Abstract
Background:
The association between acute kidney injury (AKI) and outcome of coronavirus disease 2019 (COVID-19) has not yet been conclusively established. Therefore, we conducted a meta-analysis of recent scientific literature to assess whether AKI may be associated with worse prognosis and increased mortality in COVID-19 patients.
Methods:
A systematic search of literature was conducted between 1st November 2019 and 15th May 2020 on Medline (PubMed interface) and China National Knowledge Infrastructure (CNKI) to identify potentially eligible studies. Cohort or case-control studies reporting data on AKI in patients with or without severe COVID-19 were included. Studies were divided into separate cohorts for analysis based on two endpoints (severity [severe vs non-severe] and mortality [non-survivors vs survivors]). Data were pooled into a meta-analysis to estimate pooled odds ratio (OR) with 95% confidence interval (95% CI) for either outcome.
Results:
A total of 15 studies (n= 5,832 patients) were included in the analysis. Overall, AKI was found to be associated with significantly increased odds of COVID-19 severity (OR= 18.5; 95% CI 8.99-38.08) and mortality (OR= 23.9; 95% CI 18.84-30.31). No heterogeneity was observed for both outcomes (Cochran’s Q= 6.21, p=0.52, I2=0% and Cochran’s Q= 4.56, p=0.47, I2=0% respectively).
Conclusion:
According to current data, AKI seems to be associated with worse prognosis in COVID-19 patients. Further investigation of the underlying mechanism of renal disease in COVID-19 would be needed to clarify possible therapeutic targets. AKI could be used as a clinical characteristic in severity classification and risk stratification.
Keywords: Acute Kidney Injury, COVID-19, Mortality
Supplementary Material (Publication Bias and Meta-Regression)
Introduction
Coronavirus disease 2019 (COVID 19) is a novel zoonotic disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1,2]. Since the outbreak began in December 2019, the disease has rapidly spread all over the world persuading the World Health Organization (WHO) to declare it a global pandemic in March, 2020 [3]. Currently, transmission of SARS-CoV-2 is through person-to-person contact with infected COVID-19 patients either directly or via droplets [4]. This has resulted in major travel restrictions and lockdowns in many countries with concomitant untoward economic and social repercussions.
The infectivity of SARS-CoV-2 is via its attachment to the angiotensin-converting enzyme 2 (ACE2) receptor, which is widely found in many immune and non-immune cells including epithelial cells of intestinal and respiratory mucosa, endothelial cells and renal tubules [5]. This has resulted to the seeding of the virus to many organs as evidenced by its isolation not only from respiratory samples but also from other body fluids, including conjuctival secretions [6], semen [7], stool [8] and even occasionally urine [9], thus supporting active renal involvement. Consequently, the clinical course of COVID 19 is highly variable. Although initial reports indicated that it mainly caused respiratory disease with alveolar damage and acute respiratory distress [10], current understanding is that COVID-19 encompasses a broader spectrum ranging from asymptomatic disease to multiple organ failure (MOF) and death [11]. The severity of disease and likelihood of mortality has further been linked with many other factors including advanced age, male sex and pre-existing chronic medical conditions [11]. In severe cases of COVID-19, the development of acute organ injury, including acute kidney injury (AKI), has also been documented.
The occurrence of AKI in COVID-19 patients has been reported to range between 5% and 27% [12-14]. In a few instances, patients were known to present to the emergency department with AKI- related symptoms as the only presenting features [15,16]. Previous studies have also demonstrated that elevated creatinine levels at admission is associated with increased risk of severe disease [17]. This renal involvement has been directly linked to the severity of respiratory disease [18] and has been heightened by preponderance of ACE2 expression at the surface of renal tubular epithelial cells [19]. Although COVID-19 patients were shown to have higher risk of in-hospital mortality [13,18], this association has not been conclusively established. Furthermore, the relationship of AKI as a predictor to the severity of COVID-19 has largely not been defined. Therefore, this study aims at clarify the clinical association between AKI and COVID-19 severity and mortality.
Methods
Study protocol and registration
This systematic review and meta-analysis was conducted in strict conformity with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20]. The study protocol has been reported in the International Prospective Register of Systematic Reviews (PROSPERO identifier: CRD42020184330).
Literature Search Strategy
A comprehensive and systematic search of scientific literature was conducted between November 1st, 2019 to May 15th, 2020 on PubMed and China National Knowledge Infrastructure (CNKI) to identify eligible studies. The electronic search was carried out using the following keywords: (1) (((COVID-19) OR SARS-CoV-2) OR 2019-nCoV (2) (((((Acute kidney injury) OR Acute renal injury) OR AKI) OR Creatinine) OR Urine output))) OR Laboratory characteristics (3) 1 AND 2. No language restriction was applied. When the articles were published by the same study group and an overlap was found, only the most recent article was included to avoid duplication of data. The PubMed function “related articles” was used to extend the search. We also searched major infectious disease, nephrology and general medicine journals reporting articles about COVID-19 infection to look for additional studies. We then performed hand-search of bibliography of included studies, to identify other potentially eligible investigations.
Eligibility Criteria
All studies were screened and assessed for eligibility by three independent reviewers (I.C, V.K, and B.N). Search results were screened by title and abstract, with those of potential relevance evaluated by full text. Studies were deemed eligible for inclusion if they fulfilled the following criteria: (1) observational cohort or case-control studies reporting AKI frequency data, (2) clearly defined AKI as per the KDIGO clinical practice guidelines [21], (3) used appropriate definition of severe disease or compared survivors to non-survivors in a general cohort or compared survival to non-survivors in a critically ill cohort, (4) disease severity was monitored over the course of study, (5) clearly outlined the definition of “severe disease” and (6) sample size >10. Severe disease was defined in this analysis as a composite of: (1) respiratory distress, respiratory rate ≥30 per min; (2) oxygen saturation on room air at rest ≤93%; (3) partial pressure of oxygen in arterial blood / fraction of inspired oxygen ≤300 mmHg; (4) patients requiring mechanical ventilation/vital life support/intensive care unit admission (ICU); (5) death. Reviews and studies with incomplete or irrelevant data were excluded. Any disagreement between reviewers arising during the eligibility assessment was settled through consensus.
Data Extraction and Quality Assessment
Data extraction was conducted by three independent reviewers (I.C, V.K and B.N). For each study, the following information was extracted: surname of the first author and year of publication, country and city where the study was performed, type of study, sample size, baseline demographic characteristics, proportion of patients with severe and non-severe COVID-19, proportion of patients with AKI, and mortality from COVID-19. Any variances were resolved by consensus. Quality assessment and analysis of risk of bias of all selected full-text articles was performed using the methodological index for non‐randomized studies (MINORS) tool.
Outcomes of Interest
The primary outcome of interest was the association between AKI and COVID-19 severity, while the secondary outcome was the association between AKI and COVID-19 mortality. A tertiary outcome was the association between AKI and mortality in patients with severe COVID-19 disease. Thus, a total of three separate meta-analyses were performed.
