Abstract
Background
The Functional Comorbidity Index (FCI) was developed for community-based adult populations, with function as the outcome. The original FCI was a survey tool, but several International Classification of Diseases (ICD) code lists—for calculating the FCI using administrative data—have been published. However, compatible ICD-9-CM and ICD-10-CM versions have not been available.
Objectives
We developed ICD-9-CM and ICD-10-CM diagnosis code lists to optimize FCI concordance across ICD lexicons.
Research Design
We assessed concordance and frequency distributions across ICD lexicons for the FCI and individual comorbidities. We used length of stay and discharge disposition to assess continuity of FCI criterion validity across lexicons.
Subjects
State Inpatient Databases (SID) from Arizona, Colorado, Michigan, New Jersey, New York, Utah, and Washington State (calendar year 2015) were obtained from the Healthcare Cost and Utilization Project. SID contained ICD-9-CM diagnoses for the first 3 calendar quarters of 2015, and ICD-10-CM diagnoses for the fourth quarter of 2015. Inpatients under 18 years old were excluded.
Measures
Length of stay and discharge disposition outcomes were assessed in separate regression models. Covariates included age, gender, state, ICD lexicon, and FCI/lexicon interaction.
Results
The FCI demonstrated stability across lexicons, despite small discrepancies in prevalence for individual comorbidities. Under ICD-9-CM, each additional comorbidity was associated with an 8.9% increase in length of stay and an 18.5% decrease in the odds of a routine discharge, compared to an 8.4% increase and 17.4% decrease, respectively, under ICD-10-CM.
Conclusions
This study provides compatible ICD-9-CM and ICD-10-CM diagnosis code lists for the FCI.
Keywords: Functional Comorbidity Index, comorbidity, risk adjustment, International Classification of Diseases, health status
INTRODUCTION
Measuring health conditions using administrative claims data and electronic health records is important for health services research and risk adjustment methods. Comorbid health conditions are associated with mortality and hospital readmissions in general clinical populations,1, 2 as well as with more specific clinical outcomes such as function for people with chronic back pain3 and osteoarthritis.4 The number of comorbid health conditions is also associated with the type, amount, and cost of health care services that people receive.1, 2, 5 Comorbidity burden can be an important confounder in outcomes research, and it is one important factor that payers may use to account for differences in case-mix when adjusting payments to providers.6 Deriving comorbidity measures from administrative claims data and electronic health records is advantageous because it allows for more automated and widespread collection of comorbidity burden, and several validated comorbidity indices using these types of data have been published.1, 2, 7–9
In the United States, health care systems switched from ICD-9-CM codes to ICD-10-CM codes as of October 1, 2015. Using comorbidity indices with consistent performance across this ICD-9-CM to ICD-10-CM transition is crucial for researchers conducting longitudinal studies, studies involving surveillance of health conditions over time, or outcome studies for which comorbidity may be a confounder. The transition in coding lexicon presents a challenge when using comorbidity indices based on diagnosis codes in administrative data, due to differences in number and organization of codes, changes in diagnosis definitions, and changes in coding and billing practices.
The Functional Comorbidity Index (FCI) is a unique comorbidity measure, in that it was developed with function as the outcome.10 The FCI was originally developed as a survey tool, but several International Classification of Diseases (ICD) code lists—for calculating the FCI using administrative data—have since been published. Various ICD versions have been used to calculate the FCI based on administrative/billing data in acute, post-acute, outpatient, and workers’ compensation settings.3, 11–15 We are aware of one published ICD-10-AM (Australian Modification) version of the FCI, but are unaware of any published ICD-10-CM version.16 In addition, existing ICD diagnosis code lists for the FCI are variable with regard to (1) interpretation of the breadth and focus of each comorbidity category and (2) the specific codes included in each category. There is a pressing need to develop, harmonize and test ICD-9-CM and ICD-10-CM versions of the FCI for consistency, in order to have reliable and valid measures of comorbidity across the ICD lexicon transition.
In this project, we developed updated FCI diagnosis code lists based on both ICD-9-CM and ICD-10-CM diagnoses, with the goal of optimizing concordance across ICD lexicons in order to facilitate (1) measurement continuity across the lexicon change and (2) use of administrative data sets involving both lexicons. We assessed concordance and frequency distributions across ICD lexicons for the FCI and for individual comorbidities. We also used short-term inpatient outcomes (length of stay and discharge disposition) to assess continuity of criterion validity across ICD lexicons.
METHODS
Data Source
A convenience sample of 7 distinct population-based state hospital discharge databases, representing diverse geographic areas, were used for this study. Hospital discharge data from Arizona, Colorado, Michigan, New Jersey, New York, Utah, and Washington State were obtained from the State Inpatient Databases (SID), Healthcare Cost and Utilization Project (HCUP).17 The SID contain nearly all community hospital discharges for the respective states. SID data for 2015 were available to us, having been purchased for another study (data re-use was approved by HCUP). The ICD-10-CM lexicon took effect on October 1, 2015.18 The SID diagnosis fields contained diagnoses based on the ICD-9-CM lexicon for the first 3 calendar quarters of 2015; the ICD-10-CM lexicon was used for the fourth calendar quarter of 2015. Inpatients under 18 years old were excluded because the FCI was developed for adult populations. All available diagnosis fields for each hospitalization were used to identify comorbidities—the most sensitive approach. The number of diagnosis fields did not vary across the 4 quarters within each state, but did vary across states (Arizona, New Jersey, New York, and Washington State had 25; Colorado and Michigan had 30; Utah had 21). Although this project did not involve individually identifiable human subjects, it was conducted under the parent study approved by the University of Washington Institutional Review Board.
