Abstract
Introduction:
The widespread outbreak of the novel SARS-CoV-2 has raised numerous questions about the origin and transmission of the virus. Knowledge about the mode of transmission as well as assessing the effectiveness of the preventive measures would aid in containing the outbreak of the coronavirus. Presently, respiratory droplets, physical contact and aerosols/air-borne have been reported as the modes of SARS-CoV-2 transmission of the virus. Besides, some of the other possible modes of transmission are being explored by the researchers, with some studies suggesting the viral spread through fecal-oral, conjunctival secretions, flatulence (farts), sexual and vertical transmission from mother to the fetus, and through asymptomatic carriers, etc.
Aim:
The primary objective was to review the present understanding and knowledge about the transmission of SARS-CoV-2 and also to suggest recommendations in containing and preventing the novel coronavirus.
Methods:
A review of possible modes of transmission of the novel SARS-CoV-2 was conducted based on the reports and articles available in PubMed and ScienceDirect.com that were searched using keywords, ‘transmission’, ‘modes of transmission’, ‘SARS-CoV-2’, ‘novel coronavirus’, and ‘COVID-19’. Articles referring to air-borne, conjunctiva, fecal-oral, maternal-fetal, flatulence (farts), and breast milk transmission were included, while the remaining were excluded.
Result and Conclusion:
The modes of transmission linked to SARS-CoV-2 were identified and the available literature on each of these is described in detail in view of the possibilities of viral transmission through various modes of transmission. The review provides updated and necessary information on the possible modes of transmission for the health care workers and the lay public under one umbrella that can also be considered during framing guidelines in order to prevent and control the viral spread.
Keywords: SARS-CoV-2, Transmission, Modes of transmission, Air-borne, Conjunctiva, Fecal-oral, Maternal-fetal, Flatulence (farts), Breast milk
Introduction
The end of 2019 saw emergence of a novel coronavirus from Wuhan, China, that in no time spread to the entire world. The novel coronavirus 2019-nCoV was officially named as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and the disease was termed as COVID-19 (Coronavirus disease 2019) by the International Committee on Taxonomy of Viruses on 11th February 2020 (1). SARS-CoV-2 is assumed to share its genetic sequence with the coronavirus that once resulted in an epidemic way back in 2002 and 2012 in the form of Severe Acute Respiratory Syndrome (i.e. SARS caused by SARS-CoV-1) and Middle East Respiratory Syndrome (i.e. MERS caused by MERS-CoV) respectively. On 11th March 2020, World Health Organization assessed the COVID-19 outbreak globally, and in view of the continuously increasing number of new cases, associated mortality, and absence of any specific treatment and vaccine, declared COVID-19 to be a global pandemic (2). Till July 16, 2020, a total of 13,517,846 confirmed coronavirus cases and 583,253 deaths with fatality rate of 4.31% have been reported globally (3). These numbers are continuously increasing with each passing second.
The Coronavirus genome is a single-strand ribonucleic acid virus that is enveloped, non-segmented and positive-sense with a size varying between 26 kb and 32 kb belonging to the subfamily Orthocoronavirinae of the family Coronaviridae, Order Nidovirales (4). There are mainly four genera of the subfamily, namely Alpha-coronavirus (α-CoV), Beta-coronavirus (β-CoV), Gamma-coronavirus (γ -CoV) and Delta-coronavirus (δ-CoV) (5,6). It is known that α-CoV and β-CoV genera infect mammals including humans and various animal species (swine, cattle, camels, cats, dogs, rodents, birds, bats, ferrets, civets, mink, snake, and other wildlife animals), while the other two, that is, δ- and γ -CoVs are known to infect birds. Existing knowledge revealed that this unusual coronavirus belongs to the B-lineage of the Beta-coronaviruses (7) and both SARS-CoV and MERS-CoV are zoonotic in origin basically originating from bats (8,9) with palm civets being an intermediate or a cross-host between bats and humans for the spread of SARS (10,11) and camels as a cross-host between bats and humans for spreading MERS (12,13). The existing literature indicate that 96.2% of the genetic sequence of bat coronavirus RaTG13 and 79.5% of the genetic sequence of SARS-CoV is identical to that of SARS-CoV-2 speculating bats to be the environmental host origin of this virus for further transmitting it to humans via unknown intermediate cross host (14).
The major clinical symptoms of the SARS-CoV-2 are influenza-like that comprise of fever, cough, headache, generalized myalgia, malaise, drowsy, diarrhea, confusion, dyspnea, pneumonia and rigorous shivering (15). The symptoms thus indicate that the viral infection likely contaminates and spreads primarily through respiratory tract from human to human via respiratory droplets, direct and indirect physical contact, aerosols or probably through digestive tract, urine, eyes and other routes (16).
The upsurge in the coronavirus cases indicates a multi-fold level growth in the transmission rate of the virus. Li et al. reported an R0 of approximately 2.2 signifying that on an average a single infected person is capable of spreading the infection to 2.2 new hosts (17); similarly, WHO has estimated an R0 between 1.4-2.5, where R0 is the expected number of new hosts produced by a single infected host in a completely vulnerable population without external interference (18). Rothe et al., in their research shows that asymptomatic carriers can still transmit virus during the incubation period (19). The incubation period and transmissibility routes of the virus thus become crucial to understand for controlling this escalation. Therefore, despite of all the speculations regarding the origin of the virus and its transmissibility routes, there are questions that remain unanswerable representing the likelihood of multiple routes of transmission (Figure 1). Thus, the widespread rise of this respiratory syndrome triggering COVID-19 has raised an alarm amongst various scientific and health sectors in order to prevent and limit the outburst for safeguarding the general public.
