Abstract
The purpose of this paper is to briefly present a methodological framework that does not require cumbersome investigations for a first assessment of the financial sustainability of policies aiming to remove or reduce healthcare user fees (the so-called free healthcare policy [FHCP]). This paper is organized in two main sections. The first analyzes the various possibilities available to finance an FHCP. Using several scenarios, it includes a special focus devoted to the calculus of what to consider when assessing the sustainability of expanding fiscal space for financing the FHCP. The second section relies on the current FHCP being implemented in Burkina Faso to illustrate a selection of specific issues raised in the methodological framework. The results suggest that sustainable FHCP financing is not outside the range of the government but does represent a significant challenge, as it will require, both currently and in the future, complex and delicate budget trade-offs at the highest governmental levels, regardless of other policy options to be considered.
Electronic supplementary material
The online version of this article (10.1007/s40258-019-00506-2) contains supplementary material, which is available to authorized users.
Key Points for Decision Makers
| Many countries have embarked on policies to remove or reduce user fees (the so-called free healthcare policy). It is not enough to be able to finance it for a year or two. It is essential to consider the medium- and long-term sustainability of the financing of this policy. Here, we propose a methodological framework for a rapid first assessment that is easy to apply in various contexts. |
| The financing strategy must be based on realistic assumptions and scenarios. |
| It is cautious to anticipate a need to adjust the policy in order to be able to provide a relevant response to a possible funding gap and avoid making important decisions in a hurry. |
| A commitment at the highest level of the State, above the Ministry of Health, will be necessary if funding requires an increase in public health expenditure and/or delicate trade-offs at sectoral or macroeconomic levels. |
Introduction
The adoption of health-related sustainable development goals (SDGs) and the momentum towards universal health coverage have reinforced the need to increase health financing and simultaneously revived the debate over the abolition or reduction of health user fees.
Critics of user fees argue that they are a strong barrier to healthcare access and an obstacle to better health outcomes and are to blame for “catastrophic” health expenditures, pushing a significant number of households below the poverty line or increasing the poverty of those who are already poor [1–4]. However, beyond specific country experiences, which are abundant in the literature, systematic reviews show that the conclusions are not as clear cut, especially when considering a medium- and long-term perspective and controlling for relevant and potentially confounding factors with robust methodologies [5–7].
A growing number of countries are implementing a policy that removes or reduces user fees—the so-called free healthcare policy (FHCP)—relying on advocacy from non-governmental organizations (NGOs), the World Health Organization (WHO) and the United Nations International Children’s Emergency Fund (UNICEF) (among others) and generally benefiting from the financial support of several of their external partners. Most of these countries do not remove or reduce all user fees for everyone, instead targeting either specific services and specific diseases (HIV, tuberculosis [TB], malaria, renal failure, obstetric care, etc.) or specific population groups (mothers and children, elderly individuals, those in poverty).
The main expected effects from these FHCPs are a large increase in the utilization of healthcare facilities (based on the price elasticity of demand), especially by those in poverty (therefore improving equity in access to and the financing of care), a sharp decline in catastrophic health expenditures, and better health outcomes. However, the literature shows that the expected effects are not always achieved, far from it, and that the situation is often much more complex than some advocates suggest. Some country-specific studies [8–11] and studies on groups of countries [12–18] have shown a growth and then a decline in the use of healthcare facilities, drug shortages, deteriorations in quality of care, increased staff absenteeism, that the FHCP has not always been proportionally beneficial to the poorest, and a lack of robust overall relationship between the policies implemented and improvements in health outcomes.
Most of these studies have shown that the careful design of FHCPs is crucial for their success and to limit the risks of effects running counter to those intended. They have highlighted that financing issues are generally at the origin or have been factors amplifying the deleterious effects or leading to results lagging behind those that were expected. Weaknesses in financing mainly include a lack of funding to offset the decrease in resources due to the removal or reduction of user fees and inappropriate compensation processes for health facilities. Such weaknesses often mirror a lack of rigorous ex ante preparation1 and overly optimistic expectations regarding the sustainability of FHCP financing strategies beyond the very short term.
Currently, despite pressure from their civil societies and advocacy groups, many governments are reluctant to engage in significant policies to reduce user fees or are very cautious because of concerns over their financial sustainability.
Therefore, it would be useful for decision makers to have a methodology to quickly assess, as a preliminary analysis, whether or not FHCP financing appears broadly sustainable before undertaking detailed studies on the content and funding modalities of such a policy. Thus, the objective of this paper is to present a methodological approach that does not require cumbersome investigations and that uses existing data to approximate the scope of possibilities and to provide useful information to decision makers to gradually develop a realistic and viable strategy for financing an FHCP.
This paper is structured as follows. The first section presents the proposed methodological framework and its strengths and weaknesses. The second section, which is based on the experience of Burkina Faso, illustrates and discusses a selection of issues highlighted in the methodological framework. A short conclusion summarizes the results and highlights the potential advantages of implementing a cautious gradual policy.
Methodological Framework for Analyzing the Financial Sustainability of a Free Healthcare Policy (FHCP)
What is Meant by the Financial Sustainability of an FHCP
As noted by Walugembe et al. [19], interest in understanding the sustainability of effective public health interventions is increasing, leading to a multiplicity of terminologies and constructs across definitions of sustainability. For example, Moore et al. [20] provide a definition of sustainability of public health interventions that is one of the broadest in the literature. It is structured around five blocks of elements: the continued delivery or institutionalization of clinical interventions or programs, the maintenance of outcomes for individuals or for the system after the initial implementation phase, the maintenance of behavioral change at the level of providers and patients, evolution-adaptation, and a time perspective. Walugembe et al. [19] highlight that decision makers often have a limited focus on sustainability in designing public health interventions, which, in turn, limits the likelihood of their sustainability.
Models or methods for analyzing sustainability in public health interventions [20–22] undeniably provide a useful framework for decision makers, but they are of little help in concretely assessing the sustainability of financial strategies for substituting user fees, as the critical point is to consider how to mobilize the total resources required in a medium-long-term perspective.
In the abstract, the financing of an FHCP is not unsustainable in the economic sense as long as governments make the necessary trade-offs and are willing to pay the price so that health expenditures absorb an increasing share of gross domestic product (GDP). However, in the real world, the situation is different. The consequences of the measures taken may prove unsustainable, first in the political sense of the term and then economically, since, in one way or another, they raise the issue of society’s tolerance for (in)equity and for the redistribution of resources through taxes and the structure of public spending, with “winners and losers.”
Conceptually, six main options must be combined to design financial strategies to substitute user fees (Fig. 1): (1) the potentially available fiscal space, (2) improvements in productivity and efficiency in healthcare delivery, (3) adjusting the bundle of free health services, (4) the conditions under which households can benefit, (5) considering cross-subsidies, and (6) insurance development.
Fig. 1.