Functional Comorbidity Index
The FCI was originally developed as an unweighted index of 18 self-reported chronic conditions.10 It was developed to predict functional outcomes in community-based adult populations, rather than the outcomes for which comorbidity indices are typically developed: mortality, hospital length of stay, charges, or costs among inpatient populations.1, 2, 19, 20 Many of the chronic conditions in the FCI are not included in other comorbidity indices; they were selected based on their theorized association with functional status, through a process involving literature review and a series of focus groups conducted among patients and health care professionals.10 The FCI was further developed and tested using a randomly sampled Canadian survey of noninstitutionalized adults, the Canadian Multi Centre Osteoporosis Study (N=9,423) and a U.S. database of patients with spine conditions from the National Spine Network (N=28,348).10 It is commonly used as an additive index, but a weighted index or a set of indicators for individual comorbidities may perform better in some circumstances.10, 21, 22
Development
Our goal during the development process was to optimize concordance between the ICD-9-CM and ICD-10-CM code lists—minimizing discrepancies in capture of individual comorbidities and FCI counts across the two lexicons. The FCI code lists presented herein were developed by the co-authors. JMS is a registered nurse with a doctorate in health services research and over 20 years of experience with ICD coding for research and clinical purposes; her expertise includes surveillance methodology and use of administrative billing data to develop various prevalence and trend metrics based on ICD and other coding lexicons. SDR is a licensed physical therapist and epidemiologist; he has led several research projects assessing/validating the FCI and comparing the FCI to other risk adjustment tools.
We started with published FCI code lists, including the ICD-9-CM code lists developed by Kumar et al (2016),11 and the ICD-10-AM code list developed by Gabbe et al (2013).16 We also obtained unpublished ICD-9-CM and ICD-10-CM code lists used by Marcum et al (2018).14 Where there were discrepancies between these existing lists, we used Groll et al (2005)10 to guide decisions based on original intent, scope, and FCI category descriptions. We also reviewed the FCI-related literature (including later articles co-authored by Groll23–25) to check for conceptual/definitional drift or refinement. For the stroke category, we relied heavily on the American Heart Association/American Stroke Association expert consensus document.26 We reviewed Charlson and Elixhauser ICD-9-CM and ICD-10 comorbidity code lists published by Quan et al (2005),9 and added codes as indicated. However, the FCI focus on chronic conditions was intentionally maintained; i.e., acute comorbidity codes on the Charlson and Elixhauser lists were not added. During this process, we avoided expanding or modifying category definitions where feasible. We aimed to optimize concordance between codes included on the ICD-9-CM and ICD-10-CM lists, in order to facilitate (1) measurement continuity across the lexicon change and (2) use of data sets involving both lexicons. Using ICD coding and mapping manuals,27–29 as well as the American Academy of Professional Coders (AAPC) online code converter,30 we translated and back-translated all codes between ICD-9-CM and ICD-10-CM to identify potential discrepancies, and made adjustments to ensure concordance across lexicons.
We used two internal data sets for development purposes, to assess concordance and identify inconsistencies in coding and code translation: (1) adult inpatients in Washington State, dual-coded by hospital coders in 2014 (N=2,351), and (2) a set of Washington State workers’ compensation data for allowed work-related conditions (N=6,528). The latter data set was not technically dual-coded, but included ICD diagnoses using both ICD lexicons, because this subset of workers’ compensation claims had remained open across the lexicon change, and codes in the alternate lexicon were either autofilled using computer algorithms or coded by hand. Neither data set allowed for assessment of the full range of FCI comorbidities. Hearing impairment was not fully coded in the former data set. The latter data set consisted of conditions accepted for workers’ compensation coverage as a direct result of—or related to recovery from—the work injury, and had very low prevalence of FCI comorbidities other than back disease, arthritis, anxiety, and depression. However, among those individual comorbidities having adequate prevalence, kappa values for most individual comorbidities were well above 0.81 (considered almost perfect agreement31), and kappa values for the FCI counts were 0.83 (SE 0.01; FCI ranged 0 to 10) for the inpatient data set and 0.85 (SE 0.01; FCI ranged 0 to 3) for the workers’ compensation data set. One notable exception was the angina category, which had a kappa value of only 0.30 (considered fair agreement31) in the inpatient data set (there too few cases to test angina using the workers’ compensation data set). This was primarily due to cases that were coded as angina using ICD-9-CM but as congestive heart failure or heart disease using ICD-10-CM (because the ICD-10-CM codes I25.11× and I25.7× included angina together with other heart disease diagnoses). We did not make further code list changes to improve cross-lexicon concordance for angina, because there was no apparent way to improve concordance for the angina category without degrading concordance for the heart disease category, or without violating our decision rules, which included not listing the same diagnosis code in more than one FCI category. Kappa and related statistics are provided for these analyses in Supplemental Table S1 (Supplemental Digital Content 1, http://links.lww.com/MLR/C109).
We have provided our updated ICD diagnosis code lists for the FCI herein (Table 1), which can be modified as needed. Further details, including decision rules and rationale guiding code inclusion/exclusion, are provided for transparency (see Supplemental Table S2, Supplemental Digital Content 1, http://links.lww.com/MLR/C109). Stata code for calculating FCI from ICD diagnoses is available from the first author on request.
