Abstract
In 2010, forgoing curative therapies was removed as a hospice eligibility criteria for children through section 2302 of the Patient Protection and Affordable Care Act called Concurrent Care for Children. Given that concurrent care is a federally-mandated option for children and their families, no review of the science has been conducted. The purpose of this study was to systematically collect the evidence on concurrent hospice care, critically appraise the evidence, and identify areas for future nursing research. Of the 186 articles identified for review, 14 met inclusion and exclusion criteria. Studies in this review described concurrent hospice care from a variety of perspectives: policy, legal, and ethics. However, only one article evaluated impact of concurrent hospice care on outcomes, while several studies explained clinical and state-level implementation. There is a need for further studies that move beyond conceptualization and generate baseline and outcomes data. Understanding the effectiveness of concurrent hospice care might provide important information for future nursing research. The approaches used to disseminate and implement concurrent hospice care at state-, provider-, and family-levels should be explored.
Keywords: Pediatric, hospice care, concurrent care, scoping review, end-of-life
Over 30,000 children die in the United States (U.S.) each year; a large number of these deaths occur in the pediatric intensive care unit without access to hospice services.1 It is common for these children to have multiple chronic, complex, life-limiting conditions such as chromosomal anomalies, congenital malformations, complications related to prematurity, neurological conditions, and/or cancer.2,3 In addition, it is not unusual for a child with serious illness at end of life to have marked functional limitations and require technology for activities of daily living such as oxygen, gastronomy tubes, and assistive devices.4 Children at end of life also have significant symptom management needs and complicated care plans that extend across numerous clinical specialties.5 Because of the complex care requirements, there is often a substantial caregiving burden, which can result in family strain.6,7 Standard hospice services offer a family-centered model of care that can assist with symptom management, psychosocial care, respite, and bereavement support for children and families.
The Institute of Medicine publication, Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life, reported on the need to strengthen organization and delivery of services for children at the end of life, including the need for comprehensive hospice care models.8 In the years that followed, there has not been a significant increase in hospice use among children at the end of life with estimates of only 10–15 percent of pediatric decedents enrolling in hospice.9,10 Historically, one of the consistent barriers to utilization for children and families was the regulatory provision requiring the need to forgo curative therapies in order to enroll in hospice services.11 For many children with serious illness, forgoing curative therapies meant altering long-standing regimens necessary for improved quality of life and symptom management at end of life.2
In 2010, forgoing curative therapies was removed as a hospice eligibility criteria for children through the Patient Protection and Affordable Care Act of 2010 (ACA), Section 2302 called Concurrent Care for Children. As a care delivery model, concurrent hospice care allows children enrolled in Medicaid/Children’s Health Insurance Program (CHIP) in all U.S. states to receive hospice services, while maintaining access to curative therapies.12 Implementation of concurrent care into state Medicaid plans occurred from 2010 to 2017.2 Children must still have a life expectancy of 6 months or less to qualify for concurrent hospice care. In addition, children and families may still opt to enroll in standard hospice care without receiving curative care. Pediatric concurrent hospice care was included in the ACA after rigorous pilot work conducted in the 1990s in such states as California, Washington, and Florida.13 Furthermore, adult concurrent hospice care was introduced into the Veteran’s Administration (VA) health care system in the early 2000s,14,15 and in 2015 concurrent hospice care demonstration projects were initiated for Medicare adult beneficiaries.16,17 Thus, concurrent hospice care has been implemented in pediatric and adult patient populations.
Although it has been a decade since enactment of concurrent hospice care, few studies have examined the use of this care model in practice or research. The pediatric and adult literature on concurrent care is rarely cited in end-of-life literature and it is still common for pediatricians, pediatric specialists, and hospice clinicians, along with families, to be unaware of concurrent hospice care. Given that concurrent care is a federally-mandated option for children and their families, no review of the science has been conducted. Therefore, the purpose of this study was to systematically collect the evidence on concurrent hospice care, critically appraise the evidence, and identify areas for future nursing research.