Figure 1:
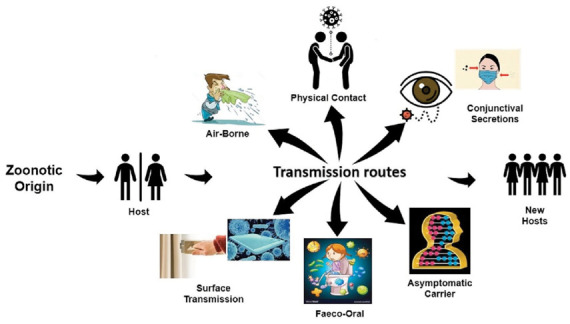
Diagrammatic representation of multiple routes of transmission of SARS-CoV-2
For the continuously changing facets of the pandemic, and the chaos regarding the various possibilities relating to the spread of the novel coronavirus, the present article is intended to review the existing literature on the various possible modes of transmission in the ongoing COVID-19 pandemic. The aim of the article is to review and highlight the existing literature on the possible modes of transmission; to develop an understanding about the cause and spread of SARS-CoV-2, and to suggest recommendations in containing and preventing the spread of novel coronavirus. A review of possible modes of transmission of the novel SARS-CoV-2 was conducted based on the reports and articles available in PubMed and ScienceDirect.com that were searched using keywords, ‘transmission’, ‘modes of transmission’, ‘SARS-CoV-2’, ‘novel coronavirus’, and ‘COVID-19’. Articles referring to air-borne, conjunctiva, fecal-oral, maternal-fetal, flatulence (farts), and breast milk transmission were included, while the remaining articles were excluded. We included scientific articles published in English as well as other languages for a comprehensive review of the topic in question. A total of 77 scientific papers were included in this review, which suggested several modes of transmission for COVID-19 and SARS-CoV-2.
Modes of Transmission
From the onset of the novel SARS-CoV-2 till date, real-time figures and information about the etymology, symptoms, transmission, morbidity, mortality and basic preventive measures of the COVID-19 has been the prime focus of the studies by various researchers and medical agencies in order to control and combat this epidemic. The well-established route of viral infection so far, is through respiratory droplets and contact with COVID-19 affected individuals (20). The possibility of its spread through other modes is continuously being explored. For the understanding of this novel virus transmission, general public are reliant on the scientific research being carried out and, in this scenario, a wrong interpretation of the etymology, symptoms and transmission may be damaging. Therefore, caution should be taken while outlining the inferences regarding the persistence and sustainability of the already known human coronaviruses to the novel SARS-CoV-2 (21). Pan et al., reported that viral RNA in the throat swab and sputum samples was maximum, at around 5-6 days after the commencement of the symptoms, and ranged from 104-107 copies per mL. The sputum samples showed higher levels of viral infection than the samples extracted from the throat (22).
Saliva
Angiotensin converting enzyme-II (ACE-II) is supposed to be the receptor for SARS-CoV and SARS-CoV-2. It is the viral binding enzyme found in abundance in the epithelial cells of the oral mucosa and can be transmitted through the saliva. Xu et al. have reported high expression of this receptor cells on the tongue (95.86%) than in the buccal and gingival tissues (23). The levels of ACE-II receptors infected by the SARS-CoV-2 sequence in the saliva showed a decline after being treated in the hospital. The presence of viral load or viral RNA on the epithelial cells does not necessarily mean that the cells are infected by the coronavirus. To et al., have suggested viral culture test to assess the presence of viral RNA in the saliva for possible transmission (24). Although saliva is presently seemed as an antagonist in combating against COVID-19, it is also apparent that it can be channelled as an associate in the detection of the virus (25).
Surface contact
One may limit person-to-person transmission of SARS-CoV-2, but it may still be transmitted to a new host through infected surfaces. This zoonotic virus has the capability of staying for longer durations on various surfaces making it contaminated for hours and days. Therefore, it can be transmitted via indirect contact with the surfaces or objects contaminated by the infected person. Also, the large viral droplets expired by the infected person may also get deposited on the surface in their close proximity. A study by Warnes et al. reveals that the human coronavirus 229E persists to stay infectious on common touch surface materials like polytetrafluoroethylene (Teflon; PTFE), polyvinylchloride (PVC), ceramic tiles, glass, silicone rubber, and stainless steel and are inefficient on a variety of copper alloys (26). The mechanism of transmission is similar to that followed by SARS and MERS, but with a difference in the persistence of virus on various surfaces such as clothes, utensils, furniture, cardboard, plastic door handles, seats, elevator buttons and surfaces etc. (27-29). Existing literature revealed that SARS-CoV-2 remains viable on plastic and stainless steel for a maximum of 72 hours, and eventually there is a decline in the virus stability and titer. Its stability on copper and cardboard was not shown to exceed after the contamination period of 4 hours and 24 hours respectively (30). While a study shows that on inanimate surfaces, another coronavirus strain (HCoV-229E) is capable to survive for up to nine days (31).
