Abstract
Objective
Italy has been largely involved by the COVID-19 pandemic. The present study aimed at evaluating the impact of the lockdown during the pandemic on mental health adopting both a longitudinal and a cross-sectional design. Accordingly, the study investigated general psychopathology a few weeks before the COVID-19 outbreak (T0) and during lockdown (T1), and the associations between lockdown-related environmental conditions, self-perceived worsening in daily living and psychopathology.
Methods
130 subjects (aged 18–60 years) were included in the longitudinal design, and an additional subsample of 541 subjects was recruited for the in-lockdown evaluation. Socio-demographic data and the Brief Symptom Inventory were collected both at T0 and T1. Moreover, at T1 an online survey was administered for the evaluation of lockdown-related environmental conditions and self-perceived variations in daily living induced by quarantine, along with the Impact of Event Scale-Revised.
Results
Longitudinal analysis showed that phobic anxiety and depressive symptoms increased at T1 as compared with T0, whereas interpersonal sensitivity and paranoid ideation decreased. Pre-existing general psychopathology predicted COVID-19-related post-traumatic symptomatology. Cross-sectional analyses underlined that self-perceived deteriorations in various areas of daily living were associated with general and post-traumatic psychopathology, and with several lockdown-related conditions, especially economic damage.
Conclusion
The present study underlined a different trend of increased internalizing and decreased interpersonal symptoms during COVID-19 quarantine in Italy. Furthermore, the results showed that subjects with pre-existing psychopathology and those reporting economic damage during the pandemic were more likely to develop deterioration of their mental health.
Keywords: Covid-19, Post-traumatic stress disorders, Lockdown, Quarantine, Pandemic, Depression
Highlights
-
•
COVID-19 impacted on many daily living aspects and self-perceived mental health.
-
•
There was an increase in depression and phobic anxiety during the lockdown.
-
•
Interpersonal sensitivity and paranoid ideation decreased during the lockdown.
-
•
Economic damage was associated with psychological and behavioural deteriorations.
-
•
Pre-lockdown psychopathology predicted the likelihood of PTSD symptoms onset.
1. Introduction
The first cases of Coronavirus Disease 2019 (COVID-19) in Italy were reported on the 31st of January 2020 in two tourists in Rome, and the first epidemic outbreak was detected in northern Italy at the end of February 2020 [1]. The emergence of the epidemic created a confused and rapidly evolving situation. After the spread of the first cases, the national and regional governments imposed a progressively increasing level of isolation, with the final general lockdown sanctioned by the Decree of the President of the Council of Ministers (DPCM) of March 9th, 2020 [2]. To lower the risk of further disease transmission, the authority suspended many activities, such as schools, factories, offices, restaurants, cinemas and almost all the recreational activities. People not involved in indispensable activities were mandatorily confined at home.
Psychopathological consequences of the COVID-19 pandemic and related adversities are still a matter of debate in the scientific literature [3]. People may experience an increased sense of efficacy, adapting to the situational needs and remaining effective in their work and families. However, others may experience adverse mental states, worsening pre-existing psychopathology or developing psychiatric symptoms [4], especially depression, anxiety, post-traumatic stress disorder (PTSD) and suicidal ideation [5]. Previous studies on similar events such as the SARS outbreak reported an increased prevalence of anger [6], emotional exhaustion [7], low mood and irritability [8]. Furthermore, people may report fear, nervousness, sadness, guilt [9,10], frustration and boredom due to confinement, loss of usual routine, and reduced social and physical contact with other people [[11], [12], [13]]. Consequently, several problematic behaviours (e.g. binge eating, alcohol consumption) may increase during quarantine, as dysfunctional ways to manage aversive emotional states [4,13].
Up to now, the scientific literature provided a large number of cross-sectional observations regarding different psychopathological features and behaviours following the spread of COVID-19, and the first meta-analyses focused particularly on depression and anxiety symptoms [[14], [15], [16], [17], [18]]. However, only a few data are available concerning subjectively reported worsening in some areas, such as relationships, overeating and fear of gaining weight, increased use of social networks and drugs to manage stress, while to date there are no studies that investigated the relationship between these variables and post-traumatic stress or general psychopathology. Furthermore, although some longitudinal studies are already available [[19], [20], [21], [22], [23], [24], [25], [26], [27], [28]], only a few of them considered the psychopathological characteristics of the general population before the spread of COVID-19 [[29], [30], [31], [32]], and none of these studies investigated a large spectrum of psychopathology, including also interpersonal sensitivity, paranoid ideation, psychoticism, and hostility.