Methods
This study represents a scoping review of concurrent hospice care articles.18 Scoping reviews are best used when a body of literature has not yet been comprehensively reviewed and is not amenable to a more precise systematic review.18 General guidelines were followed to determine sources from the literature to be used for this review.19 The literature was identified by systematic searches on the Medline, CINAHL, and Web of Science databases. Pertinent search terms for concurrent hospice care (e.g., hospice, concurrent, curative, palliative, end-of-life) were combined to search titles, abstracts, and subject headings from 2000 to 2019. Additional sources of interest were identified by reviewing the references from the above search to include other references missed in the original search.
All articles relevant to concurrent care were eligible for inclusion (Figure 1). Inclusion criteria for the review included articles pertaining to concurrent care, peer-reviewed, English language, and U.S. studies. Articles were excluded if the publication date was prior to the year 2000 because adult or pediatric concurrent care was not implemented before this date, or if the article reported on conference proceedings, other medical procedures, or methodological studies. Articles that focused on concurrent palliative care were also excluded. Although pediatric palliative care is specialized health care for children living with a serious illness that focuses on providing relief from the symptoms and stress of the illness, the delivery, payment, and timeframe of delivery are different from hospice. However, because palliative care and hospice care are often used interchangeably in the literature, we conducted abstract and full-text reviews of the palliative care studies to ensure that the focus was limited to concurrent hospice care. The appraisal of articles was conducted under three main, a priori themes: description, evaluation, and dissemination/implementation of the concurrent hospice care.
Figure 1.
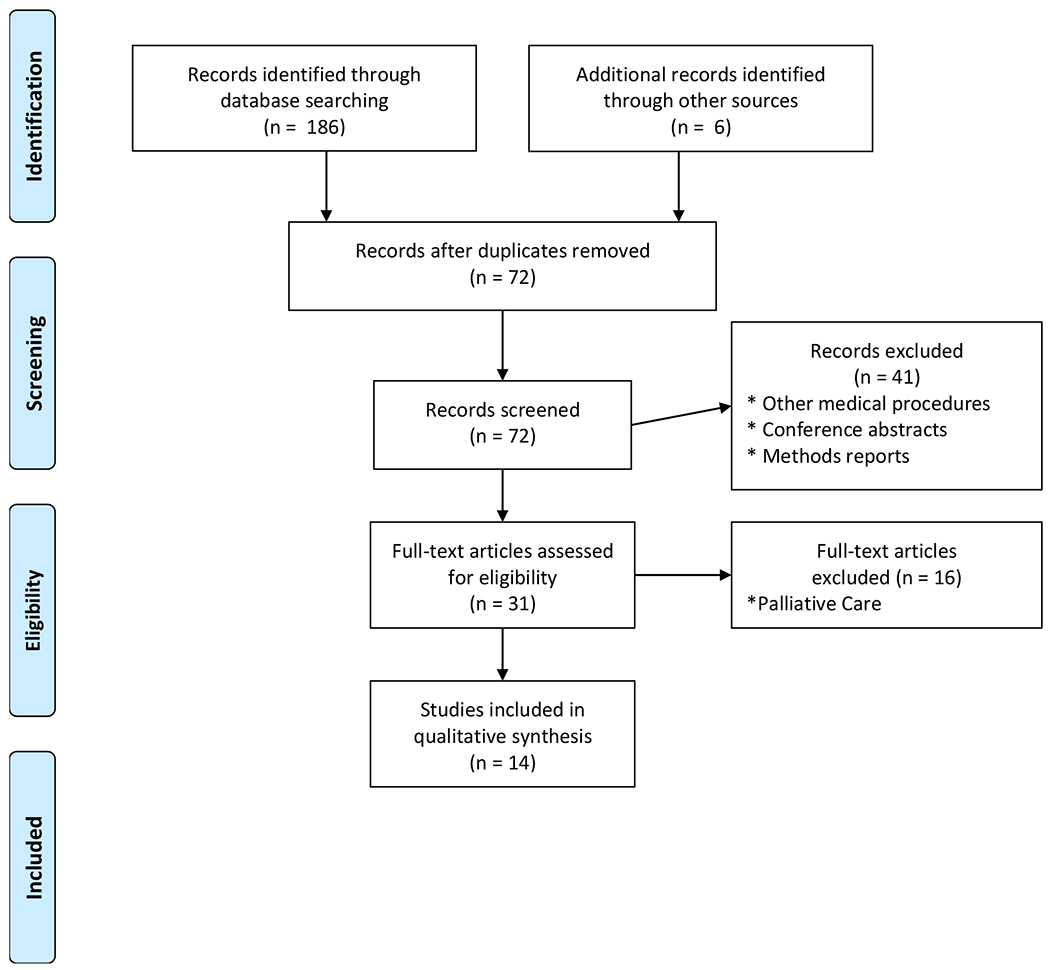
Study Flow Diagram
Results
Fourteen articles of pediatric and adult concurrent hospice care were included in our review.2, 11–17,20–25 These are summarized in Table 1. All studies were published between 2011 and 2019. Narrative study designs dominated with seven studies,2,11–13,16,20,24 followed by three case studies,17,21,23 three quantitative studies,14,15,25 and one qualitative study22. Nine of the studies restricted their perspective to pediatrics and Medicaid.2,11–13,20,21,23–25 Five studies were adult-focused.14–17,22 which included a Veterans Administration14,15,22 or Medicare16,17 perspective. There was wide variation in the level of analysis: patient,11,14,15,17,21 provider,21–24, state,2,13,25 and system.12,16,20
Table 1.