Aerosol and Airborne
Aerosols and airborne transmission may also be considered as the possible route of spread of SARS-CoV-2. The large-virus containing droplets are generated in the close environment to the infected person during sneezing, coughing or even talking, and these may get transferred to the uninfected persons. SARS-CoV-2 infected individuals may produce both droplets and aerosols on a uniform basis but most of these secretions may not infect other people; and at present, there are no perfect investigational data verifying or refuting droplet vs aerosol-based transmission (32). The size of the droplet plays a vital role in being a carrier of the virus. Droplet nuclei particles of <5μm diameter are considered to be the carriers as these can persist in the air for longer durations and can be transported to distances greater than 1 meter. A study conducted by van Doremalen et al., revealed that the infectious virus remained in the aerosols for approximately 3 hours with a gradual reduction from 103.5 to 102.7 TCID50 per litre of air under controlled conditions (30). It has been shown that the small droplets expired by an infected person that can travel a distance of 1-10 meters in the air (33). Wang et al., have reported a viral transmission rate through respired air by infected patients in a nosocomial environment as approximately 41.3% indicating an urgent need of consideration of the airborne passage of transmission (34). Despite of studies claiming SARS-CoV-2 virus RNA in air samples for up to 3 hours in one study (36) and 16 hours in another (35), the various agencies earlier, did not considered airborne route of transmission as a mode of spread except for the indoor confined environment. However, in an open letter to the WHO, 239 scientists in 32 countries summarized the evidence exhibiting that smaller particles can infect individuals (35). Therefore, in the latest update released on 29th June 2020, WHO stated that airborne mode of transmission of the coronavirus is likely to be spread and “cannot be ruled out” only after medical procedures that produce aerosols, or droplets smaller than 5 microns (37).
In addition, the SARS-CoV-2 could be possibly transmitted through airborne dust as it is believed that microorganisms in the airborne dust particles are associated to infectious diseases (38). Likewise, the worldwide air pollution and the particulate matters in the air could probably transmit the infectious virus. However, this aspect of viral diffusion is still not explored. In this regard, Qu et al., had suggested a critical requirement of investigations on the role of air pollution and other environmental factors in transmission of COVID-19 as these particulate matters are capable of transmitting the virus to long distances (39).
Fecal-oral
COVID-19 patients have shown gastrointestinal manifestations. Shedding of viral RNA or live infectious virus has been reported in the stools and fecal material of the infected patients. Positive presence of viral RNA in feces, on toilet seat and washbasin sink samples is suggestive of fecal-oral route as a probable route of transmission (40). Ong et al. in their research presented a distinct example of fecal-oral transmission by collecting bathroom samples from confirmed positive infected fecal by reverse transcription- polymerase chain reaction (RT-PCR) with no signs of diarrhea; found infected surface samples before sanitization and negative post-cleaning (41). Liu et al. analyzed the aerodynamics of SARS-CoV-2 in two Wuhan hospitals and detected lower concentration of viral RNA in aerosols in isolation wards and ventilated rooms of the patients, but showed raised levels in their toilet areas (42). Studies have revealed that the virus may remain live in the fecal samples for up to 4 days (43) and evidence supporting the possibility of a fecal-oral route of transmission of SARS-CoV-2 has also been accumulated (44). Negative post washing samples however, indicate that the sanitization measures were satisfactory.
In previous studies, other coronaviruses are found to retain their infectious nature in water and sewage for several days to weeks (45). Heller et al. also raised the need for an in-depth exploration to discover the role of water and sanitation in ceasing this mode of transmission. Viral RNA shedding in the digestive tract was found to stay for longer duration than in the respiratory system (46). Zhu et al. reported positive rectal swab test results despite of negative nasopharyngeal swab test among confirmed COVID-19 patients. That is, even after becoming asymptomatic and recovering from respiratory illness, 8 out of 10 pediatric patients continued to discharge the infectious viral RNA in feces displaying probable fecal-oral route of transmission (47). Similarly, the studies have reported presence of viral RNA in stools even after negative test results of the respiratory samples (48,49). The presence of virus in the rectal swab also explains the potential re-appearance of the disease.
It is evident from the case studies that rectal swab testing is more useful and accurate in diagnosing and determining the extent of viral RNA in the patients’ body and thus, should be used in estimating the duration of discharge from the hospital and termination of the quarantine period. However, the lack of evidence of viral replication in fecal swabs makes the fecal-oral route of transmission debatable. While the transmission dynamics of SARS-CoV-2 through gastrointestinal tract remains unidentified, it is believed that ACE-II mRNA receptor cells are also highly expressed in the gastrointestinal system. In a preliminary study, Xiao et al. strongly revealed the presence of SARS-CoV-2 viral RNA in the gastrointestinal tissue samples recovered from a COVID-19 patient (50). A few other studies have reported the presence of SARS-CoV-2 nucleic acid in the fecal material and rectal swabs of the infected children (48,51). Along-lasting retention period of viral nucleic acid has been shown in the stool sample (53).
Interestingly, it was observed in the Hong Kong population sample that 15.3% of patients with no gastrointestinal symptoms still discharged the viral RNA in their feces, whereas, patients with diarrhea had higher amount of viral load than with patients with no diarrhea. During the course of illness, 48.1% of patients showed viral shedding in the stool, while 70.3% of patients displayed prolonged shedding of viral RNA in feces (up to 33 days from the onset of illness) than in the nasopharyngeal samples (54).
A recent study has also suggested post-flush toilet plume to be a potential route of transmission through ‘aerosolized feces’. Another aspect of probable transmission could be through flatulence by infected patients, although no such published data has been found. But, according to several existing investigations, farts do have the tendency to carry micro-particles which have the capacity to spread bacteria (55). However, additional research is still warranted to estimate the intensity of such infections; presence of undergarments/ clothing would however, lower the risk of transmission through this passage. The same was claimed by the Chinese Centres of Disease Control and Prevention that pants do act as a hindrance in the transmission of disease via flatulence that contains the SARS-CoV-2 virus (56).
