Abstract
Background and objective
Ultra rapid lispro (URLi) is a novel insulin lispro formulation developed to more closely match physiological insulin secretion and improve postprandial glucose control. This study compared the insulin lispro pharmacokinetics and glucodynamics, safety and tolerability of URLi and Humalog® after a single subcutaneous dose in patients with type 2 diabetes mellitus (T2DM).
Methods
This was a phase I, randomised, two-period, two-treatment, double-blind, crossover study in 38 patients with T2DM. At each dosing visit, patients received either 15 units of URLi or Humalog, followed by a 10 h automated euglycaemic clamp procedure. Serum insulin lispro and blood glucose were measured.
Results
Insulin lispro appeared in the serum 5 min faster (p < 0.0001) and exposure was 6.4-fold greater in the first 15 min (p < 0.0001) with URLi versus Humalog. Exposure beyond 3 h postdose was 26% lower and the duration of exposure was 51 min shorter with URLi versus Humalog. Onset of insulin action was 13 min faster (p < 0.0001) and insulin action was 4.2-fold greater within the first 30 min (p < 0.0001) with URLi versus Humalog. Insulin action beyond 4 h postdose was 20% lower (p = 0.0099) with URLi versus Humalog. Overall insulin lispro exposure and total glucose infused were similar for URLi and Humalog. Both treatments were well tolerated.
Conclusions
This is the first study to investigate URLi in patients with T2DM using a euglycaemic clamp procedure. URLi demonstrated ultra-rapid pharmacokinetics and glucodynamics in patients with T2DM.
ClinicalTrials.gov identifier:
Electronic supplementary material
The online version of this article (10.1007/s40262-020-00901-2) contains supplementary material, which is available to authorized users.
Key Points
| After an ultra rapid insulin lispro (URLi) injection, insulin appeared in the blood four times faster, and early insulin exposure increased up to six-fold, resulting in a greater early glucose-lowering effect with URLi. |
| Insulin also left the blood sooner after URLi, reducing the late glucose-lowering effect compared with Humalog; potentially reducing the occurrence of late hypoglycaemia observed with rapid-acting insulin analogues. |
| The ultra-rapid pharmacokinetic and glucodynamic profile of URLi has the potential to improve post-meal glucose control over current rapid-acting insulin analogues. |
Introduction
In the past three decades, innovations have contributed to the development of novel insulins that have improved glycaemic control in patients with type 2 diabetes mellitus (T2DM). Despite these improvements, there are still significant unmet needs. Current guidelines recommend that patients with T2DM who are receiving basal insulin therapy and are not maintaining glycaemic control, add bolus (prandial) insulin therapy [1, 2]. Although newer basal and prandial insulins have improved glycaemic control, many patients continue to struggle with achieving stable glycaemic control and often experience blood glucose peaks and lows. Even patients who achieve target glycated haemoglobin (HbA1c) levels may experience significant daily excursions in blood glucose levels [3]. Evidence suggests that glycaemic variability may contribute to increased morbidity and mortality, as well as reduced quality of life [4–6]. Thus, there is a need for prandial insulins that more closely match the actions of endogenous insulin and minimise blood glucose excursions.
Rapid-acting insulins, such as insulin lispro, aspart and glulisine, are absorbed more rapidly from subcutaneous (SC) tissue and have a faster onset of action compared with regular human insulin [7]. Although rapid-acting insulins are more effective at reducing postprandial glycaemic excursions in comparison with regular insulin, they may not be rapid enough to match carbohydrate absorption, limiting their efficacy in postprandial glycaemic control [7]. A faster-acting insulin preparation that matches carbohydrate absorption profiles and more closely matches physiological insulin release is needed.
Insulin lispro (Humalog®) is a commercially available, rapid-acting human insulin analogue indicated for the improvement of glycaemic control in adults and children with diabetes [8]. Ultra rapid lispro (URLi; LY900014) is a novel insulin lispro formulation utilising two locally acting excipients, treprostinil and citrate, with independent mechanisms of action that accelerate the absorption of insulin lispro. A microdose of treprostinil, a prostacyclin analogue [9], in the URLi formulation enhances insulin lispro absorption by local vasodilation [10]. Sodium citrate further enhances the absorption of insulin lispro by increasing local vascular permeability [11]. URLi was formulated to more closely match the secretion pattern of physiological prandial insulin and improve postprandial glucose (PPG) control. Initial disclosures of phase III results demonstrated superiority of URLi to Humalog in controlling PPG excursions in patients with type 1 or 2 diabetes [12, 13].
The objectives of this study were to compare the insulin lispro pharmacokinetics, glucodynamic (GD) characteristics during a euglycaemic clamp procedure, and the safety and tolerability of URLi and Humalog after a single 15-unit SC dose in patients with T2DM.
Materials and Methods
Study Design
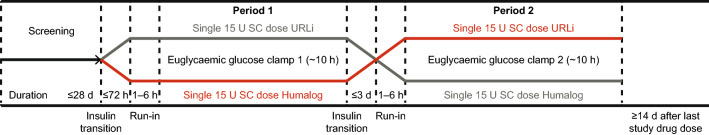
This was a phase I, randomised, two-period, two-treatment, double-blind, crossover glucose clamp study in patients with T2DM (Fig. 1). The study was conducted at one site (Profil, Neuss, Germany), from 16 October, 2017 to 14 December, 2017. The protocol was approved by an independent ethics committee. The study was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonisation guidelines for Good Clinical Practice, and applicable laws and regulations. All patients provided written informed consent before participating in the study. The study was registered at www.clinicaltrials.gov (NCT03305822).