Finally, regarding the individual vulnerability to the adverse conditions during COVID-19 outbreak, several factors occurring during quarantine might interact with pre-existing vulnerability conditions in determining different reactions. Some of these include social distancing, self-isolation, forced cohabitation with one's family which can exacerbate the adverse interactions between family members, or finally reporting severe economic damage [33].
The present study attempted to overcome some of the limitations of the existing literature through a double design including both a longitudinal and a cross-sectional observation. A group of subjects were recruited before the spread of COVID-19, and they were re-evaluated during lockdown (longitudinal study). An additional subsample of participants was assessed during quarantine (cross-sectional evaluation), in order to strengthen the evaluation of in-lockdown specific associations between self-perceived worsening in daily living and various areas of psychopathology.
Thus, the aims of the present study were as follows: 1) to analyze the variation of specific psychopathological features after the beginning of the lockdown as compared with an evaluation performed before the spread of COVID-19 pandemic in a sample of the Tuscan population (longitudinal design); 2) to evaluate predictors of psychopathological change (longitudinal design); 3) to evaluate the prevalence of pathological behaviours and psychopathological distress and the associations with different adverse conditions consequent to the COVID-19 pandemic (cross-sectional design).
2. Method
2.1. Study design
The longitudinal observation involved subjects recruited in the Italian general population a few weeks before the first cases of COVID-19 (T0) who were re-evaluated six weeks after the Italian Government declaration of lockdown [2] (T1). The cross-sectional observation was performed at T1 and it included both data regarding the subsample of subjects included in the longitudinal design and data of additional subjects recruited at T1.
2.2. Participants and procedure
The study was designed as an online survey by the Psychiatric Unit of the University of Florence, and it was approved by the Ethics Committee of the Institution. All subjects were asked to provide consent for their participation. Participants were recruited using convenience and snowball sampling methods, with the following inclusion criteria: age between 18 and 60 years, Italian nationality, being resident in Tuscany. Exclusion criteria included: illiteracy or inability to provide the consent or to complete the survey online. A series of 50 participants were initially selected to limit the selection bias associated with the non-probabilistic sampling method and to cover the age group, gender, and geographical area. The initial subjects were selected by sharing the research protocol in the University spaces of the structure and on the community pages on the main social media. Each selected participant was then asked to choose ten people they considered suitable for the survey and to send them the questionnaire. Further participants were reached out in the same way until data saturation.
2.2.1. Longitudinal observation
The cohort for the longitudinal observation was originally recruited from December 1st, 2019 until January 15th, 2020 (T0), as part of an observational study on mental health in the Tuscan general population. The follow-up evaluation (T1) was performed from April 22nd, 2020 until May 3rd, 2020. The present time frame covered the advanced phase of the COVID-19 pandemic in Italy, starting one month and a half after the declaration of lockdown [2] until the last days of the so-called “phase one” of the lockdown. Of the initial cohort of 153 subjects included in the pre-COVID-19 investigation, 130 agreed to perform the follow-up survey (32 men and 98 women).
2.2.2. Cross-sectional observation
The recruitment for the cross-sectional study was performed during the same period of the follow-up of the longitudinal design (T1). Of the 624 participants who were invited, 83 refused to participate and 541 (160 men and 381 women) were recruited into the cross-sectional study.
2.3. Assessment and measures
The baseline evaluation (T0) of the participants selected for the longitudinal observation included socio-demographic data and the Brief Symptom Inventory (BSI) [34], a self-administered questionnaire for the evaluation of general psychopathology. It provides nine subscales: Somatization, Obsessive-Compulsive, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation and Psychoticism. An overall index (Global Severity Index – GSI) can be obtained by averaging the scores obtained in all items. The BSI was chosen because it allowed investigating psychopathological features related to the interpersonal area (such as hostility, paranoid ideation and interpersonal sensitivity) which was substantially neglected in previous longitudinal studies; furthermore, the fact that data before the spread of COVID-19 in Italy were available for this questionnaire made it possible to carry out a longitudinal assessment.
At T1 all subjects were asked to provide the following data: age, gender, height and weight, educational level, occupation, marital status, and geographical area of residence. Moreover, the BSI was administered alongside a dedicated, self-report questionnaire, set up to collect the following data:
-
-
Lockdown-related environmental conditions: having a partner, living alone, changes in working activities, having a loved one with a confirmed diagnosis of COVID-19, having personally received this diagnosis, being unable to see one's partner because of lockdown, reporting a moderate to severe economic damage because of COVID-19 pandemic, having left home during the previous seven days.
