Abstract
Objectives:
Developmental coordination disorder (DCD) compromises bone health purportedly due to lower levels of physical activity. The potential of an exercise intervention to improve bone health parameters in adolescents with DCD has not previously been studied. This study thus aimed to determine the impact of a multimodal exercise intervention on bone health in this population at-risk of secondary osteoporosis.
Methods:
Twenty-eight adolescents (17 male, 11 female) aged between 12-17 years (Mage=14.1) with DCD participated in a twice weekly, 13-week generalised multimodal exercise intervention. Peripheral quantitative computed tomography scans of the tibia (4% and 66%) were performed over a six month period. Generalised estimating equations were used to examine the impact of fitness measures on bone parameters over time.
Results:
An overall improvement trend was observed for bone health, with significant increases at the 66% tibial site for bone mass (4.12% increase, dcohen=0.23, p=0.010) and cortical area (5.42% increase, η2 =12.09, p=0.014). Lower body fitness measures were significantly associated with improvements in bone health parameters, tempered by the degree of motor impairment.
Conclusion:
A multimodal exercise intervention may be effective in improving bone health of adolescents with DCD. Given the impact of motor impairments, gains may be greater over an extended period of study.
Keywords: Bone Health, Developmental Coordination Disorder, Developmental Disorder, Exercise, Physical Activity
Introduction
Developmental Coordination Disorder (DCD) is a neurodevelopmental disorder typified by the slow acquisition and poor performance of motor skills across an individual’s lifespan[1]. Persons with DCD tend to have low levels of physical activity[2-4] which has been purportedly linked to detrimental bone health[5], including bone health impairments[6-10] and increased rates of fracture[6,11] placing them at risk of osteoporotic fractures later in life. Furthermore, suboptimal bone health is not just a consequence of reduced overall physical activity in paediatric DCD populations, but also from a lack of diversity in activities engaged[7], such that paediatric DCD populations appear to benefit most from physical activity that is diverse and intense[12]. As diverse mechanical loading modalities, methods, and intensity are known to be an essential part of all osteogenic activities[13] it is likely that a similar association between incidental physical activity and prescribed exercise with bone-specific outcomes also applies to adolescent and adult DCD populations, however this has not as yet been established. Furthermore, while physical activity (i.e. incidental and/or nonspecific activities requiring bodily movement) appears to improve bone health in DCD populations, exercise (i.e. purposeful, prescriptive, programmed and progressive activities targeting physiological outcomes) is likely to produce even greater benefits[13].
No studies, to our knowledge, have investigated the relationship between physical activity or exercise and bone health in adolescents with DCD. Weight bearing activity is known to have a particularly strong osteogenic effect during the early to mid-puberty time frame due to the velocity of bone growth and endocrine changes seen at this age[14,15] with significant improvements noted in bone health from a broad range of exercise interventions within adolescent populations[16-20]. Exercise interventions are known to be particularly effective in populations who are relatively inactive[21], with a substantial benefit anticipated for the typically inactive DCD population[2-4]. The benefits of exercise interventions in this age group, however, are heavily influenced by the types of activities or exercise modalities used[16,17,22]. Given the difficulties of motor skill acquisition and performance inefficiency inherent with DCD[1,23] it is likely there will be specific challenges concerning the implementation of prescribed exercise interventions in DCD populations. Thus, it is not yet known whether adolescents with DCD can engage in exercise interventions to a degree that would induce improvements in muscle and bone parameters. Indeed, to have an osteogenic effect, physical activity and/or exercise is required to be frequent, with a variety of different loading types, and be progressive through increasing magnitudes and rates of loading[13]. However, as individuals with DCD have a slower rate of mastering movements and a lower level of engagement in physical activity[24] such effects may be impeded. Accordingly, this study examined whether participating in a multimodal exercise intervention designed to address the general needs of adolescents with DCD, shown to improve the physical fitness[25] and self-perception of physical abilities among adolescents with DCD[26], would also have the capacity to produce improvements in bone health parameters.
Materials and methods
Experimental Design
A longitudinal, single-cohort study design was used to explore the feasibility and preliminary efficacy of a 13-week exercise program in adolescents with DCD to improve tibial bone health outcomes. All participants attended two testing sessions, six months apart, for anthropometry and lower-limb muscle bone morphology, with the first session taking place immediately prior to the commencement of the exercise program. Participants attended the local tertiary paediatric hospital to have their anthropometry (height, weight and tibial length) and lower limb muscle-bone morphology measures taken. Lower limb fitness assessments and motor performance tests were performed at The University of Notre Dame Australia’s exercise clinic on the first and last session of the exercise intervention. Bone measurements were performed approximately three months following the completion of the exercise program to allow time for bone adaptation. Participants were also required to attend the exercise clinic two days per week throughout the program to complete their supervised exercise sessions.
Participants
Participants were recruited from the Adolescent Movement Program (AMPitup: www.movegrowengage.com.au/ampitup/), a research program providing an exercise intervention for adolescents with movement difficulties[4,25,26]. The program is aimed at adolescents aged 12 to 18 years with a reported history of movement difficulties below what would be expected for their age that has impacted upon their activities of daily living as per the diagnostic criteria for DCD[1]. Participants in the study are recruited through referral from allied health professionals (e.g. Occupational Therapists, Physiotherapists) or through word of mouth. All participants in the Adolescent Movement Program were offered the opportunity to participate in this bone health study. Participants whose movement difficulties did not occur early in the developmental period or were due to an intellectual or physical disability were excluded from this analysis in keeping with the diagnostic criteria for DCD[1]. As indicated in Figure 1, two participants were excluded for this reason, with another participant being excluded due to use of bone affecting medication for epilepsy. The study had ethics approval from the Human Research Ethics Committee of the University of Notre Dame Australia (Reference 011004F, 09004F, 09050F, 09039F) and written informed consent was provided by participants and their caregivers prior to participation. The study and its procedures conformed to the World Medical Associations’ Declaration of Helsinki for Medical Research Involving Human Subjects.
Figure 1.
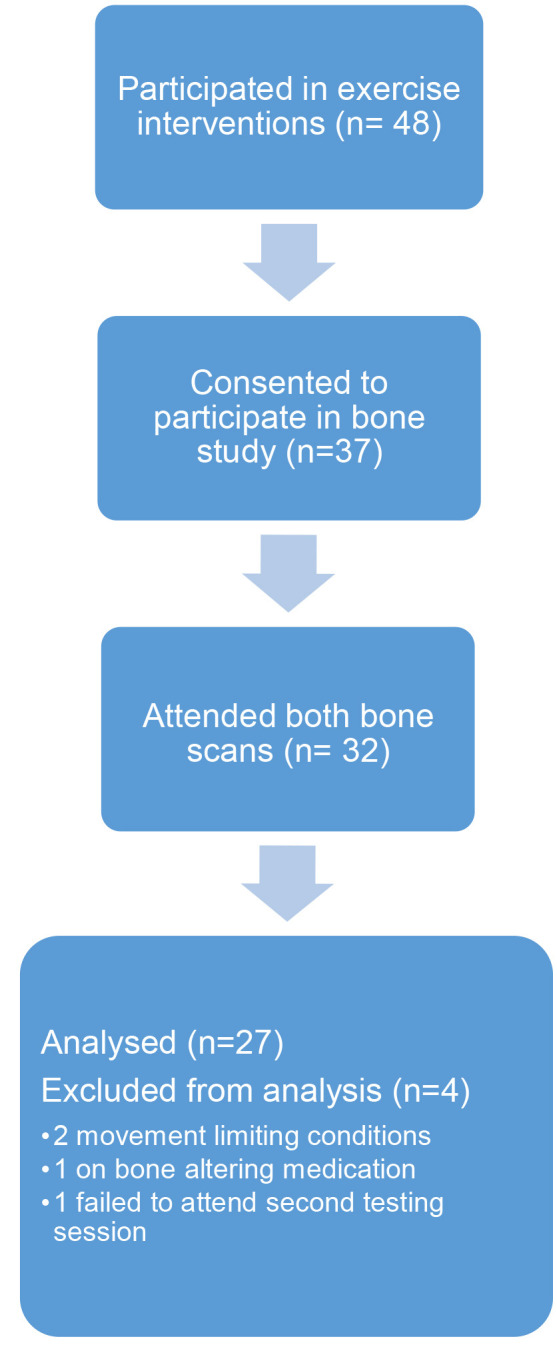
Inclusion of participants for bone health analysis.
Intervention
A multimodal exercise intervention was undertaken as part of the AMPitup program. Participants received individualised exercise training over thirteen weeks consisting of two 90-minute sessions per week after school, overseen by an accredited exercise physiologist (AEP; Exercise and Sport Science Australia) and clinically experienced academics. Each participant received one to one coaching from physiotherapy and exercise sport science undergraduate students, together with exercise physiology postgraduate students. The use of one to one coaching has been found to increase the participants engagement in the intervention[26] and also allows for individualised feedback on technique. Each participant had two assigned trainers through-out the intervention, one for each exercise session of the week, to encourage variability in exercise routines. The AMPitup program is general and broad in focus, thus activities are not explicitly targeting osteogenesis. All exercise sessions include a combination of aerobic training (cardiorespiratory fitness), resistance training (muscle and strength development) and other activities aimed at improving motor skills and balance. Stretching and flexibility activities, core strength, and postural exercises, were also included dependent on the participant’s individual fitness interests, goals and needs. Fitness games and group activities were often included to improve participant’s engagement and enjoyment of physical activity. A full list of activities used are included in Table 1. The volume and intensity of exercises were prescribed as recommended by Faigenbaum and colleagues[27], and Falk and Klentrou[28], relative to the participant’s physical abilities and fitness. Progression in sets, repetitions and weight occurred after proper technique was achieved as determined by the trainer[29].
Table 1.
List of activities performed by participants.
| Cardiovascular exercises | Core strength and flexibility | Motor and postural skills |
|---|---|---|
| • Arm ergometer • Bike • Boxing • Cross-trainer • Hula hooping • Mountain climbers • Rower • Running • Stair run • Step aerobics combinations • Walk |
• Abdominal crunch • Ball rollouts • Dead bugs • Farmers walk • Fitball knee tucks • Glute bridge • Heel slide • Hover • Leg lifts • Oblique leg slide • Oblique twist • Pilates Machine • Plank • Rotary torso • Stretches • Wheelbarrow |
• Balance on beam • Balance on bosu • Balance on one leg • Catching • Fitball balance on all fours • Heel-toe walk • Kicking • Obstacle course • Star excursion balance • Throwing over object • Throwing into bucket/bin/net • Throwing while balancing • Throwing while standing on one leg |
| Resistance training (for lower body) | Resistance training (general) | Plyometrics |
| • Bear crawls • Burpees • Calf raises • Chair sit to stand • Climbing frame • Heel press • Heel raises • Leg curl • Leg extension • Leg press • Leg raises • Lunges • Reverse leg curls • Side kicks • Squats • Travelling lunges • Tricep dip • Tricep extension |
• Arnold dumbbell press • Arm raises • Arm extension • Bridge • Back extension • Bent over barbell row • Bicep curl • Bicep extension • Cable pull down • Chest press • Chin ups • Deadlifts • Dead row • Dumbbell snatches • High pull • Kettlebell swings • Lateral pulldown • Lateral shoulder raise • Medicine ball passes • Medicine ball slam • Medicine ball twist • Overhead press • Pectoral fly • Pelvic lift • Pull up • Push press • Rope climbing • Seated cable row • Shoulder press • Shoulder shrug • Supine rows |
• Body weight jump squat • Bounding • Box jumps • Broad jumps • Hopping • Hopscotch • Horizontal jumps • Hurdles • Jump over board • Lateral jump • Side to side hops/jumps • Skipping • Star jumps • Toe taps • Vertical jump |
| Group and partner games | ||
|
• Baseball • Basketball • British bulldog • Circuit of park equipment • Dodgeball • Four square • Frisbee • Kick to kick • Piggy in the middle • Soccer • Tennis • Two square |
Measures
Musculoskeletal Morphology
Tibial scans were performed using peripheral Quantitative Computed Tomography (pQCT; Stratec XCT-3000, Stratec GmbH; slice thickness 2.3 mm, pixel size 0.4 × 0.4 mm) at proximal (66% of tibial length, T66) and distal (4% of tibial length, T4) sites of the tibia, of the non-dominant side as reported by the participant. Participants sat on a height-adjustable chair with their lower limb fully extended through the acrylic cylinder and central gantry of the pQCT machine and secured to the foothold attachment under the supervision of a trained bone densitometry hospital technician. A 30-mm scout scan was produced at the base of the malleolus in order to identify the talocrural joint, as an internal reference point from which the scan commenced to measure cross-sectional slices at 4% (T4) and 66% (T66) of tibial length. Scans per participant spanned approximately five minutes and were performed approximately six months (20.4 (8.4) weeks) after baseline testing; approximately three months following the completion of the 13-week exercise program. Following scan completion, total tibial mass (g/cm) and cross-sectional area (mm2) were assessed at both sites. In addition, total density (mg/cm3) and trabecular density (mg/cm3) were assessed at the T4 site, and cortical density(mg/cm3), cortical area (mm2), stress strain index (SSI, mm3), fracture load on the X and Y axis (N), muscle and fat cross-sectional area were assessed at T66. SSI and fracture load were used as surrogates for bone strength. To account for the absence of a concurrently assessed control group, Z-scores were calculated using height and sex-specific means and standard deviations from the Stratec reference database (Version 6.20, Stratec, Stratec GmbH)[30] using the formula:

where x is the individual value, μ is the sex and height specific mean and σ is the associated standard deviation.
Anthropometry
Stature was recorded to the nearest 0.1 cm using a wall-mounted stadiometer (Mentone Educational Centre), with body weight recorded to the nearest 0.1 kg using an electronic scale (Homedics). Tibial length of the non-dominant leg was assessed using a retractable measuring tape, defined as the tibial plateau at the knee joint (proximal end) to the medial malleolus (distal end), recorded to the nearest 0.1 cm. Body mass index (BMI) was subsequently calculated using weight (kg) / height (m)[2].