Statistical Analysis
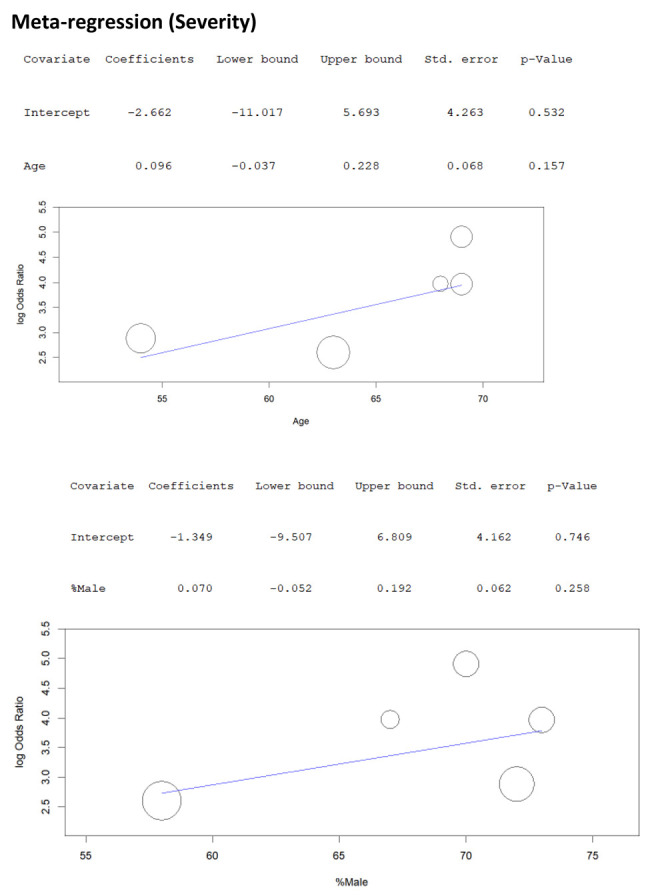
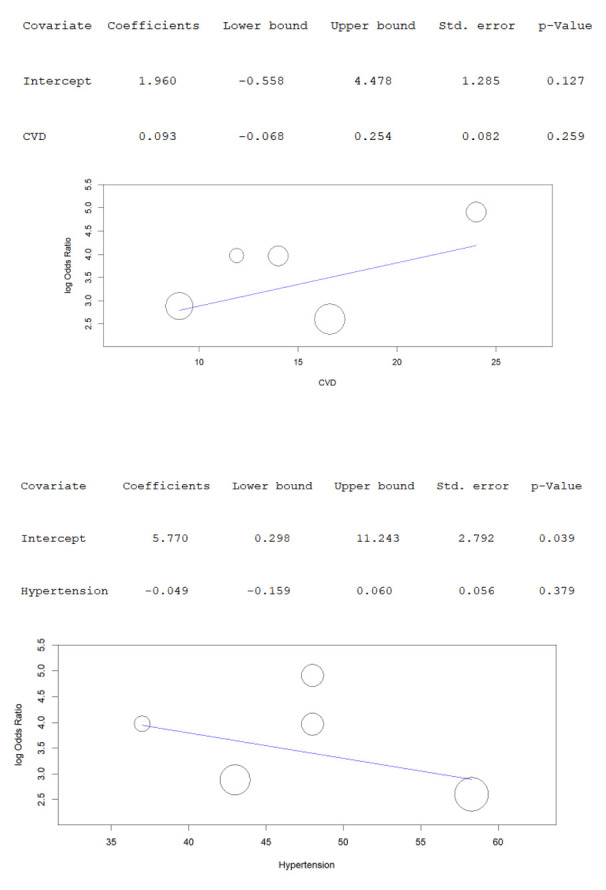
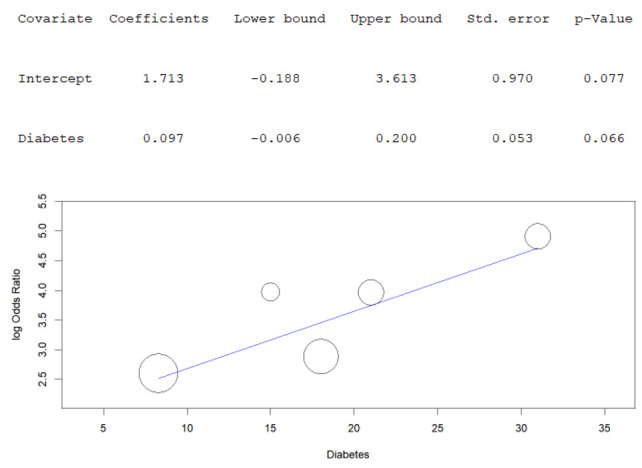
The statistical analysis was carried out using MetaXL (software Version 5.3, EpiGear International Pty Ltd., Sunrise Beach, Australia) and the Meta-Analyst (software version 5.26.14, Center for Evidence-Based Medicine, Brown University, Providence, USA). The strength of association between AKI and COVID-19 severity and mortality was estimated using odds ratio (OR). A random-effects model was applied. The magnitude of heterogeneity among the included studies was assessed using the chi-squared test (Chi2) and I-squared statistic (I2). For the Chi2 test, a Cochrane’s Q p value of <0.10 was considered significant. The values of the I2 statistic were interpreted as follows at a 95% confidence interval: Thresholds of 25%, 50% and 75% to designate low, moderate, and high heterogeneity were applied [22]. Publication bias was assessed by funnel plot analysis. A random effects meta-regression using log OR was performed to evaluate the impact of baseline characteristics (age and sex) and co-morbidities (diabetes, cardiovascular disease, chronic lung disease, cancer, and hypertension) on association of AKI with disease severity in patients with COVID-19. Additionally, leave-one out sensitivity analysis was performed to assess the robustness of the results, and to further probe the sources of inter-study heterogeneity.
Results
Study Identification
The initial search generated 346 potentially relevant articles. Following duplicate removal and primary screening, 52 articles were assessed by full text for eligibility in the meta-analysis. Of these, 37 were excluded because the primary and secondary outcome of the study did not match the criteria set in this review. A total of 15 articles could hence be included in this systematic review and meta-analysis (Figure 1; Table 1 and 2).
Figure 1.
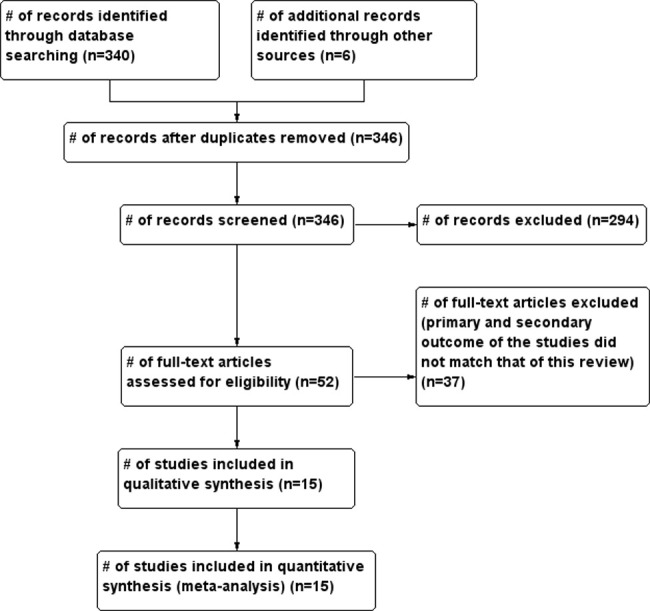
Flow of studies through the meta-analysis
Table 1.
