Abstract
Employment is a social determinant of health that is important for understanding health behaviors, health outcomes and HIV transmission among people living with HIV. This study is a scoping review of the literature that addresses (a) the relationship between employment and the HIV continuum of care, (b) determinants of employment among PLWH and (c) experiences with employment. We searched two databases, PubMed and Embase, and identified a total of 5622 articles that were subjected to title and abstract review. Of these, 5387 were excluded, leaving 235 articles for full-text review. A total of 66 articles met inclusion criteria and were included in the study. The literature suggests that employment status is positively associated with HIV testing, linkage to HIV care, retention in HIV care, and HIV medication adherence. Guided by a social-ecological framework, we identified determinants of employment at the individual, interpersonal, organizational, community, and policy levels that are amenable to public health intervention. Experiences with employment, including barriers, facilitators, advantages, disadvantages, and needs, provide additional insight for future research and programs.
Keywords: Employment, Return-to-work, HIV continuum of care, Social determinants of health
Introduction
There is increased recognition of the role social determinants of health play in shaping health behavior and disease transmission. The National HIV AIDS Strategy calls for comprehensive care for people living with HIV (PLWH) that includes supportive services for employment [1]. Once considered a terminal illness, with the advent of antiretroviral therapy (ART), and enhancements in contemporary ART, HIV is now considered a chronic disease [2]. People living with HIV who have a timely diagnosis, access to medication, and sustained life-long HIV medication adherence are expected to live nearly as long as the general population [3]. Given that the majority of PLWH are of working age—91% of PLWH are between the ages of 20–65 [4]—unemployment and job loss related to HIV will likely play a critical role in the social well-being and health of people living with HIV over the life course.
The purpose of this scoping review is to assess the state of the science on the relationship between employment and HIV. There are several literature reviews which focus on employment among PLWH that are relevant to our study. A scoping review synthesized the literature on labor force participation among PLWH through 2008 with a focus on the meaning of work, key factors that influence labor force participation, factors effecting vulnerable populations, risks and benefits of work, and strategies to support returning to work. The review identified a number of barriers to labor force participant and highlighted the need for future research on the long-term impact of HIV on employment, women, and long-term employment outcomes [5]. An earlier review explored the state of employment in the decade following the release of combination ART in the late 1990′s, with a focus on employment related needs, barriers to returning to work, and return-to-work programs. The review identified barriers related to mental health, physical health, identity, training and education [6]. Our study aims to update these reviews by including the literature though 2017. A recent, informative critical review of the literature identified employment needs and challenges among populations disproportionately impacted by HIV, the relationship between employment and important health outcomes associated with the HIV Care Continuum, and implications for policy, service provision, and future research. This critical review didn’t use a systematic methodology characteristic of systematic reviews or scoping reviews. The review identified the need for research on the causal mechanisms through which employment impacts health and the impact of employment health services on health outcomes [7]. Two additional reviews asked narrow questions related to employment among PLWH. A 2015 Cochrane Systematic Review evaluated the effect of interventions aimed at sustaining and improving employment among PLWH. The review identified four studies that met their inclusion criteria and found low-quality evidence that ART interventions may improve employment outcomes for PLWH [8]. Finally, a 2015 review focused on the role of employment on neurocognitive reserve among adults with a focus on the role of social engagement, learning new skills, established routines, life purpose, and income. This review concluded that there is a need for research to examine the neurocognitive impacts of returning to work [9].
Our study builds off of the work outlined above and addresses some of the existing gaps in the literature. The aim of our study is to identify determinants related to employment among PLWH which are potentially amendable to public health intervention to inform intervention development. Specifically, our review uses a scoping methodology to synthesize the literature in following areas: (a) the relationship between employment and movement along the HIV continuum of care, (b) determinants of employment among PLWH across the multiple levels outlined by the social-ecological model, and (c) experiences with employment (including barriers, facilitators, advantages, disadvantages, and needs). Our review adds to the literature by up-dating the findings of the reviews completed by Braveman and Worthington through 2017, using a reproducible scoping methodology to assess the relationship between employment and the HIV continuum of care, and using the social-ecological model to frame determinants of employment identified through the literature.
Methods
In conducting this scoping review, we adhered to the methodological guidelines outlined by Levac [10] and Colquhoun [11]. These guidelines further clarify and refine the six steps for conducting scoping reviews outlined by Arksey and O’Malley 2005: (1) identifying the research question, (2) identifying relevant studies, (3) study selection, (4) charting the data, (5) collating, summarizing, and reporting the results, and (6) consultation [12]. The objective of this review was to develop a better understanding of the current landscape of the literature on employment among people living with HIV with an aim to identify gaps in the literature and provide recommendations for future areas of research, focusing upon public health intervention development.
This scoping review was conducted by three individuals: two researchers from the Johns Hopkins School of Public Health and an informationist from the Welch Medical Library. In conjunction with the study team, the informationist developed the search strategy which was translated and executed in PubMed and Embase (Table 1). We used the following selection criteria: (a) full-text studies, (b) published in the peer-review literature, (c) written in English, (d) published between 1999 and 2017, (e) all study designs, and (f) focus on HIV and employment.
Table 1.
Search terms
| Database | Concept | Search terms |
|---|---|---|
| Pubmed | Concept # 1 | Employment[mesh] OR Return to work[mesh] OR Vocational guidance[mesh] OR Employment, Supported[mesh] OR Job Application[mesh] OR Work[mesh] OR Rehabilitation, Vocational[mesh] OR Occupational Status[tiab] OR Underemployment[tiab] OR back to work[tiab] OR return to work[tiab] OR vocational education[tiab] OR Career Counseling[tiab] OR Vocational Guidance[tiab] OR Vocational Training[tiab] OR vocational education[tiab] OR supported employment[tiab] OR Job Application*[tiab] OR Employment Application*[tiab] OR Vocational Rehabilitation*[tiab] OR workforce re-entry[tiab] OR returning to work[tiab] OR job seeking[tiab] OR vocational counseling[tiab] OR job training[tiab] OR job skill*[tiab] OR job readiness[tiab] OR career oriented[tiab] OR unemployment[tiab] |
| Concept # 2 | HIV[mesh] OR Human Immunodeficiency Virus*[tiab] OR AIDS Virus*[tiab] OR HIV[tiab] | |
| Concept # 1 and # 2 | 1934 | |
| Embase | Concept # 1 | ‘employment’/exp OR ‘supported employment’/exp OR ‘employment status’/exp OR ‘vocational guidance’/exp OR ‘return to work’/exp OR ‘job finding’/exp OR ‘work’/exp OR ‘vocational rehabilitation’/exp OR ‘underemployment’/exp OR ‘professional counseling’:ab,ti,kw OR ‘vocation guidance’:ab,ti,kw OR ‘vocational counseling’:ab,ti,kw OR ‘vocational service*’:ab,ti,kw OR ‘employment application’:ab,ti,kw OR ‘job application*’:ab,ti,kw OR ‘job finding’:ab,ti,kw OR ‘occupational rehabilitation’:ab,ti,kw OR ‘vocational rehabilitation’:ab,ti,kw OR ‘vocational retraining’:ab,ti,kw OR ‘Occupational Status’:ab,ti,kw OR ‘Underemployment’:ab,ti,kw OR ‘back to work’:ab,ti,kw OR ‘return to work’:ab,ti,kw OR ‘vocational education’:ab,ti,kw OR ‘Career Counseling’:ab,ti,kw OR ‘Vocational Guidance’:ab,ti,kw OR ‘Vocational Training’:ab,ti,kw OR ‘vocational education’:ab,ti,kw OR ‘supported employment’:ab,ti,kw OR ‘Job Application*’:ab,ti,kw OR ‘Employment Application*’:ab,ti,kw OR ‘Vocational Rehabilitation*’:ab,ti,kw OR ‘workforce re-entry’:ab,ti,kw OR ‘returning to work’:ab,ti,kw OR ‘job seeking’:ab,ti,kw OR ‘vocational counseling’:ab,ti,kw OR ‘job training’:ab,ti,kw OR ‘job skill*’:ab,ti,kw OR ‘job readiness’:ab,ti,kw OR ‘career oriented’:ab,ti,kw OR ‘unemployment’:ab,ti,kw |
| Concept # 2 | ‘Human Immunodeficiency Virus’/exp OR ‘AIDS Virus*’:ab,ti,kw OR ‘HIV’:ab,ti,kw OR ‘Human immuno deficiency virus’:ab,ti,kw OR ‘immunodeficiency associated virus*’:ab,ti,kw | |
| Concept # 1 and Concept # 2 | 4831 |
We first conducted a title and abstract screen and excluded articles that did not focus on HIV and employment and were therefore not relevant to our study. We then examined the full text of the remaining articles for compliance with selection criteria. Next, we categorized the existing literature into the following topic areas: (a) the relationship between employment and the HIV continuum care; (b) determinants of employment among PLWH; (c) barriers and facilitators of employment; and (d) the employment-related experiences of PLWH. We used these categories to answer three overarching research questions: “What is the relationship between employment and movement along the HIV continuum of care?”; “What are the determinants of employment among PLWH?”; and “What is known about the employment-related experiences of PLWH?” Because we were interested in findings that were most relevant to the social context of the United States, at this stage, we revised our search criteria to include only studies conducted within the United States, Western Europe, and Canada. We included findings from one systematic review of studies in low, middle and high income countries but only reported the findings from high income countries (United States, France, and the United Kingdom) as well as one study that included the member states of the Organization for Economic Cooperation and Development. We excluded studies that where conducted in Europe but had a focus on recent migrants. We excluded studies with only abstracts available. Finally, we excluded intervention research studies (including studies of interventions, programs, models and frameworks related to employment and vocational services). We excluded these studies because the authors felt that intervention studies (and related topics) warrant a separate, standalone review to present the findings in detail and to provide thorough, robust recommendations.