Fig. 1.
Trial design. SC subcutaneous, U units, URLi ultra rapid lispro
Study Population
Male and female patients with T2DM (≥ 1-year duration) based on medical history, aged between 18 and 70 years and with a body mass index of 18.5–35.0 kg/m2 were eligible. Patients had HbA1c < 9.0%, fasting C-peptide ≤ 1.0 nmol/L, without any reports of severe hypoglycaemia over a period of 6 months before study enrolment, and were receiving stable prandial insulin ± basal insulin ± a stable dose of oral antidiabetic drugs. Patients receiving a continuous SC insulin infusion, daily insulin treatment ≥ 1.2 U/kg/body weight, insulin degludec or dulaglutide were excluded.
Treatment Protocol
Patients were randomised to receive a single 15-unit SC dose of the study drug (URLi or Humalog U100 formulations [Eli Lilly, Indianapolis, IN, USA]) in the first dosing period and the other study drug in the second dosing period (Fig. 1).
Each study period was separated by a wash-out period of at least 72 h. At any time in the 2 weeks before day − 1 of period 1, patients discontinued dipeptidyl peptidase-4 inhibitors, sulphonylureas and sodium-glucose co-transporter-2 inhibitors. Patients were not permitted to receive long-term systemic or inhaled glucocorticoids (> 14 consecutive days) during or within 4 weeks of commencing the study. Patients taking a stable dose of metformin were permitted to continue their medication during the study.
Before each dosing period, patients were to discontinue their basal insulin for a predefined treatment-specific wash-out period. The last injection of basal insulin was to occur no later than 72 h before dosing (insulin glargine U300), 48 h before dosing (insulin detemir or glargine U100) or 24 h before dosing (neutral protamine Hagedorn insulin, insulin mixtures or other intermediate-acting insulin). Any injection of more than 6 units of short-acting insulin was not to occur between 11 and 6 h before dosing and no injection was to occur less than 6 h before dosing.
Euglycaemic Clamp Procedure
At each dosing visit, patients underwent a 10 h, automated euglycaemic clamp procedure using the ClampArt® device (Profil, Neuss, Germany). Procedures were performed following an overnight fast of at least 8 h. Before study drug dosing, patients were connected to the clamp device for continuous glucose monitoring and the start of the baseline run-in period. A variable intravenous infusion of either glucose (20% dextrose solution) or insulin glulisine was started to reach a target blood glucose concentration of 100 mg/dL ± 20% (5.5 ± 1.1 mmol/L) during the run-in period. Blood glucose was maintained at 100 mg/dL ± 10% (5.5 ± 0.55 mmol/L) for the last 30 min before study drug injection, without any glucose infusion or insulin glulisine infusion. If stable blood glucose was not achieved, the run-in period was prolonged or study drug dosing was postponed. Baseline was defined as the mean of blood glucose concentrations at 6, 4 and 2 min before study drug administration and the onset of insulin action was defined as when the blood glucose concentration dropped by 5 mg/dL (0.3 mmol/L) from baseline.
Once the target blood glucose level was attained and remained stable, the patient received study treatment (URLi or Humalog; time = 0). After the onset of insulin action was reached, a variable intravenous glucose infusion rate (GIR) was initiated to maintain blood glucose at the target concentration (100 mg/dL; 5.5 mmol/L). The GIR necessary to maintain blood glucose at the target level was recorded every minute throughout the glucose clamp procedure. Blood samples were measured (SuperGL glucose analyser, Dr Müller; Hitado, Möhnesee, Germany) at least every 30 min during the clamp procedure to validate clamp glucose sensor measurements. The clamp procedure was continued for approximately 10 h postdose or until after blood glucose concentrations increased to > 200 mg/dL (11.1 mmol/L) without any glucose being administered for at least 30 min, whichever was earlier.
Bioanalysis Procedures
Serum free insulin lispro was analysed using a validated enzyme-linked immunosorbent assay specific to insulin lispro without cross-reactivity to endogenous insulin. Samples were collected at time 0, every 5 min for the first hour, at 70, 90, 120, 150 and 180 min, and hourly thereafter up to 10 h postdose. The lower limit of quantification (LLOQ) was 8.6 pmol/L. Inter-assay accuracy (% relative error) and inter-assay precision (% relative standard deviation) during validation were ≤ 16%.
Serum blood samples were collected at time 0, 30 min, and hourly after the first hour until completion of the clamp procedure for C-peptide and were analysed using a validated enzyme-linked immunosorbent assay. The LLOQ was 0.07 ng/mL. The inter-assay precision (% relative standard deviation) was < 8% and there was no cross-reactivity to insulin or proinsulin.
Outcome Measures
Free serum insulin lispro pharmacokinetic parameters were calculated by non-compartmental methods using Phoenix® version 6.4 and S PLUS® version 8.2. Early exposure endpoints included: time to early half-maximal drug concentration (early 50% tmax); area under the concentration–time curve (AUC) from 0 to 15 min (AUC0-15min), to 30 min (AUC0-30min), and onset of appearance, defined as the time that serum insulin lispro reached the LLOQ. The determination of onset of appearance used a linear interpolation between the time of dosing (0 concentration) and the time of the first quantifiable insulin lispro concentration and was only conducted in those patients where the predose sample was below the LLOQ. Late exposure endpoints included: time to late half-maximal drug concentration (late 50% tmax); AUC from time 3 to 10 h (AUC3-10h) and duration of exposure, defined as the time from dosing until serum insulin lispro reached the LLOQ. Overall exposure endpoints were AUC from time 0 to infinity (AUC0-∞) and maximum observed drug concentration (Cmax).