Characteristics of studies included in the severity cohort analysis
| Study | Country & City | Sample Size | Severe patients | Non-severe patients | ||||||
| n (%) | Age (yrs) | Women (%) | AKI (%) | n (%) | Age (yrs) | Women (%) | AKI (%) | |||
| Guan et al. [4] | Outside Hubei, China | 1099 | 173 (15.7%) | 52 (40–65) | 73 (42%) | 5 (2.9%) | 926 (84.3%) | 45 (34-57) | 386 (42%) | 1 (0.1%) |
| Huang et al. [23] | Wuhan, China | 41 | 13 (31.7%) | 49 (41-61) | 2 (15%) | 3 (23.1%) | 28 (68.3%) | 49 (41-57.5) | 15 (53.6%) | 0 (0%) |
| Zhang Guqin et al., [24] | Wuhan, China | 221 | 55 (24.9%) | 62 (52-74) | 20 (36.4%) | 8 (14.5%) | 166 (75.1%) | 51 (36-64.3) | 93 (56%) | 2 (1.2%) |
| Yao et al., [25] | Dabieshan, China | 108 | 25 (23.1%) | - | 12 (48%) | 9 (36%) | 83 (76.9%) | 50.0 (34.0 56.0) |
53 (63.9%) | 7 (8.4%) |
| Aggarwal et al., [26] | Iowa, USA | 16 | 8 (50%) | 67 (38-70) | 3 (38%) | 8 (100%) | 8 (50%) | 68.5 (41-95) | 1 (13%) | 3 (37.5%) |
| Wang D et al., [27] | Wuhan, China | 138 | 36 (26.1%) | 66 (57-78) | 14 (38.9) | 3 (8.3%) | 102 (73.9%) | 51 (37-62) | 49 (48%) | 2 (1.9%) |
| Chen G et al., [28] | Wuhan, China | 21 | 11 (52.4%) | 61 (56.5-66) | 1 (9.1%) | 2 (18.2%) | 10 (47.6%) | 52 (42.8-56) | 3 (30%) | 0 (0%) |
| Hong et al., [29] | Daegu, South Korea | 98 | 13 (13.2%) | 63.2±10.1 | 7 (53.8%) | 8 (61.5%) | 85 (86.8%) | 54.2±17.7 | 53 (62.4%) | 1 (1.2%) |
Characteristics of the Included Studies and Quality Assessment
A total of 15 studies (n= 5,832 patients) were included. Of the included studies, 12 were from China, 2 from the United States (US) and 1 from South Korea. Seven studies reported AKI data in patients with and without severe COVID-19, seven studies reported data on mortality, while one study reported both. The essential characteristics of the included studies are outlined in tables 1 and 2. Summary of the methodological index for non‐randomized studies (MINORS) assessment for the included studies is provided in figure 2.
Table 2.
Characteristics of studies included in the mortality analysis cohort
| Study | Country & City | Sample Size | Survivors | Non-survivors | ||||||
| n (%) | Age (yrs) | Women (%) | AKI (%) | n (%) | Age (yrs) | Women (%) | AKI (%) | |||
| Zhou F et al., [10] | Wuhan, China | 191 | 137 (71.7%) | 52 (45-58) | 56 (41%) | 36 (26.3%) | 54 (28.3%) | 69 (63-76) | 16 (30%) | 41 (75.9%) |
| Chen T et al., [12] | Wuhan, Chins | 274 | 161 (58.8%) | 51 (37-66) | 73 (45%) | 8 (5%) | 113 (41.2%) | 68 (62-77) | 30 (27%) | 44 (40%) |
| Yao et al., [25] | Dabieshan, China | 108 | 12 (11.1%) | - | - | 5 (41.7%) | 96 (88.9%) | 65.0 (51.0,73.5) |
5 (41%) | 18 (18.75%) |
| Wang Y et al., [30] | Wuhan, China | 344 | 211 (61.3%) | 57 (47-69) | 106 (50.2%) | 6 (2.8%) | 133 ((38.7%) | 70 (62-77) | 59 (44.4%) | 80 (60.2%) |
| Yang et al., [11] | Wuhan, China | 52 | 20 (38.5%) | 51.9±12.9 | 6 (30%) | 3 (15%) | 32 (61.5%) | 64.6±11.2 | 11 (34%) | 12 (37.5%) |
| Deng et al., [31] | Wuhan, China | 225 | 116 (51.6%) | 40 (33-57) | 65 (56%) | 0 (0%) | 109 (48.4%) | 69 (62-74) | 36 (33%) | 20 (18.3%) |
| Ruan et al., [32] | Wuhan, China | 150 | 82 (54.7%) | 50 (44-81) | 29 (35%) | 2 (2.4%) | 68 (45.3%) | 67 (15-81) | 19 (28%) | 21 (30.9%) |
| Richardson et al., [33] | New York, USA | 2358 | 1869 (79.3%) | - | - | 176 (9.4%) | 489 (20.7%) | - | - | 347 (70.9%) |
Figure 2.