To organize and manage the data, we extracted information on the study characteristics as well as the main study findings. Specifically, we extracted information on first author and year of publication, study location, study population, sample size, sampling strategy, study design, and key findings into tables. In addition, we charted the data on determinants of employment to organize our findings visually and to categorize our findings by the levels of the Social-Ecological Model. We used the Social-Ecological Model as our guiding framework [13], and categorized our findings as being either at the individual, inter-personal, organizational, community, or policy level. The Social-Ecological Model recognizes that multiple layers of embedded factors operate across and between levels to influence behavior [13].
Our initial study questions and preliminary findings were presented to a community advisory board for feedback and input. The community advisory board provided recommendations and suggestions on which findings were most meaningful to them and provided suggestions for how the findings could be framed and presented. The community advisory board was comprised of individuals living with and impacted by HIV and included students, current and former HIV peer navigators at a local clinic, community advocates, community leaders, and individuals who work in HIV prevention intervention development and implementation.
Results
Our search yielded 6765 results (1934 from Pubmed and 4831 from Embase) with 1143 duplicates, resulting 5622 articles that were subjected to title and abstract review. Of those, 5387 were excluded, leaving 235 articled for full-text review. One hundred and sixty-nine articles were excluded after full-text review. Fifty-seven articles were excluded due to location (e.g. not in United States, Western Europe, or Canada), 80 due to relevance of the topic area (e.g. focus are was not HIV and employment), 17 due to publication type (e.g. only abstract available or conference abstract), and 15 due to the study population (e.g. study population not people living with HIV). The remaining 66 articles were included in the scoping review (Fig. 1).
Fig. 1.
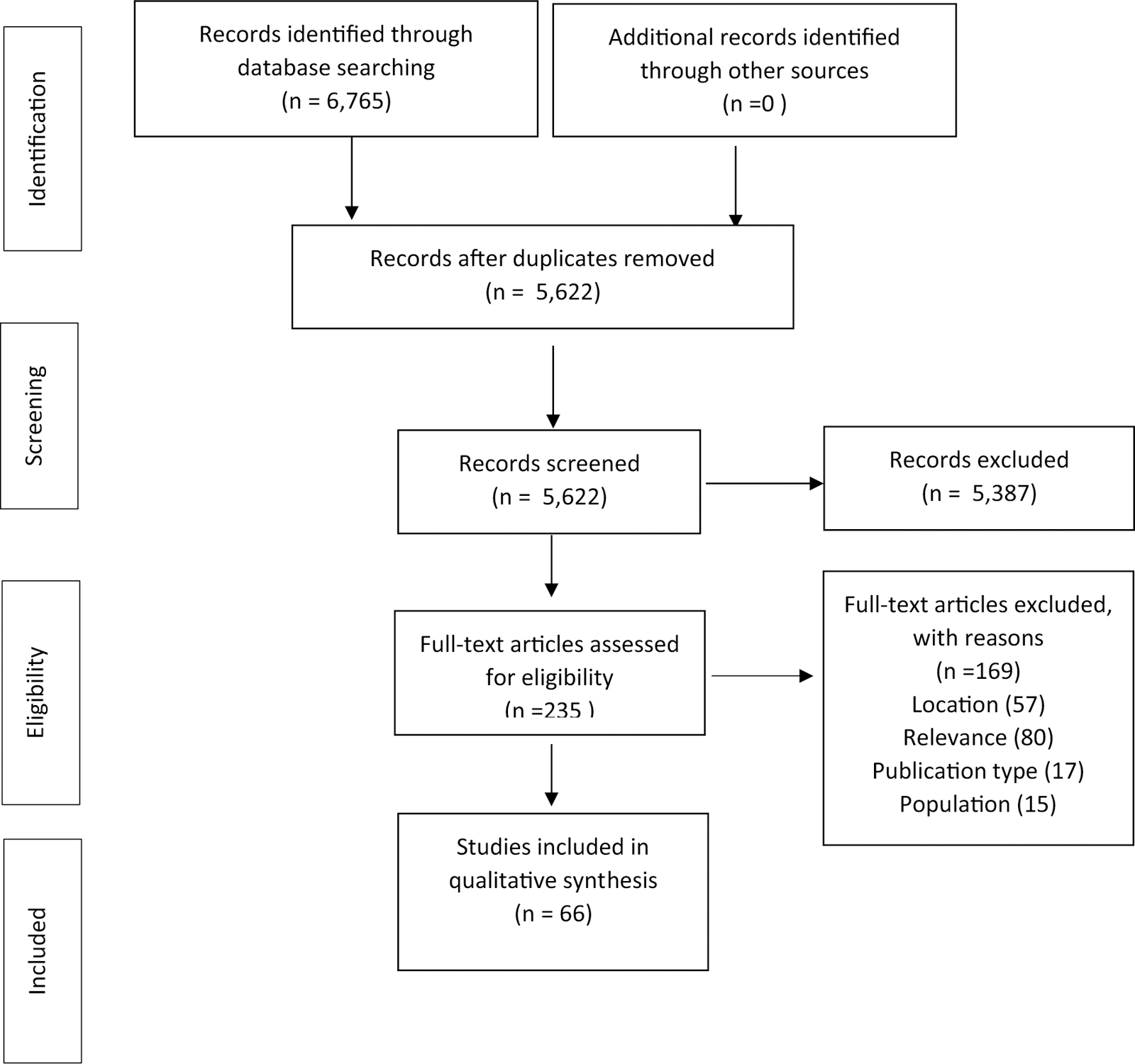
Flow diagram of study selection
Employment Status and the HIV Continuum of Care
The literature suggests that employment status is associated with movement along the HIV continuum of care (Table 2). Not being employed is associated with not being tested for HIV [14] and with late diagnosis [15–17]. Research among individuals in the Southern United States found that PLWH who are unemployed are two times more likely to miss their initial scheduled HIV medical visit compared to individuals who were employed [18]. Similarly, a cohort study in Philadelphia of patients at hospital-affiliated outpatient clinics, emergency departments, and inpatient units found that unemployed patients were 6.5 times more likely to fail to link to care within 6 months of receiving a HIV positive test result [19], while a study in Italy found that unemployed people living with HIV were 2.75 times more likely to fail to present for HIV care within 6 months of diagnosis [20]. Research has also found associations between unemployment and delayed access to highly active antiretroviral therapy [21]. A recent systematic review of 28 studies from low, middle, and high income countries found that employment was associated with HIV medication adherence (OR 1.33, 95% CI 1.02–1.74) in high-income geographies [22]. In neighborhoods with higher rates of unemployment, PLWH are less likely to have current antiretroviral prescriptions [23]. Employment characteristics may modify the relationship between employment and adherence. Among employed individuals, those who have workplace accommodations are more likely to be adherent to HIV medications than those without an accommodation [24]. Employment loss is associated with both incident and persistent elevated viral load [25].