Glucodynamics were derived from the glucose clamp procedure, with GIR over time used as a measure of insulin effect. A locally weighted scatterplot smoothing (LOESS) function with a span of 0.1 was applied to all individual GIR-versus-time profiles in each treatment group and/or period. The fitted data for each patient were used to calculate the GD parameters, except for the time to onset of insulin action (Tonset), which was based on the raw GIR data. Glucodynamic analyses were conducted using Phoenix® version 6.4 or higher and S PLUS® version 8.2. Early insulin action endpoints were: Tonset, defined as the time when blood glucose drops by 0.3 mmol/L (5 mg/dL) from baseline, time to half-maximal GIR before time to maximum GIR (early 50% tRmax), and the total amount of glucose infused over the first 30 min (Gtot,0–30min) and the first 1 h (Gtot,0–1h). Late insulin action endpoints were: time to half-maximal GIR after time to maximum GIR (late 50% tRmax), total amount of glucose infused from 4 h to the end of the clamp (Gtot,4h–End), and duration of insulin action, defined as the time from Tonset to the first time when the GIR was less than the average LOESS GIR, which was calculated from all patients from 9 to 10 h after injection and remained below this value for at least 30 min. Total insulin action endpoints were maximum GIR (Rmax) and total amount of glucose infused over the duration of the clamp Gtot). Safety assessments included adverse events, injection-site assessments (immediately after dosing, and at 20 and 60 min), clinical laboratory assessments (predose period 1 and as deemed necessary), and vital signs and electrocardiograms (predose and end of the clamp procedure).
Statistical Analysis
At least 34 completers provided approximately 95% power to demonstrate a 40% increase in insulin lispro AUC0-30min between URLi and Humalog. Pharmacokinetic (PK) and GD analyses included all patients who completed both clamp procedures and had evaluable PK and GD data for both study periods. Log-transformed PK and GD parameters were evaluated using linear mixed models with treatment, sequence, and period as fixed effects and patient as a random effect; the treatment ratios of geometric least squares (LS) means were estimated from the model. The same model without log transformation was used to analyse the PK and GD time parameters. Least squares means, treatment differences in LS means and the corresponding 95% confidence intervals for the treatment differences were estimated from the model. For the GD analyses, the p value for the difference between LS means or the ratio of geometric LS means was used to determine statistical significance. The 95% confidence interval for the treatment ratio was estimated using Fieller’s theorem [14]. Statistical analyses were conducted using SAS® version 9.4, SAS Institute, Cary, NC, USA at a 5% significance level.
Results
Demographic and Baseline Characteristics
A total of 38 patients, 35 male and three female, were enrolled, randomised and completed the study (Table 1). The mean age was 60.0 years, mean duration of diabetes was 17.4 years and mean HbA1c was 7.4%.
Table 1.
Demographics and clinical characteristics
| Variable | Total (N = 38) |
|---|---|
| Mean age, years (SD) [range] | 60 (7.9) [38–70] |
| Sex, n (%) | |
| Male | 35 (92.1) |
| Female | 3 (7.9) |
| Mean BMI, kg/m2 (SD) [range] | 30.0 (2.97) [22.3–35.0] |
| Mean HbA1c, % (SD) [range] | 7.4 (0.80) [6.0–8.8] |
| Mean duration of T2DM, years (SD) [range] | 17.4 (7.7) [4.53–41.82] |
| Mean total daily insulin dose, U (SD) | 56.0 (25.9) |
| Previous insulin regimen, n (%) | |
| Basal/bolus | 32 (84.2) |
| Bolus only | 6 (15.8) |
| Previous insulin type, n (%) | |
| Basal | 32 (84.2) |
| Rapid acting | 29 (76.3) |
| Short acting | 9 (23.7) |
| Oral antidiabetic medications, n (%) | |
| Metformin | 15 (39.5) |
| SGLT-2 inhibitor | 3 (7.9) |
| DPP-4 inhibitor/metformin | 1 (2.6) |
BMI body mass index, DPP-4 dipeptidyl peptidase-4, HbA1c glycated haemoglobin, SD standard deviation, SGLT-2 sodium glucose cotransporter-2, T2DM type 2 diabetes mellitus, U units
Pharmacokinetics
Insulin Lispro Concentration Profiles
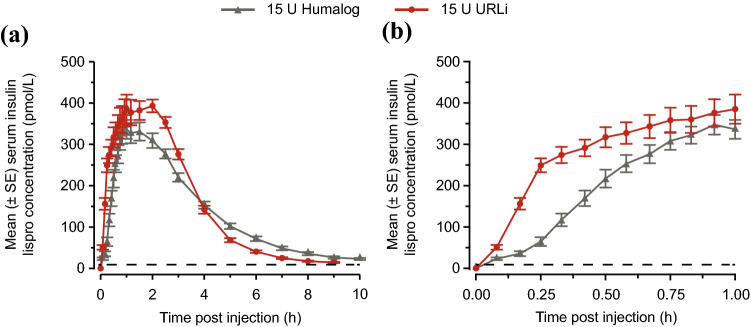
Mean serum insulin lispro concentration–time profiles following URLi were left shifted compared with those seen following Humalog (Fig. 2), demonstrating accelerated insulin lispro absorption, reduced late exposure and overall shorter exposure duration with URLi compared with Humalog.