Pubertal Status
Pubertal status was assessed using the Pubertal Developmental Scale, a non-invasive self-report scale which covers five aspects of pubertal development including sex specific questions[31]. Items are scored on a scale of one to five, with five indicating a mature stage. The scale can be converted to correspond to five categories of pubertal development (Peterson et al 1998 in Bond et al[32]). Validity has been established against physical exams and self-report measures of puberty[31], with a Kappa concordance of 0.5 with self-reported Tanner stage[32]. Reliability has been established in rural and urban populations[33].
Motor Performance
Motor performance was assessed using the McCarron Assessment of Neuromuscular Development (MAND)[34] as part of the screening process for the AMPitup program. The MAND is a ten-item test designed for the assessment of gross and fine motor skills in adolescents and young adults. Scores from the ten items are scaled and summed to produce a Neuromuscular Developmental Index (NDI), with a mean of 100 and standard deviation of 15. Lower NDI scores indicate poorer performance of motor skills and as such a greater degree of motor impairment. A NDI of more than one standard deviation below the mean (85) was required in order to be eligible for participation in the intervention, however participants with a NDI above 85 were included if a substantial history of motor difficulties impacting on their daily life was reported. The MAND has a test-retest of 0.99 after one month and concurrent validity to a number of different motor skill tests[34].
Lower Limb Fitness Measures
Lower limb fitness was measured using three assessments: the standing broad jump, vertical jump and a 1 repetition maximum (1RM) leg press. All measures are reliable forms of evaluation of lower limb fitness validated under similar conditions to their use in this study. The standing broad jump has an intraclass correlation coefficients (ICC) from test-retest of 0.98 in an adolescent population[35], while the vertical jump, as measured by the Vertec system, has an 0.91 ICC in college aged females (Mage=19.5, SD=1.3), and 0.94 in college aged males (Mage=19.7, SD=1.5)[36]. The 1 RM leg press has an test-retest ICC of 0.95 in college aged athletes (Mage=18.9, SD =1.2)[37] and 0.99 in untrained adults[38]. The measures were taken for each participant at the first and last session of the thirteen-week exercise intervention. The standing broad jump was measured as the horizontal distance achieved by the participant jumping forwards from a standing stationary position, by drawing a line behind their heels following the landing point. Each participant had three attempts with the best achieved jump being recorded in inches (in)[34]. The vertical jump was measured as the maximum vertical height achieved in a standing jump (Vertec, Sports Imports, Hilliard) by determining the difference in the number of vanes between the participant’s standing reach and jump reach at peak height. Vanes are spaced 1.27 cm apart with vertical jump height in centimetres calculated as the number of vanes multiplied by 1.27. Each participant was provided with multiple attempts with short rests of about a minute until a plateau in performance was observed, with the best achieved jump retained for analysis[25]. Leg strength was assessed using 1RM leg press, recording the maximum weight that could be lifted through a full range of motion in kilograms (kg). Failure was defined as an incomplete range of motion through execution, or an inability to lift the weight in two attempts[39]. Due to technical specifications of the leg press machine, increase of weight was in 5 kg increments. Fitness procedures were performed in the same set pattern for all participants with the 1RM leg press being performed last.
Statistical analysis
All statistical calculations, except effect sizes, were completed using SPSS[40]. Effect sizes were calculated using Psychometrica online calculator[41]. Normality of data distribution was explored using a Shapiro-Wilk test. Full statistical analysis was performed for bone measurements in both the raw data and Z-scores. Baseline and post intervention differences in bone parameters and fitness assessments were explored using paired sample t-tests for parametric variables or Wilcoxon signed rank tests for non-parametric variables. Effect sizes were calculated using Cohen’s d for parametric variables and eta squared for non-parametric variables. Sex differences for bone parameters, fitness measures, and descriptive characteristics were determined via independent t-tests for parametric variables and Mann Whitney U tests for non-parametric variables. Generalised estimating equations (GEE) were used to identify determinants of bone parameters. Sex, puberty score, age, height, and weight were included in the GEE model as they were considered likely influencers of improvements in bone health in this age group. Physical fitness measures were included in order to evaluate the impact of the intervention. Separate GEE models were performed including age[2] to assess for the effects of growth but did not substantially alter the results (Supplementary Tables), and due to sample size the more simple model was retained and reported. As participants who had prior fitness intervention exposure were included in the sample, a sensitivity analysis was conducted to determine any differences in baseline bone parameters and fitness measures as well as differences in changes over the course of the intervention. The impact of age between the intervention groups was explored using a two-way between groups analysis of variance. Alpha of <0.05 was considered statistically significant. Sample size was not formally calculated as participation in the bone health study was offered to all participants of AMPItUp. The program is limited to a maximum of 25 participants per semester for accommodation purposes[26].
Results
Baseline
The sample comprised 28 participants, 17 male and 11 female, ranging in age between 12.57 and 17.59 years with a mean age of 14.06 (SD=1.28) years. The mean pubertal score was 6.41 (SD=1.78) with conversion of pubertal scores to categories indicating that the majority (92.9%) were in a mid or post-pubertal stage. Fourteen participants were mid-pubertal, 12 were post-pubertal and two were pre-pubertal. Four participants (14.8%) changed pubertal category over the course of the intervention, two moved from pre-pubertal to mid-pubertal and two moved from mid-pubertal to post-pubertal. There were no statistically significant differences between sexes for age, puberty score, height, weight, BMI or NDI. Baseline descriptive characteristics of the sample are presented in Table 2. Eleven participants had taken part in the 13-week intervention program at least once prior to bone parameter measurements being taken. Prior participants had completed between one and five programs, with a mean prior attendance of 2.18 (SD=1.11) programs.
Table 2.
Descriptive characteristics of the total sample, males and females.
| Characteristic | Total Sample (n=28) | Male (n=17) | Female (n=11) | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Age (years) | 14.06 | 1.28 | 13.98 | 0.92 | 14.18 | 1.75 |
| Height (cm) | 163.81 | 10.55 | 163.86 | 9.97 | 163.74 | 11.89 |
| Weight (kg) | 61.40 | 14.94 | 61.11 | 16.15 | 61.85 | 13.59 |
| Puberty score | 6.41 | 1.78 | 6.35 | 2.03 | 6.50 | 1.35 |
| NDI | 66.29 | 17.90 | 68.12 | 17.94 | 63.45 | 18.34 |
Baseline measurements of bone parameters indicated a deficit in bone health with Z-scores indicating the deficit was also present when compared to sex and heighted matched norms (Table 3). The 11 participants who had previously taken part in the fitness intervention (intervention-experienced participants) had higher baseline parameters on all measurements of bone health than those who had never previously taken part (intervention-naïve participants). The differences between groups based on prior intervention engagement were statistically significant for all bone health parameters except total area (T4 and T66), fracture load on the Y-axis (Y3N), trabecular density and the Z-scores for SSI and cortical density. Fitness parameters, however, were not significantly different between groups based on prior participation status, apart from the 1RM leg press which was significantly higher in the intervention-experienced group (61.81% increase, dcohen=1.35, t=-3.01, p=0.008). All baseline measurements for both groups are presented in Tables 3 and 4.
Table 3.
Intervention group difference.
| Intervention-Naive (n=17) | Intervention – Experienced (n=11) | |||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | dcohen | d 95% Confidence Interval | T test | P- value | |
| Age (years) | 13.38 | 0.53 | 15.11 | 1.40 | 12.13b | -3.62a | *<0.001 | |
| Height (cm) | 161.27 | 11.39 | 167.73 | 8.07 | 0.25 | -0.28 to 0.78 | 1.63 | 0.116 |
| Weight (kg) | 57.88 | 13.66 | 66.84 | 15.82 | 12.10b | 1.53a | 0.134 | |
| T4 | ||||||||
| Mass (g/cm) | 2.87 | 0.52 | 3.54 | 0.61 | 1.18 | 0.61 to 1.75 | -3.14 | *0.004 |
| Total area (mm2) | 1100.74 | 164.81 | 1211.21 | 199.90 | 0.60 | 0.07 to 1.14 | -1.59 | 0.123 |
| Total density (mg/cm3) | 261.19 | 29.28 | 293.55 | 24.20 | 4.93 | 3.88 to 5.98 | -3.05 | *0.005 |
| Trabecular density (mg/cm3) | 224.86 | 35.50 | 249.75 | 22.18 | 0.84 | 0.29 to 1.39 | -2.07 | *0.048 |
| Trabecular density Z-score | 0.38 | 1.58 | 0.25 | 1.05 | -0.10 | -0.62 to 0.43 | -1.28 | 0.212 |
| T66 | ||||||||
| Mass (g/cm) | 2.88 | 0.52 | 3.57 | 0.49 | 1.37 | 0.78 to 1.95 | -3.56 | *0.001 |
| Total area (mm2) | 616.58 | 161.00 | 612.00 | 122.12 | 12.11b | -0.21a | 0.853 | |
| Cortical density (mg/cm3) | 1022.87 | 49.65 | 1061.69 | 44.79 | 12.12b | -2.19a | *0.029 | |
| Cortical area (mm2) | 207.11 | 58.15 | 278.50 | 36.68 | 12.13b | -3.65a | *<0.001 | |
| SSI (mm3) | 1639.67 | 323.05 | 1910.04 | 374.69 | 0.77 | 0.23 to 1.32 | -2.03 | 0.050 |
| Fracture load X3N | 4112.75 | 883.31 | 5038.25 | 1188.45 | 0.88 | 0.34 to 1.43 | -2.36 | *0.026 |
| Fracture load Y3N | 3215.80 | 765.04 | 3540.28 | 727.05 | 0.44 | -0.10 to 0.97 | -1.12 | 0.274 |
| Cortical density Z-score | -0.33 | 1.44 | 0.45 | 0.87 | 0.66 | 0.12 to 1.19 | -1.79 | 0.084 |
| Cortical area Z-score | -1.72 | 1.72 | -0.25 | 1.11 | 1.02 | 0.46 to 1.57 | -2.75 | *0.011 |
| SSI Z-score | -0.71 | 1.00 | -0.52 | 0.95 | 0.20 | -0.33 to 0.72 | -0.50 | 0.619 |
| Fitness parameters | ||||||||
| 1 RM leg press (kg) | 59.33 | 20.17 | 96.00 | 32.86 | 1.35 | 0.77 to 1.93 | -3.01 | *0.008 |
| Vertical jump (cm) | 33.39 | 11.59 | 34.52 | 7.78 | 0.11 | -0.41 to 0.64 | -0.28 | 0.779 |
| Standing broad jump (in) | 41.71 | 15.50 | 47.00 | 15.13 | 0.35 | -0.18 to 0.87 | -0.89 | 0.381 |
=Mann-Whitney U test standardized test statistic,
=eta squared
Table 4.
Pre-post group difference on fitness measures.
| Baseline | Post-intervention | |||||||
|---|---|---|---|---|---|---|---|---|
| Fitness measure | M | SD | M | SD | dcohen | d 95% Confidence Interval | T-test statistic | P-value |
| 1 RM leg press (kg) | 68.50 | 28.14 | 83.00 | 26.77 | 0.53 | -0.01 to 1.06 | -3.68 | *0.002 |
| Standing broad jump (in) | 43.79 | 15.30 | 46.14 | 15.10 | 0.16 | -0.37 to 0.68 | -2.74 | *0.011 |
| Vertical jump (cm) | 33.84 | 10.11 | 35.61 | 12.60 | 0.16 | -0.37 to 0.68 | -1.21 | 0.235 |
As the intervention-experienced participants were significantly older (15.11 years compared to 13.38 years respectively) (η[2]=12.13, t=-3.62, p<0.001), a two-way between groups analysis of variance was conducted in order to explore the impact of prior intervention and age. The interaction effect between age and intervention status was not statistically significant for any variable. There was a statistically significant main effect for age only for fracture load F(5,20)=3.26, p=0.026, ηp[2] =0.45. A statistically significant main effect for intervention was found only for T4 trabecular density score, F(1,15)=5.34, p=0.025, partial eta squared=0.26.
Intervention
Participants attended between 15 through to 25 out of a possible 26 sessions during the 13-week intervention, with a median attendance of 22 sessions (95% CI 20.58 -22.63). All fitness measures improved on average over the course of the intervention; 1RM leg press increased by 21.1% (dcohen=0.53, p=0.002), standing broad jump by 5.36% (dcohen=0.16, p=0.011), and vertical jump by 5.23% (dcohen=0.16, p=0.235) (Table 4).
An improvement trend in bone health measurements was observed over the course of the 13 week intervention, with a statistically significant increase present for T66 measurements for bone mass (4.12% increase, dcohen=0.23, t=-2.75, p=0.010) and cortical area (5.42% increase, η[2]=12.09, t=2.45, p=0.014). A sensitivity analysis to limit analyses to only intervention-naïve participants indicated similar results for bone health parameters, except for the change in T66 mass which was no longer statistically significant (p=0.065). Non-statistically significant improvements were seen in the Z-scores for cortical area and cortical density. All pQCT measurements, prior and post-intervention, are shown in Table 5.
Table 5.