Table 2.
The relationship between employment and continuum of care outcomes
| Author, year | Location | Study design | Sample (N) | Sampling strategy | Employment measure | Continuum of care measure | Main finding |
|---|---|---|---|---|---|---|---|
| Diagnosis | |||||||
| Delpierre, 2006 | France | Prospective multicenter cohort | Patients from 6 hospitals from 1996–2005 (N = 5702) | Non-probability sample of all patients who sought care from 6 hospitals | Employment status: stable employment, on employment benefits, unemployed or other | Late testing: presenting with symptoms of AIDS or CD4 < 200 mm3 during the year of diagnosis | Among MSM, unemployment associated with late testing (OR = 2.23, 95% CI 1.14–4.36); among women and heterosexuals employment status not associated with late testing |
| Massari, 2011 | France | Prospective cohort | General population living in the Paris metropolitan area, SIRS Cohort (N = 3023) | Multistage, random sample | Employment status: employed, unemployed and inactive, which includes retired or student | HIV testing: Never having been tested for HIV | Among women, unemployment was associated with no history of HIV testing (OR 1.85, 95% CI 1.24–2.77). Among men, a significant association was not observed |
| D’Arminio, 2011 | Italy | Observational Cohort Study | Antiretroviral-naïve patients with a recent HIV diagnosis and CDC + T-cell count (N = 2276) | All patients enrolled in the Icona Foundation Study who met eligibility criteria from 1997 to 2009 | Employment status: becoming unemployed, as opposed to retiring | Late diagnosis: patients presenting with symptoms of AIDS or CD4 T-cell count less than or equal to 350/mm3 | Unemployment (in comparison to retirement) was associated with late diagnosis (OR = 0.36, 95% CI 0.21–0.61) |
| Sheehan, 2017 | Florida, USA | Surveillance study | Florida Department of Health Enhanced HIV/AIDS Reporting System and American Community Survey (eHARS)(N = 5522) | Reported surveillance cases between 2007 and 2011 | Neighborhood employment level: the percent of the population who is 16 of older and are unemployed | Late diagnosis: receiving an AIDS diagnosis within 3 months of receiving their HIV diagnosis | Among Latino men, neighborhood unemployment strata were associated with late testing. By 2nd, 3rd, and 4th strata of unemployment, ORs (95% CIs): 1.37 (1.06–1.78), 1.29 (1.01–1.66), 1.33 (1.03–1.72) |
| Linkage to HIV Care | |||||||
| Girardi, 2004 | Italy | Multi-center cohort | Individuals living with HIV over the age of 18 (n = 4453) | Antiretroviral-naïve patients enrolled from 59 clinical centers from 1997 to 2000 | Employment status, coded as stable employment, unemployed, or other | Delayed presentation: greater than 6 months from positive test result to presenting for HIV medical care | Unemployment associated with delayed presentation to care (OR = 2.75, 95% CI 1.66–4.53) |
| Aaron, 2015 | Philadelphia, USA | Retrospective cohort | Individuals with an HIV positive diagnosis who attended a large urban healthcare center (n = 87) | Medical records were used to ascertain HIV positive diagnoses in inpatient and outpatient settings from 2007 to 2011 | Employment status: dichotomous variable, where either employed or unemployed | Linkage to care: one visit to an HIV medical provider within 6 months of receiving a positive test result | Unemployment was associated with failure to link to care (OR = 6.50, 95% CI 1.13–37.32) |
| Nijhawan, 2017 | Texas, USA | Retrospective chart review | Individuals who were scheduled for a new patient visit after January 1st, 2014 from two clinics (n = 200; 100 per clinic) | Consecutive sample of patient records from 2014–2016 | Employment status, coded as employed, unemployed, or disabled | Linkage to care: missing vs. attending the first scheduled medical visit | Unemployment was associated with missing the first scheduled appointment. (OR = 2.33, 95% CI 1.04–5.24) |
| Retention in HIV care | |||||||
| Joy, 2008 | British Columbia, Canada | Prospective cohort | Treatment-naïve patients accessing HAART between September 1, 1997 and November 30, 2004 (n = 2168) | Enrollment in provincial drug treatment program (the only method by which patients can access HAART in British Columbia) | Neighborhood measurement of percentage of unemployed individuals | Delayed access to treatment: not accessing treatment until patient’s CD4 count was low (< 50 cells/mm) | Unemployment was associated with delayed access to treatment (OR = 1.41, 95% CI 1.14–1.74) |
| Shacham, 2013 | St Louis, USA | Cross-sectional study | All patients who attended the Washington University HIV clinic in 2008 (n = 762) | All patients who attended the Washington University HIV clinic in 2008 were required to complete a behavioral survey as a part of their medical visit. Data was gathered from these surveys | Employment level, measured as a neighborhood-level variable | Receipt of ART prescription:, use of at least three drugs from two different antiretroviral drug classes or the use of at least three nucleoside reverse transcriptase inhibitors | Neighbourhoods with higher rates of unemployment had individuals who were less likely to have a current ART prescription (OR = 1.47, 95% CI 1.05–2.04) |
| HIV medication adherence | |||||||
| Torres-Madriz, 2011 | Boston, USA | Randomized, crossover trial | Patients on ART with a detectable viral load in the greater Boston area (n = 156) | Convenience sample of patients from five patient care settings | Work accommodations dichotomized as any or none | ART adherence: percentage of doses taken correctly during the 30 days prior to each study visit | Patients with accommodations had a 12% higher mean adherence than those without accommodations (Parameter estimate 0.12, 95% CI 0.03–0.20) |
| Nachega, 2015 | N/A – previously conducted trials were used | Meta-analysis | 28 articles meeting all criteria were included. This yielded information on 8743 individuals from 14 different countries | Records were identified from Medline, Embase, and Cochrane Central Register of Controlled Trials | Employment was globally assessed across all the included studies | Adherence was globally assessed across all the included studies | In low and high-income countries, being employed was favorably linked to adherence. Low: (OR = 1.85, 95% CI 1.58–2.18);Middle: (OR = 0.94, 95% CI 0.62–1.42); High: (OR = 1.33, 95% CI 1.02–1.74) |
| Viral load | |||||||
| Dray-Spira, 2005 | France | Prospective cohort study | Patients from 66 hospitals across France, enrolled between 1996 and 2002 (n = 319) | Convenience sample of patients recruited through hospitals who were recently diagnosed and ARV-naïve | Employment loss: change from employment to inactivity between two semi-annual visits | High viral load: greater than 10,000 copies/mm3 | Both persistent and incident high viral loads were associated with employment loss. Respectively, (OR = 2.4, 95% CI 1.1–5.0); (OR = 3.7, 95% CI 1.0–13.9) |
Determinants of Employment
Various studies have assessed determinants of employment among people living with HIV. This is important for identifying the populations that are most heavily impacted and for understanding possible mechanisms, in particular those which might be amenable to public health interventions. Studies suggest that demographic, biologic, and social factors are associated employment status among PLWH.
Employment
A variety of factors predict employment among PLWH including social demographic characteristics, health status, attitudes and beliefs. Several studies suggest that younger individuals are more likely to be employed than older individuals [26–28]. However, a study in France of individuals who had maintained employment since their HIV diagnosis found that individuals between the ages of 20–49 were more likely to maintain employment than those less than 20 years of age [29]. Research also suggests that those with a college degree are more likely to be employed than those with less education [29–32], and that men are more likely to be employed than women [29, 31, 33].
