Abstract
Humeral non-union is a rare complication in shaft fractures, as well as humeral head necrosis is a possible complication in fracture involving the proximal third especially in four-part fractures. The presence of head osteonecrosis and diaphyseal non-union in the same arm represents a formidable challenge for an orthopaedic surgeon. We could not find any similar report in the literature dealing with this issue thus far. We present a case of a 65 years old woman referred to our hospital being affected by an atrophic humeral diaphyseal non-union with a massive bone loss (>10cm) associated to a humeral head osteonecrosis following a previous surgical procedures with a clear loosening of the hardware. At our institution, she was treated with hardware removal and insertion of a diaphyseal antibiotic spacer with Gentamycin for 2 months suspecting an active septic process at the union site despite negative cultural exams. Finally, she was treated with a cemented modular humeral megaprosthesis. At 20 months follow up, the patient, despite a reduced shoulder range of motion, referred to a pain-free recovery to an almost normal lifestyle, including car driving with no major disturbances. This case suggests that, in extreme selected cases following several failed treatments, megaprosthesis can represent a viable solution, especially in huge bone loss associated to joint degeneration, to ensure an acceptable return to a normal lifestyle. (www.actabiomedica.it)
Keywords: Humerus, non-union, necrosis, megaprosthesis
Introduction
Humeral non-union can represent a complication in the diaphyseal fractures, especially in older people aged over 50 years affected by osteoporosis-related fractures, ranging from 2.6% to 13.4% (average 4.2%) after conservative treatment (1,2). Likewise, such a complication is not uncommon even following surgical treatment, according to the surgical technique with 4.5% using retrograde locking nailing, 11.6% after anterograde locking nailing and 4.2% after plate osteosynthesis (1,2).
Treatment of non-union ranges from low intensity pulsed ultrasound and administration of parathyroid hormone (PTH) to surgical treatment with intramedullary nails, plate fixation and external fixation with reported unions rate above 90% with open reduction and internal stable fixation associated to the use of autologous bone graft (ABG) (2). Currently, several Authors suggested alternatives to use ABG like the implantation of mesenchymal stem cells (MSCs), growth factors (GFs), Platelet Rich plasma (PRP), bone morphogenetic proteins (rhBMPs) and even vascularised bone graft (3-5). Likewise, Ilizarov bone transport has been proposed as a valid surgical technique in managing the complication associated to bone loss in atrophic non-union (6).
Osteonecrosis of the humeral head is a disorder that involves osteocytes and bone marrow, being characterized by bone death causing subchondral bone collapse and arthritic changes. It was first described by Cruess (7) in 1976 and it is reported ranging from the second to the third most common location after hip and knee in the human body, because of the vascularization of the humeral head, very similar to the femoral head; with a frequency between 3% and 35% according to some authors and between 5% and 17% according to others authors (7,8), because of osteonecrosis of the humeral head may be unrecognised for a long time with not specific symptoms. There are two forms of humeral head osteonecrosis: traumatic and atraumatic both compromising the bone blood supply. The traumatic type can develop after an injury such as a bone fracture or shoulder dislocation (9). The non-traumatic form occurs with the use of corticosteroids and alcohol abuse or it can be associated with other diseases or blood disorders (e.g., sickle cell disease, problems with coagulation or making blood clots) (7,8).
Several different treatment for humeral head avascular osteonecrosis have been reported such as nonsurgical treatment, core decompression, arthroscopic debridement, humeral head resurfacing or shoulder arthroplasty or vascularised bone grafting (10). Core decompression and arthroscopic debridement are a useful treatment option in the early stages with pre-collapse of the humeral head, while humeral head resurfacing or hemi-arthroplasty and shoulder arthroplasty are a viable treatment option in the late stages with collapse of the humeral head. The reported overall success rate of any surgical procedure, averages more than 70% independently from disease stage and procedure, suggesting that surgery is an important therapeutic option in the humeral head osteonecrosis cases (10).
Case Presentation
A healthy old female aged 65 was referred to our department suffering from an atrophic non-union of the right humerus with a clear hardware loosening and massive bone loss complaining a stiff painful shoulder and referring three previous surgeries to her arm. All limited movements of her arm were located at the non-union site. Her medical history started on September 2012 when, because of diaphyseal humeral fracture, she was treated with an intramedullary reamed retrograde nail. On April 2013, because of a non-union at the fracture site, with a clear loosening of the proximal locking screws (fig 1a), she was treated with nail removal, debridement of the non-union and new fixation with a 9 holed 3.5 LCP plate using an extended antero-lateral approach to the humerus. On December 2013, because of proximal plate and screws loosing without any clear sign of bone healing (fig 1b), she underwent a third surgery with new debridement, autologous bone graft from iliac crest and repositioning of a new 9 holes plate adding 3 metallic cerclages to the construct to increase stability. On February 2015, the patient was referred to our institution because a catastrophic situation: more than 9 cm of diaphyseal bone loss (grade 3 according to Non-Union Scoring System – NUSS) (11) with a complete loose hardware palpable under the skin, and a reabsorbed humeral head, supposing a necrotic process (fig 2a, 2b). Clinically, the patient was extremely depressed and feed up for the unsuccessful previous treatments. She was complaining a stiff painful shoulder with a residual movement through the non-union site despite no evident peripheral neurological deficit.