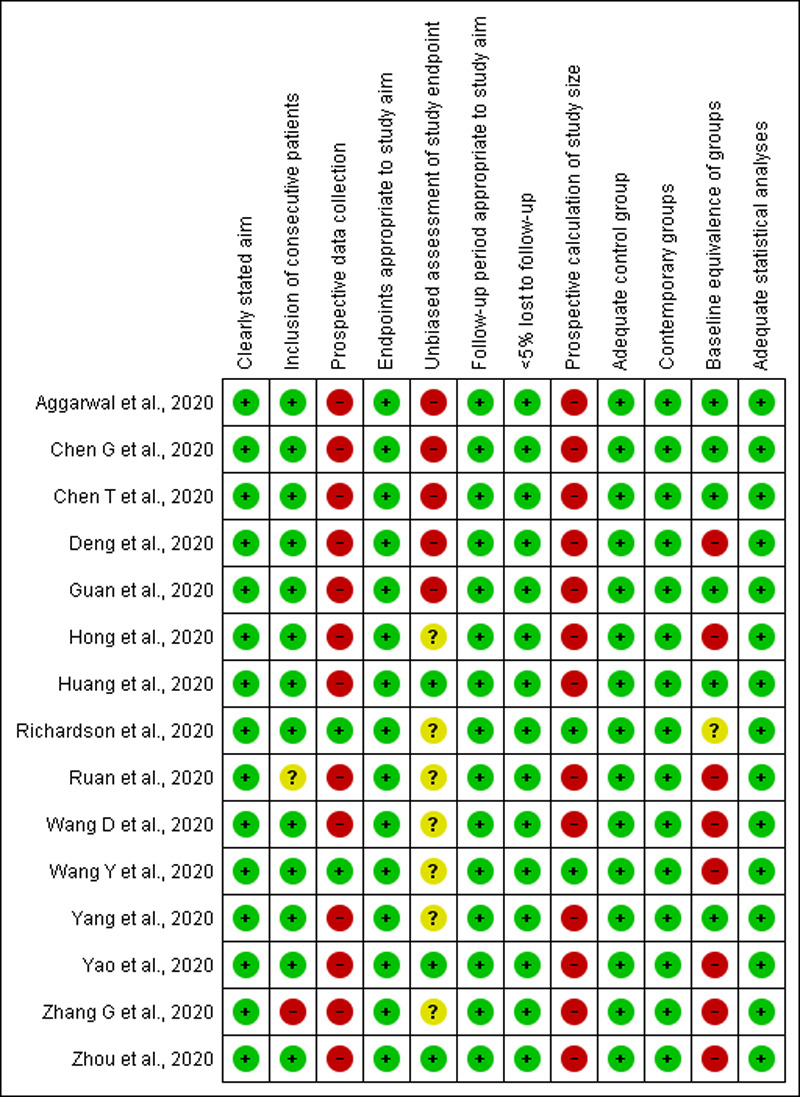
Summary of the MINORS quality assessment of the included studies
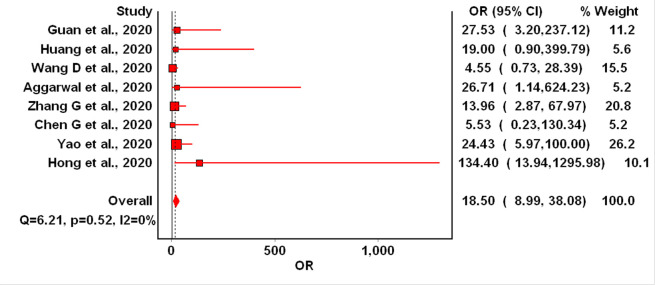
Meta-analysis on the association between AKI and COVID-19 severity
A total of 8 studies (n=1,730 patients) reported data on association between AKI and COVID-19 severity. In five out of these eight studies, AKI was associated with significantly enhanced odds of severe COVID-19 (Figure 3). In pooled analysis, AKI was found to be associated with significantly increased odds of severe COVID-19 (OR=18.5; 95% CI 8.99-38.08). No evidence of inter-study heterogeneity was observed for this outcome (Cochran’s Q= 6.21, p=0.52, I2=0%). No significant changes in the OR could be seen in the leave-one-out sensitivity analysis.
Figure 3.
Forest plot for association between AKI and COVID-19 severity
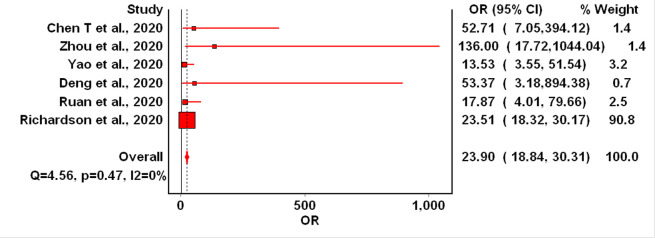
Meta-analysis on the association between CVD and overall COVID-19 mortality
A total of 6 studies (n=2,296 patients) reported data on association between AKI and COVID-19 mortality in all hospitalized patients (with both severe and non-severe form of the disease. In all these studies