Live SARS-CoV-2 virus has also been demonstrated in the urine samples of the infected person (57) making it a potential source of virus transmission. Thus, the potential carriers of SARS-CoV-2 and the time points for which the infection stays onto them are described under Table 1.
Table 1:
Potential carriers of SARS-CoV-2 and the time points for which the infection stays onto them
| Potential carriers of SARS-CoV-2 | Duration (time points) of stay |
| Aerosols | Approximately 3 hours |
| Copper | Not more than 4 hours |
| Cardboard | Not more than 24 hours |
| Plastic | Up to 72 hours |
| Stainless steel | Up to 72 hours |
| Fecal sample | Up to 96 hours (4 days) |
Sexual Transmission
Another probable route of transmission could be through sexual intercourse. In a letter to the editor, Patri et al. have raised concern regarding the sexual route of transmission for SARS-CoV-2 virus (58). This supposition has mainly arrived after the reporting of fecal-oral transmission (59). It is assumed that certain sexual behaviors could even result in alternative ways of transmission by both direct or indirect exposure of oral-anal contact within few days after recovery since, the gastrointestinal tract may continue shedding the viral RNA (58).
In addition, SARS coronavirus has been known to cause impairment to multiple organs including inflammation of human testes/ orchitis. Coronaviruses are also known to cause defects in spermatogenesis (60). Since, SARS-CoV-2 shares the same receptor cell ACE-II as that of SARS-CoV-1, it raises the probability of infecting the human testes with the novel virus. Thus, indicating human testis to be a vulnerable organ to COVID-19 virus and suggesting reproductive behavior should be assessed in recovered COVID-19 male patients (61). Nevertheless, future studies should be focused to check whether the reproductive system is vulnerable to SARS-CoV-2 infection or not.
Maternal-to-neonate transmission
Another debatable factor that exists regarding the transmission of SARS-CoV-2 is the vertical transmission of virus from mother to the fetus or the neonate. Woo et al. reported higher levels of IgM antibodies (with sensitivity of IgM for SARS-CoV-2 reaching 70.2%) and abnormal amount of cytokine in a neonate born to a mother suffering from COVID-19. The tests conducted 2 hours after birth, revealed that the infection was transmitted to the neonate while in utero (62) and not through the placenta (63). In addition to this, a new-born’s laboratory reports revealed inflammation and liver injury indirectly supporting the probability of vertical transmissibility. Cao et al. presumes that a neonate born to a confirmed COVID-19 mother via vaginal delivery may cause perinatal infection (64), as transmission of infection during delivery via caesarean section was not found to be substantial among nine neonates born to confirmed COVID-19 mothers (65). A recent study also detected shedding of viral RNA in the breast milk of lactating mothers, but the sample size was small and therefore, further investigation with large sample size would be helpful in early detecting this particular mode of transmission (66). Although, previous literatures have reported poor pregnancy outcomes including maternal illness and fatality, vertical transmission of virus from mother to fetus and perinatal disease and mortality (67,68), cases suggestive of this mode of transmission are limited (65,66), and warrants further investigation into this arena.
Conjunctival secretions (eyes)
Conjunctival secretions are another possible mode of viral transmission; the infected droplets and body fluids (tear fluid) can infect the conjunctival epithelium (69). It is evident from the scientific studies that respiratory viruses have the power to induce ocular (visual) complications among infected patients leading to respiratory infections; thereby increasing the risk of transmission of SARS-CoV-2 through exposed mucous membranes of the unprotected eyes, mouth and nose (70,71). Conjunctival mucosa and respiratory tract are connected by the nasolacrimal duct and are share the same ACE-II receptor cell of SARS-CoV-2 (71,72). Lu et al. have raised the possibility of transmission through ocular surface (73). Till date, there is a single report of conjunctivitis along with the viral RNA in the tear body fluid. However, an absence of the virus in the patients’ conjunctival sac implicated an unusual route of transmission of SARS-CoV-2 (74). More research is suggested to develop a detailed understanding of the transmission mechanism through tear secretions and ocular surfaces.
Asymptomatic carriers
Another matter of concern in the transmission of COVID-19 is through asymptomatic carriers who are capable of transmitting the virus during the incubation period (75). A 10-year old boy in Wuhan reportedly behaved as an asymptomatic carrier of virus, showing lung infiltrates on CT scans (76). Similar route of transmission was also reported in a group of workers in Bavaria but it was later on disproved, yet the index patient confirmed the presence of mild symptoms during the course of transmission (19,77). It was also found that since asymptomatic carriage is common in other viral infections, but it is strikingly uncommon with SARS-CoV-2 and may be accompanied by underlying organ damage (78). Asymptomatic carriers may be one of the probable sources of SARS-CoV-2 infection, that poses a great challenge to control the infection; and further calling out for an immediate reassessment of transmission dynamics of the epidemic. It is difficult to identify the asymptomatic and pre-symptomatic patients of COVID-19. The frequency of fever in SARS-CoV-2 was found to be more (12.1%) than in case of SARS-CoV (1%) and MERS (2%) infection (79).
Recommendations based on existing information of COVID-19 pandemic
Considering the possibility of viral spread through the various described modes of transmission, following recommendations and certain preventive measures that might help in controlling this pandemic, have been detailed:
At the onset of the symptoms, one must visit the hospital for diagnosis immediately and should quarantine oneself for at least 21 days, since the virus can retain in the digestive tract and can be transmitted through fecal-oral route. Therefore, before discharging from the hospital, a second check on the respiratory as well as fecal specimens must be assessed until negative shedding of the RNA virus in stool is obtained.
