Abstract
Multimorbidity refers to the co-occurrence of two or more chronic conditions, where no one disease is considered the central disease. Individuals with multimorbidity experience increased patient health complexity, increased disability and functional decline, and increased health care utilization. Rehabilitation therapists are well positioned to address the complex functional needs that can contribute to disability for people living with multimorbidity; however, it is not well understood how they address these needs within the home care setting. A rapid review was conducted to identify and synthesize the existing literature on home care rehabilitation services for clients with multimorbidity and the effect of those services. Two electronic databases (Medline and CINAHL) were searched. The Journal of Comorbidity was hand-searched for thoroughness because this journal focuses on populations with multiple chronic conditions. This rapid review included observational and experimental studies that focused on rehabilitation therapy interventions embedded within existing home care systems for adults with multimorbidity. Four studies were included in the final review. The results revealed that therapists delivered interventions aimed towards improving functional outcomes related to activities of daily living and instrumental activities of daily living. Physical therapy interventions were the only therapy delivered in three of the four studies included. Furthermore, 50% of these studies explicitly included people with chronic conditions impacting the musculoskeletal system only. This review offers an important perspective on how home care rehabilitation therapy interventions and outcomes are operationalized for individuals with multimorbidity. Despite the varying definitions of multimorbidity, therapeutic intervention supported functional improvements.
Keywords: Rehabilitation, home care, multimorbidity, occupational therapy, physical therapy
Introduction
Nearly 919,000 Canadians receive home care services annually.1 Of those receiving home care services, nearly 494,300 (approximately 54%) home care clients have two or more chronic conditions and of those with multiple chronic conditions, 277,700 report unmet home care needs.1 The prevalence of chronic conditions is trending upward as the aging population grows and more than one in 30 adults aged 20 years and older experience the impact of more than one chronic condition.2 Internationally, a meta-analysis of studies reporting prevalence rates of multimorbidity has reported that the pooled prevalence rate of multimorbidity is 33.1%.3 Multimorbidity is the umbrella term used to capture the complex concept of multiple co-occurring chronic conditions, wherein no one condition is considered the central disease.4–8 There are varied definitions and methodologies in the literature with respect to defining multimorbidity and which chronic conditions should be used in the definition of multimorbidity. The variation in operationalizing multimorbidity influences the ability to consistently evaluate and compare across different health care settings and regions.9–13 Despite the inconsistency in the literature surrounding the definition of multimorbidity, there is evidence to demonstrate that living with multiple chronic conditions increases patient health complexity, increases disability and functional decline, and increases health care utilization.8,14–19
Occupational therapists and physical therapists are health care professionals that work in the home care setting and assess and provide a variety of interventions to address the complex functional impairments and subsequent disability that can be experienced by those with multimorbidity. Rehabilitation therapists consider the broader determinants of health in clinical practice and align with a biopsychosocial framework of health care. The interaction between the clinical, biological, and psychosocial determinants of health are seen as the antecedents for disability and overall functioning.20 There is growing literature that supports occupational and physical therapy interventions improve functional outcomes for individuals experiencing multiple chronic conditions in primary care.21,22 It is not however, well understood how rehabilitation therapy addresses the functional complexities that individuals with multimorbidity experience in the home care setting. A large proportion of home care clients have multiple chronic conditions and unmet home care needs.1 This rapid review was guided by the following research question: does receipt of rehabilitation therapy (occupational therapy and/or physical therapy) influence functional outcomes and health care utilization for home care clients with multimorbidity? The review aims to identify and synthesize the existing literature on home care rehabilitation services delivered within the existing home care setting for clients with multimorbidity and the effect of those services.
Methods
Rapid reviews provide a systematic framework to gather and appraise the available literature about a practice or policy issue within an accelerated timeframe.23,24 In order to satisfy the timeline criterion, the reviewer constructs a very specific research question, introduces a variety of search strategy limitations (e.g., dates, geographic location, and search engines), and conducts a “simple” critical appraisal.24 The research question and practice issue evolved from the need to better understand multimorbidity and evidence-based rehabilitation interventions that are delivered within the existing home care infrastructure.
