Abstract
Introduction
Weekly iron–folic acid (IFA) supplements are recommended for all menstruating women in countries where anaemia prevalence is >20%. Anaemia caused by folate deficiency is low worldwide, and the need to include folic acid is in question. Including folic acid might reduce the risk of a neural tube defect (NTD) should a woman become pregnant. Most weekly supplements contain 0.4 mg folic acid; however, WHO recommends 2.8 mg because it is seven times the daily dose effective in reducing NTDs. There is a reluctance to switch to supplements containing 2.8 mg of folic acid because of a lack of evidence that this dose would prevent NTDs. Our aim was to investigate the effect of two doses of folic acid, compared with placebo, on red blood cell (RBC) folate, a biomarker of NTD risk.
Methods
We conducted a three-arm double-blind efficacy trial in Malaysia. Non-pregnant women (n=331) were randomised to receive 60 mg iron and either 0, 0.4, or 2.8 mg folic acid once weekly for 16 weeks.
Results
At 16 weeks, women receiving 0.4 mg and 2.8 mg folic acid per week had a higher mean RBC folate than those receiving 0 mg (mean difference (95% CI) 84 (54 to 113) and 355 (316 to 394) nmol/L, respectively). Women receiving 2.8 mg folic acid had a 271 (234 to 309) nmol/L greater mean RBC folate than those receiving 0.4 mg. Moreover, women in the 2.8 mg group were seven times (RR 7.3, 95% CI 3.9 to 13.7; p<0.0001) more likely to achieve an RBC folate >748 nmol/L, a concentration associated with a low risk of NTD, compared with the 0.4 mg group.
Conclusion
Weekly IFA supplements containing 2.8 mg folic acid increases RBC folate more than those containing 0.4 mg. Increased availability and access to the 2.8 mg formulation is needed.
Trail registration number
This trial is registered with the Australian New Zealand Clinical Trial Registry (ACTRN12619000818134).
Keywords: nutrition, randomised control trial, anaemia, prevention strategies, neural tube defects, folic acid
Key questions.
What is already known?
Women should take folic acid supplements prior to and during early pregnancy to reduce the risk of neural tube defects (NTDs). However, many pregnancies are unplanned and women may not take supplements.
In countries where anaemia prevalence is >20%, WHO recommends all menstruating women 15–49 years of age take a weekly supplement containing 60 mg iron and 2.8 mg folic acid to prevent anaemia and reduce the risk of NTDs, but most supplements currently available in countries implementing programmes contain only 0.4 mg of folic acid.
Evidence is needed to determine whether 2.8 mg would be more effective than 0.4 mg folic acid weekly to reduce NTDs.
What are the new findings?
In this efficacy trial, we showed that weekly iron–folic acid (IFA) supplements containing 2.8 mg folic acid increased red blood cell (RBC) folate, a biomarker of NTD risk, four times as much as 0.4 mg compared with 0 mg.
Sixty-eight per cent of women receiving 2.8 mg folic acid per week achieved a RBC folate concentration >748 nmol/L, a level associated with a low NTD risk, compared with 8% in the 0.4 mg group.
What do the new findings imply?
Weekly IFA supplements containing the WHO recommended 2.8 mg dose of folic acid should be made more widely available.
Introduction
WHO recommends blanket weekly iron–folic acid (IFA) supplementation for all non-pregnant adolescent girls and women (15–49 years) of reproductive age to prevent anaemia in areas where the prevalence of anaemia is higher than 20%.1 Globally, WHO estimates that 50% of anaemia is caused by iron deficiency.2 However, the burden of anaemia caused by folate deficiency is very low, and the need to include folic acid in the weekly supplement is in question. Folic acid taken before and during early pregnancy can reduce the incidence of neural tube defects (NTD),3–5 birth defects such as spina bifida and anencephaly. As standard practice, WHO recommends that all women, from the moment they begin trying to conceive until 12 weeks of gestation, take a daily 0.4 mg folic acid supplement.6 Unfortunately, many pregnancies are unplanned, especially among adolescent girls, and the neural tube closes early in pregnancy (~28 days) before most women know they are pregnant. At least 10 million unplanned pregnancies occur each year among adolescent girls aged 15–19 years in low-income and middle-income countries.7 Therefore, a potential benefit of retaining folic acid in weekly IFA supplements is that if a woman were to have an unplanned pregnancy, it might reduce her risk of an NTD-affected pregnancy.
To help prevent NTDs, WHO recommends weekly IFA supplementation with 2.8 mg folic acid.1 This dose of folic acid was chosen because it is seven times the daily 0.4 mg dose found to be effective in reducing NTDs in controlled trials.5 Most weekly supplements currently available contain 60 mg iron and 0.4 mg folic acid, as this formulation is the standard for anaemia prevention and is readily available.8 Moreover, 0.4 mg folic acid with 60 mg of iron is what is recommended daily during pregnancy,6 thus, the 2.8 mg requires a different formulation. Of the 4.2 million IFA packs distributed by UNICEF in 2019, only 284 000 contained the WHO recommended folic acid dose of 2.8 mg (Personal communication, Andreas Tjornehoj, UNICEF Supply Division, Copenhagen, 2020). There is a reluctance to switch to IFA supplements containing 2.8 mg of folic acid because of a lack of evidence this dose, or any weekly dose, would prevent NTDs. New folic acid trials with NTD as an outcome are unlikely. Fortunately, cohort studies have found that red blood cell (RBC) folate in early pregnancy is inversely associated with subsequent NTD risk. RBC folate is now a well-accepted biomarker of NTD risk at the population level.9 10 While the optimal RBC folate for NTD prevention is not known with certainty, WHO has recommended a concentration >748 nmol/L for women of reproductive age as desirable at the population level.11 However, the relationship between RBC folate and NTD risk is continuous, and any increase in RBC folate would be expected to decrease NTD risk. Although the relationship is continuous, there appears to be little additional benefit above this threshold, as the reduction in risk approaches an asymptote at concentrations of ~1058–1216 nmol/L (calibrator adjusted).10
Our primary aim was to determine the effect of 16 weeks of weekly iron (60 mg) with 0 mg, 0.4 mg or 2.8 mg of folic acid on RBC folate concentrations in women of reproductive age. We also examined the percentage of women by treatment group who achieved an RBC folate concentration >748 nmol/L, the concentration associated with a low risk of NTDs. As IFA supplementation is commonly initiated during adolescence in school settings, we secondarily assessed the effect of a 4-week washout period on RBC folate concentrations in an attempt to mimic the effect of school holiday periods.