Fig. 2.
Mean (± standard error [SE]) serum insulin lispro concentration–time profile for ultra rapid lispro (URLi) and Humalog. a Insulin lispro concentration–time profile 0–10 h after injection and b insulin lispro concentration–time profile 0–1 h after injection. The dashed line indicates the lower limit of quantification (LLOQ). U units
Early Insulin Lispro Exposure
Onset of insulin lispro appearance was 5 min faster for URLi compared with Humalog (2.0 vs. 7.3 min, p < 0.0001) and the early 50% tmax was 11 min earlier (18.6 vs. 29.6 min, p < 0.0001) with URLi versus Humalog (Table 2). This accelerated insulin lispro absorption with URLi led to significantly increased early serum insulin lispro exposure. The greatest difference in insulin lispro exposure was seen during the first 15 min after dosing, when exposure was 6.4-fold greater (p < 0.0001) with URLi compared with Humalog (Table 2). Early insulin lispro exposure during the first 30 min after dosing was also significantly greater for URLi compared with Humalog (Table 2).
Table 2.
Pharmacokinetics of insulin lispro
| Parameter | Treatment | N | Geometric LSM | Difference in LSM URLi–Humalog (95% CI) |
p value | Ratio of geometric LSM URLi:Humalog (95% CI) |
|---|---|---|---|---|---|---|
| Early insulin lispro exposure | ||||||
| Onset of appearancea, min | Humalog | 33b | 7.28 | − 5.31 (− 6.65 to − 3.98) | < 0.0001 | 0.271 (0.145–0.374 |
| URLi | 33b | 1.97 | ||||
| Early 50% tmaxa, min | Humalog | 38 | 29.6 | − 10.9 (− 15.2 to − 6.63) | < 0.0001 | 0.630 (0.518–0.758) |
| URLi | 38 | 18.6 | ||||
| AUC0–15min, pmol•h/L | Humalog | 37 | 3.84 | – | < 0.0001 | 6.38 (4.55–8.94) |
| URLi | 37 | 24.5 | ||||
| AUC0–30min, pmol•h/L | Humalog | 38 | 29.7 | – | < 0.0001 | 2.92 (2.27–3.76) |
| URLi | 38 | 86.6 | ||||
| Late insulin lispro exposure | ||||||
| Late 50% tmaxa, min | Humalog | 38 | 223 | − 14.3 (− 36.4 to 7.78) | 0.1974 | 0.936 (0.851–1.04) |
| URLi | 38 | 209 | ||||
| Durationa, min | Humalog | 18 | 559 | − 50.8 (− 93.5 to − 8.05) | 0.0220 | 0.909 (0.854–0.965) |
| URLi | 31 | 508 | ||||
| AUC3–10h, pmol•h/L | Humalog | 38 | 498 | – | < 0.0001 | 0.736 (0.643–0.844) |
| URLi | 38 | 367 | ||||
| Overall exposure | ||||||
| Cmax, pmol/L | Humalog | 38 | 370 | – | 0.0005 | 1.19 (1.09–1.31) |
| URLi | 38 | 441 | ||||
| AUC0–∞, pmol•h/L | Humalog | 38 | 1321 | – | 0.0676 | 1.05 (0.996–1.11) |
| URLi | 38 | 1387 | ||||
AUC area under the concentration–time curve, AUC0–∞ AUC from time 0 to infinity, AUC0–15min AUC from 0 to 15 min, AUC0–30min AUC from 0 to 30 min, AUC3–10h AUC from 3 to 10 h, CI confidence interval, Cmax maximum observed drug concentration, early 50% tmax time to early half-maximal drug concentration, late 50% tmax time to late half-maximal drug concentration, LSM least squares mean, URLi ultra rapid lispro
ap value is for the treatment difference in LSM. For all other parameters, the p value is for the ratio of geometric LSM
bFive patients had detectable insulin lispro concentrations at time 0 (predose) for both treatment periods and were excluded from the calculation of the onset of appearance
Late Insulin Lispro Exposure
Late insulin lispro exposure, from 3 to 10 h after dosing, was 26% lower (p < 0.0001) for URLi compared with Humalog (Table 2). Duration of insulin lispro exposure was significantly shorter by 51 min (508 vs. 559 min, p = 0.0220) for URLi compared with Humalog (Table 2).
Overall Insulin Lispro Exposure
Overall insulin lispro exposure (AUC0-∞) was similar between URLi and Humalog; however, Cmax was significantly greater for URLi than for Humalog (p < 0.001; Table 2).
Glucodynamics
Glucose Infusion Profiles
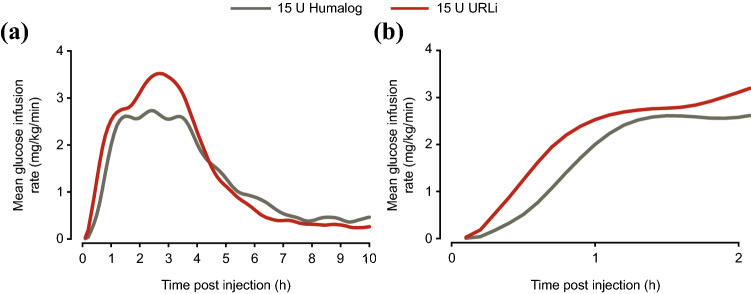
Mean GIR with URLi was also left shifted compared with Humalog (Fig. 3), indicating a faster onset of insulin action, and reduced late insulin action with URLi compared with Humalog. Importantly, the mean blood glucose concentration was maintained at the target of ~ 100 mg/dL throughout the procedure for both study drugs (Fig. S1 of the Electronic Supplementary Material [ESM]).