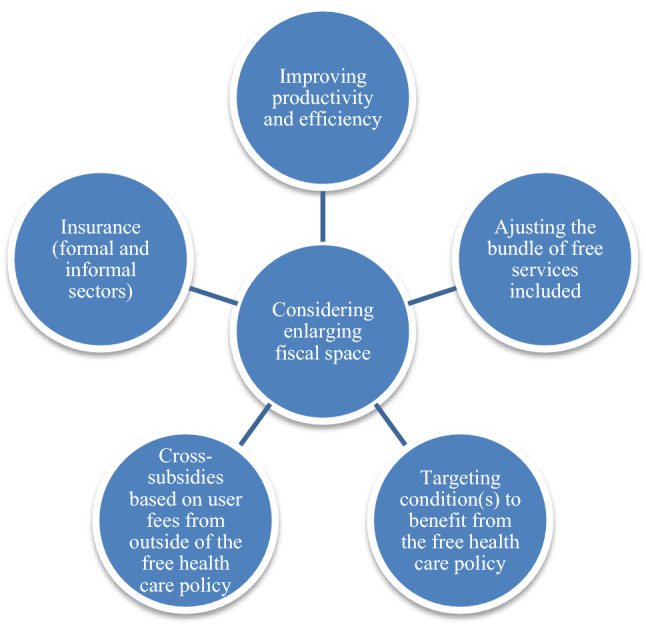
Main options to finance a free healthcare policy
In sub-Saharan African countries, the largest share of health financing is public financing. In 2016, public financing represented 37% of total health expenditures, direct payments represented 32%, and health aid represented 14% [23].2 As public insurance mechanisms are very limited in most countries, public financing is essentially budgetary financing, including part of health aid. As a result, the issue of FHCP sustainability is first and foremost a matter of fiscal space, although additional options must be mobilized. For this reason, this issue is the focus of the case study developed in Sect. 3.
We consider that a sustainable strategy for a partial or total replacement of user fees must fulfill four closely intertwined conditions.
It must be based on a rigorous assessment of the financial amount required to achieve the government’s FHCP objectives and consider how to realistically and cautiously finance a potential funding gap.
The short- and medium-term availability of the resources required must not risk weakening the state’s financial position or its commitments to its external partners. In particular, this would be the case if the financing strategy adopted led the government to accumulate arrears in payments to domestic or external creditors.
Regardless of the financing strategy adopted, the disbursement process of the required resources must not lead to instability in healthcare financing, and the annual disbursement timetable must match the timing of expenditure needs to achieve the objectives set out by the health policy. For example, the disbursement of resources to compensate healthcare facilities for the reduction of user fees could be concentrated in the last two quarters of the year, which would have the effect of delaying or reducing some activities. The instability of funding from 1 year to the next, as well as an inappropriate infra-annual disbursement agenda, can create lasting dysfunctions within the implementation of the healthcare policy.
The financing of the FHCP must not erode productivity and efficiency in service delivery. A lack of resources or their late availability can lead to a decrease in the number of people attending health facilities (e.g., why go to a health center if drug disruptions are recurrent and long lasting?) or make some tests impossible, which will directly affect the productivity of health workers and health outcomes. If the additional remuneration of staff made possible by user fees is not financed in some other way, the risk of increasing absenteeism and of undermining intrinsic and extrinsic motivations of staff is substantial, impairing the quality and efficiency of health services.
The Proposed Quick Assessment Method
To the best of our knowledge, the most comprehensive operational approach that can be used to identify a strategy for replacing user fees (even if doing so is not its initial objective) is that developed by WHO and the former German Technical Cooperation Agency (now the German Corporation for International Cooperation [GIZ]) in the SimIns modeling tool [24]. SimIns is a computerized tool that allows projections for health resources and expenditures over a 10-year period. In particular, it allows simulations to be carried out to compare alternative health financing scenarios, such as (1) budget financing supplemented by premium contributions and (2) social insurance financing supplemented by insurance contributions. It requires various assumptions, including projections for revenues and expenditures, population changes, GDP, interest rates, the unit cost of care, and utilization rates for outpatient and inpatient care. An example of this methodology applied to Kenya can be found in Okungu et al. [25]. This approach has the disadvantage of its advantages: it allows in-depth and detailed analyses and offers great flexibility in combining alternatives, but it requires cumbersome investigations that do not fit well with the need for a rapid diagnostic tool as a preliminary analysis to identify the extent to which the FHCP is financially sustainable or not.
The approach proposed here is different. Considering, on the one hand, the structure of health financing in Africa, which is mainly based on a noncontributory model and, on the other hand, that the reduction of user fees requires almost immediate compensatory financing, which can only come from budgetary sources, the rapid diagnostic method proposed here focuses on the issue of fiscal space. However, it underlines the importance of also considering other options whose main effects are in the medium and long term, not the short term.
The proposed method has four main advantages. (1) It is quick to run, does not require sophisticated investigations and uses currently available data; (2) it allows a realistic assessment of the order of magnitude of the resources required and compares it with budgetary constraints; (3) it facilitates taking into account different scenarios for modulating the content of the service package that will benefit from the reduction of user fees; and (4) it provides the Ministry of Health (MoH) essential information for dialogue with the Ministry of Finance (MoF) (which plays a crucial role in this particular context) and with donors and for discussions during budgetary conferences.
However, as its main limitation, the method does not allow investigations for assessing the potential margin of maneuver given by insurance development, by improvements in productivity and efficiency, and by measures that would aim to increase cross-subsidies. This will have to be done at a later stage if necessary.
Issue of Expanding Fiscal Space and Dealing with Constraints for the Sustainable Financing of an FHCP
To finance its FHCP, the government would have to mobilize additional resources to compensate for the loss of resources as a result of abolishing or reducing user fees and to confront the expected increase in healthcare demand. This necessity raises the issue of expanding fiscal space. Understanding this calculus is a fundamental aspect of any analysis of FHCP sustainability.
First, three preliminary questions arise:
What are the sources of the data? As the first step, a rapid assessment should be based on existing data from the MoH, the MoF, and donors to make a crude estimate of any potential funding gap. The MoF is a key interlocutor in updating and complementing financial data from the MoH and in helping gain a better understanding of factors that, as observed in several countries, lead to a low budget execution rate for current expenditures.
What is the timeframe for the analysis? A reasonable period is 5 years, depending on macroeconomic projections (and medium-term expenditure frameworks [MTEFs]) for the healthcare sector, if any.
How many scenarios will there be? It will be appropriate to construct three scenarios. The first, a baseline scenario, will be built from existing data. However, experience shows that projections often underestimate expenditures and can be optimistic about expected resources. A “low-assumption” scenario will therefore be essential and should be complemented with a “high-assumption” scenario based on the most favorable assumptions of the macroeconomic projections.
In his pioneering work, Heller [26] defined the concept of fiscal space as “the availability of budgetary room that allows a government to provide resources for a desired purpose without any prejudice to the sustainability of a government’s financial position [emphasis added].” One must keep in mind that an FHCP will always compete with other health expenditures or sectors when expanding fiscal space.3
There are different ways in which a government can create such fiscal space to finance a reduction in user fees. Additional revenues can be raised through tax measures or by strengthening tax administration. A government can reprioritize public expenditures in favor of the health sector or make cuts in lower-priority health spending to fund the reduction of user fees. Borrowing resources, from either domestic or external sources, is theoretically an option, although doing so is not advisable for the reasons we explain in Sect. 4.2. Governments may also benefit from any fiscal space arising from external grants. Finally, governments can use their power of seigniorage.4
Table 1, which is based on a simplified standard budget framework, highlights the main specific cases that we focus on to assess the sustainability of the public financing of an FHCP. It presents several hypothetical scenarios constructed as cases from 2015 to 2017.5
Table 1.