Figure 1.
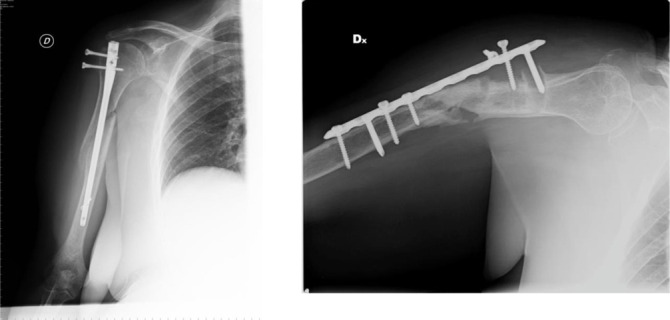
(a, b) Failures of the first 2 surgeries
Figure 2.
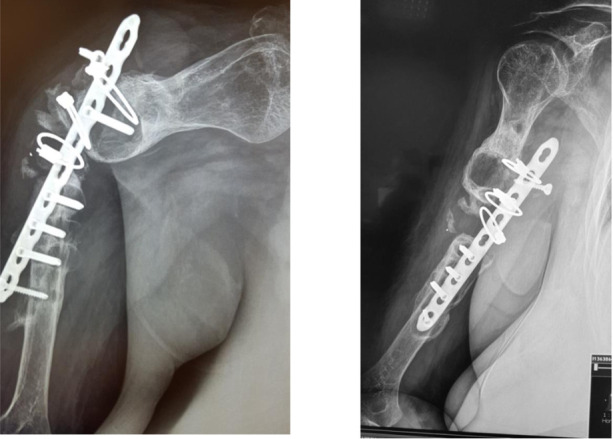
(a, b) Bone loss and mobilisation of fixation devices after 3rd intervention with clear areas of bone reabsorption in the femoral head
At our institution, she was assessed to exclude any infection and all the blood tests, ultrasound guided biopsy with white cells count, and cultures from the non-union site were all negative despite a positive labeled leukocyte scintigraphy performed few weeks before our department admission. The shoulder status was assessed using a CT scan, showing visible reabsorption areas of the necrotic bone (fig 3b) and an evident previous nail hole in the metaphyseal region below the humeral head (fig 3a).
Figure 3.
(a, b). CT scan showing a still open nail hole in the proximal metaphysis (fig 3a) and clear areas of necrotic bone in the humeral head (fig 3b).
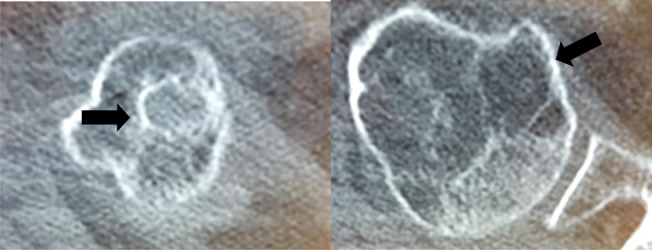
On April 2015, all hardware was removed in association together with debridement and a wide (11 cm) diaphyseal bone resection replaced by an handmade antibiotic loaded spacer (Gentamicin + Clindamycin) (fig 4). All the intraoperative specimens, including the removed hardware and cultures, resulted negative for any infection.
Figure 4.

Antibiotic loaded cementic spacer following hardware removal and wide bone resection
Two months later, the patient underwent the final surgical procedure with antibiotic spacer removal, debridement and a further 1+1 cm bone resection, and implanting a custom made cemented megaprosthesis (Megasytem-C, Waldemar Link, Hamburg, Germany). At 20 months postoperatively, the patient was extremely satisfied with a pain-free recovery to an almost normal lifestyle including car driving despite an incomplete shoulder range of motion recovery (<110° in shoulder elevation/abduction). At the radiological assessment, there were no radiological sign either of implant loosening or glenoid reabsorption or proximal migration of the humeral head (fig 5).
Figure 5.