Inclusion/exclusion criteria
The following inclusion criteria were applied: 1) studies including occupational therapy and/or physical therapy delivered interventions, 2) observational and experimental studies, 3) studies where services were delivered within the home care setting, 4) studies where occupational therapy and/or physical therapy were delivered as part of usual care (i.e., clients were already receiving usual home care therapy or were referred to existing home care therapeutic services), and were embedded within the home care setting, and 5) studies that included adults with multiple chronic conditions (multimorbidity). The following exclusion criteria were applied: 1) case studies, reviews, qualitative studies and government reports, 2) non-English literature, 3) occupational therapy and/or physical therapy interventions delivered within a community setting that extended beyond home care delivered rehabilitation services (e.g., outpatient rehabilitation, community falls prevention) and 4) palliative clients with multimorbidity.
An additional exclusion criterion was applied within the MEDLINE database because of the quantity of articles retrieved in the initial search. Given the expedited nature of this type of review, and the context (Ontario, Canada) within which the review was conducted, the search was limited to articles published within the last 12 years in MEDLINE. This timeframe coincides with the development and publication of the Ontario framework for preventing and managing chronic disease.25 This timeframe also includes a systematic review from 2012 that captures interventions delivered to people with multimorbidity.22 The systematic review by Smith et al.,22 was broader in professional scope, and health care context than the current review being conducted. It identified 10 studies targeting interventions for individuals with multimorbidity.
Search strategy
Two electronic databases (Medline and CINAHL) were searched in October/November 2019. The Journal of Comorbidity was also hand-searched for thoroughness because this journal targets research aimed at individuals with multiple chronic conditions, which is the population of interest for this review. A health sciences librarian provided search strategy guidance and reviewed key words/phrases and medical subheadings in addition to providing recommendations about broadening the search through truncation. Key words/phrases and medical subheadings used included: rehabilitation, occupational therapy, physical therapy, home care services, multimorbidity, comorbidity, and chronic disease. Additionally, variations on these terms were applied such as truncation and expansion to encompass a broader range of articles that touched on these subjects. One author (AM) checked reference lists of relevant articles in addition to the database searches. Relevant articles wherein the reference list was hand-searched included: articles that were retained for the final analysis, and articles that discussed therapeutic interventions delivered for individuals with multimorbidity, irrespective of the context it was delivered. Additionally, a second author (CD) screened approximately 10% of the articles retrieved from the databases to ensure consistency across the applied inclusion/exclusion criteria.
Assessment of study quality
The quality of each study included in the review was assessed using the Joanna Briggs Institute Critical Appraisal Checklists. The Joanna Briggs Institute is an established international leader in evidence-based healthcare that offers online access to several critical appraisal tools and accompanying reviewer manuals designed for systematic reviews.26 These tools can also be used for assessing study quality in other forms of reviews or in less formal settings for learning and critical appraisal development.26 One author (AM) assessed the quality of each study and a second author (CD) reviewed these assessments in conjunction with the studies to support article inclusion.
Results
Article selection
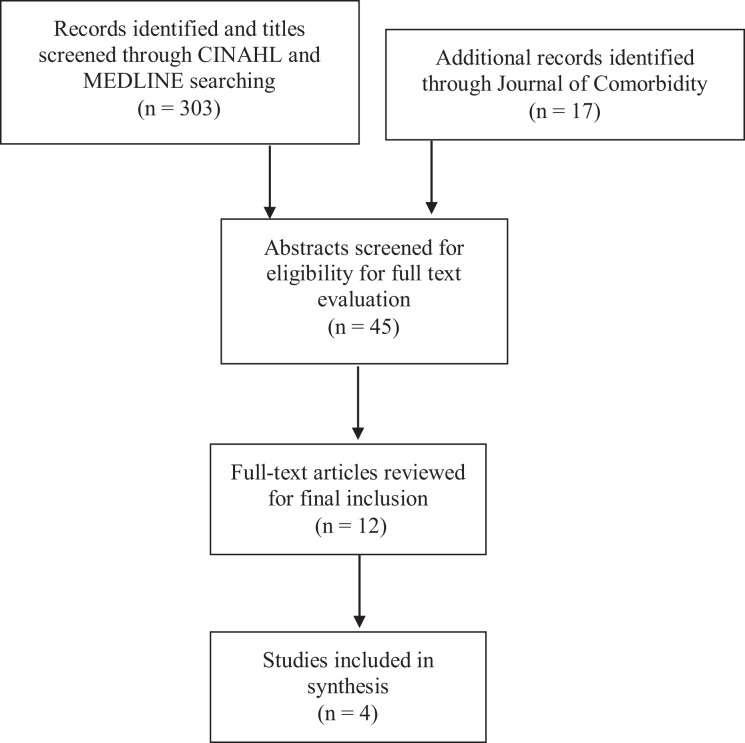
Title screening within each database yielded a total of 45 articles that underwent further abstract screening. Reasons for article exclusion at the abstract screening stage included: articles focused on singular chronic conditions (27%), the treatment was not delivered by an occupational therapist or physical therapist (18%), and the delivery setting was not in the home (13%). After title and abstract review, 12 articles remained for a full text review. After full text review, four articles met the studies inclusion/exclusion criteria and underwent data abstraction. Reasons for article exclusion after full text review were: care delivery setting was not home care (n = 2), there was an emphasis on single chronic conditions (n = 1), and the rehabilitation intervention was delivered by other health care professionals (n = 6). In one of the studies reviewed, the intervention was delivered by a health professional other than an occupational therapist and/or physical therapist in addition to the care delivery setting not being in the home. The process for article selection is outlined in Figure 1.