Scenarios for illustrating the main options regarding expanding fiscal space for a sustainable free healthcare policy
| 2015 | 2016 A | 2016 B | 2016 C | 2017 A | 2017 B with 5% GDP growth | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LCU | % GDP | LCU | % GDP | LCU | % GDP | LCU | % GDP | LCU | % GDP | LCU | % GDP | ||
| 1 = 2 + 3 | Total revenue and grants | 20,000 | 16.7 | 20,000 | 16.7 | 22,000 | 18.3 | 22,000 | 18.3 | 22,000 | 18.3 | 22,990 | 18.3 |
| 2 | Total revenue | 18,000 | 15.0 | 18,000 | 15.0 | 19,800 | 16.5 | 19,800 | 16.5 | 19,800 | 16.5 | 20,790 | 16.5 |
| 3 | Grants | 2000 | 1.7 | 2000 | 1.7 | 2200 | 1.8 | 2200 | 1.8 | 2200 | 1.8 | 2200 | 1,7 |
| 4 = 5 + 9 | Expenditure and net lending | 25,000 | 20.8 | 26,000 | 21.7 | 26,000 | 21.7 | 25,000 | 20.8 | 25,300 | 21.1 | 25,600 | 21.3 |
| 5 = 6 + 7+ 8 | Current expenditure | 25,000 | 20.8 | 26,000 | 21.7 | 26,000 | 21.7 | 25,000 | 20.8 | 25,300 | 21.1 | 25,600 | 21.3 |
| 6 | Healthcare | 3000 | 2.5 | 4000 | 3.3 | 4000 | 3.3 | 4000 | 3.3 | 4000 | 3.3 | 4150 | 3,3 |
| 7 | Other sectors | 22,000 | 18.3 | 22,000 | 18.3 | 22,000 | 18.3 | 21,000 | 17.5 | 21,000 | 17.5 | 21,150 | 17.6 |
| 8 | Interest payments | 0 | 0 | 0 | 0 | 300 | 300 | ||||||
| 9 | Investment expenditure (all sectors) | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| 10 = 1 − 4 | Overall balance (cash basis) | − 5000 | − 4.2 | − 6000 | − 5.0 | − 4000 | − 3.3 | − 3000 | − 2.5 | − 3300 | − 2.8 | − 2610 | − 2.2 |
| 11 = 12 + 15 | Financing | 5000 | 5000 | 4000 | 3000 | 2700 | 2610 | ||||||
| 12 = 13 + 14 | Domestic (net) | 2000 | 2000 | 1000 | 1000 | 900 | 810 | ||||||
| 13 | Drawings | 2000 | 2000 | 1000 | 1000 | 1000 | 910 | ||||||
| 14 | Amortization | 0 | 0 | − 100 | − 100 | ||||||||
| 15 = 16 + 17 | External (net) | 3000 | 3000 | 3000 | 2000 | 1800 | 1800 | ||||||
| 16 | Drawings | 3000 | 3000 | 3000 | 2000 | 2000 | 2000 | ||||||
| 17 | Amortization | 0 | 0 | 0 | 0 | − 200 | − 200 | ||||||
| 18 = 11 − 10 | Financing gap | 0 | − 1000 | 0 | 0 | − 600 | 0 | ||||||
| 19 | GDP | 120,000 | 120,000 | 120,000 | 120,000 | 120,000 | 126,000 | ||||||
| 20 | GDP growth (%) | 0 | 0 | 0 | 0 | 5 | |||||||
| 21 | Public health expenditure % total public expenditure | 12.0 | 15.4 | 15.4 | 16.0 | 15.8 | 16.2 | ||||||
| 22 | Public health expenditure % GDP | 2.5 | 3.3 | 3.3 | 3.3 | 3.3 | 3.3 | ||||||
GDP gross domestic product, LCU local currency unit
Notably, in every country, many of the questions arising over the sustainable financing of an FHCP are exogenous to the MoH and relate to overall macroeconomic policy and commitments made by the state to its external financial partners, including the International Monetary Fund (IMF). Therefore, analysis will have to abide by the major data in the macroeconomic projections (including the MTEF).
In the 2015 scenario of Table 1, public expenditure on health (PHE; line 6) is 3000 currency units (CU), which represents 12% (line 21) of total public expenditures (line 4) and 2.5% of GDP (line 22). There is a deficit (line 10) of 5000 CU; this deficit is financed through domestic borrowing of 2000 CU (line 12) and external borrowing of 3000 CU (line 15). In the following year, the 2016A scenario, the government decides to increase PHE by 1000 CU to finance its FHCP, which was found to be underfinanced. As a result, PHE is 4000 CU (line 6), i.e., 15.4% of public expenditures and 3.3% of GDP. Nothing else has changed in terms of revenue, grants, or deficit financing (lines 12–15). Because, in this context, PHE has increased, the overall deficit balance of 5000 CU in 2015 (4.2% of GDP) increases to 6000 CU in 2016, which corresponds to a new financing requirement. However, the resources mobilized, unchanged from 2015, are 5000 CU. Therefore, there is a financing gap: this gap means that the government cannot finance all its planned expenditures without resorting to other options.
The first conceivable way to fill this gap is presented in the 2016B scenario. The government increases fiscal revenue by 1800 CU, which thus rises to 19,800 CU. Since GDP has not increased, this increased revenue comes from raising taxes, widening the tax base, or improving tax collection. Between 2015 and 2016, the overall tax rate thus increases from 15 to 16.5% of GDP. At the same time, let us assume that discussions between the government and its external partners have resulted in a grant increase of 200 CU (line 3). As a result, the deficit is lowered to − 4000 CU (3.3% of GDP) instead of − 5000 CU (4.2% of GDP) in 2015.
Thus, the government can reduce its borrowing (in this case, domestic borrowing) by 1000 CU (line 12), and there is no longer a financing gap (line 18). The decisions made have released an additional 2000 CU (lines 2 and 3), whereas overall expenditure has risen only by the additional 1000 CU allocated to the FHCP. In this example, increasing the tax rate and grants has made it possible to expand the fiscal space required to finance free healthcare while reducing the need for borrowing. However, the tax rate is not within the purview of the MoH, and the increase in grants is largely exogenous. These aspects demonstrate that financing an FHCP is not only a question of healthcare policy but also must necessarily be integrated into overall socioeconomic policy.
The 2016C scenario presents another possibility for expanding fiscal space for the FHCP that supplements the 2016B scenario, i.e., modifying the composition of public expenditures by reducing expenditures other than those on healthcare (− 1000 CU; line 7). The share of healthcare expenditures in overall expenditures thus automatically increases from 15.4% in 2016B to 16%, without an increase in healthcare expenditures compared with 2016B. At the same time, a reduction in expenditures other than those on healthcare has created a reduction in total expenditures (line 4) and a reduction in the deficit, which falls from − 4000 to − 3000 CU (line 10). Thus, there is a new reduction in the borrowing requirement (line 16).