TABLE 1.
ICD-9-CM and ICD-10-CM Diagnosis Code Lists for the Functional Comorbidity Index (FCI)
| FCI comorbidity | ICD-9-CM | ICD-10-CM |
|---|---|---|
| Arthritis (rheumatoid and osteoarthritis) | 714.×, 715.× | M05.×, M06.×, M08.0×, M08.2×, M08.3, M08.4×, M08.8×, M08.9×, M12.0×, M15.×, M16.×, M17.×, M18.×, M19.× |
| Osteoporosis | 733.0× | M80.×, M81.× |
| Asthma | 493.× | J45.× |
| Chronic respiratory disease (chronic obstructive pulmonary disease, chronic respiratory distress, or emphysema) | 491.2×, 492.×, 494.×, 495.×, 496, 500, 501, 502, 503, 504, 505, 506.4, 508.1, 518.83, 518.84 | J43.×, J44.×, J47.×, J60, J61, J62.×, J63.×, J64, J65, J66.×, J67.×, J68.4, J70.1, J96.1×, J96.2× |
| Angina | 413.× | I20.1, I20.8, I20.9 |
| Congestive heart failure or heart disease | 398.91, 411.×, 414.×, 428.× | I09.81, I24.×, I25.1×, I25.3, I25.4×, I25.5, I25.6, I25.7×, I25.8×, I25.9, I50.× |
| Myocardial infarction (heart attack) | 410.×, 412 | I21.×, I22.×, I25.2 |
| Neurological disease | 330.9, 331.0, 331.1×, 331.2, 331.6, 331.82, 331.83, 331.89, 331.9, 332.×, 333.4, 333.5, 333.71, 333.92, 334.×, 335.×, 340, 341.×, 342.×, 343.×, 344.0×, 344.1, 344.2, 344.3×, 344.4×, 344.5, 344.8×, 344.9, 345.×, 348.1 | G04.1, G10, G11.×, G12.×, G20, G21.×, G25.4, G25.5, G30.×, G31.0×, G31.1, G31.83, G31.84, G31.85, G31.89, G31.9, G32.81, G35, G36.×, G37.×, G40.×, G80.×, G81.×, G82.×, G83.0, G83.1×, G83.2×, G83.3×, G83.5, G83.8×, G83.9, G93.1 |
| Stroke or transient ischemic attack | 430, 431, 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91, 435.×, 438.× | G45.0, G45.1, G45.2, G45.8, G45.9, G46.0, G46.1, G46.2, I60.×, I61.×, I63.×, I67.84×, I69.× |
| Peripheral vascular disease | 440.2×, 440.3×, 440.4, 443.9× | I70.2×, I70.3×, I70.4×, I70.5×, I70.6×, I70.7×, I70.92, I73.9 |
| Diabetes (type I or II) | 249.×, 250.× | E08.×, E09.×, E10.×, E11.×, E13.× |
| Upper gastrointestinal disease | 530.1×, 530.2×, 530.81, 530.85, 531.×, 532.×, 533.×, 534.×, 535.× | K20.×, K21.×, K22.1×, K22.7×, K25.×, K26.×, K27.×, K28.×, K29.× |
| Depression | 296.2×, 296.3×, 296.4×, 296.5×, 296.6×, 296.7×, 296.8×, 296.9×, 298.0, 300.4, 301.10, 301.12, 301.13, 311 | F31.×, F32.×, F33.×, F34.×, F39 |
| An×iety or panic disorder | 300.0×, 300.2×, 300.3, 309.81 | F40.×, F41.×, F42.×, F43.1× |
| Visual impairment | 369.× | H54.× |
| Hearing impairment | 388.01, 388.1×, 388.2, 389.× | H83.3×, H90.×, H91.× |
| Back disease (degenerative disc disease, spinal stenosis, or severe chronic back pain) | 720.0, 721.2, 721.3, 721.4×, 721.9×, 722.1×, 722.2, 722.3×, 722.5×, 722.6, 722.70, 722.72, 722.73, 722.80, 722.82, 722.83, 722.90, 722.92, 722.93, 724.0×, 724.3, 724.4 | M08.1, M45.0, M45.4, M45.5, M45.6, M45.7, M45.8, M45.9, M46.4×, M47.10, M47.14, M47.15, M47.16, M47.20, M47.24, M47.25, M47.26, M47.27, M47.28, M47.814, M47.815, M47.816, M47.817, M47.818, M47.819, M47.894, M47.895, M47.896, M47.897, M47.898, M47.899, M47.9, M48.00, M48.04, M48.05, M48.06, M48.07, M48.08, M51.×, M54.14, M54.15, M54.16, M54.17, M54.3×, M54.4×, M96.1 |
| Obesity (body mass index ≥ 30) | 278.00, 278.01, 278.03, V85.3×, V85.4× | E66.0×, E66.1, E66.2, E66.8, E66.9, Z68.3×, Z68.4× |
FCI indicates Functional Comorbidity Index; ICD, International Classification of Diseases.
