Abstract
Background
There is little evidence about the utilisation of healthcare services and disease recognition in the older population, which was urged to self-isolate during the COVID-19 lockdown.
Objectives
We aimed to describe the utilisation of physician consultations, specialist referrals, hospital admissions and the recognition of incident diseases in Germany for this age group during the COVID-19 lockdown.
Design
Cross-sectional observational study.
Setting
1,095 general practitioners (GPs) and 960 specialist practices in Germany.
Subjects
2.45 million older patients aged 65 or older.
Methods
The number of documented physician consultations, specialist referrals, hospital admissions and incident diagnoses during the imposed lockdown in 2020 was descriptively analysed and compared to 2019.
Results
Physician consultations decrease slightly in February (−2%), increase before the imposed lockdown in March (+9%) and decline in April (−18%) and May (−14%) 2020 compared to the same periods in 2019. Volumes of hospital admissions decrease earlier and more intensely than physician consultations (−39 versus −6%, respectively). Overall, 15, 16 and 18% fewer incident diagnoses were documented by GPs, neurologists and diabetologists, respectively, in 2020. Diabetes, dementia, depression, cancer and stroke were diagnosed less frequently during the lockdown (−17 to −26%), meaning that the decrease in the recognition of diseases was greater than the decrease in physician consultations.
Conclusion
The data suggest that organisational changes were adopted quickly by practice management but also raise concerns about the maintenance of routine care. Prospective studies should evaluate the long-term effects of lockdowns on patient-related outcomes.
Keywords: COVID-19, older people, lockdown, healthcare utilisation, recognition
Key Points
We quantified the effect of the lockdown by comparing healthcare service utilisation and recognition of incident disease in German ambulatory care during the imposed COVID-19 lockdown in 2020 to those in 2019.
The decrease in physician consultations (−6%) was smaller than that in the recognition of incident diseases (−16%) and hospital admissions (−39%).
Physician consultations and disease recognition decrease slightly before the imposed lockdown, deteriorate tremendously during the lockdown and mitigate at the end of the lockdown.
Volumes of hospital admissions decreased at a much earlier stage and more intensely than physician consultations.
The data collected may aid policymakers in retracing the adoption of organisational changes in terms of practice management and imposed strategies and its impact on the maintenance of routine primary and specialised care during lockdowns.
Introduction
The first case of an infectious disease named COVID-19, caused by the coronavirus strain severe acute respiratory syndrome corona virus 2 (SARS-CoV-2), was reported in Wuhan, China, in December 2019 [1]. From that point, the disease spread rapidly, infecting more than 38 million individuals worldwide and causing over 1 million deaths (as of October 15, 2020) [2]. After China, Europe became the next epicentre with the number of cases skyrocketing in countries such as Italy. The mortality rate in Italy was particularly high and affected not only the population but also medical staff, especially general practitioners (GPs) [3]. A few weeks later, the number of patients in Germany affected by COVID-19 began to grow rapidly. As at 2 March 2020, Germany had more confirmed COVID-19 cases than China, and the total number of cases in the country currently stands at more than 200,000 (July 20), representing the fourth highest number in Europe behind the UK, Italy and Spain [4,5].
Emergency lockdowns were initiated across the globe to reduce the rate of infection and to prevent strain on the healthcare systems [6]. Germany imposed limitations on social contacts (contact ban) throughout the country on 22 March 2020. Social distancing was introduced to minimise close interaction between individuals and decrease individual mobility as much as possible and has since become standard practice for preventing the spread of the infection [6–8]. Consequently, gatherings of more than two people not living in the same household were prohibited. It was recommended that social distancing should continue until June 5 [4]. The timeline and related measures in response to the COVID-19 pandemic in Germany are shown in Figure 1 and Supplementary Table S1.
Figure 1 .
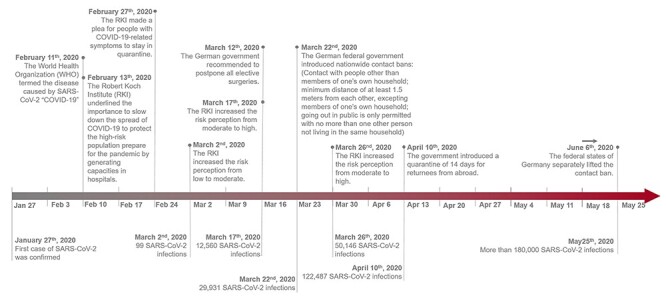
Timeline of COVID-19-related recommendations and measures in Germany.
The older population was particularly affected by these measures. This population is at a higher risk of COVID-19-related complications and death [9]. Comorbidity with hypertension, diabetes and higher body mass index is the strongest predictor of a more severe clinical course of COVID-19. Therefore, the vast majority of deaths have occurred in adults aged 65 and older [4,5,10,11]. In an attempt to shield people in this age group and thereby prevent an overburdening of the healthcare system, the older population was instructed to self-isolate and stay at home during the imposed restrictions to individual mobility and interaction with others [12].