Studies that assessed the association between health and employment among PLWH have consistently found that those with greater physical and psychiatric health challenges are less likely to be employed. Individuals with AIDS [26, 30, 31], low CD4 cell counts [28, 31] and poor physical health [29, 33] are less likely to be employed. Higher memory function and executive functioning are associated with employment [26, 34] as are higher scores for quality of life [27, 35]. Employment is also associated with greater physical, role, social, conative, and mental health functioning, well-being, and quality of life [28, 36–44]. In addition, individuals with current or past addiction and HCV co-infection are less likely to be employed [30, 31]. There is a consistent inverse association between depression and employment [27, 31, 34].
However, it is important to note that these relationships may differ by quality of employment. Individuals with poor quality jobs (high job insecurity, high psychological demands, and low decision authority) report similar levels of quality of life and depressive symptoms as those who are unemployed [41, 45]. Likewise, among those who are employed, the type of employment matters. Individuals living with HIV with nonpermanent employment are at increased risk of death compared those with stable employment [46].
Individuals who are working at the time of diagnosis are more likely to be employed, [27] and research suggests that as more time passes from initial diagnosis, the less likely it is that an individual will be employed [26, 27, 31].
Considering Work
We identified three studies that assessed predictors of returning to work. Individuals who were male, younger and Hispanic/Latino (compared to White) were more likely to contemplate returning to work [30, 47]. Health status also seems to play an important role. Individuals with AIDS were less likely to consider returning to work compared to those in HIV stage A or B [30], while those who felt their health had improved over the past year were more likely to consider employment [47]. Fear of a loss of benefits appears to influence individuals thinking about returning to work. Individuals with disability benefits are less likely to initiate employment [30] as were individuals with Medicaid [47]. Two belief systems emerged as being positively associated with considering returning to work. The belief that health will improve with employment and the absence of work-related health concerns are both associated with initiating employment [47, 48].
Unemployment
Studies that modeled associations with unemployment mirror many of the trends seen in studies that assessed employment as an outcome. Individuals with more advanced HIV and those with higher viral loads [25] were more likely to be unemployed [49–52]. Frailty [50], diabetes [49], hypertension [49], psychological distress [53], and a poor self-report of health [53, 54] were also associated with unemployment. Unemployment is independently associated with depression [45, 55–57] as well as suicide and attempted suicide [56]. Finally, there is an association between unemployment and HIV mortality [52, 58–61].
Higher levels of education have been found to be protective against unemployment [50, 57] as well as job type. Individuals with managerial public-sector permanent positions are less likely to be unemployed than those with permanent private-sector jobs, casual/temporary contract jobs, or the self-employed [49, 62]. Furthermore, individuals with nonpermanent jobs are a greater risk of job loss following HIV diagnosis [25]. One study found a relationship between workplace discrimination and unemployment among individuals with primary education [49]. The relationship between age and unemployment varies across studies and is likely highly dependent on location and context. While some research indicates lower rates of unemployment among older individuals [50] others suggest higher rates of unemployment among older individuals [53, 57]. An additional study found that unemployment was lowest among those age 30–39 and higher among those 18–29 and 50–59 [49]. Women are more likely to experience job loss following HIV diagnosis than men [25].
Experiences with Employment
A body of literature documents the experiences of PLWH and employment. In this manuscript we have organized this literature into the following sub-headings: barriers to employment, facilitators of employment, advantages and disadvantages of employment and gaps or needs. These categories have been grouped together for the purpose of organization, rather than to make artificial distinctions between often overlapping and related concepts.
Barriers
Across studies several barriers to employment emerged. Health related concerns constituted a significant barrier to employment for PLWH, including the physical symptoms of HIV and the side effect of HIV medications [63–67]. Closely related was the burden of rigorous HIV regimes and the need for frequent medical visits [64, 65, 68]. For many, these barriers (HIV related illness, side-effects of medication, burden of HIV regimes, and frequent medical visits) necessitated the need for accommodations. A study of the process of workforce re-entry found that physical health challenges constituted the most widely experienced barrier to employment (reported by 60.6% of participants) followed by mental health challenges (reported by 47.1% of participants) [69].
Across studies, PLWH reported that fewer job options were available to them after their diagnosis. The reasons for this were varied and included: outdated job skills because of long absences from employment [29, 63, 64]; the perception that some jobs were no longer suitable (for example due to physical constrains or the nature of HIV transmission) [65]; and a lack of jobs that would be able to accommodate needs of PLWH [29, 64, 70].
Fear of discrimination in the workplace was a common barrier. HIV discrimination was mentioned across several studies [29, 64–68, 70–72] as well was racism, ageism, and homophobia [63, 66]. Fears were derived from personal experiences at prior jobs, as well as the perception that HIV discrimination was prevalent. A study of health care workers living with HIV found that individuals choose not to disclose their HIV status at work because of fears about negative reactions and because disclosure is unnecessary and a nonissue [73]. Individuals with professional or managerial jobs maybe more likely to disclose their HIV status at their place of employment than those with lower level positions [74]. A study in France found that 70% of employed participants had not disclosed their HIV status in the workplace and that among those who had told their supervisors of their HIV status, 22% had received accommodations. (By means of comparison, 9% of individuals who had not disclosed received accommodations.) [29].
The final cross-cutting barrier that emerged across studies was the fear of loss of benefits, including SSI, SSDI and health insurance [63–65, 67, 68, 70, 71]. Individuals receiving government assistance have reported being overwhelmed and intimidated by the paperwork and complex procedures associated with returning to work [67].
Facilitators
Research suggests that the work environment, work schedules, and social support are three factors that facilitate employment among PLWH. Having a safe and supportive work environment that includes supervisors and co-workers who are educated about HIV and who are perceived as approachable and open to accommodations facilitates employment [63, 64, 67, 68, 72]. An important aspect of a supportive work environment is flexibility in work schedules to accommodate health needs [67, 68, 72]. A study conducted in the United States found that about half of PLWH who work have a job accommodation and that part-time employees use job accommodations more frequently that full-time employees [74]. Finally, social support from physicians, friends and family support returning to work and maintaining employment [65, 68, 70–72, 75].
Advantages and Disadvantages
Advantages to employment include material advantages, social advantages and improvements in self-concept. Material advantages are achieved through increased access to financial resources which may facilitate increased financial stability and increased financial responsibility [63, 65, 68, 70–72, 76]. With increased financial resources, individuals reported a greater sense of freedom, increased ability to provide for others, and decreased reliance on public assistance [65, 68, 70–72]. Research also suggests that employment increases social connection, social skills building, and social engagement [63, 66, 68, 70–72, 76, 77]. Finally studies have found that employment increases individuals’ self-concept, including self-worth, self-esteem, self-respect and self-dignity [63, 65, 66, 68, 70, 71, 77]. Employed individuals reported increased satisfaction, fulfillment, and improved emotional and mental health [65, 66, 72, 77]. Employment provided welcome structure and routine which helped to fill an excesses of spare time [63, 64]. Finally, research suggests that employment may prevent negative neuroplasticity and facility neurocognitive reserve [9].
Research with unemployed individuals suggests that perceived disadvantages of employment include increased threat of exposure to HIV discrimination, potential complications with adhering to complex medication regimens, and increased stress [64, 70, 71]. A study of individuals employed at an HIV service provider found high levels of burnout among employees living with HIV due to a personal and professional focus on HIV as well as decreased access to health care and social services due role conflict felt by individuals who were providers and consumers of services [76].
Needs
Employment needs and unmet gaps in services for people living with HIV include skills building in job seeking and job training [65, 66, 70, 71]. Job seeking skills are the skills one uses to identify and apply for a job, such as accessing job resources, creating a resume, completing a job application, following up with a potential employer after an interview and interview skills. In particular, research suggests that some people living with HIV would like training and assistance on how to best answer questions about gaps in their resumes [70]. Research has also identified the need for further job training due to out of date job skills or the desire to gain training in a field that better matches the needs of someone living with a chronic disease [65, 70, 71]. Furthermore, research suggests that there is need to provide education and training on requesting accommodations [65, 71]. A study of 235 PLWH entering a vocational rehabilitation program found that the most frequently reported need was support with their work situation (80%) followed by education and training (78%) and finances (78%). Approximately a third of participants reported the need for housing, 16% reported the need for medical care and 12% reported drug and alcohol problems suggesting that return-to-work programs may need to address a range of competing psychosocial needs [78]. Research has also identified the need for support that provides an individualized and incremental approach to returning to work that leverages the benefits of social and peer support [77].