Pre-post group difference on pQCT bone health parameters.
| Baseline | Post-intervention | |||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | dcohen | d 95% Confidence Interval | T-test statistic | P-value | |
| Age (years) | 14.06 | 1.28 | 14.45 | 1.25 | 12.07b | 4.62a | *<0.001 | |
| Height (cm) | 163.81 | 10.55 | 165.89 | 10.05 | 0.20 | -0.32 to 0.73 | -0.75 | 0.454 |
| Weight (kg) | 61.40 | 14.94 | 63.75 | 14.78 | 12.10b | 0.64a | 0.523 | |
| Fat/Muscle area ratio | 60.75 | 42.29 | 35.16 | 2.08 | -0.86 | -1.40 to -0.31 | 0.90 | 0.534 |
| Bone/Muscle area ratio | 40.72 | 52.86 | 35.11 | 42.19 | -0.12 | -0.64 to 0.41 | 1.07 | 0.363 |
| T4 | ||||||||
| Mass (g/cm) | 3.14 | 0.64 | 3.17 | 0.58 | 0.05 | -0.48 to 0.57 | -0.46 | 0.647 |
| Total area (mm2) | 1144.14 | 184.16 | 1159.49 | 178.54 | 0.09 | -0.44 to 0.61 | -0.69 | 0.497 |
| Total density (mg/cm3) | 273.89 | 31.37 | 273.79 | 34.48 | 0.00 | -0.53 to 0.52 | 0.03 | 0.976 |
| Trabecular density Z- score | -0.13 | 1.41 | -0.65 | 2.16 | -0.29 | -0.81 to 0.24 | 1.07 | 0.290 |
| T66 | ||||||||
| Mass (g/cm) | 3.15 | 0.61 | 3.28 | 0.53 | 0.23 | -0.30 to 0.75 | -2.75 | *0.010 |
| Cortical area (mm2) | 235.15 | 61.35 | 247.89 | 47.49 | 12.09b | 2.45a | *0.014 | |
| Total area (mm2) | 614.78 | 144.53 | 595.00 | 103.56 | 12.10b | 0.48a | 0.633 | |
| Cortical density (mg/cm3) | 1038.12 | 50.76 | 1049.26 | 38.45 | 0.25 | -0.28 to 0.77 | -0.93 | 0.359 |
| SSI (mm3) | 1745.89 | 363.21 | 1745.31 | 478.77 | 0.00 | -0.53 to 0.52 | 0.01 | 0.992 |
| Fracture load X3N | 4476.34 | 1094.24 | 4609.13 | 1312.96 | 0.11 | -0.41 to 0.63 | -1.31 | 0.202 |
| Fracture load Y3N | 3343.28 | 754.31 | 3230.69 | 853.56 | -0.14 | -0.66 to 0.39 | 0.93 | 0.363 |
| Cortical area Z-score | -1.14 | 1.66 | -0.96 | 1.18 | 0.13 | -0.40 to 0.65 | -0.47 | 0.638 |
| Cortical density Z-score | -0.03 | 1.29 | 0.18 | 0.86 | 0.19 | -0.33 to 0.72 | -0.69 | 0.495 |
| SSI Z-score | -0.64 | 0.97 | -0.81 | 1.13 | -0.16 | -0.69 to 0.36 | 0.61 | 0.546 |
| Cortical area to total area ratio | 21.43 | 5.99 | 22.55 | 5.09 | 0.20 | -0.32 to 0.73 | -1.86 | 0.071 |
=Related samples Wilcoxon signed rank test,
=eta squared.
GEE modelling indicated that the improvement in T4 total area became statistically significant when the effect of sex, puberty score, age, height, weight, degree of motor impairment, and improvement in lower fitness measures was accounted for (β=-54.02, p=0.017). A statistically significant influence was found in the model for sex (β=116.94, p=0.007), height (β=6.29, p=0.014), and NDI score (β=2.29, p=0.044), with vertical jump measurements not statistically significant (β=6.69, p=0.060). The model was such that T4 total area increased as height and vertical jump performance increased, improvements were greater for those with a lower degree of motor impairment as measured by NDI, and for males compared to females. Vertical jump also had a statistically significant impact in the model for T66 cortical area (β=2.01, p=0.043) and T66 cortical area Z score (β=0.02, p=0.037). The only other fitness measure that had a statistically significant impact on any model was 1RM leg press in the model for T66 cortical density (β=0.56, p=0.015), and cortical density Z score (β=0.02, p=0.037) as well as a negative impact on fracture load on the Y axis (β=-13.51, p=0.033). The degree of motor impairment as indicated by NDI was a statistically significant influencer in some of the models (T4 total area, total density, trabecular density, and trabecular density Z score; T66 mass) with the direction of influence varying between models. A positive association was found such that bone gains increased as NDI score increased (motor impairment decreased) in T4 total area (β=2.29, p=0.044) and T66 mass (β=0.01, p=0.044) and a negative association such that bone gains decreased as NDI score decreased (motor impairment increased) in T4 total density (β=-0.64, p=0.044), T4 trabecular density (β=-0.69, p=.028) and T4 trabecular density Z score (β=-0.04, p=0.049). Growth as indicated by age, height and weight were found to be statistically significant influences in only some of the models (T4 trabecular density, T4 trabecular density Z-score, T66 mass and T66 cortical area; T4 total area; T4 total density, T4 trabecular density and T4 trabecular density Z-score) as was sex (T4 total area, T66 mass, T66 cortical density and fracture load X3N respectively). The increase in bone mass for both T66 mass and cortical area ceased to be statistically significant after controlling for confounders. GEE models for parameters found to have a statistically significant effect in pre and post modelling, as well as models for Z-scores, are presented in Table 6 with results for all GEE models presented as appendices one, two and three.
Table 6.
GEE modelling showing relationships between changes in bone health and potential mediators.
| β Estimate | SE | β 95% Confidence interval | p-value | |
|---|---|---|---|---|
| T4 Total area | ||||
| Pre/posta | -54.02 | 22.68 | -98.47 to -9.57 | *0.017 |
| Sexb | 116.94 | 43.42 | 31.84 to 202.04 | *0.007 |
| Puberty score | -23.64 | 15.15 | -53.34 to 6.06 | 0.119 |
| Age | 20.28 | 39.61 | -57.36 to 97.91 | 0.609 |
| Height | 6.29 | 2.56 | 1.29 to 11.31 | *0.014 |
| Weight | -1.23 | 2.26 | -5.66 to 3.21 | 0.587 |
| 1 RM leg press | -1.09 | 0.83 | -2.72 to 0.53 | 0.188 |
| Vertical jump | 6.69 | 3.57 | -0.29 to 13.69 | 0.060 |
| Standing broad jump | -4.14 | 3.87 | -11.72 to 3.44 | 0.285 |
| NDI | 2.29 | 1.14 | 0.06 to 4.53 | *0.044 |
| T66 Mass | ||||
| Pre/posta | -0.02 | 0.08 | -0.18 to 0.14 | 0.783 |
| Sexb | -0.40 | 0.17 | -0.74 to -0.07 | *0.019 |
| Puberty score | 0.00 | 0.06 | -0.13 to 0.12 | 0.949 |
| Age | 0.58 | 0.17 | 0.25 to 0.91 | *<0.001 |
| Height | -0.01 | 0.01 | - 0.03 to 0.01 | 0.281 |
| Weight | 0.01 | 0.01 | -0.01 to 0.03 | 0.357 |
| 1 RM leg press | -0.01 | 0.004 | -0.01 to 0.00 | 0.137 |
| Vertical jump | 0.01 | 0.01 | -0.01 to 0.03 | 0.373 |
| Standing broad jump | -0.01 | 0.01 | -0.03 to 0.01 | 0.302 |
| NDI | 0.01 | 0.01 | 0.00 to 0.02 | *0.044 |
| T66 Cortical area | ||||
| Pre/posta | -3.38 | 9.50 | -21.99 to 15.24 | 0.722 |
| Sexb | -27.19 | 16.82 | -60.17 to 5.78 | 0.106 |
| Puberty score | -2.48 | 7.70 | -17.57 to 12.62 | 0.748 |
| Age | 34.23 | 15.72 | 3.41 to 65.04 | *0.029 |
| Height | 0.60 | 1.16 | -1.68 to 2.88 | 0.607 |
| Weight | 0.66 | 0.92 | -1.14 to 2.46 | 0.473 |
| 1 RM leg press | -0.21 | 0.36 | -0.91 to 0.49 | 0.557 |
| Vertical jump | 2.01 | 0.99 | 0.06 to 3.95 | *0.043 |
| Standing broad jump | -0.71 | 0.77 | -2.24 to 0.81 | 0.359 |
| NDI | 0.53 | 0.59 | -0.62 to 1.69 | 0.366 |
| T4 Trabecular density Z score | ||||
| Pre/Posta | 0.72 | 0.81 | -0.87 to 2.32 | 0.374 |
| Puberty score | -0.28 | 0.22 | -0.70 to 0.14 | 0.190 |
| Age | -0.83 | 0.40 | -1.61 to -0.04 | *0.039 |
| Weight | 0.05 | 0.02 | 0.01 to 0.09 | *0.016 |
| 1 RM leg press | 0.03 | 0.02 | -0.01 to 0.06 | 0.105 |
| Vertical jump | 0.07 | 0.06 | -0.06 to 0.19 | 0.304 |
| Standing broad jump | 0.00 | 0.03 | -0.06 to 0.06 | 0.997 |
| NDI | -0.04 | 0.02 | -0.08 to 0.00 | *0.049 |
| T66 Cortical density Z score | ||||
| Pre/posta | -0.06 | 0.27 | -0.58 to 0.47 | 0.835 |
| Puberty score | 0.02 | 0.14 | -0.26 to 0.31 | 0.869 |
| Age | -0.06 | 0.26 | -0.46 to 0.57 | 0.831 |
| Weight | -0.02 | 0.02 | -0.06 to 0.02 | 0.335 |
| 1 RM leg press | 0.02 | 0.01 | 0.001 to 0.03 | *0.037 |
| Vertical jump | 0.03 | 0.04 | -0.04 to 0.10 | 0.382 |
| Standing broad jump | 0.01 | 0.02 | -0.03 to 0.06 | 0.635 |
| NDI | -0.02 | 0.01 | -0.04 to 0.01 | 0.246 |
| T66 Cortical area Z score | ||||
| Pre/Posta | -0.16 | 0.31 | -0.77 to 0.45 | 0.613 |
| Puberty score | -0.08 | 0.26 | -0.58 to 0.43 | 0.764 |
| Age | 0.16 | 0.52 | -0.86 to 1.18 | 0.758 |
| Weight | 0.02 | 0.03 | -0.04 to 0.08 | 0.597 |
| 1 RM leg press | 0.01 | 0.01 | -0.02 to 0.03 | 0.655 |
| Vertical jump | 0.07 | 0.04 | -0.01 to 0.14 | 0.081 |
| Standing broad jump | -0.02 | 0.03 | -0.07 to 0.03 | 0.467 |
| NDI | 0.01 | 0.02 | -0.03 to 0.05 | 0.736 |
| T66 SSI Z score | ||||
| Pre/Posta | 0.28 | 0.22 | -1.04 to 0.35 | 0.203 |
| Puberty score | 0.04 | 0.17 | 0.30 to 0.38 | 0.824 |
| Age | -0.35 | 0.35 | -1.04 to 0.35 | 0.327 |
| Weight | 0.02 | 0.02 | -0.02 to 0.06 | 0.270 |
| 1 RM leg press | 0.00 | 0.01 | -0.02 to 0.02 | 0.804 |
| Vertical jump | 0.03 | 0.03 | -0.03 to 0.09 | 0.290 |
| Standing broad jump | 0.00 | 0.02 | -0.05 to 0.05 | 0.998 |
| NDI | 0.00 | 0.02 | -0.03 to 0.03 | 0.909 |
Where pre-intervention is the comparison group and β=1;
Where male is the comparison group and β=1; SE=standard error.
A sensitivity analysis of only intervention-naïve participants found that the changes in T66 total area (β=168.54, p=0.013), SSI (β=164.65, p=0.024), and fracture load X3N and Y3N (β=369.08, p=0.025; β=590.86, p=0.022) became statistically significant when the effect of other variables was controlled for statistically. The models for these parameters as well as T66 mass, T66 cortical area, and all Z scores are presented in Table 7, GEE models for other variables are presented in appendix three. Fitness measures in this group were implicated in more models than when intervention-experienced participants were included. Vertical jump was implicated in T4 mass (β=0.03, p=0.002), T4 total area (β=9.46, p=0.015), T4 trabecular density (β=1.77, p=0.030), T66 total area (β=-9.43, p=0.002), T66 cortical area (β=2.80, p=0.006), T66 cortical area Z-score (β=0.07, p=0.034) and an effect nearing significance in T66 cortical density (β=2.89, p=.067); 1RM leg press in T4 total area (β=-2.28, p=0.038) and T66 total area (β=2.70, p=0.011); and standing broad jump showed a statistically significant influence in T4 total density (β=1.04, p=0.033). NDI, however, had a primarily negative effect in modelling for this sample with bone gains decreasing as motor impairment decreased in models for T4 total density (β=-0.91, p<0.001), T4 trabecular density (β=-1.04, p=0.001), T66 cortical density (β=-1.03, p=0.023), T4 trabecular density Z-score (β=-0.05, p=0.010) and T66 cortical density Z-score (β=-0.03, p=0.038) while a positive effect was seen only for T66 total area (β=3.39, p<0.001).
Table 7.