There is limited quantitative evidence on the impact of COVID-19 and the measures imposed on the provision and utilisation of primary and secondary care services, like GPs and specialists, during lockdowns. At the beginning of the COVID-19 pandemic, primary care physicians were not well equipped to handle the new situation in their practices [13], which gave rise to considerable concerns and fears among physicians, including being virus transmitters or getting infected themselves [14]. GPs were worried about the continuity of regular care and the consequences of the COVID-19 measures and were concerned that these measures might pose a threat to the general health of the population [15]. A study by Joy et al. [16] revealed a decrease of 65% in the number of face-to-face consultations that coincided with the lockdown in the United Kingdom. Similar decreases in the utilisation of various healthcare services during the COVID-19 pandemic or others, such as SARS, have been confirmed by several other studies [17–23]. A declining consultation rate could also influence the recognition and detection of new incident diseases and could cause the deterioration of known chronic diseases to go unnoticed.
Presently, there is a lack of knowledge about the utilisation of different healthcare services and the recognition of incident diseases during the COVID-19 pandemic in primary and specialised care settings. Therefore, this study aimed to describe the utilization of primary and specialised care services, i.e. GPs and specialist consultations and referrals and hospital admissions, as well as the detection of several incident diseases in Germany during the COVID-19 pandemic.
Methods
Study design, setting and patients
This observational study was based on cross-sectional medical record data from the Disease Analyzer database (IQVIA), which compiles drug prescriptions, diagnoses and basic medical and demographic data obtained directly in anonymous format from computer systems used in the practices of GPs and specialists [24]. Diagnoses, prescriptions and the quality of reported data are monitored by IQVIA based on an array of criteria. In Germany, the sampling methods used to select physicians’ practices have been shown to be appropriate for obtaining a population-representative database of primary and specialised care [24].
The analysis included 2,447,356 patients aged 65 and older who visited at least one of 1,095 GPs and internal specialists or 960 specialist practices between January and May 2020 or January and May 2019 in Germany. The following specialist practices were included in this analysis: gynaecologists (n = 244); orthopaedists (n = 163); neurologists and psychiatrists (n = 155); ear, nose and throat physicians (ENT; n = 146); dermatologists (n = 97); urologists (n = 86) and diabetologists (n = 69). These were all available practices that routinely send data to the Disease Analyzer database (IQVIA).
Study outcomes
The main outcomes of this study were the utilisation of healthcare medical care services, represented by GP and specialist consultations (face to face, telephone or video contacts), specialist referrals (from one physician to another) and hospital admissions, and the diagnosis of incident diseases by the following: GPs and internal medicine specialists, neurologists/psychiatrists and diabetologists. The following ICD-10 diagnoses (International Statistical Classification of Diseases and Related Health Problems) were used to demonstrate the recognition of incident diseases in the different practices: dementia (F01, F03, G30 and F06.7), diabetes mellitus (E10–14), stroke including transient ischemic attack (I63, I64, G45), epilepsy (G40), Parkinson’s disease (G20, G21), depression (F32, F33), cancer (C00–C99), chronic bronchitis and chronic obstructive pulmonary disease (COPD) (J42–J44), as well as myocardial infarction (MI) (I21, I22) and coronary heart disease (I24, I25). All diagnoses had to be initial diagnoses that had not previously been documented by the practitioner to ensure that only the initial detection of incident diseases was included in this analysis.
Pre-pandemic and pandemic COVID-19 intervals in Germany considered
The utilisation of healthcare services and that of incident diseases recognised were demonstrated separately for each month during the COVID-19 pandemic. According to Holloway et al. [25], the pre-pandemic interval is characterised by an investigation of first cases and the recognition of an increased potential for ongoing transmission, corresponding to February in Germany. The pandemic interval between March and May was characterised by the initiation and acceleration of the pandemic wave. In Germany, there were less than 200 confirmed COVID-19 cases at the end of February (pre-pandemic interval), but 50,000, 125,000 and 180,000 cases at the end of March, April and May (pandemic interval), respectively. The number of confirmed cases per day peaked at the beginning of April (6,561 new cases/day). A downward trend was then recorded, with just 178 confirmed cases per day at the end of May.