Methods
Study design
Full details of the study design are in the published trial protocol.12 The study was a parallel design, double-blind placebo-controlled randomised efficacy trial. It was conducted at Universiti Putra Malaysia in Selangor, Malaysia. Malaysia was chosen because the prevalence of anaemia is >20% among women of reproductive age, vitamin supplement use is low, and there is no folic acid fortification.13–15 To be eligible, women had to be: between 18 and 45 years; non-pregnant (self-reported); not planning on becoming pregnant; not taking folic acid containing supplements; not participating in another nutritional intervention; and not taking any medications known to inhibit folate status (methotrexate, certain anticonvulsants or sulfasalazine). The primary outcome was RBC folate at 16 weeks postrandomisation. Secondary outcomes included plasma folate at 16 weeks and RBC folate and plasma folate at 20 weeks following a 4-week washout period in which women did not take supplements. Plasma and RBC folate were measured using a microbiological method described below.
All participants gave written informed consent.
Patient and public involvement
The development of the research question and outcome measures were not informed by the participants’ priorities, experience and preferences. Participants were not involved in the design of this study.
Procedures
Women were recruited through advertisements, word-of-mouth, and classroom presentations at Universiti Putra Malaysia. Women expressing an interest were given a participant information sheet and pre-screened for eligibility. If women were eligible and willing to participate, they were asked to attend a morning clinic at the university health centre following an overnight fast. After reconfirming eligibility and obtaining written consent, a blood sample was collected by venepuncture into two evacuated tubes containing ethylenediaminetetraacetic acid (EDTA) as an anticoagulant. After sociodemographic, health and anthropometric data were recorded, women were randomised. Women were asked to take one tablet at the clinic and then one tablet every week on the same day for 16 weeks; they were also asked not to take any nutritional supplements during the study other than the investigational products provided. Participants were reminded weekly by text message to take their supplement, to encourage adherence, and asked if they had experienced any adverse events. After 16 weeks, women returned to the clinic following an overnight fast and another blood sample was collected. Participants were instructed not to consume the supplement in the 48 hours preceding the blood draw. Adherence was assessed by counting the number of remaining tablets in the bottles at 16 weeks. Participants discontinued their supplements and returned to the clinic 4 weeks later for a final fasting blood draw.
Supplements, randomisation and masking
Supplements were manufactured by Unison Nutraceutical Sdn Bhd (Ayer Keroh, Malacca, Malaysia) and approved by the National Pharmaceutical Regulatory Agency in Malaysia. The company had no other role in the trial. Supplements were manufactured as tablets containing 60 mg of iron as ferrous fumarate and either 0, 0.4 or 2.8 mg folic acid as the active ingredients. Inactive ingredients included microcrystalline cellulose, polyvinylpyrrolidone, colloidal silicon dioxide, magnesium stearate and pregelatinised starch. The supplements were sent blinded to an external lab for independent folic acid testing (Factors Group of Nutritional Supplements, BC, Canada); the 0, 0.4 and 2.8 mg tablets had a measured value of 0, 0.38 and 2.72 mg, respectively. The supplements and the opaque glass bottles they were packed in were identical in appearance except for a coloured sticker to identify treatment group.
The randomisation schedule was prepared by an independent statistician using ralloc.ado version 3.7.6 in Stata V.15.1 (Stata Corp). Randomly permuted blocks of size six were used to assign participants to one of six colour codes; two colour codes were used per treatment to assist with blinding. Participants, outcome assessors and data analysts were blinded to treatment group. Participants were randomised using a secure web application (Research Electronic Data Capture) by trained research assistants.16 17
Laboratory analysis
After each blood collection, one EDTA tube was sent to Clinipath Malaysia Sdn. Bhd. (Selangor, Malaysia) for a full blood count determination using an automated haematology analyser (Sysmex XP-100, Sysmex). An aliquot of whole blood from the remaining tube was removed, diluted to 1 in 11 in 1% ascorbic acid, and incubated for 30 min at 38℃. The remaining blood was centrifuged at 3000 rpm for 10 min at 4°C. The resulting plasma was removed and aliquoted. All samples were stored at −80℃ until analysis.
Blood samples were shipped on dry ice to Adelaide, Australia for folate analysis. Whole blood and plasma folate concentrations were determined using the microbiological method based on the method of O’Broin and Kelleher, using standardised kits from the US Centres for Disease Control and Prevention (US CDC; Atlanta, GA).18–20 This method uses 96 well microplates, 5-methyl tetrahydrofolate (Merck) as the calibrator, and chloramphenicol resistant Lactobacillus rhamnosus (ATCC 27773TM) as the test organism. High and low quality controls (QC) for each of whole blood folate and plasma folate, provided by the US CDC, were run in quadruplets on every plate. RBC folate was calculated by subtracting plasma folate from whole blood folate and correcting for haematocrit.