Thus far, we have not accounted for the debt service resulting from deficit financing. Let us imagine that, in the 2016B scenario, increasing the deficit by 1000 CU as a result of the financing of the FHCP has been financed by borrowing and that this borrowing comes with a grace period of 1 year and is repayable over 10 years at a rate of 10%. In 2017, debt service will have increased by 100 CU for amortization and by 100 CU for interest payments. Public expenditures (line 4) will then have increased by 100 CU, as will the deficit and the need for additional borrowing, all else being equal: all this only as a result of the increase in health expenditures. The 2017A scenario reproduces this analysis for total debt in relation to 2016C. Therefore, there is a resulting financing gap of 600 CU (300 CU in interest payments, line 8; 100 CU for amortization of domestic borrowing, line 14; and 200 CU for external borrowing, line 17). Therefore, 600 CU are required to finance the total planned expenditures. Taking all sectors into account, the FHCP must thus be considered a major priority to be financed sustainably.
This last point highlights that the sustainable financing of an FHCP should consider the risk of dangerous resource instability if expanding fiscal space is not sustainable. This means that, in the future, the government must be able to finance both its desired expenditure program—including the recurring costs of health expenditures—and the total debt service, which will have resulted from borrowing to finance the FHCP in previous years: expanding fiscal space today can create an unsustainable situation tomorrow.
The 2017B scenario integrates a 5% growth in GDP, which goes from 120,000 to 126,000 CU. Fiscal revenue increases automatically for an unchanged tax rate of 16.5% of GDP and increases to 20,790 CU instead of 19,800 CU in 2017A (line 2), which results in an expanded fiscal space. In this example, the government allocates 150 CU to increase healthcare expenditures and a similar amount to other sectors or additional expenditures of 300 CU. Since the increased revenue has been 990 CU and the increased expenditures 300 CU (150 + 150), the result is a reduced deficit, which falls from − 3300 CU in 2017A to − 2610 CU in 2017B (3300 − [990 − 300]).
In fact, the government may very well have earmarked the entire fiscal gain from GDP growth to healthcare. However, to limit its borrowing, the government may have decided to spread this additional revenue between health, other sectors, and the budget deficit. The share of healthcare expenditures has reached 16.2% of total public expenditures (vs. 15.8% in 2017A). If the government had decided to earmark to the FHCP all increased fiscal revenue from growth (i.e., 990 CU), then PHE would have reached 4990 CU, approximately + 25%, without changing other expenditures. The additional resources required to finance free healthcare would have been largely mobilized.
Earmarking Resources and Financing an FHCP
According to the Abuja Agreement signed in 2001, governments made a commitment to spend at least 15% of total public expenditures on health. The indicator is ambiguous since it is a ratio, and any increase in the ratio does not necessarily correspond to an increase in the real volume of resources available for health [25]. However, this indicator is very popular and is at least a dependable advocacy element, as a greater budgetary priority given to healthcare will usually result in increased resources for the health sector. Thus, once again, the problem is the issue of fiscal space sustainability.
Earmarking domestic or external resources to an FHCP is a commonly considered approach. However, as it creates opportunities and risks, it is important to properly assess its potential contribution to the FHCP. A critical issue is fungibility. Fungibility is inherent in any earmarking scheme, including when free healthcare mechanisms are integrated into vertical funds [27, 28]. The key question is as follows: will the government simultaneously make less (or the same) effort to support the policy than could have been envisaged without the earmarked funding? Therefore, regarding foreign aid, it is critical to pay particular attention over time to the parallel development of domestic financing (earmarked or not) for the FHCP with the evolution of earmarked external assistance.6 Assessing what arrangements will replace earmarked aid when it stops (the so-called transition issue) is a hot topic. Another key point is the extent to which fragmentation in earmarked financing sources may or may not weaken the effectiveness and efficiency of the FHCP.
Contribution of Improved Productivity and Efficiency to Sustaining an FHCP
Improving productivity and (allocative and technical) efficiency must be a major priority when considering the issue of a sustainable FHCP. There are five main reasons. First, common sense makes it crucial to use the limited available resources to obtain the best value for money. Second, some low- and lower-middle-income countries are experiencing a change in their epidemiological profile, causing a dual burden: communicable diseases still account for a significant share in overall morbidity and mortality, whereas the burden of chronic diseases is progressing rapidly. Third, while these countries have benefited from the remarkable rise in health aid over the last two decades, health aid has entered a plateau phase. Additionally, an increasing number of voices in various forums are considering that, in recent years, too much attention has been paid to social sectors—that the pendulum has swung too far—to the detriment of public expenditure in sectors with more directly productive effects; this should temper a vision about future donor interest in financing FHCPs that is too optimistic. Fourth, improving efficiency in expenditure on an FHCP heavily depends on factors on which the MoH can directly act, especially since the care targeted by such policies is mainly at the first level of healthcare systems and relies on well-known and generally unsophisticated, cost-efficient protocols. Lastly, the literature suggests a large margin of maneuver to improve efficiency in the healthcare system [27, 29]; however, most monetary gains from improved productivity and efficiency will not be materialized in the short term.
Using Other Options
Adjusting the contents of the bundle of care covered by the FHCP. A policy can move from unsustainable to sustainable by adjusting the types of care and services covered. This option is particularly interesting when the financing gap is large.
Qualified free healthcare. This is the issue of opting for a policy of no user fees conditioned on income and poverty (or other) criteria. Among those households benefiting unconditionally from the FHCP, some are able to contribute.
Cross-subsidies. One must consider the extent to which a government can use cross-subsidies to contribute to financing its FHCP, i.e., making some people pay more for their own healthcare to generate a “surplus” to contribute to FHCP financing.
Developing insurance. Some countries have paired the implementation of free healthcare strategies with the development of insurance mechanisms. Although insurance is conceptually a preferred approach, it does not necessarily guarantee sustainable free healthcare financing, and it takes time to be implemented on a large scale, as shown among others by the experiences of Ethiopia, Ghana, China, and Thailand [30, 31].
Illustration of the Methodological Framework: Brief (and Partial) Assessment of the Sustainability of FHCP Financing in Burkina Faso
The case of Burkina Faso is used to illustrate a selection of the issues we have presented.
Background
The Macroeconomic Context and the Health Situation
Burkina Faso is a sub-Saharan country whose 2016 population was 18.5 million. Classified as a low-income country (LIC), in 2017, it had a per capita GDP of approximately purchasing power parity (PPP) $US1800.7 The government has engaged in implementing an ambitious 5-year national economic and social development plan (PNDES) for 2016–2020 adopted in July 2016. Following the political transition of 2014–2015, the government had to address social tensions and deliver tangible improvements in the living standards of the population. The PNDES aims for a sharp acceleration in economic growth and a lowering of the poverty rate from 40.1% in 2014 to below 35% by 2020 [32]. The plan is based on three strategic pillars: (1) improved economic governance; (2) human capital development; and (3) structural transformation of the economy and private sector development. This proactive policy requires a significant financial effort from the government and large donor support. Uncertainty still hangs over the amounts of external funding that will be available for 2018–2021.