Fig. 3.
Mean locally weighted scatterplot smoothing (LOESS) fit of the glucose infusion rate over time for ultra rapid lispro (URLi) and Humalog. a Glucose infusion rate profile 0–10 h after injection and b glucose infusion rate profile 0–2 h after injection. U units
Early Insulin Action
The onset of insulin action was significantly sooner with URLi by 12.9 min (32.1 vs. 45.0 min, p < 0.0001; Table 3) compared with Humalog. The faster onset of insulin action of URLi increased the amount of glucose infused in the early part of the euglycaemic clamp procedure. The greatest difference between URLi and Humalog was seen during the first 30 min after dosing where there was a 4.2-fold increase in insulin action with URLi (p < 0.0001; Table 3). The amount of glucose infused was 1.75-fold greater for URLi compared with Humalog during the first hour after dosing (p < 0.0001), indicating a greater early glucose-lowering effect for URLi versus Humalog (Table 3). No significant difference was observed in early 50% tRmax.
Table 3.
Glucodynamics of ultra rapid lispro (URLi) and Humalog in patients who completed both treatment periods
| Parameter | Treatment | N | Geometric LSM | Difference in LSM URLi–Humalog (95% CI) |
p value | Ratio of geometric LSM URLi:Humalog (95% CI) |
|---|---|---|---|---|---|---|
| Early insulin action | ||||||
| Tonseta, min | Humalog | 37 | 44.99 | − 12.89 (− 18.67 to − 7.12) | < 0.0001 | 0.71 (0.62–0.82) |
| URLi | 37 | 32.10 | ||||
| Early 50% tRmaxa, min | Humalog | 36 | 55.94 | − 2.16 (− 11.69 to 7.37) | 0.6486 | 0.96 (0.80–1.14) |
| URLi | 36 | 53.78 | ||||
| Gtot,0–30mina, mg/kg | Humalog | 37 | 2.82 | 9.14 (5.02 to 13.25) | < 0.0001 | 4.24 (2.46–11.15) |
| URLi | 37 | 11.96 | ||||
| Gtot,0–1ha, mg/kg | Humalog | 37 | 41.95 | 31.39 (19.68 to 43.11) | < 0.0001 | 1.75 (1.42–2.33) |
| URLi | 37 | 73.35 | ||||
| Late insulin action | ||||||
| Duration of actiona, min | Humalog | 37 | 404.90 | − 18.38 (− 60.70 to 23.94) | 0.3840 | 0.95 (0.86–1.06) |
| URLi | 37 | 386.52 | ||||
| Late 50% tRmaxa, min | Humalog | 36 | 269.18 | − 23.62 (− 58.64 to 11.40) | 0.1795 | 0.91 (0.80–1.05) |
| URLi | 36 | 245.56 | ||||
| Gtot,4h–Enda, mg/kg | Humalog | 37 | 286.44 | − 55.90 (− 97.52 to − 14.27) | 0.0099 | 0.80 (0.68–0.94) |
| URLi | 37 | 230.54 | ||||
| Total insulin actionBlevins T, Zhang Q, Frias JP, Jinnouchi H, | ||||||
| Rmax, mg/kg/min | Humalog | 37 | 2.89 | – | 0.0008 | 1.27 (1.11–1.44) |
| URLi | 37 | 3.66 | ||||
| Gtot, mg/kg | Humalog | 37 | 670.26 | – | 0.0575 | 1.12 (1.00–1.26) |
| URLi | 37 | 750.27 | ||||
CI confidence interval, early 50% tRmax time to half-maximal glucose infusion rate before maximum glucose infusion rate, Gtot total amount of glucose infused over the duration of the clamp, Gtot,0–1h Gtot over 1 h, Gtot,0–30min Gtot over 30 min, Gtot,4h–End Gtot 4 h to end of clamp, late 50% tRmax time to half-maximal infusion rate after maximum glucose infusion rate, LSM least squares mean, Rmax maximum glucose infusion rate, Tonset time to onset of insulin action, tRmax time to maximum glucose infusion rate
ap value is for the treatment difference in LSM. For all other values, the p value is for the ratio of geometric LS mean
Late Insulin Action
Late insulin action, from 4 h after dosing, was significantly reduced by 20% with URLi compared with Humalog (p = 0.0099) (Table 3). Late 50% tRmax and duration of insulin action were not significantly different between treatments (Table 3).
Total Insulin Action
Total insulin action was similar between URLi and Humalog (p = 0.0575; Table 3). Rmax was significantly greater (p = 0.0008) for URLi compared with Humalog, mirroring the PK data (Table 3).
C-Peptide
The mean serum C-peptide profiles during the euglycaemic clamp procedure were similar following a 15-unit SC dose of URLi and Humalog (Fig. 4). Upon injection of the study drugs, the C-peptide concentrations reduced from baseline indicating a suppression by the exogenous insulins. The reduction in the C-peptide concentration in the first 2 h after the start of the clamp procedure was greater with URLi compared with Humalog, which aligns with the faster insulin action observed with LY900014. There was a rise above baseline in the C-peptide concentration with both treatments at 6 h after the start of the clamp procedure, which corresponds to the time when the insulin lispro concentration approached the LLOQ.