Mega prosthesis at the 20 months follow-up
Discussion
Post-traumatic osteonecrosis of the humeral head is a known complication after trauma and fracture to the shoulder girdle compromising the blood supply. Several authors reported humeral head osteonecrosis following proximal nailing in 3-4 part fractures with poor outcome associated to proximal screw perforation meanwhile there are few reports regarding humeral osteonecrosis following surgical treatment of diaphyseal fracture (9,12) and mainly as a heat induced complication of reamed intramedullary nailing occurring from the metaphysis to the diaphysis (13). In our case, the original intramedullary humeral canal was wide enough for a safe reaming without heat induced osteonecrosis and the implanted nail was undersized questioning its stability but not as a potential cause of humeral head devascularization. Nevertheless the CT scan performed at more than 2 years following the first surgical procedure, documented a still unfilled nail canal in the remaining part of the proximal metaphysis suggesting both a compromised bone healing capacity and a poor bloody supply. Furthermore, we believe that even the new joint articulation at the non-union site could had caused a pathological overstress on the humeral head blood supply.
According to some authors, osteonecrosis of the humeral head could be pain-free with no major issues in daily life especially for older people (14). In our case, the patient referred an already painful shoulder. This makes questionable if any new fixation prolonged to an already compromised humeral head would have had increased pain and stiffness with a need for a further secondary replacement.
Likewise, compromised bone stock and heavily impaired structural integrity after multiple revision surgeries due to non-union, inadequate fixation, compromised vascular supply leads to a comparable condition as encountered in musculoskeletal tumor surgery needing salvage surgeries such as megaprosthesis or amputation (15,16). Modern modular megaprostheses have allowed for limb preserving surgery being the gold standard in oncologic orthopaedic surgery, as they facilitate efficient reconstruction of large skeletal defects, combined with high limb salvage rate. They also offer valuable solutions in the case of major trauma or end-stage revision arthroplasty (15-17) even if we could find only few cases of modular humeral megaprostheses implanted for non-oncological causes and mainly following distal humeral issues. Wodayo et al. in 2003 and Waha et al. in 2015 both reported that even humeral endoprosthetic reconstruction offers a method to preserve a functional upper extremity with a preserved functional hand and some limitations to elbow and shoulder motion (18,19).
We considered a mega-endoprosthesis the best suitable implant for our patient in accordance to the literature assuming in these challenging cases no significant advantages in replacing even the glenoid but preserving anyway the possibility to reattach the rotator cuff and/or deltoid muscles (19,20).
To our knowledge, the case we proposed is the first report in the literature dealing with a recalcitrant diaphyseal humeral non-union associated simultaneously to a humeral head osteonecrosis.
In selected cases, megaprosthesis could represent a viable solution to manage repeated unresolved failures of traditional treatment of long bone fractures with the simultaneously association of bone loss and joint degeneration.
List of abbreviations
- Availability of data and materials
- ROM =
range of motion
- LCP =
locking compression plate
- CT =
computerized tomography
- NUSS =
Non-Union Scoring System
Ethics approval and consent to partecipate:
This study (Humeral head necrosis associated to shaft non-union with massive bone loss: a case report) has been granted an exemption from requiring ethics approval from the under reported Ethical Comitee: Ospedale L. Sacco, COMITATO ETICO, Via G.B. Grassi n.74, 20157 Milano, tel. 02 3904.351/352. An informed consent to participate in the study was obtained from the patient.
Consent to publish:
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Availability of data and materials:
The datasets used and/or analysed during this Case reposrt study are available from the corresponding author on reasonable request.