As per US CDC instructions21: if all QC results were within mean (2 SD) limits, the assay was accepted; if more than one of the QC results were outside of the mean (2 SD) limits or any of the QC results were outside of the mean (3 SD) limits, then the assay was rejected. Results from assay runs that passed QC were recorded only when the quadruplets were below 15%. If the coefficient of variation (CV) of the quadruplets was above 15%, the largest outlier was removed and the results recorded as long as the CV of the remaining triplicates was below 10%; otherwise, the sample measurement was repeated.
At the population level, WHO recommends RBC folate concentrations be >906 nmol/L in women of reproductive age to prevent NTDs. This RBC folate value was generated using folic acid as the calibrator.9 19 We used a newer method recommended by the US CDC that uses 5‐methyl tetrahydrofolate as the calibrator. Since 5‐methyl tetrahydrofolate gives lower RBC folate concentrations than folic acid, we used a cut-off of >748 nmol/L to define the optimal RBC folate concentration for NTD risk reduction.22–24
Statistical analyses
A sample size of 63 participants per treatment group was required to detect a clinically meaningful difference of 100 nmol/L in mean RBC folate concentrations across groups at the end of the intervention period (16 weeks), while adjusting for baseline RBC folate concentration, with 80% power and two-sided α of 0.0167 for pairwise comparisons between the three treatment groups (overall α=0.05). The sample size assumes an SD of 202 nmol/L,25 a correlation between RBC folate concentrations at baseline and 16 weeks of 0.6, and a drop-out rate of up to 10%. We aimed to recruit 100 participants per group to allow for some uncertainty in the assumed values.
A descriptive comparison of the randomised groups was conducted on all baseline demographic characteristics and baseline measures of the outcomes. The primary analysis was performed on the available data according to treatment allocation at randomisation (intention-to-treat analysis). A secondary ‘per-protocol’ analysis was also performed, including only women who completed the study and were >80% adherent to the treatment regime. Continuous outcomes were analysed using linear regression models, and binary outcomes were analysed using log-binomial regression models, or log Poisson regression models with robust variance estimation if convergence issues occurred. Adjustment was also made for baseline body mass index (BMI) category in an unplanned sensitivity analysis after observing a chance imbalance in BMI between the treatment groups. Treatment group, time point (16 or 20 weeks), and a treatment group by time point interaction were included as predictors and analyses were adjusted for the baseline measure of the outcome. The generalised estimating equation method with an exchangeable working correlation structure was used to account for the correlation between outcomes at 16 and 20 weeks. Global interaction tests were performed, and the difference in means or the relative risk (with two-sided 95% CI and p value) comparing each pair of treatment groups was estimated for each time point separately. Statistical significance was set at p<0.05 for interaction tests and p<0.0167 for pairwise comparisons between treatment groups. Analyses followed a prespecified statistical analysis plan and were completed using Stata SE V.15.1 (StataCorp).
Results
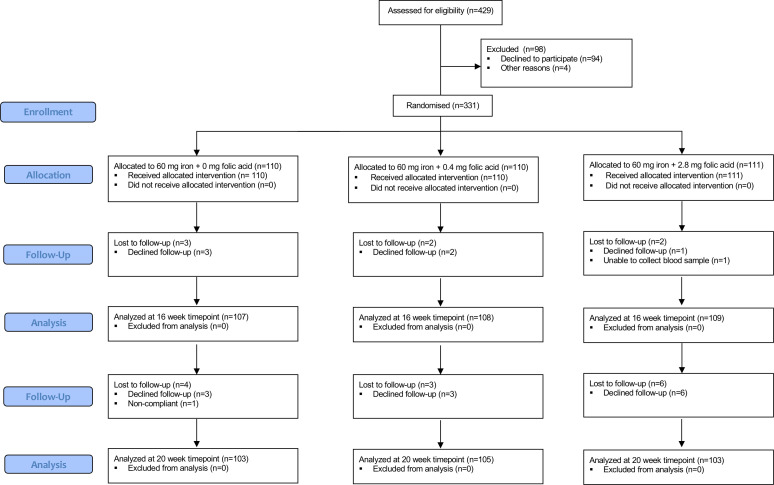
Recruitment commenced 20 August 2019, and finished 12 September 2019, with 429 women screened for eligibility. Of these, 94 declined to participate mainly due to a fear of giving blood (n=24) or their parents did not want them to participate (n=21). Four women were excluded before randomisation because a blood sample could not be obtained. The first study visit was conducted on 3 September 2019, and the final study visit occurred 13 February 2020. Of the 331 women randomised, 110, 110 and 111 were allocated to the 0, 0.4 and 2.8 mg folic acid groups, respectively. Overall, 98% (n=324) of participants returned for the 16-week visit and 94% (n=311) returned for the 20-week visit (figure 1). The study ended when the last participant who remained in the trial completed her final visit on 13 February 2020.
Figure 1.
Flow diagram of trial enrolment.
Overall, the median (IQR) age of the participants was 18 (18, 18) years, with ~95% of the 331 participants between the ages of 18 and 21 years. Eighty-nine per cent of participants were Malay (n=295), >99% had never been married, and 77% were in a Foundation year at Universiti Putra Malaysia. More than half of the participants had a healthy BMI (table 1). The overall mean±SD baseline plasma folate concentration was 10.7±5.1 nmol/L, and the overall mean±SD baseline RBC folate concentration was 482±148 nmol/L.
