authors of cited references of the 315 included studies
Among all co-cited authors, the most cited authors were KHEDR EM (118 times), followed by FREGNI F (104 times) and TAKEUCHI N (104 times). These three authors are authoritative experts in their field (Table 3).
Table 3.
Top10 authoritative authors in cited references of the 315 included studies
| Counts | Centrality | Years | Authors |
|---|---|---|---|
| 118 | 0.05 | 2006 | KHEDR EM (Egypt) |
| 104 | 0.22 | 2006 | FREGNI F (USA) |
| 104 | 0.15 | 2006 | TAKEUCHI N (Japan) |
| 78 | 0.03 | 2008 | ROSSI S (Italy ) |
| 78 | 0.03 | 2004 | WASSERMANN EM (USA) |
| 72 | 0.01 | 2005 | MURASE N (Japan) |
| 70 | 0.01 | 2006 | MANSUR CG (Brazil) |
| 69 | 0.02 | 2006 | KIM YH (South Korea) |
| 69 | 0.01 | 2008 | LEFAUCHEUR JP (France) |
| 66 | 0.59 | 2005 | CHEN R (USA) |
Authoritative institutions of cited references of the 315 included studies
Of the 315 studies, the most cited institution was Jikei Univ (Jikei University School of Medicine, Japan) (19 times), followed by Univ Queensland (The University of Queensland, Australia) (8 times), Univ Minnesota (University of Minnesota, USA) (8 times), Harvard Med Sch (Harvard Medical School, USA) (6 times), and McGill Univ (McGill University, Canada) (6 times). These five institutions are authoritative institutions in their field (Table 4).
Table 4.
Top10 authoritative institutions in cited references of the 315 included studies
| Counts | Centrality | Years | Institutions |
|---|---|---|---|
| 19 | 0 | 2011 | Jikei Univ (Jikei University School of Medicine, Japan) |
| 8 | 0 | 2011 | Univ Queensland (The University of Queensland, Australia) |
| 8 | 0 | 2015 | Univ Minnesota (University of Minnesota, USA) |
| 6 | 0 | 2016 | Harvard Med Sch (Harvard Medical School) |
| 6 | 0.01 | 2012 | McGill Univ (McGill University, Canada) |
| 5 | 0 | 2011 | Royal Brisbane & Womens Hosp (Royal Brisbane and Womens’ Hospital, Australia) |
| 4 | 0 | 2014 | Eulji Univ Hosp (Eulji University Hospital, South Korea) |
| 4 | 0 | 2017 | Univ Sao Paulo (University of Sao Paulo, Brazil) |
| 4 | 0 | 2013 | Sichuan Univ (Sichuan University, China) |
| 4 | 0.01 | 2008 | Max Planck Inst Neurol Res (Max Planck Institute, Germany) |
Distribution of authoritative countries with high-level research in burst analysis based on the citation analysis of 315 studies
There were six major burst countries, including the United Kingdom, Germany, the United States, Australia, South Korea, and China (Figure 11). The United Kingdom, Germany, and the United States, which are relatively developed in terms of imaging research, were the first to focus on rTMS for stroke treatment. The number of studies in China exploded in 2017–2019, indicating that China has paid more attention to this field in recent years.
Figure 11.
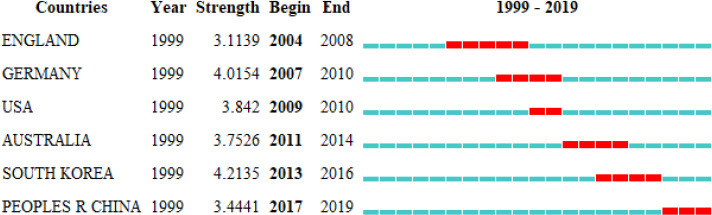
Top 6 countries with the strongest citation bursts among the 315 included studies.
There are six major burst countries, including the United Kingdom, Germany, the USA, South Korea, and China. A Burst appeared in the United Kingdom from 2004 to 2008 and in China from 2017 to 2019. The year represents the earliest year that a Burst was seen in a country. The strength represents the intensity of the frequency of the country. ‘Begin’ and ‘End’ represent the beginning and ending time of the mutation, respectively.