Discussion
Our study found that employment status is associated with movement along the HIV continuum of care. Specifically, PLWH who are employed are more likely to engage in HIV medical care, including HIV testing, timely linkage to HIV care, retention in HIV care, and HIV medication adherence. This finding is consistent with a critical review published by Conyers et al. which concluded that there is evidence to support a direct relationship between employment and HIV prevention outcomes [7]. These findings suggest that employment might play a role in reducing HIV transmission. Associations between employment and health, including continuum of care outcomes, are most likely bidirectional. For example, the health benefits of adhering to HIV medications likely facilitates employment. In addition, research among PLWH (as well as the general adult population) has found that working decreases depression, a known barrier to HIV medication adherence [27, 31, 34, 79], which suggests health benefits of working. A systematic review on the association of returning to work with improved health among working-aged adults found evidence of health selection (e.g. poor health interfering with people’s ability to return to work) as well as a beneficial effect of employment on health (e.g. a significant improvement in health after re-employment) [79].
Information on factors associated with employment and a rich understanding of employment barriers, facilitators, and unmet needs gives insight into areas that are amenable to public health intervention. We used information gathered by this literature review on determinants of employment as well as the employment experiences of people living with HIV to construct Fig. 2. Figure 2 depicts factors associated with employment across various levels of the Social-Ecological Model. Starting with the outermost oval, the policy level includes the nature and structure of local, state, and federal policies and programs such as SSI/SSDI. The community level includes access, availability, and quality of education, jobs, and employment-related services, such as vocational services programs. At the organizational level, characteristics of the work environment, such as presence or absence of HIV stigma/discrimination, availability of accommodations for individuals with a disability, and flexibility of work schedule, impact employment among PLWH. At the interpersonal level, social support and communication with family, friends, health care providers, and past/present supervisors influence employment prospects. Finally, at the individual level, a complex mix of factors related to demographics, health, employment and education history, personal knowledge, attitudes and beliefs and competing priorities appear to be associated with employment outcomes.
Fig. 2.
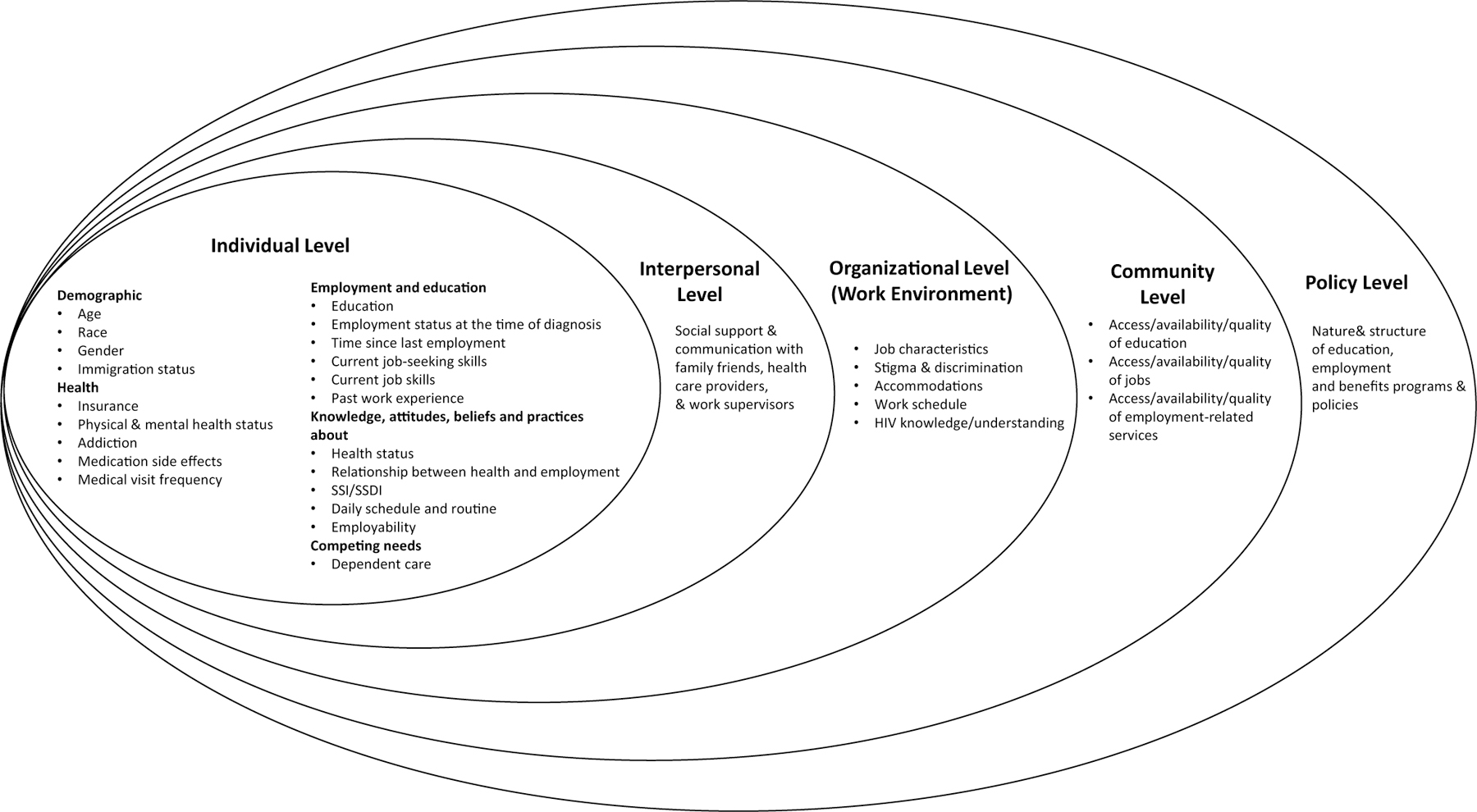
Social-ecological model of factors associated with employment among PLWH
Many of the factors depicted in Fig. 2 are amenable to public health intervention. For example, at the individual level, employment and educational factors could be addressed by increasing linkages to existing federal, state, and local community-based programs that support employment. However, research suggests that uptake of these services among PLWH is low [80, 81]. Additional research on why uptake is low would inform the type of additional intervention is needed to ensure existing programs and resources meet the needs of PLWH. Notably, many of the factors associated with employment (such as stigma and discrimination, social support, communication skills, and daily schedule/routine) are also factors associated with HIV visit and medication adherence [82]. Many PLWH have access to case management and to peer health navigators, for example through the Ryan White Program, and understanding how existing case management or peer navigation programs might be augmented to make sure the employment-related needs of PLWH are addressed might have a positive impact on health and employment outcomes [7, 65]. In addition, programs that train peer mentors who are employed in vocational coaching might help to decrease disparities in employment outcomes among PLWH. At the inter-personal level, programs that aim to increase social support for employment might include engaging endogenous support from friends, family, partners, or spouses in return-to-work efforts, or perhaps providing exogenous sources of support from navigators or community health workers. At the community level, programs to combat stigma and discrimination in the workplace might include trainings for supervisors and staff to dispel misinformation about HIV and ensuring that workplace policies for HIV discrimination are in place, monitored and strictly adhered to. Several important factors associated with employment among PLWH, such as quality of education and the nature and structure of benefits programs (such as SSI/SSDI), are deeply structural and would require significant commitment to change at the policy level.