The context in which the current FHCP is implemented has been characterized as a “solid macroeconomic situation” by the IMF [32]. The authorities and the IMF expect a constant-price GDP annual growth rate of 6.5% from 2018 to 2021. Current revenue will increase from 17.1% of GDP in 2016 to 21.1% in 2021. Following a peak at 5.4% of GDP in 2017, the overall deficit should gradually decline again to slightly below 3% in 2020–2021, which is in line with the West African Economic and Monetary Union (WAEMU) convergence criterion. In 2017, the total public debt-GDP ratio was 37% of GDP, and it is expected to remain at approximately this level through 2021. The risk of debt distress is low [32].
Despite significant progress over the past two decades, health indicators remain poor, with a life expectancy at birth of 60 years (62 in LICs), a maternal mortality rate of 371 per 100,000 live births (450 in LICs), a mortality rate for children aged < 5 years of 88.4 per 1000 live births (76.3 in LICs), and a malaria incidence of 389.2 per 1000 people at risk (109.99 in LICs) [33]. The share of health in the central government budget is relatively high, exceeding 12%8 since 2012 (vs. < 9% in Botswana, Cameroon, and Côte d’Ivoire, all of which are low-middle-income countries [23]. Despite this government effort, user fees bear the largest part of total health expenditures (38%), followed by multilateral and bilateral partners (35%) and the government (23%) [34].
The Free Healthcare Policy
The Burkinabe FHCP addresses the goals of both reducing poverty by lowering catastrophic health expenditure and developing human capital. The first significant policy for reducing user fees was formulated in 2003, followed by free curative care for those aged <5 years and pregnant women in cases of severe malaria (funded by the Global Fund, then the US Agency for International Development [USAID], in 2011, and the government in 2012) and by malaria prevention with the distribution of free impregnated nets.9 Partial exemption covering 80% of the cost for emergency obstetric and neonatal care (EmONC) was introduced in 2006. In 2010, the FHCP was enlarged to include free access to sputum examination and chest X-ray (TB), package care for prenatal visits, and antiretrovirals (ARVs). In 2016, free universal care was set up for those aged < 5 years and pregnant women at public and approved private health institutions, followed by user fee exemption for precancerous cervical lesion screening and treatment for women aged ≥ 25 years and early breast cancer detection for women aged ≥ 15 years [35, 37, 38].
Table 1 in the Electronic Supplementary Material (ESM) provides more information about the targeted services and the benefit packages of the five programs included in the FHCP.
The implementation of the FHCP has encountered severe difficulties that are not specific to Burkina Faso. Previous analyses showed an inadequate financing for removing user fees, which, in a domino effect, led to systemic dysfunction and a loss of effectiveness and efficiency [34, 35]. This issue is well-documented regarding free healthcare for pregnant women, normal delivery, cesarean delivery, and other EmONC services. Over the 2006–2015 period, the projected cumulative financing required was estimated at 31 billion West African CFA francs (CFAF), whereas the allocated amount was only 18 billion [34], resulting in a financing gap of 42% at the facilities level. However, the size of the real financial requirement was probably underestimated. As the FHCP led to an increase in the frequentation of healthcare facilities, there was a debate in the MoH and MoF regarding the adequate amount of staff remuneration to account for the extra work (overtime) and financing measures aimed at increasing health staff performance.
However, the problem was not only the shortfall in funding to compensate for the FHCP. The MoH [38] has highlighted the administrative difficulties encountered in absorbing the new aid specifically earmarked for the FHCP and the bureaucratic process implemented for compensating healthcare facilities for the removal of user fees.10
In addition, difficulties in the monitoring and evaluation process, as well as, in several facilities, irregularities in the behavior of healthcare staff, such as filing biased performance reports, perpetuating false information about free healthcare, and illegally charging user fees, have been observed by the MoH. These irregularities in behavior help explain how the actual effectiveness of the FHCP, while generally high, has been variable (80–100%) across regions and districts, as shown by studies on samples of households and health facilities.11
This combination of problems has led to severe constraints in terms of equipment and the stock replenishment of generic medicines, all of which damage the effectiveness and efficiency of healthcare structures and weaken quality of care.
Is the Current FHCP Sustainable?
A Selection of Indicators
With respect to the methodological framework presented, we considered a set of relevant indicators. We started from the cost of the five programs noted (children under 5 years, pregnant women, women with obstetric fistulas, precancerous cervical lesions for women aged 25–55 years, and breast cancer detection for women aged ≥ 15 years). The government has assessed the cost of the policy by making several assumptions regarding growth in healthcare demand and the associated productivity gains. The total cost of the FHCP for the 2018–2022 period is reported in Column C of Table 2; it includes the purchasing cost of services by the MoH (column A) and the cost of setting up support activities for implementing the strategy (column B).
Table 2.
Selection of indicators for assessing the sustainability of the free healthcare policy in Burkina Faso, 2018–2022
| Indicator | Cost of FHCP (CFAF billionsa) | Cost of support activities for implementation of the policyb (CFAF billionsa) | Total cost (CFAF billionsa) | % of MoH budget, external financing included | % of MoH budget—current expenditure only, average 2015–2016 | % of MoH budget, external financing excluded | % of external financing for healthcare | % of household payments included in MoH budget | % of total revenue and grants | % of tax revenue | % of total current expenditure | % overall deficit (cash basis)c |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | K | L | |
| 2018 | 28.87 | 1.46 | 30.33 | 10.3 | 29.2 | 15.2 | 14.1 | 131.9 | 1.4 | 2.0 | 2.3 | 7.9 |
| 2019 | 31.76 | 1.46 | 33.22 | 12.4 | 32.0 | 16.8 | 26.2 | 141.4 | 1.4 | 1.9 | 2.4 | 12.4 |
| 2020 | 34.93 | 1.46 | 36.39 | 14.5 | 35.1 | 16.8 | 82.7 | 151.6 | 1.5 | 2.0 | 2.3 | 12.4 |
| 2021 | 38.43 | 1.46 | 39.89 | 1.5 | 1.9 | 2.3 | 13.0 | |||||
| 2022 | 42.27 | 1.46 | 43.73 | |||||||||
| Total (CFAF billions) | 176.26 | 7.3 | 183.56 | |||||||||
| Total ($US millions)d | 333.59 | 13.82 | 347.41 | |||||||||
| Yearly average | 35.25 | 1.46 | 36.71 | |||||||||
| Yearly average ($US millions) | 66.72 | 2.76 | 69.48 |
Sources: Columns A, B, C: MoH [36]. Columns D–H: Calculated by the authors based on data provided by the MoH, January 2018. Columns I–L: Calculated by the authors based on data from IMF [32]
CFAF West African CFA francs, IMF International Monetary Fund, MoH Ministry of Health
aUnless otherwise indicated
bThe global figure for 2018–2022 has been divided by 5
cOverall deficit as % GDP: 2018, 4.5%; 2019 and 2020, 2.9%; 2021, 2.8% [32]
d$US1 = CFAF528.38
The total cost was compared with several aggregates to examine nine relevant indicators for a rapid assessment of the financial sustainability of the user fee reduction policy. The required financing has thus been calculated as a percentage of the following (the italicized figure indicates the number of the corresponding row in Table 1):
the MoH budget, including external financing (column D in Table 2)
MoH current expenditure, average 2015–2016 (column E)
MoH budget, without external financing (column F)
health aid (column G)
payments from households through the treasury and included in the MoH budget (column H)
the total revenues and grants in the consolidated operations of the central government12 (column I), 1
tax revenues in the consolidated operations of the central government (column J), 2
total current expenditures in the consolidated operations of the central government (column K), 4
the overall deficit cash basis (Column L); 10.