Summary of concurrent hospice care articles
| Study | Study Design | Level of Analysis | Insurance Type | Key Findings |
|---|---|---|---|---|
| Pediatric | ||||
| Children’s Project on Palliative/Hospice Services23 (2013) | Case Study | Provider | Medicaid | Implementation: Variation in implementation of concurrent care at the provider level. |
| Keim-Malpass et al.13 (2013) | Narrative | State | Medicaid | Description: Pediatric concurrent care policy founded on state-level demonstration projects |
| Keim-Malpass & Lindley2 (2017) | Narrative | State | Medicaid | Description: Policy repeal of concurrent care would reduce access to high-quality end of life care. |
| Lindley12 (2011) | Narrative | System | Medicaid | Description: Pediatric concurrent care policy will impact access and quality of care, along with political feasibility of implementation. |
| Lindley et al.25 (2013) | Quantitative | State | Medicaid | Implementation: State implementation of pediatric concurrent care influenced by state-level financial constraints. |
| Lotstein & Lindley24 (2019) | Narrative | Provider | Medicaid | Implementation: Challenges exist when concurrent care coexists with state-level policies. |
| Miller et al.21 (2012) | Case Study | Provider/Patient | Medicaid | Implementation: There are challenges of implementing pediatric concurrent care among treatment providers. |
| Mooney-Doyle et al.11 (2018) | Narrative | Patient | Medicaid | Description: Ethical provision of pediatric concurrent care is socially just ad promotes well-being of vulnerable children and families. |
| Walsh20 (2013) | Narrative | System | Medicaid | Description: Pediatric concurrent care represents a shifting legal paradigm. |
| Adult | ||||
| Hargadon et al.17 (2017) | Case Study | Patient | Medicare | Implementation: Concurrent care policy aligns with patient goals of care. |
| Harrison & Connor16 (2016) | Narrative | System | Medicare | Description: Policy of Medicare demonstration project has potential to reduce access and quality barriers. |
| Haverhals et al.22 (2018) | Qualitative | Provider | Veterans Administration | Implementation: Providers value concurrent care as an option to offer patients and families. |
| Mor et al.15 (2016) | Quantitative | Patient | Veterans Administration | Implementation: Use of concurrent care increases over time. |
| Mor et al.14 (2019) | Quantitative | Patient | Veterans Administration | Evaluation: Concurrent care was associated with a reduction in aggressive medical treatments at end of life. |
Description of concurrent hospice care
Pediatric.
Five out of 14 articles described pediatric concurrent hospice care, 2,11–13,20 and more than half were written within 3 years of ACA, Section 2302 enactment.12,13,20 Three of pediatric articles described the policy environment of concurrent care.2,12,13 One report described pediatric concurrent care from a historical policy perspective.13 It discussed how demonstration projects and preliminary legislation in California, Colorado, Illinois, Florida, Massachusetts, and Washington set the stage for concurrent hospice care to be included in the ACA. Another article provided the first policy analysis of pediatric concurrent upon enactment of ACA, Section 2302.12 The author suggested that pediatric concurrent care might generate new facilitators (e.g., patient-centered care) and barriers (e.g., care coordination) to quality, accessible end-of-life care for children and families. Concerns about the eligibility requirement of a life expectancy of 6 months or less were raised in this report. The third article described the political environment of repealing the ACA during the current administration and its impact on pediatric concurrent hospice care.2 The authors argued that replacing the ACA with state Medicaid block grants might create an environment where services such as concurrent care are eliminated from Medicaid programs because they might be perceived as insignificant and/or expensive.