Outcome Measures
The SID do not contain the type of long-term functional outcomes that the FCI was developed to predict. However, the FCI has already been well-validated in that respect.3, 10, 15, 16, 23 For purposes of assessing criterion validity spanning the ICD lexicon change, length of stay and discharge disposition were used as proxies for short-term functional status. Though limited, there is some evidence of association between functional status and these short-term outcomes. Need for functional assistance is associated with prolonged length of stay (measured as >7 days in one study,32 and ≥90 days in another33). Lower inpatient mobility was associated with three-fold higher odds of a non-routine (vs. routine) discharge in a single-hospital study (adjusted OR: 3.1; 95% CI: 2.8 to 3.6),34 and greater loss of function (based on severity of illness subclasses) was strongly and monotonically associated with the same outcome in a national study.35
HCUP calculates and cleans the length of stay uniform variable (LOS), which is generally based on subtracting the admission date from the discharge date. Length of stay was missing for 0.004% of hospital discharges in our sample.
HCUP also calculates and cleans the discharge disposition uniform variable (DISPUNIFORM). We converted this categorical variable to a binary indicator for routine discharge (discharged to home, self-care, or court/law enforcement), vs all other discharges (including transfers to short-term hospitals, skilled nursing facilities, home health care, hospice, discharges against medical advice, and deaths). The DISPUNIFORM categories for missing, invalid, or destination unknown were converted to missing values. The resulting routine discharge indicator was missing for 0.104% of hospital discharges in our sample.
Analytic Methods
FCI frequency distributions were compared descriptively, by ICD lexicon, calendar quarter (ICD-9-CM during quarters 1–3, and ICD-10-CM during quarter 4), gender, age, and state. Frequencies for individual comorbidities were also compared descriptively by calendar quarter and ICD lexicon. Criterion validity across the two ICD lexicons was assessed using regression models with robust variance estimates—gamma-log regression (generalized linear models with gamma family and log link to account for right skew36) for the length of stay outcome regressed on FCI, and logistic regression for the routine discharge outcome regressed on FCI. Covariates for each regression model included age category, gender, state fixed effects, an indicator for ICD lexicon, and a term for the interaction between ICD lexicon and FCI. We used a standard two-sided alpha of 0.05; however, our main focus was on effect size, since the large sample size (over 5 million hospitalizations) would likely assure statistical significance of unimportant differences. All analyses were conducted using Stata/MP 15.1 for Windows (College Station, Texas).37
RESULTS
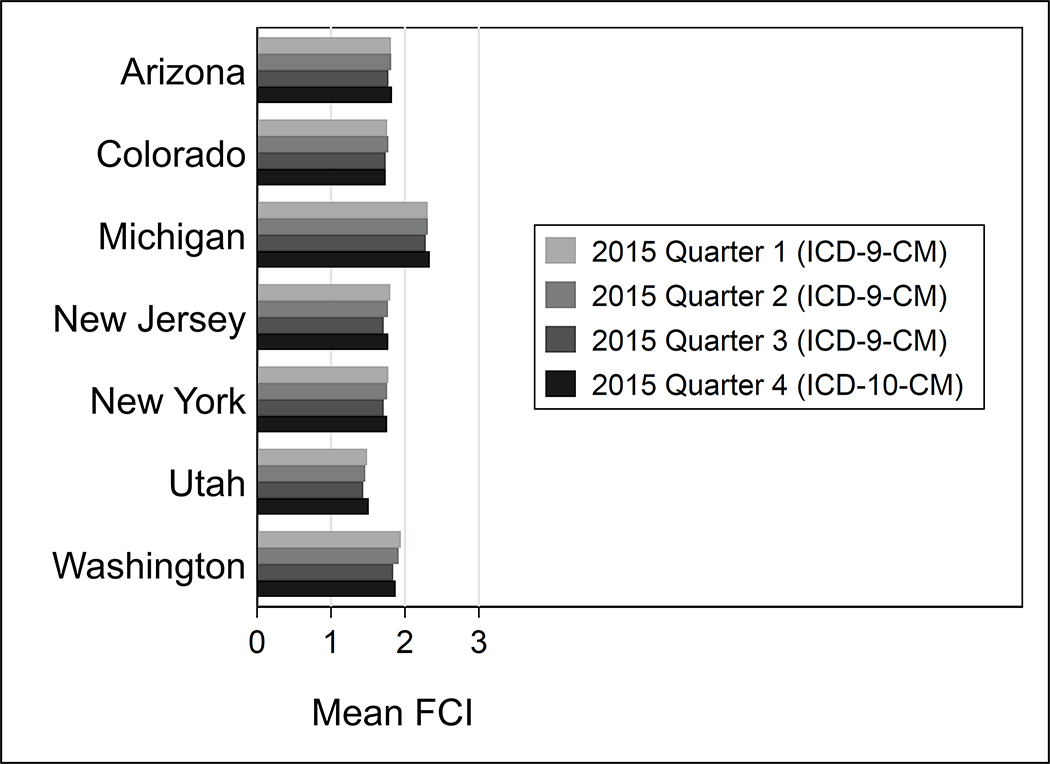
Averaged across the 7 states, women accounted for 57.53% of the sample. Mean age was 57.40 years (SD 20.77), and median age was 59. Although there is some variation across states in FCI distribution (Table 2), there was general consistency across ICD lexicon and calendar quarter. As age category increased, there was a nearly monotonic increase in mean FCI. When broken out by state, the general consistency in FCI distribution across ICD lexicon and calendar quarter remained evident (Figure 1; also see Supplemental Table S3 for means and standard deviations by state and quarter, Supplemental Digital Content 1, http://links.lww.com/MLR/C109).