-
-
Self-perceived variations in different areas of daily living and dysfunctional behaviours induced by lockdown: deterioration of the relationships with relatives, increase in household arguments, worsening of quality of sleep and sexual functioning, increase in episodes of overeating, fear of gaining weight, use of drugs against stress, use of social media. Although the nature of this part of the survey was cross-sectional, the questionnaire specifically investigated subjectively perceived worsening in the areas described above, in an attempt to better characterize how participants experienced the impact of lockdown on their psychological well-being.
All these data were collected either as dummy variables (e.g. living alone or not) or through a Likert scale ranging from zero (0) to severe (3).
Finally, the T1 evaluation comprehended the Impact of Event Scale – Revised (IES-R) [35], a self-administered questionnaire for the assessment of post-traumatic stress symptoms. Participants were specifically asked to fill it in considering the COVID-19 health emergency and the subsequent lockdown as the reference traumatic event. The questionnaire provides three subscales (Intrusion, Avoidance and Hyperarousal) and a total score. A cut-off point of 33 can be used to identify subjects at higher risk for PTSD [35].
2.4. Statistical analyses
All self-perceived COVID-19-related variations were coded and analyzed as dummy variables, dichotomized by assigning a value equal to 1 to moderate and severe variations, and 0 to absent or slight ones.
Comparisons between groups were carried out using independent samples t-test and chi-square test. Binomial logistic regression analysis was used to investigate the association of self-perceived variations with lockdown conditions and psychopathological measures. For every self-perceived variation (inserted as dependent variable), two multivariate models were run: one with BSI-GSI and the three subscales of IES-R as independent variables, and one with all lockdown-related conditions. Age, gender, and educational level were included as covariates. For the cross-sectional study, the two samples evaluated at T1 were analyzed together.
Linear mixed model analysis with random intercept was used to test for variations in BSI scores between time points. Through post hoc power analysis, it was computed that with the sample size obtained, a power of 99% was reached to identify at least an average effect size (equal to 0.25) for the within-subject factor in a repeated-measures analysis of variance (α = 0.05). Moreover, binomial logistic and linear regressions were run to test whether baseline (T0) general psychopathology could predict COVID-19-related variations and post-traumatic symptoms.
All statistical analyses were performed using IBM SPSS Statistics v.25 [36] and G*Power v.3.1.9.7 [37].
3. Results
The final sample consisted of 671 subjects (479 females and 192 males): 130 participants with both pre-lockdown (T0) and in-lockdown (T1) evaluations, and 541 additional subjects recruited at T1. Table 1 shows the socio-demographic characteristics of the whole sample at T1.
Table 1.
Socio-demographic and lockdown-related environmental conditions divided by sex, together with comparisons between groups. Continuous variables are expressed as mean ± standard deviation, whereas dichotomous variables are expressed as frequencies and percentages.
| Women (n = 479) | Men (n = 192) | t-test (t)/Chi-Square (χ2) | |
|---|---|---|---|
| Age (years) | 33.10 ± 14.07 | 34.95 ± 13.99 | −1.55 |
| BMI (kg/m2) | 21.31 ± 3.24 | 23.87 ± 3.02 | −9.13⁎⁎⁎ |
| Graduates | 279 (58.2) | 122 (63.5) | 1.60 |
| Not working | 263 (54.9) | 82 (42.7) | 8.16⁎⁎ |
| Having a partner | 336 (70.1) | 137 (71.4) | 0.10 |
| Being unable to see the partner | 147 (30.7) | 48 (25.0) | 2.15 |
| Living alone | 46 (9.6) | 30 (15.6) | 4.95⁎ |
| Having a loved one with COVID-19 | 37 (7.7) | 20 (10.4) | 1.28 |
| Reporting a moderate to severe economic damage because of COVID-19 pandemic | 151 (31.6) | 46 (24.1) | 1.22 |
| Not having left home in the last 7 days | 145 (30.3) | 35 (18.2) | 10.13⁎⁎ |
BMI = Body Mass Index.
p < 0.05;
p < 0.01;
p < 0.001.
