Abstract
Background. The purpose is to investigate the role of the first trimester ultrasound markers: cown rump lengh (CRL), gestational sac volume (GSV), embryonic volume (EV) and yolk sac volume (YSV) as parameters for outcome. Methods. Observational clinical study that was carried out in the Obstetrics and Gynecology Clinic. The study included a number of 81 unselected patients evaluated from the first trimester. Patients were evaluated in the first trimester by transvaginal ultrasound and followed up during pregnancy. Correlations between the GSV, EV, YSV and CRL was made for assessing outcome. Results. Our study results show that patients with abnormal early ultrasound parameters had a higher incidence of pregnancy complications. Conclusions. An early pregnancy evaluation can be a helpful tool in predicting outcome.
Keywords: First trimester, ultrasound, outcome
Introduction
Different ultrasound parameters and maternal demographic characteristics acquired before 12 weeks of gestation were studied [1,2].
Ultrasound has an essential role in pregnancy monitoring and both 2D and volumetric (3D) ultrasound are efficient methods for an accurate first trimester diagnosis [3].
The first trimester ultrasound can predict an abnormal fetal outcome. Literature shows that different ultrasound markers can be used to diagnose risk pregnancies or fetal anomalies [4,5].
It is feasible to measure the gestational sac volumes [6,7] embryonic volumes [6,8], yolk sac volumes [9] and fetus crown rump length [10] accurately and reliably in the first trimester by means of 3D ultrasound [11].
Studies have investigated the use of first trimester volumetric ultrasound in the prediction of miscarriage [11,12,13,14], IUGR and birth weight [15,16,17,18].
Volumetric ultrasound is more accurate and reliable compared to the conventional ultrasound [19,20,21].
Measurement of the CRL is less reliable before 7 weeks and after 10 weeks of gestation [22].
Material and Methods
This study is an observational clinical study that was carried out in the Obstetrics and Gynecology Clinic from the Emergency County Hospital of Craiova between 2016-2019 and included a number of 81 unselected patients. All patients signed a written informed consent agreeing to anonymously participate in this study, and the study was approved by the Ethics Committee of the University of Medicine and Pharmacy of Craiova.
The study inclusion criteria were: patients with singleton pregnancy. The patients were questioned about their medical history. We noted the date of last menstrual period (LMP), parity and other medical history such as smoking or drug usage.
The patients were scanned using a transvaginal probe by an experienced sonographer and the presence of the ultrasound markers were noted. The obtained markers were measured using the VOCAL method. This is a multiplanar method used to acquire sequential plans of the embryo, gestational sac and yolk sac by rotating around its axis. According to the rotation angle established by the observer the displayed plans can be variable in number [23].
In our study we used a 30-degree rotation angle.
We measured the embryo volume directly [23,24] by drawing a contour line along its head and trunk excluding the limbs [25].
The GSV and the yolk sac volume were also calculated using the VOCAL method [9,11].
The data were collected on an Excel sheet and analyzed. Scatter graphs were generated to evaluate the correlation between the collected parameters. A correlation of these ultrasound parameters and pregnancy outcome was made utilizing the Pearson correlation coefficient, in all cases significance was considered for p<0.05.
Results
81 patients were evaluated during the first trimester. The median maternal age was 30 years (ranged between 23 and 44 years). 30 patients were nulliparous and 51 patients were multiparous. 38 patients (46,9%) had a previous birth over 37 weeks of gestation and 19 patients had a previous birth less than 37 weeks (23,5%).
21 patients (25,9%) had a previous vaginal birth and 26 patients (32.1%) had a previous cesarean section.
The mean gestational age according to the CRL was 12 weeks+2 days (ranged between 11w+2d and 13w+1d).
The mean gestational age according to the GSD was 12w+2d (ranged from 9w+6 and 14w+6d).
From the patients medical history, 5 patients (6.2%) had a previous intrauterine fetal death, 7 patients (8.6%) had an intrauterine growth restricted fetus, 13 patients (16%) were diagnosed with preeclampsia, 5 patients (6.2%) have developed gestational diabetes.
Our study results show a first trimester abortion in 10 cases (12.3%) and in 2 cases (2.5%) in the second trimester. 20 cases (24.7%) were diagnosed with intrauterine growth restriction.
By means of CRL, the gestational age in the aborted cases is shown in Table 1.
Table 1.