One article described the ethical environment of pediatric concurrent hospice care.11 Using a social justice lens, these authors argued that concurrent care is socially just. Concurrent hospice care has the potential to promote well-being of vulnerable children and families, while limiting the inequity experienced by children at end of life in accessing high-quality hospice care.
The legal environment of concurrent care for children was describe in a single article.20 The author (Walsh) argued that allowing curative therapies during hospice care was a legal paradigm shift, but incomplete because the hospice eligibility requirement of a life expectancy of six month or less was still present in ACA, Section 2302. Pediatric concurrent care was expected to increase hospice access and improve outcomes for children; however, the life expectancy omission was a unique challenge for children who might live beyond six months with curative therapies.
Adult.
A single adult article described concurrent hospice care.16 This policy article presented a historical view of the adult Medicare hospice benefit and explained the 2016 Medicare concurrent care demonstration projects. The authors discussed the lessons learned from pediatric concurrent care such as complicated care coordination needs of patients between curative and hospice services. As a consequence, the Medicare demonstration projects included additional funding for adult hospices to perform care coordination.
Overall, the descriptive articles suggest that concurrent care has a rich and unique history, but recent information describing pediatric concurrent care was limited. Among the articles in the scoping review, there were no published reports describing concurrent hospice care patients, families, hospice providers, or treatment providers. No articles described curative therapies or hospice care during concurrent care.
Evaluation of concurrent hospice care
Adult.
Only one study evaluated the outcomes of concurrent hospice care; 14 in this case, the authors (Mor and colleagues) reported the results of an observational study among cancer patients. The data sources included 2006 to 2012 VA patient treatment files, VA tumor registry, the National Patient Care Database, VA Fee Basis files, and Medicare claims. Concurrent care was defined as receiving radiation therapy or chemotherapy after initiation of hospice care. The article reported on five outcomes: 2 or more hospital admissions, tube feeding, mechanical ventilation, intensive care unit admission, and total costs. The authors found that increasing the availability of concurrent care was related to less aggressive medical treatments and significantly lower costs at end of life.
Information on concurrent hospice care outcomes was sparse. We did not identify any pediatric articles that evaluated outcomes of concurrent care. No other patient, provider, or systems outcomes were evaluated.
Dissemination and implementation of concurrent hospice care
Pediatric.
Four pediatric reports highlighted implementation of concurrent hospice care.21,23–25 One report discussed clinical implication of concurrent care, using a case study approach. 21 The article reported five types of challenges a clinical team experiences during implementation of concurrent care: 1.) lack of knowledge regarding end-of-life care among private duty nurses; 2.) different perspectives on end-of-life care between palliative care practitioners, hospice clinicians, and private duty nurses; 3.) lack of experience with complex care coordination among hospice providers; 4.) durable medical equipment costs cost increases for hospices; and 5.) insurance complexities of coordinating private and Medicaid insurance for children. Pediatric concurrent hospice care required a steep learning curve for clinicians, but was valued as improving access to end-of-life care.
State-level implementation was presented in three pediatric articles.23–25 One report provided examples from California, Florida, Illinois, Kansas, Maryland, and New Jersey.23 Narrative accounts of their states’ experiences implementing pediatric concurrent hospice care within the Medicaid system were offered. The challenges of coordinating other pediatric palliative care policies with concurrent care were discussed from the perspective of California and Florida; while information on training, education, and advocacy were discussed among the other states. The article also reported that pediatric concurrent hospice care had a steep learning curve for state Medicaid offices, which often delayed implementation. A second article examined the specific case of California implementation.24 The authors argued the unique challenges of implementing pediatric concurrent hospice care in the presence of other state end-of-life policies for children. Several challenges to children and families, referring providers, and hospice providers were noted: 1.) lack of clear understanding about services provided under both plans among families; 2.) lack of awareness by referring providers about concurrent care and state plans, and 3.) lack of knowledge about pediatric policies and practices among adult-oriented hospice providers. The importance of education and advocacy to improve understanding among key stakeholders was emphasized. A third article reported on the macro-economic, political, and legal predictors of state-level implementation of pediatric concurrent hospice care.25 Using publicly-available data from 2010 to 2012, the authors found that state implementation was influenced by Medicaid cost containment efforts and budgetary crisis.