3.1. Longitudinal observation: Before COVID-19 outbreak vs during lockdown
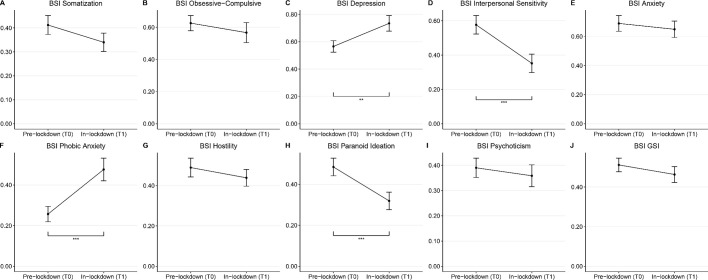
A significant increase of depressive (T0: 0.57 ± 0.48; T1: 0.73 ± 0.65; p = 0.003) and phobic anxiety symptoms (T0: 0.26 ± 0.43; T1: 0.48 ± 0.63; p < 0.001) was observed. Conversely, Interpersonal Sensitivity (T0: 0.58 ± 0.61; T1: 0.35 ± 0.61; p < 0.001) and Paranoid Ideation scores (T0: 0.49 ± 0.49; T1: 0.32 ± 0.49; p < 0.001) significantly decreased during the lockdown. No significant longitudinal variations in Somatization (T0: 0.41 ± 0.45; T1: 0.34 ± 0.44; p = 0.155), Obsessive-Compulsive (T0: 0.63 ± 0.54; T1: 0.57 ± 0.71; p = 0.325), Anxiety (T0: 0.69 ± 0.62; T1: 0.65 ± 0.64; p = 0.453), Hostility (T0: 0.49 ± 0.53; T1: 0.44 ± 0.48; p = 0.302), Psychoticism (T0: 0.39 ± 0.44; 0.36 ± 0.49; p = 0.482) or BSI-GSI (T0: 0.51 ± 0.39; T1: 0.46 ± 0.46; p = 0.198) were observed during the lockdown. Longitudinal trends of all psychopathological domains are shown in Fig. 1 .
Fig. 1.
Longitudinal course of psychopathological features. Statistically significant variations are highlighted as following: ⁎⁎ = p < 0.01; ⁎⁎⁎ = p < 0.001.
BSI = Brief Symptom Inventory; GSI = Global Severity Index.
Furthermore, greater pre-lockdown psychopathology was associated with an increased likelihood of perceiving a deterioration in relationships, quality of sleep and sexual functioning, a worsening of fear of gaining weight, and increased use of social networks and episodes of overeating (Table 2 ).
Table 2.
Data on self-perceived variations induced by COVID-19 pandemic divided by sex, together with comparisons between groups and psychopathological and lockdown-related correlates.
| Women (n = 479) | Men (n = 192) | Chi-square (χ2) | Predictors (OR with 95% CI) |
|||
|---|---|---|---|---|---|---|
| Psychopathological correlates assessed pre-lockdown (T0, n = 130) | Psychopathological correlates assessed in-lockdown (T1, n = 671) | Lockdown-related environmental conditions (n = 671) | ||||
| Worsened relationship with relatives | 103 (21.5) | 21 (10.9) | 10.16⁎⁎ | BSI-GSI: 3.43 [1.45–8.12]⁎⁎ | BSI-GSI: 2.30 [1.63–3.24]⁎⁎⁎ | Having a partner: 0.17 [0.07–0.41]⁎⁎⁎ |
| Being unable to see the partner: 2.78 [1.08–7.17]⁎ | ||||||
| Having a loved one with COVID-19: 2.52 [1.16–5.47]⁎ | ||||||
| Intensification of household arguments | 88 (26.0) | 13 (12.6) | 8.04⁎⁎ | BSI-GSI: 2.32 [1.59–3.39]⁎⁎⁎ | Having a partner: 0.25 [0.12–0.55]⁎⁎⁎ | |
| Living alone: 0.15 [0.03–0.70]⁎ | ||||||
| Being unable to see the partner: 2.30 [1.06–5.01]⁎ | ||||||
| Worsened quality of sleep | 228 (47.6) | 51 (26.6) | 24.97⁎⁎⁎ | BSI-GSI: 4.88 [1.90–2.51]⁎⁎ | IES-HY: 3.42 [2.20–5.30]⁎⁎⁎ | Economic damage: 2.14 [1.24–3.68]⁎⁎ |
| BSI-GSI: 1.53 [1.09–2.15]⁎ | ||||||
| Worsened sexual functioning | 161 (33.6) | 63 (32.8) | 0.04 | BSI-GSI: 3.47 [1.49–8.10]⁎⁎ | IES-HY: 1.82 [1.23–2.70]⁎⁎ | Economic damage: 3.40 [1.94–5.95]⁎⁎⁎ |
| Increased overeating | 108 (22.5) | 24 (12.5) | 8.76⁎⁎ | BSI-GSI: 5.32 [1.92–4.74]⁎⁎ | IES-AV: 1.53 [1.02–2.28]⁎ | Not having left home: 1.91 [1.03–3.55]⁎ |
| BSI-GSI: 3.78 [2.61–5.49]⁎⁎⁎ | Having a partner: 0.29 [0.13–0.63]⁎⁎ | |||||
| Being unable to see the partner: 2.33 [1.04–5.25]⁎ | ||||||
| Increased fear of getting fat | 245 (51.1) | 58 (30.2) | 24.27⁎⁎⁎ | BSI-GSI: 3.13 [1.37–7.16]⁎⁎ | IES-AV: 1.55 [1.09–2.20]⁎ | Having a partner: 0.35 [0.17–0.71]⁎⁎ |
| BSI-GSI: 3.24 [2.19–4.79]⁎⁎⁎ | Economic damage: 1.81 [1.00–3.25]⁎ | |||||
| Increased resort to drugs against stress | 17 (7.5) | 1 (1.7) | 2.58 | BSI-GSI: 4.29 [2.10–8.73]⁎⁎⁎ | Being unable to see the partner: 5.91 [1.44–24.26]⁎ | |
| Increased use of social networks | 305 (63.7) | 113 (58.9) | 1.36 | BSI-GSI: 2.84 [1.16–6.96]⁎ | IES-HY: 1.75 [1.15–2.68]⁎ | Having a partner: 0.30 [0.15–0.61]⁎⁎ |
| BSI-GSI: 1.58 [1.09–2.27]⁎ | Being unable to see the partner: 2.32 [1.15–4.68]⁎ | |||||
| Economic damage: 2.23 [1.19–4.17]⁎ | ||||||
AV = Avoidance; BSI-GSI = Brief Symptom Inventory-Global Severity Index; CI = Confidence Interval; IES = Impact of Event Scale; HY = Hyperarousal; IN = Intrusion; OR = Odds Ratio.