Since, WHO has also acknowledged the air-borne transmission of coronavirus, infected persons must wear masks indoors as well as outdoors, even in physically distant settings to control further spread of the virus. Previous studies have suggested that usage of high-flow nasal cannula (HFNC) and non-invasive ventilation (NIV) via specific masks with improved and adjustable vent holes may reduce the chance of airborne transmission.
Avoiding public transportation as much as possible and opting for private vehicles and ambulances with open windows for ventilation. The vehicles must be disinfected with chlorine containing disinfectant or should be sanitized properly prior to the usage.
Considering the spread of coronavirus to be airborne, especially in crowded spaces with poor ventilation, the consequences for containment will be significant. Therefore, one must shun recirculation of the probable ‘infected air’ in the same environment.
To control the spread through asymptomatic carriers of the virus, an early stage investigation of the individuals via surveillance as done in the case of ‘GPEI — Global Polio Eradication Initiative’ should be administered. Therefore, small cohort groups in schools, offices, or communities should be performed. This might help in early recognition of the attack rate and transmission routes for forecasting the development and containment of the virus.
Viral shedding studies at household levels must be followed to determine the maximum intensity of the patient to transmit the virus via fecal-oral route and the extent of isolation they should be kept for. To avoid outbreak of the virus at household level, where a single toilet is available, one must close the lid of the toilet seat when flushing to limit the spread of fecal-aerosol.
In view of the fact that, various routes of transmission are being reportedly linked to the spread of virus, numerous site testing such as molecular and serological tests of the specimens is suggested which may enhance the sensitivity, and confirm a virus carrier.
Usage of gloves along with masks and goggles must also be incorporated while using ATM machines or similar public amenities as the virus can be transmitted easily and rapidly in a close knitted environment.
Food items and packets must be kept aside for at least 48 hours, and should be washed properly with running water before its usage.
Conclusions
To recapitulate, on the basis of studies and medical researches, respiratory droplets and physical contact are being considered as the primary source of transmission of SARS-CoV-2, but other possible aspects of virus transmission, that is, spread through air, conjunctival secretions, asymptomatic carriers, fecal-oral routes, vertical transmission as well as sexual transmission must not be ignored and needs a serious consideration before it is too late. Thus, acknowledging the frequency rate by which these numerous modes of transmission are being recognized, they require an urgent call for an action plan at an individual as well as the governmental levels. If established, these could aid in public health sector for planning pandemic control strategies such as investigating the role of particulate matters as a vector for virus in air, wastewater and open defecation along with a check on the reproductive behavior of the infected and recently recovered patients to lower the risk of coronavirus spread. Self-isolation and quarantining of the suspected and infected individuals must be continued for up to 21 days or more so as to gradually achieve an R0 value of zero. Since, coronaviruses attack the ACE-II for virus binding, therefore, future studies must be directed in viral-specific target cells and organs to have a prior knowledge in fighting against such novel viruses.
Acknowledgements:
Kewal Krishan is supported by a DST PURSE grant and UGC Centre of Advanced Study (CAS-II) awarded to the Department of Anthropology, Panjab University, Chandigarh, India.
Authorship Credit Statement: Richa Mukhra:
Writing - original draft, Writing - review & editing, Final approval. Kewal Krishan: Conceptualization, Writing - review & editing, final approval and supervising the work. Tanuj Kanchan: Writing - review & editing, final approval and supervising the work.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. World Health Organization. 2020 Feb Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it . Accessed July 17, 2020. [Google Scholar]
- 2.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020. Geneva, Switzerland. 2020 Mar. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 . Accessed July 17, 2020. [Google Scholar]
- 3.World Health Organization. Coronavirus (COVID-19). World Health Organization. 2020 Available from: https://covid19.who.int/ . Accessed July 17, 2020. [Google Scholar]
- 4.Weiss SR, Leibowitz JL. Coronavirus pathogenesis. In Advances in virus research 2011 Jan 1 (Vol. 81, pp. 85-164) Academic Press. doi: 10.1016/B978-0-12-385885-6.00009-2. https://doi.org/10.1016/B978-0-12-385885-6.00009-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang D, Leibowitz JL. The structure and functions of coronavirus genomic 3′ and 5′ ends. Virus Res. 2015;206:120–133. doi: 10.1016/j.virusres.2015.02.025. https://doi.org/10.1016/j.virusres.2015.02.025 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banerjee A, Kulcsar K, Misra V, et al. Bats and coronaviruses. Viruses. 2019;11(1):41. doi: 10.3390/v11010041. https://doi.org/10.3390/v11010041 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS) World Health Organization. 2003 https://apps.who.int/iris/handle/10665/70863 . [Google Scholar]