Adult.
Three adult articles presented information on implementation of concurrent hospice care.15,17,22 All the articles reported on clinical implementation. One report used a case study approach,17 which described an elderly patient with serious illness who was admitted to hospice care. After enrollment, the patient decided to pursue further treatment. The authors argued the need for concurrent hospice care, and suggested assessing the evolving goals of care need of concurrent care patients as they transition between curative therapies and hospice care. Another report used a qualitative approach to investigate clinical implementation.22 From August 2015 to April 2016, the authors interviewed 76 VA clinicians and contracted community hospices staff about implementing concurrent hospice care. Three main themes were reported: 1.) both clinician and hospice staff viewed concurrent care as a viable care option; 2.) care coordination was facilitated with a dedicated liaison; and 3.) insurance complexities of coordinating Medicare and VA insurance benefits. A third article used quantitative techniques to investigate clinical implementation.15 This study was a retrospective cohort design with veteran decedents, who received hospice and cancer treatments during 2006 through 2012. The article reported that receipt of concurrent hospice care increased over time from 16.2% in 2006 to 24.5% in 2012. Although concurrent care offered an expansion of hospice services to cancer patients, considerable variation between VA medical centers in the use of concurrent care was found.
We found in this review emerging information on state-level information that included specific challenges and benefits, but documentation on clinical implementation of concurrent hospice care was lacking. In addition, no information on dissemination of concurrent hospice care to families, providers, or clinicians was identified.
Discussion
To our knowledge, this is the first comprehensive review of concurrent hospice care. The descriptive articles in this review assist us in understanding the rich history of pediatric concurrent care, which is embedded in a political, ethical, and legal environment. In the descriptive studies, the concept of concurrent care is defined and refined. For example, Lindley and Walsh provide a legal or regulatory definition of concurrent hospice care, while Mooney-Dole et al., offer an ethical definition.11,12,20 In addition, the early descriptive works identified major concerns with pediatric concurrent hospice care such as care coordination and the eligibility criteria of a life expectancy of 6 months or less. Both Lindley and Walsh argued that by not eliminating the hospice eligibility criteria (life expectancy of 6 month) that issues with extended length of stay under concurrent hospice care would emerge.12,20 Thus, the descriptive literature offered critical definitions and foreshadowed challenges in implementation.
The findings from our scoping review revealed that concurrent care had a positive impact on patient outcomes. The Mor et al., article assessed end-of-life outcomes such as mechanical ventilation, ICU admission, and tube feeding that are commonly referred to as aggressive or high-intensity treatments at end of life.14,26 The study used a quasi-experimental (difference-in-difference) design, which was appropriate to study relationships where randomized controlled trials (RCTs) are infeasible or unethical.27 As an alternative, non-randomized, quasi-experimental designs can be developed using statistical methods, that approximate the effect of randomization of the intervention and comparison groups with observational data, which would provide a higher level of evidence.28 However, there is still a lack of knowledge about how concurrent care might influence patient symptoms at end of life, especially given that the treating provider with pediatric expertise and the hospice with its expertise in end-of-life symptom management are involved in the care of the child. Additionally, there was no information about how concurrent care might contribute to care continuity (e.g., disruptive healthcare transitions during hospice enrollment) or care intensity, which are important to families who must manage the care for their children.
Implementation articles reinforced the challenges discussed in the descriptive studies such as care coordination and highlighted new challenges such as evolving goals of care and co-insurance. They also indicated that concurrent care implementation takes time from both from a clinical and state-level perspective, but in the long run improvement in access to hospice care were gained. The articles suggested that clinical implementation of pediatric concurrent care was challenging. Miller and colleagues discussed the clinical issues encountered in the absence of any regulations or guidelines from Medicaid.21 The authors highlighted the special challenges of care coordination in an environment where treatment and hospice have never participated in care coordination for pediatric patient and there are no state/federal rules of engagement. The articles examining state implementation of pediatric concurrent care found it was also difficult to implement at the state level. State implementation was sporadic for many years and was influenced by the economic conditions in the state.2,25 The overall findings from this literature highlighted the challenges in the absence of state or federal regulations, guidelines, or assistance. The consequence was that implementation of concurrent care was not timely or well organized.