p < 0.05;
p < 0.01;
p < 0.001.
Finally, pre-lockdown general psychopathology significantly predicted COVID-19-related post-traumatic symptomatology at follow-up (Fig. 2 ). In particular, for each one-unit increase in the pre-lockdown BSI-GSI scores, subjects had 12.70 times higher odds to exhibit COVID-19-related IES scores compatible with PTSD at the in-lockdown follow-up (95% CI: 3.24–49.81, p < 0.001).
Fig. 2.
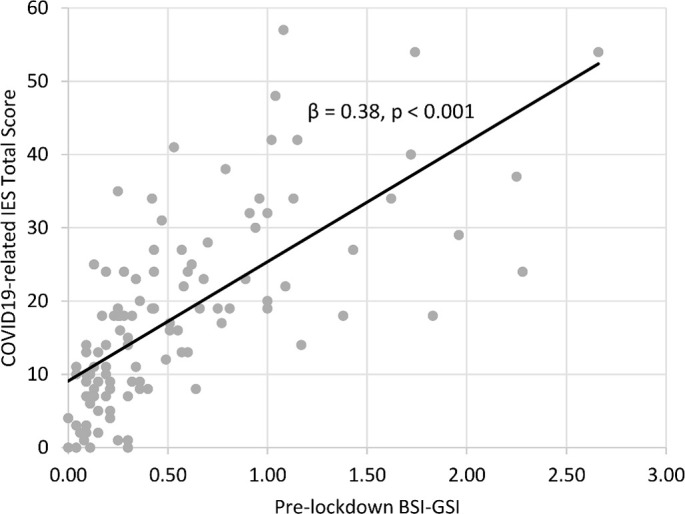
Scatter plot illustrating the relationship between pre-existing (pre-lockdown) general psychopathology and COVID-19-related post-traumatic stress symptoms.
BSI-GSI = Brief Symptom Inventory-Global Severity Index; IES = Impact of Event Scale.
3.2. Cross-sectional observation performed during lockdown
Only two of the participants (0.3%) reported a confirmed COVID-19 diagnosis. The descriptive statistics concerning the psychopathology measures at T1 are reported in Table S1 of Supplementary Materials. Table 2 shows the frequencies of different areas of self-perceived deterioration due to COVID-19 pandemic. Table 2 also shows the associations of subjectively perceived deteriorations with in-lockdown psychopathology and lockdown-related conditions. General psychopathology was associated with worsening relationships with relatives, increase in household arguments, overeating, fear of getting fat, use of social networks and medication against stress, and deterioration of the quality of sleep (Table 2). The IES-R Hyperarousal subscale was positively associated with a self-perceived increase in the use of social networks, and with the worsening of sexual function and sleep (Table 2). Furthermore, the intensification of overeating and fear of getting fat positively correlated with IES-R Avoidance subscale. Regarding the lockdown-related environmental conditions, the perception of having had moderate to severe economic damage was associated with increased social-networking, worsening of sleep and sexual functioning (Table 2). Furthermore, economic damage was associated with increased fear of getting fat (Table 2). Having a partner was negatively associated with worsening of relationships with relatives, increase in household arguments, social networks use, overeating and fear of getting fat (Table 2). Conversely, being unable to see the partner was positively associated with most of the aforementioned conditions, and with the resort to medications against stress (Table 2). Finally, having a loved one with COVID-19 was associated with worsening of family relationships (Table 2).