Table 1.
Baseline characteristics of enrolled Malaysian women by treatment group*
| 0 mg folic acid (n=110) | 0.4 mg folic acid (n=110) | 2.8 mg folic acid (n=111) | |
| Age, years | 18 (18,18) | 18 (18,18) | 18 (18,19) |
| Ethnicity | |||
| Malay | 96 (87%) | 99 (90%) | 100 (90%) |
| Chinese | 9 (8%) | 7 (6%) | 8 (7%) |
| Indian | 1 (1%) | 2 (2%) | 2 (2%) |
| Other | 4 (4%) | 2 (2%) | 1 (1%) |
| Never married | 110 (100%) | 107 (97%) | 110 (99%) |
| People living in household | 5 (4,6) | 5 (4,6) | 5 (5,6) |
| Current level of schooling | |||
| Foundation year | 84 (76%) | 87 (79%) | 83 (75%) |
| Bachelor’s degree | 22 (20%) | 19 (17%) | 22 (20%) |
| Completed Bachelor’s degree or higher | 4 (3.6%) | 4 (4%) | 6 (5%) |
| Monthly household income, US$ | |||
| Less than US$250 | 5 (5%) | 3 (3%) | 10 (9%) |
| US$250–US$450 | 18 (16%) | 20 (18%) | 12 (11%) |
| US$450–US$900 | 22 (20%) | 18 (16%) | 14 (13%) |
| US$900–US$1400 | 21 (19%) | 21 (19%) | 17 (15%) |
| US$1400 and above | 33 (30%) | 30 (27%) | 52 (47%) |
| Declined | 11 (10%) | 18 (16%) | 6 (5%) |
| BMI category (kg/m2) | |||
| Underweight, <18.5 | 19 (17%) | 25 (23%) | 16 (14%) |
| Normal weight, 18.5–24.9 | 64 (58%) | 61 (56%) | 74 (67%) |
| Overweight, 25–29.9 | 13 (12%) | 15 (14%) | 11 (10%) |
| Obese, ≥30 | 14 (13%) | 9 (8%) | 10 (9%) |
| Baseline Hb, g/L | 129±12 | 128±12 | 128±11 |
| Anaemia prevalence, Hb <120 g/L | 18 (16%) | 20 (18%) | 20 (18%) |
*Values are mean±SD, median (IQR), or n (%).
BMI, body mass index; Hb, haemoglobin.
Overall, 94% (n=312/331) participants were adherent, consuming 80% of the required tablets throughout the 16 weeks of intervention. In the 2.8 mg folic acid group, 95% (n=106/111) were adherent, while 93% (n=102/110) and 95% (n=104/110) were adherent in the 0.4 mg and 0 mg groups, respectively. Thirty-five women (11%) reported experiencing at least one side effect (n=10 in the 0 mg group, n=10 in the 0.4 mg group and n=15 in the 2.8 mg group). Common side effects included: nausea (n=9), diarrhoea (n=10), vomiting (n=4), gas (n=8) and constipation (n=7).
After 16 weeks of supplementation, the mean RBC folate was significantly higher in the groups receiving 2.8 mg and 0.4 mg folic acid than 0 mg (mean difference (MD) 355 (95% CI 316 to 394) and 84 (95% CI 54 to 113) nmol/L, respectively (p<0.0001)) (table 2). RBC folate was 271 (95% CI 234 to 309) nmol/L higher on average in the group receiving 2.8 mg than those receiving 0.4 mg (p<0.0001). Following washout, mean RBC folate remained significantly higher in the groups receiving 2.8 mg and 0.4 mg folic acid per week than 0 mg (MD 293 (95% CI 259 to 327) and 82 (95% CI 52 to 113) nmol/L, respectively (p<0.0001)). After 16 weeks of supplementation, mean plasma folate was significantly higher in the group receiving 2.8 mg folic acid than the 0.4 mg and 0 mg groups (MD 14.9 (95% CI 12.0 to 17.8) and 19.6 95% CI (16.9 to 22.4) nmol/L, respectively (p<0.0001)). Following washout, mean plasma folate remained significantly higher in the group receiving 2.8 mg folic acid than the groups receiving 0.4 mg and 0 mg (MD 8.0 (95% CI 5.7 to 10.3) and 9.5 (95% CI 6.8 to 12.3) nmol/L, respectively (p<0.0001)). The per-protocol analysis produced similar findings (online supplemental table 1), as did an unplanned sensitivity analysis adjusting for baseline BMI category due to a chance imbalance between the treatment groups (data not shown).
Table 2.
RBC and plasma folate concentrations by treatment group at 16 and 20 weeks
| Outcome | 0 mg (n=110)* | 0.4 mg (n=110)* | 2.8 mg (n=111)* | 2.8 vs 0 mg | 0.4 vs 0 mg | 2.8 vs 0.4 mg | |||
| Mean difference (95% CI)† |
P value‡ | Mean difference (95% CI)† |
P value‡ | Mean difference (95% CI)† |
P value‡ | ||||
| RBC folate, nmol/L§ | |||||||||
| Baseline | 466±136 | 474±136 | 507±168 | ||||||
| 16 weeks | 466±158 | 554±146 | 851±208 | 355 (316 to 394) | <0.0001 | 84 (54 to 113) | <0.0001 | 271 (234 to 309) | <0.0001 |
| 20 weeks | 443±134 | 534±155 | 766±183 | 293 (259 to 327) | <0.0001 | 82 (52 to 113) | <0.0001 | 211 (173 to 249) | <0.0001 |
| Plasma folate, nmol/L§ | |||||||||
| Baseline | 10.1±4.0 | 10.3±4.3 | 11.6±6.6 | ||||||
| 16 weeks | 10.7±4.8 | 15.6±7.2 | 31.5±14.5 | 19.6 (16.9 to 22.4) | <0.0001 | 4.8 (3.5 to 6.0) | <0.0001 | 14.9 (12.0 to 17.8) | <0.0001 |
| 20 weeks | 13.5±10.3 | 15.2±6.2 | 24.2±11.0 | 9.5 (6.8 to 12.3) | <0.0001 | 1.5 (−0.5 to 3.6) | 0.15 | 8.0 (5.7 to 10.3) | <0.0001 |
*Values are mean±SD based on the raw data of the intention-to-treat population.