Statistical analyses
We used descriptive statistics to map the utilisation of healthcare services and recognition of incident diseases during the COVID-19 pandemic in Germany. In order to assess the changes in the utilisation of healthcare services and the recognition of incident diseases, we compared the results for 2020 with those for the corresponding periods 1 year before (February–May 2019) and calculated the percentage change between 2019 and 2020. Special circumstances in 2019, such as the wave of influenza that was averted in 2020, may bias the results of this analysis. We therefore included a sensitivity analysis that compares the outcomes of 2020 with the monthly average of the years 2017–2019. The reporting of the results followed the STROBE guidelines [26]. Analyses were carried out using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Results
Patient characteristics
Patients were an average of 76.5 (standard deviation 8.4) years old. The majority was female (53.1%). More than one third of patients were suffering from diabetes (41%), ischemic heart disease (39%) and depression (32%), respectively. While there were no significant differences in age, patients treated in 2020 were significantly more likely to be male (48.1 versus 46.9%, P < 0.001) than those treated in 2019.
Changes in the utilisation of healthcare services during the COVID-19 pandemic
The number of physician consultations was between ±0 and −7% lower in February 2020 than in the same period in 2019. The decrease in consultations worsened in March (up to −18%) and April (up to −40%), but this decrease was mitigated in May (up to −23%). The utilisation of physicians across the entire period decreased by 6% overall. The smallest decrease was found for diabetologists (−1%), GPs (−4%) and neurologists/psychiatrists (−5%), the largest for ENT specialists (−21%). The magnitude of the decline in consultation rates varied over time and specialty. While consultations decreased for most specialist groups, there was a moderate increase in GP (+15%), psychiatrist/neurologist (+13%) and diabetologist (+12%) consultations in March, shortly before lockdown measures were introduced. During the contact ban, the relative change in consultations from 2019 to 2020 was −15% for GPs, −18% for neurologists/psychiatrists and −10% for diabetologists. The largest decrease in consultations was found for ENT specialists in April (−40%).
The overall volume of referrals from one physician to another also decreased slightly in February 2020 compared to the corresponding period in 2019 (up to −15%), followed by a sharp downturn in March (up to −27%) and April (up to −48%), and a slight recovery in May (up to −21%). Specialist referrals decreased by −20% from February to May across all practices. At the beginning of the COVID-19 pandemic in February in Germany, only the number of referrals by gynaecologists (+6%) and urologists (+5%) increased; a steady decrease in referrals was documented for all other specialists, which again was largest for ENT specialists (−48%) in April 2020, compared to the corresponding months in 2019.
Hospital admissions also decreased, but much earlier and more intensely (−39% overall). In February 2020, hospital admissions decreased by up to −32% with the lowest values documented for GPs and internal specialist practices. Again, only ENT specialists demonstrated a diverging trend with an increase of 3% in hospitalisations in February 2020 compared to 2019. During the peak of the COVID-19 pandemic in March and April, hospital admissions decreased by up to −64% compared to 2019. In line with the number of consultations and specialist referrals, there was a slight alleviation in May 2020 (up to −50%). However, the level of hospital admissions remained between −28 and −50%. Table 1 and Figure 2 show the utilisation of healthcare services in medical practices.