4. Discussion
To the best of our knowledge, this is one of the first studies which attempted to evaluate the psychopathological impact of COVID-19 outbreak in the Italian population, adopting both a longitudinal comparison of pre vs post lockdown psychopathological distress and a cross-sectional evaluation performed during lockdown. Overall, the present study confirmed that COVID-19 pandemic significantly impacted on various aspects of mental health and daily living [12,[38], [39], [40], [41]].
For the first time, the longitudinal design allowed to describe an opposed trend of internalizing symptomatology and interpersonal distress. Indeed, on one side, phobic anxiety and depressive symptoms increased during lockdown, as previously observed by other studies [[24], [25], [26]], whereas on the other hand interpersonal sensitivity and paranoid ideation resulted to be decreased, underlying a kind of “positive” effect of social isolation for some persons. These results are in line with a previous study, which observed lower interpersonal sensitivity and paranoid ideation in subjects who were forced into isolation during COVID-19 quarantine, compared to those who could leave the house [42]. Accordingly, it might be speculated that for vulnerable persons, reduced social stressors might reduce paranoid ideation [43,44]. Regarding the study of risk factors for deterioration of mental health during lockdown, the advantage of a longitudinal design allowed to demonstrate that persons with pre-existing psychopathological traits were more likely to perceive a deterioration of their mental status. In particular, the odds of developing severe COVID-19-related post-traumatic symptomatology increased by 12.70 times for each BSI-GSI point obtained before the spread of COVID-19 pandemic. Moreover, pre-existing psychopathology resulted to be associated with a higher probability of perceiving COVID-19 pandemic-induced deteriorations in different areas of daily living, including relationships with family members, quality of sleep, sexual satisfaction, overeating, fear of getting fat, and use of social networks, confirming previous observations [45].
The cross-sectional survey showed that several self-perceived deteriorations of daily living and environmental conditions were associated with general and post-traumatic psychopathology during lockdown. In particular, economic damage was one of the most relevant predictors of self-perceived deteriorations in various areas of daily living and mental health, including deterioration of relationships, sleep quality and sexual functioning, confirming previous observations [46,47]. As for romantic relationships, having a partner was a protective factor against self-perceived deteriorations, as observed by Taylor et al. during the first outbreak of equine influenza [48]. However, being unable to see the partner was associated with increased relational conflicts, overeating, use of social media and use of drugs to manage stress. Regarding the associations between psychopathology and self-perceived deteriorations, particular attention deserves the relationship between post-traumatic stress symptoms and overeating, which can be interpreted as a dysfunctional coping strategy to manage aversive emotional states rising from the isolation of the quarantine [4]. Furthermore, post-traumatic symptoms were predicted also by the use of social media. Social media were described as the prior source of information during the lockdown [49,50]. Thus, the overwhelming information regarding COVID-19 pandemic might perpetuate the sense of danger and uncertainty among persons [51]. On the opposite, the lack of clarity of media and the scarce transparency from health and government officials might increase the sense of fear [9,13,41].
The results of the present study should be considered in the light of some limitations: first of all, despite the efforts of recruiting a heterogeneous sample, the online survey limited the age range of the included persons; therefore, the conclusions may not be generalized to the wider population. The sample size for the longitudinal study is small, and the number of analyses performed may have increased the possibility of Type I errors. A large proportion of information was obtained through self-reported questionnaires. The questionnaire used to investigate lockdown-related environmental conditions and self-perceived variations did not collect information on adherence to COVID-19 protective behaviours and did not contain validated measures; moreover, since some items were formulated to only investigate negative variations, it is plausible that they were directionally biased. Furthermore, these items were dichotomized to avoid over-parameterization of statistical models, and this process could have led to a loss of data. Finally, a pre-lockdown assessment of psychiatric diagnosis or therapy was not available.
In conclusion, the COVID-19 pandemic should be considered as a novel form of stressor or traumatic experience, with different psychopathological consequences as compared with other natural disasters, such as earthquakes, tsunamis or wars [33]. In particular, the present study demonstrated peculiarities in psychopathological consequences of the lockdown with opposite trends of internalizing symptoms (i.e. phobic anxiety and depression), paranoid symptoms and interpersonal distress. Moreover, the present study identified subjects with pre-existing psychopathology as more vulnerable to the worse outcome associated with lockdown, particularly in terms of post-traumatic symptomatology. Finally, the economic insecurity was associated with a worse psychopathological outcome, confirming the importance of providing adequate support to people in precarious economic conditions.
The following are the supplementary data related to this article.