†Mean differences are adjusted for the baseline value of the outcome.
‡Statistical significance set at p<0.0167 for pairwise comparisons of treatment groups.
§P<0.0001 for treatment group by time point interaction test.
RBC, red blood cell.
bmjgh-2020-003897supp001.pdf (81.1KB, pdf)
At 16 weeks, the 2.8 mg group was more likely to have RBC folate concentrations >748 nmol/L than the 0.4 mg (relative risk (RR) 7.3, 95% CI 3.9 to 13.7) and the 0 mg folic acid group (RR 16.0, 95% CI 6.1 to 42.3), while there was no evidence of a difference between the 0.4 and 0 mg groups. Following the washout period, the 2.8 mg group was still more likely to have RBC folate >748 nmol/L than the 0.4 mg (RR 4.2, 95% CI 2.4 to 7.3) and 0 mg group (RR 14.6, 95% CI 5.2 to 41.1). The difference between the 0.4 and 0 mg groups at 20 weeks did not reach statistical significance after adjustment for multiple comparisons (table 3).
Table 3.
RBC folate concentrations >748 nmol/L by treatment group at baseline, 16 and 20 weeks
| Treatment | N | Baseline* | 16 weeks* | Relative risk (95% CI)† | P value‡ | 20 weeks* | Relative risk (95% CI)† | P value‡ |
| 2.8 mg folic acid§ | 111 | 9 (8%) | 74 (68%) | 16.0 (6.1 to 42.3) | <0.0001 | 55 (53%) | 14.6 (5.2 to 41.1) | <0.0001 |
| 0.4 mg folic acid | 110 | 4 (4%) | 9 (8%) | 2.2 (0.7 to 6.8) | 0.17 | 12 (11%) | 3.5 (1.1 to 10.7) | 0.03 |
| 0 mg folic acid | 110 | 3 (3%) | 4 (3%) | Reference | 3 (3%) | Reference |
*Values are n (%) of women with RBC folate concentrations greater than 748 nmol/L based on the raw data of the intention-to-treat population.
†Relative risks are relative to the 0 mg folic acid group and are adjusted for baseline RBC folate levels.
‡Statistical significance set at p<0.0167 for pairwise comparisons of treatment groups.
§RBC folate relative risk for 2.8 mg vs 0.4 mg was 7.3 (95% CI 3.9 to 13.7; p<0.0001) at 16 weeks and 4.2 (95% CI 2.4 to 7.3; p<0.0001) at 20 weeks. P=0.31 for treatment group by time point interaction test.
RBC, red blood cell.
Discussion
Here, we provide the first evidence that the recommended weekly dose of 2.8 mg folic acid, rather than the commonly used 0.4 mg weekly dose, is more effective at increasing RBC folate. Therefore, we would expect the 2.8 mg dose to be more protective against NTDs should a woman or adolescent girl become pregnant. After 16 weeks of treatment, 68% of women in the 2.8 mg group attained an RBC folate >748 nmol/L, compared with only 8% in the 0.4 mg weekly group. Moreover, at 16 weeks, women receiving 0.4 mg folic acid were not more likely to achieve RBC folate >748 nmol/L than women receiving 0 mg—further highlighting the minimal impact of providing 0.4 mg once weekly.
With respect to the reduction in NTD, Crider et al estimated a risk reduction from 35.9 (95% CI 28.1 to 46.2) NTDs per 10 000 births to 14.6 (12.4 to 17.0) NTDs per 10 000 births following a 300 nmol/L increase in RBC folate among US women with RBC folate concentrations in the fifth percentile.10 Given that women in our trial receiving 2.8 mg folic acid per week had a similar increase in RBC folate concentrations, a large risk reduction, such as the one demonstrated above, would be predicted—especially among women with low baseline status. Overall, weekly IFA supplements that contain 60 mg of elemental iron and 2.8 mg of folic acid could not only prevent anaemia but also reduce the risk of NTD if a woman were to become pregnant. The 2.8 mg dose of folic acid would be particularly benefit adolescent girls beause of their high rate of unplanned pregnancies.7
While no studies have compared iron with different weekly folic acid doses on RBC folate, weekly dosing has been compared with daily supplementation in at least two trials. Unsurprisingly, daily dosing is more effective than weekly at increasing blood folate indices. Among New Zealand women (18–40 years), daily supplementation with 0.4 mg folic acid was more effective than 2.8 mg weekly at increasing RBC folate after 12 weeks (MD (95% CI) 411 (325 to 504) and 265 (192 to 345) nmol/L, respectively) compared with the 0 mg group.25 Nevertheless, the authors concluded that 2.8 mg folic acid weekly would still be expected to decrease NTD risk. Moreover, in the New Zealand study, over half of the women taking the weekly folic acid supplement achieved an RBC folate concentration associated with a low risk of NTD at week 12 compared with nearly three-quarters in the daily 0.4 mg group. Compared with their respective placebo groups, the MD in RBC folate among women receiving 2.8 mg folic acid weekly in the New Zealand study was not as great as the difference reported in our study (MD 265 vs 355 nmol/L). The greater difference in mean RBC folate observed in our study may be due to the longer duration of our study compared with the New Zealand study (16 vs 12 weeks), as baseline RBC folate concentrations were similar after calibrator adjustment.