Table 1 .
Utilisation of healthcare services during the COVID-19 pandemic in Germany in 2020 compared to corresponding periods in 2019
| Pre-pandemic intervala | Pandemic intervala | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Februaryb | Marchc | Aprild | Maye | ∑f | |||||||||
| Utilisation of healthcare services, n (%) | 2019 | 2020 | Diff. (%) | 2019 | 2020 | Diff. (%) | 2019 | 2020 | Diff. (%) | 2019 | 2020 | Diff. (%) | Diff. (%) |
| Numbers (n) in thousands | |||||||||||||
| Number of consultations | |||||||||||||
| GPs, internal medicine specialists | 592.4 | 579.7 | -2% | 603.6 | 691.1 | +15% | 643 | 549 | −15% | 632 | 544 | −14% | −4% |
| Orthopaedists | 53.0 | 52.6 | −1% | 52.8 | 45.8 | −13% | 55.1 | 37.8 | −31% | 57.4 | 46.3 | −19% | −16% |
| Diabetologists | 29.0 | 29.0 | 0% | 29.1 | 32.1 | +12% | 31.0 | 28.0 | −10% | 30.3 | 28.0 | −8% | −1% |
| Psychiatrists/neurologists | 32.9 | 32.7 | −1% | 32.6 | 36.7 | +13% | 34.9 | 28.7 | −18% | 35.0 | 31.0 | −12% | −5% |
| Urologists | 32.5 | 32.2 | −1% | 31.8 | 31.8 | 0% | 32.0 | 26.1 | −18% | 33.7 | 29.3 | −13% | −8% |
| Dermatologists | 32.0 | 29.9 | −7% | 33.1 | 28.6 | −14% | 31.4 | 21.0 | −33% | 32.8 | 27.1 | 17% | −18% |
| ENT specialists | 29.8 | 28.8 | −4% | 29.5 | 24.1 | −18% | 29.3 | 17.7 | −40% | 29.8 | 23.1 | −23% | −21% |
| Gynaecologists | 16.3 | 16.1 | −1% | 16.6 | 16.0 | −4% | 16.2 | 11.8 | −27% | 17.7 | 14.3 | −19% | −13% |
| Specialists referrals | |||||||||||||
| GP, internal medicine specialists | 76.1 | 70.4 | −7% | 63.6 | 50.8 | −20% | 104.5 | 68.7 | −34% | 79.3 | 67.9 | −14% | −20% |
| Orthopaedists | 7.7 | 7.5 | −3% | 7.2 | 5.5 | −24% | 8.9 | 5.3 | −40% | 8.4 | 6.9 | −17% | −22% |
| Diabetologists | 6.1 | 5.7 | −6% | 5.2 | 4.3 | −16% | 7.8 | 5.0 | −36% | 6.3 | 5.0 | −21% | −21% |
| Psychiatrists/neurologists | 1.9 | 1.9 | +1% | 1.8 | 1.3 | −23% | 2.3 | 1.4 | −40% | 2.1 | 1.7 | −21% | −22% |
| Urologists | 5.5 | 5.1 | −5% | 5.7 | 4.8 | −16% | 5.4 | 4.0 | −26% | 5.6 | 4.1 | −10% | −14% |
| Dermatologists | 5.2 | 5.0 | −5% | 5.1 | 4.4 | −14% | 5.2 | 3.1 | −39% | 5.3 | 4.4 | −18% | −19% |
| ENT specialists | 2.4 | 1.9 | −15% | 1.9 | 1.4 | −27% | 2.5 | 1.3 | −48% | 2.3 | 1.8 | −21% | −28% |
| Gynaecologists | 3.8 | 4.0 | +6% | 3.3 | 3.1 | −7% | 4.7 | 2.8 | −41% | 4.1 | 3.8 | −8% | −14% |
| Hospital admissions | |||||||||||||
| GP, internal medicine specialists | 8.3 | 5.7 | −32% | 7.9 | 4.4 | −43% | 9.1 | 4.9 | −46% | 8.3 | 4.5 | −46% | −45% |
| Orthopaedists | 1.2 | 1.0 | −14% | 1.1 | 0.7 | −36% | 1.1 | 0.6 | −51% | 1.1 | 0.8 | −30% | −32% |
| Diabetologist | 0.6 | 0.4 | −29% | 0.6 | 0.3 | −49% | 0.6 | 0.4 | −39% | 0.6 | 0.3 | −50% | −42% |
| Psychiatrists/neurologists | 0.5 | 0.4 | −19% | 0.4 | 0.2 | −46% | 0.5 | 0.2 | −52% | 0.5 | 0.3 | −42% | −40% |
| Urologists | 1.0 | 0.8 | −18% | 0.9 | 0.6 | −29% | 1.1 | 0.6 | −41% | 1.0 | 0.7 | −28% | −29% |
| Dermatologists | 0.2 | 0.2 | −14% | 0.2 | 0.1 | −51% | 0.3 | 0.1 | −64% | 0.3 | 0.2 | −45% | −45% |
| ENT specialists | 0.3 | 0.3 | +3% | 0.3 | 0.2 | −24% | 0.4 | 0.2 | −44% | 0.4 | 0.2 | −34% | −26% |
| Gynaecologists | 0.3 | 0.2 | −19% | 0.2 | 0.2 | −5% | 0.3 | 0.1 | −55% | 0.3 | 0.2 | −34% | −31% |
aAccording to Holloway et al. [25].
bFebruary: less than 200 SARS-CoV-2 infections.
c50,000 at the end of March.
d125,000 at the end of April.
eMore than 180,000 at the end of May.
fFebruary–May.
Figure 2 .
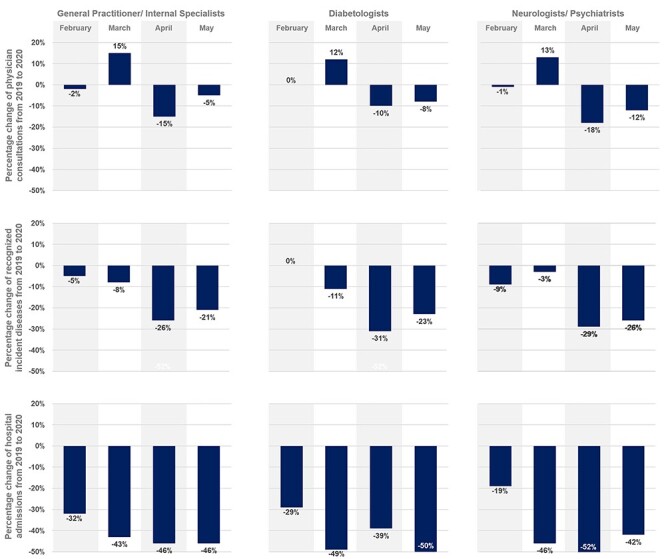
Overview of healthcare services utilised and incident diseases detected during the COVID-19 pandemic in Germany in 2020 compared to 2019.