Gestational age by CRL in the aborted cases
|
|
5.1-6.5 weeks (CRL) |
6.6-7.5 weeks (CRL) |
7.6-8.5 weeks (CRL) |
8.6-9.5 weeks (CRL) |
9.6-10.5 weeks (CRL) |
|
|
N |
Valid |
12 |
12 |
11 |
10 |
7 |
|
Missing |
0 |
0 |
1 |
2 |
5 |
|
|
Mean |
5.983 |
6.950 |
7.700 |
8.380 |
9.614 |
|
|
Median |
6.100 |
7.050 |
7.800 |
8.300 |
9.500 |
|
|
Std. Deviation |
7107 |
6142 |
6000 |
6697 |
8255 |
|
|
Minimum |
5.0 |
6.1 |
6.4 |
7.3 |
8.3 |
|
|
Maximum |
7.6 |
8.4 |
8.6 |
9.3 |
10.5 |
|
No statistical correlation between the EV and pregnancy outcome was found at this gestational age (p=0.612-Table 2).
Table 2.
Correlations between EV and pregnancy outcome
|
|
Pregnancy outcome |
Total |
|||
|
TI/TII abortion |
Birth |
||||
|
11.6-12.5 weeks EV 13-29_N |
<5p |
Count |
1 |
13 |
14 |
|
% within 11.6-12.5 weeks_EV_mm3 13-29_B |
7.1% |
92.9% |
100.0% |
||
|
>95p |
Count |
0 |
1 |
1 |
|
|
% within 11.6-12.5 weeks_EV_mm3 13-29 B |
0.0% |
100.0% |
100.0% |
||
|
N |
Count |
1 |
55 |
56 |
|
|
% within 11.6-12.5 weeks EV_mm3 13-29_B |
1.8% |
98.2% |
100.0% |
||
|
Total |
Count |
2 |
69 |
71 |
|
|
% within 11.6-12.5 weeks_EV_mm3 13-29 B |
2.8% |
97.2% |
100.0% |
||
At 12 weeks of gestation, the CRL has a low correlation (r=0.279, p=0.020) with the fetal birth weight (Figure 1).
Figure 1.
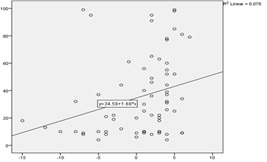
CRL and fetal birth weight correlation
There are no statistical differences regarding outcome (p=0.085) (Table 3).
Table 3.
CRL and outcome correlation
|
|
Pregnancy outcome |
Total |
|||
|
TI/TII abortion |
Birth |
||||
|
11.6-12.5 (CRL) |
-6d and-2d |
Count |
2 |
19 |
21 |
|
% within 11.6-12.5 |
9.5% |
90.5% |
100.0% |
||
|
-1d and+6d |
Count |
0 |
50 |
50 |
|
|
% within 11.6-12.5 |
0.0% |
100.0% |
100.0% |
||
|
Total |
Count |
2 |
69 |
71 |
|
|
% within 11.6-12.5 |
2.8% |
97.2% |
100.0% |
||
There are no statistical differences between the fetal CRL and fetal growth restriction at term (p=0.480-Table 4) or an unfavorable pregnancy outcome (p=0.278-Table 5).
Table 4.
Fetal CRL and IUGR correlations
|
|
IUGR |
Total |
|||
|
NO |
YES |
||||
|
11.6_12.5 (CRL) |
-6d and-2d |
Count |
15 |
4 |
19 |
|
% within 11.6-12.5 |
78.9% |
21.1% |
100.0% |
||
|
-1d and+6d |
Count |
43 |
7 |
50 |
|
|
% within 11.6-12.5 |
86.0% |
14.0% |
100.0% |
||
|
Total |
Count |
58 |
11 |
69 |
|
|
% within 11.6-12.5 |
84.1% |
15.9% |
100.0% |
||
Table 5.
Fetal CRL and unfavorable pregnancy outcome correlations
|
|
Unfavorable pregnancy outcome |
Total |
|||
|
NO |
YES |
||||
|
11.6_12.5 |
-6d and-2d |
Count |
6 |
13 |
19 |
|
% within 11.6_12.5 |
31.6% |
68.4% |
100.0% |
||
|
-1d and+6d |
Count |
23 |
27 |
50 |
|
|
% within tip 11.6_12.5 |
46.0% |
54.0% |
100.0% |
||
|
Total |
Count |
29 |
40 |
69 |
|
|
% within 11.6_12.5 |
42.0% |
58.0% |
100.0% |
||
There are no statistical differences between the GSV and pregnancy outcome (p=0.612-Table 6) or an unfavorable pregnancy outcome (p=0.421-Table 7).