Fig. 4.
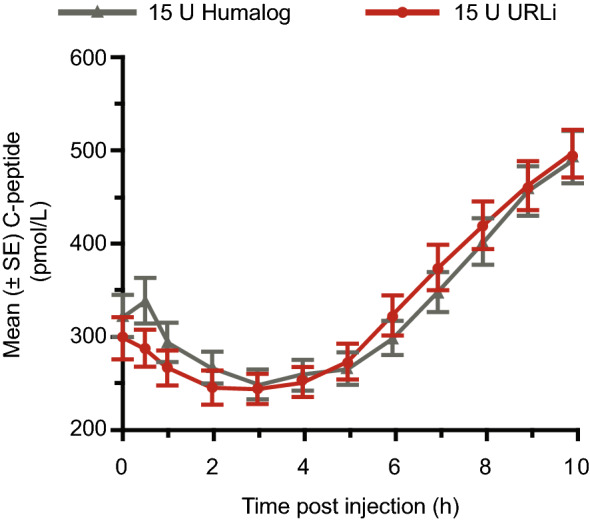
Mean (± standard error [SE]) C-peptide profiles following a single 15-unit (U) subcutaneous injection of ultra rapid lispro (URLi) or Humalog
Safety and Tolerability
URLi and Humalog were well tolerated and no unexpected safety signals were identified in the current study (Table 4). The frequency of treatment-emergent adverse events (TEAEs) following administration of Humalog or URLi was similar (eight vs. six events, respectively), with a total of 14 TEAEs in 11 patients (six vs. six). Most TEAEs were mild or moderate (seven and six, respectively) in severity and no patients discontinued because of TEAEs. One patient had a serious TEAE of coronary artery stenosis 13 days after Humalog administration in period 2, determined to be unrelated to the study drug. This patient had resumed their normal/pre-study insulin therapy when this serious TEAE occurred.
Table 4.
Treatment-emergent adverse events (TEAEs)
| TEAEs | URLi (N = 38) |
Humalog (N = 38) |
|
|---|---|---|---|
| Any TEAE, n (%) [events] | 6 (15.8) [6] | 6 (15.8) [8] | |
| Treatment-related TEAE | 1 (2.6) [1] | 0 | |
| SAE | 0 | 1 | |
| DCAE | 0 | 0 | |
| TEAEs occurring in ≥ 2 patients with any treatment, n (%) [events] | |||
| Headache | 2 (5.3) [2] | 2 (5.3) [2] | |
| Vessel puncture-site thrombosis | 2 (5.3) [2] | 0 | |
DCAE discontinuation due to adverse event, SAE serious adverse event, URLi ultra rapid lispro
The most common TEAEs that occurred in two or more patients with either treatment were headache and vessel puncture-site thrombosis. There was one report of very slight (barely perceptible) injection-site erythema following an URLi injection. There were no reports of hypoglycaemia during the period of clamp assessment. No clinically relevant changes in vital signs, electrocardiograms or laboratory values occurred during the study.
Discussion
This is the first study evaluating the PK and GD effects of URLi versus Humalog during a euglycaemic clamp procedure in patients with T2DM. The study demonstrated that URLi accelerated the absorption of insulin lispro, increased early exposure, reduced late exposure and had an overall shorter duration of exposure compared with Humalog. The study also demonstrated that URLi had a faster onset of insulin action, increased early insulin action and reduced late insulin action compared with Humalog. URLi was well tolerated with a similar safety profile to Humalog.
Insulin lispro was detectable in serum at 2 min after a SC injection of URLi, which was 5 min faster than following Humalog. This resulted in significantly greater early insulin lispro exposure with URLi compared with Humalog. Consistent with the PK profile, the onset of insulin action was significantly faster with URLi compared with Humalog, approximately 13 min earlier than with Humalog. This faster insulin action resulted in a greater early insulin action, 4.2-fold greater within the first 30 min with URLi compared with Humalog. The faster insulin action of URLi may better align with carbohydrate absorption and may improve PPG control compared with current rapid-acting insulins. Additionally, the faster absorption profile may reduce PPG excursions in patients that choose to dose their prandial insulin after meals.
Late exposure beyond 3 h after injection was reduced with URLi compared with Humalog and the duration of insulin exposure was reduced by 51 min. This reduction in duration of insulin exposure is likely underestimated as the data were calculated from those patients where the insulin lispro concentrations reached the LLOQ. The majority (31 of 38) of patients receiving URLi had insulin lispro concentrations that reached the LLOQ within the 10 h PK sampling period, while less than half of patients (18 of 38) receiving Humalog achieved insulin lispro concentrations below the LLOQ during the sampling period. This difference is reflective of a shorter insulin exposure duration of URLi compared with Humalog as each patient received a 15-unit dose of both treatments. Similar to the PK profile, late insulin action beyond 4 h postdose was reduced versus Humalog. Overall, insulin lispro exposure and total glucose infused were similar for URLi and Humalog, which suggests that no dose conversion is required when transitioning patients from Humalog to URLi. In support of this, the phase III study in patients with T2DM (PRONTO-T2D) initiated the dosing of URLi based on a unit-to-unit conversion from Humalog [13]. At the end of the 26-week treatment period, mean daily bolus dose was not statistically significantly different between groups.