Figure 1.
Articles identified at each stage of the review.
Study quality was assessed for the four articles included in this review. Each of the four articles satisfied at minimum of 7 out of 11 of the criteria on the Joanna Briggs Institute Critical Appraisal Checklist. Additionally, a minimum of two criteria on the checklist were considered “not applicable” across all four articles. Overall, all four articles remained in the review following the article appraisal. The quality of each study was evaluated but the appraisal scores were not used as inclusion/exclusion criteria. Consistent with a rapid review methodology, a simple critical evaluation process was completed to balance rigor and timeliness of the review.
Description of the studies included
Of the four articles retained for this rapid review, two were retrospective cohort studies27,28 and two were retrospective chart reviews.29,30 Two of the studies were conducted in Ontario, Canada,27,29 one study was conducted in the Basilicata Region of Italy,28 and one study was conducted in Pennsylvania, USA.30 One of the studies included both occupational therapy and physical therapy interventions27 and three of the studies included physical therapy interventions only.28–30 The studies were heterogeneous with respect to sample size, data collection, and population definition. The cohort studies had larger sample sizes that approximated the population of the given geographical region for a defined population, whereas the retrospective chart reviews had smaller, organizational boundaries for data collection. The sample sizes ranged from 99 to 99,76427–30 (refer to Table 1 for details of included studies).
Table 1.
Study characteristics of included articles.
| Study Authors and Location | Participants | How chronic conditions were reported | Intervention | Outcomes | Functional Results | Effect of multiple chronic conditions on the outcome of interest |
|---|---|---|---|---|---|---|
| Cook et al. 27
Location: Ontario, Canada |
Long-stay home care clients with musculoskeletal conditions in Ontario between 2003 and 2009 (N = 99,764). | Charlson Crosswalk Comorbidity Index as a covariate in the analysis exploring the relationship between receipt of rehabilitation therapy on changes in functional states. The mean score on the Charlson Crosswalk Comorbidity Index was 1.554 + 1.41 (age not considered in the calculation of this score, and therefore it is a lower score than what could be expected). | Occupational Therapy and Physical therapy | Health service use and functional changes. | Functional improvements observed among clients with deficits at baseline; therapy decreased the risk of hospitalization or institutionalization (HR = 0.926; 95% CI = 0.897–0.956) and increased the risk of discharge due to service completion (HR = 1.498; 95% CI = 1.447–1.550). | Lower probability of being discharged from home care (HR = 0.929; 95% CI = 0.919–0.939), higher risk of being discharged to hospital or long-term care (HR = 1.051; 95% CI = 1.042–1.059) and higher likelihood of death (HR = 1.226; 95% CI = 1.208–1.244). |
| Fusco et al.28
Location: Basilicata Region, Italy |
Older adults (aged 70+) on home care rehabilitation program in 2004 (N = 598). | Disease count and stratification for the analysis. Stratification as follows: 0–2 diseases (referent) and 3+ diseases. Average number of diseases was 2.4 (sd = 1.5). | Physical Therapy | Functional and medical indicators of health as captured by the Minimum Data Set for Home Care (MDS-HC). | Approximately 1/3 of participants improved functionally, as operationalized using activities of daily living. The remaining 66% of participants remained constant or worsened with respect to functional status. | The number of chronic conditions was not significantly predictive of the functional recovery among study participants across all models. The authors presented 5 models: 1. unadjusted univariate model (OR = 0.96; 95% CI = 0.85–1.07), 2. adjusted model with all confounders (OR = 1.01; 95% CI = 0.89–1.15), 3. adjusted model with main diseases (OR = 1.02; 95% CI = 0.88–1.17), 4. adjusted model with baseline activities of daily living scores (OR = 0.96; 95% CI = 0.85–1.07), and 5. accounting for floor to ceiling effects (OR = 1.01; 95% CI = 0.87–1.18). |
| Peng et al. 29
Location: Toronto, Ontario, Canada |
Adult (18+ year of age) home care clients receiving physical therapy between July 2009 and July 2010 with chronic conditions in Toronto, Ontario, Canada (N = 296). | Disease count (53% of participants had 1 chronic condition and 47% of the study participants had 2+ chronic conditions). | Physical Therapy | Self-management goal setting and goal achievement. | Goals were mostly action-oriented in nature and basic demographics and number of chronic conditions had no association with setting self-management goals. More than 85% of goals set were achieved irrespective of whether they were classified as self-management. | The quantity of chronic conditions did not influence the ability to set self-management goals. Irrespective of the number of chronic conditions, more than 93% of self-management goals were met. |