Future Research
The findings from our review of the literature suggest several opportunities for future nursing research. First, the science of pediatric concurrent hospice care needs to move beyond conceptualization and generate baseline and outcomes data.29 No studies were identified that described the life-prolonging treatments or unique hospice services during concurrent care (e.g., care coordination), nor did any studies describe concurrent care patients, families, hospice providers, or treatment providers. There is a need for nurse researchers to identify and describe the different types of life-prolonging treatments children receive, along with detailed information about what concurrent hospice care is and how that might be different from standard hospice care. Nursing research might also describe the children who utilize concurrent care. Data describing children who enroll in concurrent care, standard hospice care, and life-prolonging treatments-only are warranted. Additionally, descriptive studies of children with specific health conditions or rural children who use concurrent hospice care might offer a first-time glimpse into the care of these vulnerable and understudied populations. Because concurrent hospice care is not available for patients over 21 years per Medicaid rules, studies exploring the transitioning out of concurrent care by adolescents and young adults might provide insight into the unique needs of these patients and their families. Studies describing the experience of families receiving and/or clinicians providing concurrent care might shed light on the barriers and facilitators of utilizing concurrent hospice care for children. Establishing a strong foundation with baseline and outcomes data would improve nursing clinical understanding, along with the evidence needed by nurses to deliver effective concurrent hospice care for children.
Second, the science of pediatric concurrent hospice care must improve the level of evidence generated. The analysis for this study found that no articles evaluated determinants, access to care, quality of health, cost of care, disparities, and effectiveness of concurrent hospice care. Nursing research might explore the effectiveness of the concurrent hospice care on outcomes important to patients, families, hospices, and systems. Although there is emerging adult literature on the influence of concurrent care on aggressive medical treatments, well-designed and rigorous nursing studies are needed that test the effectiveness of pediatric concurrent care against other care delivery methods. The use of sophisticated statistical techniques such as comparative effectiveness analysis would permit nurse researchers to conduct studies with observational data that not only allows for a head-to-head comparison of concurrent care performance, but also increases the level of evidence from studies of association to quasi-experimental studies. Effectiveness research could also be expanded to include different settings or insurance payers of pediatric concurrent care such as Medicaid versus private insurance concurrent care.
Third, the dearth of studies examining the economics of concurrent care suggests additional opportunities for future nursing research. Research is needed to understand the important explicit and implicit components of costs associated with both the hospice and treatment side of concurrent care.30 For example, it is known that concurrent care involves significant care coordination. However, accurately measuring the time and effort that nurses spend on care coordination makes evaluation of the costs associated with concurrent care challenging. Economic models of care can be developed that incorporate both explicit (revenues) and implicit (time and effort) cost components that provide a broader picture of the economic landscape of concurrent care. In addition, well-designed economic evaluations (e.g., cost-effectiveness studies) might offer important evidence to policy-makers and hospice administrators on how pediatric concurrent hospice care impacts financial performance. Cost information on concurrent care that highlights what is being paid by insurers and what is being covered by insurance payers might stimulate the conversation about payment reform for end-of-life care for children among key stakeholders. Ultimately, understanding the effectiveness or cost effectiveness of the concurrent hospice care might provide important information for nurses on the potential benefits and burdens of concurrent care for children and their families.
Finally, the approaches used to disseminate and implement pediatric concurrent hospice care at the state-, provider-, and family-levels should be explored. Given that pediatric concurrent care was implemented by state Medicaid office with little or no guidance, regulations, or deadlines, exploring how Medicaid offices disseminated information to key stakeholders and hospices should be investigated. For example, studies of the collaborations between Medicaid offices and state pediatric end-of-life and palliative care coalitions might provide critical information on hospice-level uptake of concurrent care. Baseline and outcomes data on how concurrent care was implemented among hospices and treatment providers is also needed. Nursing studies investigating the fidelity of concurrent care implementation within and across the states might offer insights into how concurrent care has been adapted since enactment in 2010. Examining the implementation strategies used nationally (e.g., toolkits) or within states (e.g., social media) might improve nurses’ understanding of implementation uptake and sustainability among hospices and families. Thus, nursing research can contribute important new information and expand our understanding of the best practices in disseminating and implementing future policy-mandated changes for the care of children at end of life.