GEE modelling showing relationships between changes in bone health and potential mediators for intervention-naive participants only.
| β Estimate | SE | β 95% Confidence interval | p-value | |
|---|---|---|---|---|
| T66 Mass | ||||
| Pre/posta | -0.07 | 2.73 | -9.61 to 1.09 | 0.119 |
| Sexb | -0.42 | 0.15 | -0.72 to -0.12 | *0.005 |
| Puberty score | -0.04 | 0.07 | -0.18 to 0.10 | 0.579 |
| Age | 0.67 | 0.29 | 0.09 to 1.24 | *0.022 |
| Height | -0.02 | 0.01 | - 0.03 to 0.002 | 0.090 |
| Weight | 0.02 | 0.01 | 0.002 to 0.03 | *0.022 |
| 1 RM leg press | -0.01 | 0.01 | -0.02 to 0.00 | 0.130 |
| Vertical jump | 0.01 | 0.01 | -0.02 to 0.03 | 0.588 |
| Standing broad jump | 0.00 | 0.01 | -0.02 to 0.02 | 0.864 |
| NDI | 0.01 | 0.05 | 0.00 to 0.02 | 0.079 |
| T66 Total area | ||||
| Pre/Posta | 168.54 | 67.93 | 35.40 to 301.69 | *0.013 |
| Sexb | 70.55 | 36.58 | -1.15 to 142.25 | 0.054 |
| Puberty score | -14.01 | 23.37 | -59.82 to 31.81 | 0.549 |
| Age | 136.09 | 53.60 | 31.04 to 241.14 | *0.011 |
| Height | -0.77 | 1.31 | -3.34 to 1.80 | 0.555 |
| Weight | -0.51 | 1.87 | -4.18 to 3.16 | 0.785 |
| 1 RM leg press | 2.70 | 1.07 | 0.61 to 4.79 | *0.011 |
| Vertical jump | -9.43 | 2.30 | -15.31 to -3.56 | *0.002 |
| Standing broad jump | -0.94 | 1.45 | -3.78 to 1.90 | 0.516 |
| NDI | 3.39 | 0.80 | 1.82 to 4.95 | *<0.001 |
| T66 Cortical area | ||||
| Pre/posta | -27.02 | 19.80 | -65.84 to 15.96 | 0.799 |
| Sexb | -26.41 | 14.30 | -54.43 to 1.62 | 0.065 |
| Puberty score | -2.39 | 9.36 | -20.73 to 15.96 | 0.799 |
| Age | 16.62 | 32.85 | -47.76 to 81.00 | 0.613 |
| Height | 0.38 | 0.99 | -1.56 to 2.32 | 0.699 |
| Weight | 1.79 | 0.71 | 0.39 to 3.18 | *0.012 |
| 1 RM leg press | -0.61 | 0.56 | -1.70 to 0.48 | 0.274 |
| Vertical jump | 2.80 | 1.03 | 0.79 to 4.81 | *0.006 |
| Standing broad jump | 0.12 | 0.80 | -1.37 to 1.62 | 0.874 |
| NDI | 0.57 | 0.50 | -0.93 to 1.04 | 0.910 |
| T66 SSI | ||||
| Pre/Posta | 164.65 | 79.93 | 22.72 to 307.59 | *0.024 |
| Sexb | 63.19 | 144.82 | -220.65 to 347.02 | 0.663 |
| Puberty score | 32.82 | 46.83 | -58.97 to 124.60 | 0.483 |
| Age | 27.16 | 239.47 | -442.20 to 496.51 | 0.910 |
| Height | 9.96 | 8.20 | -6.12 to 26.04 | 0.225 |
| Weight | 4.79 | 5.01 | -5.02 to 14.60 | 0.339 |
| 1RM leg press | 2.76 | 3.40 | -3.91 to 9.42 | 0.418 |
| Vertical jump | -1.28 | 10.36 | -21.59 to 19.03 | 0.902 |
| Standing broad jump | 2.19 | 9.27 | -15.97 to 20.35 | 0.813 |
| NDI | 5.08 | 4.18 | -3.11 to 13.27 | 0.224 |
| T66 Fracture load X3N | ||||
| Pre/posta | 369.08 | 164.29 | 47.09 to 691.08 | *0.025 |
| Sexb | -270.67 | 312.20 | -882.57 to 341.23 | 0.386 |
| Puberty score | -81.70 | 96.43 | -270.70 to 107.31 | 0.397 |
| Age | 409.16 | 521.97 | -613.88 to 1432.20 | 0.433 |
| Height | 10.60 | 17.24 | -23.19 to 44.39 | 0.539 |
| Weight | 17.84 | 10.38 | -2.51 to 38.19 | 0.086 |
| 1 RM leg press | 7.99 | 7.54 | -6.79 to 22.77 | 0.289 |
| Vertical jump | 5.14 | 17.79 | -29.72 to 39.99 | 0.773 |
| Standing broad jump | 13.72 | 16.98 | -19.56 to 47.01 | 0.419 |
| NDI | 8.40 | 9.24 | -9.71 to 26.50 | 0.363 |
| T66 Fracture load Y3N | ||||
| Pre/posta | 590.86 | 258.79 | 83.65 to 1098.07 | *0.022 |
| Sexb | -224.60 | 292.11 | -347.94 to 797.13 | 0.442 |
| Puberty score | 123.73 | 124.84 | -120.95 to 368.41 | 0.322 |
| Age | 409.16 | 521.97 | -613.88 to 1432.20 | 0.433 |
| Height | 12.97 | 17.80 | -21.92 to 47.85 | 0.466 |
| Weight | 0.52 | 13.19 | -25.33 to 26.38 | 0.968 |
| 1 RM leg press | -0.32 | 6.63 | -13.32 to 12.68 | 0.962 |
| Vertical jump | -20.33 | 26.03 | -71.35 to 30.68 | 0.435 |
| Standing broad jump | 6.06 | 18.08 | -29.38 to 41.49 | 0.738 |
| NDI | 14.31 | 10.53 | -6.33 to 34.94 | 0.174 |
| T4 Trabecular density Z score | ||||
| Pre/Posta | 0.92 | 1.25 | -1.54 to 3.38 | 0.463 |
| Puberty score | -0.38 | 0.30 | -0.96 to 0.20 | 0.201 |
| Age | -1.01 | 0.75 | -2.48 to 0.47 | 0.181 |
| Weight | 0.08 | 0.03 | 0.04 to 0.13 | *<0.001 |
| 1 RM leg press | 0.04 | 0.03 | -0.02 to 0.09 | 0.171 |
| Vertical jump | 0.09 | 0.07 | -0.03 to 0.22 | 0.151 |
| Standing broad jump | -0.01 | 0.04 | -0.09 to 0.06 | 0.781 |
| NDI | -0.05 | 0.02 | -0.09 to -0.01 | *0.010 |
| T66 Cortical density Z score | ||||
| Pre/posta | -0.48 | 0.53 | -1.52 to 0.56 | 0.366 |
| Puberty score | 0.11 | 0.23 | -0.33 to 0.56 | 0.616 |
| Age | -0.41 | 0.61 | -1.60 to 0.79 | 0.506 |
| Weight | -0.01 | 0.02 | -0.05 to 0.03 | 0.476 |
| 1 RM leg press | 0.01 | 0.01 | -0.01 to 0.03 | 0.339 |
| Vertical jump | 0.06 | 0.04 | -0.03 to 0.14 | 0.174 |
| Standing broad jump | 0.02 | 0.02 | -0.03 to 0.06 | 0.500 |
| NDI | -0.03 | 0.01 | -0.05 to -0.001 | *0.038 |
| T66 Cortical area Z score | ||||
| Pre/Posta | -1.02 | 0.75 | -2.48 to 0.44 | 0.172 |
| Puberty score | 0.29 | 0.31 | -0.33 to 0.90 | 0.360 |
| Age | 1.21 | 0.86 | -2.91 to 0.48 | 0.161 |
| Weight | 0.02 | 0.03 | -0.04 to 0.07 | 0.609 |
| 1 RM leg press | 0.00 | 0.02 | -0.05 to 0.04 | 0.865 |
| Vertical jump | 0.07 | 0.03 | 0.01 to 0.13 | *0.034 |
| Standing broad jump | 0.00 | 0.03 | -0.06 to 0.05 | 0.934 |
| NDI | 0.01 | 0.02 | -0.03 to 0.05 | 0.735 |
| T66 SSI Z score | ||||
| Pre/Posta | 0.39 | 0.21 | -0.02 to 0.80 | 0.061 |
| Puberty score | 0.28 | 0.11 | 0.05 to 0.50 | *0.015 |
| Age | -0.66 | 0.35 | -1.35 to 0.02 | 0.057 |
| Weight | -0.01 | 0.02 | -0.04 to 0.02 | 0.541 |
| 1 RM leg press | 0.01 | 0.01 | -0.01 to 0.03 | 0.188 |
| Vertical jump | -0.01 | 0.02 | -0.06 to 0.03 | 0.547 |
| Standing broad jump | 0.00 | 0.02 | -0.05 to 0.04 | 0.961 |
| NDI | 0.02 | 0.01 | -0.01 to 0.05 | 0.148 |
Where pre-intervention is the comparison group and β=1;
Where male is the comparison group and β=1.
To compensate for the non-linear effect of age on growth, models were also run using age[2] as a growth estimate. While recognising that the models are likely underpowered, models which included age[2] as an estimate of growth found a statistically significant influence for growth, as indicated by age[2], age, height or weight, for the following measures T4 mass, T4 total area, T4 total density, T4 trabecular density, T4 trabecular density Z-score, T66 mass, T66 SSI, T66 cortical area, and T66 fracture load X3N. Models including age[2] also showed a stronger role for fitness measures which were additionally implicated in T4 mass, T4 total area, T4 total density, T4 trabecular density, and cortical density Z scores (appendix 2). It was not possible to run models including age[2] in the intervention naïve group only due to the smaller sample size .
Discussion
This study explored whether a prescribed multimodal exercise intervention established to improve physical abilities among adolescents with DCD[25,26] could also improve measures of bone health. Positively, AMPitup Program improved fitness parameters over the 13-week intervention, with improvements in bone parameters subsequently observed in bone scans conducted during the follow-up assessment period (approximately 3 months post-intervention). Prior research on fitness improvements in AMPitup have found that fitness gains tend to return to baseline over the break between interventions and thus can be attributed to the intervention rather than due to growth[25]. Statistical modelling also indicated that improvements in bone health parameters were related to improvements in fitness measures and gains were above what could be attributed to growth. Considering the short intervention time and sample size, these findings indicate that participation in a generalised multimodal exercise intervention may be effective in improving bone health of adolescents with DCD.
Bone parameters indicated an impairment at baseline and improvement over the course of the intervention, with the group overall moving towards a healthier bone phenotype. The size of the gains demonstrated in this study appear similar to what has been shown in other exercise interventions in comparable age groups, which have shown increases of between 1 to 8% in bone strength at the loaded sites[15,22]. The pattern of changes in bone parameters were primarily in bone mass and cortical area as would be anticipated for changes during an exercise intervention in a peri pubertal population[14,15,42,43], since loading in this age group results in reshaping of bone cross-sectionally along with a redistribution of bone minerals to the cortical area[15,42,43].
GEE modelling indicated that improvements in physical fitness contributed to changes in bone parameters beyond the effects of growth as indicated by age, height, weight, age[2] and pubertal stage, with vertical jump and 1RM leg press being implicated in several models. Fitness measures had a stronger role in models of only intervention-naïve participants, which likely reflects a low level of baseline physical activity in this population. Individuals who have lower baseline physical activity levels tend to show more substantial bone changes in response to an exercise intervention[21]. A low baseline of physical activity may also explain the finding in many models that bone gains increased as motor impairment increased (lower NDI). Physical activity has been found previously to decrease as motor impairment increases[44] and as such it is probable that those with greater motor impairment had lower baseline levels of physical activity. Some bone measures however, had an inverse finding with bone gains found to increase as degree of motor impairment decreased (higher NDI). This may reflect the impact of motor impairment on exercise performance with improvements in fitness being more limited in those that have more motor impairment which is then reflected in bone gains.
The role of motor impairment upon bone gains is also implicated by the smaller scale of change in muscle strength than would be anticipated based on other similar exercise interventions[19,20,22]. Although this could reflect on the osteogenic potential of the program, it may also indicate that the impact of exercise interventions on bone parameters is somewhat less effective in this population. It was noted in this study that exercise progression, including increasing loading, was slow for many participants with some participants remaining at the same level of loading throughout the intervention. Other studies have found that gains in fitness are more limited in individuals with DCD when compared to individuals without DCD[45] and have indicated the need for a longer learning period[24]. As increased loading and variety are required to stimulate osteogenic change[13], a slower exercise progression will limit the osteogenic potential of the exercise program. A longer time frame therefore may be needed by individuals with DCD to learn and effectively execute the exercise tasks before the osteogenic effects can be accurately observed and assessed.
This study had the advantage of including intervention experienced participants and sensitivity analysis supported the need for a longer intervention period by showing continued improvement in those participants. This would seem to indicate that once necessary motor skills are acquired for the exercise program modalities, participants are then able to achieve the increased loading and variety required to stimulate osteogenic change[13]. The study was strengthened by the use of a program specifically designed for individuals with DCD and already established to improve strength in an adolescent population with DCD[25], however it is likely that the 13 week program in this study was insufficient to allow for skill mastery. A longer study period would also allow more time for bone adaptation, however the five to seven-month epoch between the scans should have been sufficient to allow bone remodelling to occur[46]. The study was conspicuously limited by the absence of a control group, however the use of sex and height-matched Z-scores derived from the Stratec reference values[30] and statistical modelling to control for variables related to growth provided the advantage of being able to indicate that the effect of the exercise interventions on changes in bone outcomes were possibly above what would be anticipated from growth. Future research should include a control group to determine the impact of DCD specific impairments upon exercise intervention. The impact of the exercise program upon other exercise benefits such as improved muscle function and balance was beyond the reach of this study, however these are likely to magnify the benefits of the found small gains in bone mass[15,47]. Combined benefits, including improvements in muscle function and balance, as well as clinical benefits such as fracture rates are a potential avenue for future research along with confirmation of improvements in bone parameters.
The outcomes of this study are promising in relation to the ability of the intervention to be effective in improving muscle and bone parameters in adolescents with DCD. The changes detected in this study are small but reasonable given the timing of the study and the motor difficulties of the individuals with DCD. Further research should be undertaken over a longer period to determine whether bone improvements can be achieved and sustained to promote maximal bone mass accrual closer to the normal range during this critical developmental period. This is important for the prevention of future bone-health related adverse outcomes, particularly as this group reports a higher falls rate.
Acknowledgements
The authors would like to acknowledge the adolescents (and their parents) who participated in this study. The authors would also like to acknowledge Mr Brendan Beeson for his expertise and provision of pQCT scans in this patient population at Princess Margaret Hospital. The AMPitup program was in part supported by the Australian Government’s Collaborative Research Network (CRN) program and by a generous grant from the Princess Margaret Hospital Foundation.
Appendix
Appendix A.