Recognition of incident diseases
The number of incident diseases recognised decreased in February 2020. Diagnoses documented by GPs and internal medicine specialists decreased by up to −11% (MI) in February 2020. However, and in contrast to the general downward trend, chronic heart diseases (+2%), stroke (+5%), diabetes (+13%) and dementia (+2%) were detected more frequently in February and March 2020 compared to 2019. The decreased number of incident diseases diagnosed remained stable until the end of March, with a nadir of −11% (depression), shortly before the contact ban was introduced. However, the recognition of incident diagnoses decreased significantly in April (up to −38%) and also in May (up to −32%), although the figure for May indicated a slightly smaller decrease. In an analysis for specific diseases, dementia (−38%), diabetes (−38%), stroke (−38%) and Parkinson’s (−32%) were diagnosed less often in April and May 2020 than in the corresponding months in 2019. Over the entire period, the number of incident diseases detected decreased by 15, 16 and 18% at GPs and internal specialists, neurologists/psychiatrists and diabetologist practices, respectively. Thus, the recognition of incident diseases decreased more intensely than the frequency of consultations (versus −5, −6 and −2%, respectively). Table 2 and Figure 2 represent the change in the detection of different incident diseases.
Table 2 .
Recognition of incident diseases during the COVID-19 pandemic in Germany in 2020 compared to 2019
| Recognised incident disease, n (%) | Pre-pandemic intervala | Pandemic intervala | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Februaryb | Marchc | Aprild | Maye | ∑ f | |||||||||
| 2019 | 2020 | Diff. (%) | 2019 | 2020 | Diff. (%) | 2019 | 2020 | Diff. (%) | 2019 | 2020 | Diff. (%) | Diff. (%) | |
| GP, internal medicine specialists | |||||||||||||
| Diabetes | 2,892 | 2,719 | −6% | 2,957 | 2,703 | −9% | 2,919 | 2,027 | −31% | 2,690 | 2,025 | −25% | −17% |
| Cancer | 2,321 | 2,140 | −8% | 2,333 | 2,106 | −10% | 2,539 | 1,853 | −27% | 2,330 | 1,885 | −19% | −16% |
| Coronary heart disease | 2,047 | 2,078 | 2% | 2,127 | 1,964 | −8% | 2,205 | 1,644 | −25% | 1,956 | 1,536 | −21% | −13% |
| Dementia | 1,467 | 1,383 | −6% | 1,561 | 1,429 | −8% | 1,710 | 1,380 | −19% | 1,544 | 1,254 | −19% | −13% |
| COPD | 1,636 | 1,498 | −8% | 1,659 | 1,519 | −8% | 1,607 | 1,067 | −34% | 1,358 | 956 | −30% | −19% |
| Depression | 1,484 | 1,427 | −4% | 1,607 | 1,438 | −11% | 1,668 | 1,271 | −24% | 1,505 | 1,260 | −16% | −14% |
| Acute stroke | 711 | 667 | −6% | 723 | 757 | 5% | 765 | 621 | −19% | 668 | 587 | −12% | −8% |
| Myocardial infarction | 429 | 381 | −11% | 402 | 393 | −2% | 441 | 377 | −15% | 367 | 319 | −13% | −10% |
| Psychiatrists/neurologists | |||||||||||||
| Dementia | 768 | 690 | −10% | 612 | 627 | 2% | 730 | 449 | −38% | 718 | 529 | −26% | −19% |
| Depression | 726 | 668 | −8% | 626 | 598 | −4% | 549 | 445 | −19% | 597 | 457 | −23% | −13% |
| Parkinson | 238 | 230 | −3% | 202 | 188 | −7% | 187 | 160 | −14% | 214 | 164 | −32% | −15% |
| Epilepsy | 183 | 169 | −8% | 158 | 172 | 9% | 170 | 120 | −29% | 148 | 115 | −22% | −13% |
| Acute stroke | 126 | 109 | −13% | 138 | 104 | −25% | 113 | 70 | −38% | 122 | 87 | −29% | −26% |
| Diabetologists | |||||||||||||
| Diabetes | 655 | 742 | +13% | 668 | 637 | −5% | 593 | 367 | −38% | 582 | 467 | −20% | −11% |
aAccording to Holloway et al. [25].
bFebruary: less than 200 confirmed SARS-CoV-2 infections.
c50,000 at the end of March.
d125,000 at the end of April.
eMore than 180,000 at the end of May.
fFebruary–May.
Sensitivity analysis
The sensitivity analysis revealed the same results and tendencies as the base case analysis. By comparing 2020 with the average of 2017–2019 for each month separately, the decrease of consultations, specialists’ referrals and hospital admissions were slightly lower, especially due to a slight increase of the outcomes in February, the months before the lockdown. The sensitivity analysis is represented in Supplementary Tables S2 and S3.