In summary, the scoping review revealed that the science of pediatric concurrent care is dated and focused on descriptive studies and narratives. There is emerging, adult research on the effect of concurrent care on patient outcomes, while there is sparse evidence about how concurrent care has been implemented. Future nursing research should focus on producing baseline data about pediatric concurrent care from which to conduct outcomes studies that generate a higher level of evidence needed to inform nursing practice while understanding the clinical, economic, and policy implications of concurrent hospice care for children at end of life and their families.
Acknowledgments
Funding Source: This publication was made possible by Grant Number R01NR017848 from the National Institute of Nursing Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Contributor Information
Lisa C. Lindley, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
Jessica Keim-Malpass, School of Nursing, University of Virginia, Charlottesville, Virginia 22908.
Radion Svynarenko, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
Melanie J. Cozad, Department of Health Services Policy and Management, Center for Effectiveness Research in Orthopedics, University of South Carolina, Columbia, SC 29201.
Jennifer W. Mack, Department of Pediatric Oncology and Division of Population Sciences, Dana-Farber Cancer Institute, Boston Children’s Hospital, Boston, MA 02214.
Pamela S. Hinds, The William and Joanne Conway Chair in Nursing Research, Executive Director, Department of Nursing Science, Professional Practice, and Quality Outcomes, Research Integrity Officer, Children’s National Hospital, Washington, D.C. 20010, Professor, Department of Pediatrics, The George Washington University.
References
- 1.Murphy SL, Mathews TJ, Martin JA, Minkovitz CS, Strobino DM. Annual Summary of Vital Statistics: 2013–2014. Pediatr. 2017;139(6):1–12. [DOI] [PubMed] [Google Scholar]
- 2.Keim-Malpass J, Lindley LC. Repeal of the affordable care act will negatively impact children at end of life. Pediatr. 2017;, 140(3):epub. [DOI] [PubMed] [Google Scholar]
- 3.Lindley LC, Cozad MJ, Fortney CA. Pediatric complex chronic conditions: Evaluating two versions of the classification system. West J Nurs Research. 2019; Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindley LC, Mack JW, Bruce DJ. (2016). Clusters of multiple complex chronic conditions: A latent class analysis of children at end of life. J Pain Symptom Manage. 2016; 51(5): 868–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyden JY, Curley MAQ, Deatrick JA, Ersek M. Factors Associated With the Use of U.S. Community–Based Palliative Care for Children With Life-Limiting or Life-Threatening Illnesses and Their Families: An Integrative Review. J Pain Symptom Manage. 2018;55(1): 117–31. [DOI] [PubMed] [Google Scholar]
- 6.Brown CC, Tilford JM, Payakachat N, Williams DK, Kuhlthau KA, Pyne JM, et al. Measuring Health Spillover Effects in Caregivers of Children with Autism Spectrum Disorder : A Comparison of the EQ - 5D - 3L and SF - 6D. PharmacoEcon. 2019;37(4): 609–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mooney-Doyle K, Lindley LC. The association between poverty and family financial challenges of caring for medically complex children. Nurs Econ. 2019; 37(4):198–208. [Google Scholar]
- 8.Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, D.C.: National Academy Press; 2015. [PubMed] [Google Scholar]
- 9.Lindley LC, Keim-Malpass J. Quality of pediatric hospice care for children with and without multiple complex chronic conditions. Intl Jf Palliativ Nurs. 2017;23(5):112–9. [DOI] [PubMed] [Google Scholar]
- 10.Lindley LC, Cohrs AC, Keim-Malpass J, Leslie DL. Children enrolled in hospice care under commercial insurance: A comparison of different age groups. Am J Hospice Palliativ Med.2019:36(2):123–9. [DOI] [PubMed] [Google Scholar]
- 11.Mooney-Doyle K, Keim-Malpass J, Lindley LC. The ethics of concurrent care for children: A social justice perspective. Nursing Ethics. 2018: epub. [DOI] [PubMed] [Google Scholar]