Table 6.
GSV and pregnancy outcome correlations
|
|
Pregnancy outcome |
Total |
|||
|
TI/TII abortion |
Birth |
||||
|
11.6-12.5_ weeks_GSV_mm3 75.2-144.1_N |
>95p |
Count |
0 |
1 |
1 |
|
% within 11.6-12.5_weeks 75.2 144.1_N |
0.0% |
100.0% |
100.0% |
||
|
<5p |
Count |
1 |
1 |
2 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
50.0% |
50.0% |
100.0% |
||
|
>95p |
Count |
0 |
20 |
20 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
0.0% |
100.0% |
100.0% |
||
|
N |
Count |
1 |
47 |
48 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
2.1% |
97.9% |
100.0% |
||
|
Total |
Count |
2 |
69 |
71 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
2.8% |
97.2% |
100.0% |
||
Table 7.
GSV and unfavorable pregnancy outcome correlations
|
|
Unfavorable pregnancy outcome |
Total |
|||
|
NO |
YES |
||||
|
11.6-12.5_weeks_GSV 75.2-144.1_N |
>95p |
Count |
0 |
1 |
1 |
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
0.0% |
100.0% |
100.0% |
||
|
<5p |
Count |
0 |
2 |
2 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
0.0% |
100.0% |
100.0% |
||
|
>95p |
Count |
8 |
12 |
20 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
40.0% |
60.0% |
100.0% |
||
|
N |
Count |
16 |
32 |
48 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
33.3% |
66.7% |
100.0% |
||
|
Total |
Count |
24 |
47 |
71 |
|
|
% within 11.6-12.5_weeks_GSV 75.2-144.1_N |
33.8% |
66.2% |
100.0% |
||
There are no statistical differences between the YSV and pregnancy outcome (p=0.994-Table 8) or an unfavorable pregnancy outcome (p=0.546-Table 9).
Table 8.
YSV and pregnancy outcome correlations
|
|
Pregnancy outcome |
Total |
|||
|
TI/TII abortion |
Birth |
||||
|
11.6-12.5_weeks_YSV_mm3 0.05-0.250_N |
>95p |
Count |
0 |
2 |
2 |
|
% within 11.6-12.5_weeks_YSV 0.05-0.250_N |
0.0% |
100.0% |
100.0% |
||
|
N |
Count |
2 |
67 |
69 |
|
|
% within 11.6-12.5_weeks_YSV 0.05-0.250_N |
2.9% |
97.1% |
100.0% |
||
|
Total |
Count |
2 |
69 |
71 |
|
|
% within 11.6-12.5_weeks_YSV 0.05-0.250_N |
2.8% |
97.2% |
100.0% |
||
Table 9.
YSV and unfavorable pregnancy outcome correlations
|
|
Unfavorable pregnancy outcome |
Total |
|||
|
NO |
YES |
||||
|
11.6-12.5_weeks_YSV 0.05-0.250_N |
>95p |
Count |
0 |
2 |
2 |
|
% within 11.6-12.5_weeks_YSV 0.05-0.250_N |
0.0% |
100.0% |
100.0% |
||
|
N |
Count |
29 |
38 |
67 |
|
|
% within 11.6-12.5_weeks_YSV 0.05-0.250_N |
43.3% |
56.7% |
100.0% |
||
|
Total |
Count |
29 |
40 |
69 |
|
|
% within 11.6-12.5_weeks_YSV 0.05-0.250_N |
42.0% |
58.0% |
100.0% |
||
Discussion
Studies predicting pregnancy outcome approached to much earlier stages of the pregnancy.
Various ultrasound parameters, such as GSV and YSV [26,27,28] and the relationship between them and the average size of the CRL are used in early pregnancy [29,30].
There are several studies that correlated the first trimester ultrasound volumetric markers with outcome [31,32].
Literature showed that the EV has a good correlation with the fetal birth weight than the GSV or CRL [17].
Our study results showed no statistical correlation (p=0.612) between the EV and pregnancy outcome in the first trimester. Also, at 12 weeks of gestation, the CRL had a low correlation (r=0.279, p=0.020) with the fetal birth weight. There were also no statistical differences (p=0.480) between the fetal CRL and fetal growth restriction at term or fetal outcome.
In the first trimester, the GS consists of amniotic and celomic cavity and it reflects the embryonic development environment. GSV measurements can help to distinguish between normal and abnormal pregnancies. Steiner et al. described a strong correlation between the gestational age and GSV during the first trimester [33].