| Kim et al.30
Location: York, Pennsylvania |
All patients who had an orthopedic diagnosis and were admitted to and discharged from home health care in 2005 in York, Pennsylvania (N = 99). | Disease count where the average number of diseases was 5.15 (range 2–14). | Physical Therapy | Functional outcomes (toileting, transferring, and ambulation/ locomotion) as identified using the Outcome and Assessment Information Set (OASIS) functional activity scores. | Functional improvements were observed in patients across all three activities of daily living. For toileting, 91% of patients improved by at least one score. 64.3% of patients improved in their ability to transfer, and 33.4% of patients improved in their ability to ambulate. | There was no relationship between “comorbidities,” physiotherapy visits, and the three functional outcomes (toileting, ambulation and transferring). |
How chronic conditions were considered
Individuals with musculoskeletal (MSK) conditions or orthopedic conditions were the population of interest in two of the studies.27,30 These two studies were retained for this rapid review because they considered arthritis, osteoporosis, and degenerative disc disease; however, they also included individuals who had experienced an acute injury/fracture.27,30 The inclusion criteria for the study by Cook et al.27 required participants to have “at least one MSK condition” (p. 1039). The authors considered chronic conditions as a covariate in their analysis of the association between rehabilitation therapy and functional state changes. The Charlson Crosswalk Comorbidity Index, a version of the Charlson Comorbidity Index, was used as a measure of multiple chronic conditions without considering age. The Charlson Comorbidity Index is a common method used to capture multimorbidity and the impact of multimorbidity on mortality in community and primary care settings.31 All patients in the study by Kim et al.,30 had at least one orthopedic condition and could have another co-occurring chronic condition. Because the definition of orthopedic conditions inherently included multiple chronic conditions, it was not possible to determine if the patients’ chronic conditions were all orthopedic or were a combination of orthopedic and other medical diagnoses. All patients included did have two or more chronic conditions (chronic condition counts per patient ranged from 2 to 14) and therefore satisfied the inclusion criteria for the definition of multimorbidity in this review.30
Chronic conditions were used to define the population of interest in the studies by Fusco et al.,28 and Peng et al.29 In the studies by Fusco et al.,28 and Peng et al.,29 the inclusion criteria was broader with respect to disease diagnosis so the authors were able to capture a broader range of chronic conditions such as: cardiorespiratory, neurological, musculoskeletal, cancer, and diabetes. Peng et al.,29 did not exclude participants with only one chronic condition; however, the authors did consider multiple chronic conditions and how the number of chronic conditions influenced the outcome of goal setting and goal-attainment for both self-management and non-self-management goals. Fusco et al,28 categorized diseases as main diseases or associated diseases, which initially presents as comorbidity not multimorbidity. “Main diseases” and “associated diseases” are stratified based on their association to a rehabilitation program and not in fact index conditions. When considered in the final model, the authors used a simple disease count and the average number of diseases reported in this study was 2.4 (sd = 1.5).
Overall, none of the included studies explicitly defined multimorbidity, nor was multimorbidity explicitly the population of interest. Each study however, considered this population and reported on the effect of multiple chronic conditions on the outcome(s) of interest. These studies were included because they considered multiple chronic conditions in their analysis without explicitly labeling one condition as an index condition. These studies were included for final retention because they were the only studies that explicitly reported on multiple chronic conditions in the analysis and explored the association of chronic conditions on the respective outcome(s) of interest within the home care setting.
Description of outcomes measured
The primary outcome measured across three of the studies was function and/or functional changes following rehabilitation interventions.27,28,30 In two of these studies, function was conceptualized as performance of activities of daily living.28,30 One study extended function to include instrumental activities of daily living (IADLs), such as meal preparation, shopping, and finances for example.27 In the study by Kim et al.,30 function was defined as encompassing three key activities: toileting, ambulation and transfers.