Funding:
The authors declare that they did not receive any funding to support this study
Authors’ contributions:
All authors have equally participated to the present study
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.C Tzioupis, P.V Giannoudis. Prevalence of long-bone non-unions. Injury. 2007;38S:S3–S9. doi: 10.1016/s0020-1383(07)80003-9. [DOI] [PubMed] [Google Scholar]
- 2.Koutalos A, Varitimidis S, Dailiana Z, Bargiotas K, Koutsogiannis A, Malizos K. Operative management of humeral nonunions. Factors that influence the outcome. ActaOrthop. Belg. 2015;81:501–510. [PubMed] [Google Scholar]
- 3.G.M Calori, E Mazza, M Colombo, C Ripamonti, L Tagliabue. Treatment of long bone non-unions with polytherapy: indications and clinical results. Injury. 2011;42:587–590. doi: 10.1016/j.injury.2011.03.046. [DOI] [PubMed] [Google Scholar]
- 4.Giannoudis PV, Kanakaris NK, Schmidmaier G, Marsh D. the diamond concept: open questions. Injury. 2008;39(Suppl 2):S5–S8. doi: 10.1016/S0020-1383(08)70010-X. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez-Bances I, Perez-Basterrechea M, Perez-Lopez S, Nunez Batalla D, Fernandez Rodriguez MA, Alvarez-Viejo M, et al. Repair of long-bone pseudoarthrosis with autologous bone marrow mononuclear cells combined with allogenic bone graft. Cytotherapy. 2013;15(5):571–7. doi: 10.1016/j.jcyt.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Atkins RM. Principles of management of septic non-union of fracture. Injury. 2007 May;38(Suppl 2):S23–32. doi: 10.1016/s0020-1383(07)80006-4. [DOI] [PubMed] [Google Scholar]
- 7.RL Cruess Steroid-induced avascular necrosis of the head of the humerus. Natural history and management. J Bone Joint Surg Br. 1976;58(3):313–317. doi: 10.1302/0301-620X.58B3.956247. [DOI] [PubMed] [Google Scholar]
- 8.Harreld KL, Marker DR, Wiesler ER, Shafiq B, Mont MA. Osteonecrosis of the humeral head. J Am Acad Orthop Surg. 2009 Jun;17(6):345–55. doi: 10.5435/00124635-200906000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Patel S, Colaco HB, Elvey ME, Lee MH. Post-traumatic osteonecrosis of the proximal humerus. Injury. 2015;46:1878–84. doi: 10.1016/j.injury.2015.06.026. [DOI] [PubMed] [Google Scholar]
- 10.F Franceschi, E Franceschetti, M Paciotti, G Torre, K Samuelsson, R Papalia, J Karlsson, V Denaro. Surgical management of osteonecrosis of the humeral head: a systematic review. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-016-4169-z. DOI 10.1007/s00167-016-4169-z. [DOI] [PubMed] [Google Scholar]
- 11.Calori GM, Phillips M, Jeetle S, et al. Classification of non-union: need for a new scoring system? Injury. 2008;39(Suppl 2):S59–S63. doi: 10.1016/S0020-1383(08)70016-0. [DOI] [PubMed] [Google Scholar]
- 12.Zirngibl B, Biber R, Bail HJ. Humeral head necrosis after proximal humeral nailing: what are the reasons for bad outcomes? Injury. 2016;47(Suppl 7):S10–S13. doi: 10.1016/S0020-1383(16)30847-6. [DOI] [PubMed] [Google Scholar]
- 13.Ochsner PE, Baumgart F, Kohler G. Heat-induced segmental necrosis after reaming of one humeral and two tibial fractures with a narrow medullary canal. Injury. 1998;29(Suppl 2):B1–B10. doi: 10.1016/s0020-1383(98)80057-0. [DOI] [PubMed] [Google Scholar]
- 14.Arcuri PP, Barbalace G, Porpiglia H, Tamburrini O. A case of asymptomatic bilateral osteonecrosis of the humeral head. Radiol Med. 1998;96(5):513–5. [PubMed] [Google Scholar]
- 15.Evans S, Laugharne E, Kotecha A, Hadley L, Ramasamy A, Jeys L. Megaprostheses in the management of trauma of the knee. J Orthop. 2015;13(4):467–471. doi: 10.1016/j.jor.2015.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calori GM, Colombo M, Malagoli E, Mazzola S, Bucci M, Mazza E. Megaprosthesis in post-traumatic and periprosthetic large bone defects: Issues to consider. Injury. 2014;45(Suppl 6):S105–S110. doi: 10.1016/j.injury.2014.10.032. [DOI] [PubMed] [Google Scholar]
- 17.Toepfer A, Harrasser N, Petzschner I, Pohlig F, Lenze U, Gerdesmeyer L, Pförringer D, Toepfer M, Beirer M, Crönlein M, von Eisenhart-Rothe R, Mühlhofer H. Short- to long-term follow-up of total femoral replacement in non-oncologic patients. BMC Musculoskelet Disord. 2016;17(1):498. doi: 10.1186/s12891-016-1355-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wodajo FM, Bickels J, Wittig J, Malawer M. Complex reconstruct-ion in the management of extremity sarcomas. Curr Opin Oncol. 2003;15(4):304–12. doi: 10.1097/00001622-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Wafa H, Reddy K, Grimer R, Abudu A, Jeys L, Carter S, Tillman R. Does total humeral endoprosthetic replacement provide reliable reconstruction with preservation of a useful extremity? Clin Orthop Relat Res. 2015 Mar;473(3):917–25. doi: 10.1007/s11999-014-3635-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong JC, Abraham JA. Upper extremity considerations for oncologic surgery. Orthop Clin North Am. 2014;45(4):541–64. doi: 10.1016/j.ocl.2014.06.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during this Case reposrt study are available from the corresponding author on reasonable request.