Discussion
This analysis provides valuable information on the utilisation of healthcare services and the recognition of incident diseases in primary and specialised care settings during the COVID-19-related lockdown, demonstrating a tremendous decrease during this period. Physician consultations, specialist referrals and hospital admissions decreased slightly in February, worsened in March and April and recovered slightly in May 2020, coinciding with the upward and downward trends in the number of confirmed COVID-19 cases in Germany. While volumes of hospital admissions decreased earlier and more intensely than physician consultations and specialist referrals, there was only a slight decrease in the number of incident diseases diagnosed in February, and this figure remained stable until the end of March before dropping tremendously in April and May. However, the decrease in the detection of incident diseases was larger than that in the utilisation of GP and specialist consultations. These results were consistent with those from the sensitivity analyses, demonstrating the robustness of our findings.
A number of studies have evaluated the impact of the COVID-19 pandemic on the utilisation of hospital services [17,19–21,27], demonstrating, in line with this study, a remarkable reduction of hospital service capacities. It seems that hospitals immediately followed the government’s recommendation to prepare for the pandemic by generating emergency and, particularly, mechanical ventilation capacities announced in mid-February 2020. However, less is known about the utilisation of physician services during the pandemic. Lu et al. [22] reported a significant drop of up to −53% in the utilisation of physician services during the SARS outbreak and showed that this decrease was smaller than that in the utilisation of inpatient hospital care services, which reached up to −82%. These tendencies are in line with the findings of this study, demonstrating that the utilisation of services by physicians dropped by up to 40%, while hospital admissions declined considerably more (up to −64%). However, the decline in the utilisation of physician services and the number of specialist referrals issued was still more pronounced during the peak of the COVID-19 pandemic in Germany. The pandemic required organisational adjustments within physicians’ practices to prevent the transmission and spread of COVID-19 [28]. Verhoeven et al. [15] highlighted that organisational changes in practice management and consultation strategies were quickly adopted in Belgium, with a major switch towards telephone triage and telemedical consultations for COVID-19-related and non-COVID-related problems. This was confirmed by Mangiapane et al. [29], who demonstrated that the utilisation of new services such as remote telephone and video consultation increased considerably in Germany and that nearly 1 million additional consultations were held for the medical evaluation of COVID-19-related symptoms as recommended by the German College of General Practitioners and Family Physicians.
Furthermore, GPs thought that they were at a higher risk of contracting SARS-CoV-2 themselves, with the effect that they would be quarantined and would subsequently no longer be able to maintain primary care. Even more than getting ill themselves, GPs were concerned that they might become virus transmitters and put their patients at risk [15]. These are all good arguments in favour of the absolute necessity of reducing the number of consultations, ideally by cancelling or postponing unnecessary treatments and consultations. These concerns are also reflected in the results of the present study. We found the largest decrease in consultations and referrals issued for ENT specialists, who are exposed to a higher risk of becoming transmitters of the virus due to the nature of treatments of the throat and upper airways, the areas where the highest virus load is found. Furthermore, at the beginning of the pandemic, the German College of General Practitioners and Family Physicians recommend treating patients with serious illnesses or infections in hospitals and not in ambulatory practices, separating infected from the non-infected patients in physician practices, avoiding or postponing unnecessary treatments in the practices and reducing home visits, especially nursing home visits [30]. Such organisational adjustments automatically lead to reduced consultation rates and treatment capacities.
However, the demonstrated decrease is not only caused by organisational adjustments according to the recommendations for practices and the perception and burden of the physician specialists. Patients themselves have likely promoted decreasing trends. The acceleration of COVID-19 cases in China in December 2019 and Italy in January 2020 was widely reported in the worldwide press. When the first studies reported that older people are at a higher risk of complications in the clinical course of COVID-19 and are more likely to die [9,31], the older population became aware and very concerned about the seriousness of the situation. Betsch [32] revealed that more than 70% of the population were (very) concerned about COVID-19 at the beginning of March and hence very early on in the COVID-19 pandemic. Therefore, it can reasonably be assumed that the sharp and unprecedented decrease was caused by patients’ and physicians’ concerns, in combination with the organisational adjustments of the healthcare sector.
Kostev et al. [33] furthermore demonstrated that the prescription rate of cardiovascular and diabetes therapies increased significantly before the COVID-19 lockdown in Germany and that the increase was largest for the age group 18–40 years and smallest in patients aged 80 years or older. The tremendous decrease in April and May in our analysis is likely not generalisable to the entire population, including the younger population. However, receiving less likely continued treatments and diagnoses of incident diseases could have a significant impact on the health of older populations. Therefore, further research is needed to reveal whether or not and if yes how intensively the older population was more severely affected by the COVID-19 pandemic.