Studies made at different gestational ages (5-12 weeks of gestation) [34] concluded that the GSV was smaller in the aborted cases [35].
Our study results show that there is no statistical correlation (p=0.421/0.612) between GSV in the first trimester and unfavorable/ pregnancy outcome.
Bagratee et al. conducted a study that showed that first trimester YSV reference intervals increased for up to 10 weeks of gestation, then up to 11 weeks it plateaued and decreased afterwards. They suggested that it was caused by decreased vascularization [36].
According to literature, YS normally increases during the first trimester. A small YS is correlated with an abnormal outcome [37].
In the present study, YS increased with gestational week and was found to be positively associated with the CRL. Our results show that there is no statistical correlation between YSV in the first trimester and unfavorable/pregnancy outcome (p=0.546-0.994).
Conclusions
First-trimester volumetric ultrasound represents an important tool for pregnancy outcome prediction.
3D ultrasound is a useful and reproductible method. In the first trimester, at 12 weeks of gestation, only CRL showed a low correlation (r=0.279, p=0.020) with the fetal birth weight.
Application of this method is feasible in prediction of IUGR, birth weight and other pregnancy complications.
Conflict of interests
None to declare.
References
- 1.Papaioannou G, Syngelaki A, Maiz N, Ross JA, Nicolaides KH. Ultrasonographic prediction of early miscarriage. Hum Reprod. 2011;26(7):1685–1692. doi: 10.1093/humrep/der130. [DOI] [PubMed] [Google Scholar]
- 2.Oates J, Casikar I, Campain A, Müller S, Yang J, Reid S, Condous G. A prediction model for viability at the end of the first trimester after a single early pregnancy evaluation. Aust N Z J Obstet Gynaecol. 2013;53(1):51–57. doi: 10.1111/ajo.12046. [DOI] [PubMed] [Google Scholar]
- 3.Malhotra N, Malhotra J, Mathur V, Ahuja B. Application of three dimensional ultrasound in reproductive health gynecology and infertility. Ultrasound in Obstetrics and Gynecology. 2000;5(1):340–348. [Google Scholar]
- 4.Lang FC, Frates MC. Ultrasound evaluation during the first trimester of pregnancy. Ultrasonography in Obstetrics and Gynecology. 2000;45(3):105–145. [Google Scholar]
- 5.Dulay AT, Copel JA. First-trimester ultrasound: Current uses and applications. Semin Ultrasound CT MRI. 2008;29(1):121–131. doi: 10.1053/j.sult.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Bagratee JS, Regan L, Khullar V, Connolly C, Moodley J. Reference interval of gestational sac, yolk sac and embryo volumes using three dimensional ultrasound. Ultrasound Obstet Gynecol. 2009;34(2):503–509. doi: 10.1002/uog.7348. [DOI] [PubMed] [Google Scholar]
- 7.Odeh M, Hirsh Y, Degani S, Grinin V, Ofir E, Bornstein J. Three dimensional sonographic volumetry of the gestational sac and the amniotic sac in the first trimester. Journal Ultrasound Med. 2008;27(3):373–378. doi: 10.7863/jum.2008.27.3.373. [DOI] [PubMed] [Google Scholar]
- 8.Aviram R, Shpan DK, Markovitch O, Fishman A, Tepper R. Three dimensional first trimester fetal volumetry: comparison with crown rump length. Early Hum Dev. 2004;80(2):1–5. doi: 10.1016/j.earlhumdev.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Rolo LC, Nardozza LM, Araujo Junior E, Nowak PM, Moron AF. Yolk sac volume assessed by three dimensional ultrasonography using the VOCAL method. Gynecol. 2008;87(5):499–502. doi: 10.1080/00016340802011595. [DOI] [PubMed] [Google Scholar]