The findings from this study in patients with T2DM are similar to a recently completed PK and GD euglycaemic clamp study conducted in patients with type 1 diabetes [15]. In patients with type 1 diabetes, URLi had an accelerated insulin lispro absorption compared with Humalog, resulting in a faster onset of insulin action and a greater early insulin action. Additionally, there was a reduction in late insulin lispro exposure, and an overall shorter exposure duration compared with Humalog in patients with type 1 diabetes. These changes in insulin lispro pharmacokinetics resulted in a reduced late insulin action and a shorter duration of insulin action, which was observed in both older and younger adults. In this study, we also see a reduction in both the late insulin lispro exposure and exposure duration, along with a reduced late insulin action in patients with T2DM. However, a significant treatment difference in duration of insulin action was not observed for patients with T2DM. This likely reflects the impact of endogenous insulin secretion in patients with T2DM, which makes it challenging to accurately estimate the true duration of insulin action during the clamp procedure as the GIR does not return to 0. The duration of the insulin action was estimated using mean GIR response for all patients from 9 to 10 h after injection when the insulin lispro concentration for both Humalog and URLi had approached the LLOQ.
However, this was a conservative approach given that the C-peptide concentration modestly rose above baseline around 8 h postdose, which reflects the slow loss of study drug-related insulin action and an increase in the secretion of endogenous insulin. This increase in endogenous insulin secretion coincides with the tapering off of insulin action, thereby confounding the true duration of insulin action. URLi does achieve a lower mean GIR than Humalog at 6.5 h postdose and maintains this for the remaining duration of the clamp procedure, suggesting a shorter duration of action is likely present if accurately defined for this population. This is aligned with the shorter exposure duration with URLi, which is not influenced by endogenous insulin because the assay is specific for insulin lispro. It is important to note that there is no standard procedure to correct GD parameters that could have been applied. C-peptide levels were similar between Humalog and URLi throughout the clamp procedure.
For many patients on insulin regimens, it remains challenging to coordinate premeal insulin injections with post-meal glucose responses. The first part of this challenge is related to the delay in absorption of exogenous insulin from SC tissues into the systemic circulation. URLi has been developed to reduce this delay by accelerating insulin absorption and more closely matching endogenous insulin secretion. The results of this study demonstrate that insulin lispro is absorbed more quickly with URLi compared with Humalog and that this results in earlier insulin action. These findings explain the improved postprandial glycaemic control reported for URLi compared with Humalog in the recently completed, phase III PRONTO-T2D study [13].
The second part of the challenge stems from extended postprandial exogenous insulin action. Late postprandial hypoglycaemia may occur when the duration of insulin action of exogenous insulin exceeds the duration of elevated blood glucose levels. Late insulin action was significantly reduced by URLi, which may help avoid late postprandial hypoglycaemia. URLi had a 27% lower hypoglycaemia rate (glucose level ≤ 70 mg/dL [3.9 mmol/L]) compared with Humalog in the period > 4 h postdose in the PRONTO-T2D study. The third part of this challenge relates to patient compliance with premeal insulin injection practices. Several surveys of patients with T2DM have suggested that premeal insulin injection rates are suboptimal and that many patients administer their bolus insulin injections after a meal [16, 17], potentially exacerbating delayed absorption of exogenous insulin and leading to late hypoglycaemic events. The accelerated absorption and faster insulin action of URLi compared with Humalog may offer benefits over standard of care if post-meal insulin dosing is required.
The strengths of the study include the crossover design, which allowed patients to act as their own control, and the washout step before treatment, which allowed the characterisation of only the test insulins. Importantly, the glucose and insulin glulisine infusions were terminated 30 min before dosing to avoid any carry over effect on the PK and GD responses. A limitation of the study is that, despite its status as the gold standard for assessing insulin action, the clamp method does not not provide a direct measure of the insulin on PPG.
Conclusions
This study demonstrated that URLi had an accelerated insulin lispro absorption, increased early exposure, reduced late exposure and an overall shorter exposure duration in comparison with Humalog. URLi displayed a faster onset of insulin action, increased early insulin action and a reduced late insulin action compared with Humalog. Overall, there was no difference in the overall insulin lispro exposure or amount of glucose infused between the two treatments. Furthermore, URLi was well tolerated with no differences in safety and tolerability observed between URLi and Humalog. The ultra-rapid PK and GD profile of URLi is likely to explain the greater PPG lowering observed in the phase III study in patients with T2DM [13].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank all study participants. Medical writing assistance was provided by Tania Dickson, PhD, CMPP and Linda Donnini, PhD, CMPP of ProScribe – Envision Pharma Group, and was funded by Eli Lilly and Company. ProScribe’s services complied with international guidelines for Good Publication Practice (GPP3).
Author contributions
All authors participated in the interpretation of the study results, and in the drafting, critical revision and approval of the final version of the manuscript. HL, GA, TH and JL were involved in the study design, HL, DC, GA, TH and JL were responsible for data collection and data analyses. HL was responsible for study monitoring and EL and JL were responsible for data analysis and plotting.
Compliance with Ethical Standards
Funding
This study was funded by Eli Lilly and Company.