GEE modelling showing relationships between changes in bone health and potential mediators.
| β | SE | β 95% Confidence interval | p | |
|---|---|---|---|---|
| T4 Mass | ||||
| Pre/Posta | -0.09 | 0.10 | -0.29 to 0.10 | 0.348 |
| Sexb | 0.23 | 0.16 | -0.08 to 0.54 | 0.146 |
| Puberty score | -0.11 | 0.07 | -0.25 to 0.03 | 0.108 |
| Age | -0.02 | 0.13 | -0.27 to 0.23 | 0.870 |
| Height | 0.01 | 0.09 | 0.00 to 0.03 | 0.122 |
| Weight | 0.02 | 0.01 | 0.00 to 0.04 | 0.056 |
| 1 RM leg press | 0.00 | 0.004 | -0.01 to 0.01 | 0.844 |
| Vertical jump | 0.02 | 0.01 | 0.00 to 0.05 | 0.074 |
| Standing broad jump | 0.00 | 0.01 | -0.02 to 0.02 | 0.694 |
| NDI | 0.00 | 0.004 | -0.01 to 0.01 | 0.701 |
| T4 Total area | ||||
| Pre/Posta | -54.02 | 22.68 | -98.47 to -9.57 | *0.017 |
| Sexb | 116.94 | 43.42 | 31.84 to 202.04 | *0.007 |
| Puberty score | -23.64 | 15.15 | -53.34 to 6.06 | 0.119 |
| Age | 20.28 | 39.61 | -57.36 to 97.91 | 0.609 |
| Height | 6.29 | 2.56 | 1.29 to 11.31 | *0.014 |
| Weight | -1.23 | 2.26 | -5.66 to 3.21 | 0.587 |
| 1 RM leg press | -1.09 | 0.83 | -2.72 to 0.53 | 0.188 |
| Vertical jump | 6.69 | 3.57 | -0.29 to 13.69 | 0.060 |
| Standing broad jump | -4.14 | 3.87 | -11.72 to 3.44 | 0.285 |
| NDI | 2.29 | 1.14 | 0.06 to 4.53 | *0.044 |
| T4 Total density | ||||
| Pre/Posta | 4.23 | 6.13 | -7.79 to 16.25 | 0.490 |
| Sexb | -10.05 | 6.83 | -23.44 to 3.34 | 0.141 |
| Puberty score | -2.46 | 3.17 | -8.64 to 3.81 | 0.447 |
| Age | -7.56 | 5.76 | -18.86 to 3.74 | 0.190 |
| Height | -0.15 | 0.48 | -1.11 to 0.80 | 0.754 |
| Weight | 1.88 | 0.45 | 1.00 to 2.77 | *<0.001 |
| 1 RM leg press | 0.23 | 0.22 | -0.19 to 0.65 | 0.287 |
| Vertical jump | 0.33 | 0.27 | -0.99 to 1.66 | 0.624 |
| Standing broad jump | 0.79 | 0.45 | -0.08 to 1.66 | 0.076 |
| NDI | -0.64 | 0.32 | -1.25 to -0.02 | *0.044 |
| T4 Trabecular density | ||||
| Pre/Posta | 5.67 | 8.61 | -11.21 to 22.55 | 0.510 |
| Sexb | 6.59 | 8.53 | -10.12 to 23.31 | 0.439 |
| Puberty score | -4.83 | 3.69 | -12.06 to 2.39 | 0.190 |
| Age | -15.53 | 7.18 | -29.60 to -1.47 | *0.030 |
| Height | 0.61 | 0.54 | -0.44 to 1.66 | 0.256 |
| Weight | 1.46 | 0.50 | 0.47 to 2.44 | *0.004 |
| 1 RM leg press | 0.45 | 0.25 | -0.05 to 0.95 | 0.079 |
| Vertical jump | 0.89 | 0.94 | -0.95 to 2.75 | 0.341 |
| Standing broad jump | -0.06 | 0.69 | -1.42 to 1.29 | 0.929 |
| NDI | -0.69 | 0.32 | -1.32 to -0.08 | *0.028 |
| T4 Trabecular density Z score | ||||
| Pre/Posta | 0.72 | 0.81 | -0.87 to 2.32 | 0.374 |
| Puberty score | -0.28 | 0.22 | -0.70 to 0.14 | 0.190 |
| Age | -0.83 | 0.40 | -1.61 to -0.04 | *0.039 |
| Weight | 0.05 | 0.02 | 0.01 to 0.09 | *0.016 |
| 1 RM leg press | 0.03 | 0.02 | -0.01 to 0.06 | 0.105 |
| Vertical jump | 0.07 | 0.06 | -0.06 to 0.19 | 0.304 |
| Standing broad jump | 0.00 | 0.03 | -0.06 to 0.06 | 0.997 |
| NDI | -0.04 | 0.02 | -0.08 to 0.00 | *0.049 |
| T66 Mass | ||||
| Pre/Posta | -0.02 | 0.08 | -0.18 to 0.14 | 0.783 |
| Sexb | -0.40 | 0.17 | -0.74 to -0.07 | *0.019 |
| Puberty score | 0.00 | 0.06 | -0.13 to 0.12 | 0.949 |
| Age | 0.58 | 0.17 | 0.25 to 0.91 | *<0.001 |
| Height | -0.01 | 0.01 | -0.03 to 0.01 | 0.281 |
| Weight | 0.01 | 0.01 | -0.01 to 0.03 | 0.357 |
| 1 RM leg press | -0.01 | 0.004 | -0.01 to 0.00 | 0.137 |
| Vertical jump | 0.01 | 0.01 | -0.01 to 0.03 | 0.373 |
| Standing broad jump | -0.01 | 0.01 | -0.03 to 0.01 | 0.302 |
| NDI | 0.01 | 0.01 | 0.00 to 0.02 | *0.044 |
| T66 SSI | ||||
| Pre/Posta | 111.08 | 70.30 | -26.71 to 248.88 | 0.114 |
| Sexb | -180.33 | 135.79 | -446.48 to 85.82 | 0.184 |
| Puberty score | 10.32 | 46.17 | -80.17 to 100.80 | 0.823 |
| Age | 135.27 | 115.95 | -91.99 to 365.53 | 0.243 |
| Height | 0.86 | 9.47 | -17.71 to 19.43 | 0.928 |
| Weight | 9.57 | 6.34 | -2.86 to 21.99 | 0.131 |
| 1RM leg press | -3.28 | 3.02 | -9.19 to 2.63 | 0.277 |
| Vertical jump | 10.15 | 11.75 | -12.87 to 33.19 | 0.387 |
| Standing broad jump | 0.85 | 8.39 | -15.59 to 17.28 | 0.920 |
| NDI | 2.76 | 3.65 | -4.39 to 9.90 | 0.450 |
| T66 SSI Z score | ||||
| Pre/Posta | -0.28 | 0.22 | -1.04 to 0.35 | 0.203 |
| Puberty score | 0.04 | 0.17 | 0.30 to 0.38 | 0.824 |
| Age | -0.35 | 0.35 | -1.04 to 0.35 | 0.327 |
| Weight | 0.02 | 0.02 | -0.02 to 0.06 | 0.270 |
| 1RM leg press | 0.00 | 0.01 | -0.02 to 0.02 | 0.804 |
| Vertical jump | 0.03 | 0.03 | -0.03 to 0.09 | 0.290 |
| Standing broad jump | 0.00 | 0.02 | -0.05 to 0.05 | 0.998 |
| NDI | 0.00 | 0.02 | -0.03 to 0.03 | 0.909 |
| T66 Total area | ||||
| Pre/Posta | 37.08 | 33.62 | -28.81 to 102.98 | 0.270 |
| Sexb | 7.82 | 48.15 | -86.56 to 102.19 | 0.871 |
| Puberty score | -7.82 | 18.14 | -42.58 to 28.52 | 0.698 |
| Age | 51.29 | 38.33 | -23.82 to 126.41 | 0.181 |
| Height | -3.04 | 2.15 | -7.25 to 1.16 | 0.156 |
| Weight | 3.24 | 2.93 | -2.50 to 8.97 | 0.269 |
| 1RM leg press | -0.84 | 0.85 | -2.51 to 0.82 | 0.321 |
| Vertical jump | -1.85 | 3.22 | -8.16 to 4.46 | 0.566 |
| Standing broad jump | -0.34 | 2.32 | -4.88 to 4.21 | 0.885 |
| NDI | 1.48 | 1.69 | -1.84 to 4.79 | 0.382 |
| T66 Cortical density | ||||
| Pre/Posta | -2.68 | 10.20 | -22.67 to 17.32 | 0.793 |
| Sexb | -39.82 | 10.61 | -60.62 to -19.02 | *<0.001 |
| Puberty score | -1.91 | 4.55 | -10.82 to 7.00 | 0.674 |
| Age | 13.32 | 8.34 | -3.04 to 29.67 | 0.110 |
| Height | -0.30 | 0.49 | -1.27 to 0.67 | 0.544 |
| Weight | 0.09 | 0.67 | -1.22 to 1.40 | 0.893 |
| 1 RM leg press | 0.56 | 0.23 | 0.11 to 1.01 | *0.015 |
| Vertical jump | 1.71 | 1.26 | -0.76 to 4.18 | 0.175 |
| Standing broad jump | -0.10 | 0.67 | -1.41 to 1.22 | 0.888 |
| NDI | -0.55 | 0.49 | -1.52 to 0.42 | 0.267 |
| T66 Cortical density Z score | ||||
| Pre/Posta | -0.06 | 0.27 | -0.58 to 0.47 | 0.835 |
| Puberty score | 0.02 | 0.14 | -0.26 to 0.31 | 0.869 |
| Age | -0.06 | 0.26 | -0.46 to 0.57 | 0.831 |
| Weight | -0.02 | 0.02 | -0.06 to 0.02 | 0.335 |
| 1 RM leg press | 0.02 | 0.01 | 0.001 to 0.03 | *0.037 |
| Vertical jump | 0.03 | 0.04 | -0.04 to 0.10 | 0.382 |
| Standing broad jump | 0.01 | 0.02 | -0.03 to 0.06 | 0.635 |
| NDI | -0.02 | 0.01 | -0.04 to 0.01 | 0.246 |
| T66 Cortical area | ||||
| Pre/Posta | -3.38 | 9.50 | -21.99 to 15.24 | 0.722 |
| Sexb | -27.19 | 16.82 | -60.17 to 5.78 | 0.106 |
| Puberty score | -2.48 | 7.70 | -17.57 to 12.62 | 0.748 |
| Age | 34.23 | 15.72 | 3.41 to 65.04 | *0.029 |
| Height | 0.60 | 1.16 | -1.68 to 2.88 | 0.607 |
| Weight | 0.66 | 0.92 | -1.14 to 2.46 | 0.473 |
| 1RM leg press | -0.21 | 0.36 | -0.91 to 0.49 | 0.557 |
| Vertical jump | 2.01 | 0.99 | 0.06 to 3.95 | *0.043 |
| Standing broad jump | -0.71 | 0.77 | -2.24 to 0.81 | 0.359 |
| NDI | 0.53 | 0.59 | -0.62 to 1.69 | 0.366 |
| T66 Cortical area Z-score | ||||
| Pre/Posta | -0.16 | 0.31 | -0.77 to 0.45 | 0.613 |
| Puberty Score | -0.08 | 0.26 | -0.58 to 0.43 | 0.764 |
| Age | 0.16 | 0.52 | -0.86 to 1.18 | 0.758 |
| Weight | 0.02 | 0.03 | -0.04 to 0.08 | 0.597 |
| 1 RM leg press | 0.01 | 0.01 | -0.02 to 0.03 | 0.655 |
| Vertical jump | 0.07 | 0.04 | -0.01 to 0.14 | 0.081 |
| Standing broad jump | -0.02 | 0.03 | -0.07 to 0.03 | 0.467 |
| NDI | 0.01 | 0.02 | -0.03 to 0.05 | 0.736 |
| T66 Fracture load X3N | ||||
| Pre/Posta | 132.07 | 154.73 | -171.20 to 435.34 | 0.393 |
| Sexb | -766.77 | 338.21 | -1429.64 to -103.91 | *0.023 |
| Puberty score | -73.44 | 118.54 | -305.77 to 158.89 | 0.536 |
| Age | 606.97 | 316.71 | -13.78 to 1227.72 | 0.055 |
| Height | -4.25 | 22.52 | -48.39 to 39.89 | 0.850 |
| Weight | 26.64 | 15.23 | -3.21 to 56.48 | 0.080 |
| 1RM leg press | -7.92 | 6.75 | -21.15 to 5.30 | 0.240 |
| Vertical jump | 33.00 | 22.55 | -11.19 to 77.20 | 0.143 |
| Standing broad jump | 6.58 | 15.49 | -23.78 to 36.94 | 0.671 |
| NDI | 4.96 | 8.76 | -12.21 to 22.14 | 0.571 |
| T66 Fracture load Y3N | ||||
| Pre/Posta | 240.39 | 176.35 | -105.25 to 586.03 | 0.173 |
| Sexb | -150.89 | 243.10 | -627.37 to 325.58 | 0.535 |
| Puberty score | 113.34 | 96.31 | -75.42 to 302.11 | 0.239 |
| Age | 320.16 | 200.73 | -73.26 to 713.58 | 0.111 |
| Height | -1.02 | 16.40 | -33.17 to 31.13 | 0.950 |
| Weight | 14.01 | 10.79 | -7.14 to 35.17 | 0.194 |
| 1 RM leg press | -13.51 | 6.34 | -25.94 to -1.08 | *0.033 |
| Vertical jump | 4.21 | 23.18 | -41.23 to 49.66 | 0.856 |
| Standing broad jump | 3.49 | 16.42 | -28.69 to 35.67 | 0.832 |
| NDI | 10.53 | 8.64 | -6.41 to 27.46 | 0.223 |
Where pre-intervention is the comparison group and β=1;
Where male is the comparison group and β=1.
Appendix B.