Discussion
Advantages and challenges related to the application of TMS in stroke rehabilitation
TMS and motor function recovery after stroke
In addition to its application in the rehabilitation of motor function after stroke, TMS has a positive effect on the early prediction of motor recovery (Lüdemann-Podubecká and Nowak, 2016). However, there are still many issues to be resolved in the application of TMS in the early prediction of motor function recovery after stroke, such as the optimal detection time after stroke, whether it can be equally effective in the prediction of rehabilitation results for the upper and lower limbs, and whether it can be used together with other evaluation tools to provide more accurate predictions.
rTMS and swallowing function rehabilitation after stroke
This treatment has gradually become a hot topic (Ünlüer et al., 2019). Based on the neurophysiological mechanisms of swallowing, multiple treatment schemes have been developed involving different frequencies, intensities, and locations. However, these have specific effects on the rehabilitation of swallowing function. Further study regarding the neurophysiological mechanisms of rTMS is needed. A practical and individualized scheme could be developed by studying the swallowing neural network and exploring the optimal time window of neural stimulation for swallowing regulation.
rTMS and neurological repair in the subacute and chronic phases of stroke
Kang et al. (2019) found no obvious adverse reactions for rTMS and determined that the treatment was safe. Nevertheless, different rTMS stimulation programs have been found to have different effects. High-frequency rTMS can increase cortical excitability, while low-frequency rTMS can decrease cortical excitability. Therefore, rTMS treatment schemes should vary according to the outcomes for different neurological impairment in patients with stroke, such as dyskinesia, cognitive impairment, and dysphagia.
Generally accepted conclusions regarding rTMS
(1) rTMS has a positive effect on motor recovery in patients with subcortical stroke (Hsu et al., 2012). (2) Within 12 months after stroke, slow-frequency rTMS could be used in unaffected hemispheres to reduce the inter-hemispheric inhibition of damaged hemispheres and improve motor function (Mansur et al., 2005). It is suggested that low-frequency rTMS in the unaffected hemisphere may be more beneficial than high-frequency rTMS in the affected hemisphere. (3) Low-frequency rTMS has become a potential tool for neurorehabilitation and language recovery of chronic non-fluent aphasia after chronic stroke (Barwood et al., 2011).
Timing of research hotspots revealed by analysis of keywords in rTMS studies
Noninvasive brain stimulation (2014–2019) and motor recovery (2016–2017) have become the latest hot keywords, which is in line with the main trends in current research (Fisicaro et al., 2019; Lee et al., 2019; Veldema et al., 2019).
Analysis of authoritative countries obtained by analyzing highly-cited references of related rTMS studies
Chinese scholars have been more active in researching post-stroke rTMS for rehabilitation. According to the Chinese expert consensus on rTMS, the biggest problem is accurate stimulation of the target (Chinese Society of ECT & Neurostimulation, 2018). The main problems in the application of rTMS for related diseases include: (1) factors that influence the treatment effect; (2) the action mechanism of various diseases; (3) the combination of rTMS with drug treatment, for which there is not currently an effective standard.
Limitations in the application of rTMS
Although most rTMS studies have shown positive therapeutic effects, large-sample randomized controlled data are lacking. The number of case studies is high. Further, few high-level clinical studies have examined the treatment of acute stroke. In addition, because of a limitation of the CiteSpace software, this paper only analyzed references in the WOS database. The data in other databases such as PubMed have not been comprehensively analyzed. Therefore, the 315 included studies only represent information from the WOS database, and not all of the information in the rTMS field.
Significance and contribution
Based on bibliometric visual analysis, we present a visualization map of rTMS in the treatment of post-stroke rehabilitation. The map shows the hot research directions of rTMS in recent years, such as the influence of rTMS on the unaffected hemisphere, hemispatial neglect, language function, and motor function recovery in stroke patients. Simultaneously, we observed deficiencies in the research in this field. With the continuous improvement and development of rTMS technology, new insights regarding the pathogenesis of various related diseases, which will greatly promote the research and application of rTMS, are expected. The international research hotspots obtained from our bibliometrics analysis of 315 studies using CiteSpace software are in line with current clinical practice of rTMS for stroke rehabilitation, indicating that the methodology is valid.
Footnotes
Conflicts of interest: The authors declare that there are no conflicts of interest associated with this manuscript.