The two retrospective cohort studies analyzed rehabilitation therapy data collected through the Resident Assessment Instrument for Home Care27,28 and one of the studies explored functional outcomes using the Outcome and Assessment Information Scale (OASIS).30 Both of these assessment instruments capture data on admission status, discharge status, functional status and demographics. Irrespective of how functional change was captured in each of these studies, the results indicated that functional improvement was seen after therapeutic intervention in two of the studies.27,30 The study by Fusco et al.28 had mixed results with respect to functional change wherein one third of participants improved functionally and the remaining participants stayed the same or worsened.28 Fusco et al.,28 found that the number of diseases was not a predictive factor in the functional recovery of the sample of older community-dwelling adults receiving home care. Similarly, in the study by Kim et al.,30 it was found that there was no relationship between comorbidities, physiotherapy visits, and the three functional outcomes (toileting, ambulation and transferring). Comorbidities was the term used in the article by Kim et al.30 to capture a simple chronic disease count wherein all patients had two or more co-occurring chronic conditions.
The outcome in the study by Peng et al.29 was the ability to set self-management goals, achievement of these goals and how demographic information influenced self-management goals for individuals with chronic conditions. Specifically, the authors explored self-management goals within the context of physical therapy treatment and how these were set and achieved. The authors found that demographic characteristics and quantity of chronic conditions did not influence the ability to set self-management goals. Furthermore, the authors found that the majority of self-management goals that were set, were met (89–100%).29
In addition to the functional outcomes measured in these studies, one study highlighted the association between rehabilitation therapy services and institutionalization among individuals with musculoskeletal conditions. The results showed that receiving therapy increased the probability of being discharged from home care (HR = 1.498, 95% CI = 1.447–1.550), reduced the risk of hospital admissions and/or long-term care admissions (HR = 0.926, 95% CI = 0.897–0.956) and reduced the risk of death (HR = 0.905, 95% CI = 0.851–0.964).27 The results also revealed that when considering the Charlson Crosswalk Comorbidity Index score, there was a lower probability of being discharged from home care (HR = 0.929, 95% CI = 0.919–0.939), higher risk of being discharged to hospital or long-term care (HR = 1.051, 95% CI = 1.042–1.059) and higher likelihood of death (HR = 1.226, 95% CI = 1.208–1.244).27
Discussion
This review offers an in-depth exploration of rehabilitation specific therapeutic interventions for individuals with multimorbidity within the home care setting. Multimorbidity is becoming increasingly recognized in the health care literature. As such, there is a growing interest in research aimed at understanding the impact of multimorbidity on individual health, the effectiveness of different interventions delivered by health care providers with different professional backgrounds, and the influence of these interventions on the health care system. The review highlights that there is currently a lack of research on home care rehabilitation services for people with multimorbidity. This review also supports two key messages within the multimorbidity literature: 1) there is ambiguity in the interpretation and application of the terms comorbidity and multimorbidity that transcends profession and care setting and, 2) regardless of the mode of rehabilitative intervention and how multimorbidity was interpreted and applied, functional improvements were measured and achieved within the home care rehabilitation literature.27–30
This review offers an important perspective on the effect of home care rehabilitation interventions for individuals with multimorbidity. Rehabilitation therapists are well positioned to provide interventions that impact daily function and activity engagement. The concept of care delivery to individuals with multiple chronic conditions is not new. Operationalizing rehabilitation interventions while considering the functional complexities associated with multimorbidity is a newer concept that is beginning to be explored within the primary care context and more loosely within the home care setting.21,22,32
In the existing multimorbidity literature wherein interventions are delivered in community and primary care settings, interventions were typically delivered by health care professionals other than rehabilitation therapists.22 The review by Smith et al.22 further highlighted two main types of interventions among individuals with multimorbidity: organizational interventions and patient-oriented interventions. Only one of the studies that emphasized patient-oriented interventions was delivered by rehabilitation therapists (occupational therapists and physical therapists).32 The remainder of the studies that focused on patient-oriented interventions were delivered by health educators, coaches, and/or volunteers. The outcomes however, focused broadly on activity engagement, mobility, activities of daily living, instrumental activities of daily living and health utilization.22 These outcomes are all areas in which rehabilitation therapists are trained to assess and intervene. It’s important to highlight that the only study that had a significantly positive outcome was the study where care was delivered by rehabilitation therapists.32 This presents an important area for future research.