However, the decrease in the recognition of incident diseases was twice as large as the decrease in the utilisation of GPs and specialists, demonstrating a significant risk of late diagnoses and consequently delayed initiation of evidence-based treatment and care, which could result in adverse patient-related outcomes. Mangiapane et al. [29] demonstrated that remote telephone and video consultation increased considerably in Germany during the lockdown. Such consultations were included in our analyses as well. It can be assumed that the reduced consultation rate in combination with a higher percentage of remote telephone or video consultation makes it more difficult for practitioners to detect new incident diseases as compared to the common and in-person face-to-face consultations. However, it remains to be seen whether the downturn in the detection of incident diseases will be partly compensated for by an upturn later this year or whether it will result in adverse patient-related outcomes such as higher levels of disease-specific hospitalisation or mortality rates. Further research is needed to analyse the possible compensatory effects and their impact on important patient-specific outcomes. Given the possibility of a second pandemic wave, strategic considerations are urgently needed regarding how to implement a strategy to maintain diagnosis, treatment and care for the older population during lockdowns. This includes the conditions experienced by older people during the pandemic, characterised by social isolation, which could cause additional serious mental health problems [12,34]. Therefore, further research is needed to analyse the upcoming consequences of COVID-19 social distancing measures. Evidence should be used to guide governmental action in mitigating the mental and physical health consequences of the COVID-19 lockdown.
Limitations
The data documentation may be less accurate than usual due to the organisational challenges faced by physician practices and the circumstances during the COVID-19 pandemic. Moreover, it is not possible to assess the extent to which emergency, urgent and deferrable services have been provided within the available diagnostic categories. This considerably limits an assessment of whether the appropriate priorities for diagnosis and treatment strategies have been followed in the individual medical practices in view of the high-risk situation and the lockdown. In addition, special circumstances in 2019, such as the wave of influenza that was averted in 2020, may have biased the results. Finally, the database does not allow for the establishment of a patient-related connection between different specialists. Therefore, double reporting of patients’ diagnoses cannot be precluded.
Conclusion
COVID-19 poses novel challenges for global primary and secondary care provided by GPs and specialists, maintaining routine care of multimorbid older patients to avoid deterioration of health status as well as excess morbidity and mortality. The novel and COVID-19-related challenges required organisational changes in practice management and consultation strategies that aimed to avoid or postpone unnecessary consultations, especially with older patients who are most at risk of COVID-19, and to increase remote telephone and video consultation. As a result, physician consultations, specialist referrals and hospital admissions decreased tremendously during the COVID-19 lockdown. In particular, the decrease in the detection of incident diseases was larger than the consultation rate, probably caused by a tremendous increase in the proportion of remote telephone and video compared to in-person consultations during the lockdown. It is of vital importance to analyse compensatory effects, like an increased consultation and disease detection rate, probably emerging subsequently after COVID-19-related lockdowns, as well as long-term effects of the altered utilisation and disease detection rate in the older population.
Supplementary Material
Contributor Information
Bernhard Michalowsky, German Center for Neurodegenerative Diseases (DZNE) Site Rostock/Greifswald, Greifswald D-17487, Germany.
Wolfgang Hoffmann, German Center for Neurodegenerative Diseases (DZNE) Site Rostock/Greifswald, Greifswald D-17487, Germany; Section Epidemiology of Health Care and Community Health, Institute for Community Medicine, University Medicine Greifswald (UMG), Greifswald D-17487, Germany.
Jens Bohlken, Institute for Social Medicine, Occupational Medicine, and Public Health (ISAP) of the Medical Faculty, University of Leipzig, Leipzig, Germany.
Karel Kostev, Epidemiology, IQVIA, Frankfurt am Main 60549, Germany.
Declaration of Sources of Funding
None.
Declaration of Conflicts of Interest
None.
References
- 1. Wu P, Hao X, Lau EHY et al. Real-time tentative assessment of the epidemiological characteristics of novel coronavirus infections in Wuhan, China, as at 22 January 2020. Euro Surveill 2020; 25: 2000044. doi: 10.2807/1560-7917.ES.2020.25.3.2000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lapolla P, Mingoli A, Lee R. Deaths from COVID-19 in healthcare workers in Italy-what can we learn? Infect Control Hosp Epidemiol 2020; 1–2. doi: 10.1017/ice.2020.241. Epub ahead of print. PMID: 32408922; PMCID: PMC7256220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. R.K.I . COVID-19-Dashboard, 2020. Berlin: Robert Koch Institute.