- 10.Nardozza LM, Nowak PM, Araujo Júnior E, Guimarães Filho HA, Rolo LC, Torloni MR. Evaluation of placental volume at 7 to 10+6 weeks of pregnancy by 3D sonography. Placenta. 2009;30(2):585–589. doi: 10.1016/j.placenta.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Rolo LC, Nardozza LM, Araujo Junior E, Nowak PM, Moron AF. Gestational sac volume by 3D-sonography at 7 to 10 weeks of pregnancy using the VOCAL method. Arch Gynecol Obstet. 2009;79(3):821–827. doi: 10.1007/s00404-008-0828-8. [DOI] [PubMed] [Google Scholar]
- 12.Acharya G, Morgan H. First trimester, three dimensional trans-vaginal ultrasound volumetry in normal pregnancies and spontaneous miscarriage. Ultrasound Obstet Gynecol. 2002;19(4):575–579. doi: 10.1046/j.1469-0705.2002.00712.x. [DOI] [PubMed] [Google Scholar]
- 13.Acharya G, Morgan H. Does gestational sac volume predict the outcome of missed miscarriage managed expectantly? . Journal Clin Ultrasound. 2002;30(1):526–531. doi: 10.1002/jcu.10107. [DOI] [PubMed] [Google Scholar]
- 14.Hafner E, Metzenbauer M, Höfinger D, Stonek F, Schuchter K, Waldhör T. Comparison between three-dimensional placental volume at 12 weeks and uterine artery impedance/notching at 22 weeks in screening for pregnancy-induced hypertension, pre-eclampsia and fetal growth restriction in a low-risk population . Ultrasound Obstet Gynecol. 2006;27(2):652–657. doi: 10.1002/uog.2641. [DOI] [PubMed] [Google Scholar]
- 15.Hafner E, Metzenbauer M, Höfinger D, Munkel M, Gassner R, Schuchter K. Placental growth from the first to the second trimester of pregnancy in SGA-foetuses and pre-eclamptic pregnancies compared to normal fetuses. Placenta. 2003;24(2):336–342. doi: 10.1053/plac.2002.0918. [DOI] [PubMed] [Google Scholar]
- 16.Plasencia W, Akolekar R, Dagklis T, Veduta A, Nicolaides KH. Placental volume at 11 to 13 week’s gestation in the prediction of birth weight percentile. Fetal Diagn Ther. 2011;30(3):233–238. doi: 10.1159/000324318. [DOI] [PubMed] [Google Scholar]
- 17.Antsaklis A, Anastasakis E, Komita O, Theodora M, Hiridis P, Daskalakis G. First trimester 3D volumetry. association of the gestational volumes with the birth weight. Journal Matern Fetal Neonatal Med. 2011;24(1):1055–1058. doi: 10.3109/14767058.2010.545915. [DOI] [PubMed] [Google Scholar]
- 18.Falcon O, Cavoretto P, Peralta CF, Csapo B, Nicolaides KH. Fetal head to trunk volume ratio in chromosomally abnormal fetuses at 11+0 to 13+6 weeks of gestation. Ultrasound Obset Gynecol. 2005;26(5):755–760. doi: 10.1002/uog.1991. [DOI] [PubMed] [Google Scholar]
- 19.Falcon O, Wegrzyn P, Faro C, Peralta CF, Nicolaides KH. Gestational sac volume measured by three dimensional ultrasound at 11 to 13+6 weeks of gestation: relation to chromosomal defects. Ultrasound Obstet Gynecol. 2005;25(2):546–550. doi: 10.1002/uog.1898. [DOI] [PubMed] [Google Scholar]
- 20.Riccabona M, Nelson TR, Pretorius DH. Three dimensional ultrasound: accuracy of distance and volume measurements. Ultrasound Obstet Gynecol. 1996;7(1):429–434. doi: 10.1046/j.1469-0705.1996.07060429.x. [DOI] [PubMed] [Google Scholar]
- 21.Raine-Fenning NJ, Clewes JS, Kendall NR, Bunkheila A, Campbell BK, Johnson IR. The interobserver reliability and validity of volume calculation from three-dimensional ultrasound datasets in the in vitro setting. Ultrasound Obstet Gynecol. 2003;21(1):283–291. doi: 10.1002/uog.61. [DOI] [PubMed] [Google Scholar]
- 22.Sladkevicius P, Saltvedt S, Almstr AM, Kublickas M, Grunewald C, Valentin L. Ultrasound dating at 12 to 14 weeks of gestation. A prospective cross-validation of established dating formulae in invitro fertilized pregnancies. Ultrasound Obstet Gynecol. 2005;26(4):504–511. doi: 10.1002/uog.1993. [DOI] [PubMed] [Google Scholar]