In-lockdown psychopathological characteristics of the sample divided by sex, together with comparisons between groups.
Authors' contributions
All Authors contributed to the conceptualization, data curation, formal analysis and methodology of the research, and to the writing, review and editing of the manuscript.
Declaration of Competing Interest
The Authors have no competing interests to report.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Day M. Covid-19: Italy confirms 11 deaths as cases spread from north. BMJ. 2020:m757. doi: 10.1136/bmj.m757. [DOI] [PubMed] [Google Scholar]
- 2.Gazzetta Ufficiale della Repubblica Italiana DECRETO-LEGGE 9 marzo 2020, n. 14. Disposizioni urgenti per il potenziamento del Servizio sanitario nazionale in relazione all'emergenza COVID-19. (20G00030), GU Ser. Gen. n.62 Del 09-03-2020. 2020. https://www.gazzettaufficiale.it/eli/id/2020/03/09/20G00030/sg
- 3.Kontoangelos K., Economou M., Papageorgiou C. Mental health effects of COVID-19 pandemia: a review of clinical and psychological traits. Psychiatry Investig. 2020;17:491–505. doi: 10.30773/pi.2020.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morganstein J.C., Ursano R.J. Ecological disasters and mental health: causes, consequences, and interventions. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J., the COVID-19 Suicide Prevention Research Collaboration Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marjanovic Z., Greenglass E.R., Coffey S. The relevance of psychosocial variables and working conditions in predicting nurses' coping strategies during the SARS crisis: an online questionnaire survey. Int. J. Nurs. Stud. 2007;44:991–998. doi: 10.1016/j.ijnurstu.2006.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:1245–1251. http://www.ncbi.nlm.nih.gov/pubmed/12743065 [PMC free article] [PubMed] [Google Scholar]
- 8.Lee S., Chan L.Y.Y., Chau A.M.Y., Kwok K.P.S., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61:2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desclaux A., Badji D., Ndione A.G., Sow K. Accepted monitoring or endured quarantine? Ebola contacts' perceptions in Senegal. Soc. Sci. Med. 2017;178:38–45. doi: 10.1016/j.socscimed.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 10.DiGiovanni C., Conley J., Chiu D., Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur. Bioterror. 2004;2:265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- 11.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeong H., Yim H.W., Song Y.-J., Ki M., Min J.-A., Cho J., Chae J.-H. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol. Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2020 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ren X., Huang W., Pan H., Huang T., Wang X., Ma Y. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 2020;91:1033–1045. doi: 10.1007/s11126-020-09796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.da Silva Neto R.M., Benjamim C.J.R., de Medeiros Carvalho P.M., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;104:110062. doi: 10.1016/j.pnpbp.2020.110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li H.Y., Cao H., Leung D.Y.P., Mak Y.W. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int. J. Environ. Res. Public Health. 2020;17:3933. doi: 10.3390/ijerph17113933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castellini G., Cassioli E., Rossi E., Innocenti M., Gironi V., Sanfilippo G., Felciai F., Monteleone A.M., Ricca V. The impact of COVID-19 epidemic on eating disorders: a longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int. J. Eat. Disord. 2020 doi: 10.1002/eat.23368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y., Wang Y., Jiang J., Valdimarsdóttir U.A., Fall K., Fang F., Song H., Lu D., Zhang W. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 2020:1–3. doi: 10.1017/S0033291720001555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou Y., MacGeorge E.L., Myrick J.G. Mental health and its predictors during the early months of the COVID-19 pandemic experience in the United States. Int. J. Environ. Res. Public Health. 2020;17:6315. doi: 10.3390/ijerph17176315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ji G., Wei W., Yue K.-C., Li H., Shi L.-J., Ma J.-D., He C.-Y., Zhou S.-S., Zhao Z., Lou T., Cheng J., Yang S.-C., Hu X.-Z. Effects of the COVID-19 pandemic on obsessive-compulsive symptoms among university students: prospective cohort survey study. J. Med. Internet Res. 2020;22 doi: 10.2196/21915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gopal A., Sharma A.J., Subramanyam M.A. Dynamics of psychological responses to COVID-19 in India: a longitudinal study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Planchuelo-Gómez Á., Odriozola-González P., Irurtia M.J., de Luis-García R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J. Affect. Disord. 2020;277:842–849. doi: 10.1016/j.jad.