- 8.Alanagreh L, Alzoughool F, Atoum M. The Human Coronavirus Disease COVID-19: Its Origin, Characteristics, and Insights into Potential Drugs and Its Mechanisms. Pathogens. 2020;9:331. doi: 10.3390/pathogens9050331. https://doi:10.3390/pathogens9050331 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lau SK, Li KS, Huang Y, et al. Ecoepidemiology and complete genome comparison of different strains of severe acute respiratory syndrome-related Rhinolophus bat coronavirus in China reveal bats as a reservoir for acute, self-limiting infection that allows recombination events. J Virol. 2010;84(6):2808–2819. doi: 10.1128/JVI.02219-09. https://doi.org/10.1128/jvi.02219-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chinese SARS Molecular Epidemiology Consortium. Molecular evolution of the SARS coronavirus during the course of the SARS epidemic in China. Science. 2004;303(5664):1666–1669. doi: 10.1126/science.1092002. https://doi.org/10.1126/science.1092002. [DOI] [PubMed] [Google Scholar]
- 11.Wang LF, Eaton BT. Bats, civets and the emergence of SARS. Curr Top Microbiol Immunol. 2007;315:325–344. doi: 10.1007/978-3-540-70962-6_13. https://doi.org/10.1007/978-3-540-70962-6_13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Müller MA, Corman VM, Jores J, et al. MERS coronavirus neutralizing antibodies in camels, Eastern Africa, 1983-1997. Emerg Infect Dis. 2014;20(12):2093. doi: 10.3201/eid2012.141026. https://doi.org/10.3201/eid2012.141026 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chu DK, Poon LL, Gomaa MM, et al. MERS coronaviruses in dromedary camels, Egypt. Emerg Infect Dis. 2014;20(6):1049. doi: 10.3201/eid2006.140299. https://doi.org/10.3201/eid2006.140299 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil Med Res. 2020;7(1):1–10. doi: 10.1186/s40779-020-00240-0. https://doi.org/10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. SARS (Severe Acute Respiratory Syndrome) World Health Organization. 2020 Available from: https://www.who.int/ith/diseases/sars/en/ . Accessed July 11, 2020. [Google Scholar]
- 16.World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. World Health Organization. 2020 https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations . (Accessed July 13, 2020) [Google Scholar]
- 17.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. https://doi.org/10.1056/NEJMoa2001316 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phan LT, Nguyen TV, Luong QC, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382:872–874. doi: 10.1056/NEJMc2001272. https://doi.org/10.1056/NEJMc2001272 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-NCOV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. https://doi.org/10.1056/NEJMc2001468 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Signorelli C, Odone A, Riccò M, Bellini L, Croci R, Oradini-Alacreu A, Fiacchini D, Burioni R. Major sports events and the transmission of SARS-CoV-2: analysis of seven case-studies in Europe. Acta Bio Med [Internet] 2020 May 11 [cited 2020 Jul.14];91(2):242–4. doi: 10.23750/abm.v91i2.9699. Available from: https://www.mattioli1885journals.com/index.php/actabiomedica/article/view/9699 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krishan K, Kanchan T. Aerosol and surface persistence: Novel SARS-CoV-2 versus other coronaviruses. J Infec Dev Contri [In Press] 2020 doi: 10.3855/jidc.12887. [DOI] [PubMed] [Google Scholar]
- 22.Pan Y, Zhang D, Yang P, et al. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020;20:411–412. doi: 10.1016/S1473-3099(20)30113-4. https://doi.org/10.1016/S1473-3099(20)30113-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:1–5. doi: 10.1038/s41368-020-0074-x. https://doi.org/10.1038/s41368-020-0074-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.To KKW, Tsang OTY, Chik-Yan Yip C, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020:4–6. doi: 10.1093/cid/ciaa149. https://doi.org/10.1093/cid/ciaa149 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Han P, Ivanovski S. Saliva-Friend and Foe in the COVID-19 Outbreak. Diagnostics (Basel) 2020;10(5):290. doi: 10.3390/diagnostics10050290. https://doi.org/10.3390/diagnostics10050290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Warnes SL, Little ZR, Keevil CW. Human coronavirus 229E remains infectious on common touch surface materials. MBio. 2015;6:1–10. doi: 10.1128/mBio.01697-15. https://doi.org/10.1128/mBio.01697-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dowell SF, Simmerman JM, Erdman DD, et al. Severe Acute Respiratory Syndrome Coronavirus on Hospital Surfaces. Clin Infect Dis. 2004;39:652–657. doi: 10.1086/422652. https://doi.org/10.1086/422652 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Booth TF, Kournikakis B, Bastien N, et al. Detection of Airborne Severe Acute Respiratory Syndrome (SARS) Coronavirus and Environmental Contamination in SARS Outbreak Units. J Infect Dis. 2005;191:1472–1477. doi: 10.1086/429634. https://doi.org/10.1086/429634 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chinese Preventive Medicine Association. New Group of Experts on the prevention and control of Chinese Preventive Medicine Association coronavirus pneumonia. The latest understanding of the epidemiological characteristics of pneumonia novel coronavirus. [Article in Chinese] Chin J Epidemiol. 2020;41:139–144. https://doi.org/10.3760/cma.j.issn.0254-6450.2020.02.002 . [Google Scholar]
- 30.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. https://doi.org/10.1056/NEJMc2004973 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carraturo F, Del Giudice C, Morelli M, et al. Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. Environ Pollut. 2020 doi: 10.1016/j.envpol.2020.115010. 115010. https://doi.org/10.1016/j.envpol.2020.115010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klompas M, Baker MA, Rhee C. Airborne Transmission of SARS-CoV-2: Theoretical Considerations and Available Evidence. JAMA. 2020 doi: 10.1001/jama.2020.12458. https://doi.org/10.1001/jama.2020.12458 . [DOI] [PubMed] [Google Scholar]