AKI was associated with significantly enhanced odds of mortality in COVID-19. In the pooled analysis, AKI was found to be associated with a significantly increased odds of mortality in COVID-19 patients (OR= 23.9; 95% CI 18.84-30.31). No evidence of inter-study heterogeneity was observed for this outcome (Cochran’s Q= 4.56, p=0.47, I2=0%). No significant changes in the OR were seen in the leave-one-out sensitivity analysis (Figure 4).
Figure 4.
Forest plot for association between AKI and overall COVID-19 mortality
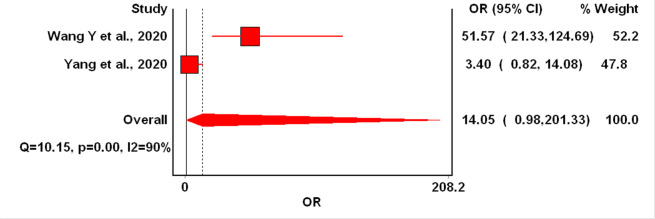
Meta-analysis on the association between AKI and mortality in severe COVID-19 disease
A total of two studies (n= 396 patients) reported data on mortality in patients with severe COVID-19 disease. In the pooled analysis, we found a non-significant trend toward increased mortality in AKI patients with severe COVID-19 disease, with high level of inter-study heterogeneity (OR=14.05; 95% CI: 0.98-201.33, I2=90%, Cochran’s Q=10.15, p=0.001). The bulk of the confidence interval extended well beyond the null value of 1, indicating a substantial elevated probability of a clinically important effect of AKI on mortality in patients with severe form of COVID-19 (Figure 5).