TABLE 2.
FCI Distribution by ICD Lexicon, Calendar Quarter (2015), Gender, Age, and State
| Variable | N | Maximum* | Median (IQR) | Mean (SD) |
|---|---|---|---|---|
| Overall | 5,644,720 | 13 | 2 (3) | 1.87 (1.66) |
| Lexicon | ||||
| ICD-9-CM | 4,239,818 | 13 | 2 (3) | 1.87 (1.66) |
| ICD-10-CM | 1,404,902 | 13 | 2 (3) | 1.88 (1.68) |
| Calendar quarter | ||||
| 2015 Q1 | 1,405,729 | 13 | 2 (2) | 1.89 (1.65) |
| 2015 Q2 | 1,424,145 | 12 | 2 (3) | 1.88 (1.66) |
| 2015 Q3 | 1,409,944 | 13 | 2 (3) | 1.83 (1.65) |
| 2015 Q4 | 1,404,902 | 13 | 2 (3) | 1.88 (1.68) |
| Gender | ||||
| Male | 2,337,089 | 13 | 2 (2) | 2.00 (1.58) |
| Female | 3,247,413 | 13 | 1 (3) | 1.77 (1.72) |
| Age | ||||
| 18–24 | 353,770 | 10 | 0 (1) | 0.62 (0.92) |
| 25–34 | 771,877 | 10 | 0 (1) | 0.63 (1.00) |
| 35–44 | 552,359 | 11 | 1 (2) | 1.17 (1.35) |
| 45–54 | 690,842 | 12 | 2 (2) | 1.86 (1.57) |
| 55–64 | 933,617 | 12 | 2 (2) | 2.22 (1.66) |
| 65–74 | 971,355 | 13 | 2 (3) | 2.49 (1.68) |
| 75–84 | 807,083 | 12 | 2 (3) | 2.55 (1.62) |
| 85+ | 563,817 | 12 | 2 (2) | 2.41 (1.55) |
| State | ||||
| Arizona | 616,399 | 11 | 2 (3) | 1.81 (1.61) |
| Colorado | 391,069 | 12 | 1 (3) | 1.75 (1.65) |
| Michigan | 1,074,377 | 13 | 2 (2) | 2.31 (1.83) |
| New Jersey | 844,415 | 12 | 2 (3) | 1.76 (1.58) |
| New York | 1,966,178 | 13 | 1 (3) | 1.75 (1.58) |
| Utah | 216,037 | 10 | 1 (2) | 1.47 (1.44) |
| Washington | 536,245 | 12 | 2 (3) | 1.89 (1.70) |
Minimum FCI value uniformly 0
FCI indicates Functional Comorbidity Index; ICD, International Classification of Diseases; IQR, interquartile range; Q, quarter, SD, standard deviation.
FIGURE 1.
Mean Functional Comorbidity Index (FCI) by State, Calendar Quarter (2015), and International Classification of Diseases Lexicon (ICD-9-CM vs. ICD-10-CM)
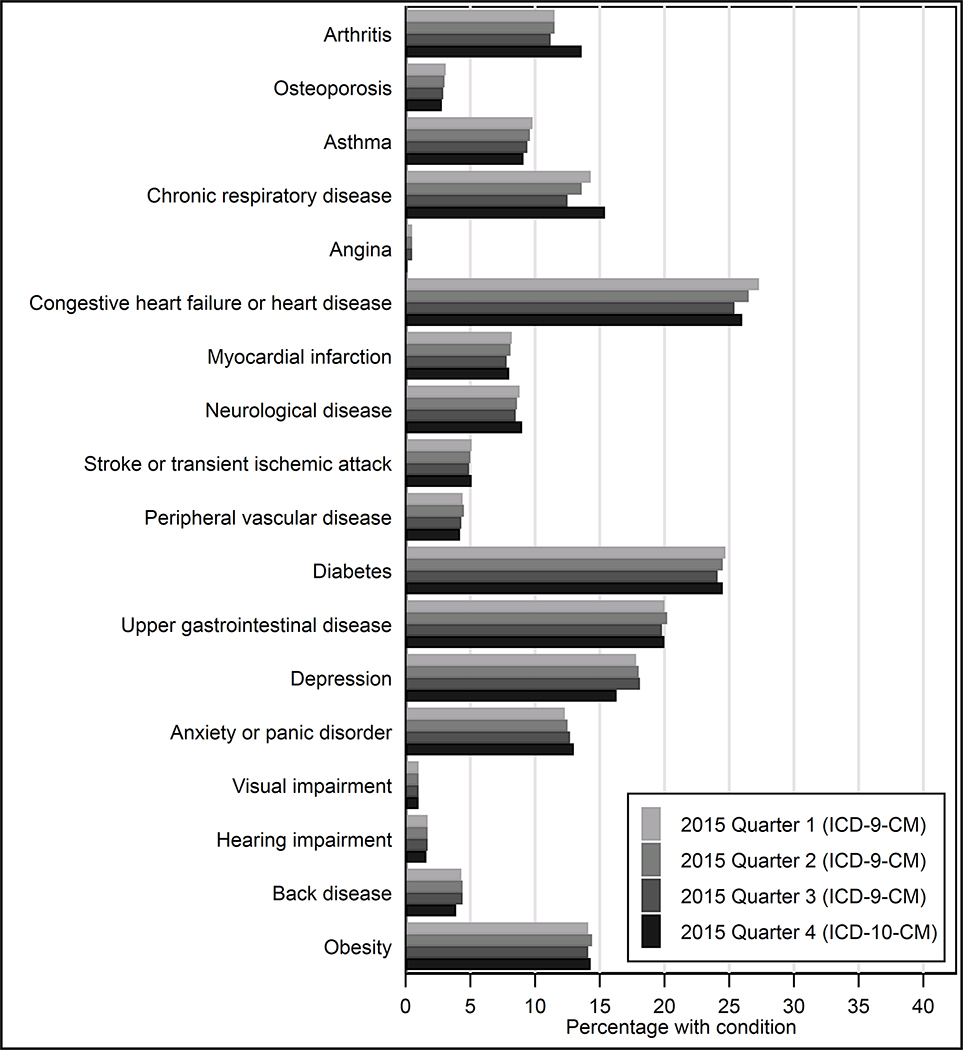
The general consistency in FCI distribution across ICD lexicon and calendar quarter remained evident at the individual comorbidity level, with a few minor exceptions (Figure 2; also see Supplemental Table S4 for individual comorbidity frequencies by quarter, Supplemental Digital Content 1, http://links.lww.com/MLR/C109). Five of the 18 comorbidities had small (1 to 2 percentage point) discrepancies in prevalence across lexicons. The direction was inconsistent, with angina, depression, and back disease slightly more prevalent under ICD-9-CM, while arthritis and chronic respiratory disease were slightly more prevalent under ICD-10-CM.