- 12.Lindley LC. Healthcare Reform and Concurrent Curative Care for Terminally Ill Children. J Hospice Palliativ Nurs, 2011;13(2):81–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keim-Malpass J, Hart TG, Miller JR. Coverage of palliative and hospice care for pediatric patients with a life-limiting illness: A policy brief. J Ped Health Care. 2013;27:511–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mor V, Wagner TH, Levy C, Ersek M, Miller SC, Gidwani-Marszowski R, et al. Association of Expanded VA Hospice Care with Aggressive Care and Cost for Veterans with Advanced Lung Cancer. JAMA Oncology. 2019;5(6): 810–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mor V, Joyce NR, Cote DL, Gidwani RA, et al. The rise of concurrent care for veterans with advanced cancer at end of life. Cancer. 2016;22(5):782–90. [DOI] [PubMed] [Google Scholar]
- 16.Harrison KL, Connor SR. First medicare demonstration of concurrent porovision of curative and hospice services for end-of-life care. AJPH. 2016;106(8):1405–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hargadon A, Tran Q, Stephen K, Homler H. A trial of concurrent care: Shedding light on the gray zone. J Palliativ Med. 2017: 20(2):207–10. [DOI] [PubMed] [Google Scholar]
- 18.Peters M, Godfrey C, Khalil H, et al. Guidance for Conducting Systematic Scoping Reviews. Int J Evid Based Healthc. 2015;13:141–146. [DOI] [PubMed] [Google Scholar]
- 19.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Method. 2018;18(143):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walsh RA. A metter of life, death, and children: The patient protection and affordable care act section 2302 and a shifting legal paradigm. Southern CA Law Rev. 2013:86(119):1119–64. [Google Scholar]
- 21.Miller EG, Laragione G, Kang TI, Feudtner C. Concurrent care for the medically complex child: lessons of implementation. J Palliat Med, 2012: 15: 1281–3. [DOI] [PubMed] [Google Scholar]
- 22.Haverhals LM, Manheim CE, Mor V, Ersek M, Kinosian B, et al. The experience of providing hospice care concurrent with cancer treatment in the VA. Supportiv Care Cancer. 2019:27(4):1263–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Hospice and Palliative Care Organization – Children’s Project on Palliative/Hospice Services. ChiPPS Pediatric Palliative Care Newsletter – November 2013 (#33). Available at https://www.nhpco.org/sites/default/files/public/ChiPPS/ChiPPS_Nov-2013_Issue-33.pdf. Accessed January 15, 2017.
- 24.Lotstein D, Lindley LC. Improving home hospice and palliative care policies. Pediatr. 2019;144(2):e20183287. [DOI] [PubMed] [Google Scholar]
- 25.Lindley LC, Edwards SL, Bruce DJ. (2014). Factors influencing the implementation of healthcare reform: An examination of the Concurrent Care for Children provision. Am J Hospice Palliativ Med, 2014:31(5):527–53. [DOI] [PubMed] [Google Scholar]
- 26.Mack JW, Chen K, Boscoe FP, Gesten FC, et al. High intensity of end-of-life care among adolescent and young adult cancer patients in the New York State Medicaid program. Med Care. 2015; 53(12):1018–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oliver DP, Washington KT, Demiris G, White P. Challenges in implementing hospice clinical trials: Preserving scientific integrity while facing challenges. J Pain Symptom Manage. 2020; 59(2): 365–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maetens A, De Schreye R, Faes K, Houttekier D, Deliens L, Gielen B, De Gendt C, Lusyne P, Annemans L, Cohen J. Using linked administrative and disease-specific databases to study end-of-life care on a population level. BMC Palliat Care. 2016; 15(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Romo RD, Carpenter JG,Buck HG, Lindley LC, Xu J, Owen JA, Sullivan SS, Bakitas M, Dionne-Odom JN, Zubkoff L, Matzo M. On behalf of the HPNA Research Advisory Council. HPNA 2019-2022 research agenda: Development and rationale. J Hospice Palliativ Nurs. 2019; 21(4): e17–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.May P, Cassel JB, Economic outcomes in palliative and end-of-life care: Current state of affaors. Ann Palliat Med. 2018; 7(suppl 3):s244–8. [DOI] [PubMed] [Google Scholar]