GEE modelling showing relationships between changes in bone health and potential mediators with age2 included.
| β | SE | β 95% Confidence interval | p | |
|---|---|---|---|---|
| T4 Mass | ||||
| Pre/Posta | 0.04 | 0.09 | -0.14 to 0.22 | 0.636 |
| Sexb | 0.15 | 0.14 | -0.13 to 0.42 | 0.291 |
| Puberty score | -0.20 | 0.06 | -0.33 to -0.07 | *0.002 |
| Age | 5.54 | 1.33 | 2.94 to 8.14 | *<0.001 |
| Age2 | -0.19 | 0.05 | -0.28 to -0.10 | *<0.001 |
| Height | 0.00 | 0.01 | -0.01 to 0.02 | 0.726 |
| Weight | 0.03 | 0.01 | 0.01 to 0.05 | *0.003 |
| 1 RM leg press | 0.00 | 0.002 | 0.00 to 0.01 | 0.250 |
| Vertical jump | 0.03 | 0.01 | 0.00 to 0.05 | *0.018 |
| Standing broad jump | 0.00 | 0.01 | -0.02 to 0.02 | 0.933 |
| NDI | 0.00 | 0.004 | -0.01 to 0.004 | 0.414 |
| T4 Total area | ||||
| Pre/Posta | -24.39 | 21.88 | -67.28 to 18.50 | 0.265 |
| Sexb | 98.91 | 38.27 | 23.90 to 173.91 | *0.010 |
| Puberty score | -42.11 | 12.66 | -66.92 to -17.30 | *0.001 |
| Age | 1212.31 | 225.24 | 770.85 to 1653.76 | *<0.005 |
| Age2 | -40.32 | 7.01 | -54.06 to -26.59 | *<0.005 |
| Height | 3.89 | 2.62 | -1.25 to 9.02 | 0.138 |
| Weight | 0.58 | 2.04 | -3.42 to 4.58 | 0.776 |
| 1 RM leg press | -0.66 | 0.74 | -2.10 to 0.79 | 0.372 |
| Vertical jump | 6.96 | 3.30 | 0.48 to 13.43 | *0.035 |
| Standing broad jump | -3.42 | 3.55 | -10.38 to 3.55 | 0.336 |
| NDI | 2.02 | 1.04 | -0.02 to 4.06 | 0.052 |
| T4 Total density | ||||
| Pre/Posta | 8.76 | 6.30 | -3.58 to 21.10 | 0.164 |
| Sexb | -12.81 | 6.46 | -25.46 to -0.15 | *0.047 |
| Puberty score | -5.24 | 3.08 | -11.28 to 0.81 | 0.089 |
| Age | 174.66 | 89.32 | -0.42 to 349.73 | 0.051 |
| Age2 | -6.16 | 3.07 | -12.18 to -0.15 | *0.045 |
| Height | -0.52 | 0.41 | -1.32 to 0.28 | 0.201 |
| Weight | 2.17 | 0.46 | 1.26 to 3.07 | *<0.001 |
| 1 RM leg press | 0.30 | 0.19 | -0.07 to 0.66 | 0.110 |
| Vertical jump | 0.37 | 0.59 | -0.78 to 1.53 | 0.527 |
| Standing broad jump | 0.90 | 0.43 | 0.06 to 1.74 | *0.036 |
| NDI | -0.68 | 0.31 | -1.30 to -0.06 | *0.031 |
| T4 Trabecular density | ||||
| Pre/Posta | 10.55 | 8.86 | -6.82 to 27.91 | 0.234 |
| Sexb | 3.63 | 8.96 | -13.94 to 21.19 | 0.686 |
| Puberty score | -7.87 | 4.11 | -15.94 to 0.19 | 0.056 |
| Age | 180.77 | 111.25 | -37.28 to 398.82 | 0.104 |
| Age2 | -6.64 | 3.73 | -13.96 to 0.68 | 0.075 |
| Height | 0.21 | 0.57 | -0.91 to 1.33 | 0.709 |
| Weight | 1.76 | 0.53 | 0.72 to 2.79 | *0.001 |
| 1 RM leg press | 0.52 | 0.21 | 0.11 to 0.94 | *0.014 |
| Vertical jump | 0.94 | 0.82 | -0.67 to 2.55 | 0.253 |
| Standing broad jump | 0.06 | 0.66 | -1.23 to 1.35 | 0.930 |
| NDI | -0.74 | 0.32 | -1.37 to -0.11 | *0.021 |
| T4 Trabecular density Z score | ||||
| Pre/Posta | 0.91 | 0.82 | -0.70 to 2.52 | 0.268 |
| Puberty score | -0.40 | 0.24 | -0.86 to 0.07 | 0.094 |
| Age | 6.66 | 4.08 | -1.33 to 14.66 | 0.102 |
| Age2 | -0.26 | 0.14 | -0.53 to 0.01 | 0.060 |
| Weight | 0.06 | 0.02 | 0.02 to 0.10 | *0.003 |
| 1 RM leg press | 0.03 | 0.02 | 0.00 to 0.07 | 0.057 |
| Vertical jump | 0.07 | 0.06 | -0.0 to 0.19 | 0.288 |
| Standing broad jump | 0.01 | 0.03 | -0.05 to 0.07 | 0.822 |
| NDI | -0.04 | 0.02 | -0.08 to 0.00 | *0.034 |
| T66 Mass | ||||
| Pre/Posta | 0.10 | 0.08 | -0.07 to 0.26 | 0.243 |
| Sexb | -0.48 | 0.13 | -0.72 to -0.22 | *<0.001 |
| Puberty score | -0.08 | 0.06 | -0.20 to 0.04 | 0.184 |
| Age | 5.45 | 0.89 | 3.70 to 7.19 | *<0.001 |
| Age2 | -0.17 | 0.03 | -0.22 to -0.11 | *<0.001 |
| Height | -0.02 | 0.01 | -0.04 to 0.01 | *0.007 |
| Weight | 0.02 | 0.01 | 0.00 to 0.03 | *0.048 |
| 1 RM leg press | 0.00 | 0.003 | -0.01 to 0.003 | 0.243 |
| Vertical jump | 0.01 | 0.01 | -0.01 to 0.03 | 0.355 |
| Standing broad jump | -0.01 | 0.01 | -0.02 to 0.01 | 0.507 |
| NDI | 0.01 | 0.004 | 0.00 to 0.02 | *0.036 |
| T66 SSI | ||||
| Pre/Posta | 170.88 | 66.81 | 39.94 to 301.83 | *0.011 |
| Sexb | -216.73 | 124.13 | -460.02 to 26.57 | 0.081 |
| Puberty score | -29.96 | 48.34 | -121.71 to 67.79 | 0.577 |
| Age | 2541.25 | 982.46 | 615.66 to 4466.84 | *0.010 |
| Age2 | -81.38 | 31.96 | -144.02 to -18.75 | *0.011 |
| Height | -4.01 | 9.44 | -22.51 to 14.49 | 0.671 |
| Weight | 13.22 | 6.41 | 0.66 to 25.78 | *0.039 |
| 1 RM leg press | -2.41 | 3.21 | -8.70 to 3.88 | 0.454 |
| Vertical jump | 10.68 | 12.43 | -13.69 to 35.05 | 0.390 |
| Standing broad jump | 2.31 | 8.47 | -14.30 to 18.92 | 0.786 |
| NDI | 2.20 | 3.77 | -5.19 to 9.59 | 0.559 |
| T66 SSI Z score | ||||
| Pre/Posta | 0.27 | 0.23 | -0.19 to 0.72 | 0.255 |
| Puberty score | 0.05 | 0.21 | -0.36 to 0.46 | 0.814 |
| Age | -1.03 | 4.53 | -9.91 to 7.85 | 0.820 |
| Age2 | 0.02 | 0.15 | -0.28 to 0.32 | 0.877 |
| Weight | 0.02 | 0.02 | -0.02 to 0.06 | 0.341 |
| 1 RM leg press | 0.00 | 0.01 | -0.02 to 0.02 | 0.837 |
| Vertical jump | 0.03 | 0.03 | -0.03 to 0.09 | 0.292 |
| Standing broad jump | 0.00 | 0.02 | -0.05 to 0.04 | 0.976 |
| NDI | 0.00 | 0.02 | -0.03 to 0.04 | 0.899 |
| T66 Total area | ||||
| Pre/Posta | 47.28 | 36.08 | -23.44 to 118.00 | 0.190 |
| Sexb | 1.61 | 46.52 | -89.56 to 92.78 | 0.972 |
| Puberty score | -13.39 | 18.20 | -49.05 to 22.28 | 0.462 |
| Age | 461.60 | 306.75 | -139.62 to 1062.82 | 0.132 |
| Age2 | -13.88 | 10.39 | -34.23 to 6.48 | 0.181 |
| Height | -3.88 | 2.16 | -8.10 to 0.35 | 0.072 |
| Weight | 3.86 | 3.07 | -2.15 to 9.87 | 0.208 |
| 1 RM leg press | -0.70 | 0.84 | -2.34 to 0.95 | 0.409 |
| Vertical jump | -1.76 | 3.30 | -8.23 to 4.71 | 0.594 |
| Standing broad jump | -0.09 | 2.38 | -4.75 to 4.58 | 0.971 |
| NDI | 1.39 | 1.66 | -1.88 to 4.65 | 0.405 |
| T66 Cortical density | ||||
| Pre/Posta | 0.77 | 11.02 | -20.83 to 22.37 | 0.944 |
| Sexb | -41.92 | 9.50 | -60.54 to -23.29 | *<0.001 |
| Puberty score | -4.06 | 4.84 | -13.55 to 5.43 | 0.401 |
| Age | 152.09 | 79.73 | -4.17 to 308.35 | 0.056 |
| Age2 | -4.69 | 2.74 | -10.06 to 0.67 | 0.086 |
| Height | -0.58 | 0.42 | -1.41 to 0.25 | 0.171 |
| Weight | 0.30 | 0.67 | -1.02 to 1.62 | 0.655 |
| 1 RM leg press | 0.61 | 0.23 | 0.15 to 1.07 | *0.010 |
| Vertical jump | 1.74 | 1.22 | -0.65 to 4.12 | 0.153 |
| Standing broad jump | -0.01 | 0.67 | -1.32 to 1.30 | 0.987 |
| NDI | -0.58 | 0.48 | -1.51 to 0.35 | 0.222 |
| T66 Cortical density Z score | ||||
| Pre/Posta | -0.04 | 0.29 | -0.61 to 0.53 | 0.893 |
| Puberty score | 0.01 | 0.16 | -0.29 to 0.32 | 0.930 |
| Age | 0.72 | 2.45 | -4.08 to 5.51 | 0.770 |
| Age2 | -0.02 | 0.08 | -0.18 to 0.14 | 0.784 |
| Weight | -0.02 | 0.02 | -0.06 to 0.02 | 0.364 |
| 1 RM leg press | 0.02 | 0.01 | 0.001 to 0.03 | *0.034 |
| Vertical jump | 0.03 | 0.04 | -0.04 to 0.10 | 0.380 |
| Standing broad jump | 0.01 | 0.02 | -0.03 to 0.06 | 0.621 |
| NDI | -0.02 | 0.01 | -0.04 to 0.01 | 0.232 |
| T66 Cortical area | ||||
| Pre/Posta | 8.46 | 8.95 | -9.07 to 26.00 | 0.344 |
| Sexb | -34.40 | 12.77 | -59.43 to -9.37 | *0.007 |
| Puberty score | -9.86 | 6.79 | -23.17 to 3.45 | 0.147 |
| Age | 510.67 | 123.36 | 268.90 to 752.45 | *<0.001 |
| Age2 | -16.12 | 4.23 | -24.41 to -7.82 | *<0.001 |
| Height | -0.37 | 0.80 | -1.94 to 1.21 | 0.648 |
| Weight | 1.38 | 0.82 | -0.23 to 2.99 | 0.093 |
| 1 RM leg press | -0.04 | 0.32 | -0.66 to 0.59 | 0.911 |
| Vertical jump | 2.11 | 0.99 | 0.17 to 4.05 | *0.033 |
| Standing broad jump | -0.42 | 0.79 | -1.98 to 1.13 | 0.593 |
| NDI | 0.42 | 0.56 | -0.68 to 1.53 | 0.450 |
| T66 Cortical area Z-score | ||||
| Pre/Posta | -0.01 | 0.32 | -0.64 to 0.61 | 0.969 |
| Puberty Score | -0.17 | 0.28 | -0.71 to 0.38 | 0.549 |
| Age | 5.97 | 6.14 | -6.07 to 18.01 | 0.331 |
| Age2 | -0.20 | 0.21 | -0.61 to 0.21 | 0.340 |
| Weight | 0.02 | 0.03 | -0.05 to 0.09 | 0.515 |
| 1 RM leg press | 0.01 | 0.01 | -0.02 to 0.03 | 0.463 |
| Vertical jump | 0.07 | 0.04 | 0.00 to 0.14 | 0.065 |
| Standing broad jump | -0.02 | 0.03 | -0.07 to 0.04 | 0.595 |
| NDI | 0.00 | 0.02 | -0.04 to 0.05 | 0.833 |
| T66 Fracture load X3N | ||||
| Pre/Posta | 372.85 | 131.02 | 116.04 to 629.65 | *0.004 |
| Sexb | -913.33 | 266.30 | -1435.27 to -391.39 | *0.001 |
| Puberty score | -223.51 | 107.92 | -435.04 to -11.99 | *0.038 |
| Age | 1204.22 | 2129.87 | 6119.76 to 14468.68 | *<0.001 |
| Age2 | -327.68 | 68.88 | -462.67 to -192.68 | *<0.001 |
| Height | -23.86 | 19.92 | -62.90 to 15.19 | 0.231 |
| Weight | 41.35 | 14.03 | 13.86 to 68.84 | *0.003 |
| 1 RM leg press | -4.40 | 6.93 | -17.98 to 9.18 | 0.525 |
| Vertical jump | 35.11 | 25.48 | -14.83 to 85.05 | 0.168 |
| Standing broad jump | 12.45 | 16.27 | -19.44 to 44.34 | 0.444 |
| NDI | 2.73 | 7.84 | -12.63 to 18.09 | 0.728 |
| T66 Fracture load Y3N | ||||
| Pre/Posta | 304.03 | 184.08 | -56.77 to 664.83 | 0.099 |
| Sexb | -189.64 | 239.69 | -659.42 to 280.15 | 0.429 |
| Puberty score | 73.68 | 105.01 | -132.13 to 279.49 | 0.483 |
| Age | 2880.67 | 22225.56 | -1481.34 to 7242.68 | 0.196 |
| Age2 | -86.61 | 75.07 | -233.75 to 60.53 | 0.249 |
| Height | -6.20 | 16.06 | -37.69 to 25.28 | 0.699 |
| Weight | 17.90 | 12.12 | -5.86 to 41.66 | 0.140 |
| 1 RM leg press | -12.58 | 6.47 | -25.26 to 0.11 | 0.052 |
| Vertical jump | 4.77 | 24.19 | -42.64 to 52.18 | 0.844 |
| Standing broad jump | 5.04 | 16.55 | -27.39 to 37.47 | 0.761 |
| NDI | 9.94 | 8.70 | -7.12 to 26.99 | 0.254 |
Where pre-intervention is the comparison group and β=1;
Where male is the comparison group and β=1.