Table 3 shows the specific costs and indicators of the programs for pregnant women, for children under 5 years, and for the precancerous cervical lesion screening subprogram as a percentage of the MoH budget, total revenues and grants, tax revenues, total current expenditures, and the overall deficit (cash basis).
Table 3.
Selection of indicators for the programs included in Burkina Faso’s free healthcare policy and macro-economic context
| Indicator | 2018 | 2019 | 2020 |
|---|---|---|---|
| Pregnant womena (CFAF billions) | 7.18 | 7.67 | 8.17 |
| % of total free healthcare policy | 23.7 | 23.1 | 2.4 |
| % of MoH budget | 2.4 | 2.9 | 3.3 |
| % of total revenues and grants | 0.3 | 0.3 | 0.3 |
| % of tax revenues | 0.5 | 0.4 | 0.4 |
| % of current expenditures | 0.5 | 0.6 | 0.5 |
| % of overall deficit (cash basis) | 1.9 | 2.9 | 2.8 |
| Curative care for those aged < 5 yearsa (CFAF billions) | 12.48 | 12.88 | 13.30 |
| % of total free healthcare policy | 41.1 | 38.8 | 36.6 |
| % of MoH budget | 4.2 | 4.8 | 5.3 |
| % of total revenues and grants | 0.6 | 0.6 | 0.5 |
| % of tax revenues | 0.8 | 0.8 | 0.7 |
| % of current expenditures | 0.9 | 0.9 | 0.8 |
| % of overall deficit (cash basis) | 3.3 | 4.8 | 4.5 |
| Cost of screening for precancerous cervical lesionsb (CFAF billions) | 4.38 | 4.54 | 4.69 |
| % of total free healthcare policy | 14.5 | 13.7 | 12.9 |
| % of MoH budget | 1.5 | 1.7 | 1.9 |
| % of total revenues and grants | 0.2 | 0.2 | 0.2 |
| % of tax revenues | 0.3 | 0.3 | 0.3 |
| % of current expenditures | 0.3 | 0.3 | 0.3 |
| % of overall deficit (cash basis) | 1.1 | 1.7 | 1.6 |
Reading the table: The “pregnant women” program represents, in 2018, 23.7% of the total cost of the free healthcare policy, 2.4% of the MoH budget, etc
Sources: Authors. Data from MoH [36]. July 2017 for the cost of the free healthcare strategy; MoH budget, data provided by the MoH, January 2018; total revenues and grants, tax revenues, current expenditures, overall deficit: data from IMF [30]
CFAF West African CFA francs, IMF International Monetary Fund, MoH Ministry of Health
aCost of supporting activities excluded
Based on the available data, calculations were made for the years 2018–2020.
Results and Discussion
In what the results reveal, one must differentiate between what is specifically the responsibility of the MoH and what falls under the purview of the MoF, global fiscal policy, and other sectoral policies. The main conclusions are as follows.
-
The FHCP will impose a heavy burden on the MoH budget
- It will absorb 10% of the total projected MoH budget (current and investment expenditures) for 2018 and 15% for 2020. If external financing anticipated for the end of 2017 is excluded from the 2018–2021 period, the Ministry will have to allocate 15–17% of its own resources to the provision of free healthcare.13 These figures are not benchmarks, but they show that, compared with the situation with user fees, the policy adopted by the government requires financing an additional expenditure of 10–17% for the same quantity of health services delivered by facilities, all else being equal. This challenge leads to further questions since authorities anticipated a very large (optimistic) increase in the 2018 health budget (≈ 40%) compared with the 2012–2017 trend (Fig. 2).14
- Depending on the year, the cost of the FHCP will represent the equivalent of 30% of the MoH’s current average annual expenditure for 2015–2016.
- In 2020, the equivalent of more than 80% of external financing allocated to health will have to be earmarked for the FHCP.
- The FHCP will absorb a volume of resources equivalent to approximately one and a half times the payments made by households that will pass through the MoH’s budget.
There is no benchmark in these fields, but these figures suggest that constraints will be significant, and, in the current state of affairs, the opportunity cost of financing the FHCP will require strong political will and, undoubtedly, fairly delicate budget trade-offs within the MoH itself.
-
If the need for financing the FHCP is put in the context of the overall macroeconomic framework (columns I–L), the constraints seem smaller than those that emerge from the MoH budget. The resources needed for implementing the FHCP will require the government to allocate approximately 1% of total revenues and grants annually and approximately 2% of fiscal revenues. The required amounts correspond to slightly less than 2.5% of the country’s total current expenditures. Is this amount low or not? The answer is fundamentally a matter of choice and political feasibility based on the analysis of opportunity costs. In addition, without even mentioning expenditures for which there is no or little margin for maneuver in the very short term,15 increasing PHE is always de facto in competition with other sectors (education, etc.).
For the 2019–2021 period, the cost of the FHCP will contribute approximately 12–13% to the projected deficit. As we have seen, the government has planned to reduce it to 2.8% by 2020. Therefore, the government will have to find other resources, reduce non-health public spending, or accept a broader deficit target. This latter option is not to be recommended because it mechanically leads to an increase in domestic or external borrowing (in one form or another). However, as noted in Sect. 3.1.1, the risk of debt distress is low. While this point is true, the argument is hard to defend here because FHCP expenditures are recurrent expenditures. Additionally, they will remain recurrent as long as they have not been offset by an improvement in productivity or efficiency and by a substantial increase in insurance coverage, all of which are essential developments but will take several years. Consequently, the snowball effect on deficit will make domestic or external borrowing to finance the FHCP an extremely adventurous option.
Looking at the challenging picture that emerges from this set of results, we propose that another option for the government will be to consider reducing the coverage and content of the FHCP—reducing the eligible bundle of care—as their benefits are not currently subject to any socioeconomic condition in Burkina Faso. Table 3 presents the weight of the three major FHCP programs (free care for pregnant women, curative care for children under 5 years, and precancerous cervical lesion screening), placing each in relation to a selection of sustainability indicators. As an illustration, one can observe that, for example, in 2019 and 2020, free curative care for children aged < 5 years will absorb approximately 5% of the MoH budget and that the MoH will need to earmark 3% of its resources to the program covering pregnant women. Each of these two essential (in terms of SDGs) programs will absorb less than 1% of total fiscal revenues for the corresponding periods. In other words, adopting a temporal progressivity in the universality of user fee reduction programs can bring a double benefit: reducing the constraints for FHCP financial sustainability and lowering the risk of a worsening quality of care, which is crucial for the development of insurance coverage.