Conflict of interest
Jennifer Leohr, Mary Anne Dellva, David E. Coutant, Elizabeth LaBell and Helle Linnebjerg are employees and shareholders of Eli Lilly and Company. Tim Heise has received consulting fees or honoraria from Mylan and Novo Nordisk. Additionally, research funds to Tim Heise’s institution were received from Adocia, Boehringer Ingelheim, Dance Pharmaceuticals, Eli Lilly and Company, Gan & Lee Pharmaceuticals, Johnson & Johnson, Mars, Medimmune, Mylan, Nordic Bioscience, Novo Nordisk, Pfizer, Poxel, Saniona, Sanofi, Wockhardt and Zealand Pharma. Time Heise, Grit Andersen, Eric Zijlstra, Lidia Hermanski and Leszek Nosek are employees of Profil. Additionally, Eric Ziljstra has received payments for lectures from Eli Lilly and Company, Novo Nordisk, Roche Diabetes Care and Aerami Therapeutics.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethik-Kommission der Ärztekammer Nordrhein, Düsseldorf, Germany) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Data Sharing
Eli Lilly and Company provides access to all individual participant data collected during the trial, after anonymisation, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and the European Union and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data-sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
References
- 1.Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycaemia in type 2 diabetes, 2018: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2018;61(12):2461–2498. doi: 10.1007/s00125-018-4729-5. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association, 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S90–102. [DOI] [PubMed]
- 3.Chon S, Lee YJ, Fraterrigo G, Pozzilli P, Choi MC, Kwon MK, et al. Evaluation of glycemic variability in well-controlled type 2 diabetes mellitus. Diabetes Technol Ther. 2013;15(6):455–460. doi: 10.1089/dia.2012.0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Umpierrez GE, Kovatchev BP. Glycemic variability: how to measure and its clinical implication for type 2 diabetes. Am J Med Sci. 2018;356(6):518–527. doi: 10.1016/j.amjms.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zinman B, Marso SP, Poulter NR, Emerson SS, Pieber TR, Pratley RE, et al. Day-to-day fasting glycaemic variability in DEVOTE: associations with severe hypoglycaemia and cardiovascular outcomes (DEVOTE 2) Diabetologia. 2018;61(1):48–57. doi: 10.1007/s00125-017-4423-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirsch IB. Glycemic variability and diabetes complications: does it matter? Of course it does! Diabetes Care. 2015;38(8):1610–1614. doi: 10.2337/dc14-2898. [DOI] [PubMed] [Google Scholar]
- 7.Heinemann L, Heise T, Wahl LC, Trautmann ME, Ampudia J, Starke AA, et al. Prandial glycaemia after a carbohydrate-rich meal in type I diabetic patients: using the rapid acting insulin analogue [Lys(B28), Pro(B29)] human insulin. Diabet Med. 1996;13(7):625–629. doi: 10.1002/(SICI)1096-9136(199607)13:7<625::AID-DIA134>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 8.Humalog [package insert]. Indianapolis (IN); Eli Lilly and Company; 2015.
- 9.Remodulin [package insert for US]. Research Triangle Park (NC); United Therapeutics Corporation; 2014.
- 10.Pratt E, Leohr J, Heilmann C, Johnson J, Landschulz W. Treprostinil causes local vasodilation, is well tolerated, and results in faster absorption of insulin lispro. Diabetes. 2017;66(Suppl. 1):A253. [Google Scholar]
- 11.Paavola CD, Cox AL, Sperry AE, Hansen RJ, Li S, Bradley SA, et al. A stable, hexameric, ultra-rapid insulin formulation containing citrate. Diabetes. 2017;66(Suppl. 1):A254. [Google Scholar]
- 12.Klaff LJ, Cao D, Dellva MA, Tobian J, Miura J, Dahl D, et al. Ultra rapid lispro (URLi) improves postprandial glucose (PPG) control vs. Humalog (Lispro) in T1D: PRONTO-T1D study. Diabetes. 2019;68(Suppl. 1):144-OR.
- 13.Blevins T, Zhang Q, Frias JP, Jinnouchi H, Chang AM. Randomized double-blind clinical trial comparing Ultra rapid lispro with Lispro in a basal-bolus regimen in patients with type 2 diabetes: PRONTO-T2D. Diabetes Care. 2020 (in press). [DOI] [PMC free article] [PubMed]
- 14.Chow S, Liu J. Design and analysis of bioavailability and bioequivalence studies. 3. Boca Raton, FL: Taylor and Francis Group, LLC; 2009. pp. 88–90. [Google Scholar]
- 15.Linneberg H, Zhang Q, LaBell ES, Dellva MA, Coutant DE, Hovelmann U, et al. Pharmacokinetics and glucodynamics of ultra rapid lispro (URLi) vs Humalog® (Lispro) in younger adults and elderly patients with type 1 diabetes: a randomized controlled trial. Clin Pharmacokinet. 2020 doi: 10.1007/s40262-020-00903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brod M, Nikolajsen A, Weatherall J, Pfeiffer KM. Understanding post-prandial hyperglycemia in patients with type 1 and type 2 diabetes: a web-based survey in Germany, the UK, and USA. Diabetes Ther. 2016;7(2):335–348. doi: 10.1007/s13300-016-0175-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schaper NC, Nikolajsen A, Sandberg A, Buchs S, Bogelund M. Timing of insulin injections, adherence, and glycemic control in a multinational sample of people with type 2 diabetes: a cross-sectional analysis. Diabetes Ther. 2017;8(6):1319–1329. doi: 10.1007/s13300-017-0317-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.