Figure 5.
Forest plot for association between AKI and mortality in severe COVID-19
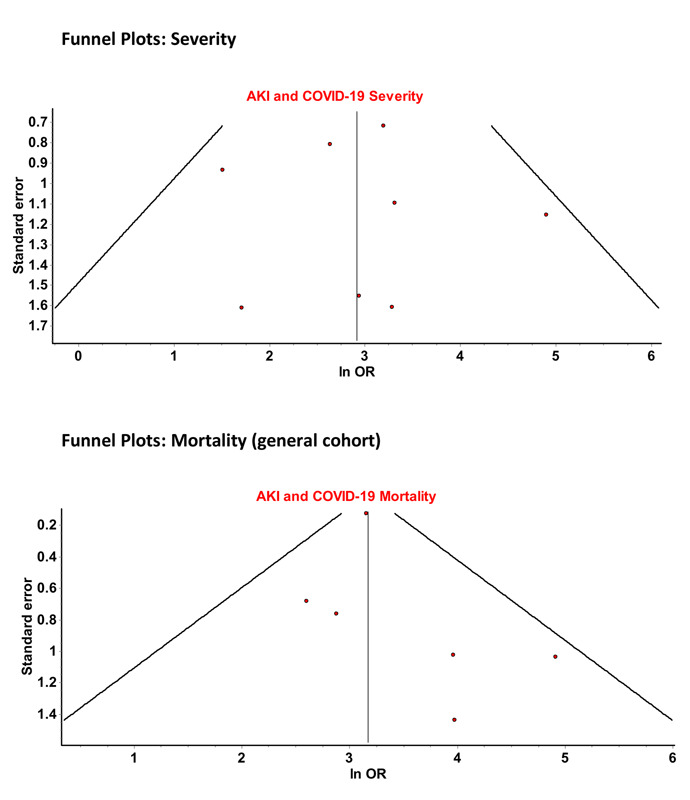
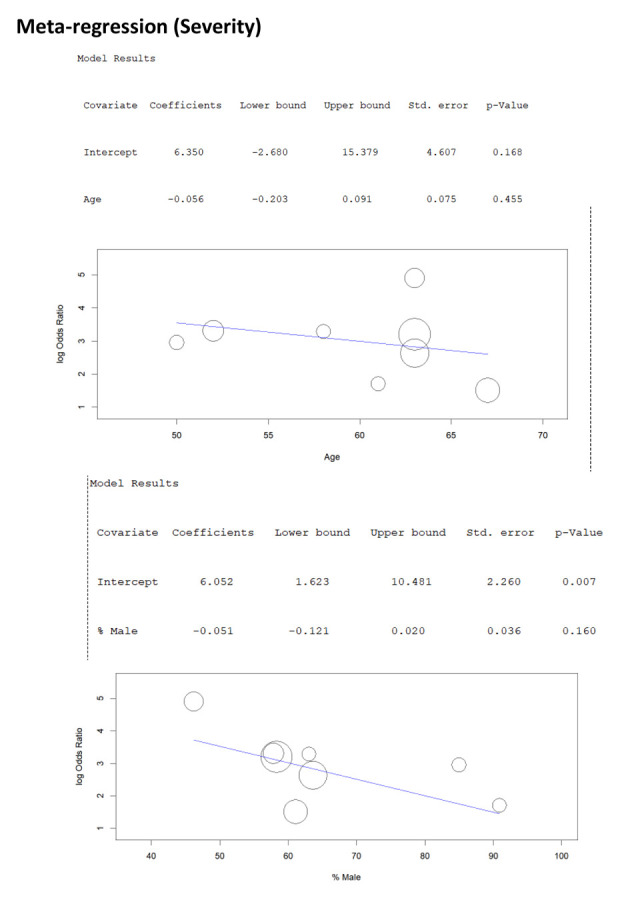
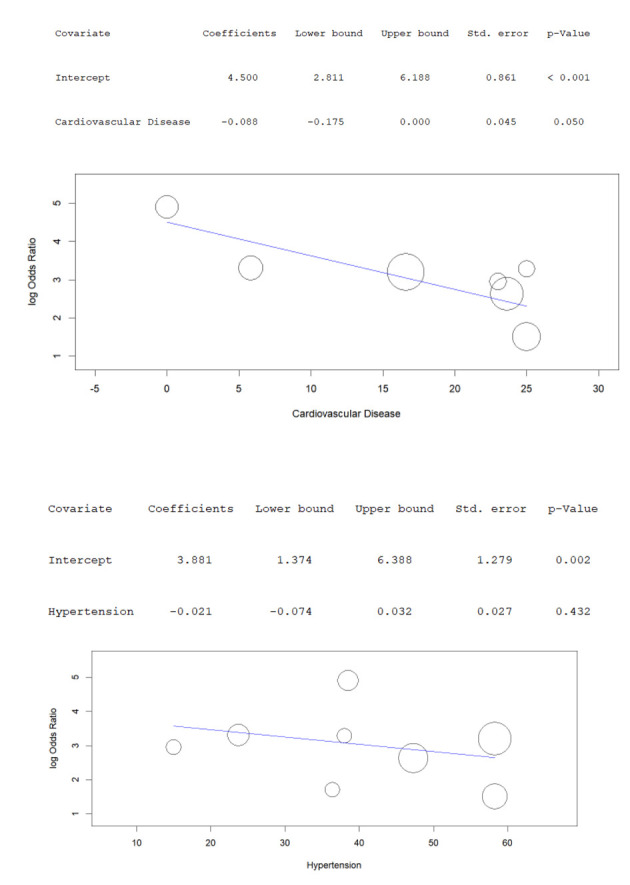
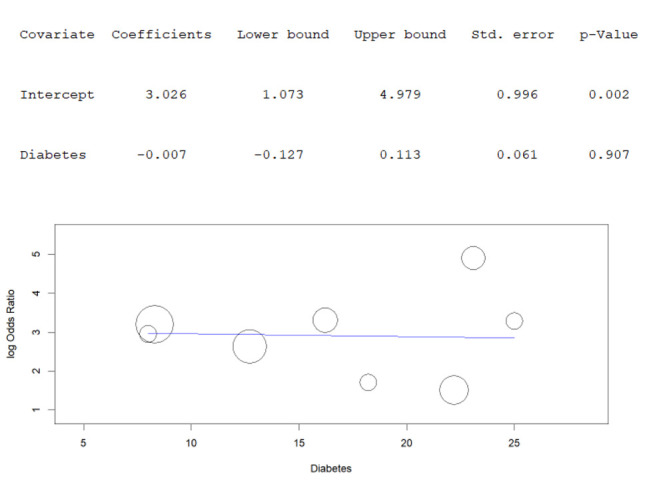
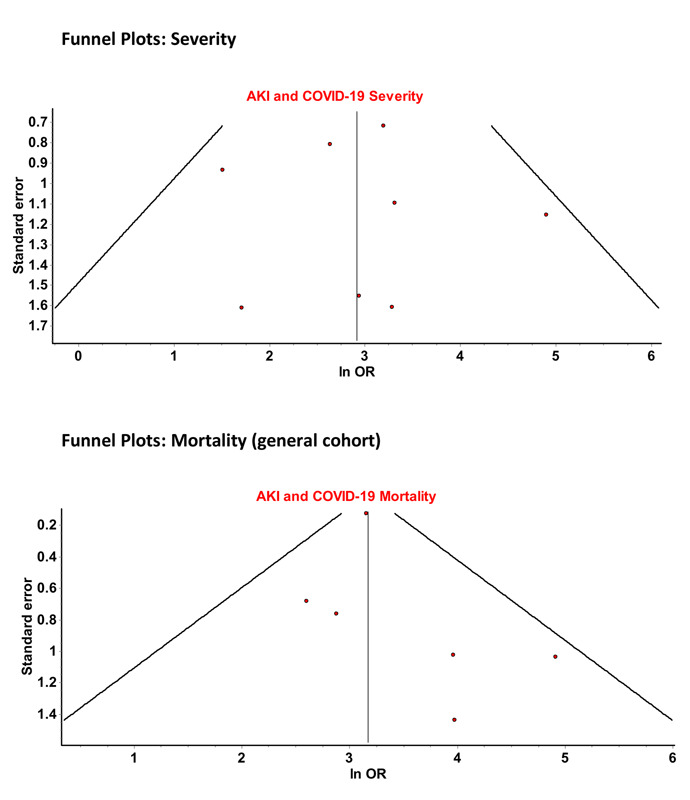
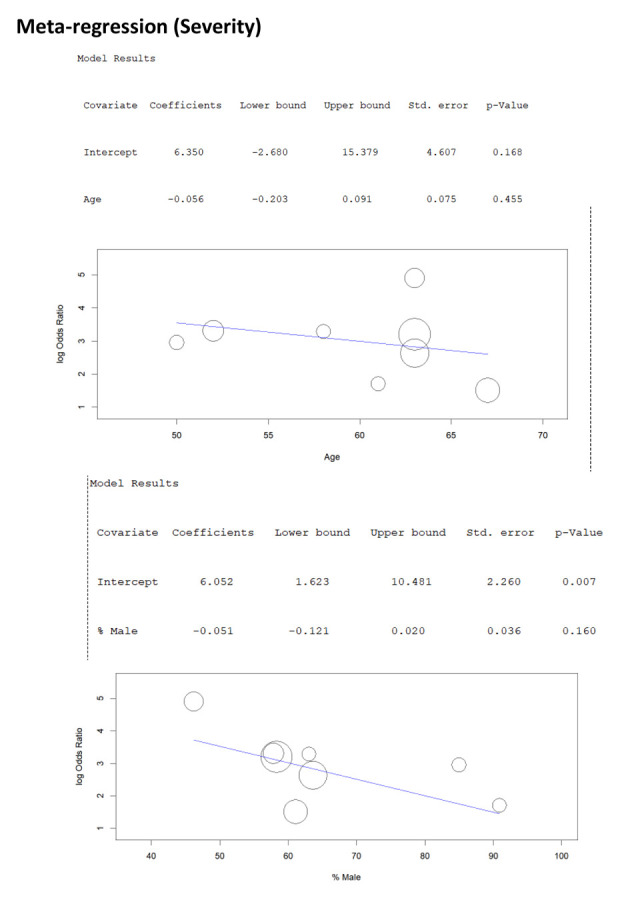
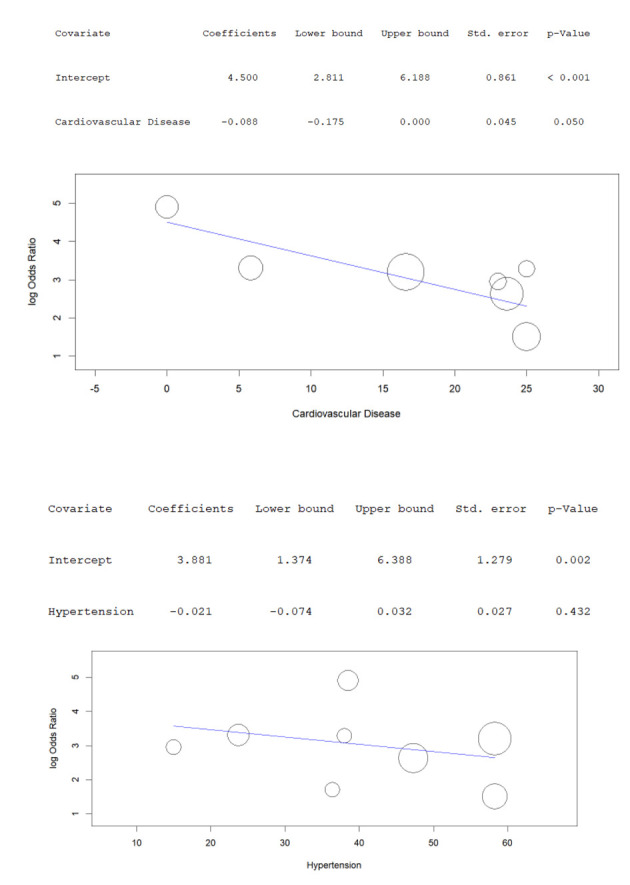
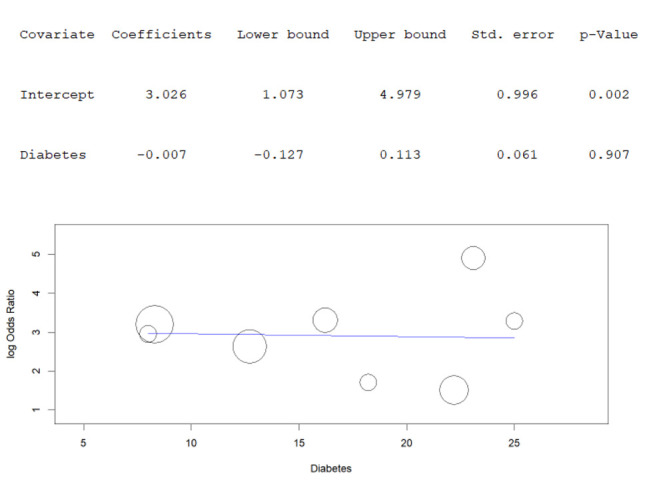
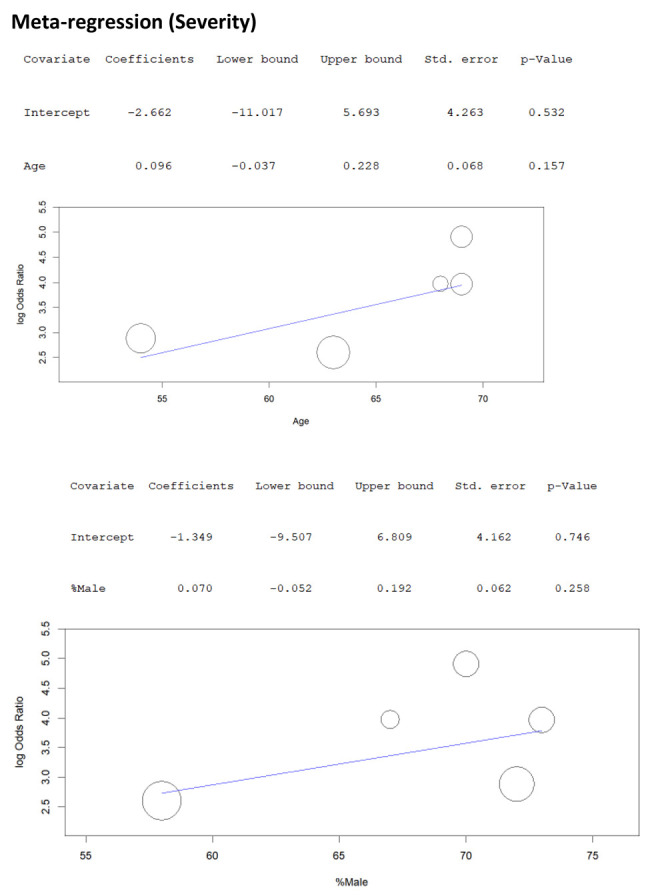
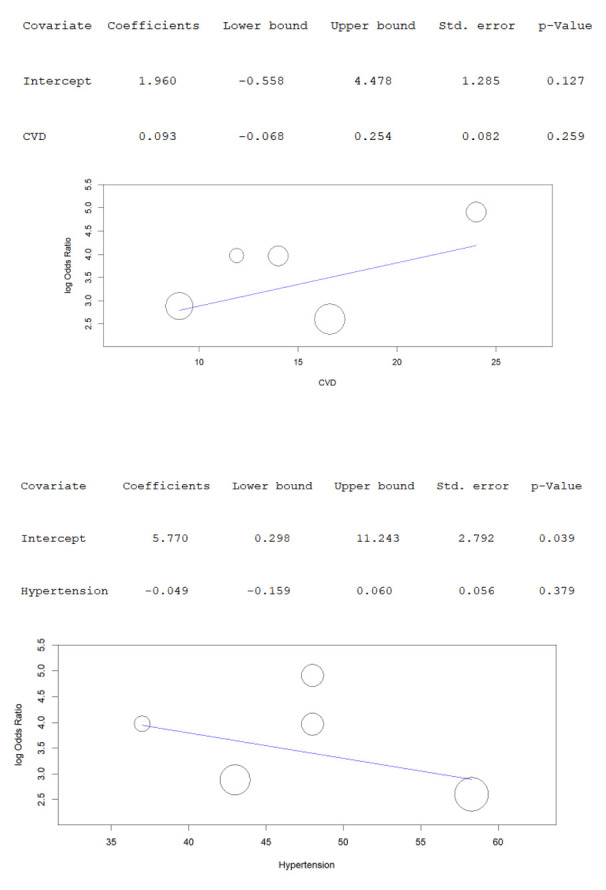
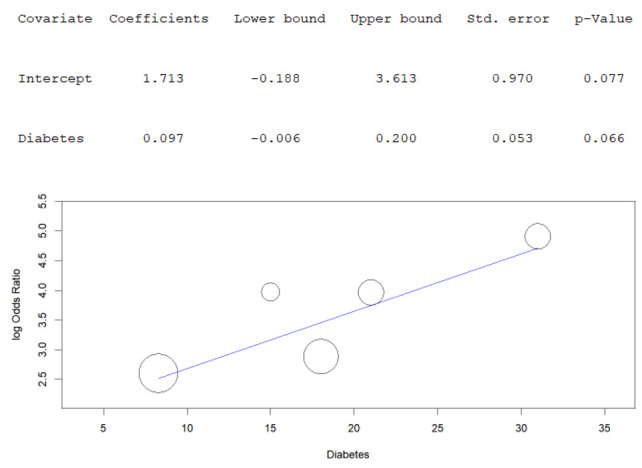
Publication Bias and Meta-Regression
The potential for publication bias was evaluated in funnel plots (supplementary material). No asymmetry was noted in funnel plot for AKI and COVID-19 severity, while mild asymmetry was noted in the funnel plot for AKI and overall COVID-19 mortality. In the meta-regression of odds of severe disease/mortality with AKI, the age, sex and co-morbidities (history of cardiovascular disease, hypertension or diabetes) in patients in the severe group had no significant influence on calculated pooled OR (supplementary material).