Fig. 2.
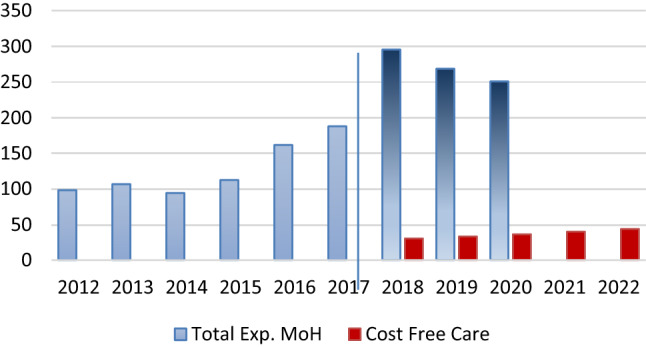
Projections for the Ministry of Health budget (CFAF billions) and free healthcare policy in Burkina Faso.
Sources of the data: Ministry of Health database, Burkina-Faso, 2018
Globally, this set of results suggests that a sustainable financing of the FHCP is not outside the range of possibility in Burkina Faso. However, it represents a very significant challenge in the sense that it will require budget trade-offs at the highest governmental levels. Without such trade-offs, it is likely that FHCP implementation will be chaotic or will have to be scaled down in its ambition, either in terms of the healthcare services covered or in imposing specific conditions on access to the services included in the FHCP.
Conclusion
Advocating for an FHCP means finding additional funding to substitute user fees. The purpose of this paper was to propose a methodological framework for a quick assessment to explore the different margins of maneuver that governments may have for ensuring the sustainable financing of these policies. The first part of this paper presented the various options to be considered. Since the need to find financing alternatives to user fees will mainly be based in the short and medium term on budgetary adjustments, particular attention has been paid to the issue of expanding fiscal space to sustainably finance the FHCP. In the second part of this paper, a brief case study of Burkina Faso was used to illustrate selected aspects of the proposed methodological framework. It shows that financing a sustainable FHCP is not outside the range of the government of Burkina Faso. However, fiscal space constraints will raise very serious challenges and trade-offs at the highest governmental levels, unless the government decides to opt for a gradual approach regarding targeted populations and the content of the package of benefits. This gradual approach would make it possible to progressively mobilize the potential of the complementary options available while reducing the risk of slippage in quality of care due to funding problems.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This article is based on a research report that was prepared and funded by the Health Care Financing in Sub-Saharan African Collaborative Research Program of the African Economic Research Consortium (AERC; http://www.aercafrica.org) with the support of the FERDI (Fondation pour les Etudes et Recherches sur le Développement International). The authors thank two anonymous referees and the participants of the AERC’s Final Review Workshop (31 May–1 June 2018) and two anonymous referees from this journal for their comments and suggestions. However, the authors are solely responsible for the analyses presented in this article.
Author contributions
JM is the main author for the development of the methodology and the writing of the article. Each co-author contributed to the drafting of the paper and to the reflections and analyses presented therein.
Compliance with Ethical Standards
Conflict of interest
Jacky Mathonnat, Martine Audibert, and Salam Belem have no conflicts of interest that are directly relevant to the content of this review/study.
Footnotes
How much will it cost? Where will the resources come from? What is the most appropriate scheme to make them available to stakeholders?
Notably, the aid directly dedicated to health is a much higher proportion of health expenditures in some countries. For example, in 2015, it accounted for 80% in Mozambique, approximately 57% in the Central African Republic and Burundi, and 40–50% in Congo, Ethiopia, Eritrea, Guinea, Guinea Bissau, Malawi, and Tanzania [23]. In some countries, user fee policies are largely donor driven.
For example, Ghana imposed an additional 2.5% value-added tax (VAT) that goes specifically to fund the National Health Insurance Scheme (NHIS) (it has expanded its fiscal space), but the government could have assigned it to another sector, such as education.
We do not address here the numerous issues that potentially arise from increasing tax revenues, aid, or public spending on health, with or without an increase in total public spending. Examples include issues of tax distortions and optimal taxation, taxation and growth, the effects of crowding out the private sector or not, changes in the relative price structure, differentiated evolutions in sectoral productivity (Baumol effects), and the effects of increased aid on growth. These issues are essential in the problematic expanding of fiscal space. They are highly debated, are often context dependent, and cannot be reduced to a handful of simple conclusions. However, they must be carefully considered because they can generate “negative” effects that will more than offset the expected health benefits of an expansion of fiscal space.
We assumed that there are no capital expenditures and no inflation (which does not alter the analysis).
Channeled through the treasury, from an extra-budgetary account, or going directly to an implementing entity such as a health center or NGO.
That is, currently $US686.
Burkina Faso is one of the few countries in sub-Saharan Africa to have been approaching the so-called Abuja indicator for several years.
First, for those aged < 5 years and pregnant women and, in 2010, for the entire population.
Delays in providing the MoF and donors with the information required for aid disbursement; cumbersome procedures for verifying the information provided by health facilities; slowness in the process of making funds available to health facilities (a matter of public financial management).
Presented at the workshop on free healthcare policy, Ouagadougou, 26 July 2017.
Consolidated operations of the central government are from the IMF, 2017 [32].
This would bring the share of PHE closer to the 15% Abuja “target.” However, despite its popularity, one must be very careful in interpreting this indicator, which is not intended to provide information on the sustainability or unsustainability of such a level of spending.
In nominal value; however, inflation will remain stable at 2%.
Mainly debt service and the civil servants' wage bill.
The original online version of this article was revised due to a retrospective Open Access order.
Change history
11/30/2020
.
References
- 1.WHO (2010) World health report, Geneva.