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Creese B., Henley W., O'dwyer S., Silva D., Ballard C. 2020. Loneliness, Physical Activity and Mental Health During Covid-19: A Longitudinal Analysis of Depression and Anxiety Between 2015 and 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pinkham A.E., Ackerman R.A., Depp C.A., Harvey P.D., Moore R.C. A longitudinal investigation of the effects of the COVID-19 pandemic on the mental health of individuals with pre-existing severe mental illnesses. Psychiatry Res. 2020;294:113493. doi: 10.1016/j.psychres.2020.113493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sadiković S., Branovački B., Oljača M., Mitrović D., Pajić D., Smederevac S. Daily monitoring of emotional responses to the coronavirus pandemic in Serbia: a citizen science approach. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.02133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Tilburg T.G., Steinmetz S., Stolte E., van der Roest H., de Vries D.H. Loneliness and mental health during the COVID-19 pandemic: a study among Dutch older adults. J. Gerontol. B. Psychol. Sci. Soc. Sci. 2020 doi: 10.1093/geronb/gbaa111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim A.W., Nyengerai T., Mendenhall E. Evaluating the mental health impacts of the COVID-19 pandemic in Urban South Africa: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. Psychol. Med. 2020 doi: 10.1101/2020.06.13.20130120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U., Ribeaud D., Eisner M. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schäfer S.K., Sopp M.R., Schanz C.G., Staginnus M., Göritz A.S., Michael T. Impact of COVID-19 on public mental health and the buffering effect of a sense of coherence. Psychother. Psychosom. 2020;89:1–7. doi: 10.1159/000510752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63 doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Derogatis L.R., Melisaratos N. The brief symptom inventory: an introductory report. Psychol. Med. 1983;13:595. doi: 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- 35.Creamer M., Bell R., Failla S. Psychometric properties of the impact of event scale—revised. Behav. Res. Ther. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 36.IBM Corp . 2019. IBM SPSS Statistics for Windows, Version 26.0. [Google Scholar]
- 37.Faul F., Erdfelder E., Buchner A., Lang A.-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 38.Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Public Health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Braunack-Mayer A., Tooher R., Collins J.E., Street J.M., Marshall H. Understanding the school community's response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health. 2013;13:344. doi: 10.1186/1471-2458-13-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caleo G., Duncombe J., Jephcott F., Lokuge K., Mills C., Looijen E., Theoharaki F., Kremer R., Kleijer K., Squire J., Lamin M., Stringer B., Weiss H.A., Culli D., Di Tanna G.L., Greig J. The factors affecting household transmission dynamics and community compliance with Ebola control measures: a mixed-methods study in a rural village in Sierra Leone. BMC Public Health. 2018;18:248. doi: 10.1186/s12889-018-5158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reynolds D.L., Garay J.R., Deamond S.L., Moran M.K., Gold W., Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008;136:997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sfendla A., Hadrya F. Factors associated with psychological distress and physical activity during the COVID-19 pandemic. Health Secur. 2020 doi: 10.1089/hs.2020.0062. [DOI] [PubMed] [Google Scholar]
- 43.Pot-Kolder R., Veling W., Counotte J., Van Der Gaag M. Self-reported cognitive biases moderate the associations between social stress and paranoid ideation in a virtual reality experimental study. Schizophr. Bull. 2018;44:749–756. doi: 10.1093/schbul/sbx119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Collip D., Oorschot M., Thewissen V., Van Os J., Bentall R., Myin-Germeys I. Social world interactions: how company connects to paranoia. Psychol. Med. 2011;41:911–921. doi: 10.1017/S0033291710001558. [DOI] [PubMed] [Google Scholar]
- 45.Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Codagnone C., Bogliacino F., Gómez C., Charris R., Montealegre F., Liva G., Lupiáñez-Villanueva F., Folkvord F., Veltri G.A. Assessing concerns for the economic consequence of the COVID-19 response and mental health problems associated with economic vulnerability and negative economic shock in Italy, Spain, and the United Kingdom. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Witteveen D., Velthorst E. Economic Hardship and Mental Health Complaints During COVID-19. Proc Natl Acad Sci USA. 2020;(117) doi: 10.1073/pnas.2009609117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taylor M.R., Agho K.E., Stevens G.J., Raphael B. Factors influencing psychological distress during a disease epidemic: data from Australia's first outbreak of equine influenza. BMC Public Health. 2008;8:347. doi: 10.1186/1471-2458-8-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Osatuyi B. Information sharing on social media sites. Comput. Hum. Behav. 2013;29:2622–2631. doi: 10.1016/j.chb.2013.07.001. [DOI] [Google Scholar]
- 50.Westerman D., Spence P.R., Van Der Heide B. Social media as information source: Recency of updates and credibility of information. J. Comput.-mediated Commun. 2014;19:171–183. doi: 10.1111/jcc4.12041. [DOI] [Google Scholar]
- 51.Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In-lockdown psychopathological characteristics of the sample divided by sex, together with comparisons between groups.