Financial support: None.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
C-Editor: Zhao M; S-Editors: Wang J, Li CH; L-Editors: Koke S, Frenchman B, Qiu Y, Song LP; T-Editor: Jia Y
References
- 1.Ameli M, Grefkes C, Kemper F, Riegg FP, Rehme AK, Karbe H, Fink GR, Nowak DA. Differential effects of high-frequency repetitive transcranial magnetic stimulation over ipsilesional primary motor cortex in cortical and subcortical middle cerebral artery stroke. Ann Neurol. 2009;66:298–309. doi: 10.1002/ana.21725. [DOI] [PubMed] [Google Scholar]
- 2.Avenanti A, Coccia M, Ladavas E, Provinciali L, Ceravolo MG. Low-frequency rTMS promotes use-dependent motor plasticity in chronic stroke: a randomized trial. Neurology. 2012;78:256–264. doi: 10.1212/WNL.0b013e3182436558. [DOI] [PubMed] [Google Scholar]
- 3.Barwood CH, Murdoch BE, Whelan BM, Lloyd D, Riek S, O’ Sullivan JD, Coulthard A, Wong A. Improved language performance subsequent to low-frequency rTMS in patients with chronic non-fluent aphasia post-stroke. Eur J Neurol. 2011;18:935–943. doi: 10.1111/j.1468-1331.2010.03284.x. [DOI] [PubMed] [Google Scholar]
- 4.Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;101:5303–5310. doi: 10.1073/pnas.0307513100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen C, Dubin R, Kim M. Emerging trends and new developments in regenerative medicine: a scientometric update (2000-2014) Exp Opin Biol Ther. 2014;14:1295–1317. doi: 10.1517/14712598.2014.920813. [DOI] [PubMed] [Google Scholar]
- 6.Chen C, Song M. Visualizing a field of research: A methodology of systematic scientometric reviews. PLoS One. 2019;14:e0223994. doi: 10.1371/journal.pone.0223994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chinese Society of ECT & Neurostimulation (2018) Chinese experts consensus on repetitive transcranial magnetic stimulation. Zhonghua Yixue Zazhi. 7:4–9. [Google Scholar]
- 8.Du J, Yang F, Hu J, Hu J, Xu Q, Cong N, Zhang Q, Liu L, Mantini D, Zhang Z, Lu G, Liu X. Effects of high- and low-frequency repetitive transcranial magnetic stimulation on motor recovery in early stroke patients: Evidence from a randomized controlled trial with clinical, neurophysiological and functional imaging assessments. Neuroimage Clin. 2019;21:101620. doi: 10.1016/j.nicl.2018.101620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisicaro F, Lanza G, Grasso AA, Pennisi G, Bella R, Paulus W, Pennisi M. Repetitive transcranial magnetic stimulation in stroke rehabilitation: review of the current evidence and pitfalls. Ther Adv Neurol Disord. 2019 doi: 10.1177/1756286419878317. doi: 101177/1756286419878317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fregni F, Boggio PS, Valle AC, Rocha RR, Duarte J, Ferreira MJ, Wagner T, Fecteau S, Rigonatti SP, Riberto M, Freedman SD, Pascual-Leone A. A sham-controlled trial of a 5-day course of repetitive transcranial magnetic stimulation of the unaffected hemisphere in stroke patients. Stroke. 2006;37:2115–2122. doi: 10.1161/01.STR.0000231390.58967.6b. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg D, McCouch, Kleinberg J. Constructing comparative genome maps with unresolved marker order. Pac Symp Biocomput. 2002;7:139–150. [PubMed] [Google Scholar]
- 12.Hordacre B, Comacchio K, Moseley GL. The unusual case of dental pain with sham repetitive transcranial magnetic stimulation: benign idiosyncrasy or diagnostic opportunity? Brain Stimul. 2019 doi: 10.1016/j.brs.2019.12.003. doi: 101016/jbrs201912003. [DOI] [PubMed] [Google Scholar]
- 13.Hsu WY, Cheng CH, Liao KK, Lee IH, Lin YY. Effects of repetitive transcranial magnetic stimulation on motor functions in patients with stroke: a meta-analysis. Stroke. 2012;43:1849–1857. doi: 10.1161/STROKEAHA.111.649756. [DOI] [PubMed] [Google Scholar]
- 14.Kang N, Lee RD, Lee JH, Hwang MH. Functional balance and postural control improvements in patients with stroke after noninvasive brain stimulation: a meta-analysis. Arch Phys Med Rehabil. 2020;101:141–153. doi: 10.1016/j.apmr.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Khedr EM, Abdel-Fadeil MR, Farghali A, Qaid M. Role of 1 and 3 Hz repetitive transcranial magnetic stimulation on motor function recovery after acute ischaemic stroke. Eur J Neurol. 2009;16:1323–1330. doi: 10.1111/j.1468-1331.2009.02746.x. [DOI] [PubMed] [Google Scholar]