- 2.Akazili J, McIntyre D, Kanmiki EW, Gyapong J, Oduro A, Sankoh O, Ataguba JE. Assessing the catastrophic effects of out-of-pocket healthcare payments prior to the uptake of a nationwide health insurance scheme in Ghana. Glob Health Action. 2017;10(1):1289735. doi: 10.1080/16549716.2017.1289735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan J, Ahmed S, Evans TG. Catastrophic healthcare expenditure and poverty related to out-of-pocket payments for healthcare in Bangladesh—an estimation of financial risk protection of universal health coverage. Health Pol Plan. 2017;32(8):1102–1110. doi: 10.1093/heapol/czx048. [DOI] [PubMed] [Google Scholar]
- 4.Xu K, Evans DB, Kadama P, Nabyonga J, Ogwang Ogwal P, Nabukhonzo P, Aguilar AM. Understanding the impact of eliminating user fees: utilization and catastrophic health expenditures in Uganda. Soc Sci Med. 2006;62:866–876. doi: 10.1016/j.socscimed.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Qin VM, Hone T, Millett C, et al. The impact of user charges on health outcomes in low-income and middle-income countries: a systematic review. BMJ Global Health. 2019;3:e001087. doi: 10.1136/bmjgh-2018-001087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiysonge CS, Paulsen E, Lewin S, Ciapponi A, Herrera CA, Opiyo N, Pantoja T, Rada G, Oxman AD. Financial arrangements for health systems in low-income countries: an overviews of systematic reviews. Cochrane Data Base Syst Rev. 2017 doi: 10.1002/14651858.CD011084.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lagarde M, Palmer N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bull World Health Organ. 2008;86:839–847. doi: 10.2471/BLT.07.049197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen HT, Zombré D, Ridde V, De Allegri M. The impact of reducing and eliminating user fees on facility-based delivery: a controlled interrupted time series in Burkina Faso. Health Pol Plan. 2018;33(8):948–956. doi: 10.1093/heapol/czy077. [DOI] [PubMed] [Google Scholar]
- 9.Koné G, Audibert M, Lalou R, Lafarge H, Le Hesran J-Y. Subsidized antimalarial drugs in Dakar (Senegal): do the poor benefit? Études et Documents CERDI, ED 2017;11. halshs-01535112, version 1
- 10.Mladovsky P, Ba M. Removing user fees for health services: a multi-epistemological perspective on access inequities in Senegal. Soc Sci Med. 2017;188:91–99. doi: 10.1016/j.socscimed.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Pyone T, Smith H, van den Broek N. Implementation of the free maternity services policy and its implications for health system governance in Kenya. BMJ Glob Health. 2017 doi: 10.1136/bmjgh-2016-000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Witter S, et al. Cost and impact of policies to remove and reduce fees for obstetric care in Benin, Burkina Faso, Mali and Morocco. Int J Equity Health. 2016;15(1):123. doi: 10.1186/s12939-016-0412-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKinnon B, Harper S, Kaufman JS. Who benefits from removing user fees for facility-based delivery services? Evidence of socioeconomic differences from Ghana, Senegal, and Sierra Leone. Soc Sci Med. 2015;2(135):117–123. doi: 10.1016/j.socscimed.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Ridde V. From institutionalization of user fees to their abolition in West Africa: a story of pilot projects and public policies. BMC Health Serv Res. 2015;15(3):S6. doi: 10.1186/1472-6963-15-S3-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toure L. User fee exemption policies in Mali: sustainability jeopardized by the malfunctioning of the health system. BMC Health Serv Res. 2015;15(Suppl. 3):S8. doi: 10.1186/1472-6963-15-S3-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dzakpasu S, Powell-Jackson T, Campbell OM. Impact of user fees on maternal health service utilization and related health outcomes: a systematic review. Health Pol Plan. 2014;29(2):137–150. doi: 10.1093/heapol/czs142. [DOI] [PubMed] [Google Scholar]
- 17.Ridde V, Robert E, Meessen B. A literature review of the disruptive effects of user fee exemption policies on health systems. BMC Public Health. 2012;12:289.10. doi: 10.1186/1471-2458-12-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meessen B, Hercot D, Noirhomme M, Ridde V, Tibouti A, Tashobya C, et al. Removing user fees in the health sector: a review of policy processes in six sub-Saharan African countries. Health Pol Plan. 2011;26(2):ii16–ii29. doi: 10.1093/heapol/czr062. [DOI] [PubMed] [Google Scholar]
- 19.Walugembe D, Sibbald S, Le Ber M, Kothari A. Sustainability of public health interventions: where are the gaps? Health Res Pol Syst. 2019;17:8. doi: 10.1186/s12961-018-0405-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore JE, Mascarenhas A, Bain J, Straus SE. Developing a comprehensive definition of sustainability. Implement Sci. 2017;12(1):110. doi: 10.1186/s13012-017-0637-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Birch S, Murphy GT, MacKenzie A, Cumming J. In place of fear: aligning health care planning with system objectives to achieve financial sustainability. J Health Serv Res Pol. 2015;20(2):109–114. doi: 10.1177/1355819614562053. [DOI] [PubMed] [Google Scholar]
- 22.Liaropoulos L, Goranitis I. Health care financing and the sustainability of health systems. Int J Equity Health. 2015;14:80. doi: 10.1186/s12939-015-0208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO, Global expenditure data base. https://apps.who.int/nha/database
- 24.WHO-GTZ, SimIns health financing policy tool. https://www.who.int/health_financing/tools/simins/en/
- 25.Okungu V, Chuma J, McIntyre D. The cost of free health care for all Kenyans: assessing the financial sustainability of contributory and non-contributory financing mechanisms. Int J Equity Health. 2017;16:39. doi: 10.1186/s12939-017-0535-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heller P. Understanding the fiscal space, IMF Policy Discussion Paper, PDP 05/04. 2005.
- 27.Mathonnat J, Petitfour L, Tapsoba Y. 2017. Espace budgétaire pour la santé—mesure, évolution, déterminants, Report for WHO and Agence Française de Développement, p 107.
- 28.Mathonnat J, Audibert M. 2016. Fonds fiduciaires et programmes verticaux : quelles contributions aux politiques sectorielles? Revue de la littérature et exemple du secteur de la santé, Research Paper Serie 20, Agence Française de Développement, p 84.
- 29.Barroy H, Sparkes S, Dale E, Mathonnat J. Can low-and-middle income countries increase domestic fiscal space for health: a mixed-methods approach to assess possible sources of expansion. Health Syst Reform. 2018;4(2):1–13. doi: 10.1080/23288604.2018.1441620. [DOI] [PubMed] [Google Scholar]
- 30.Reich MR, Harris J, Ikegami N, Maeda A, Cashin C, Araujo EC, Takemi K, Evans TG. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387(10020):811–816. doi: 10.1016/S0140-6736(15)60002-2. [DOI] [PubMed] [Google Scholar]
- 31.Shan L, Wu Q, Liu C, Li Y, Cui Y, Liang Z, Hao Y, Liang L, Ning N, Ding D, Pan Q, Han L. Perceived challenges to achieving universal health coverage: a cross-sectional survey of social health insurance managers/administrators in China. BMJ Open. 2017;7(5):e014425. doi: 10.1136/bmjopen-2016-014425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.IMF. 2017. Burkina Faso: Seventh Review Under the Extended Credit Facility Arrangement, Staff Report, Country Report No. 17/222, July 18.
- 33.WHO Global Health Observatory. https://www.who.int/gho/en/
- 34.Ministère de la Santé Publique . Stratégie nationale de gratuité des soins chez la femme enceinte, des accouchements, de la césarienne, et des autres SONU. Ougadougou, Burkina Faso: Mimeo; 2016. [Google Scholar]
- 35.Ministère de la Santé Publique . Stratégie nationale d’exemption de paiement des soins curatifs pour les enfants de moins de 5 ans. Ougadougou, Burkina Faso: Mimeo; 2016. [Google Scholar]
- 36.Ministère de la Santé Publique . Stratégie nationale de gratuité du dépistage et de destruction des lésions précancéreuses du col de l’utérus et de l’examen clinique du sein. Ougadougou, Burkina Faso: Mimeo; 2016. [Google Scholar]
- 37.Ministère de la Santé Publique . Manuel d’éxécution des stratégies de gratuité au Burkina Faso. Ougadougou, Burkina Faso: Mimeo; 2016. [Google Scholar]
- 38.Ministère de la Santé publique . Politique nationale des mesures de gratuité des soins – Stratégie de mise en oeuvre 2018–2022. Ougadougou, Burkina Faso: Mimeo; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