Research among working-aged adults suggests that some of the mechanism through which a return-to-work might impact health include the degree of economic uncertainty at the environmental level as well as moderating effects of financial strain and stress [79]. The studies included in our review identified the following as mechanisms through which employment status might positively impact physical and mental health among people living with HIV: increased financial resources, increased social support, increased self-concept, decreased spare time and overall improved quality of life. These findings are supported by prominent employment theories. The Pathways between Sectoral Job Training and Increased Health Equity model points to access to material resources, reduced chronic stress, and increased political power as important mechanisms for achieving health equity [83]. Social support models and the Latent Deprivation Theory identify social support and increase shared experiences as pathways to improved health, in particular mental health [84, 85]. In particular, Latent Deprivation Theory recognizes the role of a structured routine, status, identity and sharing collective goals or purpose as important functions of employment for wellbeing and health [85, 86]. Our review also identified mechanisms through which employment may have a negative impact on health including, decreased flexibility, decreased time, and a loss of benefits (including health benefits).
This scoping review identified a number of areas where there is a need for future research. As demonstrated by Fig. 2, the majority of the existing research on employment among PLWH is focused at the individual level, and further work is needed at the interpersonal and environmental levels. Most of the research literature uses dichotomous measures of employment status (such as employed vs. unemployed). Additional research is needed to better understand the employment characteristics (such as part-time vs. full-time, professional vs. non-professional, temporary vs. permanent, with vs. without accommodations) that produce optimal outcomes for PLWH so that those who choose to work can maximize the benefits of work and minimize the disadvantages of work [7, 25, 46]. Negative health consequences of returning to work such as increased stress and decreased access to HIV care also need to be researched and more fully understood [65, 71, 72]. In addition, the majority of the literature focuses on men or samples of both men and women. We identified a limited number of studies that focus exclusively on women living with HIV. Research suggests that women living with HIV are less likely to be employed than men living with HIV [31–33], and further research is needed to explore barriers and facilitators of work among women living with HIV [7, 25, 80]. The majority of the qualitative literature we reviewed focused on barriers to work among individuals who were unemployed. There is a very limited literature that explores resiliencies among PLWH who are employed, and further research in this area may inform return-to-work and work maintenance interventions. Finally, additional research is needed to understand the mechanisms through which employment impacts HIV health behaviors and HIV health outcomes [7].
There are several limitations to this literature review which are worthy of mention. First, our search included two databases, PubMed and Embase. Searching additional databases might have identified additional articles that could have informed this scoping review. In particular, there are counseling and employment journals that are not indexed in PubMed or Embase. As a result, manuscripts from these rehabilitation, psychology and employment journals were not identified by our search. Never the less, the findings from this scoping review were consistent across the literature. Second, our review doesn’t provide an assessment of the risk of bias of the studies included in the review. While this step is a critical part of the methods for systematic reviews, it is not typically included in scoping reviews. Many of the studies included in this review were either qualitative or cross-sectional and were not designed to test causal hypothesis. It is important to note that Fig. 2 only focuses on factors that have been identified through this scoping review as being associated with employment among PLWH. There are important factors which are not listed, such as structural racism, incarceration and experiences with trauma [7], which were not identified by this review but which likely impact employment trajectories among PLWH. Finally, this review did not include articles related to program models, interventions (such as vocational rehabilitation services), or frameworks to improve employment outcomes among PLWH. The authors felt this literature warranted a separate review due to its importance and the volume of this growing body literature.
Conclusion
In conclusion, the National HIV AIDS Strategy calls for comprehensive HIV programs and policies that support the employment needs of PLWH. The findings from this scoping review suggest that employment is positively associated with movement along the HIV continuum of care. The determinants of employment among PLWH are highly complex, operate across many levels, and are amenable to public health intervention. Areas in need of additional research include: determinants of employment among women; employment needs of specific populations disproportionately impacted by HIV (including incarcerated individuals, LGBTQ individuals, ethnic minorities, and people with addiction, mental health, and other disabling conditions) who may encounter unique employment challenges; resiliencies among PLWH who are employed; and longitudinal studies of the mechanisms through which employment many impact HIV health behaviors and HIV health outcomes.
Acknowledgements
Dr. Maulsby was supported by the following grant from National Institutes of Mental Health: 5K01-MH111388. The authors would like to recognize and thank the members of the Exert Advisory Panel for their contributions to this manuscript.
References
- 1.White House Office of National AIDS Policy. National HIV AIDS Strategy for the United States: Updated to (2020). Washington, DC: The White House: December 2015. Available at: https://www.hiv.gov/sites/default/files/nhas-2020-action-plan.pdf. Accessed 13 May 2019. [Google Scholar]
- 2.Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet. 2013;382(9903):1525–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakagawa F, May M, Phillips A. Life expectancy living with HIV: recent estimates and future implications. Curr Opin Infect Dis. 2013;26(1):17–25. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. HIV Surveillance Report (2017). 2018; 29 https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018. Accessed 5 Feb 2019
- 5.Worthington C, O’Brien K, Zack E, McKee E, Oliver B. Enhancing labour force participation for people living with HIV: a multi-perspective summary of the research evidence. AIDS Behav. 2012;16(1):231–43. [DOI] [PubMed] [Google Scholar]
- 6.Braveman B, Levin M, Kielhofner G, Finlayson M. HIV/AIDS and return to work: a literature review one-decade post-introduction of combination therapy (HAART). Work. 2006;27(3):295–303. [PubMed] [Google Scholar]
- 7.Conyers LM, Richardson LA, Datti PA, Koch LC, Misrok M. A critical review of health, social, and prevention outcomes associated with employment for people living with HIV. AIDS Educ Prev. 2017;29(5):475–90. [DOI] [PubMed] [Google Scholar]
- 8.Robinson R, Okpo E, Mngoma N. Interventions for improving employment outcomes for workers with HIV. Cochrane Database Syst Rev. 2015;5:CD010090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vance DE, Cody SL, Yoo-Jeong M, Jones GL, Nicholson WC. The role of employment on neurocognitive reserve in adults with HIV: a review of the literature. J Assoc Nurses AIDS Care. 2015;26(4):316–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4. [DOI] [PubMed] [Google Scholar]
- 12.Arksey H, O’Malley H. Scoping studies: towards a methodological framework. Int J Soc Res. 2005;8(1):19–32. [Google Scholar]