The study by Gitlin et al,32 focused on occupational therapy and physical therapy interventions to improve functional outcomes, self-efficacy, and fear of falling among older adults with chronic conditions. Similar to our own findings, the therapeutic interventions in the study by Gitlin et al.,32 targeted environmental and behavioral contributors to functional decline and found similar positive results including less difficulty with activities of daily living and instrumental activities of daily living at the 6-month follow-up. This randomized controlled trial however delivered the therapeutic intervention to community-dwelling older adults who were not receiving occupational therapy or physical therapy and were experiencing difficulty with activities of daily living and instrumental activities of daily living.32 Furthermore, the study reported descriptive statistics on the percentage of participants with singular chronic conditions, but the authors do not explicitly report on the co-occurrence of these chronic conditions.32 This speaks further to the inconsistencies observed in the literature surrounding how multimorbidity is operationalized. A follow-up study by Gitlin et al.,33 evaluated 4-year mortality survivorship and the authors found that participants who received therapeutic intervention had a lower mortality rate for up to 3.5 years from study entry. This supports the positive effect of rehabilitation interventions for people with chronic conditions on health care outcomes.
Additionally, a recent study conducted in primary care, explored the development, implementation, and impact of self-management programs for people with multimorbidity.21 The outcomes measured in this study included activity engagement and participation, quality of life and self-efficacy. The results demonstrated a positive impact across all four domains.21 Self-management interventions delivered by trained occupational therapists and/or physical therapists are common in the literature for individuals with chronic conditions. This study demonstrated the effectiveness of self-management interventions in primary care.21 Therapeutic interventions have extended to include those with multimorbidity across the health care continuum, with positive results being observed in home care, community care and primary care settings.21,29 This sheds light on how primary care rehabilitation interventions among this population take a preventative approach through the use of self-management interventions whereas therapists in home care and community settings tend to focus on interventions when a loss of function and/or dysfunction limit engagement in activities of daily living. This presents an opportunity for future research to explore how collaborative rehabilitation service providers across the health care continuum enact their full scope of practice with shared clients.
Multimorbidity in the home care rehabilitation research included in this review was not explicitly defined as “multimorbid” however, the inclusion criteria of the included studies all satisfy the most common global definition of multimorbidity, which is the presence of two or more co-occurring chronic conditions.9 There is ambiguity in the literature surrounding the definition of multimorbidity and the methodologies used to identify this cohort; most commonly what chronic conditions are included in the definition and the number of chronic conditions required to qualify as being multimorbid.9 Because of this ambiguity, multimorbidity and the nuances of experiencing the broader health impact of multiple chronic conditions, oftentimes is camouflaged under other descriptors more common in the health literature such as: comorbid, frail or more broadly older adults.
Multimorbidity is not often explicitly used to identify the population of interest in rehabilitation research. This review highlighted that a large proportion of home care clients with multimorbidity in fact had multiple co-occurring musculoskeletal conditions. This finding suggests a lack of research on the role of rehabilitation providers in the management of multimorbidity that often includes a wider range of health conditions.27–30 Occupational therapists and physical therapists are experts in approaching service delivery from a biopsychosocial lens, whereby consideration is given to the functional impact of the cognitive, social, environmental, psychoemotional and physical complexities of multimorbidity.20,34,35 Additional research is needed to describe assessments, interventions and the impact of occupational therapists and physical therapists across the spectrum of chronic health conditions. Rehabilitation research on multimorbidity should also consider using consistent definitions for multimorbidity in a way that conceptualizes multimorbidity as more than multiple physical health conditions.13
Overall, this review revealed four broad gaps within the home care rehabilitation literature for individuals with multimorbidity, namely: 1) there is a dearth of evidence on rehabilitation for individuals with multimorbidity in home care, 2) the definition of multimorbidity is vague, 3) the results have limited generalizability beyond chronic conditions affecting the musculoskeletal system, and 4) the system level impact of rehabilitation interventions for individuals with multimorbidity across the health care continuum has yet to be fully realized (due to varying definitions of multimorbidity and the emphasis on musculoskeletal conditions in rehabilitation).
Limitations
A limitation of any rapid review is the risk of missing articles, especially given the time restrictions and additional limitations of this type of review.24 Furthermore, because only one author screens each database there is an increased risk of bias in article selection. This review aimed to mitigate that risk by using a two-author abstract review of 10% of the articles screened and had two authors review the quality of included studies. Articles may have been missed or excluded due to the ambiguity in the definition and broad and inconsistent use of the term “multimorbidity,” across the literature. Additionally, gray literature was not searched or included.