- 33.Morawska L, Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ Int. 2020;139 doi: 10.1016/j.envint.2020.105730. 105730. https://doi.org/10.1016/j.envint.2020.105730 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. https://doi.org/10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fears AC, Klimstra WB, Duprex P, et al. Persistence of Severe Acute Respiratory Syndrome Coronavirus 2 in Aerosol Suspensions. Emerg Infect Dis. 2020;26(9) doi: 10.3201/eid2609.201806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morawska L, Milton DK. It is Time to Address Airborne Transmission of COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa939. ciaa939. https://doi.org/10.1093/cid/ciaa939 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organisation. Transmission of SARS-CoV-2: implications for infection prevention precautions. World Health Organisation. 2020 Available from: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions. (Accessed July 13, 2020) [Google Scholar]
- 38.Yu ITS, Li Y, Wong TW, et al. Evidence of Airborne Transmission of the Severe Acute Respiratory Syndrome Virus. N Engl J Med. 2004;350:1731–1739. doi: 10.1056/NEJMoa032867. https://doi.org/10.1056/NEJMoa032867 . [DOI] [PubMed] [Google Scholar]
- 39.Qu G, Li X, Hu L, et al. An Imperative Need for Research on the Role of Environmental Factors in Transmission of Novel Coronavirus (COVID-19) Environ Sci Technol. 2020;54(7):3730–3732. doi: 10.1021/acs.est.0c01102. https://doi.org/10.1021/acs.est.0c01102. [DOI] [PubMed] [Google Scholar]
- 40.Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic Features and Clinical Course of Patients Infected with SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488–1494. doi: 10.1001/jama.2020.3204. https://doi.org/10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) from a Symptomatic Patient. JAMA. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. https://doi.org/10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Y, Ning Z, Chen Y, et al. Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak. bioRxiv. 2020 982637 https://doi.org/10.1101/2020.03.08.982637 . [Google Scholar]
- 43.Weber DJ, Rutala WA, Fischer WA, et al. Emerging infectious diseases: Focus on infection control issues for novel coronaviruses (Severe Acute Respiratory Syndrome-CoV and Middle East Respiratory Syndrome-CoV), hemorrhagic fever viruses (Lassa and Ebola), and highly pathogenic avian influenza viruses, A(H5N1) and A(H7N9) Am J Infect Control. 2016;44:E91–E100. doi: 10.1016/j.ajic.2015.11.018. https://doi.org/10.1016/j.ajic.2015.11.018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Amirian ES. Potential fecal transmission of SARS-CoV-2: current evidence and implications for public health. Int J Infect Dis. 2020 Apr 23 doi: 10.1016/j.ijid.2020.04.057. https://doi.org/10.1016/j.ijid.2020.04.057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Casanova L, Rutala WA, Weber DJ, et al. Survival of surrogate coronaviruses in water. Water Res. 2009;43:1893–1898. doi: 10.1016/j.watres.2009.02.002. https://doi.org/10.1016/j.watres.2009.02.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heller L, Mota CR, Greco DB. Science of the Total Environment COVID-19 faecal-oral transmission : Are we asking the right questions. Sci Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138919. 138919. https://doi.org/10.1016/j.scitotenv.2020.138919 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhu Z, Liu Y, Xu L, et al. Extra-pulmonary viral shedding in H7N9 Avian Influenza patients. J Clin Virol. 2015;69:30–32. doi: 10.1016/j.jcv.2015.05.013. https://doi.org/10.1016/j.jcv.2015.05.013 . [DOI] [PubMed] [Google Scholar]
- 48.Xu Y, Li X, Zhu B, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502–505. doi: 10.1038/s41591-020-0817-4. https://doi.org/10.1038/s41591-020-0817-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen Y, Chen L, Deng Q, et al. The Presence of SARS-CoV-2 RNA in Feces of COVID-19 Patients. J Med Virol. 2020 doi: 10.1002/jmv.25825. 10.1002/jmv.25825. https://doi.org/10.1002/jmv.25825 . [DOI] [PubMed] [Google Scholar]
- 50.Xiao F, Tang M, Zheng X, et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831–1833.e3. doi: 10.1053/j.gastro.2020.02.055. https://doi.org/10.1053/j.gastro.2020.02.055 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. https://doi.org/10.1056/NEJMoa2001191 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang T, Cui X, Zhao X, et al. Detectable SARS-CoV-2 Viral RNA in Feces of Three Children during Recovery Period of COVID-19 Pneumonia. J Med Virol. 2020 doi: 10.1002/jmv.25795. 10.1002/jmv.25795. https://doi.org/10.1002/jmv.25795 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu Y, Guo C, Tang L, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. The Lancet Gastroenterol Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. https://doi.org/10.1016/S2468-1253(20)30083-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cheung KS, Hung IF, Chan PP, et al. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples from the Hong Kong Cohort and Systematic Review and Meta-analysis. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.065. S0016-5085(20)30448-0. https://doi.org/10.1053/j.gastro.2020.03.065 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DNA Web Team. Coronavirus spreading through farts? Here is what experts say. 2020 Available from: https://www.dnaindia.com/world/photo-gallery-coronavirus-spreading-through-farts-here-is-what-experts-say-2821809 . Accessed July 11, 2020. [Google Scholar]
- 56.Global Times. Do farts spread novel coronavirus? A Beijing district CDC answers. 2020. https://www.globaltimes.cn/content/1180514.shtml. Accessed July 11, 2020. [Google Scholar]