FIGURE 2.
Functional Comorbidity Index (FCI) Individual Comorbidity Frequencies by Calendar Quarter (2015) and International Classification of Diseases Lexicon (ICD-9-CM vs. ICD-10-CM)
Regression results are shown in Table 3. Length of stay was highly skewed, ranging from 0 to 365, with a median of 3, and mean of 5.10 (SD 7.21); interquartile range was 3 (3 to 6), and the 99th percentile was 31. For regression models with length of stay as the outcome (generalized linear models with gamma family and log link), R2 went from 0.017 without FCI to 0.023 with FCI included. Discharge disposition was routine for 64.72% of the regression sample (3,611,301/5,580,053). For logistic regression models with discharge disposition as the outcome, pseudo R2 went from 0.153 without FCI to 0.167 with FCI included. For both outcomes, the same R2 values were observed whether or not ICD lexicon-related parameters were included in the models.
TABLE 3.
Regression Results: Length of Stay and Routine Discharge Outcomes
| Variable | Length of stay (days), gamma-log
regression*
(N=5,584,284) |
Routine discharge, logistic
regression (N=5,580,053) |
||
|---|---|---|---|---|
| Exp(β) | 95% CI | OR | 95% CI | |
| FCI (continuous comorbidity count) | 1.089 | 1.088 to 1.089 | 0.815 | 0.813 to 0.816 |
| ICD-10-CM lexicon (base: ICD-9-CM) | 1.003 | 0.999 to 1.007 | 0.977 | 0.970 to 0.985 |
| Interaction term: FCI × ICD lexicon | 0.995 | 0.994 to 0.997 | 1.013 | 1.011 to 1.016 |
| Female (base: male) | 0.843 | 0.841 to 0.845 | 1.082 | 1.078 to 1.087 |
| Age (base: 18–24) | ||||
| 25–34 | 0.947 | 0.941 to 0.953 | 1.043 | 1.029 to 1.058 |
| 35–44 | 1.048 | 1.041 to 1.055 | 0.669 | 0.660 to 0.679 |
| 45–54 | 1.150 | 1.143 to 1.157 | 0.396 | 0.391 to 0.401 |
| 55–64 | 1.187 | 1.180 to 1.194 | 0.270 | 0.267 to 0.274 |
| 65–74 | 1.185 | 1.178 to 1.192 | 0.180 | 0.178 to 0.183 |
| 75–84 | 1.213 | 1.206 to 1.220 | 0.109 | 0.108 to 0.111 |
| 85+ | 1.204 | 1.197 to 1.211 | 0.054 | 0.054 to 0.055 |
| State (base: Arizona) | ||||
| Colorado | 0.928 | 0.923 to 0.933 | 0.815 | 0.808 to 0.823 |
| Michigan | 0.934 | 0.931 to 0.938 | 0.739 | 0.733 to 0.744 |
| New Jersey | 1.067 | 1.062 to 1.071 | 0.746 | 0.740 to 0.752 |
| New York | 1.192 | 1.187 to 1.196 | 0.668 | 0.663 to 0.673 |
| Utah | 0.881 | 0.873 to 0.889 | 0.682 | 0.673 to 0.691 |
| Washington | 0.940 | 0.935 to 0.945 | 1.157 | 1.146 to 1.167 |
| Intercept | 3.991 | 3.966 to 4.015 | 14.00 | 13.81 to 14.19 |
Generalized linear model with gamma family and log link.
P-values were uniformly P<0.001, with the exception of the P-value for ICD-10-CM lexicon in the length of stay model (P=0.21).
CI indicates confidence interval; Exp(β), exponentiated coefficient; FCI, Functional Comorbidity Index; ICD, International Classification of Diseases; OR, odds ratio.