Conclusions
Multimorbidity continues to be ambiguous and inconsistently defined, which makes it difficult to compare and contrast the effect of a variety of interventions. Furthermore, the term multimorbidity is often used synonymously with other similar terms such as frailty and comorbidity. None of the included studies in this review explicitly define multimorbidity, rather the studies account for the cumulative effect of multimorbid conditions in their analysis on overall health and function.27–30 This review sheds light on the lack of home care rehabilitation services focused on the broader multimorbid population. Of the included studies, improvements were observed following therapeutic intervention across the four articles included in this review, which is consistent in the literature across sectors for multimorbid clients exposed to rehabilitation. Given the scope of both occupational therapists and physical therapists, research needs to extend beyond multimorbidity in the context of musculoskeletal conditions to include a wider range of healthcare conditions (such as neurological conditions, mental health conditions, and cardiorespiratory conditions) that encompasses the broader determinants of health (e.g., physical, psychosocial, and cognitive).32,36–40 The rehabilitation therapy professions are lagging with respect to defining and describing the breadth and depth of their respective practice scope with this population. This presents a significant opportunity to understand the broader impact of rehabilitation therapy interventions delivered to this population on health system use and unpack how that role changes across various health care sectors.
Acknowledgement
We would like to acknowledge Paola Durando, MLS for her assistance with search term development and refinement.
Footnotes
Author contributions: This review was conceptualized by AM. AM and CD were involved in article selection, retention and evaluation methods. AM took the lead in manuscript development and all authors were involved editing the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Amanda Mofina  https://orcid.org/0000-0002-9748-3816
https://orcid.org/0000-0002-9748-3816
References
- 1. Gilmour H. Unmet home care needs in Canada. Health Rep 2018; 29: 3–11. [PubMed] [Google Scholar]
- 2. Public Health Agency of Canada. How healthy are Canadians? A trend analysis of the health of Canadians from a healthy living and chronic disease perspective. Report, Ottawa, Canada, December 2016. [Google Scholar]
- 3. Nguyen H, Manolova G, Daskalopoulou C, et al. Prevalence of multimorbidity in community settings: a systematic review and meta-analysis of observational studies. J Comorb 2019; 9: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cesari M, Pérez-Zepeda MU, Marzetti E. Frailty and multimorbidity: different ways of thinking about geriatrics. J Am Med Dir Assoc 2017; 18: 361–364. [DOI] [PubMed] [Google Scholar]
- 5. Boyd CM, Fortin M. Future of multimorbidity research: How should understanding of multimorbidity inform health system design? Public Health Rev 2011; 32: 451–474. [Google Scholar]
- 6. Tonelli M, Wiebe N, Fortin M, et al. Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 2015; 15 DOI: 10.1186/s12911-015-0155-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Med Sci 2004; 59: 255–263. [DOI] [PubMed] [Google Scholar]
- 8. Koné Pefoyo AJ, Bronskill SE, Gruneir A, et al. The increasing burden and complexity of multimorbidity. BMC Public Health 2015; 15 DOI: 10.1186/s12889-015-1733-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fortin M, Stewart M, Poitras ME, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 2012; 10: 142–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nicholson K, Makovski TT, Griffith LE, et al. Multimorbidity and comorbidity revisited: refining the concepts for international health research. J Clin Epidemiol 2019; 105: 142–146. [DOI] [PubMed] [Google Scholar]
- 11. Feely A, Lix LM, Reimer K. Estimating multimorbidity prevalence with the Canadian chronic disease surveillance system. Heal Promot Chronic Dis Prev Canada 2017; 37: 215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nicholson K, Terry A, Fortin M, et al. Examining the prevalence and patterns of multimorbidity in Canadian primary healthcare: a methodologic protocol using a national electronic medical record database. J Comorb 2015; 5: 150–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnston MC, Crilly M, Black C, et al. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health 2019; 29: 182–189. [DOI] [PubMed] [Google Scholar]
- 14. Condelius A, Edberg AK, Jakobsson U, et al. Hospital admissions among people 65+ related to multimorbidity, municipal and outpatient care. Arch Gerontol Geriatr 2008; 46: 41–55. [DOI] [PubMed] [Google Scholar]