- 13.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Massari V, Lapostolle A, Cadot E, Parizot I, Dray-Spira R, Chauvin P. Gender, socio-economic status, migration origin and neighbourhood of residence are barriers to HIV testing in the Paris metropolitan area. AIDS Care. 2011;23(12):1609–18. [DOI] [PubMed] [Google Scholar]
- 15.Sheehan DM, Trepka MJ, Fennie KP, Prado G, Madhivanan P, Dillon FR, et al. Individual and neighborhood determinants of late HIV diagnosis Among Latinos, Florida, 2007–2011. J Immigr Minor Health. 2017;19(4):825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delpierre C, Cuzin L, Lauwers-Cances V, Marchou B, Lang T, Group N. High-Risk groups for late diagnosis of HIV infection: a need for rethinking testing policy in the general population. AIDS Patient Care STDS. 2006;20(12):838–47. [DOI] [PubMed] [Google Scholar]
- 17.d’Arminio Monforte A, Cozzi-Lepri A, Girardi E, Castagna A, Mussini C, Di Giambenedetto S, et al. Late presenters in new HIV diagnoses from an Italian cohort of HIV-infected patients: prevalence and clinical outcome. Antivir Ther. 2011;16(7):1103–12. [DOI] [PubMed] [Google Scholar]
- 18.Nijhawan AE, Liang Y, Vysyaraju K, Munoz J, Ketchum N, Saber J, et al. Missed Initial medical visits: predictors, timing, and implications for retention in HIV care. AIDS Patient Care STDS. 2017;31(5):213–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aaron E, Alvare T, Gracely EJ, Riviello R, Althoff A. Predictors of linkage to care for newly diagnosed HIV-positive adults. West J Emerg Med. 2015;16(4):535–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Girardi E, Aloisi MS, Arici C, Pezzotti P, Serraino D, Balzano R, et al. Delayed presentation and late testing for HIV: demographic and behavioral risk factors in a multicenter study in Italy. J Acquir Immune Defic Syndr. 2004;36(4):951–9. [DOI] [PubMed] [Google Scholar]
- 21.Joy R, Druyts EF, Brandson EK, Lima VD, Rustad CA, Zhang W, et al. Impact of neighborhood-level socioeconomic status on HIV disease progression in a universal health care setting. J Acquir Immune Defic Syndr. 2008;47(4):500–5. [DOI] [PubMed] [Google Scholar]
- 22.Nachega JB, Uthman OA, Peltzer K, Richardson LA, Mills EJ, Amekudzi K, et al. Association between antiretroviral therapy adherence and employment status: systematic review and meta-analysis. Bull World Health Organ. 2015;93(1):29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shacham E, Lian M, Onen NF, Donovan M, Overton ET. Are neighborhood conditions associated with HIV management? HIV Med. 2013;14(10):624–32. [DOI] [PubMed] [Google Scholar]
- 24.Torres-Madriz G, Lerner D, Ruthazer R, Rogers WH, Wilson IB. Work-related barriers and facilitators to antiretroviral therapy adherence in persons living with HIV infection. AIDS Behav. 2011;15(7):1475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dray-Spira R, Persoz A, Boufassa F, Gueguen A, Lert F, Allegre T, et al. Employment loss following HIV infection in era of highly active antiretroviral therapies. Eur J Pub Health. 2005;16(1):89–95. [DOI] [PubMed] [Google Scholar]
- 26.van Gorp WG, Rabkin JG, Ferrando SJ, Mintz J, Ryan E, Borkowski T, et al. Neuropsychiatric predictors of return to work in HIV/AIDS. J Int Neuropsychol Soc. 2007;13(1):80–9. [DOI] [PubMed] [Google Scholar]
- 27.Wagener MN, van den Dries L, Exel JV, Miedema HS, van Gorp ECM, Roelofs PDDM. Determinants of employment in people living with HIV in the Netherlands. J Occup Rehabil. 2017;28:45. [DOI] [PubMed] [Google Scholar]
- 28.Burns S, Young LRL. Predictors of employment and disability among people living with HIV/AIDS. Rehabil Psychol. 2006;51(2):127–34. [Google Scholar]
- 29.Dray-Spira R, Lert F, Group VS. Living and working with HIV in France in 2003: results from the ANRS-EN12-VESPA Study. AIDS. 2007;21(Suppl 1):S29–S36. [DOI] [PubMed] [Google Scholar]
- 30.Dray-Spira R, Lert F, Marimoutou C, Bouhnik AD, Obadia Y. Socio-economic conditions, health status and employment among persons living with HIV/AIDS in France in 2001. AIDS Care. 2003;15(6):739–48. [DOI] [PubMed] [Google Scholar]
- 31.Oliva J Labour participation of people living with HIV/AIDS in Spain. Health Econ. 2010;19(4):491–500. [DOI] [PubMed] [Google Scholar]
- 32.Dray-Spira R, Gueguen A, Ravaud JF, Lert F. Socioeconomic differences in the impact of HIV infection on workforce participation in France in the era of highly active antiretroviral therapy. Am J Public Health. 2007;97(3):552–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conover CJ, Arno P, Weaver M, Ang A, Ettner SL. Income and employment of people living with combined HIV/AIDS, chronic mental illness, and substance abuse disorders. J Ment Health Policy Econ. 2006;9(2):71–86. [PubMed] [Google Scholar]
- 34.Rabkin JG, McElhiney M, Ferrando SJ, Van Gorp W, Lin SH. Predictors of employment of men with HIV/AIDS: a longitudinal study. Psychosom Med. 2004;66(1):72–8. [DOI] [PubMed] [Google Scholar]
- 35.Lem M, Moore D, Marion S, Bonner S, Chan K, O’Connell J, et al. Back to work: correlates of employment among persons receiving highly active antiretroviral therapy. AIDS Care. 2005;17(6):740–6. [DOI] [PubMed] [Google Scholar]
- 36.George S, Bergin C, Clarke S, Courtney G, Codd MB. Health-related quality of life and associated factors in people with HIV: an Irish cohort study. Health Qual Life Outcomes. 2016;14(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rueda S, Raboud J, Mustard C, Bayoumi A, Lavis JN, Rourke SB. Employment status is associated with both physical and mental health quality of life in people living with HIV. AIDS Care. 2011;23(4):435–43. [DOI] [PubMed] [Google Scholar]
- 38.Rueda S, Raboud J, Plankey M, Ostrow D, Mustard C, Rourke SB, et al. Labor force participation and health-related quality of life in HIV-positive men who have sex with men: the Multicenter AIDS Cohort Study. AIDS Behav. 2012;16(8):2350–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Worthington C, Krentz HB. Socio-economic factors and health-related quality of life in adults living with HIV. Int J STD AIDS. 2005;16(9):608–14. [DOI] [PubMed] [Google Scholar]
- 40.Blalock AC, McDaniel JS, Farber EW. Effect of employment on qualit of life and psychological functioning in patients with HIV/AIDS. Psychosomatics. 2001;43(5):400–4. [DOI] [PubMed] [Google Scholar]
- 41.Rueda S, Raboud J, Rourke SB, Bekele T, Bayoumi A, Lavis J, et al. Influence of employment and job security on physical and mental health in adults living with HIV: cross-sectional analysis. Open Med. 2012;6(4):e118–e12626. [PMC free article] [PubMed] [Google Scholar]
- 42.Nobre N, Pereira M, Roine RP, Sintonen H, Sutinen J. Factors associated with the quality of life of people living with HIV in Finland. AIDS Care. 2017;29(8):1074–8. [DOI] [PubMed] [Google Scholar]
- 43.Rueda S, Rabound J, Mustard C, Rourke S, Bayoumi A, Lavis J, Ostrow D, Plankey M, Lacobson L, Silvestre A. Labour force participation improves health-related quality of life in men who have sex wtih men living with HIV: the multicenter AIDS Cohort Study. Can J INfect Dis Med Microbiol. 2010;21(Suppl B):31B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Razzano LA, Hamilton MM. Health-related barriers to employment among people with HIV/AIDS. J Vocat Rehabil. 2005;22:179–88. [Google Scholar]
- 45.Rueda S, Smith P, Bekele T, O’Brien K, Husbands W, Li A, et al. Is any job better than no job? Labor market experiences and depressive symptoms in people living with HIV. AIDS Care. 2015;27(7):907–15. [DOI] [PubMed] [Google Scholar]
- 46.Dray-Spira R, Gueguen A, Persoz A, Deveau C, Lert F, Delfraissy JF, et al. Temporary employment, absence of stable partnership, and risk of hospitalization or death during the course of HIV infection. J Acquir Immune Defic Syndr. 2005;40(2):190–7. [DOI] [PubMed] [Google Scholar]
- 47.Brooks RA, Martin DJ, Ortiz DJ, Veniegas RC. Perceived barriers to employment among persons living with HIV/AIDS. AIDS Care. 2004;16(6):756–66. [DOI] [PubMed] [Google Scholar]
- 48.Martin DJ, Brooks RA, Ortiz DJ, Veniegas RC. Perceived employment barriers and their relation to workforce-entry intent among people with HIV/AIDS. J Occup Health Psychol. 2003;8(3):181–94. [DOI] [PubMed] [Google Scholar]