- 5.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis; 20: 533–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chu DK, Akl EA, Duda S et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020; 395: 1973–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Glass RJ, Glass L, Beyeler W, Min H. Targeted social distancing design for pandemic influenza. Emerg Infect Dis 2006; 12: 1671–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med 2020; 27: taaa020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lian J, Jin X, Hao S et al. Analysis of epidemiological and clinical features in older patients with coronavirus disease 2019 (COVID-19) outside Wuhan. Clin Infect Dis 2020; 71: 740–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen Q, Zheng Z, Zhang C et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection 2020; 48: 543–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lithander FE, Neumann S, Tenison E et al. COVID-19 in older people: a rapid clinical review. Age Ageing 2020; 49: 501–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health 2015; 105: 1013–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Paffenholz P, Peine A, Hellmich M et al. Perception of the 2020 SARS-CoV-2 pandemic among medical professionals in Germany: results from a nationwide online survey. Emerg Microbes Infect 2020; 9: 1590–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bohlken J, Schömig F, Seehagen T et al. Experience of practice-based psychiatrists and neurologists during the COVID-19 pandemic. Psychiatr Prax 2020; 47: 214–7. [DOI] [PubMed] [Google Scholar]
- 15. Verhoeven V, Tsakitzidis G, Philips H, van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open 2020; 10: e039674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Joy M, McGagh D, Jones N et al. Reorganisation of primary care for older adults during COVID-19: a cross-sectional database study in the UK. Br J Gen Pract 2020; 70:e540–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Houshyar R, Tran-Harding K, Glavis-Bloom J et al. Effect of shelter-in-place on emergency department radiology volumes during the COVID-19 pandemic. Emerg Radiol 2020; 27: 781–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Turan Ç, Metin N, Utlu Z, Öner Ü, Kotan ÖS Change of the diagnostic distribution in applicants to dermatology after COVID-19 pandemic: what it whispers to us? Dermatol Ther 2020; 33: e13804. 10.1111/dth.13804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kenyon CC, Hill DA, Henrickson SE, Bryant-Stephens TC, Zorc JJ. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract 2020; 8: 2774–6.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoyer C, Ebert A, Szabo K, Platten M, Meyer-Lindenberg A, Kranaster L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci 2020; 9: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guo H, Zhou Y, Liu X, Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci 2020. doi: 10.1016/j.jds.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lu TH, Chou YJ, Liou CS. Impact of SARS on healthcare utilization by disease categories: implications for delivery of healthcare services. Health Policy 2007; 83: 375–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen TJ, Lin MH, Chou LF, Hwang SJ. Hospice utilization during the SARS outbreak in Taiwan. BMC Health Serv Res 2006; 6: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rathmann W, Bongaerts B, Carius HJ, Kruppert S, Kostev K. Basic characteristics and representativeness of the German disease Analyzer database. Int J Clin Pharmacol Ther 2018; 56: 459–66. [PubMed] [Google Scholar]
- 25. Holloway R, Rasmussen SA, Zaza S, Cox NJ, Jernigan DB. Updated preparedness and response framework for influenza pandemics. MMWR Recomm Rep 2014; 63: 1–18. [PubMed] [Google Scholar]
- 26. von Elm E, Altman DG, Egger M et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Haffer H, Schömig F, Rickert M et al. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery in university hospitals in Germany: results of a nationwide survey. J Bone Joint Surg Am 2020; 102: e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blankenfeld, H.K., Kochen, M., Pömsl, J., Neues Coronavirus (SARS-CoV-2)–Informationen für die hausärztliche, Praxis: DEGAM S1-Handlungsempfehlung. Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM), Editor 2020. [Google Scholar]
- 29. Mangiapane SZL, Czihal T, von Stillfried D. Veränderung der vertragsärztlichen Leistungsinanspruchnahme während der COVID-Krise - Tabellarischer Trendreport für das 1. Quartal 2020. Berlin: Zentralinstitut für die kassenärztliche Versorgung in Deutschland, 2020. [Google Scholar]
- 30. (DEGAM), Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin . S1-Handlungsempfehlung: Neues Coronavirus – Informationen für die hausärztliche Praxis. 2020. https://www.awmf.org/leitlinien/detail/ll/053-054.html. 2020 (accessed 31 July 2020).
- 31. Ji M, Yuan L, Shen W et al. A predictive model for disease progression in non-severely ill patients with coronavirus disease 2019. Eur Respir J. 2020; 56: 2001234. doi: 10.1183/13993003.01234-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Betsch, C., Ergebnisse aus dem COVID-19 Snapshop Monitoring COSMO: Die psychologische Lage. https://projekte.uni-erfurt.de/cosmo2020/archiv/, University of Erfurt, Editor 2020. (accessed 31 July 2020).
- 33. Kostev K, Kumar S, Konrad M, Bohlken J. Prescription rate of cardiovascular and diabetes therapies prior to and during the COVID-19 lockdown. Int J Clin Pharmacol Ther 2020;58: 475–81. [DOI] [PubMed] [Google Scholar]
- 34. Santini ZI, Jose PE, York Cornwell E et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health 2020; 5: e62–70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