- 15. Friedman B, Jiang HJ, Elixhauser A, et al. Hospital inpatient costs for adults with multiple chronic conditions. Med Care Res Rev 2006; 63: 327–346. [DOI] [PubMed] [Google Scholar]
- 16. Mondor L, Maxwell CJ, Bronskill SE, et al. The relative impact of chronic conditions and multimorbidity on health-related quality of life in Ontario long-stay home care clients. Qual Life Res 2016; 25: 2619–2632. [DOI] [PubMed] [Google Scholar]
- 17. Mondor L, Maxwell CJ, Hogan DB, et al. Multimorbidity and healthcare utilization among home care clients with dementia in Ontario, Canada: A retrospective analysis of a population-based cohort. PLoS Med 2017; 14: e1002249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med 2002; 162: 2269–2276. [DOI] [PubMed] [Google Scholar]
- 19. Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 2011; 10: 430–439. [DOI] [PubMed] [Google Scholar]
- 20. World Health Organization. Towards a common language for functioning, disability and health: ICF Report, Geneva, Switzerland, 2002. [Google Scholar]
- 21. Garvey J, Connolly D, Boland F, et al. OPTIMAL, an occupational therapy led self-management support programme for people with multimorbidity in primary care: a randomized controlled trial. BMC Fam Pract 2015; 16 DOI: 10.1186/s12875-015-0267-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith SM, Soubhi H, Fortin M, et al. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012; 345: e5205 DOI: 10.1136/bmj.e5205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Onwuegbuzie AJ, Frels R. 7 steps to a comprehensive literature review: a multimodal & cultural approach. Los Angeles: SAGE Publications, Ltd, 2016, pp. 26–27. [Google Scholar]
- 24. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009; 26: 91–108. [DOI] [PubMed] [Google Scholar]
- 25. Government of Ontario. Preventing and managing chronic disease: Ontario’s framework Report, Ontario Canada, May 2007. [Google Scholar]
- 26. Joanna Briggs Institute. Checklist for cohort studies, The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews, 2017. [Google Scholar]
- 27. Cook RJ, Berg K, Lee K, et al. Rehabilitation in home care is associated with functional improvement and preferred discharge. Arch Phys Med Rehabil 2013; 94: 1038–1047. [DOI] [PubMed] [Google Scholar]
- 28. Fusco D, Bochicchio GB, Onder G, et al. Predictors of rehabilitation outcome among frail elderly patients living in the community. J Am Med Dir Assoc 2009; 10: 335–341. [DOI] [PubMed] [Google Scholar]
- 29. Peng K, Bourret D, Khan U, et al. Self-management goal setting: Identifying the practice patterns of community-based physical therapists. Physiother Canada 2014; 66: 160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kim TA, Gordes KL, Alon G. Utilization of physical therapy in home health care under the prospective payment system. J Geriatr Phys Ther 2010; 33: 2–9. [PubMed] [Google Scholar]
- 31. Huntley AL, Johnson R, Purdy S, et al. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med 2012; 10: 134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gitlin LN, Winter L, Dennis MP, et al. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc 2006; 54: 809–816. [DOI] [PubMed] [Google Scholar]
- 33. Gitlin LN, Hauck WW, Dennis MP, et al. Long-term effect on mortality of a home intervention that reduces functional difficulties in older adults: results from a randomized trial. J Am Geriatr Soc 2009; 57: 476–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Roush SE, Sharby N. Disability reconsidered: the paradox of physical therapy. Phys Ther 2011; 91: 1715–1727. [DOI] [PubMed] [Google Scholar]
- 35. Gentry K, Snyder K, Barstow B, et al. The biopsychosocial model: application to occupational therapy practice Open J Occup Ther 2018; 6 DOI: 10.15453/2168-6408.1412. [Google Scholar]
- 36. Pimouguet C, Le Goff M, Wittwer J, et al. Benefits of occupational therapy in dementia patients: findings from a real-world observational study. J Alzheimers Dis 2017; 56: 509–517. [DOI] [PubMed] [Google Scholar]
- 37. Bennett S, Laver K, Voigt-Radloff S, et al. Occupational therapy for people with dementia and their family carers provided at home: a systematic review and meta-analysis. BMJ Open 2019; 9 DOI: 10.1136/bmjopen-2018-026308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Graff MJL, Adang EMM, Vernooij-Dassen MJM, et al. Community occupational therapy for older patients with dementia and their care givers: cost effectiveness study. BMJ 2008; 336: 134–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011; 377: 1693–1702. [DOI] [PubMed] [Google Scholar]
- 40. Canadian Home Care Association. Rehabilitation therapy services in home care. Report, Mississauga, Canada, September 2011. [Google Scholar]