Appendix C.
GEE modelling showing relationships between changes in bone health and potential mediators for intervention-naive participants only.
| β | SE | β 95% Confidence interval | p | |
|---|---|---|---|---|
| T4 Mass | ||||
| Pre/Posta | -0.08 | 0.17 | -0.41 to 0.36 | 0.653 |
| Sexb | -0.07 | 0.01 | -0.27 to 0.12 | 0.461 |
| Puberty score | -0.23 | 0.09 | -0.41 to 0.05 | *0.011 |
| Age | 0.29 | 0.20 | -0.10 to 0.68 | 0.141 |
| Height | 0.00 | 0.01 | -0.02 to 0.01 | 0.683 |
| Weight | 0.04 | 0.01 | 0.02 to 0.06 | *<0.001 |
| 1 RM leg press | 0.00 | 0.004 | -0.01 to 0.01 | 0.571 |
| Vertical jump | 0.03 | 0.01 | 0.01 to 0.06 | *0.002 |
| Standing broad jump | 0.00 | 0.08 | -0.02 to 0.02 | 0.941 |
| NDI | -0.01 | 0.004 | -0.01 to 0.00 | 0.060 |
| T4 Total area | ||||
| Pre/Posta | -62.18 | 43.93 | -148.29 to 23.92 | 0.157 |
| Sexb | 57.40 | 39.04 | -19.12 to 133.93 | 0.141 |
| Puberty score | -39.77 | 17.27 | -73.63 to -5.91 | *0.021 |
| Age | 72.35 | 68.03 | -60.99 to 205.69 | 0.288 |
| Height | 2.96 | 2.90 | -2.73 to 8.66 | 0.308 |
| Weight | 2.74 | 2.48 | -2.12 to 7.60 | 0.269 |
| 1 RM leg press | -2.28 | 1.10 | -4.43 to -0.12 | *0.038 |
| Vertical jump | 9.46 | 3.87 | 1.87 to 17.04 | *0.015 |
| Standing broad jump | -3.35 | 3.70 | -10.69 to 3.91 | 0.366 |
| NDI | 1.40 | 1.32 | -1.18 to 3.98 | 0.289 |
| T4 Total density | ||||
| Pre/Posta | -0.28 | 6.56 | -13.13 to 12.57 | 0.966 |
| Sexb | -21.66 | 7.53 | -36.42 to -6.91 | *0.004 |
| Puberty score | -6.79 | 4.56 | -15.73 to 2.15 | 0.137 |
| Age | -4.64 | 17.02 | -37.99 to 28.72 | 0.785 |
| Height | -0.73 | 0.58 | -1.86 to 0.41 | 0.211 |
| Weight | 2.88 | 0.41 | 2.08 to 3.68 | *<0.001 |
| 1 RM leg press | 0.07 | 0.28 | -0.48 to 0.61 | 0.811 |
| Vertical jump | 0.76 | 0.56 | -0.35 to 1.87 | 0.178 |
| Standing broad jump | 1.04 | 0.49 | 0.09 to 1.99 | *0.033 |
| NDI | -0.91 | 0.22 | -1.33 to -0.48 | *<0.001 |
| T4 Trabecular density | ||||
| Pre/Posta | 6.58 | 13.67 | -20.21 to 33.37 | 0.630 |
| Sexb | -11.91 | 11.39 | -34.25 to 10.42 | 0.296 |
| Puberty score | -11.64 | 5.93 | -23.26 to -0.03 | *0.050 |
| Age | 0.20 | 19.83 | -38.67 to 39.07 | 0.992 |
| Height | -0.32 | 0.70 | -1.70 to 1.06 | 0.648 |
| Weight | 2.62 | 0.55 | 1.54 to 3.70 | *<0.001 |
| 1 RM leg press | 0.34 | 0.37 | -0.39 to 1.07 | 0.360 |
| Vertical jump | 1.77 | 0.82 | 0.17 to 3.37 | *0.030 |
| Standing broad jump | -0.09 | 0.74 | -1.55 to 1.36 | 0.900 |
| NDI | -1.04 | 0.31 | -1.65 to -0.42 | *0.001 |
| T4 Trabecular density Z score | ||||
| Pre/Posta | 0.92 | 1.25 | -1.54 to 3.38 | 0.463 |
| Puberty score | -0.38 | 0.30 | -0.96 to 0.20 | 0.201 |
| Age | -1.01 | 0.75 | -2.48 to 0.47 | 0.181 |
| Weight | 0.08 | 0.03 | 0.04 to 0.13 | *<0.001 |
| 1 RM leg press | 0.04 | 0.03 | -0.02 to 0.09 | 0.171 |
| Vertical jump | 0.09 | 0.07 | -0.03 to 0.22 | 0.151 |
| Standing broad jump | -0.01 | 0.04 | -0.09 to 0.06 | 0.781 |
| NDI | -0.05 | 0.02 | -0.09 to -0.01 | *0.010 |
| T66 Mass | ||||
| Pre/Posta | -0.07 | 2.73 | -9.61 to 1.09 | 0.119 |
| Sexb | -0.42 | 0.15 | -0.72 to -0.12 | *0.005 |
| Puberty score | -0.04 | 0.07 | -0.18 to 0.10 | 0.579 |
| Age | 0.67 | 0.29 | 0.09 to 1.24 | *0.022 |
| Height | -0.02 | 0.01 | - 0.03 to 0.00 | 0.090 |
| Weight | 0.02 | 0.01 | 0.002 to 0.03 | *0.022 |
| 1 RM leg press | -0.01 | 0.01 | -0.02 to 0.00 | 0.130 |
| Vertical jump | 0.01 | 0.01 | -0.02 to 0.03 | 0.588 |
| Standing broad jump | 0.00 | 0.01 | -0.02 to 0.02 | 0.864 |
| NDI | 0.01 | 0.05 | 0.00 to 0.02 | 0.079 |
| T66 SSI | ||||
| Pre/Posta | 164.65 | 79.93 | 22.72 to 307.59 | *0.024 |
| Sexb | 63.19 | 144.82 | -220.65 to 347.02 | 0.663 |
| Puberty score | 32.82 | 46.83 | -58.97 to 124.60 | 0.483 |
| Age | 27.16 | 239.47 | -442.20 to 496.51 | 0.910 |
| Height | 9.96 | 8.20 | -6.12 to 26.04 | 0.225 |
| Weight | 4.79 | 5.01 | -5.02 to 14.60 | 0.339 |
| 1 RM leg press | 2.76 | 3.40 | -3.91 to 9.42 | 0.418 |
| Vertical jump | -1.28 | 10.36 | -21.59 to 19.03 | 0.902 |
| Standing broad jump | 2.19 | 9.27 | -15.97 to 20.35 | 0.813 |
| NDI | 5.08 | 4.18 | -3.11 to 13.27 | 0.224 |
| T66 SSI Z score | ||||
| Pre/Posta | 0.39 | 0.21 | -0.02 to 0.80 | 0.061 |
| Puberty score | 0.28 | 0.11 | 0.05 to 0.50 | *0.015 |
| Age | -0.66 | 0.35 | -1.35 to 0.02 | 0.057 |
| Weight | -0.01 | 0.02 | -0.04 to 0.02 | 0.541 |
| 1 RM leg press | 0.01 | 0.01 | -0.01 to 0.03 | 0.188 |
| Vertical jump | -0.01 | 0.02 | -0.06 to 0.03 | 0.547 |
| Standing broad jump | 0.00 | 0.02 | -0.05 to 0.04 | 0.961 |
| NDI | 0.02 | 0.01 | -0.01 to 0.05 | 0.148 |
| T66 Total area | ||||
| Pre/Posta | 168.54 | 67.93 | 35.40 to 301.69 | *0.013 |
| Sexb | 70.55 | 36.58 | -1.15 to 142.25 | 0.054 |
| Puberty score | -14.01 | 23.37 | -59.82 to 31.81 | 0.549 |
| Age | 136.09 | 53.60 | 31.04 to 241.14 | *0.011 |
| Height | -0.77 | 1.31 | -3.34 to 1.80 | 0.555 |
| Weight | -0.51 | 1.87 | -4.18 to 3.16 | 0.785 |
| 1 RM leg press | 2.70 | 1.07 | 0.61 to 4.79 | *0.011 |
| Vertical jump | -9.43 | 2.30 | -15.31 to -3.56 | *0.002 |
| Standing broad jump | -0.94 | 1.45 | -3.78 to 1.90 | 0.516 |
| NDI | 3.39 | 0.80 | 1.82 to 4.95 | *<0.001 |
| T66 Cortical density | ||||
| Pre/Posta | -15.60 | 19.94 | -54.69 to 23.48 | 0.434 |
| Sexb | -48.27 | 12.69 | -73.14 to -23.40 | *<0.001 |
| Puberty score | -3.83 | 7.65 | -18.83 to 11.18 | 0.617 |
| Age | 15.79 | 23.52 | -30.31 to 61.89 | 0.502 |
| Height | -0.81 | 0.61 | -2.00 to 0.38 | 0.183 |
| Weight | 0.67 | 0.70 | -0.71 to 2.05 | 0.342 |
| 1 RM leg press | 0.24 | 0.27 | -0.28 to 0.77 | 0.360 |
| Vertical jump | 2.89 | 1.57 | -0.20 to 5.97 | 0.067 |
| Standing broad jump | 0.20 | 0.65 | -1.06 to 1.47 | 0.753 |
| NDI | -1.03 | 0.45 | -1.92 to -0.14 | *0.023 |
| T66 Cortical density Z score | ||||
| Pre/Posta | -0.48 | 0.53 | -1.52 to 0.56 | 0.366 |
| Puberty score | 0.11 | 0.23 | -0.33 to 0.56 | 0.616 |
| Age | -0.41 | 0.61 | -1.60 to 0.79 | 0.506 |
| Weight | -0.01 | 0.02 | -0.05 to 0.03 | 0.476 |
| 1RM leg press | 0.01 | 0.01 | -0.01 to 0.03 | 0.339 |
| Vertical jump | 0.06 | 0.04 | -0.03 to 0.14 | 0.174 |
| Standing broad jump | 0.02 | 0.02 | -0.03 to 0.06 | 0.500 |
| NDI | -0.03 | 0.01 | -0.05 to -0.001 | *0.038 |
| T66 Cortical area | ||||
| Pre/Posta | -27.02 | 19.80 | -65.84 to 15.96 | 0.799 |
| Sexb | -26.41 | 14.30 | -54.43 to 1.62 | 0.065 |
| Puberty score | -2.39 | 9.36 | -20.73 to 15.96 | 0.799 |
| Age | 16.62 | 32.85 | -47.76 to 81.00 | 0.613 |
| Height | 0.38 | 0.99 | -1.56 to 2.32 | 0.699 |
| Weight | 1.79 | 0.71 | 0.39 to 3.18 | *0.012 |
| 1 RM leg press | -0.61 | 0.56 | -1.70 to 0.48 | 0.274 |
| Vertical jump | 2.80 | 1.03 | 0.79 to 4.81 | *0.006 |
| Standing broad jump | 0.12 | 0.80 | -1.37 to 1.62 | 0.874 |
| NDI | 0.57 | 0.50 | -0.93 to 1.04 | 0.910 |
| T66 Cortical area Z score | ||||
| Pre/Posta | -1.02 | 0.75 | -2.48 to 0.44 | 0.172 |
| Puberty score | 0.29 | 0.31 | -0.33 to 0.90 | 0.360 |
| Age | -1.21 | 0.86 | -2.91 to 0.48 | 0.161 |
| Weight | 0.02 | 0.03 | -0.04 to 0.07 | 0.609 |
| 1 RM leg press | 0.00 | 0.02 | -0.05 to 0.04 | 0.865 |
| Vertical jump | 0.07 | 0.03 | 0.01 to 0.13 | *0.034 |
| Standing broad jump | 0.00 | 0.03 | -0.06 to 0.05 | 0.934 |
| NDI | 0.01 | 0.02 | -0.03 to 0.05 | 0.735 |
| T66 Fracture load X3N | ||||
| Pre/Posta | 369.08 | 164.29 | 47.09 to 691.08 | *0.025 |
| Sexb | -270.67 | 312.20 | -882.57 to 341.23 | 0.386 |
| Puberty score | -81.70 | 96.43 | -270.70 to 107.31 | 0.397 |
| Age | 690.74 | 513.25 | -315.22 to 1696.69 | 0.178 |
| Height | 10.60 | 17.24 | -23.19 to 44.39 | 0.539 |
| Weight | 17.84 | 10.38 | -2.51 to 38.19 | 0.086 |
| 1 RM leg press | 7.99 | 7.54 | -6.79 to 22.77 | 0.289 |
| Vertical jump | 5.14 | 17.79 | -29.72 to 39.99 | 0.773 |
| Standing broad jump | 13.72 | 16.98 | -19.56 to 47.01 | 0.419 |
| NDI | 8.40 | 9.24 | -9.71 to 26.50 | 0.363 |
| T66 Fracture load Y3N | ||||
| Pre/Posta | 590.86 | 258.79 | 83.65 to 1098.07 | *0.022 |
| Sexb | -224.60 | 292.11 | -347.94 to 797.13 | 0.442 |
| Puberty score | 123.73 | 124.84 | -120.95 to 368.41 | 0.322 |
| Age | 409.16 | 521.97 | -613.88 to 1432.20 | 0.433 |
| Height | 12.97 | 17.80 | -21.92 to 47.85 | 0.466 |
| Weight | 0.52 | 13.19 | -25.33 to 26.38 | 0.968 |
| 1 RM leg press | -0.32 | 6.63 | -13.32 to 12.68 | 0.962 |
| Vertical jump | -20.33 | 26.03 | -71.35 to 30.68 | 0.435 |
| Standing broad jump | 6.06 | 18.08 | -29.38 to 41.49 | 0.738 |
| NDI | 14.31 | 10.53 | -6.33 to 34.94 | 0.174 |
Where pre-intervention is the comparison group and β=1;
Where male is the comparison group and β=1.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
Funding
JT is supported by a Commonwealth Research Training Program Doctoral Scholarship. NHH is supported by a Postdoctoral Research Fellowship with Cancer Council of Western Australia.