Discussion
The main findings of the current study demonstrate that development of AKI in COVID-19 patients seems to be a predictor of worse outcome in the course of illness, including disease severity and mortality.
AKI has been previously found to be an independent predictor of mortality throughout an ample array of critical illnesses [34]. Acute renal failure commonly complicates acute respiratory distress (ARDS) due to impaired oxygenation, fluid overload, cardiogenic shock, superimposed sepsis or injurious mechanical ventilation [21]. In COVID-19, the incidence of AKI has been seen in up to 29% of patient cohorts [10,11]. Nevertheless, the pathophysiology of acute renal injury still remains a subject of current investigation in COVID-19. Several mechanisms have been postulated. It is known that SARS-CoV-2 spike protein binds to ACE2 receptor in host cells [5]. Puelles et al., [35] recently demonstrated that the RNA for angiotensin-converting enzyme 2 (ACE2), the receptor that is considered to facilitate SARS-CoV-2 infection is enriched in multiple kidney-cell types from fetal development through adulthood [35]. In the kidney, host cells have been identified as podocytes and proximal straight tubule cells [36]. Puelles et al.,[35] in their study successfully identified SARS-CoV-2 in all kidney compartments examined, supporting the hypothesis of renal tropism. It is postulated that the cytopathic effects of the virus on these cells is responsible for the renal manifestations of COVID-19 [37]. Indeed, acute tubular necrosis with inflammatory cell infiltration has been demonstrated at autopsy [14,38]. In a case series 12 patients who died for COVID-19, Wichmann et al also found clear histopathologic evidence of cytopathic involvement and severe shock injury in renal tissue [39]. These findings have been recently confirmed in another case series of 11 autopsy of patients who have died for COVID-19, which showed dramatic cytopathic injuries of proximal tubules, nodular glomerulosclerosis and regenerating abnormalities with flattened tubular epithelium [40]. The clinical appearance of AKI in COVID-19 may also be a manifestation of microangiopathy and hypercoagulability which have been observed in the heart where they result in infarction [41] and inflammation [42]. Further, the hypercytokinemia that is a feature of this illness [43] and the resultant activation of the innate immune system can result in direct injury in the kidney. This is in the background of hypotension that attends this cytokine storm and superimposed sepsis which may itself cause AKI [44]. An interplay among these factors may therefore explain the clinical appearance of AKI in COVID-19. Regardless of the underlying pathophysiology, it seems unquestionable that occurrence of AKI in COVID-19 will be associated with worse clinical progression and/or mortality as seen in current data.
Taken together, the results of our meta-analysis would lead us to conclude that AKI is a relatively frequent manifestation in COVID-19 and, when it occurs in the clinical course of the disease, is a predisposing factor for development of worse clinical outcome (e.g., more severe illness) and/or death. Further investigation on the underlying mechanism of renal disease in COVID-19 would be needed to clarify possible therapeutic targets, whilst AKI could be used as clinical characteristic in severity classification and risk stratification for predicting unfavourable disease progression.
Author contributions
Conceptualization- IC, MM
Methodology-IC, VK, BMH
Data curation- IC, VK, BN
Software & Formal Analysis- IC
Investigation- All authors
Writing – Original Draft Preparation- IC, JM, MM
Writing – Review & Editing- All authors
Supervision- IC
Approval for submission- All authors
Funding:
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval:
Not applicable.
Author contribution:
All authors contributed to design and execution of the study. All authors participated in article drafting and critical revision.