The FCI/ICD lexicon interaction coefficients were small but statistically significant in both outcome models (Table 3). Under ICD-9-CM, each additional comorbidity was associated with an 8.9% increase in length of stay and an 18.5% decrease in the odds of a routine discharge, compared to an 8.4% increase and 17.4% decrease, respectively, under ICD-10-CM. The inclusion of lexicon-related parameters had negligible effect on explained variance, and the combined (main effect and interaction) lexicon effect size was small relative to the FCI, on the order of a 0.1% decrease in mean length of stay and a 1.0% decrease in the odds of a routine discharge after the lexicon change.
DISCUSSION
This study provides code lists for the FCI that can be used for studies spanning the ICD lexicon change in 2015, or with data sets that include diagnosis codes from both lexicons. Although there were small discrepancies in prevalence across ICD lexicons for a few individual comorbidities, the FCI demonstrated general stability across lexicons. Although there was a statistically significant structural break at lexicon change, the effect size was quite small, and likely ignorable for most purposes. However, if trend analysis were a specific research focus, it might be advisable to include ICD lexicon-related main effect and interaction terms in statistical models in order to adjust for the small structural break. Given the differences in ICD-10-CM with respect to ICD-9-CM, such as conditions being grouped differently, higher granularity, and nearly 5 times as many diagnosis codes,38 it is both fortunate and remarkable that ICD lexicon was not associated with larger discrepancies in FCI.
The FCI was developed and validated based on physical function as the outcome, in contrast to other comorbidity indices based on mortality, and thus includes certain chronic conditions such as arthritis and asthma that are not generally included in other comorbidity indices. Although it has not out-performed other comorbidity indices among inpatients, and is a weak predicter of function among inpatients,11 or readmission,13 it has shown some promise in predicting long-term recovery, function, and health-related quality of life.3, 16 Even so, it is not necessarily a better predictor than the Charlson or Elixhauser comorbidity indices in that role.15 One study among osteoarthritis patients, while finding the FCI to be an important predictor of 5-year health utility, also found that functional impairment did not appear to mediate the association between the FCI and health utility.39 However, the FCI has face validity and criterion validity to support its use when adjustment for comorbidities is desirable, particularly in community-based studies with long-term outcomes related to function or health status. There might be good reason to revisit and potentially adjust some of the categories used for the FCI (e.g., whether to continue to separate angina from the category for congestive heart failure or heart disease), but that issue went beyond the scope of this study.
Limitations
During code list development, certain inclusion/exclusion decisions were arbitrary. We have provided our ICD code lists and decision rules for transparency, which can be modified as needed. These code lists were not designed for surveillance of individual comorbidities across the lexicon change; further adjustments to the code lists might be needed for that purpose, particularly for the categories of arthritis, chronic respiratory disease, angina, depression, and back disease. The SID did not contain longer-term functional measures with which to assess criterion validity; however, the FCI has been previously validated in that regard.3, 10, 15, 16, 23 Given the absence of better alternatives, length of stay and discharge disposition were used as proxies for short-term functional status. Using the binary version of the discharge disposition variable may potentially have masked important variation. The primary goal of this study was to develop diagnosis code lists that could be used across lexicons, and the available shorter-term outcomes served that purpose, despite low explained variance. We encourage further research to validate these FCI diagnosis code lists using long-term functional outcomes. The FCI has been based variously on patient interviews,25 patient questionnaires,24 chart review,23 and diagnoses in administrative data.3, 11, 16 In future research, it would be useful to compare FCI performance across these varying sources.
Conclusions
The FCI ICD-9-CM and ICD-10-CM code lists provided herein can be used for studies spanning the ICD lexicon change in 2015, or with data sets that include diagnosis codes from both lexicons. Using these code lists, the FCI demonstrated general concordance and similar distribution across lexicons, though there were small discrepancies in prevalence of a few individual comorbidities.
Supplementary Material
Funding:
JMS received a research grant from the National Institute for Occupational Safety and Health (NIOSH); award number R21OH011355. The contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50:1109–1118. [DOI] [PubMed] [Google Scholar]
- 2.Yurkovich M, Avina-Zubieta JA, Thomas J, et al. A systematic review identifies valid comorbidity indices derived from administrative health data. J Clin Epidemiol. 2015;68:3–14. [DOI] [PubMed] [Google Scholar]
- 3.Rundell SD, Resnik L, Heagerty PJ, et al. Performance of the Functional Comorbidity Index (FCI) in prognostic models for risk adjustment in patients with back pain. PM R. 2020. [DOI] [PubMed] [Google Scholar]
- 4.Zullig LL, Bosworth HB, Jeffreys AS, et al. The association of comorbid conditions with patient-reported outcomes in veterans with hip and knee osteoarthritis. Clin Rheumatol. 2015;34:1435–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Machlin SR, Soni A. Health care expenditures for adults with multiple treated chronic conditions: estimates from the Medical Expenditure Panel Survey, 2009. Prev Chronic Dis. 2013;10:E63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mnatzaganian G, Ryan P, Hiller JE. Does co-morbidity provide significant improvement on age adjustment when predicting medical outcomes? Methods Inf Med. 2014;53:115–120. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 8.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 9.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 10.Groll DL, To T, Bombardier C, et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58:595–602. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A, Graham JE, Resnik L, et al. Examining the association between comorbidity indexes and functional status in hospitalized Medicare fee-for-service beneficiaries. Phys Ther. 2016;96:232–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar A, Graham JE, Resnik L, et al. Comparing comorbidity indices to predict post-acute rehabilitation outcomes in older adults. Am J Phys Med Rehabil. 2016;95:889–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar A, Karmarkar AM, Graham JE, et al. Comorbidity indices versus function as potential predictors of 30-day readmission in older patients following postacute rehabilitation. J Gerontol A Biol Sci Med Sci. 2017;72:223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marcum JL, McHugh A, Foley M, et al. The economic effect of chronic comorbidities in carpal tunnel syndrome workers’ compensation claimants, Washington State. J Occup Environ Med. 2018;60:1128–1135. [DOI] [PubMed] [Google Scholar]
- 15.Rundell SD, Resnik L, Heagerty PJ, et al. Comparing performance of comorbidity indices in predicting functional status, health-related quality of life, and total health care use in older adults with back pain. J Orthop Sports Phys Ther. 2019:1–18. [DOI] [PubMed] [Google Scholar]
- 16.Gabbe BJ, Harrison JE, Lyons RA, et al. Comparison of measures of comorbidity for predicting disability 12-months post-injury. BMC Health Serv Res. 2013;13:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.HCUP State Inpatient Databases (SID). Healthcare Cost and Utilization Project (HCUP). 2010–2014. Available at: www.hcup-us.ahrq.gov/sidoverview.jsp. Accessed March 12, 2020.