PC and TR’s work in this project was partly supported by the WA Department of Health FutureHealth WA First Year Initiatives – Mentoring Grant 2016
The funders had no involvement in study design; data collection, analysis and interpretation; writing of the report; or the decision to submit the article for publication.
Authorship contribution
Author #1 is responsible for statistical analysis of the data and prepared the first draft of the paper. Authors #2, #3, #4 and #7 contributed to the bone analysis. Authors #5 and #6 designed and contributed to the exercise intervention. All authors revised the paper critically for intellectual content and approved the final version. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and resolved.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Cairney J, Hay JA, Veldhuizen S, Missiuna C, Faught BE. Developmental coordination disorder, sex, and activity deficit over time:A longitudinal analysis of participation trajectories in children with and without coordination difficulties. Dev Med Child Neurol. 2010;52:e67–e72. doi: 10.1111/j.1469-8749.2009.03520.x. [DOI] [PubMed] [Google Scholar]
- 3.Haga M. Physical fitness in children with high motor competence is different from that in children with low motor competence. Phys Ther. 2009;89:1089–97. doi: 10.2522/ptj.20090052. [DOI] [PubMed] [Google Scholar]
- 4.Hands B. Changes in motor skill and fitness measures among children with high and low motor competence:A five-year longitudinal study. J Sci Med Sport. 2008;11:155–62. doi: 10.1016/j.jsams.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Tsang WWN, Guo X, Fong SSM, Mak K-K, Pang MYC. Activity participation intensity is associated with skeletal development in pre-pubertal children with developmental coordination disorder. Res Dev Disabil. 2012;33:1898–904. doi: 10.1016/j.ridd.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Hands B, Chivers P, McIntyre F, Bervenotti FC, Blee T, Beeson B, et al. Peripheral quantitative computed tomography (pQCT) reveals low bone mineral density in adolescents with motor difficulties. Osteoporos Int. 2015;26:1809–18. doi: 10.1007/s00198-015-3071-8. [DOI] [PubMed] [Google Scholar]
- 7.Fong SSM, Vackova D, Choi A, Cheng YTY, Yam TTT, Guo X. Diversity of activity participation determines bone mineral content in the lower limbs of pre-pubertal children with developmental coordination disorder. Osteoporos Int. 2018;29:917–25. doi: 10.1007/s00198-017-4361-0. [DOI] [PubMed] [Google Scholar]
- 8.Cantell M, Crawford SG, Doyle-Baker PK. Physical fitness and health indices in children, adolescents and adults with high or low motor competence. Hum Movement Sci. 2008;27:344–62. doi: 10.1016/j.humov.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Chivers P, Rantalainen T, McIntyre F, Hands B, Weeks BK, Beck B, et al. Suboptimal bone status for adolescents with low motor competence and developmental coordination disorder:It's sex specific. Res Dev Disabil. 2019:84. doi: 10.1016/j.ridd.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins M, Hart NH, Nimphius S, Chivers P, Rantalainen T, Rothacker KM, et al. Characterisation of peripheral bone mineral density in youth at risk of secondary osteoporosis - a preliminary insight. J Musculoskelet Neuronal Interact. 2019 Accepted Article. [PMC free article] [PubMed] [Google Scholar]
- 11.Ma D, Morley R, Jones G. Risk-taking, coordination and upper limb fractures in children:A population based case-control study. Osteoporos Int. 2004;15:633–8. doi: 10.1007/s00198-003-1579-9. [DOI] [PubMed] [Google Scholar]
- 12.Ma AWW, Fong SSM, Guo X, Liu KPY, Fong DYT, Bae YH, et al. Adapted taekwondo training for prepubertal children with developmental coordination disorder:A randomized, controlled trial. Sci Rep. 2018;8:1–9. doi: 10.1038/s41598-018-28738-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hart NH, Nimphius S, Rantalainen T, Ireland A, Siafarikas A, Newton RU. Mechanical basis of bone strength:Influence of bone material, bone structure and muscle action. J Musculoskelet Neuronal Interact. 2017;17:114–39. [PMC free article] [PubMed] [Google Scholar]
- 14.MacKelvie KJ, Khan KM, McKay HA. Is there a critical period for bone response to weight-bearing exercise in children and adolescents?A systematic review. Br J Sports Med. 2002;36:250–7. doi: 10.1136/bjsm.36.4.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hind K, Burrows M. Weight-bearing exercise and bone mineral accrual in children and adolescents:A review of controlled trials. Bone. 2007;40:14–27. doi: 10.1016/j.bone.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Bernardoni B, Thein-Nissenbaum J, Fast J, Day M, Li Q, Wang S, et al. A school-based resistance intervention improves skeletal growth in adolescent females. Osteoporos Int. 2014;25:1025–32. doi: 10.1007/s00198-013-2535-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu J, Lombardi G, Jiao W, Banfi G. Effects of exercise on bone status in female subjects, from young girls to postmenopausal women:An overview of systematic reviews and meta-analyses. Sports Med. 2016;46:1165–82. doi: 10.1007/s40279-016-0494-0. [DOI] [PubMed] [Google Scholar]
- 18.Vlachopoulos D, Barker AR, Ubago-Guisado E, Williams CA, Gracia-Marco L. A 9-month jumping intervention to improve bone geometry in adolescent male athletes. Med Sci Sports Exerc. 2018;50:2544–54. doi: 10.1249/MSS.0000000000001719. [DOI] [PubMed] [Google Scholar]
- 19.Blimkie CJ, Rice S, Webber CE, Martin J, Levy D, Gordon CL. Effects of resistance training on bone mineral content and density in adolescent females. Can J Physiol Pharmacol. 1996;74:1025. [PubMed] [Google Scholar]
- 20.Nichols DL, Sanborn CF, Love AM. Resistance training and bone mineral density in adolescent females. J Pediatr. 2001;139:494–500. doi: 10.1067/mpd.2001.116698. [DOI] [PubMed] [Google Scholar]
- 21.Ireland AJ, Rittweger J. Exercise for osteoporosis:how to navigate between overeagerness and defeatism. J Musculoskelet Neuronal Interact. 2017;17:155–61. [PMC free article] [PubMed] [Google Scholar]
- 22.Nikander R, Sievänen H, Heinonen A, Daly RM, Uusi-Rasi K, Kannus P. Targeted exercise against osteoporosis:A systematic review and meta-analysis for optimising bone strength throughout life. BMC Med. 2010;8:47. doi: 10.1186/1741-7015-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martini R, Wall AET, Shore BM. Metacognitive processes underlying psychomotor performance in children with differing psychomotor abilities. Adapt Phys Act Q. 2004;21:248–68. [Google Scholar]
- 24.Yu JJ, Burnett AF, Sit CH. Motor skill interventions in children with developmental coordination disorder:A systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99:2076–99. doi: 10.1016/j.apmr.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Hands B, Chivers P, Grace T, McIntyre F. Time for change:Fitness and strength can be improved and sustained in adolescents with low motor competence. Res Dev Disabil. 2018 doi: 10.1016/j.ridd.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 26.McIntyre F, Chivers P, Larkin D, Rose E, Hands B. Exercise can improve physical self perceptions in adolescents with low motor competence. Hum Movement Sci. 2015;42:333–43. doi: 10.1016/j.humov.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Faigenbaum AD, Kraemer WJ, Blimkie CJR, Jeffreys I, Micheli LJ, Nitka M, et al. Youth resistance training:Updated position statement paper from the national strength and conditioning association. J Strength Cond Res. 2009;23(Suppl5):S60–S79. doi: 10.1519/JSC.0b013e31819df407. [DOI] [PubMed] [Google Scholar]
- 28.Falk B, Braid S, Moore M, Yao M, Sullivan P, Klentrou N. Bone properties in child and adolescent male hockey and soccer players. J Sci Med Sport. 2010;13:387–91. doi: 10.1016/j.jsams.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 29.Bernhardt DT, Gomez J, Johnson MD, Martin TJ, Rowland TW, Small E, et al. Strength training by children and adolescents. Pediatrics. 2001;107:1470. doi: 10.1542/peds.107.6.1470. [DOI] [PubMed] [Google Scholar]
- 30.Ashby RL, Ward KA, Roberts SA, Edwards L, Mughal MZ, Adams JE. A reference database for the Stratec XCT-2000 peripheral quantitative computed tomography (pQCT) scanner in healthy children and young adults aged 6-19 years. Osteoporos Int. 2009;20:1337–46. doi: 10.1007/s00198-008-0800-2. [DOI] [PubMed] [Google Scholar]
- 31.Brooks-Gunn J, Warren MP, Rosso J, Gargiulo J. Validity of self-report measures of girls'pubertal status. Child Dev. 1987;58:829–41. [PubMed] [Google Scholar]
- 32.Bond L, Clements J, Bertalli N, Evans-Whipp T, McMorris BJ, Patton GC, et al. A comparison of self-reported puberty using the Pubertal Development Scale and the Sexual Maturation Scale in a school-based epidemiologic survey. J Adolesc. 2006;29:709–20. doi: 10.1016/j.adolescence.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 33.Robertson EB, Skinner ML, Love MM, Elder GH, Conger RD, Dubas JS, et al. The Pubertal Development Scale:A rural and suburban comparison. J Early Adolesc. 1992;12:174–86. [Google Scholar]
- 34.McCarron LT. McCarron assessment of neuromuscular development. 3rd ed. Dallas,TX: McCarron; 1997. [Google Scholar]
- 35.Thomas C, Dos'Santos T, Comfort P, Jones PA. Between-session reliability of common strength - and power-related measures in adolescent athletes. Sports. 2017;5:15. doi: 10.3390/sports5010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nuzzo JL, Anning JH, Scharfenberg JM. The reliability of three devices used for measuring vertical jump height. J Strength Cond Res. 2011;25:2580–90. doi: 10.1519/JSC.0b013e3181fee650. [DOI] [PubMed] [Google Scholar]
- 37.Kraemer WJ, Ratamess N, Fry AC, Triplett-McBride T, Koziris LP, Bauer JA, et al. Influence of resistance training volume and periodization on physiological and performance adaptations in collegiate women tennis players. The American Journal of Sports Medicine. 2000;28:626–33. doi: 10.1177/03635465000280050201. [DOI] [PubMed] [Google Scholar]
- 38.Levinger I, Goodman C, Hare DL, Jerums G, Toia D, Selig S. The reliability of the 1RM strength test for untrained middle-aged individuals. J Sci Med Sport. 2009;12:310–6. doi: 10.1016/j.jsams.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 39.Faigenbaum AD, Milliken LA, Westcott WL. Maximal strength testing in healthy children. J Strength Cond Res. 2003;17:162–6. doi: 10.1519/1533-4287(2003)017<0162:mstihc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 40.IBM Corporation. IBM SPSS Statistics for Windows. 24 ed. Armonk, NY: IBM Corp; 2016. [Google Scholar]
- 41.Lenhard W, Lenhard A. Calculation of Effect Sizes. Dettelbach (Germany): Psychometrica; 2016. [Google Scholar]
- 42.Haapasalo H, Kontulainen S, Sievänen H, Kannus P, Järvinen M, Vuori I. Exercise-induced bone gain is due to enlargement in bone size without a change in volumetric bone density:A peripheral quantitative computed tomography study of the upper arms of male tennis players. Bone. 2000;27:351–7. doi: 10.1016/s8756-3282(00)00331-8. [DOI] [PubMed] [Google Scholar]
- 43.Gabel L, Macdonald HM, Nettlefold L, McKay HA. Physical activity, sedentary time, and bone strength from childhood to early adulthood:A mixed longitudinal HR-pQCT study. J Bone Miner Res. 2017;32:1525–36. doi: 10.1002/jbmr.3115. [DOI] [PubMed] [Google Scholar]
- 44.Wrotniak BH, Epstein LH, Dorn JM, Jones KE, Kondilis VA. The relationship between motor proficiency and physical activity in children. Pediatrics. 2006;118:e1758. doi: 10.1542/peds.2006-0742. [DOI] [PubMed] [Google Scholar]
- 45.Rivilis I, Hay J, Cairney J, Klentrou P, Liu J, Faught BE. Physical activity and fitness in children with developmental coordination disorder:A systematic review. Res Dev Disabil. 2011;32:894–910. doi: 10.1016/j.ridd.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 46.Allen MR, Burr DB. Burr DBA M.R, editor. Bone modeling and remodeling. Basic and Applied Bone Biology:Academic Pressure. 2014:75–90. [Google Scholar]
- 47.Kemmler W, von Stengel S, Engelke K, Häberle L, Kalender WA. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women:The randomized controlled senior fitness and prevention (SEFIP) study. Arch Intern Med. 2010;170:179–85. doi: 10.1001/archinternmed.2009.499. [DOI] [PubMed] [Google Scholar]