References
- 1.Contini C, Nuzzo M Di, Barp N, Bonazza A, de Giorgio R, Tognon M, et al. The novel zoonotic COVID-19 pandemic: An expected global health concern. J Infect Dev Ctries. 2020;14(3):254–64. doi: 10.3855/jidc.12671. [DOI] [PubMed] [Google Scholar]
- 2.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun [Internet] 2020 doi: 10.1016/j.jaut.2020.102433. 109(February):102433. Available from: https://doi.org/10.1016/j.jaut.2020.102433 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Coronavirus disease. World Health Organ [Internet] 2020 2019(March):2633. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 . [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magrone T, Magrone M, Jirillo E. Focus on Receptors for Coronaviruses with Special Reference to Angiotensin-converting Enzyme 2 as a Potential Drug Target - A Perspective. Endocr Metab Immune Disord Drug Targets. 2020;20(00):1–5. doi: 10.2174/1871530320666200427112902. [DOI] [PubMed] [Google Scholar]
- 6.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92(6):589–94. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li D, Jin M, Bao P, Zhao W, Zhang S. Clinical Characteristics and Results of Semen Tests Among Men With Coronavirus Disease 2019. 2020;3(5):2019–21. doi: 10.1001/jamanetworkopen.2020.8292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kipkorir V, Cheruiyot I, Ngure B, Misiani M, Munguti J. Prolonged SARS-Cov-2 RNA Detection in Anal/ Rectal Swabs and Stool Specimens in COVID-19 Patients After Negative Conversion in Nasopharyngeal RT-PCR Test. J Med Virol. 2020 doi: 10.1002/jmv.26007. Pre Print:0-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peng L, Liu J, Xu W, Luo Q, Chen D, Lei Z, Huang Z, Li X, Deng K, Lin B, Gao Z. SARS-CoV-2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens. J Med Virol. 2020 Apr 24 doi: 10.1002/jmv.25936. doi: 10.1002/jmv.25936. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet [Internet] 2020;395(10229):1054–62. doi: 10.1016/S0140-6736(20)30566-3. Available from: http://dx.doi.org/10.1016/S0140-6736(20)30566-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med [Internet] 2020;8(5):475–81. doi: 10.1016/S2213-2600(20)30079-5. Available from: http://dx.doi.org/10.1016/S2213-2600(20)30079-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ [Internet] 2020;368(March):1–14. doi: 10.1136/bmj.m1091. Available from: http://dx.doi.org/doi:10.1136/bmj.m1091 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int [Internet] 2020;97(5):829–38. doi: 10.1016/j.kint.2020.03.005. Available from: https://doi.org/10.1016/j.kint.2020.03.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diao B, Feng Z, Wang C, Wang H, Liu L, Wang C, et al. Human Kidney is a Target for Novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection. medRxiv. 2020 doi: 10.1038/s41467-021-22781-1. 2:2020.03.04.20031120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gopalakrishnan A, Mossaid A, Lo KB, Vasudevan V, McCullough PA, Rangaswami J. Fulminant Acute Kidney Injury in a Young Patient with Novel Coronavirus 2019. Cardiorenal Med. 2020;11201:1–6. doi: 10.1159/000508179. http://www.ncbi.nlm.nih.gov/pubmed/32375150 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peleg Y, Kudose S, D’Agati V, Siddall E, Ahmad S, Kisselev S, et al. Acute Kidney Injury Due to Collapsing Glomerulopathy Following COVID-19 Infection. Kidney Int Reports. 2020:1–6. doi: 10.1016/j.ekir.2020.04.017. https://linkinghub.elsevier.com/retrieve/pii/S2468024920312195 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henry BM, De Oliveira MH, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020 Apr 10 doi: 10.1515/cclm-2020-0369. 1(ahead-of-print) [DOI] [PubMed] [Google Scholar]
- 18.Pei G, Zhang Z, Peng J, Liu L, Zhang C, Yu C, et al. Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia. J Am Soc Nephrol. 2020 doi: 10.1681/ASN.2020030276. http://www.jasn.org/lookup/doi/10.1681/ASN.2020030276 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Angel-Korman A, Brosh T, Glick K, Leiba A. [COVID-19, THE KIDNEY AND HYPERTENSION] Harefuah [Internet] 2020 Apr [cited 2020 May 17];159(4):231–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32307955 . [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joannidis M, Forni LG, Klein SJ, Honore PM, Kashani K, Ostermann M, et al. Lung–kidney interactions in critically ill patients: consensus report of the Acute Disease Quality Initiative (ADQI) 21 Workgroup. Intensive Care Med [Internet] 2020;46(4):654–72. doi: 10.1007/s00134-019-05869-7. Available from: https://doi.org/10.1007/s00134-019-05869-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions 4.2.6 [updated September 2006] The cochrane library. 2006;4(2006) [Google Scholar]
- 23.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang G, Hu C, Luo L, Fang F, Chen Y, Li J, Peng Z, Pan H. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. Journal of Clinical Virology. 2020 Apr 9:104364. doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yao Q, Wang P, Wang X, Qsie G, Meng M, Tong X, Bai X, Ding M, Liu W, Liu K, Chu Y. Retrospective study of risk factors for severe SARS-Cov-2 infections in hospitalized adult patients. Pol Arch Intern Med. 2020;130(5):390–9. doi: 10.20452/pamw.15312. [DOI] [PubMed] [Google Scholar]
- 26.Aggarwal S, Garcia-Telles N, Aggarwal G, Lavie C, Lippi G, Henry BM. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States. Diagnosis. 2020 May 26;7(2):91–6. doi: 10.1515/dx-2020-0046. [DOI] [PubMed] [Google Scholar]
- 27.Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, Zhang X, Chen H, Yu H, Zhang X. Clinical and immunologic features in severe and moderate forms of Coronavirus Disease. J Clin Invest. 2019:137244. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hong KS, Lee KH, Chung JH, Shin KC, Choi EY, Jin HJ, Jang JG, Lee W, Ahn JH. Clinical Features and Outcomes of 98 Patients Hospitalized with SARS-CoV-2 Infection in Daegu, South Korea: A Brief Descriptive Study. Yonsei Med J. 2020 May 1;61(5):431–7. doi: 10.3349/ymj.2020.61.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Y, Lu X, Chen H, Chen T, Su N, Huang F, Zhou J, Zhang B, Li Y, Yan F, Wang J. Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19. Am J Respir Crit Care Med. 2020 Apr 8(ja) doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deng Y, Liu W, Liu K, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin Med J (Engl) 2020 doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. Jama. 2020 Apr 22 doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson JG, Calfee CS. ARDS Subphenotypes: Understanding a Heterogeneous Syndrome. Crit Care. 2020;24(1) doi: 10.1186/s13054-020-2778-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Puelles VG, Lütgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, Chilla S, Heinemann A, Wanner N, Liu S, Braun F. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. 2020;383(6):590–2. doi: 10.1056/NEJMc2011400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pan X wu, Xu D, Zhang H, Zhou W, Wang L hui, Cui X gang. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. Intensive Care Med. 2020:2–4. doi: 10.1007/s00134-020-06026-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Batlle D, Soler MJ, Sparks MA, Hiremath S, South AM, Welling PA, et al. Acute Kidney Injury in COVID-19: Emerging Evidence of a Distinct Pathophysiology. J Am Soc Nephrol [Internet] 2020 May 4 doi: 10.1681/ASN.2020040419. [cited 2020 May 17];ASN.2020040419. Available from: http://www.jasn.org/lookup/doi/10.1681/ASN.2020040419 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Su H, Yang M, Wan C, Yi LX, Tang F, Zhu HY, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int [Internet] 2020 doi: 10.1016/j.kint.2020.04.003. Available from: https://doi.org/10.1016/j.kint.2020.04.003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann Intern Med. 2020 May 6 doi: 10.7326/M20-2003. doi: 10.7326/M20-2003. [Epub ahead of print]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lax SF, Skok K, Zechner P, Kessler HH, Kaufmann N, Koelblinger C, Vander K, Bargfrieder U, Trauner M. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med. 2020;173(5):350–61. doi: 10.7326/M20-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stefanini GG, Montorfano M, Trabattoni D, Andreini D, Ferrante G, Ancona M, et al. ST-Elevation Myocardial Infarction in Patients with COVID-19: Clinical and Angiographic Outcomes. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047525. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.047525 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Doyen D, Moceri P, Ducreux D, Dellamonica J. Myocarditis in a patient with COVID-19: a cause of raised troponin and ECG changes. Lancet. 2020;395(C):2020. doi: 10.1016/S0140-6736(20)30912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’’ in COVID-19.’. Journal of Infection. W.B. Saunders Ltd. 2020 doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material (Publication Bias and Meta-Regression)