Hao et al compared the effect of 4.0 mg folic acid weekly vs 0.4 mg folic acid daily on RBC folate concentrations in Chinese women (24–42 years).26 After 3 and 6 months of supplementation, RBC folate concentrations increased by ~171 and ~278 nmol/L, respectively, in the 4.0 mg weekly group compared with ~310 and ~430 nmol/L in the group receiving 0.4 mg folic acid daily. The increase seen when supplementing with 4.0 mg folic acid weekly was half that in our study at a similar time point (12 and 16 weeks), despite using a higher dose. The women in the study by Hao et al had a high prevalence (>30%) of the TT variant of the methylenetetrahydrofolate reductase (MTHFR) 677C→T genotype, an enzyme polymorphism that is associated with altered folate metabolism. The increase in those with the TT variant receiving the weekly supplement was only half that of those with the CC wildtype at 3 months (~123 vs 220 nmol/L, respectively).27 The global prevalence of this variant is estimated at less than 10%.28 29 In our recent study in a similar group in Malaysia (n=75), only one woman carried the TT variant.30 Thus, this Chinese population may not be representative of the wider global population.
Plasma folate concentrations at week 16 by treatment group generally paralleled RBC folate. Plasma folate is affected by recent dietary intake, especially folic acid supplement use, and is less stable than RBC folate, which better reflects tissue folate concentrations.24 Moreover, WHO recommends that plasma folate not be used as a biomarker for NTD prevention, and no sufficiency threshold for plasma folate is given.11
Strengths of this trial include the randomised placebo controlled design and high retention (98% at 16 weeks) and adherence rates (94% at 16 weeks). Further, there is no fortification with folic acid in Malaysia and the prevalence of anaemia among women of reproductive age is greater than 20%,13 suggesting that WHO recommended intermittent IFA programming is warranted in this population for non-pregnant women. We used a well-accepted biomarker of NTD risk, RBC folate, which is inversely associated with NTD risk in diverse populations, including Irish and Chinese women.9 10 Moreover, the finding that folic acid fortification, which typically provides women with less than 0.4 mg/daily, has increased RBC folate and lowered NTD risk in countries where it has been implemented further supports the use of this biomarker.31–33 The work was carried out in Malaysia because it had anaemia rates high enough to justify a weekly IFA programme and the necessary infrastructure and expertise to carry out a high-quality efficacy trial. However, we are confident that our results are generalisable to other countries where weekly IFA supplements are used and will reduce the burden of these devastating birth defects.
Limitations include that no trial has shown that weekly folic acid, at any dose, lowers NTDs. Evidence supporting weekly folic acid comes from México, where a 50% reduction in NTDs was found following a public health campaign that recommended women take 5 mg folic acid weekly.34 Moreover, the 16-week duration of our intervention likely underestimates the full potential of the intervention effect on RBC folate concentrations. It has been previously shown that women consuming 0.4 mg folic acid daily for 40 weeks had still not yet reached a steady-state of RBC folate concentrations. Houghton et al estimated that it would likely require 96 weeks for women to achieve 90% of the estimated steady-state when supplementing with 0.4 mg folic acid per day.35 While our intervention was short, intermittent IFA supplementation is recommended to commence after menarche and continue through to menopause,1 meaning that adolescent girls and women participating in IFA programmes could be consuming the supplements for long periods and will reach a steady-state. Also, our secondary analyses examining the dichotomized outcome presented for RBC folate >748 does not have the same degree of statistical precision as our pre-specified primary outcome on which the trial’s sample size was based, RBC folate as a continuous variable (which had excellent statistical precision (table 2)).
Finally, we did not measure MTHFR genotype nor account for differences in efficacy based on BMI. The MTHFR TT variant is associated with lower plasma and RBC folate concentrations27; however, the prevalence of the TT variant is thought to be relatively low in the Malay population. A higher BMI has been shown to alter distributions of plasma and cellular folate, leading to lower plasma concentrations and higher RBC folate concentrations.36–38 WHO guideline states that weekly IFA supplementation is to be targeted to all menstruating adolescent girls and women in populations where the prevalence of anaemia in non-pregnant women of reproductive age is 20% or higher.1 In practice, there is unlikely to be different doses of IFA supplements for populations depending on their BMI or MTHFR genotype.
Daily supplementation with folic acid remains the best practice to prevent NTDs in women planning a pregnancy. Where women are not planning to become pregnant, or do not take a daily supplement, our findings show that weekly IFA supplements containing the WHO recommended dose of 2.8 mg folic acid are more effective at improving RBC folate concentrations and reducing the risk of NTDs than the dose currently used in practice (0.4 mg folic acid per week). In order to achieve success in a real world setting, weekly IFA programmes must be designed using evidence-based best practices that encourage maximal coverage and adherence.39 40 We recommend that countries currently using weekly IFA supplements containing 0.4 mg folic acid be enabled and supported to switch to 2.8 mg.
Acknowledgments
KLIS received a Frederick Banting and Charles Best Canada Graduate Scholarship. We also thank The Factors Group of Nutritional Companies (Burnaby, BC, Canada) for testing the iron and folic acid content of the supplements.