- 23.Aviram R, Shpan DK, Markovitch O, Fishman A, Tepper R. Three dimensional first trimester fetal volumetry:comparison with crown rump length. Early Hum Dev. 2004;80(2):1–5. doi: 10.1016/j.earlhumdev.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Sur SD, Jayaprakasan K, Jones NW, Clewes J, Winter B, Cash N. A novel technique for the semi-automated measurement of embryo volume: an intra observer reliability study. Ultrasound Med Biol. 2010;36(5):719–725. doi: 10.1016/j.ultrasmedbio.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 25.Hafner E, Schuchter K, van Leeuwen M, Metzenbauer M, Dillinger-Paller B, Philipp K. Three-dimensional sonographic volumetry of the placenta and the fetus between weeks 15 and 17 of gestation . Ultrasound Obstet Gynecol. 2001;18(6):116–120. doi: 10.1046/j.1469-0705.2001.00489.x. [DOI] [PubMed] [Google Scholar]
- 26.Verwoerd-Dikkeboom CM, Koning AH, Hop WC, Rousian M, Van Der Spek PJ, Exalto N. Reliability of three dimen-sional sonographic measurements in early pregnancy using virtual reality . Ultrasound Obstet Gynecol. 2008;32(1):910–916. doi: 10.1002/uog.5390. [DOI] [PubMed] [Google Scholar]
- 27.Reece EA, Scioscia AL, Pinter E, Hobbins JC, Green J, Ma-honey MJ. Prognostic significance of the human yolk sac assessed by ultrasonography . Am J Obstet Gynecol. 1988;159(2):1191–1194. doi: 10.1016/0002-9378(88)90445-0. [DOI] [PubMed] [Google Scholar]
- 28.Lindsay DJ, Lovett IS, Lyons EA, Levi CS, Zheng XH, Holt SC, Dashefsky SM. Yolk sac diameter and shape at endovaginal US: predictors of pregnancy outcome in the first trimester. Radiology. 1992;183(2):115–118. doi: 10.1148/radiology.183.1.1549656. [DOI] [PubMed] [Google Scholar]
- 29.Dickey RP, Olar TT, Taylor SN, Curole DN, Matulich EM. Relationship of small gestational sac-crown-rump length differences to abortion and abortus karyotypes . Obstet Gynecol. 1992;79(3):554–556. [PubMed] [Google Scholar]
- 30.Nazari A, Check JM, Epstein RM, Dietterich C, Farazner S. Relationship of small for dates sac size to crown-rump length and spontaneous abortion in patients with a known date of ovulation . Obstet Gynecol. 1991;78(3):369–373. [PubMed] [Google Scholar]
- 31.Figueras F, Torrents M, Muñoz A, Comas C, Antolin E, Echevarria M. Three-dimensional yolk and gestational sac volume. A prospective study of prognostic value . J Reprod Med. 2003;48(1):252–255. [PubMed] [Google Scholar]
- 32.Acharya G, Morgan H. First-trimester, three-dimensional trans-vaginal ultrasound volumetry in normal pregnancies and sponta-neous miscarriages . Ultrasound Obstet Gynecol. 2002;19(2):575–576. doi: 10.1046/j.1469-0705.2002.00712.x. [DOI] [PubMed] [Google Scholar]
- 33.Steiner H, Gregg AR, Bogner G, Graf AH, Weiner CP, Staudach A. First trimester three-dimensional ultrasound volumetry of the gestational sac . Arch Gynecol Obstet. 1994;25(5):165–166. doi: 10.1007/BF02335080. [DOI] [PubMed] [Google Scholar]
- 34.Cunningham FG, Gant NF, Leveno KJ, Gilstrap LC, Health JC, Wenstrom KD. In: Williams Obstetrics. Cunningham FG, Bloom SL, Dashe JS, Hoffman BL, Casey BM, Spong CY, editors. New York: McGraw-Hill; 2001. Fetal Growth Disorders; pp. 847–849. [Google Scholar]
- 35.Müller T, Sütterlin M, Pöhls U, Dietl J. Transvaginal volumetry of first trimester gestational sac: a comparison of conventional with three dimensional ultrasound . J Perinat Med. 2000;28(3):214–216. doi: 10.1515/JPM.2000.029. [DOI] [PubMed] [Google Scholar]
- 36.Bagratee JS, Regan L, Khullar V, Connolly C, Moodley J. Reference intervals of gestational sac, yolk sac and embryo volumes using three-dimensional ultrasound . Ultrasound Obstet Gynecol. 2009;34(1):503–506. doi: 10.1002/uog.7348. [DOI] [PubMed] [Google Scholar]
- 37.Fotios K, Nicolaos M, Prapas Georgios A. Yolk sac size and embryonic heart rate as prognostic factors of first trimester pregnancy outcome. European J Obstetr Gynecol Reproduct Biol. 2008;138(1):10–13. doi: 10.1016/j.ejogrb.2007.06.023. [DOI] [PubMed] [Google Scholar]