- 57.Naicker S, Yang CW, Hwang SJ, et al. The Novel Coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97:824–828. doi: 10.1016/j.kint.2020.03.001. https://doi.org/10.1016/j.kint.2020.03.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patrì A, Gallo L, Guarino M, et al. Sexual transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): A new possible route of infection. J Am Acad Dermatol. 2020;82(6):e227. doi: 10.1016/j.jaad.2020.03.098. https://doi.org/10.1016/j.jaad.2020.03.098 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi: 10.1038/s41368-020-0075-9. https://doi.org/10.1038/s41368-020-0075-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu J, Qi L, Chi X, et al. Orchitis: A Complication of Severe Acute Respiratory Syndrome (SARS) Biol Reprod. 2006;74:410–416. doi: 10.1095/biolreprod.105.044776. https://doi.org/10.1095/biolreprod.105.044776 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang Z, Xu X. scRNA-seq Profiling of Human Testes Reveals the Presence of the ACE2 Receptor, A Target for SARS-CoV-2 Infection in Spermatogonia, Leydig and Sertoli Cells. Cells. 2020;9:920. doi: 10.3390/cells9040920. https://doi.org/10.3390/cells9040920 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dong L, Tian J, He S, et al. Possible Vertical Transmission of SARS-CoV-2 from an Infected Mother to Her Newborn. JAMA. 2020;323(18):1846–1848. doi: 10.1001/jama.2020.4621. https://doi.org/10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Woo PCY, Lau SKP, Wong BHL, et al. Detection of Specific Antibodies to Severe Acute Respiratory Syndrome (SARS) Coronavirus Nucleocapsid Protein for Serodiagnosis of SARS Coronavirus Pneumonia. J Clin Microbiol. 2004;42:2306–2309. doi: 10.1128/JCM.42.5.2306-2309.2004. https://doi.org/10.1128/JCM.42.5.2306-2309.2004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cao Q, Chen YC, Chen CL, et al. SARS-CoV-2 infection in children: Transmission dynamics and clinical characteristics. J Formos Med Assoc. 2020;119:670–673. doi: 10.1016/j.jfma.2020.02.009. https://doi.org/10.1016/j.jfma.2020.02.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. https://doi.org/10.1016/S0140-6736(20)30360-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Groß R, Conzelmann C, Müller J, et al. Detection of SARS-CoV-2 in Human Breast Milk. Lancet. 2020;395:1757–1758. doi: 10.1016/S0140-6736(20)31181-8. https://doi.org/10.1016/S0140-6736(20)31181-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schwartz DA. An Analysis of 38 Pregnant Women with COVID-19, Their Newborn Infants, and Maternal-Fetal Transmission of SARS-CoV-2: Maternal Coronavirus Infections and Pregnancy Outcomes. Arch Pathol Lab Med. 2020 doi: 10.5858/arpa.2020-0901-SA. 10.5858/arpa.2020-0901-SA. https://doi.org/10.5858/arpa.2020-0901-SA . [DOI] [PubMed] [Google Scholar]
- 68.Elkafrawi D, Joseph J, Schiattarella A, et al. Intrauterine transmission of COVID-19 in Pregnancy: case report and review of literature. Acta Bio Med [Internet] 2020 May 28 [cited 2020Jul.14];91(3) doi: 10.23750/abm.v91i3.9795. Available from: https://www.mattioli1885journals.com/index.php/actabiomedica/article/view/9795 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Olofsson S, Kumlin U, Dimock K, et al. Avian influenza and sialic acid receptors: more than meets the eye. Lancet Infect Dis. 2005;5:184–188. doi: 10.1016/S1473-3099(05)01311-3. https://doi.org/10.1016/s1473-3099(05)01311-3 . [DOI] [PubMed] [Google Scholar]
- 70.Peiris JS, Yuen KY, Osterhaus AD, et al. The severe acute respiratory syndrome. N Engl J Med. 2003;349:2431–2441. doi: 10.1056/NEJMra032498. https://doi.org/10.1056/NEJMra032498 . [DOI] [PubMed] [Google Scholar]
- 71.Belser JA, Rota PA, Tumpey TM. Ocular Tropism of Respiratory Viruses. Microbiol Mol Biol Rev. 2013;77:144–156. doi: 10.1128/MMBR.00058-12. https://doi.org/10.1128/mmbr.00058-12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sun C, Wang Y, Liu G, et al. Role of the eye in transmitting human coronavirus: What we know and what we Do not know. Front Public Health. 2020;8:155. doi: 10.3389/fpubh.2020.00155. https://doi.org/10.3389/fpubh.2020.00155 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lu C, Liu X, fen Jia, et al. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. https://doi.org/10.1016/S0140-6736(20)30313-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Xia J, Tong J, Liu M, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020 doi: 10.1002/jmv.25725. 10.1002/jmv.25725. https://doi.org/10.1002/jmv.25725 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ye F, Xu S, Rong Z, et al. Delivery of infection from asymptomatic carriers of COVID-19 in a familial cluster. Int J Infect Dis. 2020;94:133–138. doi: 10.1016/j.ijid.2020.03.042. https://doi.org/10.1016/j.ijid.2020.03.042 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chan JFW, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. https://doi.org/10.1016/S0140-6736(20)30154-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kuperferschmidt K. Study claiming new coronavirus can be transmitted by people without symptoms was flawed. Science. 2020 Available from: https://www.sciencemag.org/news/2020/02/paper-non-symptomatic-patient-transmitting-coronavirus-wrong# . Accessed July 11, 2020. [Google Scholar]
- 78.Kinnear J. Asymptomatic Covid-19 patients can still develop lung damage. The Print. 2020 Available from: https://theprint.in/health/asymptomatic-covid-19-patients-can-still-develop-lung-damage/449337/ . Accessed July 13, 2020. [Google Scholar]
- 79.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly. 2020;2(8):113–122. https://doi.org/10.46234/ccdcw2020.032. [PMC free article] [PubMed] [Google Scholar]