- 16.Khedr EM, Ahmed MA, Fathy N, Rothwell JC. Therapeutic trial of repetitive transcranial magnetic stimulation after acute ischemic stroke. Neurology. 2005;65:466–468. doi: 10.1212/01.wnl.0000173067.84247.36. [DOI] [PubMed] [Google Scholar]
- 17.Khedr EM, Etraby AE, Hemeda M, Nasef AM, Razek AA. Long-term effect of repetitive transcranial magnetic stimulation on motor function recovery after acute ischemic stroke. Acta Neurol Scand. 2010;121:30–37. doi: 10.1111/j.1600-0404.2009.01195.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim YH, You SH, Ko MH, Park JW, Lee KH, Jang SH, Yoo WK, Hallett M. Repetitive transcranial magnetic stimulation-induced corticomotor excitability and associated motor skill acquisition in chronic stroke. Stroke. 2006;37:1471–1476. doi: 10.1161/01.STR.0000221233.55497.51. [DOI] [PubMed] [Google Scholar]
- 19.Mansur CG, Fregni F, Boggio PS, Riberto M, Gallucci-Neto J, Santos CM, Wagner T, Rigonatti SP, Marcolin MA, Pascual-Leone A. A sham stimulation-controlled trial of rTMS of the unaffected hemisphere in stroke patients. Neurology. 2005;64:1802–1804. doi: 10.1212/01.WNL.0000161839.38079.92. [DOI] [PubMed] [Google Scholar]
- 20.Lee J, Lee A, Kim H, Shin M, Yun SM, Jung Y, Chang WH, Kim YH. Different brain connectivity between responders and nonresponders to dual-mode noninvasive brain stimulation over bilateral primary motor cortices in stroke patients. Neural Plast. 2019;2019:3826495. doi: 10.1155/2019/3826495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, Cantello RM, Cincotta M, de Carvalho M, De Ridder D, Devanne H, Di Lazzaro V, Filipović SR, Hummel FC, Jääskeläinen SK, Kimiskidis VK, Koch G, Langguth B, Nyffeler T, Oliviero A, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS) Clin Neurophysiol. 2014;125:2150–2206. doi: 10.1016/j.clinph.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 22.Lüdemann-Podubecká J, Nowak DA. Mapping cortical hand motor representation using TMS: a method to assess brain plasticity and a surrogate marker for recovery of function after stroke. Neurosci Biobehav Rev. 2016;69:239–251. doi: 10.1016/j.neubiorev.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Rossi S, Hallett M, Rossini PM, Pascual-Leone A Safety of TMS Consensus Group. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120:2008–2039. doi: 10.1016/j.clinph.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takeuchi N, Chuma T, Matsuo Y, Watanabe I, Ikoma K. Repetitive transcranial magnetic stimulation of contralesional primary motor cortex improves hand function after stroke. Stroke. 2005;36:2681–2686. doi: 10.1161/01.STR.0000189658.51972.34. [DOI] [PubMed] [Google Scholar]
- 25.Ünlüer NÖ, Temuçin ÇM, Demir N, Serel Arslan S, Karaduman AA. Effects of low-frequency repetitive transcranial magnetic stimulation on swallowing function and quality of life of post-stroke patients. Dysphagia. 2019;34:360–371. doi: 10.1007/s00455-018-09965-6. [DOI] [PubMed] [Google Scholar]
- 26.van Lieshout ECC, van der Worp HB, Visser-Meily JMA, Dijkhuizen RM. Timing of repetitive transcranial magnetic stimulation onset for upper limb function after stroke: a systematic review and meta-analysis. Front Neurol. 2019;10:1269. doi: 10.3389/fneur.2019.01269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Veldema J, Bösl K, Neumann G, Verheyden G, Nowak DA. Noninvasive brain stimulation in rehabilitation of hemispatial neglect after stroke. CNS Spectr. 2019 doi: 10.1017/S1092852918001748. doi: 101017/S1092852918001748. [DOI] [PubMed] [Google Scholar]
- 28.Zhang C, Zheng X, Lu R, Yun W, Yun H, Zhou X. Repetitive transcranial magnetic stimulation in combination with neuromuscular electrical stimulation for treatment of post-stroke dysphagia. J Int Med Res. 2019;47:662–672. doi: 10.1177/0300060518807340. [DOI] [PMC free article] [PubMed] [Google Scholar]