Footnotes
Handling editor: Sanni Yaya
Contributors: MLR, CDK and TJG conceived the trial and proposed the initial trial design. KLIS, SPL, GLK, ZBMS, IZI, MM, MLR, CDK and TJG revised and finalised the protocol; LNY, SL and JAH advised on sample size calculations, trial design and analysis; statistical analyses were completed by LNY; KLIS, SPL, SSL, DCS and IZI were responsible for organisation and conduct of the study; KLIS, SSL and DCS collected data. KLIS, DCS and TJG conducted the blood folate analyses; KLIS, CDK and TJG drafted the manuscript, all authors reviewed the manuscript and approved the final submission.
Funding: This trial was supported by a grant in aid from Nutrition International (grant 10-1798-SOUAUS-02). The funder was involved with designing the trial and reviewed the manuscript before submission. The funder had no role in data collection, analysis or interpretation. Nutrition International is a not-for-profit organisation governed by a dedicated international Board of Directors and led by an internationally recognised team of technical experts, programme designers, advocates, analysts, evaluators, implementers, educators, resource managers and nutrition champions.
Competing interests: MM reports being on the Scientific Board of Trajan Nutrition, outside the submitted work. LNY reports grants from Australian National Health and Medical Research Council, during the conduct of the study. MLR is an employee of the sponsor.
Patient consent for publication: Not required.
Ethics approval: Ethical approval was received from the Ethics Committee for Research Involving Human Subjects of Universiti Putra Malaysia (JKEUPM-2018–255) and The University of British Columbia Clinical Research Ethics Board (H18-00768).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on request. Deidentified data will be made available 12 months after publication. Person(s) requesting the data must provide a methodologically sound research proposal which will reviewed by the trial steering committee. If approved, a signed data access agreement will be required before the data is released. Please contact the corresponding author for access to the data.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.World Health Organization Guideline: intermittent iron and folic acid supplementation in menstruating women. Geneva, Switzerland, 2011. [PubMed] [Google Scholar]
- 2.Stevens GA, Finucane MM, De-Regil LM, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: a systematic analysis of population-representative data. Lancet Glob Health 2013;1:e16–25. 10.1016/S2214-109X(13)70001-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MRC Vitamin Study Research Group Prevention of neural tube defects: results of the medical Research Council vitamin study. MRC vitamin study Research Group. Lancet 1991;338:131–7. [PubMed] [Google Scholar]
- 4.Czeizel AE, Dudás I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 1992;327:1832–5. 10.1056/NEJM199212243272602 [DOI] [PubMed] [Google Scholar]
- 5.Berry RJ, Li Z, Erickson JD, et al. Prevention of neural-tube defects with folic acid in China. N Engl J Med 1999;341:1485–90. 10.1056/NEJM199911113412001 [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization Who recommendation on antenatal care for positive pregnancy experience. Geneva, Switzerland, 2016. [PubMed] [Google Scholar]
- 7.Darroch J, Woog V, Bankole A, et al. Adding it up: costs and benefits of meeting the contraceptive needs of adolescents. New York, 2016. [Google Scholar]
- 8.Stoltzfus R, Dreyfuss M. Guidelines for the use of iron supplements to prevent and treat iron deficiency anemia. Washington, DC: ILSI Press, 1998. [Google Scholar]
- 9.Daly LE, et al. Folate levels and neural tube defects. JAMA 1995;274:1698–702. 10.1001/jama.1995.03530210052030 [DOI] [PubMed] [Google Scholar]
- 10.Crider KS, Devine O, Hao L, et al. Population red blood cell folate concentrations for prevention of neural tube defects: Bayesian model. BMJ 2014;349:1–12. 10.1136/bmj.g4554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization Guideline: optimal serum and red blood cell folate concentrations in women of reproductive age for prevention of neural tube defects. Geneva, Switzerland, 2015. [PubMed] [Google Scholar]
- 12.Samson KLI, Loh SP, Khor GL, et al. Effect of once Weekly folic acid supplementation on erythrocyte folate concentrations in women to determine potential to prevent neural tube defects: a randomised controlled dose-finding trial in Malaysia. BMJ Open 2020;10:1–6. 10.1136/bmjopen-2019-034598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Prevalence of anaemia in women of reproductive age. http://apps.who.int/gho/data/view.main.ANAEMIAWOMENPREVANEMIAREG?lang=en 2017
- 14.Khor GL, Duraisamy G, Loh SP, et al. Dietary and blood folate status of Malaysian women of childbearing age. Asia Pac J Clin Nutr 2006;15:341–9. [PubMed] [Google Scholar]
- 15.Green TJ, Skeaff CM, Venn BJ, et al. Red cell folate and predicted neural tube defect rate in three Asian cities. Asia Pac J Clin Nutr 2007;16:269–73. [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Broin S, Kelleher B. Microbiological assay on microtitre plates of folate in serum and red cells. J Clin Pathol 1992;45:344–7. 10.1136/jcp.45.4.344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Molloy AM, Scott JM. Microbiological assay for serum, plasma, and red cell folate using cryopreserved, microtiter plate method. Methods Enzymol 1997;281:43–53. 10.1016/s0076-6879(97)81007-5 [DOI] [PubMed] [Google Scholar]