- 49.Dray-Spira R, Gueguen A, Lert F, Group VS. Disease severity, self-reported experience of workplace discrimination and employment loss during the course of chronic HIV disease: differences according to gender and education. Occup Environ Med. 2008;65(2):112–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gross M, Herr A, Hower M, Kuhlmann A, Mahlich J, Stoll M. Unemployment, health, and education of HIV-infected males in Germany. Int J Public Health. 2016;61(5):593–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chow JY, Alsan M, Armstrong W, del Rio C, Marconi VC. Risk factors for AIDS-defining illnesses among a population of poorly adherent people living with HIV/AIDS in Atlanta. Georgia AIDS Care. 2015;27(7):844–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Delpierre C, Cuzin L, Lauwers-Cances V, Datta GD, Berkman L, Lang T. Unemployment as a risk factor for AIDS and death for HIV-infected patients in the era of highly active antiretroviral therapy. Sex Transm Infect. 2008;84(3):183–6. [DOI] [PubMed] [Google Scholar]
- 53.Fogarty AS, Zablotska I, Rawstorne P, Prestage G, Kippax SC. Factors distinguishing employed from unemployed people in the positive health study. AIDS. 2007;21(Suppl 1):S37–42. [DOI] [PubMed] [Google Scholar]
- 54.Rodger AJ, Brecker N, Bhagani S, Fernandez T, Johnson M, Tookman A, et al. Attitudes and barriers to employment in HIV-positive patients. Occup Med (Lond). 2010;60(6):423–9. [DOI] [PubMed] [Google Scholar]
- 55.Feuillet P, Lert F, Tron L, Aubriere C, Spire B, Dray-Spira R, et al. Prevalence of and factors associated with depression among people living with HIV in France. HIV Med. 2017;18(6):383–94. [DOI] [PubMed] [Google Scholar]
- 56.Protopopescu C, Raffi F, Brunet-Francois C, Salmon D, Verdon R, Reboud P, et al. Incidence, medical and socio-behavioural predictors of psychiatric events in an 11-year follow-up of HIV-infected patients on antiretroviral therapy. Antivir Ther. 2012;17(6):1079–83. [DOI] [PubMed] [Google Scholar]
- 57.Cline SK, Wang S, Van Wyk J, Baran RW, Gooch KL. An assessment of unemployment among people living with HIV/AIDS in Canada and Europe. Value Health. 2013;16:A363. [Google Scholar]
- 58.Hessol NA, Kalinowski A, Benning L, Mullen J, Young M, Palella F, et al. Mortality among participants in the Multicenter AIDS Cohort Study and the Women’s Interagency HIV Study. Clin Infect Dis. 2007;44(2):287–94. [DOI] [PubMed] [Google Scholar]
- 59.Maruthappu M, Zhou C, Williams C, Zeltner T, Atun R. Unemployment and HIV mortality in the countries of the organisation for economic co-operation and development: 1981–2009. JRSM Open. 2017;8(7):2054270416685206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Richardson LA, Milloy MJ, Kerr TH, Parashar S, Montaner JS, Wood E. Employment predicts decreased mortality among HIV-seropositive illicit drug users in a setting of universal HIV care. J Epidemiol Community Health. 2014;68(1):93–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wada N, Jacobson LP, Cohen M, French A, Phair J, Munoz A. Cause-specific life expectancies after 35 years of age for human immunodeficiency syndrome-infected adn Human Immunodeficiency syndrome-negative individuals followed simultaneously in long-term cohort studies, 1984–2008. Pract Epidemiol. 2013;177(2):116–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dray-Spira R, Legeai C, Le Den M, Boue F, Lascoux-Combe C, Simon A, et al. Burden of HIV disease and comorbidities on the chances of maintaining employment in the era of sustained combined antiretoviral therapies use. AIDS. 2012;26(2):207–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ferrier SE, Lavis JN. With health comes work? People living with HIV/AIDS consider returning to work. AIDS Care. 2003;15(3):423–35. [DOI] [PubMed] [Google Scholar]
- 64.Maticka-Tyndale E, Adam BD, Cohen JJ. To work or not to work: combination therapies and HIV. Qual Health Res. 2002;12(10):1353–72. [DOI] [PubMed] [Google Scholar]
- 65.Timmons JC, Fesko SL. The impact, meaning, and challenges of work: perspectives of individuals with HIV/AIDS. Health Soc Work. 2004;29(2):137–44. [DOI] [PubMed] [Google Scholar]
- 66.Serrano A “How am I going to work?” Barriers to employment for immigrant Latinos and Latinas living with HIV in Toronto. Work. 2015;51(2):365–72. [DOI] [PubMed] [Google Scholar]
- 67.McGinn F, Gahagan J, Gibson E. Back to work: vocational issues and strategies for Canadians living with HIV/AIDS. Work. 2005;25(2):163–71. [PubMed] [Google Scholar]
- 68.Barkey V, Watanabe E, Solomon P, Wilkins S. Barriers and facilitators to participation in work among Canadian women living with HIV/AIDS. Can J Occup Ther. 2009;76(4):269–75. [DOI] [PubMed] [Google Scholar]
- 69.Martin D, Steckart MJ, Arns PG. Returning to work with HIV/AIDS: a qualitative study. Work. 2006;27:209–19. [PubMed] [Google Scholar]
- 70.Hergenrather KC, Rhodes SD, Clark G. Windows to work: exploring employment-seeking behaviors of persons with HIV/AIDS through Photovoice. AIDS Educ Prev. 2006;18(3):243–58. [DOI] [PubMed] [Google Scholar]
- 71.Hergenrather KC, Rhodes SD, Clark G. The employment perspectives study: identifying factors influencing the job-seeking behavior of persons living with HIV/AIDS. AIDS Educ Prev. 2005;17(2):131–42. [DOI] [PubMed] [Google Scholar]
- 72.Wagener MN, van Opstal SE, Miedema HS, Brandjes DP, Dahmen R, van Gorp EC, et al. Employment-related concerns of HIV-positive people in the Netherlands: input for a multidisciplinary guideline. J Occup Rehabil. 2014;24(4):790–7. [DOI] [PubMed] [Google Scholar]
- 73.Sutterheim S, Brands R, Baas I, Lechner L, Kok G, Bos A. HIV status disclosure in the workplace: Positive and stigmatizing experiences of health care workers living with HIV. J Assoc Nurses AIDS Care. 2017;28:923–37. [DOI] [PubMed] [Google Scholar]
- 74.Conyers LM, Boomer KB. Factors associated with disclosure of HIV/AIDS to employers among individuals who use job accomodations and those who do not. J Vocat Rehabil. 2005;22(3):189–98. [Google Scholar]
- 75.Nixon S, Renwick R. Experiences of contemplating returning to work for people living with HIV/AIDS. Qual Health Res. 2003;13(9):1272–90. [DOI] [PubMed] [Google Scholar]
- 76.Li AT, Wales J, Wong JP, Owino M, Perreault Y, Miao A, et al. Changing access to mental health care and social support when people living with HIV/AIDS become service providers. AIDS Care. 2015;27(2):176–81. [DOI] [PubMed] [Google Scholar]
- 77.Conyers LM. The impact of vocational services and employment on people with HIV/AIDS. Work. 2004;23(3):205–14. [PubMed] [Google Scholar]
- 78.Arns PG, Martin DJ, Chernoff RA. Psychosocial needs of HIV-positive individuals seeking workforce re-entry. AIDS Care. 2004;16(3):377–86. [DOI] [PubMed] [Google Scholar]
- 79.Rueda S, Chambers L, Wilson M, Mustard C, Rourke SB, Bayoumi A, et al. Association of returning to work with better health in working-aged adults: a systematic review. Am J Public Health. 2012;102(3):541–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Conyers LM, Datti PA. The unmet vocational rehabilitation needs of women with HIV/AIDS. Work. 2008;31(3):277–90. [PubMed] [Google Scholar]
- 81.Datti PA, Conyers LM. Application of the behavioral model of service utilization to predicting factors assoicated with vocational rehabilitation use among a sample of Latino men with HIV/AIDS in New York State. J Vocat Rehabil. 2010;33(1):15–25. [Google Scholar]
- 82.Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3(11):e438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tsui EK. Sectoral job training as an intervention to improve health equity. Am J Public Health. 2010;100(Suppl 1):S88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Roberts H, Pearson JC, Madeley RJ, Hanford S, Magowan R. Unemployment and health: the quality of social support among residents in the Trent region of England. J Epidemiol Community Health. 1997;51(1):41–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jahoda M Employment and uneployment: a socialpsychological analysis. Cambridge: University Press; 1982. [Google Scholar]
- 86.Paul K, Batinic B. The need for work: Johada’s latent functions of employment in a representative sample of the German population. J Organ Behav. 2009;31(1):45–644. [Google Scholar]