- 18.National Center for Health Statistics. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Available at: https://www.cdc.gov/nchs/icd/icd10cm.htm. Accessed March 12, 2020. [PubMed]
- 19.Horn SD, Sharkey PD, Buckle JM, et al. The relationship between severity of illness and hospital length of stay and mortality. Med Care. 1991;29:305–317. [DOI] [PubMed] [Google Scholar]
- 20.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25:119–141. [PMC free article] [PubMed] [Google Scholar]
- 21.Resnik L, Gozalo P, Hart DL. Weighted index explained more variance in physical function than an additively scored functional comorbidity scale. J Clin Epidemiol. 2011;64:320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kabboord AD, van Eijk M, van Dingenen L, et al. Reliability and usability of a weighted version of the Functional Comorbidity Index. Clin Interv Aging. 2019;14:289–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Groll DL, Heyland DK, Caeser M, et al. Assessment of long-term physical function in acute respiratory distress syndrome (ARDS) patients: comparison of the Charlson Comorbidity Index and the Functional Comorbidity Index. Am J Phys Med Rehabil. 2006;85:574–581. [DOI] [PubMed] [Google Scholar]
- 24.Hoang-Kim A, Busse JW, Groll D, et al. Co-morbidities in elderly patients with hip fracture: recommendations of the ISFR-IOF hip fracture outcomes working group. Arch Orthop Trauma Surg. 2014;134:189–195. [DOI] [PubMed] [Google Scholar]
- 25.Parry M, Arthur H, Brooks D, et al. Measuring function in older adults with co-morbid illnesses who are undergoing coronary artery bypass graft (CABG) surgery. Arch Gerontol Geriatr. 2012;54:477–483. [DOI] [PubMed] [Google Scholar]
- 26.Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buck CJ. ICD-9-CM Volumes 1, 2, & 3 for Hospitals, Professional Edition. St. Louis, MO: Elsevier; 2011. [Google Scholar]
- 28.American Medical Association. ICD-10-CM Mappings: Linking ICD-9-CM to All Valid ICD-10-CM Alternatives. USA: Optum360, LLC; 2016. [Google Scholar]
- 29.American Medical Association. The Complete Official Codebook: ICD-10-CM. USA: Optum360, LLC; 2016. [Google Scholar]
- 30.American Academy of Professional Coders. Online ICD Code Translator Tool. Available at: https://www.aapc.com/icd-10/codes/. Accessed February 28, 2020.
- 31.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–363. [PubMed] [Google Scholar]
- 32.Huggan PJ, Akram F, Er BH, et al. Measures of acute physiology, comorbidity and functional status to differentiate illness severity and length of stay among acute general medical admissions: a prospective cohort study. Intern Med J. 2015;45:732–740. [DOI] [PubMed] [Google Scholar]
- 33.Kerminen H, Huhtala H, Jantti P, et al. Frailty Index and functional level upon admission predict hospital outcomes: an interRAI-based cohort study of older patients in post-acute care hospitals. BMC Geriatr. 2020;20:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoyer EH, Young DL, Friedman LA, et al. Routine inpatient mobility assessment and hospital discharge planning. JAMA Intern Med. 2019;179:118–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sonig A, Lin N, Krishna C, et al. Impact of transfer status on hospitalization cost and discharge disposition for acute ischemic stroke across the US. J Neurosurg. 2016;124:1228–1237. [DOI] [PubMed] [Google Scholar]
- 36.Moran JL, Solomon PJ, Peisach AR, et al. New models for old questions: generalized linear models for cost prediction. J Eval Clin Pract. 2007;13:381–389. [DOI] [PubMed] [Google Scholar]
- 37.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 38.National Center for Health Statistics. International Classification of Diseases, (ICD-10-CM/PCS) Transition - Background. November 6, 2015. Available at: http://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm. Accessed March 12, 2020.
- 39.Omorou AY, Achit H, Wieczorek M, et al. Impact of comorbidities and functional impairment on 5-year loss of health utility in patients with lower-limb osteoarthritis in the KHOALA cohort. Qual Life Res. 2019;28:3047–3054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.