- 20.Zhang M, Sternberg MR, Pfeiffer CM. Harmonizing the calibrator and microorganism used in the folate microbiological assay increases the comparability of serum and whole-blood folate results in a CDC Round-Robin study. J Nutr 2018;148:807–17. 10.1093/jn/nxy030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Centers for Disease Control and Prevention Folate microbiological assay training manual version 1, 2018. [Google Scholar]
- 22.Tinker SC, Hamner HC, Qi YP, et al. U.S. women of childbearing age who are at possible increased risk of a neural tube defect-affected pregnancy due to suboptimal red blood cell folate concentrations, National health and nutrition examination survey 2007 to 2012. Birth Defects Res A Clin Mol Teratol 2015;103:517–26. 10.1002/bdra.23378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pfeiffer CM, Sternberg MR, Hamner HC, et al. Applying inappropriate cutoffs leads to misinterpretation of folate status in the US population. Am J Clin Nutr 2016;104:1607–15. 10.3945/ajcn.116.138529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bailey LB, Hausman DB. Folate status in women of reproductive age as basis of neural tube defect risk assessment. Ann N Y Acad Sci 2018;1414:82–95. 10.1111/nyas.13511 [DOI] [PubMed] [Google Scholar]
- 25.Norsworthy B, Skeaff CM, Adank C, et al. Effects of once-a-week or daily folic acid supplementation on red blood cell folate concentrations in women. Eur J Clin Nutr 2004;58:548–54. 10.1038/sj.ejcn.1601843 [DOI] [PubMed] [Google Scholar]
- 26.Hao L, Yang Q-H, Li Z, et al. Folate status and homocysteine response to folic acid doses and withdrawal among young Chinese women in a large-scale randomized double-blind trial. Am J Clin Nutr 2008;88:448–57. 10.1093/ajcn/88.2.448 [DOI] [PubMed] [Google Scholar]
- 27.Crider KS, Zhu J-H, Hao L, et al. MTHFR 677C->T genotype is associated with folate and homocysteine concentrations in a large, population-based, double-blind trial of folic acid supplementation. Am J Clin Nutr 2011;93:1365–72. 10.3945/ajcn.110.004671 [DOI] [PubMed] [Google Scholar]
- 28.Yadav U, Kumar P, Gupta S, et al. Distribution of MTHFR C677T Gene Polymorphism in Healthy North Indian Population and an Updated Meta-analysis. Indian J Clin Biochem 2017;32:399–410. 10.1007/s12291-016-0619-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yafei W, Lijun P, Jinfeng W, et al. Is the prevalence of MTHFR C677T polymorphism associated with ultraviolet radiation in Eurasia? J Hum Genet 2012;57:780–6. 10.1038/jhg.2012.113 [DOI] [PubMed] [Google Scholar]
- 30.Henderson AM, Aleliunas RE, Loh SP, et al. l-5-Methyltetrahydrofolate supplementation increases blood folate concentrations to a greater extent than folic acid supplementation in Malaysian women. J Nutr 2018;148:885–90. 10.1093/jn/nxy057 [DOI] [PubMed] [Google Scholar]
- 31.De Wals P, Tairou F, Van Allen MI, et al. Reduction in neural-tube defects after folic acid fortification in Canada. N Engl J Med 2007;357:135–42. 10.1056/NEJMoa067103 [DOI] [PubMed] [Google Scholar]
- 32.Williams J, Mai CT, Mulinare J, et al. Updated estimates of neural tube defects prevented by mandatory folic Acid fortification - United States, 1995-2011. MMWR Morb Mortal Wkly Rep 2015;64:1–5. [PMC free article] [PubMed] [Google Scholar]
- 33.Colapinto CK, Tremblay MS, Aufreiter S, et al. The direction of the difference between Canadian and American erythrocyte folate concentrations is dependent on the assay method employed: a comparison of the Canadian health measures survey and national health and nutrition examination survey. Br J Nutr 2014;112:1873–81. 10.1017/S0007114514002906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martínez de Villarreal L, Pérez JZV, Vázquez PA, et al. Decline of neural tube defects cases after a folic acid campaign in Nuevo León, México. Teratology 2002;66:249–56. 10.1002/tera.10094 [DOI] [PubMed] [Google Scholar]
- 35.Houghton LA, Gray AR, Rose MC, et al. Long-Term effect of low-dose folic acid intake: potential effect of mandatory fortification on the prevention of neural tube defects. Am J Clin Nutr 2011;94:136–41. 10.3945/ajcn.110.004549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.da Silva VR, Hausman DB, Kauwell GPA, et al. Obesity affects short-term folate pharmacokinetics in women of childbearing age. Int J Obes 2013;37:1608–10. 10.1038/ijo.2013.41 [DOI] [PubMed] [Google Scholar]
- 37.Stern SJ, Matok I, Kapur B, et al. A comparison of folic acid pharmacokinetics in obese and nonobese women of childbearing age. Ther Drug Monit 2011;33:336–40. 10.1097/FTD.0b013e318219407a [DOI] [PubMed] [Google Scholar]
- 38.Tinker SC, Hamner HC, Berry RJ, et al. Does obesity modify the association of supplemental folic acid with folate status among nonpregnant women of childbearing age in the United States? Birth Defects Res A Clin Mol Teratol 2012;94:749–55. 10.1002/bdra.23024 [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization Western Pacific Region Weekly iron and folic acid supplementation programmes for women of reproductive age: an analysis of best programme practices. Geneva: World Health Organization, 2011. [Google Scholar]
- 40.World Health Organization Weekly iron and folic acid supplementation as an anaemia-prevention strategy in women and adolescent girls: lessons learnt from implementation of programmes among non–pregnant women of reproductive age. Geneva: World Health Organization, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-003897supp001.pdf (81.1KB, pdf)